Fesoterodine
 | |
 | |
| Names | |
|---|---|
| Trade names | Toviaz, others |
| |
| Clinical data | |
| Drug class | Antimuscarinic[1] |
| Main uses | Overactive bladder syndrome (OAB)[1] |
| Side effects | Dry mouth, constipation[1] |
| Pregnancy category |
|
| Routes of use | By mouth |
| Typical dose | 4 to 8 mg/day[1] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a609021 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 52% (active metabolite) |
| Protein binding | 50% (active metabolite) |
| Metabolism | Liver (CYP2D6- and 3A4-mediated) |
| Elimination half-life | 7–8 hours (active metabolite) |
| Excretion | Kidney (70%) and fecal (7%) |
| Chemical and physical data | |
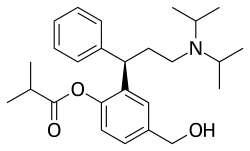
| Formula | C26H37NO3 |
| Molar mass | 411.586 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Fesoterodine, sold under the brand name Toviaz among others, is a medication used to treat the symptoms of overactive bladder syndrome (OAB).[1][3] It is a second line medication for this use.[4] It is taken by mouth.[1]
Common side effects include dry mouth and constipation.[1] Other side effects may include urinary retention, trouble sleeping, and dizziness.[1][4] It is not recommended in people with severe liver problems or myasthenia gravis.[3] It is an antimuscarinic and works via the same chemical as tolterodine.[1]
Fesoterodine was approved for medical use in Europe in 2007,[3] the United States in 2008,[1] and Canada in 2012.[5] In the United States it costs about 310 USD per month as of 2021.[6] This amount in the United Kingdom costs the NHS about £26.[4]
Medical uses
Fesoterodine has the advantage of allowing more flexible dosage than other muscarinic antagonists.[7] Its tolerability and side effects are similar to other muscarinic antagonists and as a new drug seems unlikely to make great changes in practices of treatment for overactive bladder.[7]
A Japanese study from 2017, showed that urgency and urge incontinence are improved after 3 days administration of the drug, with full efficacy able to be judged after 7 days administration. Overactive bladder was found to be resolved in 88% of patients after seven days usage. [8]
Dosage
It is usually used at 4 to 8 mg once per day.[1]
Mechanism of action
Fesoterodine is a prodrug. It is broken down into its active metabolite, desfesoterodine, by plasma esterases.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 "Fesoterodine Monograph for Professionals". Drugs.com. Archived from the original on 26 January 2021. Retrieved 23 July 2021.
- ↑ "Fesoterodine (Toviaz) Use During Pregnancy". Drugs.com. 7 November 2019. Archived from the original on 29 November 2020. Retrieved 12 August 2020.
- ↑ 3.0 3.1 3.2 "Toviaz". Archived from the original on 12 November 2020. Retrieved 4 August 2021.
- ↑ 4.0 4.1 4.2 BNF (80 ed.). BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 821. ISBN 978-0-85711-369-6.
{{cite book}}: CS1 maint: date format (link) - ↑ "Notice of Decision for TOVIAZ". Archived from the original on 2012-04-23. Retrieved 2012-04-20.
- ↑ "Toviaz Prices, Coupons & Savings Tips - GoodRx". GoodRx. Retrieved 4 August 2021.
- ↑ 7.0 7.1 Vella M, Cardozo L (September 2011). "Review of fesoterodine". Expert Opinion on Drug Safety. 10 (5): 805–8. doi:10.1517/14740338.2011.591377. PMID 21639817. S2CID 9653506.
- ↑ "Sato N, Fuji K, Ogawa Y (2017). "Transactions of The Showa University Society: The 335th Meeting". The Showa University Journal of Medical Sciences. 29 (2): 201–217. doi:10.15369/sujms.29.201. ISSN 2185-0968.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Pages using duplicate arguments in template calls
- CS1 maint: date format
- Drugs with non-standard legal status
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- Drug has EMA link
- Drugboxes which contain changes to verified fields
- Articles with changed CASNo identifier
- Articles with changed EBI identifier
- Muscarinic antagonists
- Prodrugs
- Primary alcohols
- Isobutyrate esters
- Pfizer brands
- Diisopropylamino compounds
- Phenol esters
- RTT