Reactive arthritis
| Reactive arthritis | |
|---|---|
 | |
| Reactive arthritis of the knee | |
| Specialty | Rheumatology |
Reactive arthritis, formerly known as Reiter's syndrome, is a form of inflammatory arthritis[1] that develops in response to an infection in another part of the body (cross-reactivity). Coming into contact with bacteria and developing an infection can trigger the disease.[2] By the time the patient presents with symptoms, often the "trigger" infection has been cured or is in remission in chronic cases, thus making determination of the initial cause difficult.
The arthritis often is coupled with other characteristic symptoms; this was previously referred to as Reiter's syndrome, Reiter's disease or Reiter's arthritis. The term "reactive arthritis" is strongly preferred by some and increasingly used as a substitute for this designation because Hans Conrad Julius Reiter was not the first to describe the syndrome, his conclusions regarding its pathogenesis were incorrect, and because he committed war crimes as a Nazi at Buchenwald concentration camp during World War II.
The manifestations of reactive arthritis include the following triad of symptoms: an inflammatory arthritis of large joints, inflammation of the eyes in the form of conjunctivitis or uveitis, and urethritis in men or cervicitis in women. Arthritis occurring alone following sexual exposure or enteric infection is also known as reactive arthritis. Patients can also present with mucocutaneous lesions, as well as psoriasis-like skin lesions such as circinate balanitis, and keratoderma blennorrhagicum. Enthesitis can involve the Achilles tendon resulting in heel pain.[3] Not all affected persons have all the manifestations.
The clinical pattern of reactive arthritis commonly consists of an inflammation of fewer than five joints which often includes the knee or sacroiliac joint. The arthritis may be "additive" (more joints become inflamed in addition to the primarily affected one) or "migratory" (new joints become inflamed after the initially inflamed site has already improved).[4][5]
Reactive arthritis is an RF-seronegative, HLA-B27-linked arthritis[6] often precipitated by genitourinary or gastrointestinal infections. The most common triggers are intestinal infections (with Salmonella, Shigella or Campylobacter) and sexually transmitted infections (with Chlamydia trachomatis);[7] however, it also can happen after group A streptococcal infections.[8][9]
It most commonly strikes individuals aged 20–40 years of age, is more common in men than in women, and more common in white than in black people. This is owing to the high frequency of the HLA-B27 gene in the white population.[10][11] It can occur in epidemic form. Patients with HIV have an increased risk of developing reactive arthritis as well.
Numerous cases during World Wars I and II focused attention on the triad of arthritis, urethritis, and conjunctivitis (often with additional mucocutaneous lesions), which at that time was also referred to as Fiessenger-Leroy-Reiter syndrome.[12]
Signs and symptoms
- Because common systems involved include the eye, the urinary system, and the hands and feet, one clinical mnemonic in reactive arthritis is "Can't see, can't pee, can't climb a tree."[13]
- The classic triad consists of:
- Conjunctivitis
- Nongonococcal urethritis
- Asymmetric oligoarthritis
- Symptoms generally appear within 1–3 weeks but can range from 4 to 35 days from the onset of the inciting episode of the disease.
- The classical presentation of the syndrome starts with urinary symptoms such as burning pain on urination (dysuria) or an increased frequency of urination. Other urogenital problems may arise such as prostatitis in men and cervicitis, salpingitis and/or vulvovaginitis in women.
- It presents with monoarthritis affecting the large joints such as the knees and sacroiliac spine causing pain and swelling. An asymmetrical inflammatory arthritis of interphalangeal joints may be present but with relative sparing of small joints such as the wrist and hand.
- Patient can have enthesitis presenting as heel pain, Achilles tendinitis or plantar fasciitis, along with balanitis circinata (circinate balanitis), which involves penile lesions present in roughly 20 to 40 percent of the men with the disease.
- A small percentage of men and women develop small hard nodules called keratoderma blennorrhagicum on the soles of the feet and, less commonly, on the palms of the hands or elsewhere. The presence of keratoderma blennorrhagica is diagnostic of reactive arthritis in the absence of the classical triad. Subcutaneous nodules are also a feature of this disease.
- Ocular involvement (mild bilateral conjunctivitis) occurs in about 50% of men with urogenital reactive arthritis syndrome and about 75% of men with enteric reactive arthritis syndrome. Conjunctivitis and uveitis can include redness of the eyes, eye pain and irritation, or blurred vision. Eye involvement typically occurs early in the course of reactive arthritis, and symptoms may come and go.
- Dactylitis, or "sausage digit", a diffuse swelling of a solitary finger or toe, is a distinctive feature of reactive arthritis and other peripheral spondylarthritides but can also be seen in polyarticular gout and sarcoidosis.
- Mucocutaneous lesions can be present. Common findings include oral ulcers that come and go. In some cases, these ulcers are painless and go unnoticed. In the oral cavity, the patients may suffer from recurrent aphthous stomatitis, geographic tongue and migratory stomatitis in higher prevalence than the general population.[14]
- Some patients suffer serious gastrointestinal problems similar to those of Crohn's disease.
- About 10 percent of people with reactive arthritis, especially those with a prolonged course of the disease, will develop cardiac manifestations, including aortic regurgitation and pericarditis. Reactive arthritis has been described as a precursor of other joint conditions, including ankylosing spondylitis.
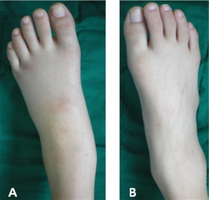
-
HLA-B27-associated reactive arthritis after Salmonella enteritis - a) swelling of left ankle joint b) and normal right ankle joint
-
Keratoderma blennorrhagicum due to reactive arthritis
Causes
Reactive arthritis is associated with the HLA-B27 gene on chromosome 6 and by the presence of enthesitis as the basic pathologic lesion[15] and is triggered by a preceding infection. The most common triggering infection in the US is a genital infection with Chlamydia trachomatis. Other bacteria known to cause reactive arthritis which are more common worldwide are Ureaplasma urealyticum, Salmonella spp., Shigella spp., Yersinia spp., and Campylobacter spp.[16]
A bout of food poisoning or a gastrointestinal infection may also precede the disease (the last four genera of bacteria mentioned above are enteric bacteria).[17] Shigella is the most common organism causing reactive arthritis following diarrhea. Chlamydia trachomatis is the most common cause of reactive arthritis following urethritis. Ureaplasma and mycoplasma are rare causes. There is some circumstantial evidence for other organisms causing the disease, but the details are unclear.[17]
Reactive arthritis usually manifests about 1–3 weeks after a known infection. The mechanism of interaction between the infecting organism and the host is unknown. Synovial fluid cultures are negative, suggesting that reactive arthritis is caused either by an autoimmune response involving cross-reactivity of bacterial antigens with joint tissues or by bacterial antigens that have somehow become deposited in the joints.
Diagnosis
There are few clinical symptoms, but the clinical picture is dominated by arthritis in one or more joints, resulting in pain, swelling, redness, and heat sensation in the affected areas.
The urethra, cervix and the throat may be swabbed in an attempt to culture the causative organisms. Cultures may also be carried out on urine and stool samples or on fluid obtained by arthrocentesis.
Tests for C-reactive protein and erythrocyte sedimentation rate are non-specific tests that can be done to corroborate the diagnosis of the syndrome. A blood test for the genetic marker HLA-B27 may also be performed. About 75 percent of all the patients with reactive arthritis have this gene.
Diagnostic criteria
Although there are no definitive criteria to diagnose the existence of reactive arthritis, the American College of Rheumatology has published sensitivity and specificity guidelines.[18]
| Method of diagnosis | Sensitivity | Specificity |
|---|---|---|
| 1. Episode of arthritis of more than 1 month with urethritis and/or cervicitis | 84.3% | 98.2% |
| 2. Episode of arthritis of more than 1 month and either urethritis or cervicitis, or bilateral conjunctivitis | 85.5% | 96.4% |
| 3. Episode of arthritis, conjunctivitis, and urethritis | 50.6% | 98.8% |
| 4. Episode of arthritis of more than 1 month, conjunctivitis, and urethritis | 48.2% | 98.8% |
Treatment
The main goal of treatment is to identify and eradicate the underlying infectious source with the appropriate antibiotics if still present. Otherwise, treatment is symptomatic for each problem. Nonspecific urethritis may be treated with a short course of tetracycline. Analgesics, particularly NSAIDs, are used. Steroids, sulfasalazine and immunosuppressants may be needed for patients with severe reactive symptoms that do not respond to any other treatment. Local corticosteroids are useful in the case of iritis.
Prognosis
Reactive arthritis may be self-limiting, frequently recurring, chronic or progressive. Most patients have severe symptoms lasting a few weeks to six months. 15 to 50 percent of cases involve recurrent bouts of arthritis. Chronic arthritis or sacroiliitis occurs in 15–30 percent of cases. Repeated attacks over many years are common, and patients sometimes end up with chronic and disabling arthritis, heart disease, amyloid deposits, ankylosing spondylitis, immunoglobulin A nephropathy, cardiac conduction abnormalities, or aortitis with aortic regurgitation.[19] However, most people with reactive arthritis can expect to live normal life spans and maintain a near-normal lifestyle with modest adaptations to protect the involved organs.
Epidemiology
Because women may be underdiagnosed, the exact incidence of reactive arthritis is difficult to estimate. A few studies have been completed, though. In Norway between 1988 and 1990, the incidence was 4.6 cases per 100,000 for chlamydia-induced reactive arthritis and 5 cases per 100,000 for that induced by enteric bacteria.[20] In 1978 in Finland, the annual incidence was found to be 43.6 per 100,000.[21]
History
When reactive arthritis appears in a triad that also includes ophthalmic and urogenital manifestations, the eponym "Reiter's syndrome" was often applied; German physician Hans Conrad Julius Reiter, a physician and leader of the Nazi party, described the condition in a soldier he treated during World War I. Reiter allowed for experiments on concentration camp victims and the use of the term "Reiter's syndrome" has fallen out of favor.[22]
A number of physicians have suggested that the eponym is undeserved and use of the eponym has declined.[22][23][24] Dr. Reiter's Nazi Party affiliation, and in particular his involvement in forced human experimentation in the Buchenwald concentration camp (which, after his capture at the end of World War II, resulted in his prosecution in Nuremberg as a war criminal), have come to overshadow his medical accomplishments. Furthermore, he was not the first physician to make associations between the arthritis and other symptoms: the terms "arthritis urethritica", "venereal arthritis" and "polyarteritis enterica" had previously been applied, and the full triad was described by another physician in the nineteenth century.[24]
Notable cases
- It has been postulated that Italian-born explorer Christopher Columbus had reactive arthritis, dying from a heart attack caused by the condition.[25]
- Pat Buchanan, American conservative political commentator, author, syndicated columnist, politician and broadcaster
- P. J. Gallagher[26]
- Ian Murray, Scottish football player[27]
- Mark St. John, one-time guitarist for Kiss
- Kirk Brandon, lead singer for Spear of Destiny
- Daniel Johns, Australian musician, lead singer for Silverchair[28]
- Steve Walters, football player and victim of sexual abuse by football trainer Barry Bennell[29]
See also
List of medical eponyms with Nazi associations
References
- ↑ American College of Rheumatology. "Reactive Arthritis". Archived from the original on May 15, 2020. Retrieved January 24, 2017.
- ↑ Mayo Staff (March 5, 2011). "Reactive Arthritis (Reiter's Syndrome)". Mayo Clinic. Archived from the original on January 2, 2014. Retrieved May 16, 2011.
- ↑ H. Hunter Handsfield (2001). Color atlas and synopsis of sexually transmitted diseases, Volume 236. McGraw-Hill Professional. p. 148. ISBN 978-0-07-026033-7. Archived from the original on 2021-08-29. Retrieved 2021-07-27.
- ↑ Primer on the Rheumatic Diseases, By John H. Klippel, page 218
- ↑ Rheumatology in Practice, By J. A. Pereira da Silva, Anthony D. Woolf page 5.9
- ↑ Ruddy, Shaun (2001). Kelley's Textbook of Rheumatology, 6th Ed. W. B. Saunders. pp. 1055–1064. ISBN 978-0-7216-9033-9.
- ↑ Siala, Mariam; et al. (2008). "Analysis of bacterial DNA in synovial tissue of Tunisian patients with reactive and undifferentiated arthritis by broad-range PCR, cloning and sequencing". Arthritis Research & Therapy. BioMed Central. 10 (2): R40. doi:10.1186/ar2398. PMC 2453759. PMID 18412942.
- ↑ Infectious Diseases Immunization Committee (1995). "Poststreptococcal arthritis". The Canadian Journal of Infectious Diseases. 6 (3): 133–135. doi:10.1155/1995/470341. PMC 3327910. PMID 22514384.
- ↑ "Reactive Arthritis". www.rheumatology.org. Archived from the original on 2019-01-26. Retrieved 2019-09-18.
- ↑ Sampaio-Barros PD, Bortoluzzo AB, Conde RA, Costallat LT, Samara AM, Bértolo MB (June 2010). "Undifferentiated spondyloarthritis: a longterm followup". The Journal of Rheumatology. 37 (6): 1195–1199. doi:10.3899/jrheum.090625. PMID 20436080. S2CID 45438826.
- ↑ Geirsson AJ, Eyjolfsdottir H, Bjornsdottir G, Kristjansson K, Gudbjornsson B (May 2010). "Prevalence and clinical characteristics of ankylosing spondylitis in Iceland – a nationwide study". Clinical and Experimental Rheumatology. 28 (3): 333–40. PMID 20406616.
- ↑ Harrison's Rheumatology, Second Edition [Anthony Fauci, Carol Langford], Ch.9 THE SPONDYLOARTHRITIDES, Reactive Arthritis, page.134
- ↑ Mark A. Marinella (1 September 2001). Recognizing Clinical Patterns: Clues to a Timely Diagnosis. Hanley & Belfus. p. 44. ISBN 978-1-56053-485-3. Archived from the original on 27 June 2014. Retrieved 27 July 2021.
- ↑ Zadik Y, Drucker S, Pallmon S (Aug 2011). "Migratory stomatitis (ectopic geographic tongue) on the floor of the mouth". J Am Acad Dermatol. 65 (2): 459–60. doi:10.1016/j.jaad.2010.04.016. PMID 21763590.
- ↑ Kataria, RK; Brent LH (June 2004). "Spondyloarthropathies". American Family Physician. 69 (12): 2853–2860. PMID 15222650. Archived from the original on 2008-07-09. Retrieved 2021-07-27.
- ↑ Hill Gaston JS, Lillicrap MS (2003). "Arthritis associated with enteric infection". Best Pract Ice & Research. Clinical Rheumatology. 17 (2): 219–239. doi:10.1016/S1521-6942(02)00104-3. PMID 12787523.
- ↑ 17.0 17.1 Paget, Stephen (2000). Manual of Rheumatology and Outpatient Orthopedic Disorders: Diagnosis and Therapy (4th ed.). Lippincott, Williams, & Wilkins. pp. chapter 36. ISBN 978-0-7817-1576-8.
- ↑ American College of Rheumatology. "Arthritis and Rheumatism". Archived from the original on April 29, 2011. Retrieved May 16, 2011.
- ↑ eMedicine/Medscape (Jan 5, 2010). "Reactive Arthritis". Archived from the original on December 28, 2019. Retrieved May 16, 2011.
- ↑ Kvien, T.; Glennas, A.; Melby, K.; Granfors, K; et al. (1994). "Reactive arthritis: Incidence, triggering agents and clinical presentation". Journal of Rheumatology. 21 (1): 115–22. PMID 8151565.
- ↑ Isomäki, H.; Raunio, J.; von Essen, R.; Hämeenkorpi, R. (1979). "Incidence of rheumatic diseases in Finland". Scandinavian Journal of Rheumatology. 7 (3): 188–192. doi:10.3109/03009747809095652. PMID 310157.
- ↑ 22.0 22.1 Vajda, FJ; Davis, SM; Byrne, E (April 2015). "Names of infamy: tainted eponyms". Journal of Clinical Neuroscience. 22 (4): 642–4. doi:10.1016/j.jocn.2014.09.022. PMID 25564271. S2CID 30840398.
- ↑ Strous, RD; Edelman, MC (March 2007). "Eponyms and the Nazi era: time to remember and time for change" (PDF). The Israeli Medical Association Journal. 9 (3): 207–14. PMID 17402342. Archived (PDF) from the original on 2021-01-17. Retrieved 2021-07-27.
- ↑ 24.0 24.1 Wallace, D. J.; Weisman, M. (2000). "Should a war criminal be rewarded with eponymous distinction? The double life of Hans Reiter (1881–1969)". Journal of Clinical Rheumatology. 6 (1): 49–54. doi:10.1097/00124743-200002000-00009. PMID 19078450.
- ↑ "Cause of the death of Columbus (in Spanish)". Eluniversal.com.mx. Archived from the original on 24 September 2014. Retrieved 29 July 2009.
- ↑ Kelly, Fiach (4 January 2008). "Comedian reveals how he tracked birth parents to solve family health mystery". Irish Independent. Archived from the original on 20 October 2012. Retrieved 4 January 2008.
- ↑ Lisa Gray (Nov 29, 2006). "Murray targets Christmas as date for Rangers return". The Independent. Archived from the original on December 22, 2019. Retrieved July 27, 2021.
- ↑ "Silverchair frontman's dramatic fight-back from crippling illness". The Sydney Morning Herald. 1 December 2002. Archived from the original on 2016-09-11. Retrieved 2016-07-22.
- ↑ Daniel Taylor (Nov 22, 2016). "Second footballer reveals abuse by serial paedophile Barry Bennell". The Guardian. Archived from the original on November 22, 2016. Retrieved July 27, 2021.
External links
| Classification | |
|---|---|
| External resources |
- eMedicine Archived 2013-11-03 at the Wayback Machine
- Questions and Answers about Reactive Arthritis Archived 2015-01-16 at the Wayback Machine - US National Institute of Arthritis and Musculoskeletal and Skin Diseases