User:BMacapinlacG13/sandbox
 | |
| Clinical data | |
|---|---|
| Trade names | various |
| License data | |
| Routes of administration | Oral, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 35.1% |
| Metabolism | Hepatic |
| Elimination half-life | 2.8-7.4 hours |
| Excretion | Renal: 11% |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
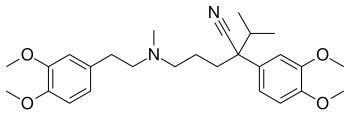
| Formula | C27H38N2O4 |
| Molar mass | 454.602 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Verapamil (INN) (/vɜːrˈæpəmɪl/) (sold under various trade names) is an L-type calcium channel blocker of the phenylalkylamine class. It has been used in the treatment of hypertension, angina pectoris, cardiac arrhythmia, and most recently, cluster headaches.[1][2] It is also an effective preventive medication for migraine.[3]
It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[4]
Medical uses
Verapamil is also used intra-arterially to treat cerebral vasospasm.[5] Verapamil has been used to treat cluster headaches,[6] but it can also cause headaches as a side effect.
It is a class-IV antiarrhythmic, and was approved by the U.S. Food and Drug Administration (FDA) in March 1982.[7]
Use of verapamil is to be avoided in patients with severe left ventricular dysfunction, hypotension (systolic pressure less than 90 mm Hg), cardiogenic shock, and hypersensitivity to verapamil.[8]
Side effects
Some possible side effects of the drug are headaches, facial flushing, dizziness, lightheadedness, swelling, increased urination, fatigue, nausea, ecchymosis, galactorrhea, and constipation.[9][10]

Along with other calcium channel blockers, verapamil is known to induce gingival hyperplasia. [11]
Overdose
Acute overdose is often manifested by nausea, asthenia, bradycardia, dizziness, hypotension, and cardiac arrhythmia. Plasma, serum, or blood concentrations of verapamil and norverapamil, its major active metabolite, may be measured to confirm a diagnosis of poisoning in hospitalized patients or to aid in the medicolegal investigation of fatalities. Blood or plasma verapamil concentrations are usually in a range of 50-500 μg/l in persons on therapy with the drug, but may rise to 1–4 mg/l in acute overdose patients and are often at levels of 5–10 mg/l in fatal poisonings.[12][13]
Mechanism of action
Verapamil's mechanism in all cases is to block voltage-dependent calcium channels. In cardiac pharmacology, calcium channel blockers are considered class-IV antiarrhythmic agents. Since calcium channels are especially concentrated in the sinoatrial and atrioventricular nodes, these agents can be used to decrease impulse conduction through the AV node, thus protecting the ventricles from atrial tachyarrhythmias.
Calcium channels are also present in the smooth muscle lining blood vessels. By relaxing the tone of this smooth muscle, calcium channel blockers dilate the blood vessels. This has led to their use in treating high blood pressure and angina pectoris. The pain of angina is caused by a deficit in oxygen supply to the heart. Calcium channel blockers like verapamil dilate blood vessels, which increases the supply of blood and oxygen to the heart. This controls chest pain, but only when used regularly. It does not stop chest pain once it starts. A more powerful vasodilator such as nitroglycerin may be needed to control pain once it starts.
Pharmacokinetic details
More than 90% of verapmil is absorbed when given orally,[14] but due to high first-pass metabolism, bioavailability is much lower (10–35%). It is 90% bound to plasma proteins and has a volume of distribution of 3–5 l/kg. It takes 1 to 2 hours to reach peak plasma concentration after oral administration.[15] It is metabolized in the liver to at least 12 inactive metabolites (though one metabolite, norverapamil, retains 20% of the vasodilating activity of the parent drug). As its metabolites, 70% is excreted in the urine and 16% in feces; 3–4% is excreted unchanged in urine. This is a nonlinear dependence between plasma concentration and dosage. Onset of action is 1–2 hours after oral dosage. Half-life is 5–12 hours (with chronic dosages). It is not cleared by hemodialysis. It is excreted in human milk. Because of the potential for adverse reaction in nursing infants, nursing should be discontinued while verapamil is administered.
Verapamil has been reported to be effective in both short-term[16] and long-term treatment of mania and hypomania.[17] Addition of magnesium oxide to the verapamil treatment protocol enhances the antimanic effect.[18] It has on occasion been used to control mania in pregnant patients, especially in the first three months. It does not appear to be significantly teratogenic. For this reason, when one wants to avoid taking valproic acid (which is high in teratogenicity) or lithium (which has a small but significant incidence of causing cardiac malformation), verapamil is usable as an alternative, albeit presumably a less effective one.
Veterinary use
Intra-abdominal adhesions are common in rabbits following surgery. Verapamil can be given postoperatively in rabbits which have suffered trauma to abdominal organs to prevent formation of these adhesions.[19][20][21] Such effect was not documented in another study with ponies.[22]
Uses in cell biology
Verapamil is also used in cell biology as an inhibitor of drug efflux pump proteins such as P-glycoprotein.[23] This is useful, as many tumor cell lines overexpress drug efflux pumps, limiting the effectiveness of cytotoxic drugs or fluorescent tags. It is also used in fluorescent cell sorting for DNA content, as it blocks efflux of a variety of DNA-binding fluorophores such as Hoechst 33342. Radioactively labelled verapamil and positron emission tomography can be used with to measure P-glycoprotein function.[24]
Research
Verapamil is being studied for diabetes in animal models. Human trials are expected to begin in 2015.
Trade names
Trade names for verapamil include Isoptin, Verelan, Verelan PM, Calan, Bosoptin, Calaptin, Verogalid ER and Covera-HS.
See also
References
- ^ Koda-Kimble and Young's Applied Therapeutics: The Clinical Use of Drugs. USA: LWW; Tenth, North American Edition edition. 2012. pp. 320–322. ISBN 978-1609137137.
- ^ "Management of Cluster Headache - American Family Physician". www.aafp.org. Retrieved 4 November 2015.
- ^ Koda-Kimble and Young's Applied Therapeutics: The Clinical Use of Drugs. USA: LWW; Tenth, North American Edition edition. 2012. p. 1340. ISBN 978-1609137137.
- ^ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ^ Jun, P.; Ko, N. U.; English, J. D.; Dowd, C. F.; Halbach, V. V.; Higashida, R. T.; Lawton, M. T.; Hetts, S. W. (2010). "Endovascular Treatment of Medically Refractory Cerebral Vasospasm Following Aneurysmal Subarachnoid Hemorrhage". American Journal of Neuroradiology. 31 (10): 1911–6. doi:10.3174/ajnr.A2183. PMC 4067264. PMID 20616179.
- ^ Drislane, Frank; Benatar, Michael; Chang, Bernard S.; Acosta, Juan; Tarulli, Andrew (1 January 2009). Blueprints Neurology. Lippincott Williams & Wilkins. pp. 71–. ISBN 978-0-7817-9685-9. Retrieved 14 November 2010.
- ^ "verapamil, Calan, Verelan, Verelan PM, Isoptin, Covera-HS". MedicineNet.com. Retrieved 6 October 2011.
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/018817s021lbl.pdf.
{{cite web}}: Missing or empty|title=(help) - ^ "Verapamil". PubMed Health. Retrieved 10 January 2012.
- ^ "verapamil, Calan, Verelan, Verelan PM, Isoptin, Covera-HS (cont.)". MedicineNet.com. Retrieved 10 January 2012.
- ^ Steele, RM; Schuna, AA; Schreiber, RT (1994). "Calcium antagonist-induced gingival hyperplasia". Annals of Internal Medicine. 120 (8): 663–4. doi:10.7326/0003-4819-120-8-199404150-00006. PMID 8135450. S2CID 41746099.
- ^ Wilimowska, Jolanta; Piekoszewski, Wojciech; Krzyanowska-Kierepka, Ewa; Florek, Ewa (2006). "Monitoring of Verapamil Enantiomers Concentration in Overdose". Clinical Toxicology. 44 (2): 169–71. doi:10.1080/15563650500514541. PMID 16615674. S2CID 10351499.
- ^ Baselt, R. (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, California: Biomedical Publications. pp. 1637–9.
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/018817s021lbl.pdf.
{{cite web}}: Missing or empty|title=(help) - ^ http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/018817s021lbl.pdf.
{{cite web}}: Missing or empty|title=(help) - ^ Giannini, AJ; Houser Jr, WL; Loiselle, RH; Giannini, MC; Price, WA (1984). "Antimanic effects of verapamil". The American Journal of Psychiatry. 141 (12): 1602–3. doi:10.1176/ajp.141.12.1602. PMID 6439057.
- ^ Giannini, AJ; Taraszewski, R; Loiselle, RH (1987). "Verapamil and lithium in maintenance therapy of manic patients". Journal of Clinical Pharmacology. 27 (12): 980–2. doi:10.1002/j.1552-4604.1987.tb05600.x. PMID 3325531. S2CID 34536914.
- ^ Giannini, A.James; Nakoneczie, Ann M.; Melemis, Stephen M.; Ventresco, James; Condon, Maggie (2000). "Magnesium oxide augmentation of verapamil maintenance therapy in mania". Psychiatry Research. 93 (1): 83–7. doi:10.1016/S0165-1781(99)00116-X. PMID 10699232. S2CID 18216795.
- ^ Elferink, Jan G.R.; Deierkauf, Martha (1984). "The effect of verapamil and other calcium antagonists on chemotaxis of polymorphonuclear leukocytes". Biochemical Pharmacology. 33 (1): 35–9. doi:10.1016/0006-2952(84)90367-8. PMID 6704142.
- ^ Azzarone, Bruno; Krief, Patricia; Soria, Jeannette; Boucheix, Claude (1985). "Modulation of fibroblast-induced clot retraction by calcium channel blocking drugs and the monoclonal antibody ALB6". Journal of Cellular Physiology. 125 (3): 420–6. doi:10.1002/jcp.1041250309. PMID 3864783. S2CID 10911875.
- ^ Steinleitner, Alex; Lambert, Hovey; Kazensky, Carol; Sanchez, Ignacio; Sueldo, Carlos (1990). "Reduction of primary postoperative adhesion formation under calcium channel blockade in the rabbit". Journal of Surgical Research. 48 (1): 42–5. doi:10.1016/0022-4804(90)90143-P. PMID 2296179.
- ^ Baxter, Gary M.; Jackman, Bradley R.; Eades, Susan C.; Tyler, David E. (1993). "Failure of Calcium Channel Blockade to Prevent Intra-abdominal Adhesions in Ponies". Veterinary Surgery. 22 (6): 496–500. doi:10.1111/j.1532-950X.1993.tb00427.x. PMID 8116206.
- ^ Bellamy, W T (1996). "P-Glycoproteins and Multidrug Resistance". Annual Review of Pharmacology and Toxicology. 36: 161–83. doi:10.1146/annurev.pa.36.040196.001113. PMID 8725386.
- ^ Luurtsema, Gert; Windhorst, Albert D.; Mooijer, Martien P.J.; Herscheid, Jacobus D.M.; Lammertsma, Adriaan A.; Franssen, Eric J.F. (2002). "Fully automated high yield synthesis of (R)- and (S)-[11C]verapamil for measuring P-glycoprotein function with positron emission tomography". Journal of Labelled Compounds and Radiopharmaceuticals. 45 (14): 1199–207. doi:10.1002/jlcr.632.
External links
Category:Antiarrhythmic agents Category:Calcium channel blockers Category:Nitriles Category:Phenol ethers Category:World Health Organization essential medicines Category:Glycine receptor antagonists