Mefloquine
 | |
 | |
| Names | |
|---|---|
| Trade names | Lariam, Mephaquin, Mefliam, others |
| |
| Clinical data | |
| Main uses | Prevent or treat malaria[1] |
| Side effects | Vomiting, diarrhea, headaches, sleep disorders, rash[1] |
| Pregnancy category |
|
| Routes of use | By mouth (tablets) |
| Defined daily dose | 1 g [2] |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| Legal status | |
| Pharmacokinetics | |
| Metabolism | Extensive liver; main metabolite is inactive |
| Elimination half-life | 2 to 4 weeks |
| Excretion | Primarily bile and feces; urine (9% as unchanged drug, 4% as primary metabolite) |
| Chemical and physical data | |
| Formula | C17H16F6N2O |
| Molar mass | 378.318 g·mol−1 |
| 3D model (JSmol) | |
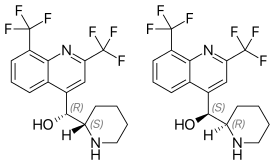
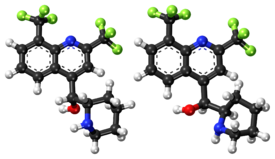
| Chirality | Racemic mixture |
| |
| |
Mefloquine, sold under the brand names Lariam among others, is a medication used to prevent or treat malaria.[1] When used for prevention it is typically started before potential exposure and continued for several weeks after potential exposure.[1] It can be used to treat mild or moderate malaria but is not recommended for severe malaria.[1] It is taken by mouth.[1]
Common side effects include vomiting, diarrhea, headaches, sleep disorders, and a rash.[1] Serious side effects include potentially long-term mental health problems such as depression, hallucinations, and anxiety and neurological side effects such as poor balance, seizures, and ringing in the ears.[1] It is therefore not recommended in people with a history of mental health problems or epilepsy.[1] It appears to be safe during pregnancy and breastfeeding.[3]
Mefloquine was developed by the United States Army in the 1970s and came into use in the mid 1980s.[4][5][6] It is on the World Health Organization's List of Essential Medicines.[7] It is available as a generic medication.[1] The wholesale price in the developing world is about US$0.6–1.3 per dose.[8] In the United Kingdom it costs the NHS £1.82 per dose.[9] In the United States it costs about $10 a dose.[1]
Medical uses

Mefloquine is used to both prevent and treat certain forms of malaria.[10]
Malaria prevention
Mefloquine is useful for the prevention of malaria in all areas except for those where parasites may have resistance to multiple medications,[11] and is one of several anti-malarial medications recommended by the United States Centers for Disease Control and Prevention for this purpose. It is also recommended by the Infectious Disease Society of America for malaria prophylaxis as a first or second-line agent, depending on resistance patterns in the malaria found in the geographic region visited.[12][13] It is typically taken for one to two weeks before entering an area with malaria.[10] Doxycycline and atovaquone/proguanil provide protection within one to two days and may be better tolerated.[14][15] If a person becomes ill with malaria despite prophylaxis with mefloquine, the use of halofantrine and quinine for treatment may be ineffective.[16]: 4
Malaria treatment
Mefloquine is used as a treatment for chloroquine-sensitive or resistant Plasmodium falciparum malaria, and is deemed a reasonable alternative for uncomplicated chloroquine-resistant Plasmodium vivax malaria.[10][16] It is one of several drugs recommended by the United States' Centers for Disease Control and Prevention.[17] It is not recommended for severe malaria infections, particularly infections from P. falciparum, which should be treated with intravenous antimalarials.[10][16] Mefloquine does not eliminate parasites in the liver phase of the disease, and people with P. vivax malaria should be treated with a second drug that is effective for the liver phase, such as primaquine.[16]: 4
Resistance
Resistance to mefloquine is common around the west border in Cambodia and other parts of Southeast Asia.[18] The mechanism of resistance is by increase in Pfmdr1 copy number.[19]
Dosage
The defined daily dose is 1 gram (by mouth).[2] In adults the dose for prevention is 250 mg once per week.[1] This should be started 1 to 2 weeks before potential exposure and continued for 4 weeks after potential exposure.[1] For the treatment of malaria 750 mg followed by 500 mg after 6 to 12 hours may be used, but is generally only recommended if other options are not avaliable.[20]
Side effects
Common side effects include vomiting, diarrhea, headaches, and a rash.[1] Severe side effects requiring hospitalization are rare,[11] but include mental health problems such as depression, hallucinations, anxiety and neurological side effects such as poor balance, seizures, and ringing in the ears.[1] Mefloquine is therefore not recommended in people with a history of psychiatric disorders or epilepsy.[1]
Neurologic and psychiatric
In 2013 the United States Food and Drug Administration added a boxed warning to the U.S. label of mefloquine regarding the potential for neuropsychiatric side effects that may persist even after discontinuing administration of the drug.[21][22] In 2013 the FDA stated "Neurologic side effects can occur at any time during drug use, and can last for months to years after the drug is stopped or can be permanent."[23] Neurologic effects include dizziness, loss of balance, seizures, and tinnitus. Psychiatric effects include nightmares, visual hallucinations, auditory hallucinations, anxiety, depression, unusual behavior, and suicidal ideations.
Central nervous system events requiring hospitalization occur in about one in 10,000 people taking mefloquine for malaria prevention, with milder events (e.g., dizziness, headache, insomnia, and vivid dreams) in up to 25%.[24] When some measure of subjective severity is applied to the rating of adverse events, about 11-17% of travelers are incapacitated to some degree.[14]
Cardiac
Mefloquine may cause abnormalities with heart rhythms that are visible on electrocardiograms. Combining mefloquine with other drugs that cause similar effects, such as quinine or quinidine, can increase these effects. Combining mefloquine with halofantrine can cause significant increases in QTc intervals.[16]: 10
Contraindications
Mefloquine is contraindicated in those with a previous history of seizures or a recent history of psychiatric disorders.[10]
Pregnancy and breastfeeding
Available data suggests that mefloquine is safe and effective for use by pregnant women during all trimesters of pregnancy,[25] and it is widely used for this indication.[26] In pregnant women, mefloquine appears to pose minimal risk to the fetus,[26][27] and is not associated with increased risk of birth defects or miscarriages.[28] Compared to other malaria chemoprophylaxis regimens, however, mefloqinone may produce more side effects in non-pregnant travelers.
Mefloquine is also safe and effective for use during breastfeeding,[25] though it appears in breast milk in low concentrations.[11][16]: 9 The World Health Organization (WHO) gives approval for the use of mefloquine in the second and third trimesters of pregnancy and use in the first trimester does not mandate termination of pregnancy.[11]
Pharmacology
Elimination
Mefloquine is metabolized primarily through the liver. Its elimination in persons with impaired liver function may be prolonged, resulting in higher plasma levels and an increased risk of adverse reactions. The mean elimination plasma half-life of mefloquine is between two and four weeks. Total clearance is through the liver, and the primary means of excretion is through the bile and feces, as opposed to only 4% to 9% excreted through the urine. During long-term use, the plasma half-life remains unchanged.[29][30]
Liver function tests should be performed during long-term administration of mefloquine.[31] Alcohol use should be avoided during treatment with mefloquine.[32]
Chemistry
Specifically it is used as mefloquine hydrochloride.
Mefloquine is a chiral molecule with two asymmetric carbon centres, which means it has four different stereoisomers. The drug is currently manufactured and sold as a racemate of the (R,S)- and (S,R)-enantiomers by Hoffman-LaRoche, a Swiss pharmaceutical company. Essentially, it is two drugs in one. Plasma concentrations of the (–)-enantiomer are significantly higher than those for the (+)-enantiomer, and the pharmacokinetics between the two enantiomers are significantly different. The (+)-enantiomer has a shorter half-life than the (–)-enantiomer.[14]
History
Mefloquine was formulated at Walter Reed Army Institute of Research (WRAIR) in the 1970s shortly after the end of the Vietnam war. Mefloquine was number 142,490 of a total of 250,000 antimalarial compounds screened during the study.[4]
Mefloquine was the first Public-Private Venture (PPV) between the US Department of Defense and a pharmaceutical company. WRAIR transferred all its phase I and phase II clinical trial data to Hoffman-LaRoche and Smith Kline. FDA approval as a treatment for malaria was swift. Most notably, phase III safety and tolerability trials were skipped.[4]
The drug was first approved in Switzerland in 1984 by Hoffmann-LaRoche,[33] who brought it to market with the name Lariam.[34]
However, mefloquine was not approved by the FDA for prophylactic use until 1989. This approval was based primarily on compliance, while safety and tolerability were overlooked.[4] Because of the drug's very long half-life, the Centers for Disease Control originally recommended a mefloquine dosage of 250 mg every two weeks; however, this caused an unacceptably high malaria rate in the Peace Corps volunteers who participated in the approval study, so the drug regimen was switched to once a week.[14]
By 1991, Hoffman was marketing the drug on a worldwide basis.[34]
By the 1992 UNITAF, Canadian soldiers were being prescribed the drug en masse.[35]
By 1994, medical professionals were noting "severe psychiatric side effects observed during prophylaxis and treatment with mefloquine", and recommending that "the absence of contraindications and minor side effects during an initial course of mefloquine should be confirmed before another course is prescribed."[36] Other doctors at the University Hospital of Zurich noted in a case of "a 47-year-old, previously healthy Japanese tourist" who had severe neuropsychiatric side-effects from the drug that[37]
The neuropsychiatric side effects of the antimalarial drug mefloquine are well documented. They include anxiety, depression, hallucinations, acute psychosis, and seizures. The incidence of these side effects is 1 in 13,000 with prophylactic use and 1 in 250 with therapeutic use.
The first randomized, controlled trial on a mixed population was performed in 2001. Prophylaxis with mefloquine was compared to prophylaxis with atovaquone-proguanil. Roughly 67% of participants in the mefloquine arm reported greater than or equal to one adverse event, vs 71% in the atovaquone-proguanil arm. In the mefloquine arm, 5% of the users reported severe events requiring medical attention, vs 1.2% in the atovaquone-proguanil arm.[4][38]
In August 2009, Roche stopped marketing Lariam in the United States.[39]
Retired soldier Johnny Mercer, who was later appointed Minister for Veterans Affairs by Boris Johnson, told in 2015 that he had received "a letter about once or twice a week" about ill-effects from the drug.[40] In July 2016, Roche took this brand off the market in Ireland.[39]
Military
In 2006, the Australian military deemed mefloquine "a third-line drug" alternative, and over the five years from 2011 only 25 soldiers had been prescribed the drug, and only in cases of their intolerance for other alternatives.[39] Between 2001 and 2012, 16000 Canadian soldiers sent to Afghanistan were given the drug as a preventative measure.[39] In 2013, the US Army banned mefloquine from use by its special forces such as the Green Berets.[39] In autumn 2016, the UK military followed suit with their Australian peers after a parliamentary inquiry into the matter revealed that it can cause permanent side effects and brain damage.[39]
In early December 2016, the German defence ministry removed mefloquine from the list of medications it would provide to its soldiers.[39]
In autumn 2016, Canadian Surgeon General Brigadier General Hugh Colin MacKay told a parliamentary committee that faulty science supported the assertion that the drug has indelible noxious side effects. An expert from Health Canada named Barbara Raymond told the same committee that the evidence she had read failed to support the conclusion of indelible side effects.[39] Canadian soldiers who took mefloquine when deployed overseas have claimed they have been left with ongoing mental health problems.[41]
Research
In June 2010, the first case report appeared of a progressive multifocal leukoencephalopathy being successfully treated with mefloquine. Mefloquine can also act against the JC virus. Administration of mefloquine seemed to eliminate the virus from the patient's body and prevented further neurological deterioration.[42]
WRAIR has published several papers outlining ongoing efforts at that institution to make mefloquine safer by producing a drug composed of only the (+)-enantiomer.
Mefloquine alters cholinergic synaptic transmission through both postsynaptic [43] and presynaptic actions.[44] The postsynaptic action to inhibit acetylcholinesterase changes transmission across synapses in the brain.[45]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 "Mefloquine Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 2015-12-08. Retrieved 27 Nov 2015.
- ↑ 2.0 2.1 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 3 August 2020. Retrieved 22 September 2020.
- ↑ "Mefloquine (Lariam) Use During Pregnancy". Drugs.com. Archived from the original on 31 March 2019. Retrieved 31 March 2019.
- ↑ 4.0 4.1 4.2 4.3 4.4 Croft, AM (2007). "A lesson learnt: the rise and fall of Lariam and Halfan". J R Soc Med. 100 (4): 170–4. doi:10.1258/jrsm.100.4.170. PMC 1847738. PMID 17404338.
- ↑ Ravina, Enrique (2011). The evolution of drug discovery : from traditional medicines to modern drugs (1. Aufl. ed.). Weinheim: Wiley-VCH. p. 136. ISBN 9783527326693.
- ↑ Jeremy Farrar; Peter J. Hotez; Thomas Junghanss (2013). Manson's tropical diseases (23rd ed.). Oxford: Elsevier/Saunders. p. 569. ISBN 9780702053061.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ "Mefloquine". International Drug Price Indicator Guide. Archived from the original on 22 January 2018. Retrieved 27 November 2015.
- ↑ British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 607. ISBN 9780857113382.
- ↑ 10.0 10.1 10.2 10.3 10.4 "Lariam". The American Society of Health-System Pharmacists. Archived from the original on 7 January 2012. Retrieved 3 April 2011.
- ↑ 11.0 11.1 11.2 11.3 Schlagenhauf, P; Adamcova, M; Regep, L; Schaerer, MT; Rhein, HG (2010-12-09). "The position of mefloquine as a 21st century malaria chemoprophylaxis". Malaria Journal. 9: 357. doi:10.1186/1475-2875-9-357. PMC 3224336. PMID 21143906.
- ↑ "www.idsociety.org" (PDF). Archived (PDF) from the original on 2015-03-19.
- ↑ "Malaria - Chapter 3 - 2014 Yellow Book | Travelers' Health | CDC". Archived from the original on 2014-12-26.
- ↑ 14.0 14.1 14.2 14.3 Schlagenhauf, P. (1999). "Mefloquine for malaria chemoprophylaxis 1992-1998". Travel Med. 6 (2): 122–123. doi:10.1111/j.1708-8305.1999.tb00843.x. PMID 10381965.
- ↑ Tickell-Painter, M; Maayan, N; Saunders, R; Pace, C; Sinclair, D (30 October 2017). "Mefloquine for preventing malaria during travel to endemic areas". The Cochrane Database of Systematic Reviews. 10: CD006491. doi:10.1002/14651858.CD006491.pub4. PMC 5686653. PMID 29083100.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 "Lariam medication guide" (PDF). Hoffman La Roche. Archived (PDF) from the original on 2 October 2013. Retrieved 27 September 2013.
- ↑ "www.cdc.gov" (PDF). Archived (PDF) from the original on 2015-02-09.
- ↑ "Malaria Information". Traveldoctor. Archived from the original on 28 June 2016. Retrieved 9 July 2016.
- ↑ Price RN, Uhlemann AC, Brockman A, McGready R, Ashley E, Phaipun L, Patel R, Laing K, Looareesuwan S, White NJ, Nosten F, Krishna S (2004). "Mefloquine resistance in Plasmodium falciparum and increased pfmdr1 gene copy number". Lancet. 364 (9432): 438–47. doi:10.1016/S0140-6736(04)16767-6. PMC 4337987. PMID 15288742.
- ↑ "Treatment of Malaria (Guidelines for Clinicians)" (PDF). CDC. Archived (PDF) from the original on 29 August 2017. Retrieved 17 August 2020.
- ↑ "www.accessdata.fda.gov" (PDF). Archived (PDF) from the original on 2016-03-04.
- ↑ "www.fda.gov" (PDF). Archived (PDF) from the original on 2014-06-30.
- ↑ "FDA Drug Safety Communication: FDA approves label changes for antimalarial drug mefloquine hydrochloride due to risk of serious psychiatric and nerve side effects". Archived from the original on 2019-12-13. Retrieved 2019-06-15.
- ↑ AlKadi, HO (2007). "Antimalarial drug toxicity: a review". Chemotherapy. 53 (6): 385–91. doi:10.1159/000109767. PMID 17934257.
- ↑ 25.0 25.1 "Mefloquine" (PDF). Medicines for the Prevention of Malaria While Traveling. Atlanta, Georgia: Centers for Disease Control and Prevention. 2019. Archived (PDF) from the original on 2020-08-03. Retrieved 2019-03-30.
- ↑ 26.0 26.1 González R, Hellgren U, Greenwood B, Menéndez C (2014). "Mefloquine safety and tolerability in pregnancy: a systematic literature review". Malaria Journal. 13: 75. doi:10.1186/1475-2875-13-75. PMC 3942617. PMID 24581338.
- ↑ Croft AM (2010). "Malaria: prevention in travellers". Clin Evid (Online). 2010. PMC 3217660. PMID 21418669.
- ↑ Schlagenhauf P, Blumentals WA, Suter P, et al. (2012). "Pregnancy and fetal outcomes after exposure to mefloquine in the pre- and periconception period and during pregnancy". Clin Infect Dis. 54 (11): e124–31. doi:10.1093/cid/cis215. PMC 3348951. PMID 22495078.
- ↑ "Lariam product monogram" (PDF). Hoffman La Roche Limited. p. 3. Archived from the original (PDF) on 17 December 2011. Retrieved 24 April 2011.
- ↑ "Lariam product monogram" (PDF). Hoffman La Roche Limited. p. 4. Archived from the original (PDF) on 17 December 2011. Retrieved 24 April 2011.
- ↑ "Lariam product monogram" (PDF). Hoffman La Roche Limited. p. 6. Archived from the original (PDF) on 17 December 2011. Retrieved 24 April 2011.
- ↑ "Lariam product monogram" (PDF). Hoffman La Roche Limited. p. 18. Archived from the original (PDF) on 17 December 2011. Retrieved 24 April 2011.
- ↑ "Roche Submission to Committee Secretary Senate Foreign Affairs Australia". Archived from the original on 2020-01-24. Retrieved 2020-01-24.
- ↑ 34.0 34.1 "'It's not a benign drug - it has ruined my life'". Guardian News & Media Limited. 24 October 2002. Archived from the original on 3 August 2019. Retrieved 3 August 2019.
- ↑ Adams, Sharon (6 September 2017). "Cure or curse?". Canvet Publications Ltd. Legion Magazine. Archived from the original on 4 August 2019. Retrieved 4 August 2019.
- ↑ Hennequin, C.; Bourée, P.; Bazin, N.; Bisaro, F.; Feline, A. (1994). "Severe psychiatric side effects observed during prophylaxis and treatment with mefloquine". Archives of Internal Medicine. 154 (20): 2360–2. doi:10.1001/archinte.1994.00420200116012. PMID 7944858.
- ↑ Speich, Rudolf; Haller, Alois (1994). "Central Anticholinergic Syndrome with the Antimalarial Drug Mefloquine". New England Journal of Medicine. 331 (1): 57–58. doi:10.1056/NEJM199407073310120. PMID 8202114.
- ↑ Overbosch D, Schilthuis H, Bienzle U, et al. (October 2001). "Atovaquone-proguanil versus mefloquine for malaria prophylaxis in nonimmune travelers: results from a randomized, double-blind study". Clin. Infect. Dis. 33 (7): 1015–21. doi:10.1086/322694. PMID 11528574.
- ↑ 39.0 39.1 39.2 39.3 39.4 39.5 39.6 39.7 "Germany bans drug linked to brain damage, ramps up pressure on Canada". iPolitics. 9 December 2016. Archived from the original on 3 August 2019. Retrieved 3 August 2019.
- ↑ "Did Lariam send Cambridge student Alana Cutland to her death… and what anti-malarials should children take on their gap year?". Telegraph Media Group Limited. 3 August 2019. Archived from the original on 3 August 2019. Retrieved 3 August 2019.
- ↑ Haines, Avery (18 October 2019). "Canadian soldiers allege anti-malaria medication left them with intense rage, suicidal ideations". W5. Archived from the original on 16 April 2020. Retrieved 16 April 2020.
- ↑ Gofton TE, Al-Khotani A, O'Farrell B, Ang LC, McLachlan RS (June 2010). "Mefloquine in the treatment of progressive multifocal leukoencephalopathy". J Neurol Neurosurg Psychiatry. 82 (4): 452–455. doi:10.1136/jnnp.2009.190652. PMID 20562463. Archived from the original on 2012-03-21.
- ↑ McArdle JJ, Sellin LC, Coakley KM, Potian JG, Quinones-Lopez MC, Rosenfeld CA, Sutatos LG, Hognason K (June 2005). "Mefloquine inhibits cholinesterases at the mouse neuromuscular junction". Neuropharmacology. 49 (8): 1132–1139. doi:10.1016/j.neuropharm.2005.06.011. PMID 16081111.
- ↑ McArdle JJ, Sellin LC, Coakley KM, Potian JG, Hognason K (September 2006). "Mefloquine selectively increases asynchronous acetylcholine release from motor nerve terminals". Neuropharmacology. 50 (3): 345–353. doi:10.1016/j.neuropharm.2005.09.011. PMID 16288931.
- ↑ Zhou C, Xiao C, McArdle JJ, Ye JH (February 2006). "Mefloquine enhances nigral gamma-aminobutyric acid release via inhibition of cholinesterase". Journal of Pharmacology and Experimental Therapeutics. 317 (3): 1155–1160. doi:10.1124/JPET.106.101923. PMID 16501066. Archived from the original on 2021-08-28. Retrieved 2019-12-01.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Manufacturer's information
- Roche Medication Guide for Lariam Archived 2018-11-01 at the Wayback Machine
- Mefloquine (Lariam) Action, Clearinghouse for information on mefloquine news, research, toxicity
- Controversies and Misconceptions in Malaria Chemoprophylaxis for Travelers Archived 2011-12-17 at the Wayback Machine
- The position of mefloquine as a 21st century malaria chemoprophylaxis Archived 2015-07-08 at the Wayback Machine (Paper based on data collated for an F. Hoffmann-La Roche regulatory update)
- Crazy Pills - NYTimes Op-Ed Archived 2018-11-01 at the Wayback Machine
- The Lariam Files - Keith Epstein, Washington Post Archived 2017-02-09 at the Wayback Machine
- Pages using duplicate arguments in template calls
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- Drugboxes which contain changes to verified fields
- Drugboxes which contain changes to watched fields
- Articles with hatnote templates targeting a nonexistent page
- Articles with changed EBI identifier
- Webarchive template wayback links
- American inventions
- Antimalarial agents
- Chirality
- Chloroarenes
- Drug safety
- Hoffmann-La Roche brands
- Medical controversies
- Piperidines
- Quinolines
- Racemate
- Trifluoromethyl compounds
- World Health Organization essential medicines
- RTT