Zaleplon
| |||
| Names | |||
|---|---|---|---|
| Pronunciation | zal-a-plon | ||
| Trade names | Sonata, Starnoc, Andante, others | ||
| |||
| Clinical data | |||
| Drug class | Z drug[1] | ||
| Main uses | Trouble sleeping[2] | ||
| Side effects | Headache, dizziness, abdominal pain, sleep walking[2] | ||
| Pregnancy category |
| ||
| Breastfeeding | Not recommended[3] | ||
| Routes of use | By mouth (medical), intranasal (recreational) | ||
| Typical dose | 10 to 20 mg[2] | ||
| External links | |||
| AHFS/Drugs.com | Monograph | ||
| MedlinePlus | a601251 | ||
| Legal | |||
| Legal status |
| ||
| Pharmacokinetics | |||
| Bioavailability | 30% (by mouth) | ||
| Metabolism | Liver | ||
| Elimination half-life | 1–1.5 h | ||
| Excretion | Kidney | ||
| Chemical and physical data | |||
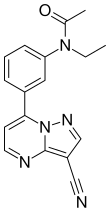
| Formula | C17H15N5O | ||
| Molar mass | 305.341 g·mol−1 | ||
| 3D model (JSmol) | |||
| |||
| |||
Zaleplon, sold under the brand names Sonata among others, is a medication used to treat trouble sleeping.[2] Use is not recommended for more than two weeks.[2][4] It is taken by mouth.[2]
Common side effects include headache, dizziness, and abdominal pain.[2] Serious side effects can include sleepwalking or other complex sleep behavior, aggression, anaphylaxis, and abuse.[2] Use is not recommended in those with significant liver problems.[2] Safety in pregnancy and breastfeeding is unclear and such use is not recommended.[3] It is a nonbenzodiazepine hypnotic from the pyrazolopyrimidine class.[2]
Zaleplon was approved for medical use in the United States in 1999.[2] In the United States it costs about 13 USD per month as of 2021.[5] It is not currently sold in Canada and is no longer approved in the United Kingdom.[6][1]
Medical uses
Zaleplon is slightly effective in insomnia,[7] primarily characterized by difficulty falling asleep. Zaleplon reduces the time required to fall asleep by improving sleep latency and may therefore facilitate sleep induction rather than sleep maintenance.[8][9][10] Due to its ultrashort elimination half-life, zaleplon may not be effective in reducing premature awakenings; however, it may be administered to alleviate middle-of-the-night awakenings.[8] However, zaleplon has not been empirically shown to increase total sleep time.[10][8]
It may result in an impaired ability to drive the next day, though it has proven promising when compared to other sedative/hypnotics and next-day residual sedation.[11] It may have advantages over benzodiazepines with fewer adverse effects.[12]
Neither zaleplon, nor any nonbenzodiazepine hypnotic class medication should be combined with alcohol, as both modulate GABAA receptor sites, and in a synergistic manner increase the chances of fatal respiratory depression and asphyxiation from vomiting.[citation needed]
Special populations
Zaleplon is not recommended for long term use in the elderly.[13] The elderly are more sensitive to the adverse effects of zaleplon such as cognitive side effects. Zaleplon may increase the risk of injury among the elderly. It should not be used while in pregnancy or lactation, and in patients with a history of alcohol or drug abuse, psychotic illness or depression, clinicians should devote more attention.[14]
When compared with benzodiazepines, nonbenzodiazepines (including zaleplon) offer few significant advantages in efficacy and tolerability among elderly individuals. Long-term use of sedative/hypnotics for insomnia has traditionally been discouraged for reasons that include concerns about addiction and rebound insomnia, as well to the risk of side effects associated to GABAA agonists, such as cognitive impairment, anterograde amnesia, daytime sedation, musculoskeletal impairment, and subsequently an increased risk of harm to oneself (e.g. falling) and to others (e.g. automotive accidents). Though, quite obviously as the body and brain age, these aforementioned phenomena are expected events, as they occur daily regardless of ingestion of a sedative/hypnotic. Thus, statistically significant and empirical evidence are arguably still absent as dramatic precautions and conclusions are drawn irrespective of the debilitating realities that accompany insomnia and the fact that these medicines do indeed provide assistance to millions of elderly individuals. It is important to distinguish between the extrapolation of potential side effects relative to the vast number of examples, wherein the sedative/hypnotic has proven therapeutically beneficial and appropriate.
In addition, some contend the efficacy and safety of long-term use of these agents remains to be enumerated, but nothing concrete suggests long-term use poses any direct harm to a person.[15] Still, as of today neither benzodiazepines nor nonbenzodiazepines are recommended for the long-term treatment of insomnia.
Dosage
The typical dose is 10 to 20 mg before bed.[2]
Side effects
The side effects of zaleplon are similar to the adverse effects of benzodiazepines, although with less next-day sedation,[16] and in two studies zaleplon use was found not to cause an increase in traffic accidents, as compared to other hypnotics currently on the market.[17][18]
Sleeping pills, including zaleplon, have been associated with an increased risk of death.[19]
Available data cannot provide a reliable estimate of the incidence of dependence during treatment at recommended doses of zaleplon (typically 5–20 mg before bed). Other sedative/hypnotics have been associated with various signs and symptoms of a withdrawal syndrome, following abrupt discontinuation, ranging from mild dysphoria and insomnia to more serious cases that include abdominal and muscle cramps, vomiting, sweating, tremors, and convulsions. Following abrupt cessation, the seizure threshold is further lowered, wherein coma and death are possible outcomes if untreated.
Some evidence suggests zaleplon is not as chemically reinforcing and exhibits far fewer rebound effects when compared with other nonbenzodiazepines, or Z-drugs.[20]
Interactions
Cimetidine, rifampicin, and thioridazine cause interactions with zaleplon.[21]
Cimetidine and grapefruit are known to increase blood plasma concentrations of benzodiazepines metabolized by the P450 CYP3A4 liver enzyme (e.g. alprazolam) by extending the time by which the drug leaves the body, effectively extending the half-life and enhancing effects to potentially toxic levels. Thus, given the similarities between zaleplon and benzodiazepines, particularly in effect, and not just chemical structure, it is reasonable to take precautions (e.g. inquire at a pharmacy) before one consumes cimetidine (or grapefruit) while also taking zaleplon.
Pharmacology
Mechanism of action
Zaleplon is a high-affinity ligand of positive modulator sites of GABAA receptors, which enhances GABAergic inhibition of neurotransmission in the central nervous system. The ultrashort half-life gives zaleplon a unique advantage over other hypnotics because of its lack of next-day residual effects on driving and other performance-related skills.[22][23] Unlike nonselective benzodiazepine drugs and zopiclone, which distort the sleep pattern, zaleplon appears to induce sleep without disrupting the natural sleep architecture.[24]
A meta-analysis of randomized, controlled clinical trials which compared benzodiazepines against zaleplon or other Z-drugs such as zolpidem, zopiclone, and eszopiclone has found few clear and consistent differences between zaleplon and the benzodiazepines in terms of sleep onset latency, total sleep duration, number of awakenings, quality of sleep, adverse events, tolerance, rebound insomnia, and daytime alertness.[25]
Zaleplon has a pharmacological profile similar to benzodiazepines, characterized by an increase in slow wave deep sleep (SWDS) with rapid onset of hypnotic action. Zaleplon is a full agonist for the benzodiazepine α1 receptor located on the GABAA receptor complex in the body, with lower affinity for the α2 and α3 subsites. It selectively enhances the action of GABA similar to, but more selectively than benzodiazepines. Zaleplon, although not a benzodiazepine, maintains a very similar pharmacological profile nonetheless, known for inducing hypnotic effects by α1 subreceptor sites, anxiolytic and muscle relaxant effects via α2 and α3 subsites, with negligible anticonvulsant properties (via α5 subsite), as zaleplon action is modulated at benzodiazepine receptor sites. The elimination half-life of zaleplon is about 1–1.5 hours. The absorption rate of zaleplon is rapid and the onset of therapeutic effects is typically breached within 5–15 minutes following ingestion.
Zaleplon should be understood as an ultrashort-acting sedative-hypnotic drug for the treatment of insomnia. Zaleplon increases EEG power density in the δ-frequency band and a decrease in the energy of the θ-frequency band[26][27]
Pharmacokinetics
Zaleplon is primarily metabolised by aldehyde oxidase, and its half-life can be affected by substances which inhibit or induce aldehyde oxidase. Taken orally, zaleplon reaches full concentration in about one hour. It is extensively metabolised into 5-oxozaleplon and 5-oxodesethylzaleplon (the latter via desethylzaleplon), with less than 1% of it excreted intact in urine.
Chemistry
Pure zaleplon in its solid state is a white to off-white powder with very low solubility in water, as well as low solubility in ethanol and propylene glycol. It has a constant octanol-water partition coefficient of log P = 1.23 in the pH range between 1 and 7.
It is classified as a pyrazolopyrimidine.[28]
Synthesis

The synthesis starts with the condensation of 3-acetylacetanilide[31][32] (1) with N,N-dimethylformamide dimethyl acetal (DMFDMA)[33] to give the eneamide (2). The anilide nitrogen is then alkylated by means of sodium hydride and ethyl iodide to give 3. The first step in the condensation with 3-amino-4-cyanopyrazole can be visualized as involving an addition-elimination reaction sequence on the eneamide function to give a transient intermediate such as 5. Cyclization then leads to formation of the fused pyrimidine ring to afford zaleplon (6).
Society and culture
Recreational use
Zaleplon has the potential to be a drug of recreational use, and has been found to have an addictive potential similar to benzodiazepine and benzodiazepine-like hypnotics.[34] The mind- and judgment-altering effects of zaleplon are similar to those of many benzodiazepines, but the fast-acting nature and short half-life of the chemical mean high doses set on much more quickly and last for short periods of time (usually from 45 to 60 minutes).
Some individuals use a different delivery method than prescribed, such as insufflation, to induce effects faster.[35]

A common effect of recreational zaleplon use is the occurrence of (typically short-lived) hallucinations. Fewer visual and auditory hallucinations/disruptions occur with the use of zaleplon than with other Z-drugs, like zolpidem.[citation needed] Anterograde amnesia can occur and can cause one to lose track of the amount of zaleplon already ingested, prompting the ingesting of more than originally planned.[36][37] However, continuous ingestion is extremely unlikely precisely because of zaleplon's quick onset of action.
The combination of alcohol and zaleplon can result in fatal respiratory depression and asphyxiation from vomiting.[citation needed]
Aviation
The Federal Aviation Administration allows zaleplon with a 12-hour wait period and no more than twice a week, which makes it the sleep medication with the shortest allowed waiting period after use.[38] The substances with the 2nd shortest period, which is of 24 hours, are zolpidem and ramelteon.[38]
Military
The United States Air Force uses zaleplon as one of the hypnotics approved as a "no-go pill" to help aviators and special-duty personnel sleep in support of mission readiness (with a four-hour restriction on subsequent flight operation). "Ground tests" are required prior to authorization being issued to use the medication in an operational situation.[39] The other hypnotics used as "no-go pills" are temazepam and zolpidem, which both have longer mandatory recovery periods.[39]
See also
References
- ↑ 1.0 1.1 "Sleeping pills". www.mind.org.uk. Archived from the original on 2021-02-26. Retrieved 2021-08-04.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 "Zaleplon Monograph for Professionals". Drugs.com. Archived from the original on 17 April 2021. Retrieved 4 August 2021.
- ↑ 3.0 3.1 "Zaleplon (Sonata) Use During Pregnancy". Drugs.com. Archived from the original on 18 April 2021. Retrieved 4 August 2021.
- ↑ "Zaleplon" (PDF). Archived (PDF) from the original on 29 August 2021. Retrieved 4 August 2021.
- ↑ "Zaleplon Prices, Coupons & Savings Tips - GoodRx". GoodRx. Archived from the original on 17 May 2020. Retrieved 4 August 2021.
- ↑ "Authorized Sleep-Aid Medications in Canada". www.healthycanadians.gc.ca. Archived from the original on 9 November 2017. Retrieved 4 August 2021.
- ↑ Huedo-Medina TB, Kirsch I, Middlemass J, Klonizakis M, Siriwardena AN (December 2012). "Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: meta-analysis of data submitted to the Food and Drug Administration". BMJ. 345: e8343. doi:10.1136/bmj.e8343. PMC 3544552. PMID 23248080.
- ↑ 8.0 8.1 8.2 Bhandari, Priyanka; Sapra, Amit (2020), "Zaleplon", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31855398, archived from the original on 2021-08-27, retrieved 2020-07-08
- ↑ Ebbens, Marieke M; Verster, Joris C (2010-07-20). "Clinical evaluation of zaleplon in the treatment of insomnia". Nature and Science of Sleep. 2: 115–126. doi:10.2147/nss.s6853. ISSN 1179-1608. PMC 3630939. PMID 23616704.
- ↑ 10.0 10.1 Dooley, M.; Plosker, G. L. (August 2000). "Zaleplon: a review of its use in the treatment of insomnia". Drugs. 60 (2): 413–445. doi:10.2165/00003495-200060020-00014. ISSN 0012-6667. PMID 10983740.
- ↑ Verster JC, Veldhuijzen DS, Volkerts ER (August 2004). "Residual effects of sleep medication on driving ability". Sleep Medicine Reviews. 8 (4): 309–25. doi:10.1016/j.smrv.2004.02.001. hdl:1874/11902. PMID 15233958.
- ↑ Barbera J, Shapiro C (2005). "Benefit-risk assessment of zaleplon in the treatment of insomnia". Drug Safety. 28 (4): 301–18. doi:10.2165/00002018-200528040-00003. PMID 15783240. S2CID 24222535.
- ↑ American Geriatrics Society 2012 Beers Criteria Update Expert Panel (April 2012). "American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults". Journal of the American Geriatrics Society. 60 (4): 616–31. doi:10.1111/j.1532-5415.2012.03923.x. PMC 3571677. PMID 22376048.
- ↑ Antai-Otong D (August 2006). "The art of prescribing. Risks and benefits of non-benzodiazepine receptor agonists in the treatment of acute primary insomnia in older adults". Perspectives in Psychiatric Care. 42 (3): 196–200. doi:10.1111/j.1744-6163.2006.00070.x. PMID 16916422. Archived from the original on 2013-01-06.
- ↑ Bain KT (June 2006). "Management of chronic insomnia in elderly persons". The American Journal of Geriatric Pharmacotherapy. 4 (2): 168–92. doi:10.1016/j.amjopharm.2006.06.006. PMID 16860264.
- ↑ Wagner J, Wagner ML, Hening WA (June 1998). "Beyond benzodiazepines: alternative pharmacologic agents for the treatment of insomnia". The Annals of Pharmacotherapy. 32 (6): 680–91. doi:10.1345/aph.17111. PMID 9640488. S2CID 34250754.
- ↑ Menzin J, Lang KM, Levy P, Levy E (January 2001). "A general model of the effects of sleep medications on the risk and cost of motor vehicle accidents and its application to France". PharmacoEconomics. 19 (1): 69–78. doi:10.2165/00019053-200119010-00005. PMID 11252547. S2CID 45013069.
- ↑ Vermeeren A, Riedel WJ, van Boxtel MP, Darwish M, Paty I, Patat A (March 2002). "Differential residual effects of zaleplon and zopiclone on actual driving: a comparison with a low dose of alcohol". Sleep. 25 (2): 224–31. PMID 11905433.
- ↑ Kripke, DF (February 2016). "Mortality Risk of Hypnotics: Strengths and Limits of Evidence" (PDF). Drug Safety. 39 (2): 93–107. doi:10.1007/s40264-015-0362-0. PMID 26563222. S2CID 7946506. Archived (PDF) from the original on 2020-03-14. Retrieved 2021-06-18.
- ↑ Lader MH (January 2001). "Implications of hypnotic flexibility on patterns of clinical use". International Journal of Clinical Practice. Supplement (116): 14–9. PMID 11219327.
- ↑ Wang JS, DeVane CL (2003). "Pharmacokinetics and drug interactions of the sedative hypnotics" (PDF). Psychopharmacology Bulletin. 37 (1): 10–29. doi:10.1007/BF01990373. PMID 14561946. S2CID 1543185. Archived from the original (PDF) on 2007-07-09. Retrieved 2008-12-28.
- ↑ Patat A, Paty I, Hindmarch I (July 2001). "Pharmacodynamic profile of Zaleplon, a new non-benzodiazepine hypnotic agent". Human Psychopharmacology. 16 (5): 369–392. doi:10.1002/hup.310. PMID 12404558. S2CID 21096374.
- ↑ Rowlett JK, Spealman RD, Lelas S, Cook JM, Yin W (January 2003). "Discriminative stimulus effects of zolpidem in squirrel monkeys: role of GABA(A)/alpha1 receptors". Psychopharmacology. 165 (3): 209–15. doi:10.1007/s00213-002-1275-z. PMID 12420154. S2CID 37632215.
- ↑ Noguchi H, Kitazumi K, Mori M, Shiba T (January 2002). "Binding and neuropharmacological profile of zaleplon, a novel nonbenzodiazepine sedative/hypnotic". European Journal of Pharmacology. 434 (1–2): 21–8. doi:10.1016/S0014-2999(01)01502-3. PMID 11755161.
- ↑ Dündar Y, Dodd S, Strobl J, Boland A, Dickson R, Walley T (July 2004). "Comparative efficacy of newer hypnotic drugs for the short-term management of insomnia: a systematic review and meta-analysis". Human Psychopharmacology. 19 (5): 305–22. doi:10.1002/hup.594. PMID 15252823. S2CID 10888200.
- ↑ Noguchi H, Kitazumi K, Mori M, Shiba T (March 2004). "Electroencephalographic properties of zaleplon, a non-benzodiazepine sedative/hypnotic, in rats" (pdf). Journal of Pharmacological Sciences. 94 (3): 246–51. doi:10.1254/jphs.94.246. PMID 15037809. Archived from the original on 2008-12-11. Retrieved 2021-06-18.
- ↑ Petroski RE, Pomeroy JE, Das R, Bowman H, Yang W, Chen AP, Foster AC (April 2006). "Indiplon is a high-affinity positive allosteric modulator with selectivity for alpha1 subunit-containing GABAA receptors". The Journal of Pharmacology and Experimental Therapeutics. 317 (1): 369–77. doi:10.1124/jpet.105.096701. PMID 16399882. S2CID 46510829.
- ↑ "Zaleplon". pubchem.ncbi.nlm.nih.gov. U.S. National Library of Medicine. Archived from the original on 12 June 2018. Retrieved 10 June 2018.
- ↑ J. P. Dusza et al., U.S. Patent 4,626,538 (1986 to Am. Cyanamid).
- ↑ http://en.cnki.com.cn/Article_en/CJFDTotal-ZYSG200205002.htm Archived 2018-09-20 at the Wayback Machine 《China Pharmacist》 2002-05 Synthesis of Zaleplon.
- ↑ Banasik M, Komura H, Shimoyama M, Ueda K (January 1992). "Specific inhibitors of poly(ADP-ribose) synthetase and mono(ADP-ribosyl)transferase". The Journal of Biological Chemistry. 267 (3): 1569–75. PMID 1530940.
- ↑ Dehmel F, Weinbrenner S, Julius H, Ciossek T, Maier T, Stengel T, Fettis K, Burkhardt C, Wieland H, Beckers T (July 2008). "Trithiocarbonates as a novel class of HDAC inhibitors: SAR studies, isoenzyme selectivity, and pharmacological profiles". Journal of Medicinal Chemistry. 51 (13): 3985–4001. doi:10.1021/jm800093c. PMID 18558669.
- ↑ Salomon, Robert G.; Raychaudhuri, Swadesh R. (1984). "Convenient preparation of N,N-dimethylacetamide dimethyl acetal". The Journal of Organic Chemistry. 49 (19): 3659. doi:10.1021/jo00193a045.
- ↑ "Sonata®(zaleplon)Capsules". Archived from the original on 2014-12-11. Retrieved 2021-06-18.
- ↑ Paparrigopoulos T, Tzavellas E, Karaiskos D, Liappas I (November 2008). "Intranasal zaleplon abuse". The American Journal of Psychiatry. 165 (11): 1489–90. doi:10.1176/appi.ajp.2008.08030452. PMID 18981079. Archived from the original on 2010-07-05. Retrieved 2021-06-18.
- ↑ Rush CR, Frey JM, Griffiths RR (July 1999). "Zaleplon and triazolam in humans: acute behavioral effects and abuse potential". Psychopharmacology. 145 (1): 39–51. doi:10.1007/s002130051030. PMID 10445371. S2CID 12061258.
- ↑ Ator NA (December 2000). "Zaleplon and triazolam: drug discrimination, plasma levels, and self-administration in baboons". Drug and Alcohol Dependence. 61 (1): 55–68. doi:10.1016/S0376-8716(00)00123-X. PMID 11064184.
- ↑ 38.0 38.1 "Medication Database – AMAS". Archived from the original on 2021-08-27. Retrieved 2021-06-18.
- ↑ 39.0 39.1 Caldwell JA, Caldwell JL (July 2005). "Fatigue in military aviation: an overview of US military-approved pharmacological countermeasures" (pdf). Aviation, Space, and Environmental Medicine. 76 (7 Suppl): C39-51. PMID 16018329. Archived (PDF) from the original on 2020-05-24. Retrieved 2021-06-18.
External links
| Identifiers: |
|
|---|
- Pages using duplicate arguments in template calls
- Webarchive template wayback links
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- Drugboxes which contain changes to watched fields
- All articles with unsourced statements
- Articles with unsourced statements from May 2014
- Articles with invalid date parameter in template
- Articles with unsourced statements from February 2013
- Articles with unsourced statements from August 2013
- Acetanilides
- GABAA receptor positive allosteric modulators
- Nitriles
- Pfizer brands
- Nonbenzodiazepines
- Pyrazolopyrimidines
- RTT