Nortriptyline
 | |
 | |
| Names | |
|---|---|
| Trade names | Pamelor, Noritren, Nortrilen, others |
| Other names | Desitriptyline; ELF-101; E.L.F. 101; N-7048 |
| |
| Clinical data | |
| Drug class | Tricyclic antidepressant (TCA) |
| Main uses | Depression, neuropathic pain, attention deficit hyperactivity disorder (ADHD), stopping smoking. anxiety[1][2] |
| Side effects | Dry mouth, constipation, blurry vision, sleepiness, low blood pressure with standing, weakness[2] |
| Pregnancy category |
|
| Routes of use | By mouth |
| Defined daily dose | 75 mg (by mouth)[3] 30 mg (by injection)[3] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682620 |
| Legal | |
| License data | |
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 32–79[4] |
| Protein binding | 92%[4] |
| Metabolism | Liver |
| Metabolites | 10-E-Hydroxynortriptyline |
| Elimination half-life | 18–44 hours (mean 30 hours)[4] |
| Excretion | Urine: 40%[4] Feces: minor[4] |
| Chemical and physical data | |
| Formula | C19H21N |
| Molar mass | 263.384 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Nortriptyline, sold under the brand name Pamelor, among others, is a medication used to treat depression, neuropathic pain, attention deficit hyperactivity disorder (ADHD), stopping smoking, and anxiety.[1][2] It does not appear to be useful for young people with depression.[2] Nortriptyline is a less preferred treatment for ADHD and stopping smoking.[2] It is taken by mouth.[2]
Common side effects include dry mouth, constipation, blurry vision, sleepiness, low blood pressure with standing, and weakness.[2] Serious side effects may include seizures, an increased risk of suicide in those less than 25 years of age, urinary retention, glaucoma, mania, and a number of heart issues.[2] Nortriptyline may cause problems if taken during pregnancy.[2] Use during breastfeeding appears to be relatively safe.[1] It is a tricyclic antidepressant (TCA) and is believed to work by altering levels of serotonin and norepinephrine.[2]
Nortriptyline was approved for medical use in the United States in 1964.[2] It is available as a generic medication.[1] A month supply of nortriptyline at 75mg/day in the United Kingdom costs the NHS around £35.00 as of 2020.[1] In the United States the wholesale cost of this amount is about US$4.20.[5] In 2017, it was the 183rd most commonly prescribed medication in the United States, with more than three million prescriptions.[6][7]
Medical uses
Nortriptyline is used to treat depression.[8] This medication is in capsule or liquid and is taken by the mouth one to four times a day, with or without food.[8] Usually people are started on a low dose and it is gradually increased.[8] A level between 50-150 ng/mL of nortriptyline in the blood generally corresponds with an antidepressant effect.[9]
In the United Kingdom, it may also be used for treating nocturnal enuresis, with courses of treatment lasting no more than three months. It is also used off-label for the treatment of panic disorder, irritable bowel syndrome, migraine prophylaxis and chronic pain or neuralgia modification, particularly temporomandibular joint disorder.[10]
Neuropathic pain
Although not approved by the FDA for neuropathic pain, many randomized controlled trials have demonstrated the effectiveness of TCAs for the treatment of this condition in both depressed and non-depressed individuals. In 2010, an evidence-based guideline sponsored by the International Association for the Study of Pain recommended nortriptyline as a first-line medication for neuropathic pain.[11] However, in a 2015 Cochrane systematic review the authors did not recommend nortriptyline as a first-line agent for neuropathic pain.[12]
Dosage
The defined daily dose is 75 mg by mouth and 30 mg by injection.[3]
Side effects
The most common side effects include dry mouth, sedation, constipation, increased appetite, blurred vision and tinnitus.[13][14] An occasional side effect is a rapid or irregular heartbeat. Alcohol may exacerbate some of its side effects.[13]
Nortriptyline should not be used in the acute recovery phase after myocardial infarction (heart attack).[15]
Closer monitoring is required for those with a history of cardiovascular disease,[16] stroke, glaucoma, or seizures, as well as in persons with hyperthyroidism or receiving thyroid hormones.
Overdose
The symptoms and the treatment of an overdose are generally the same as for the other TCAs, including serotonin syndrome and adverse cardiac effects. Because TCAs have a relatively narrow therapeutic index, the likelihood of serious overdose (both accidental and intentional) is fairly high. A nortriptyline overdose is considered a medical emergency and frequently results in death. Symptoms of overdose include: irregular heartbeat, seizures, coma, confusion, hallucination, widened pupils, drowsiness, agitation, fever, low body temperature, stiff muscles and vomiting.[8]
Interactions
Excessive consumption of alcohol in combination with nortriptyline therapy may have a potentiating effect, which may lead to the danger of increased suicidal attempts or overdosage, especially in patients with histories of emotional disturbances or suicidal ideation.
Use of tricyclic antidepressants along with a monoamine oxidase (MAO) inhibitor, linezolid, and IV methylene blue are contraindicated as it can cause an increased risk of developing serotonin syndrome.[17]
It may interact with the following drugs:[18]
- heart rhythm medications such as flecainide, propafenone, or quinidine
- cimetidine
- guanethidine
- reserpine
Pharmacology
Pharmacodynamics
| Site | Ki (nM) | Species | Ref |
|---|---|---|---|
| SERT | 15–18 | Human | [20][21] |
| NET | 1.8–4.4 | Human | [20][21] |
| DAT | 1,140 | Human | [20] |
| 5-HT1A | 294 | Human | [22] |
| 5-HT2A | 5.0–41 | Human/rat | [23][22] |
| 5-HT2C | 8.5 | Rat | [23] |
| 5-HT3 | 1,400 | Rat | [24] |
| 5-HT6 | 148 | Rat | [25] |
| α1 | 55 | Human | [22] |
| α2 | 2,030 | Human | [22] |
| β | >10,000 | Rat | [26] |
| D2 | 2,570 | Human | [22] |
| H1 | 3.0–15 | Human | [27][22][28] |
| H2 | 646 | Human | [27] |
| H3 | 45,700 | Human | [27] |
| H4 | 6,920 | Human | [27] |
| mACh | 37 | Human | [22] |
| M1 | 40 | Human | [29] |
| M2 | 110 | Human | [29] |
| M3 | 50 | Human | [29] |
| M4 | 84 | Human | [29] |
| M5 | 97 | Human | [29] |
| σ1 | 2,000 | Guinea pig | [30] |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | |||
Nortriptyline is an active metabolite of amitriptyline by demethylation in the liver. Its pharmacologic profile is as the table to the right shows (inhibition or antagonism of all sites).[19][31]
Chemically, it is a secondary amine dibenzocycloheptene and pharmacologically it is classed as a first-generation antidepressant.[32]
These effects account for some therapeutic actions as well as for most side effects such as sedation, hypotension, anticholinergic effects, etc.[clarification needed] Nortriptyline may also have a sleep-improving effect due to antagonism of the H1 and 5-HT2A receptors.[33] In the short term, however, nortriptyline may disturb sleep due to its activating effect.
In one study of long-term efficacy, nortriptyline showed a higher relapse rate in comparison with phenelzine in individuals being treated for depression, possibly due to the toxic metabolite 10-hydroxynortriptyline being produced.[34] The authors of a review noted that the nortriptyline group had more episodes prior to treatment.[34]
In one study, nortriptyline had the highest affinity for the dopamine transporter among the TCAs (KD = 1,140 nM) besides amineptine (a norepinephrine–dopamine reuptake inhibitor), although its affinity for this transporter was still 261- and 63-fold lower than for the norepinephrine and serotonin transporters (KD = 4.37 and 18 nM, respectively).[20]
Pharmacokinetics
Pharmacogenetics
Nortriptyline is metabolized in the liver by the hepatic enzyme CYP2D6, and genetic variations within the gene coding for this enzyme can affect its metabolism, leading to changes in the concentrations of the drug in the body.[35] Increased concentrations of nortriptyline may increase the risk for side effects, including anticholinergic and nervous system adverse effects, while decreased concentrations may reduce the drug's efficacy.[36][37][38]
Individuals can be categorized into different types of CYP2D6 metabolizers depending on which genetic variations they carry. These metabolizer types include poor, intermediate, extensive, and ultrarapid metabolizers. Most individuals (about 77–92%) are extensive metabolizers,[38] and have "normal" metabolism of nortriptyline. Poor and intermediate metabolizers have reduced metabolism of the drug as compared to extensive metabolizers; patients with these metabolizer types may have an increased probability of experiencing side effects. Ultrarapid metabolizers use nortriptyline much faster than extensive metabolizers; patients with this metabolizer type may have a greater chance of experiencing pharmacological failure.[36][37][38]
The Clinical Pharmacogenetics Implementation Consortium recommends avoiding nortriptyline in persons who are CYP2D6 ultrarapid or poor metabolizers, due to the risk of a lack of efficacy and side effects, respectively. A reduction in starting dose is recommended for patients who are CYP2D6 intermediate metabolizers. If use of nortriptyline is warranted, therapeutic drug monitoring is recommended to guide dose adjustments.[38] The Dutch Pharmacogenetics Working Group recommends reducing the dose of nortriptyline in CYP2D6 poor or intermediate metabolizers, and selecting an alternative drug or increasing the dose in ultrarapid metabolizers.[39]
Chemistry
Nortriptyline is a tricyclic compound, specifically a dibenzocycloheptadiene, and possesses three rings fused together with a side chain attached in its chemical structure.[40] Other dibenzocycloheptadiene TCAs include amitriptyline (N-methylnortriptyline), protriptyline, and butriptyline.[40][41] Nortriptyline is a secondary amine TCA, with its N-methylated parent amitriptyline being a tertiary amine.[42][43] Other secondary amine TCAs include desipramine and protriptyline.[44][45] The chemical name of nortriptyline is 3-(10,11-dihydro-5H-dibenzo[a,d]cyclohepten-5-ylidene)-N-methyl-1-propanamine and its free base form has a chemical formula of C19H21N1 with a molecular weight of 263.384 g/mol.[46] The drug is used commercially mostly as the hydrochloride salt; the free base form is used rarely.[46][47] The CAS Registry Number of the free base is 72-69-5 and of the hydrochloride is 894-71-3.[46][47][48]
History
Nortriptyline was developed by Geigy.[49] It first appeared in the literature in 1962 and was patented the same year.[49] The drug was first introduced for the treatment of depression in 1963.[49][50]
Society and culture

Cost
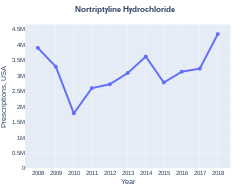
A month supply of nortriptyline at a dose 75mg/day, in the United Kingdom, costs the NHS around £35.00 as of 2020.[1] In the United States the wholesale cost of this amount is about US$4.20.[5] In 2017, it was the 183rd most commonly prescribed medication in the United States, with more than three million prescriptions.[6][7]
-
Nortriptyline costs (US)
-
Nortriptyline prescriptions (US)
Generic names
Nortriptyline is the English and French generic name of the drug and its INN, BAN, and DCF, while nortriptyline hydrochloride is its USAN, USP, BANM, and JAN.[46][47][51][52] Its generic name in Spanish and Italian and its DCIT are nortriptilina, in German is nortriptylin, and in Latin is nortriptylinum.[46][47][51][52]
Brand names
Brand names of nortriptyline include Allegron, Aventyl, Noritren, Norpress, Nortrilen, Norventyl, Norzepine, Pamelor, and Sensoval, among many others.[46][47][52]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 BNF (80 ed.). London: BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. pp. 395–396. ISBN 978-0-85711-369-6.
{{cite book}}: CS1 maint: date format (link) - ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 "Nortriptyline Hydrochloride Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 28 March 2019. Retrieved 22 March 2019.
- ↑ 3.0 3.1 3.2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 1 December 2020. Retrieved 7 September 2020.
- ↑ 4.0 4.1 4.2 4.3 4.4 Thomas L. Lemke; David A. Williams (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 588–. ISBN 978-1-60913-345-0. Archived from the original on 16 December 2019. Retrieved 15 August 2017.
- ↑ 5.0 5.1 "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Archived from the original on 2019-03-06. Retrieved 3 March 2019.
- ↑ 6.0 6.1 "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- ↑ 7.0 7.1 "Nortriptyline Hydrochloride - Drug Usage Statistics". ClinCalc. Archived from the original on 8 July 2020. Retrieved 11 April 2020.
- ↑ 8.0 8.1 8.2 8.3 "Nortriptyline". MedlinePlus. National Library of Medicine. Archived from the original on 28 March 2019. Retrieved 6 May 2019.
- ↑ Orsulak, PJ (September 1989). "Therapeutic monitoring of antidepressant drugs: guidelines updated". Therapeutic Drug Monitoring. 11 (5): 497–507. doi:10.1097/00007691-198909000-00002. PMID 2683251.
- ↑ Sweetman SC, ed. (2002). Martindale. The complete drug reference (33 ed.). Pharmaceutical Press. ISBN 0-85369-499-0.
- ↑ Dworkin RH, O'Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, Kent JL, Krane EJ, Lebel AA, Levy RM, Mackey SC, Mayer J, Miaskowski C, Raja SN, Rice AS, Schmader KE, Stacey B, Stanos S, Treede RD, Turk DC, Walco GA, Wells CD (Mar 2010). "Recommendations for the pharmacological management of neuropathic pain: an overview and literature update". Mayo Clinic Proceedings. 85 (3 Suppl): S3–14. doi:10.4065/mcp.2009.0649. PMC 2844007. PMID 20194146.
- ↑ Derry, Sheena; Wiffen; Aldington D; Moore (2015). "Nortriptyline for neuropathic pain in adults (Review)" (PDF). The Cochrane Library (1). Archived (PDF) from the original on 2018-10-03. Retrieved 2018-10-03.
- ↑ 13.0 13.1 Brayfield, A, ed. (9 January 2017). "Nortriptyline Hydrochloride – Martindale: The Complete Drug Reference". MedicinesComplete. Pharmaceutical Press. Archived from the original on 29 August 2021. Retrieved 11 August 2017.
- ↑ "ALLEGRON". TGA eBusiness Services. Arrow Pharma Pty Ltd. 13 October 2016. Archived from the original on 11 August 2017. Retrieved 11 August 2017.
- ↑ "Nortriptyline label" (PDF). FDA. 2014. Archived (PDF) from the original on 2017-02-17. Retrieved 2018-10-03.
- ↑ Bardai, Abdennasser; Amin, Ahmad S.; Blom, Marieke T.; Bezzina, Connie R.; Berdowski, Jocelyn; Langendijk, Pim N. J.; Beekman, Leander; Klemens, Christine A.; Souverein, Patrick C. (2013). "Sudden cardiac arrest associated with use of a non-cardiac drug that reduces cardiac excitability: evidence from bench, bedside, and community". European Heart Journal. 34 (20): 1506–1516. doi:10.1093/eurheartj/eht054. ISSN 1522-9645. PMID 23425522.
- ↑ Merwar, Gagindip; Saadabadi, Abdolreza (2018), "Nortriptyline", StatPearls, StatPearls Publishing, PMID 29489270, archived from the original on 2021-08-28, retrieved 2018-10-03
- ↑ "nortriptyline". www.cardiosmart.org. Archived from the original on 2018-10-03. Retrieved 2018-10-03.
- ↑ 19.0 19.1 Roth, BL; Driscol, J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 28 August 2021. Retrieved 14 August 2017.
- ↑ 20.0 20.1 20.2 20.3 Tatsumi M, Groshan K, Blakely RD, Richelson E (1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". Eur. J. Pharmacol. 340 (2–3): 249–58. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- ↑ 21.0 21.1 Owens MJ, Morgan WN, Plott SJ, Nemeroff CB (1997). "Neurotransmitter receptor and transporter binding profile of antidepressants and their metabolites". J. Pharmacol. Exp. Ther. 283 (3): 1305–22. PMID 9400006.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 Cusack B, Nelson A, Richelson E (1994). "Binding of antidepressants to human brain receptors: focus on newer generation compounds". Psychopharmacology. 114 (4): 559–65. doi:10.1007/bf02244985. PMID 7855217.
- ↑ 23.0 23.1 Pälvimäki EP, Roth BL, Majasuo H, et al. (1996). "Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor". Psychopharmacology. 126 (3): 234–40. doi:10.1007/bf02246453. PMID 8876023.
- ↑ Schmidt AW, Hurt SD, Peroutka SJ (1989). "'[3H]quipazine' degradation products label 5-HT uptake sites". Eur. J. Pharmacol. 171 (1): 141–3. doi:10.1016/0014-2999(89)90439-1. PMID 2533080.
- ↑ Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR (1993). "Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs". Mol. Pharmacol. 43 (3): 320–7. PMID 7680751.
- ↑ Bylund DB, Snyder SH (1976). "Beta adrenergic receptor binding in membrane preparations from mammalian brain". Mol. Pharmacol. 12 (4): 568–80. PMID 8699.
- ↑ 27.0 27.1 27.2 27.3 Appl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (2012). "Interactions of recombinant human histamine H₁R, H₂R, H₃R, and H₄R receptors with 34 antidepressants and antipsychotics". Naunyn Schmiedebergs Arch. Pharmacol. 385 (2): 145–70. doi:10.1007/s00210-011-0704-0. PMID 22033803.
- ↑ Ghoneim OM, Legere JA, Golbraikh A, Tropsha A, Booth RG (2006). "Novel ligands for the human histamine H1 receptor: synthesis, pharmacology, and comparative molecular field analysis studies of 2-dimethylamino-5-(6)-phenyl-1,2,3,4-tetrahydronaphthalenes". Bioorg. Med. Chem. 14 (19): 6640–58. doi:10.1016/j.bmc.2006.05.077. PMID 16782354.
- ↑ 29.0 29.1 29.2 29.3 29.4 Stanton T, Bolden-Watson C, Cusack B, Richelson E (1993). "Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics". Biochem. Pharmacol. 45 (11): 2352–4. doi:10.1016/0006-2952(93)90211-e. PMID 8100134.
- ↑ Weber E, Sonders M, Quarum M, McLean S, Pou S, Keana JF (1986). "1,3-Di(2-[5-3H]tolyl)guanidine: a selective ligand that labels sigma-type receptors for psychotomimetic opiates and antipsychotic drugs". Proc. Natl. Acad. Sci. U.S.A. 83 (22): 8784–8. Bibcode:1986PNAS...83.8784W. doi:10.1073/pnas.83.22.8784. PMC 387016. PMID 2877462.
- ↑ Brunton L, Chabner B, Knollman B. Goodman and Gilman’s The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional; 2010.
- ↑ O'Connor, Elizabeth A.; Whitlock, Evelyn P.; Gaynes, Bradley; Beil, Tracy L. (2009). Screening for Depression in Adults and Older Adults in Primary Care: An Updated Systematic Review. Agency for Healthcare Research and Quality (US). PMID 20722174. Archived from the original on 2020-11-12. Retrieved 2019-03-13.
- ↑ Thase ME (2006). "Depression and sleep: pathophysiology and treatment". Dialogues in Clinical Neuroscience. 8 (2): 217–26. PMC 3181772. PMID 16889107.
- ↑ 34.0 34.1 Kennedy SH (Mar 1997). "Continuation and maintenance treatments in major depression: the neglected role of monoamine oxidase inhibitors". Journal of Psychiatry & Neuroscience. 22 (2): 127–31. PMC 1188835. PMID 9074307.
- ↑ Rudorfer MV, Potter WZ (Jun 1999). "Metabolism of tricyclic antidepressants". Cellular and Molecular Neurobiology. 19 (3): 373–409. doi:10.1023/A:1006949816036. PMID 10319193.
- ↑ 36.0 36.1 Stingl JC, Brockmöller J, Viviani R (Mar 2013). "Genetic variability of drug-metabolizing enzymes: the dual impact on psychiatric therapy and regulation of brain function". Molecular Psychiatry. 18 (3): 273–87. doi:10.1038/mp.2012.42. PMID 22565785.
- ↑ 37.0 37.1 Kirchheiner J, Seeringer A (Mar 2007). "Clinical implications of pharmacogenetics of cytochrome P450 drug metabolizing enzymes". Biochimica et Biophysica Acta (BBA) - General Subjects. 1770 (3): 489–94. doi:10.1016/j.bbagen.2006.09.019. PMID 17113714.
- ↑ 38.0 38.1 38.2 38.3 Hicks JK, Swen JJ, Thorn CF, Sangkuhl K, Kharasch ED, Ellingrod VL, Skaar TC, Müller DJ, Gaedigk A, Stingl JC (May 2013). "Clinical Pharmacogenetics Implementation Consortium guideline for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants" (PDF). Clinical Pharmacology and Therapeutics. 93 (5): 402–8. doi:10.1038/clpt.2013.2. PMC 3689226. PMID 23486447. Archived from the original on 2021-08-27. Retrieved 2018-11-04.
- ↑ Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, Rongen GA, van Schaik RH, Schalekamp T, Touw DJ, van der Weide J, Wilffert B, Deneer VH, Guchelaar HJ (May 2011). "Pharmacogenetics: from bench to byte—an update of guidelines". Clinical Pharmacology and Therapeutics. 89 (5): 662–73. doi:10.1038/clpt.2011.34. PMID 21412232.
- ↑ 40.0 40.1 Michael S Ritsner (15 February 2013). Polypharmacy in Psychiatry Practice, Volume I: Multiple Medication Use Strategies. Springer Science & Business Media. pp. 270–271. ISBN 978-94-007-5805-6. Archived from the original on 8 September 2017. Retrieved 16 August 2017.
- ↑ Thomas L. Lemke; David A. Williams (2008). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 580–. ISBN 978-0-7817-6879-5. Archived from the original on 2020-08-03. Retrieved 2017-08-16.
- ↑ Neal R. Cutler; John J. Sramek; Prem K. Narang (20 September 1994). Pharmacodynamics and Drug Development: Perspectives in Clinical Pharmacology. John Wiley & Sons. pp. 160–. ISBN 978-0-471-95052-3. Archived from the original on 3 August 2020. Retrieved 16 August 2017.
- ↑ Pavel Anzenbacher; Ulrich M. Zanger (23 February 2012). Metabolism of Drugs and Other Xenobiotics. John Wiley & Sons. pp. 302–. ISBN 978-3-527-64632-6. Archived from the original on 8 September 2017. Retrieved 16 August 2017.
- ↑ Patricia K. Anthony (2002). Pharmacology Secrets. Elsevier Health Sciences. pp. 39–. ISBN 1-56053-470-2. Archived from the original on 2019-12-16. Retrieved 2017-08-16.
- ↑ Philip Cowen; Paul Harrison; Tom Burns (9 August 2012). Shorter Oxford Textbook of Psychiatry. OUP Oxford. pp. 532–. ISBN 978-0-19-162675-3. Archived from the original on 8 September 2017. Retrieved 16 August 2017.
- ↑ 46.0 46.1 46.2 46.3 46.4 46.5 J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 888–. ISBN 978-1-4757-2085-3.
- ↑ 47.0 47.1 47.2 47.3 47.4 Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 752–. ISBN 978-3-88763-075-1.
- ↑ "ChemIDplus - 62265-06-9 - AMLRZIZSGSCSHZ-UHFFFAOYSA-N - Desipramine dibudinate - Similar structures search, synonyms, formulas, resource links, and other chemical information". Archived from the original on 2017-08-14. Retrieved 2017-08-16.
- ↑ 49.0 49.1 49.2 Andersen J, Kristensen AS, Bang-Andersen B, Strømgaard K (2009). "Recent advances in the understanding of the interaction of antidepressant drugs with serotonin and norepinephrine transporters". Chem. Commun. (25): 3677–92. doi:10.1039/b903035m. PMID 19557250.
- ↑ Richard C. Dart (2004). Medical Toxicology. Lippincott Williams & Wilkins. pp. 836–. ISBN 978-0-7817-2845-4.
- ↑ 51.0 51.1 I.K. Morton; Judith M. Hall (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 202–. ISBN 978-94-011-4439-1. Archived from the original on 8 January 2021. Retrieved 15 August 2017.
- ↑ 52.0 52.1 52.2 "Nortriptyline". Archived from the original on 2017-08-14. Retrieved 2017-08-14.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Pages using duplicate arguments in template calls
- CS1 maint: date format
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- Drugboxes which contain changes to watched fields
- Articles with hatnote templates targeting a nonexistent page
- Wikipedia articles needing clarification from March 2016
- Articles with invalid date parameter in template
- Alpha-1 blockers
- Amines
- Antihistamines
- Dibenzocycloheptenes
- Human drug metabolites
- Muscarinic antagonists
- Serotonin antagonists
- Serotonin-norepinephrine reuptake inhibitors
- Sodium channel blockers
- Tricyclic antidepressants
- RTT