Sjögren syndrome
| Sjögren syndrome | |
|---|---|
| Other names: Primary Sjögren-Gougerot syndrome,[1] Sjögren's syndrome, sicca syndrome | |
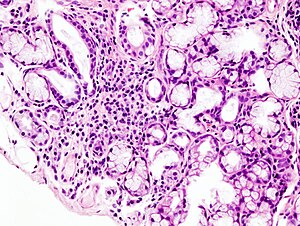 | |
| Image with a microscope of focal lymphoid infiltration in the minor salivary gland associated with Sjögren syndrome. | |
| Pronunciation |
|
| Symptoms | Dry mouth, dry eyes, other areas of dryness[3] |
| Complications | Lymphoma[3] |
| Usual onset | Middle age[3][4] |
| Duration | Long term[5] |
| Causes | Autoimmune disease (unknown cause)[5] |
| Diagnostic method | Tissue biopsy, blood tests[3] |
| Differential diagnosis | Medication side effect, anxiety, sarcoidosis, amyloidosis[6] |
| Treatment | Artificial tears, medications to reduce inflammation, surgery[5] |
| Prognosis | Normal life expectancy[7] |
| Frequency | ~0.7%[8] |
Sjögren syndrome (SjS, SS) is a long-term autoimmune disease that affects the body's moisture-producing glands.[5] Primary symptoms are a dry mouth and dry eyes.[3] Other symptoms can include dry skin, vaginal dryness, a chronic cough, numbness in the arms and legs, feeling tired, muscle and joint pains, and thyroid problems.[5] Those affected are also at an increased risk (5%) of lymphoma.[3][8]
While the exact cause is unclear, it is believed to involve a combination of genetics and an environmental trigger such as exposure to a virus or bacteria.[5] It can occur independently of other health problems (primary Sjögren syndrome) or as a result of another connective tissue disorder (secondary Sjögren syndrome).[4] The inflammation that results progressively damages the glands.[8] Diagnosis is by biopsy of moisture-producing glands and blood tests looking for specific antibodies.[3] On biopsy there are typically lymphocytes within the glands.[3]
Treatment is directed at the person's symptoms.[5] For dry eyes artificial tears, medications to reduce inflammation, punctal plugs, or surgery to shut the tear ducts may be tried.[5] For a dry mouth, chewing gum (preferably sugar-free), sipping water, or a saliva substitute may be used.[5] In those with joint or muscle pain, ibuprofen may be used.[5] Medications that can cause dryness, such as antihistamines, may also be stopped.[5]
The disease was described in 1933 by Henrik Sjögren, after whom it is named; however, a number of earlier descriptions of people with the symptoms exist.[4] Between 0.2% and 1.2% of the population are affected, with half having the primary form and half the secondary form.[8] Females are affected about ten times as often as are males.[4] Though the disease commonly begins in middle age, anyone can be affected.[3][4] Among those without other autoimmune disorders, life expectancy is unchanged.[7]
Signs and symptoms

The hallmark symptom of Sjögren syndrome is dry mouth and keratoconjunctivitis sicca (dry eyes).[9] Vaginal dryness, dry skin and dry nose may also occur.[9] Other organs of the body may also be affected, including the kidneys, blood vessels, lungs, liver, pancreas, and brain.[9]
Skin dryness in some people with SS may be the result of lymphocytic infiltration into skin glands. The symptoms may develop insidiously, with the diagnosis often not considered for several years because sicca may be attributed to medications, a dry environment, aging, or may be regarded as not of a severity warranting the level of investigation necessary to establish the presence of the underlying autoimmune disorder.[10]
SS can damage vital organs, with symptoms that may plateau or worsen, or go into remission, as with other autoimmune diseases. Some people may experience only the mild symptoms of dry eyes and mouth, while others have symptoms of severe disease. Many patients can treat problems symptomatically. Others experience blurred vision, constant eye discomfort, recurrent mouth infections, swollen parotid glands, dysphonia (vocal disorders including hoarseness), and difficulty in swallowing and eating. Debilitating fatigue and joint pain can seriously impair quality of life. Some patients can develop kidney involvement (autoimmune tubulointerstitial nephritis) leading to proteinuria (excess protein in urine), urinary concentrating defect, and distal renal tubular acidosis.[11]
Complications
Among the complications discussed above, women with anti-Ro/SS-A and anti-La/SS-B antibodies who become pregnant have an increased rate of neonatal lupus erythematosus with congenital heart block requiring a pacemaker.[12] Type I cryoglobulinemia is a known complication of SS.[13]
Sjögren's syndrome can affect such organs as the liver, pancreas, kidneys, lungs, and central nervous system.[14]
Associated conditions
SS is associated with a number of other medical conditions, many of which are autoimmune or rheumatic disorders, such as celiac disease,[15][16] fibromyalgia, SLE (lupus), autoimmune thyroiditis, multiple sclerosis and spondyloarthropathy,[17] and several malignancies, principally non-Hodgkin lymphoma.[17][18]
Causes
The cause of SS is unknown, but it may be the influence of a combination of genetic, environmental, and other factors, as is the case with many other autoimmune disorders.[19] Around 20 auto-antibodies could be involved.[20]
Genetics
The observation of high rates of autoimmune disorders in families with SS is linked with a genetic predisposition to the syndrome.[21] Studies on the polymorphisms of human leukocyte antigen (HLA)-DR and HLA-DQ gene regions in SS patients show differential susceptibility to the syndrome as the result of different types of the resulting autoantibody production.[21]
Hormones
Since SS is associated with a high prevalence in women, sex hormones, especially estrogen, are believed to affect humoral and cell-mediated immune responses affecting susceptibility to the syndrome.[21] Androgens are generally considered to prevent autoimmunity.[22] Studies on mice models suggest estrogen deficiency stimulates presentation of autoantigens, inducing SS-like symptoms.[21]
Microchimerism
Microchimerism of fetal cells (offspring lymphoid cells in maternal circulation) may generate autoimmunity in women who have previously been pregnant.[22][23] Generation of an autoimmune potential via microchimerism may lead to a switch from a silent form of autoimmunity with age-dependent decrease in self-tolerance.[22]
Environment
Viral proteins, engulfed molecules, or degraded self-structures may initiate autoimmunity by molecular mimicry and increase the chances of SS development.[22] Epstein–Barr virus, hepatitis C, and human T-cell leukemia virus-1 are among the most studied infectious agents in SS.[22] Damaged self-structures targeted for apoptosis may be mistakenly exposed to the immune system, triggering autoimmunity in exocrine glands, which are often prone to autoimmune responses.[22]
Pathogenesis

The pathogenetic mechanisms of Sjögren syndrome have not been fully elucidated, resulting in the lack of pathophysiology knowledge of the management of this autoimmune exocrinopathy. Although the numerous factors contributing to the progression of this disease have made it difficult to discover the exact origin and cause, major advances over the past decade have contributed to a proposed set of pathogenic events that occur prior to the diagnosis of SS.[21]
SS was originally proposed as a specific, self-perpetuating immune system-mediated loss of exocrine glands, specifically acinar and ductal cells. Although this explains the more obvious symptoms (such as the lack of saliva and lacrimal fluid), it does not explain the more widespread systemic effects seen in the progression of the disease.
In the presence of a susceptible genetic background, both environmental and hormonal factors are thought capable of triggering the infiltration of lymphocytes, specifically CD4+ T cells, B cells, and plasma cells, causing glandular dysfunction in the salivary and lacrimal glands.[21]
SS is associated with increased levels in cerebrospinal fluid (CSF) of IL-1RA, an interleukin 1 antagonist. This suggests that the disease begins with increased activity in the interleukin 1 system, followed by an autoregulatory upregulation of IL-1RA to reduce the successful binding of interleukin 1 to its receptors. Interleukin 1 likely is the marker for fatigue, but increased IL-1RA is observed in the CSF and is associated with increased fatigue through cytokine-induced sickness behavior.[25] However, SS is characterized by decreased levels of IL-1ra in saliva, which could be responsible for mouth inflammation and dryness.[26] Patients with secondary SS also often exhibit signs and symptoms of their primary rheumatic disorders, such as systemic lupus erythematosus, rheumatoid arthritis, or systemic sclerosis.
Genetic predisposition
The genetic locus most significantly associated with primary SS is the major histocompatibility complex/human leukocyte antigen (MHC/HLA) region, as demonstrated by the preliminary results of the first genome-wide association study (GWAS).[27] This GWAS included data from a discovery cohort of 395 patients of European ancestry with primary SS, and 1,975 healthy control individuals, and from a replication study that comprised 1,234 cases and 4,779 healthy controls. Associations with polymorphisms located at six independent loci were also detected; IRF5, STAT4, BLK, IL12A, TNIP1, and CXCR5. This also suggested the activation of the innate immune system, notably through the IFN system, B-cell activation through CXCR5-directed recruitment to lymphoid follicles and B-cell receptor (BCR) activation involving BLK, and T-cell activation owing to HLA susceptibility and the IL-12-IFN-γ-axis.[28]
Patients of different ethnic origin carry different HLA-susceptibility alleles, of which HLA-DR and HLA-DQ are involved in the pathogenesis of SS. For example, patients from Northern and Western Europe and from North America show a high prevalence of B8, DRw52, and DR3 genes.[29] HLA class II alleles are associated with the presence of specific subsets of autoantibodies, rather than with the disease itself.[30] Autoantibodies refer to the loss of B-cell tolerance leading to production of antibodies directed against diverse organ-specific and organ nonspecific antigens.[21] Association between HLA and SS is restricted to patients with anti-SSA/Ro or anti-SSB/La antibodies. Seropositivity for anti-Ro and anti-La is associated with greater severity and longer duration of disease, and findings of their high abundance from the salivary glands of SS patients suggests their imperative role in the pathogenesis of SS.[31]
Beyond genetics, epigenetic abnormality related to DNA methylation, histone acetylation, or microRNA expression probably has a key role in the pathogenesis of autoimmune diseases, including SS, though research in this area is very limited and minimal.[32]
Environmental triggers
Environmental factors, such as glandular viral infection, could prompt epithelial cells to activate the HLA-independent innate immune system through toll-like receptors.[33] Although a number of infectious, exogenous agents have been implicated in the pathogenesis of SS, such as Epstein-Barr virus (EBV), human T-lymphotropic virus 1, and hepatitis C virus, their association with SS appears weak. While EBV is present in the salivary glands of normal individuals, a high incidence of EBV reactivation in SS patients has been reported with increased levels of EBV DNA. This indicates viral reactivation and inability of lymphoid infiltrates to control EBV replication in SS, leading to the initiation or perpetuation of an immune response in target organs. Nonetheless, it remains to be clarified exactly how reactivation of EBV is induced in lesions of patients with SS, and which specific molecular mechanisms are involved in the process of viral reactivation.[34]
Inflammation
Epithelial cells in SS lesions are active participants in the induction and perpetuation of the inflammatory process. Environmental and hormonal factors, in concert with an appropriate genetic background, are believed to trigger SS, which dysregulates epithelial cells and allows aberrant homing and activation of dendritic cells (DCs), T cells, and B cells.[35] Dendritic cells are antigen-presenting cells that process antigen material and present it to other T cells. Following the migration of lymphocytes into the glands in response to chemokines and specific adhesion molecules, T cells interact with epithelial cells. Epithelial cells are further activated by proinflammatory cytokines (IL-1β, IFN-γ, and TNF), which are produced by adjacent T cells. The early accumulation of plasmacytoid dendritic cells in the target tissues, which produce high levels of type 1 IFNs, seems important, as these cells can further dysregulate the immune response through abnormal retention of lymphocytes in the tissues and their subsequent activation. IFN-α stimulates the production of B-cell activating factor (BAFF) by epithelial cells, DCs, and T cells. BAFF stimulates aberrant B-cell maturation, leading to the emergence of self-reactive B cells, which locally produce autoantibodies, in a germinal centre-like structure (GC-like), which is also the location of lymphomagenesis (origin of lymphoma).[21]
Programmed cell death
Dysregulation of apoptosis (programmed cell death) is believed to play a role in the pathogenesis of a variety of autoimmune diseases, though its role in SS is controversial. Both the Fas and Fas ligand proteins are overexpressed in primary SS patients, while expression of BCL-1, which is known to downregulate apoptosis, was found significantly reduced in acinar and ductal epithelial cells of SS patients compared to healthy people.[36][37] In situ studies did not show increased apoptosis among glandular epithelial cells, but did show reduced apoptosis among infiltrating mononuclear cells. Reduced apoptosis was also implicated in the accumulation of autoreactive B-cells found in the glands. The relationship of autoantibodies expressed in SS with apoptosis is still being researched.[19]
Hormonal factors
Sex hormones seem to influence humoral and cell-mediated immune response, with estrogen being considered one of the biggest factors responsible for sex-immunologic dimorphism.[38] Estrogen deficiency appears to play a role in development of SS.[39] It has been hypothesized that androgen administration to the ocular surface may serve as an effective therapy for dry eyes.[40]
Diagnosis

Diagnosing Sjögren syndrome is complicated by the range of symptoms that a patient may manifest, and the similarity between symptoms of SS and those of other conditions. Also, patients with SS symptoms approach different specialities for treatment, which can make diagnosis difficult. Since dry eyes and dry mouth are very common symptoms, and frequently occur in people over 40, affected people may believe that the symptoms are age-related and therefore ignore them. However, some medications can cause symptoms similar to those of SS. The combination of several tests, which can be done in a series, can eventually diagnose SS.[23][41]
SS is usually classified as either 'primary' or 'secondary'. Primary Sjögren syndrome occurs by itself and secondary Sjögren syndrome occurs when another connective tissue disease is present.
Blood tests can be done to determine if a patient has high levels of antibodies that are indicative of the condition, such as antinuclear antibody (ANA) and rheumatoid factor (because SS frequently occurs secondary to rheumatoid arthritis), which are associated with autoimmune diseases. Typical SS ANA patterns are SSA/Ro and SSB/La, of which Anti-SSB/La is far more specific; Anti-SSA/Ro is associated with numerous other autoimmune conditions, but are often present in SS. However, Anti-SSA and Anti-SSB tests are frequently not positive in SS.
The rose bengal test uses a stain that measures state and function of the lacrimal glands. This test involves placing the non-toxic dye rose bengal on the eyes. The dye’s distinctive colour helps in determining the state and functioning of tear film and the rate of tear evaporation. Any distinctive colour change can indicate SS, but confirming the condition requires many related diagnostic tools.[41]
Schirmer's test measures the production of tears: a strip of filter paper is held inside the lower eyelid for five minutes, and its wetness is then measured with a ruler. Producing less than 5 mm (0.20 in) of liquid is usually indicative of SS. This measurement analysis varies among people depending on other eye-related conditions and medications in use when the test is taken.[41] A slit-lamp examination can reveal dryness on the surface of the eye.
Symptoms of dry mouth and dryness in the oral cavity are caused by the reduced production of saliva from the salivary glands (parotid gland, submandibular gland, and sublingual gland). To check the status of salivary glands and the production of saliva, a salivary flow-rate test is performed, in which the person is asked to spit as much as they can into a cup, and the resulting saliva sample is collected and weighed. This test's results can determine whether the salivary glands are functioning adequately. Not enough saliva produced could mean the person has SS.[41] An alternative test is non-stimulated whole saliva flow collection, in which the person spits into a test tube every minute for 15 minutes. A resultant collection of less than 1.5 ml (0.053 imp fl oz; 0.051 US fl oz) is considered a positive result.[42]
A lip/salivary gland biopsy takes a tissue sample that can reveal lymphocytes clustered around salivary glands, and damage to these glands from inflammation. This test involves removing a sample of tissue from a person’s inner lip/salivary gland and examining it under a microscope. In addition, a sialogram, a special X-ray test, is performed to see if any blockage is present in the salivary gland ducts (i.e. parotid duct) and the amount of saliva that flows into the mouth.[41]
A radiological procedure is available as a reliable and accurate test for SS. A contrast agent is injected into the parotid duct, which opens from the cheek into the vestibule of the mouth opposite the neck of the upper second molar tooth. Histopathology studies should show focal lymphocytic sialadenitis. Objective evidence of salivary gland involvement is tested through ultrasound examinations, the level of unstimulated whole salivary flow, a parotid sialography or salivary scintigraphy, and autoantibodies against Ro (SSA) and/or La (SSB) antigens.
SS can be excluded from people with past head and neck radiation therapy, acquired immunodeficiency syndrome (AIDS), pre-existing lymphoma, sarcoidosis, graft-versus-host disease, and use of anticholinergic drugs.
Prevention
There is no prevention mechanism for Sjögren syndrome because of its complexity as an autoimmune disorder. However, lifestyle changes can reduce the risk factors related to developing SS or reduce the severity of the condition for patients who have already been diagnosed. Diet is strongly associated with the inflammation that is seen in many autoimmune related diseases, including SS. An experimental study concluded that SS patients show high sensitivity to gluten that directly relates to inflammation.[43] Moderate exercise is also helpful in SS patients, mainly reducing the effect of lung inflammation.[44]
Treatment
Neither a cure for Sjögren syndrome nor a specific treatment is known to permanently restore gland secretion. Instead, treatment is generally symptomatic and supportive.
Eye care
Moisture replacement therapies such as artificial tears may ease the symptoms of dry eyes. Some patients with more severe problems use goggles to increase local humidity or have punctal plugs inserted to help retain tears on the ocular surface for a longer time.
Additionally, cyclosporine (Restasis) is available by prescription to treat chronic dry eye by suppressing the inflammation that disrupts tear secretion. Prescription drugs are also available that help to stimulate salivary flow, such as cevimeline (Evoxac) and pilocarpine. Salagen, a manufactured form of pilocarpine, can be used to help produce tears, as well as saliva in the mouth and intestines. It is derived from the jaborandi plant.
Vaginal dryness
In women with SS, vaginal dryness, vulvodynia and dyspareunia (painful sexual intercourse) are often reported; personal lubricants are recommended to help lessen irritation or pain that may result from dryness in the vaginal and vulva areas.[41]
Musculoskeletal
Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to treat musculoskeletal symptoms. For individuals with severe complications, corticosteroids or immunosuppressive drugs may be prescribed, and sometimes IVIG (intravenous immunoglobulin). Also, disease-modifying antirheumatic drugs (DMARDs) such as methotrexate may be helpful. Hydroxychloroquine (Plaquenil) is another option and is generally considered safer than methotrexate. However, these prescribed drugs have a range of side effects such as nausea, loss of appetite, dizziness, hair loss, stomach aches/cramps, headache, liver toxicity, and increased risk of infections. Also, people who take drugs to suppress the immune system are more likely to develop cancer later.[41]
Systemic
For systemic symptoms, including fatigue, joint pain, myositis and neuropathy, biologic immunosuppressant drugs such as rituximab and belimumab that work via B-cell pathology are often used and have less toxic profiles than traditional immunosuppressive regimens.
Dental care
Preventive dental treatment is also necessary (and often overlooked by the patient), as the lack of saliva associated with xerostomia creates an ideal environment for the proliferation of bacteria that cause cavities.[45] Treatments include at-home topical fluoride application to strengthen tooth enamel and frequent teeth cleanings by a dental hygienist. Existing cavities must also be treated, as cavities that extend into the tooth can not be effectively treated through teeth cleaning alone, and are at a high risk of spreading into the pulp of the tooth, leading to the loss of vitality and need for extraction or root canal therapy. This treatment regimen is the same as for all xerostomia patients, such as those undergoing head and neck radiation therapy, which often damages the salivary glands, which are more susceptible to radiation than are other body tissues.
Prognosis
Published studies on the survival of Sjögren syndrome patients are limited in varied respects, perhaps owing to the relatively small sample sizes, and secondary SS is associated with other autoimmune diseases. However, results from a number of studies indicate, compared to other autoimmune diseases, SS is associated with a notably high incidence of malignant non-Hodgkin lymphoma (NHL), a cancer of white blood cells.[21] About 5% of patients with SS develop some form of lymphoid malignancy.[46] Patients with severe cases are much more likely to develop lymphomas than patients with mild or moderate cases.[47] The most common lymphomas are salivary extranodal marginal zone B cell lymphomas (MALT lymphomas in the salivary glands)[48] and diffuse large B-cell lymphoma.[47]
Lymphomagenesis in primary SS patients is considered as a multistep process, with the first step being chronic stimulation of autoimmune B cells, especially B cells that produce rheumatoid factor at sites targeted by the disease.[49][50] This increases the frequency of oncogenic mutation, leading to any dysfunction at checkpoints of autoimmune B-cell activation to transform into malignancy. A study's finding has concluded the continuous stimulation of autoimmune B cells, leading to subtle germinal abnormalities in genes having specific consequences in B cells, which underlies the susceptibility to lymphoma.[51]
Apart from this notably higher incidence of malignant NHL, SS patients show only modest or clinically insignificant deterioration in specific organ-related function, which explains the only slight increases in mortality rates of SS patients in comparison with the remainder of the population.[21]
Epidemiology
SS is the second most common rheumatic autoimmune disorder, behind rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).[10] There are no geographical differences in the rates of SS.[52] SS has been reported in all areas of the world, although regional rates have not been well studied.[52][53] Depending on the criteria for determining prevalence, studies estimate the prevalence of SS at 500,000 to 2 million people in the United States. Moreover, other broader studies of prevalence of SS range widely with some reports of up to a prevalence of 3% of the population.[10] A few studies that have been conducted on the incidence of SS report that the incidence of the syndrome varies between 3 and 6 per 100,000 per year.[10][54]
Nine out of ten SS patients are women.[19][53] In addition to prevalence in women, having a first-degree relative with an autoimmune disease and previous pregnancies have been identified as epidemiological risk factors.[55] Differences in prevalence due to race and ethnicity are unknown.
Although SS occurs in all age groups, the average age of onset is between ages 40 and 60, although experts note that up to half of all cases may be left undiagnosed or unreported.[19][10][56][57] The prevalence of SS generally increases with age.[10]
SS is reported in 30-50% of people with rheumatoid arthritis and 10-25% with systemic lupus erythematosus.[19]
History
Jan Mikulicz-Radecki (1850–1905) is generally credited with the first description of SS. In 1892, he described a 42-year-old man with enlargement of the parotid and lacrimal glands associated with a round-cell infiltrate and acinar atrophy.[41][58] However, the criteria Mikulicz established for diagnosis, often led to misdiagnosis of Mikulicz’s syndrome. Many conditions, such as tuberculosis, infections, sarcoidosis, and lymphoma present with similar conditions to those listed under Mikulicz’s syndrome.[41] Nevertheless, the term "Mikulicz’s syndrome" is still used occasionally to describe the appearance of lymphocytic infiltrates on salivary-gland biopsies.[41]
In 1930, Henrik Sjögren (1899–1986), an ophthalmologist in Jönköping, Sweden, observed a patient with low secretions from the lacrimal and salivary glands.[59] Sjögren introduced the term keratoconjunctivitis sicca for the symptom of dry eyes (keratoconjunctivitis). In 1933, he published his doctoral thesis, describing 19 females, most of whom were postmenopausal and had arthritis, showing clinical and pathological manifestations of the syndrome.[58] Sjögren clarifies that keratoconjunctivitis sicca, resulting from water deficiency, had no relation to xerophthalmia, resulting from vitamin A deficiency.[58] Sjögren's thesis was not well received as the Board of Examiners criticized some clinical aspects.[59]
After extensive research and data collection, Sjögren published an essential paper in 1951, describing 80 patients with keratoconjunctivitis sicca, 50 of whom also had arthritis.[59] His subsequent follow-up conference trips pertaining to his paper led to an international interest in SS.[59] The term keratoconjunctivitis sicca was coined by Sjögren himself and began to be identified as SS in literature,[59] although it can now have more general usage.
Research

Research on multifactorial autoimmune diseases such as SS focuses on expanding the knowledge surrounding the disorder, improving diagnostic tools and finding ways to prevent, manage, and cure the disorder. The United Kingdom Primary Sjögren's Syndrome Registry, a tissue biobank of samples taken for research, supported by the Medical Research Council, UK was established in 2010.[60]
As an autoimmune disease, susceptibility to SS is greatly influenced by the human leukocyte antigen.[61] DQA1*05:01, DQB1*02:01, and DRB1*03:01 alleles were identified as risk factors, while DQA1*02:01, DQA1*03:01 and DQB1*05:01 alleles were found to be protective factors for the disease.[62] The relationship between alleles and specific race was also established.[63] HLA-DQ2 and HLA-B8 are generally found in Caucasian patients, while HLA-DR5 is related to Greek and Israeli patients.[63] Multiple genome-wide association scans may be conducted in the future to identify key risk variants.[61]
Viruses that can trigger the immune response of the syndrome include human T-lymphotropic virus type 1 (HTLV-1), Epstein-Barr virus (EBV), human immunodeficiency virus (HIV) and hepatitis C virus (HCV).[63] The UK Primary Sjögren's Syndrome Registry supports clinical trials and genetic studies of SS and is open to people wishing to participate in research studies and researchers studying the disease.[60]
Some research showed that the lack of vitamin A and vitamin D are associated with this disease.[63] Vitamin D deficiency was found to be related to neurological manifestations and the presence of lymphoma among patients. On the other hand, vitamin A levels were inversely associated with extra-glandular manifestations of the disease.[63]
Saliva is a potential diagnostic tool of SS because the salivary component is changed after onset of the disease.[64] With the new miniaturization technology, called ‘lab on a chip’, the diagnosis can be more convenient.[64]
With regard to therapeutics, multiple monoclonal antibodies were under investigation in 2007.[65] The most promising seemed to be the anti-CD20 rituximab and the anti-CD22 epratuzumab, while the anti-TNF-α and IFN-α seemed less effective.[65]
In 2014, the Sjögren's Syndrome Foundation announced a five-year goal to cut the time to diagnoses in half.[66]
Society and culture
Notable cases
- Shannon Boxx (U.S. Olympic soccer player) has both SS and lupus.[67]
- Carrie Ann Inaba (singer-actress) is the National Awareness Ambassador & Spokesperson for the Sjögren's Syndrome Foundation.[68]
- Venus Williams (world champion tennis player) has been diagnosed with SS and said she had struggled with fatigue for years.[69]
References
- ↑ "Sjogren syndrome". NIH. Archived from the original on 28 January 2021. Retrieved 20 June 2024.
- ↑ Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier, archived from the original on 2014-01-11, retrieved 2014-06-17.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Brito-Zerón, P; Baldini, C; Bootsma, H; Bowman, SJ; Jonsson, R; Mariette, X; Sivils, K; Theander, E; Tzioufas, A; Ramos-Casals, M (7 July 2016). "Sjögren syndrome". Nature Reviews. Disease Primers. 2: 16047. doi:10.1038/nrdp.2016.47. PMID 27383445.
- ↑ 4.0 4.1 4.2 4.3 4.4 Ng, Wan-Fai (2016). Sjogren's Syndrome. Oxford University Press. pp. 10–11. ISBN 9780198736950. Archived from the original on 15 August 2016.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 "What Is Sjögren's Syndrome? Fast Facts". NIAMS. November 2014. Archived from the original on 4 July 2016. Retrieved 15 July 2016.
- ↑ Ferri, Fred F. (2010). Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. p. Chapter S. ISBN 978-0323076999.
- ↑ 7.0 7.1 Singh, AG; Singh, S; Matteson, EL (March 2016). "Rate, risk factors and causes of mortality in patients with Sjögren's syndrome: a systematic review and meta-analysis of cohort studies". Rheumatology. 55 (3): 450–60. doi:10.1093/rheumatology/kev354. PMC 5009445. PMID 26412810.
- ↑ 8.0 8.1 8.2 8.3 John H., Klippel (2008). Primer on the rheumatic diseases (13th ed.). New York, New York: Springer. p. 389. ISBN 9780387685663. Archived from the original on 15 August 2016. Retrieved 15 July 2016.
- ↑ 9.0 9.1 9.2 "Sjögren's Syndrome Information Page". nih.gov. Archived from the original on 19 May 2018. Retrieved 18 May 2018.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 Fox RI, Stern M, Michelson P (September 2000). "Update in Sjögren syndrome". Curr Opin Rheumatol. 12 (5): 391–8. doi:10.1097/00002281-200009000-00007. PMID 10990175.
- ↑ "Indian Rheumatology Association | IRA E-NEWSLETTER". www.indianrheumatology.org. Archived from the original on 6 July 2020. Retrieved 6 July 2020.
- ↑ Manthorpe, R; Svensson, A; Wirestrand, LE (November 2004). "Late neonatal lupus erythematosus onset in a child born of a mother with primary Sjögren's syndrome". Ann. Rheum. Dis. 63 (11): 1496–7. doi:10.1136/ard.2003.014944. PMC 1754813. PMID 15479901.
- ↑ Ramos-Casals, Manel; Cervera, Ricard; Yagüe, Jordi; García-Carrasco, Mario; Trejo, Olga; Jiménez, Sonia; Morlà, Rosa M; Font, Josep; Ingelmo, Miguel (December 1998). "Cryoglobulinemia in primary Sjögren's syndrome: prevalence and clinical characteristics in a series of 115 patients". Semin Arthritis Rheum. 28 (3): 200–5. doi:10.1016/S0049-0172(98)80037-1. PMID 9872481.
- ↑ "Symptoms". Sjögren’s Foundation. Archived from the original on 19 April 2020. Retrieved 14 April 2020.
- ↑ Lundin KE, Wijmenga C (Sep 2015). "Coeliac disease and autoimmune disease–genetic overlap and screening". Nat Rev Gastroenterol Hepatol (Review). 12 (9): 507–15. doi:10.1038/nrgastro.2015.136. PMID 26303674.
- ↑ Denham JM, Hill ID (August 2013). "Celiac disease and autoimmunity: review and controversies". Curr Allergy Asthma Rep (Review). 13 (4): 347–53. doi:10.1007/s11882-013-0352-1. PMC 3725235. PMID 23681421.
- ↑ 17.0 17.1 Gabriel SE, Michaud K (2009). "Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases". Arthritis Res Ther (Review). 11 (3): 229. doi:10.1186/ar2669. PMC 2714099. PMID 19519924.
- ↑ Papageorgiou A, Voulgarelis M, Tzioufas AG (Jul 2015). "Clinical picture, outcome and predictive factors of lymphoma in Sjӧgren syndrome". Autoimmun Rev (Review). 14 (7): 641–9. doi:10.1016/j.autrev.2015.03.004. PMID 25808075.
- ↑ 19.0 19.1 19.2 19.3 19.4 Borchers AT, Naguwa SM, Keen CL, Gershwin ME (August 2003). "Immunopathogenesis of Sjögren's syndrome". Clin Rev Allergy Immunol. 25 (1): 89–104. doi:10.1385/CRIAI:25:1:89. PMID 12794264.
- ↑ Martín-Nares, Eduardo; Hernández-Molina, Gabriela (February 2019). "Novel autoantibodies in Sjögren's syndrome: A comprehensive review". Autoimmunity Reviews. 18 (2): 192–198. doi:10.1016/j.autrev.2018.09.003. PMID 30572138.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 21.7 21.8 21.9 Voulgarelis M., Tzioufas A. G. (2010). "Pathogenetic mechanisms in the initiation and perpetuation of Sjögren's syndrome". Nature Reviews. Rheumatology. 6 (9): 529–537. doi:10.1038/nrrheum.2010.118. PMID 20683439.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 Delaleu N, Jonsson R, Koller MM (April 2005). "Sjögren's syndrome". Eur. J. Oral Sci. 113 (2): 101–13. doi:10.1111/j.1600-0722.2004.00183.x. PMID 15819815.
- ↑ 23.0 23.1 Whitacre C. C. (2001). "Sex differences in autoimmune disease". Nat. Immunol. 2 (9): 777–780. doi:10.1038/ni0901-777. PMID 11526384.
- ↑ Kelly, Anzola Luz; Nelson, Rivera Jose; Sara, Ramírez; Alberto, Signore (4 September 2022). "Sjögren Syndrome: New Insights in the Pathogenesis and Role of Nuclear Medicine". Journal of Clinical Medicine. 11 (17): 5227. doi:10.3390/jcm11175227. ISSN 2077-0383.
- ↑ Harboe, Erna; Tjensvoll, Anne Bolette; Vefring, Hege K.; Gøransson, Lasse G.; Kvaløy, Jan Terje; Omdal, Roald (2009). "Fatigue in primary Sjögren's syndrome – A link to sickness behaviour in animals?". Brain, Behavior, and Immunity. 23 (8): 1104–8. doi:10.1016/j.bbi.2009.06.151. PMID 19560535.
- ↑ Perrier, S; Coussediere, C; Dubost, JJ; Albuisson, E; Sauvezie, B (1998). "IL-1 receptor antagonist (IL-1RA) gene polymorphism in Sjögren's syndrome and rheumatoid arthritis". Clinical Immunology and Immunopathology. 87 (3): 309–13. doi:10.1006/clin.1998.4520. PMID 9646842.
- ↑ Reveille, JD (October 1992). "The molecular genetics of systemic lupus erythematosus and Sjögren's syndrome". Current Opinion in Rheumatology. 4 (5): 644–56. PMID 1419498.
- ↑ Lessard CJ, Li H, Adrianto I, Ice JA, Jonsson R, Illei GG, Rischmueller M (2014). "OP0020 Identification of Multiple Sjögren's Syndrome Susceptibility Loci". Annals of the Rheumatic Diseases. 72 (Suppl 3): A54.3–A55. doi:10.1136/annrheumdis-2013-eular.225. ISSN 0003-4967.
- ↑ Kang HI, Fei HM, Saito I, Sawada S, Chen SL, Yi D, Chan E, Peebles C, Bugawan TL, Erlich HA (April 1993). "Comparison of HLA class II genes in Caucasoid, Chinese, and Japanese patients with primary Sjögren's syndrome". J. Immunol. 150 (8 Pt 1): 3615–23. PMID 8468491.
- ↑ Bolstad AI, Wassmuth R, Haga HJ, Jonsson R (July 2001). "HLA markers and clinical characteristics in Caucasians with primary Sjögren's syndrome". J. Rheumatol. 28 (7): 1554–62. PMID 11469461.
- ↑ Fei HM, Kang H, Scharf S, Erlich H, Peebles C, Fox R (1991). "Specific HLA-DQA and HLA-DRB1 alleles confer susceptibility to Sjögren's syndrome and autoantibody production". J. Clin. Lab. Anal. 5 (6): 382–91. doi:10.1002/jcla.1860050604. PMID 1685512.
- ↑ Lu Q (2013). "The critical importance of epigenetics in autoimmunity". J. Autoimmun. 41: 1–5. doi:10.1016/j.jaut.2013.01.010. PMID 23375849.
- ↑ Takeda K, Kaisho T, Akira S (2003). "Toll-like receptors". Annu. Rev. Immunol. 21: 335–76. doi:10.1146/annurev.immunol.21.120601.141126. PMID 12524386.
- ↑ Pflugfelder SC, Crouse CA, Monroy D, Yen M, Rowe M, Atherton SS (July 1993). "Epstein-Barr virus and the lacrimal gland pathology of Sjögren's syndrome". Am. J. Pathol. 143 (1): 49–64. PMC 1886957. PMID 8391219.
- ↑ Manoussakis MN, Boiu S, Korkolopoulou P, Kapsogeorgou EK, Kavantzas N, Ziakas P, Patsouris E, Moutsopoulos HM (December 2007). "Rates of infiltration by macrophages and dendritic cells and expression of interleukin-18 and interleukin-12 in the chronic inflammatory lesions of Sjögren's syndrome: correlation with certain features of immune hyperactivity and factors associated with high risk of lymphoma development". Arthritis Rheum. 56 (12): 3977–88. doi:10.1002/art.23073. PMID 18050195.
- ↑ Ohlsson M, Szodoray P, Loro LL, Johannessen AC, Jonsson R (December 2002). "CD40, CD154, Bax and Bcl-2 expression in Sjögren's syndrome salivary glands: a putative anti-apoptotic role during its effector phases". Scand. J. Immunol. 56 (6): 561–71. doi:10.1046/j.1365-3083.2002.01168.x. PMID 12472667.
- ↑ Ohlsson M, Skarstein K, Bolstad AI, Johannessen AC, Jonsson R (January 2001). "Fas-induced apoptosis is a rare event in Sjögren's syndrome". Lab. Invest. 81 (1): 95–105. doi:10.1038/labinvest.3780215. PMID 11204278.
- ↑ Cutolo M, Sulli A, Capellino S, Villaggio B, Montagna P, Seriolo B, Straub RH (2004). "Sex hormones influence on the immune system: basic and clinical aspects in autoimmunity". Lupus. 13 (9): 635–8. doi:10.1191/0961203304lu1094oa. PMID 15485092.
- ↑ Mavragani CP, Fragoulis GE, Moutsopoulos HM (Dec 2012). "Endocrine alterations in primary Sjogren's syndrome: an overview". J Autoimmun (Review). 39 (4): 354–8. doi:10.1016/j.jaut.2012.05.011. PMID 22695186.
- ↑ Sullivan DA, Wickham LA, Rocha EM, Krenzer KL, Sullivan BD, Steagall R, Cermak JM, Dana MR, Ullman MD, Sato EH, Gao J, Rocha FJ, Ono M, Silveira LA, Lambert RW, Kelleher RS, Tolls DB, Toda I (1999). "Androgens and dry eye in Sjögren's syndrome". Ann N Y Acad Sci. 876 (1): 312–24. Bibcode:1999NYASA.876..312S. doi:10.1111/j.1749-6632.1999.tb07656.x. PMID 10415627.
- ↑ 41.0 41.1 41.2 41.3 41.4 41.5 41.6 41.7 41.8 41.9 Fox R. I. (2005). "Sjögren's syndrome". Lancet. 366 (9482): 321–331. doi:10.1016/s0140-6736(05)66990-5. PMID 16039337.
- ↑ Dr. J. Parks, Ancaster ON Canada
- ↑ Lidén M, Kristjánsson G, Valtýsdóttir S, Hällgren R (August 2007). "Gluten sensitivity in patients with primary Sjögren's syndrome". Scand. J. Gastroenterol. 42 (8): 962–7. doi:10.1080/00365520701195345. PMID 17613926.
- ↑ Strömbeck BE, Theander E, Jacobsson LT (May 2007). "Effects of exercise on aerobic capacity and fatigue in women with primary Sjogren's syndrome". Rheumatology (Oxford). 46 (5): 868–71. doi:10.1093/rheumatology/kem004. PMID 17308315.
- ↑ Xin, W; Leung, KC; Lo, EC; Mok, MY; Leung, MH (2016). "A randomized, double-blind, placebo-controlled clinical trial of fluoride varnish in preventing dental caries of Sjögren's syndrome patients". BMC Oral Health. 16 (1): 102. doi:10.1186/s12903-016-0296-7. PMC 5034648. PMID 27664129.
- ↑ Tzioufas, Athanasios G.; Voulgarelis, Michael (2007). "Update on Sjögren's syndrome autoimmune epithelitis: from classification to increased neoplasias". Best Pract Res Clin Rheumatol. 21 (6): 989–1010. doi:10.1016/j.berh.2007.09.001. PMID 18068857.
- ↑ 47.0 47.1 Smedby, K. E.; Baecklund, E.; Askling, J. (2006). "Malignant lymphomas in autoimmunity and inflammation: a review of risks, risk factors, and lymphoma characteristics". Cancer Epidemiol. Biomarkers Prev. 15 (11): 2069–77. doi:10.1158/1055-9965.EPI-06-0300. PMID 17119030.
- ↑ Voulgarelis, Michael; Skopouli, Fotini N. (2007). "Clinical, immunologic, and molecular factors predicting lymphoma development in Sjogren's syndrome patients". Clin Rev Allergy Immunol. 32 (3): 265–74. doi:10.1007/s12016-007-8001-x. PMID 17992593.
- ↑ Martin T, Weber JC, Levallois H, Labouret N, Soley A, Koenig S, Korganow AS, Pasquali JL (April 2000). "Salivary gland lymphomas in patients with Sjögren's syndrome may frequently develop from rheumatoid factor B cells". Arthritis Rheum. 43 (4): 908–16. doi:10.1002/1529-0131(200004)43:4<908::AID-ANR24>3.0.CO;2-K. PMID 10765938.
- ↑ Bende RJ, Aarts WM, Riedl RG, de Jong D, Pals ST, van Noesel CJ (April 2005). "Among B cell non-Hodgkin's lymphomas, MALT lymphomas express a unique antibody repertoire with frequent rheumatoid factor reactivity". J. Exp. Med. 201 (8): 1229–41. doi:10.1084/jem.20050068. PMC 2213160. PMID 15837810.
- ↑ Nocturne G, Boudaoud S, Miceli Richard C, Viengchareun S, Lazure T, Nititham J, et al. (2014). "OP0023 Germinal and Somatic Genetic Variants of TNFAIP3 Promote Lymphomagenesis Process Complicating Primary Sjögren's Syndrome". Annals of the Rheumatic Diseases. 72 (Suppl 3): A55.3–A56. doi:10.1136/annrheumdis-2013-eular.228. ISSN 0003-4967.
- ↑ 52.0 52.1 Mavragani C. P., Moutsopoulos H. M. (2010). "The geoepidemiology of Sjogren's syndrome". Autoimmunity Reviews. 9 (5): A305–A310. doi:10.1016/j.autrev.2009.11.004. PMID 19903539.
- ↑ 53.0 53.1 Jonsson R, Vogelsang P, Volchenkov R, Espinosa A, Wahren-Herlenius M, Appel S (December 2011). "The complexity of Sjögren's syndrome: novel aspects on pathogenesis". Immunol. Lett. 141 (1): 1–9. doi:10.1016/j.imlet.2011.06.007. PMID 21777618.
- ↑ Alamanos Y, Tsifetaki N, Voulgari PV, Venetsanopoulou AI, Siozos C, Drosos AA (February 2006). "Epidemiology of primary Sjögren's syndrome in north-west Greece, 1982-2003". Rheumatology (Oxford). 45 (2): 187–91. doi:10.1093/rheumatology/kei107. PMID 16332955.
- ↑ Priori R, Medda E, Conti F, Cassarà EA, Sabbadini MG, Antonioli CM, Gerli R, Danieli MG, Giacomelli R, Pietrogrande M, Valesini G, Stazi MA (2007). "Risk factors for Sjögren's syndrome: a case-control study". Clin. Exp. Rheumatol. 25 (3): 378–84. PMID 17631733.
- ↑ Haugen AJ, Peen E, Hultén B, Johannessen AC, Brun JG, Halse AK, Haga HJ (2008). "Estimation of the prevalence of primary Sjögren's syndrome in two age-different community-based populations using two sets of classification criteria: the Hordaland Health Study". Scand. J. Rheumatol. 37 (1): 30–4. doi:10.1080/03009740701678712. PMID 18189192.
- ↑ García-Carrasco M, Ramos-Casals M, Rosas J, Pallarés L, Calvo-Alen J, Cervera R, Font J, Ingelmo M (July 2002). "Primary Sjögren syndrome: clinical and immunologic disease patterns in a cohort of 400 patients". Medicine (Baltimore). 81 (4): 270–80. doi:10.1097/00005792-200207000-00003. PMID 12169882.
- ↑ 58.0 58.1 58.2 Parke AL, Buchanan WW (1998). "Sjögren's syndrome: History, clinical and pathological features". Inflammopharmacology. 6 (4): 271–87. doi:10.1007/s10787-998-0012-6. PMID 17657625.
- ↑ 59.0 59.1 59.2 59.3 59.4 Murube, J. Henrik Sjögren, 1899–1986. The ocular surface 8, 2-2 (2010)
- ↑ 60.0 60.1 Ng, W.-F.; Bowman, S. J.; Griffiths, B.; Ukpssr Study, Group (January 2011). "United Kingdom Primary Sjogren's Syndrome Registry--a united effort to tackle an orphan rheumatic disease". Rheumatology (Oxford). 50 (1): 32–9. doi:10.1093/rheumatology/keq240. PMID 20693261.
- ↑ 61.0 61.1 Ice, John A.; Li, He; Adrianto, Indra; Lin, Paul Chee; Kelly, Jennifer A.; Montgomery, Courtney G.; Lessard, Christopher J.; Moser, Kathy L. (August 2012). "Genetics of Sjögren's syndrome in the genome-wide association era". J. Autoimmun. 39 (1–2): 57–63. doi:10.1016/j.jaut.2012.01.008. PMC 3518871. PMID 22289719.
- ↑ Cruz-Tapias, Paola; Rojas-Villarraga, Adriana; Maier-Moore, Shannon; Anaya, Juan-Manuel (February 2012). "HLA and Sjögren's syndrome susceptibility. A meta-analysis of worldwide studies". Autoimmun Rev. 11 (4): 281–7. doi:10.1016/j.autrev.2011.10.002. PMID 22001416.
- ↑ 63.0 63.1 63.2 63.3 63.4 Peri, Yogev; Agmon-Levin, Nancy; Theodor, Emanuel; Shoenfeld, Yehuda (February 2012). "Sjögren's syndrome, the old and the new". Best Pract Res Clin Rheumatol. 26 (1): 105–17. doi:10.1016/j.berh.2012.01.012. PMID 22424197.
- ↑ 64.0 64.1 Liu, Jingyi; Duan, Yixiang (July 2012). "Saliva: a potential media for disease diagnostics and monitoring". Oral Oncol. 48 (7): 569–77. doi:10.1016/j.oraloncology.2012.01.021. PMID 22349278.
- ↑ 65.0 65.1 Meijer, Jiska M.; Pijpe, Justin; Bootsma, Hendrika; Vissink, Arjan; Kallenberg, Cees G. M. (June 2007). "The future of biologic agents in the treatment of SS". Clin Rev Allergy Immunol. 32 (3): 292–7. doi:10.1007/s12016-007-8005-6. PMC 2071970. PMID 17992596.
- ↑ ""Breakthrough Goal" SSF Launches 5-Year Breakthrough Goal/"To shorten the time to diagnose Sjögren's by 50% in 5 years!"". Sjogren's Syndrome Foundation. August 2016. Archived from the original on 13 August 2014.
- ↑ "Olympic soccer player Shannon Boxx's battle with lupus". CNN. 2012. Archived from the original on 22 February 2014. Retrieved 18 February 2014.
- ↑ Sjogren's Syndrome Foundation Thanks Carrie Ann Inaba for Helping Raise Awareness Archived 8 September 2017 at the Wayback Machine
- ↑ "Williams Says She Struggled With Fatigue for Years". NY Times. 2011. Archived from the original on 10 September 2012. Retrieved 18 February 2014.
- Some of the original text for this article was obtained from a public domain resource at NIH Archived 2008-10-14 at the Wayback Machine
External links
| Classification | |
|---|---|
| External resources |
- Sjögren syndrome at NHS Choices Archived 2017-10-15 at the Wayback Machine
- Sjögren syndrome Archived 2018-06-27 at the Wayback Machine – US National Institute of Arthritis and Musculoskeletal and Skin Diseases
- Price, EJ; Rauz, S; Tappuni, AR; Sutcliffe, N; Hackett, KL; Barone, F; Granata, G; Ng, WF; Fisher, BA; Bombardieri, M; Astorri, E; Empson, B; Larkin, G; Crampton, B; Bowman, SJ; British Society for Rheumatology Standards, Guideline and Audit Working, Group. (1 October 2017). "The British Society for Rheumatology guideline for the management of adults with primary Sjögren's Syndrome". Rheumatology. 56 (10): e24–e48. doi:10.1093/rheumatology/kex166. PMID 28957550.