Belimumab
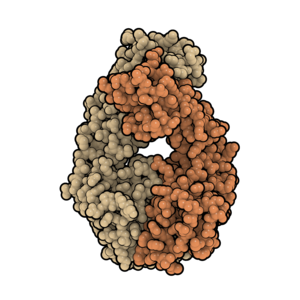 Fab fragment of belimumab. PDB: 5Y9K. | |
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Human |
| Target | B-cell activating factor (BAFF, BLyS) |
| Names | |
| Trade names | Benlysta |
| Other names | LymphoStat-B |
| Clinical data | |
| Main uses | Systemic lupus erythematosus (SLE), lupus nephritis[1] |
| Side effects | Respiratory tract infections, diarrhea, shingles[2] |
| Pregnancy category | |
| Routes of use | Intravenous |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a611027 |
| Legal | |
| License data | |
| Legal status | |
| Chemical and physical data | |
| Formula | C6714H10428O2102S52 |
| Molar mass | 126450.30 g·mol−1 |
Belimumab, sold under the brand name Benlysta, is a medication used to treat systemic lupus erythematosus (SLE) or lupus nephritis.[1] It is used in addition to other treatments, when those are not sufficient.[4] It is given by injection into a vein or under the skin.[1]
Common side effects include respiratory tract infections, diarrhea, and shingles.[2] Other side effects may include infusion reactions, progressive multifocal leukoencephalopathy, depression, and anaphylaxis.[2][1] It is a monoclonal antibody that attaches too and blocks B-cell activating factor (BAFF), shortening the lifespan of B lymphocytes.[2]
Belimumab was approved for medical use in the United States and Europe in 2011.[2][1] In the United Kingdom 400 mg costs the NHS about £405 as of 2021.[4] This amount in the United States costs about 1,950 USD.[5]
Medical uses
Belimumab is primarily used in patients with systemic lupus erythematosus. When it was introduced in 2011, it was the first new drug approved to treat lupus in 56 years.[6]
Clinical trials found belimumab to be safe in treating SLE,[7] but the magnitude of benefit was small,[6] and Phase III trials excluded the most severe cases of SLE, involving kidney and brain damage. Reviewers at the United States Food and Drug Administration (FDA) expressed concern that the drug was only "marginally" effective, and that there were more deaths in the treatment group. Defenders said that in addition to its modest efficiency, belimumab allowed patients to significantly reduce their use of corticosteroids.[8]
In December 2020 belimumab was approved by the FDA as a treatment for lupus nephritis in combination with standard treatment.[9]
Dosage
It is given at a dose of 10 mg/kg injected into a vein every two weeks for three doses and than every four weeks.[1] In adults with SLE it may also be injected under the skin at a dose of 200 mg once per week.[1]
Side effects
Common side effects reported with belimumab include nausea, diarrhea, and fever, as well as hypersensitivity and infusion-site reactions, which were severe in 0.9% of patients. Regulatory agencies recommend that patients be treated with an antihistamine prior to a belimumab infusion.[10]
Because belimumab is an immunosuppressant, more serious infections and deaths were reported among patients treated with the drug than among those treated with placebo.[11]
No interaction studies have been carried out, but combining belimumab with other immunosuppressants—especially those targeting B lymphocytes, such as anti-CD20 therapies—could increase the risk of severe infections. Likewise, combining belimumab with intravenous cyclophosphamide or live vaccines is not recommended.[1][10]
Mechanism of action

B lymphocytes (B cells), which are part of the normal immune response, are also responsible for the over-aggressive response seen in autoimmune diseases like SLE. B cells develop in the bone marrow and continue to mature peripherally in secondary lymphoid organs and in the gut. When autoimmune B cells attack the body's own tissues, they are normally destroyed by cell suicide (apoptosis). Researchers theorize that SLE is caused when autoimmune B cells proliferate and survival factors protect them from cell suicide.
B-cell activating factor (BAFF), also called B-lymphocyte stimulator (BLyS), is required for the development and survival of B cells. In SLE patients, BAFF is overexpressed, which may cause autoimmune B cell proliferation and survival. Belimumab binds to BAFF and prevents it from binding to B cells. Without BAFF, B cells commit suicide and no longer contribute to the autoimmune damage of SLE.
BAFF is secreted by a variety of cells: monocytes and macrophages; bone marrow stromal cells; astrocytes in certain glioblastomas; synoviocytes in rheumatoid arthritis; and salivary epithelial cells in Sjögren syndrome. It interacts with three membrane receptors on B lymphocytes:
- BAFF-R (BAFF receptor)
- BCMA (B cell maturation antigen)
- TACI (transmembrane activator and calcium modulator and cyclophylin ligand interactor)
When BAFF binds to BAFF-R and BCMA on B cells, levels of Bcl-2, a survival factor, are increased. When all three BAFF receptors are stimulated, levels of NF kappa B, which contributes to cell proliferation and differentiation, are increased in the nucleus.
Another B-cell activator similar to BAFF is APRIL (A proliferation-inducing ligand),[12] but APRIL activates only BCMA and TACI, not BAFF-R.
Belimumab reduces the number of circulating B cells, but anti-CD20 monoclonal antibodies reduce the number even more. It is possible that belimumab binds primarily to circulating soluble BAFF and therefore does not induce the antibody-dependent cellular cytotoxicity that could be expected from this IgG1-type antibody.[13]
History
B-cell activating factor is a naturally occurring protein that was discovered by researchers from National Jewish Health (previously the National Jewish Medical and Research Center) and the University of Colorado, who jointly published a paper detailing their findings in May 1999 and named the protein TALL-1.[14] The same protein was named BAFF in another paper published in June 1999, and in a paper published in July of that year, Human Genome Sciences (HGS) referred to it as BLyS (short for B lymphocyte stimulator).[15] Six years later, research showing the key role of BLyS in B cell differentiation, survival, and activation was published.[16]
In October 2000, HGS and Cambridge Antibody Technology (CAT) agreed to co-develop monoclonal antibodies targeted at BLyS. Under this agreement, CAT would identify antibodies and HGS would select appropriate ones to take into clinical trials.[17] In 2003, CAT researchers reported that, by using phage display technology, they had elicited an array of more than 1,000 distinct antibodies, half of which inhibited binding of BLyS to its receptor.[18] Later that year, one of these antibodies was isolated and characterized. It was named LymphoStat-B and subsequently called belimumab.[19]
In August 2006, HGS and GlaxoSmithKline (GSK) entered into a co-development and commercialization agreement under which HGS would conduct Phase III trials for belimumab with assistance from GSK. The companies would share equally in Phase III/IV development costs, sales and marketing expenses, and profits of any product commercialized under the agreement.[17] On February 13, 2007, HGS and GSK announced the initiation of the first of two Phase III clinical trials of belimumab in patients with active lupus erythematosus.[20]
Two Phase III clinical studies were conducted, involving a total of 1,684 patients with scores of ≥6 on the SELENA-SLEDAI assessment of lupus activity. The primary end point was a reduction of ≥4 on the SELENA-SLEDAI assessment, and several other factors, after 52 weeks. Belimumab significantly improved the response rate, reduced disease activity and severe flares, and was well tolerated. Among patients treated with belimumab (10mg/kg) in addition to standard therapy, 58% had SELENA-SLEDAI scores reduced by ≥4 points over 52 weeks, compared with 46% of patients treated with placebo.[21][22] However, patients of African-American or African descent did not respond significantly to belimumab.[23][24][25]
These trials did not include patients with the most severe forms of SLE, which involve active damage to the kidneys or central nervous system. Subjects with active kidney disease were included in Phase II trials.[26]
FDA approval
Under the trade name Benlysta, belimumab received FDA approval for the treatment of SLE on March 9, 2011,[27] despite concerns among advisory committee members that the improvement of 4 points on the SELENA-SLEDA scale was marginal, and despite reservations about additional deaths in the treatment group.[23][28] It was subsequently approved in Canada and the European Union as well.[29][2]
Based on the number needed to treat, approximately eleven patients must be treated for one to benefit.[medical citation needed]
Society and culture
Cost
At a typical U.S. academic center, the total cost for the first year of treatment with belimumab is $28,000.[30] Belimumab is more expensive than other drugs used to treat lupus, including prednisone ($140 per year), hydroxychloroquine ($132), oral methotrexate ($432), azathioprine ($468), and mycophenolate mofetil ($1,224).[30]
Sales rose to $31.2 million in the first quarter of 2012.[31]
In the United Kingdom, the National Institute for Health and Care Excellence calculated the cost of belimumab at £61,200 per quality-adjusted life year (QALY). This is more than the normally accepted cost of £20,000 to £30,000 per QALY. The manufacturer offered the UK National Health Service a discount of a confidential amount, which still did not bring it into the acceptable range.[32]
Related drugs
Blisibimod, an inhibitor of both soluble and membrane-bound BAFF, has demonstrated similar reductions of B cells in clinical trials and is being investigated in a Phase II clinical study for patients with lupus.
BR3-Fc, a recombinant fusion protein built with the extracellular ligand-binding portion of BAFF-R, blocks activation of this receptor by BLyS and is in early-stage pharmaceutical development.[33]
Rituximab, an anti-CD20 monoclonal antibody, has been approved for some indications. Ocrelizumab, ofatumumab, and "third-generation" anti-CD20 monoclonals are in development.
Other drugs addressing B lymphocyte hyperactivity include atacicept, a recombinant fusion protein that is built with the extracellular ligand binding portion of TACI and blocks activation of TACI by APRIL and BLyS. It failed a Phase II trial for multiple sclerosis.[34][35]
Research
Belimumab was not effective in Phase II clinical trials for rheumatoid arthritis.[36] It was moderately effective in Phase II trials for Sjögren syndrome.[37]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 "Benlysta- belimumab injection, powder, lyophilized, for solution Benlysta- belimumab solution". DailyMed. 17 January 2020. Archived from the original on 25 September 2020. Retrieved 29 July 2020.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 "Benlysta EPAR". European Medicines Agency (EMA). Archived from the original on 25 October 2020. Retrieved 29 July 2020.
- ↑ 3.0 3.1 "Belimumab (Benlysta) Use During Pregnancy". Drugs.com. 5 February 2020. Archived from the original on 4 December 2020. Retrieved 29 July 2020.
- ↑ 4.0 4.1 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 891. ISBN 978-0857114105.
- ↑ "Benlysta Prices, Coupons & Patient Assistance Programs". Drugs.com. Retrieved 8 January 2022.
- ↑ 6.0 6.1 Belimumab: The first drug to be FDA approved for the treatment of lupus since 1955 Archived 2021-09-13 at the Wayback Machine, By Rebecca Manno, Johns Hopkins Arthritis Center, July 15, 2011
- ↑ Lee, Y. H.; Song, G. G. (2018). "Comparative efficacy and safety of intravenous or subcutaneous belimumab in combination with standard therapy in patients with active systemic lupus erythematosus: A Bayesian network meta-analysis of randomized controlled trials". Lupus. 27 (1): 112–119. doi:10.1177/0961203317713143. PMID 28592201. S2CID 26026994.
- ↑ "Should Belimumab Have Been Approved? Stephen Paget, Medscape Rheumatology, Mar 24, 2011". Archived from the original on November 16, 2015. Retrieved October 20, 2021.
- ↑ "FDA Approves Belimumab & Voclosporin for Lupus Nephritis". The Rheumatologist. 24 March 2021. Archived from the original on 5 May 2021. Retrieved 20 October 2021.
- ↑ 10.0 10.1 European Medicines Agency: Benlysta Summary of Product Characteristics Archived 2018-06-18 at the Wayback Machine
- ↑ "GlaxoSmithKline and Human Genome Sciences announce FDA approval of Benlysta (belimumab) for the treatment of systemic lupus erythematosus". GlaxoSmithKline. 9 March 2011. Archived from the original on March 17, 2011. Retrieved 11 March 2011.
- ↑ Schneider P (2005). "The role of APRIL and BAFF in lymphocyte activation" (PDF). Curr. Opin. Immunol. 17 (3): 282–9. doi:10.1016/j.coi.2005.04.005. PMID 15886118.
- ↑ June 2007 European League against Rheumatism symposium.
- ↑ Shu HB, Hu WH, Johnson H (May 1999). "TALL-1 is a novel member of the TNF family that is down-regulated by mitogens". J. Leukoc. Biol. 65 (5): 680–3. doi:10.1002/jlb.65.5.680. PMID 10331498. S2CID 1498303.
- ↑ Moore PA, Belvedere O, Orr A, Pieri K, LaFleur DW, Feng P, et al. (July 1999). "BLyS: member of the tumor necrosis factor family and B lymphocyte stimulator". Science. 285 (5425): 260–3. doi:10.1126/science.285.5425.260. PMID 10398604.
- ↑ Crowley JE, Treml LS, Stadanlick JE, Carpenter E, Cancro MP (2005). "Homeostatic niche specification among naïve and activated B cells: a growing role for the BLyS family of receptors and ligands". Semin. Immunol. 17 (3): 193–9. doi:10.1016/j.smim.2005.02.001. PMID 15826824.
- ↑ 17.0 17.1 "Benlysta (belimumab)". Human Genome Sciences. Archived from the original on 21 April 2011. Retrieved 2011-03-11.
- ↑ Edwards BM, Barash SC, Main SH (November 2003). "The remarkable flexibility of the human antibody repertoire; isolation of over one thousand different antibodies to a single protein, BLyS". J. Mol. Biol. 334 (1): 103–18. doi:10.1016/j.jmb.2003.09.054. PMID 14596803.
- ↑ Baker KP, Edwards BM, Main SH (November 2003). "Generation and characterization of LymphoStat-B, a human monoclonal antibody that antagonizes the bioactivities of B lymphocyte stimulator". Arthritis Rheum. 48 (11): 3253–65. doi:10.1002/art.11299. PMID 14613291.
- ↑ "Human Genome Sciences And Glaxosmithkline Announce Initiation Of Phase 3 Clinical Trial Of Lymphostat-B In Systemic Lupus Erythematosus" (Press release). Human Genome Sciences. 2007-02-13. Archived from the original on 25 April 2011. Retrieved 2011-03-11.
- ↑ Furie R, Petri M, Zamani O, Cervera R, Wallace DJ, Tegzová D, et al. (BLISS-76 Study Group) (December 2011). "A phase III, randomized, placebo-controlled study of belimumab, a monoclonal antibody that inhibits B lymphocyte stimulator, in patients with systemic lupus erythematosus". Arthritis Rheum. 63 (12): 3918–30. doi:10.1002/art.30613. PMC 5007058. PMID 22127708.
- ↑ 23.0 23.1 FDA Questions Safety, Efficacy of Belimumab Archived 2021-03-03 at the Wayback Machine, By Emily P. Walker, Washington Correspondent, MedPage Today, November 12, 2010
- ↑ Summary Minutes of the Arthritis Advisory Committee Meeting November 16, 2010 Archived March 4, 2017, at the Wayback Machine U.S. Food and Drug Administration (FDA)
- ↑ 2010 Meeting Materials, Arthritis Advisory Committee Archived 2012-03-29 at the Wayback Machine U.S. Food and Drug Administration (FDA)
- ↑ Andrew Pollack, "F.D.A. Approves Benlysta, a New Lupus Drug" Archived 2020-11-12 at the Wayback Machine, The New York Times, March 9, 2011
- ↑ "FDA approves Benlysta to treat lupus" (Press release). U.S. Food and Drug Administration (FDA). March 9, 2011. Archived from the original on March 11, 2011.
- ↑ Pollack A (16 November 2010). "Benlysta, Lupus Treatment, Endorsed by F.D.A." The New York Times. Archived from the original on 9 November 2020. Retrieved 29 July 2020.
- ↑ DrugBank DB08879
- ↑ 30.0 30.1 Hahn BH (April 18, 2013). "Belimumab for Systemic Lupus Erythematosus". N Engl J Med. 368 (16): 1528–1535. doi:10.1056/NEJMct1207259. PMID 23594005.
- ↑ HGSI Cuts Loss on Benlysta Sales Archived 2019-04-07 at the Wayback Machine, By Zacks Equity Research, Apr 26, 2012
- ↑ NICE publishes draft guidance on belimumab for systemic lupus erythematosus Archived 2012-09-12 at the Wayback Machine, press release, 26 April 2012
- ↑ Vugmeyster Y, Seshasayee D, Chang W, Storn A, Howell K, Sa S, et al. (2006). "A Soluble BAFF Antagonist, BR3-Fc, Decreases Peripheral Blood B Cells and Lymphoid Tissue Marginal Zone and Follicular B Cells in Cynomolgus Monkeys". The American Journal of Pathology. 168 (2): 476–489. doi:10.2353/ajpath.2006.050600. PMC 1606502. PMID 16436662.
- ↑ Clinical trial number NCT00642902 for "Atacicept in Multiple Sclerosis, Phase II" at ClinicalTrials.gov
- ↑ Kappos, Ludwig; Hartung, Hans-Peter; Freedman, Mark S.; Boyko, Alexey; Radü, Ernst Wilhelm; Mikol, Daniel D.; Lamarine, Marc; Hyvert, Yann; Freudensprung, Ulrich; Plitz, Thomas; Van Beek, Johan; ATAMS Study Group (2014). "Atacicept in multiple sclerosis (ATAMS): A randomised, placebo-controlled, double-blind, phase 2 trial". The Lancet Neurology. 13 (4): 353–363. doi:10.1016/S1474-4422(14)70028-6. PMID 24613349. S2CID 38926361.
- ↑ Clinical trial number NCT00071812 for "A Safety and Efficacy Study of LymphoStat-B (Monoclonal Anti-BLyS Antibody) in Subjects With Rheumatoid Arthritis" at ClinicalTrials.gov.
- ↑ "Efficacy and Safety of Belimumab in Subjects With Primary Sjögren's Syndrome (BELISS)". Archived from the original on 2012-10-18. Retrieved 2021-10-20.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Pages using duplicate arguments in template calls
- Webarchive template wayback links
- Drugs with non-standard legal status
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Drugs missing an ATC code
- Drug has EMA link
- Drugboxes which contain changes to verified fields
- Drugboxes which contain changes to watched fields
- Drugs that are a monoclonal antibody
- All articles with unsourced statements
- Articles with unsourced statements from July 2020
- Articles with invalid date parameter in template
- Articles with changed CASNo identifier
- Chemicals that do not have a ChemSpider ID assigned
- Articles with changed KEGG identifier
- Immunosuppressants
- Monoclonal antibodies
- GlaxoSmithKline brands
- RTT