Bumetanide
 | |
 | |
| Names | |
|---|---|
| Trade names | Bumex, Burinex, others |
| |
| Clinical data | |
| Drug class | Loop diuretic[1] |
| Main uses | Swelling, high blood pressure[1] |
| Side effects | Dizziness, low blood pressure, low blood potassium, muscle cramps, kidney problems[1] |
| Pregnancy category |
|
| Routes of use | By mouth, intravenous, intramuscular |
| Defined daily dose | 1 mg[2] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684051 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | Almost complete (~80%) |
| Protein binding | 97% |
| Metabolism | Liver |
| Elimination half-life | ~0.8 hours |
| Excretion | Kidney |
| Chemical and physical data | |
| Formula | C17H20N2O5S |
| Molar mass | 364.42 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Bumetanide, sold under the trade name Bumex among others, is a medication used to treat swelling and high blood pressure.[1] This includes swelling as a result of heart failure, liver failure, or kidney problems.[1] It may work for swelling when other medications have not.[1] For high blood pressure it is not a preferred treatment.[1] It is taken by mouth, or by injection into a vein or muscle.[1] Effects generally begin within an hour and lasts for about six hours.[1]
Common side effects include dizziness, low blood pressure, low blood potassium, muscle cramps, and kidney problems.[1] Other serious side effects may include hearing loss and low blood platelets.[1] People with a sulfa allergy, may also be allergic to bumetanide.[1] Blood tests are recommended regularly for those on treatment.[1] Safety during pregnancy and breastfeeding is unclear.[3] Bumetanide is a loop diuretic and works by decreasing the reabsorption of sodium by the kidneys.[4][1]
Bumetanide was patented in 1968 and came into medical use in 1972.[5] It is on the World Health Organization's List of Essential Medicines as an alternative to furosemide.[6] It is available as a generic medication.[4] A month supply in the United Kingdom costs the NHS about £1.20 as of 2019.[4] In the United States the wholesale cost of this amount is about US$12.[7] In 2017, it was the 277th most commonly prescribed medication in the United States, with more than one million prescriptions.[8][9]
Uses
Medical uses
It used to treat swelling and high blood pressure.[1] This include swelling as a result of heart failure, liver failure, or kidney problems.[1] For high blood pressure it is not a preferred treatment.[1] It is taken by mouth, or by injection into a vein or muscle.[1]
Dosage
The defined daily dose is 1 mg by mouth or by injection.[2]
Side effects
Common side effects include dizziness, low blood pressure, low blood potassium, muscle cramps, and kidney problems.[1] Other serious side effects may include hearing loss and low blood platelets.[1] People with a sulfa allergy may also be allergic to bumetanide.[1] Blood tests are recommended regularly for those on treatment.[1] Safety during pregnancy and breastfeeding is unclear.[3]
Mechanism of action
Bumetanide is a loop diuretic and works by decreasing the reabsorption of sodium by the kidneys. The main difference between bumetanide and furosemide is in their bioavailability and potency. About 60% of furosemide is absorbed in the intestine, and there are substantial inter- and intraindividual differences in bioavailability (range 10-90%). About 80% of bumetanide is absorbed, and its absorption does not change when it is taken with food. It is said to be a more predictable diuretic, meaning that the predictable absorption is reflected in a more predictable effect.[10] Bumetanide is 40 times more potent than furosemide for people with normal renal function.[10]
Chemistry
Synthesis
Bumetanide, 3-butylamino-4-phenoxy-5-sulfamoylbenzoic acid, is synthesized from 4-chlorobenzoic acid. In the first stage of synthesis, it undergoes sulfonylchlorination by chlorosulfonic acid, forming 4-chloro-3-chlorosulfonylbenzoic acid, which is further nitrated with nitric acid to 4-chloro-3-chlorosulfonyl-5-nitrobenzoic acid. Reacting this with ammonia gives 5-aminosulfonyl-4-chloro-3-nitrobenzoic acid, which when reacted with sodium phenolate is transformed into 5-amino-sulfonyl-3-nitro-5-phenoxybenzoid acid. Reduction of the nitro group in this product by hydrogen using a palladium on carbon catalyst gives 3-amino-5-aminosulfonyl- 5-phenoxybenzoic acid. Finally, reacting this with butyl alcohol in the presence of sulfuric acid gives the desired bumetanide.[citation needed]

Society and culture
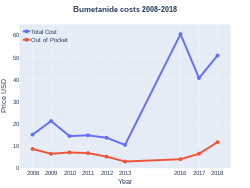
Cost
A month supply in the United Kingdom costs the NHS about £1.20 as of 2019.[4] In the United States the wholesale cost of this amount is about US$12.[7] In 2017, it was the 277th most commonly prescribed medication in the United States, with more than one million prescriptions.[8][9]
-
Bumetanide costs (US)
-
Bumetanide prescriptions (US)
Other uses
It 2008, four NFL players were being suspended under the steroid policy as a result of taking bumetanide.[16] It is sometimes used for weight loss because, as a diuretic, it removes water, but it also masks other drugs, including steroids, by diluting the contents of the user's urine, yielding a lower concentration of filtered substances, which makes them less likely to be detected.
Bumetanide was an undisclosed active ingredient in the over-the-counter weight loss supplement StarCaps, which was removed from the market after its presence was discovered by the United States Food and Drug Administration.[17]
Research
In the brain, bumetanide blocks the NKCC1 cation-chloride co-transporter, and thus decreases internal chloride concentration in neurons. In turn, this concentration change makes the action of GABA more hyperpolarizing, which may be useful for treatment of neonatal seizures, which quite often are not responsive to traditional GABA-targeted treatment, such as barbiturates. Bumetanide is therefore under evaluation as a prospective antiepileptic drug.[18]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 "Bumetanide Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 21 June 2019. Retrieved 8 April 2019.
- ↑ 2.0 2.1 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 21 January 2021. Retrieved 8 September 2020.
- ↑ 3.0 3.1 "Bumetanide (Bumex) Use During Pregnancy". Drugs.com. Archived from the original on 8 April 2019. Retrieved 8 April 2019.
- ↑ 4.0 4.1 4.2 4.3 British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 225–226. ISBN 9780857113382.
- ↑ Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 458. ISBN 9783527607495. Archived from the original on 2019-03-01. Retrieved 2019-03-01.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ↑ 7.0 7.1 "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Archived from the original on 2019-03-06. Retrieved 3 March 2019.
- ↑ 8.0 8.1 "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- ↑ 9.0 9.1 "Bumetanide - Drug Usage Statistics". ClinCalc. Archived from the original on 11 April 2020. Retrieved 11 April 2020.
- ↑ 10.0 10.1 Brunton, Laurence; Lazo, John S.; Parker, Keith L., eds. (2006). Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. pp. 749–753. ISBN 0-07-142280-3.
- ↑ Loevens Kemiske Fabrik Produktionsaktieselskab (Jul 9, 1970). "Neue Sulfamylbenzoesaeurederivate". DPMAregister (in German). Ger. Pat. 19 64 503.5: German Patent and Trade Mark Office. Archived from the original on 29 August 2021. Retrieved 20 June 2018.
{{cite web}}: CS1 maint: location (link) CS1 maint: unrecognized language (link) - ↑ Loevens Kemiske Fabrik Produktionsaktieselskab (Jul 9, 1970). "Arzneimittelzubereitung mit einem Gehalt an 3-Butylamino-4-phenoxy-5-sulfamylbenzoesaeure und deren Salzen". DPMAregister (in German). Ger. Pat. 19 64 504.6: German Patent and Trade Mark Office. Archived from the original on 28 August 2021. Retrieved 20 June 2018.
{{cite web}}: CS1 maint: location (link) CS1 maint: unrecognized language (link) - ↑ Feit, P. W. (1971). "Aminobenzoic acid diuretics. 2. 4-Substituted-3-amino-5-sulfamoylbenzoic acid derivatives". Journal of Medicinal Chemistry. 14 (5): 432–9. doi:10.1021/jm00287a014. PMID 5117690.
- ↑ Feit, Peter Werner (11 January 1972). "Pharmaceutical composition for the treatment of oedematous conditions and hypertension" (PDF). US Pat. 3634583A: Leo Pharmaceutical Products Ltd AS. Archived (PDF) from the original on 20 June 2018. Retrieved 20 June 2018.
{{cite web}}: CS1 maint: location (link) - ↑ Feit, Peter Werner; Nielsen, Ole Bent Tvaermose; Bruun, Herta; Bretting, Claus Aage Svensgaard (4 April 1978). "Sulphonamides, compositions containing the same and methods for using the same in the treatment of hypertension or odemeas" (PDF). US Pat. US4082851A: Leo Pharmaceutical Products Ltd AS. Archived (PDF) from the original on 20 June 2018. Retrieved 20 June 2018.
{{cite web}}: CS1 maint: location (link) - ↑ "McAllister, Smith, Grant, Texans' Pittman among players testing positive". ESPN.com. ESPN. October 26, 2008. Archived from the original on August 12, 2017. Retrieved June 6, 2017.
- ↑ "Food and Drug Administration Office of Criminal Investigations – U.S. Department of Justice Press Release – Pills Sold Throughout the United States Contained an Undisclosed Prescription Drug Banned By the National Football League". fda.gov. United States Food and Drug Administration. March 26, 2014. Archived from the original on July 2, 2017. Retrieved June 6, 2017.
- ↑ Löscher W, Puskarjov M, Kaila K (June 2013). "Cation-chloride cotransporters NKCC1 and KCC2 as potential targets for novel antiepileptic and antiepileptogenic treatments". Neuropharmacology. 69: 62–74. doi:10.1016/j.neuropharm.2012.05.045. PMID 22705273.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Pages using duplicate arguments in template calls
- CS1 maint: location
- CS1 maint: unrecognized language
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- All articles with unsourced statements
- Articles with unsourced statements from June 2017
- Articles with invalid date parameter in template
- RTT
- Loop diuretics
- Benzoic acids
- Diphenyl ethers
- Carbonic anhydrase inhibitors
- NMDA receptor antagonists
- World Anti-Doping Agency prohibited substances
- Anilines
- World Health Organization essential medicines (alternatives)