List of antibiotics
The following is a list of antibiotics. The highest division between antibiotics is bactericidal and bacteriostatic. Bactericidals kill bacteria directly, whereas bacteriostatics prevent them from dividing. However, these classifications are based on laboratory behavior. The development of antibiotics has had a profound effect on the health of people for many years. Also, both people and animals have used antibiotics to treat infections and diseases. In practice, both treat bacterial infections.[1]
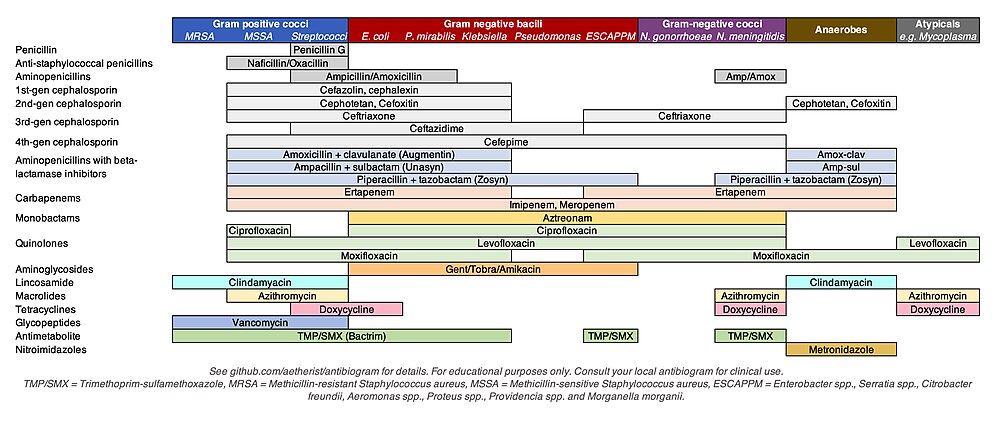
By coverage
The following are lists of antibiotics for specific microbial coverage (not an exhaustive list):
MRSA
Antibiotics that cover methicillin-resistant Staphylococcus aureus (MRSA):
- Vancomycin[2]
- Teicoplanin[2]
- Linezolid[2]
- Daptomycin[2]
- Trimethoprim/sulfamethoxazole
- Doxycycline
- Ceftobiprole[3] (5th generation)
- Ceftaroline (5th generation)
- Clindamycin
- Dalbavancin
- Delafloxacin
- Fusidic acid
- Mupirocin (topical)
- Omadacycline
- Oritavancin
- Tedizolid
- Telavancin
- Tigecycline (also covers gram negatives)
Pseudomonas aeruginosa
Antibiotics that cover Pseudomonas aeruginosa:
Certain cephalosporins, cephalosporin-beta-lactamase-inhibitor combinations, and new siderophore cephalosporins.
- Ceftazidime (3rd generation)
- Cefepime (4th generation)
- Ceftobiprole (5th generation)
- Ceftolozane/tazobactam
- Ceftazidime/avibactam
- Cefiderocol(siderophore cephalosporin)
Certain penicillins:
Certain carbapenems and carbapenem-beta-lactamase-inhibitors combinations:
- Carbapenems: (meropenem, imipenem/cilastatin, doripenem - NOT ertapenem)
- Meropenem/vaborbactam
- Imipenem/cilastatin/relebactam
Others:
- Fluoroquinolones: particularly levofloxacin, ciprofloxacin
- Polymyxins: Colistin, Polymyxin B
- Aztreonam (monobactam)
- Aminoglycosides - particularly tobramycin and amikacin
VRE
Antibiotics that usually have activity against vancomycin-resistant Enterococcus (VRE):
- Linezolid and Tedizolid
- Streptogramins such as quinupristin-dalfopristin
- Advanced generation tetracyclines: Tigecycline, Omadacycline, Eravacycline
- Daptomycin
- Oritavancin
Antibiotics with less reliable but occasional (depending on isolate and subspecies) activity:
- occasionally penicillins including penicillin, ampicillin and ampicillin-sulbactam, amoxicillin and amoxicillin-clavulnate, and piperacillin-tazobactam (not all vancomycin-resistant Enterococcus isolates are resistant to penicillin and ampicillin)
- occasionally doxycycline and minocycline
- occasionally fluoroquinolones such as moxifloxacin, levofloxacin, and ciprofloxacin
By class
See also pathogenic bacteria for a list of antibiotics sorted by target bacteria.
| Generic name | Brand names | Common uses[4] | Possible side effects[4] | Mechanism of action |
|---|---|---|---|---|
| Aminoglycosides | ||||
| Amikacin | Amikin | Infections caused by Gram-negative bacteria, such as Escherichia coli and Klebsiella particularly Pseudomonas aeruginosa. Effective against aerobic bacteria (not obligate/facultative anaerobes) and tularemia. All aminoglycosides are ineffective when taken orally as the stomach will digest the drug before it goes into the bloodstream. However aminoglycosides are effective in Intravenous, intramuscular and topical forms. | Binding to the bacterial 30S ribosomal subunit (some work by binding to the 50S subunit), inhibiting the translocation of the peptidyl-tRNA from the A-site to the P-site and also causing misreading of mRNA, leaving the bacterium unable to synthesize proteins vital to its growth. | |
| Gentamicin | Garamycin | |||
| Kanamycin | Kantrex | |||
| Neomycin | Neo-Fradin[5] | |||
| Netilmicin | Netromycin | |||
| Tobramycin | Nebcin | |||
| Paromomycin | Humatin | |||
| Streptomycin | Tuberculosis | |||
| Spectinomycin(Bs) | Trobicin | Gonorrhea | ||
| Ansamycins | ||||
| Geldanamycin | Experimental, as antitumor antibiotics | Block DNA transcription, either via inhibiting DNA-dependent RNA polymerase by binding to the β-subunit | ||
| Herbimycin | ||||
| Rifaximin | Xifaxan | Traveler's diarrhea caused by E. coli | ||
| Carbacephem | ||||
| Loracarbef | Lorabid | Discontinued | Prevents bacterial cell division by inhibiting cell wall synthesis. | |
| Carbapenems | ||||
| Ertapenem | Invanz | Bactericidal for both Gram-positive and Gram-negative organisms and therefore useful for empiric broad-spectrum antibacterial coverage. (Notes: MRSA resistance to this class. All are active against Pseudomonas aeruginosa except ertapenem.) |
|
Inhibition of cell wall synthesis |
| Doripenem | Doribax | |||
| Imipenem/Cilastatin | Primaxin | |||
| Meropenem | Merrem | |||
| Cephalosporins (First generation) | ||||
| Cefadroxil | Duricef | Good coverage against Gram-positive infections. |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. |
| Cefazolin | Ancef, Kefzol | |||
| Cephradine | ||||
| Cephapirin | ||||
| Cephalothin | ||||
| Cefalexin | Keflex | |||
| Cephalosporins (Second generation) | ||||
| Cefaclor | Distaclor, Ceclor, Raniclor | Less Gram-positive cover, improved Gram-negative cover. |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. |
| Cefoxitin | ||||
| Cefotetan | Cefotan | |||
| Cefamandole | ||||
| Cefmetazole | ||||
| Cefonicid | ||||
| Loracarbef | ||||
| Cefprozil | Cefzil | |||
| Cefuroxime | Ceftin, Zinacef (UK) | |||
| Cephalosporins (Third generation) | ||||
| Cefixime (antagonistic with Chloramphenicol)[6] | Cefspan (Fujisawa), Suprax | Improved coverage of Gram-negative organisms, except Pseudomonas. Reduced Gram-positive cover. But still not cover Mycoplasma and Chlamydia |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. |
| Cefdinir | Omnicef, Cefdiel | |||
| Cefditoren | Spectracef, Meiact | |||
| Cefoperazone [Unlike most third-generation agents, cefoperazone is active against Pseudomonas aeruginosa], combination Cefoperazone with Sulbactam makes more effective antibiotic, because Sulbactam avoid degeneration of Cefoperazone | Cefobid (discontinued) | |||
| Cefotaxime | Claforan | |||
| Cefpodoxime | Vantin, Banadoz | |||
| Ceftazidime (Unlike most third-generation agents, ceftazidime is active against Pseudomonas aeruginosa, but less active against Staphylococci and Streptococci compare to other 3rd generation of cephalosporins) | Fortaz, Ceptaz | |||
| Ceftibuten | Cedax | |||
| Ceftizoxime | ||||
| Moxalactam | ||||
| Ceftriaxone (IV and IM, not orally, effective also for syphilis and uncomplicated gonorrhea) | Rocephin | |||
| Cephalosporins (Fourth generation) | ||||
| Cefepime | Maxipime |
Covers pseudomonal infections. |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. |
| Cephalosporins (Fifth generation) | ||||
| Ceftaroline fosamil | Teflaro | Used to treat MRSA |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. |
| Ceftobiprole | Zeftera | Used to treat MRSA (methicillin-resistant Staphylococcus aureus), penicillin-resistant Streptococcus pneumoniae, Pseudomonas aeruginosa, and enterococci |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. |
| Glycopeptides | ||||
| Teicoplanin | Targocid (UK) | Active against aerobic and anaerobic Gram-positive bacteria including MRSA; Vancomycin is used orally for the treatment of C. difficile colitis | Inhibits peptidoglycan synthesis. | |
| Vancomycin | Vancocin | |||
| Telavancin | Vibativ | |||
| Dalbavancin | Dalvance | |||
| Oritavancin | Orbactiv | |||
| Lincosamides(Bs) | ||||
| Clindamycin | Cleocin | Serious staph-, pneumo-, and streptococcal infections in penicillin-allergic patients, also anaerobic infections; clindamycin topically for acne | Possible C. difficile-related pseudomembranous enterocolitis | Binds to 50S subunit of bacterial ribosomal RNA thereby inhibiting protein synthesis. |
| Lincomycin | Lincocin | |||
| Lipopeptide | ||||
| Daptomycin | Cubicin | Gram-positive organisms, but is inhibited by pulmonary surfactant so less effective against pneumonias | Binds to the membrane and cause rapid depolarization, resulting in a loss of membrane potential leading to inhibition of protein, DNA and RNA synthesis. | |
| Macrolides(Bs) | ||||
| Azithromycin | Zithromax, Sumamed, Xithrone | Streptococcal infections, syphilis, upper respiratory tract infections, lower respiratory tract infections, mycoplasmal infections, Lyme disease |
|
Inhibition of bacterial protein biosynthesis by binding reversibly to the subunit 50S of the bacterial ribosome, thereby inhibiting translocation of peptidyl tRNA. |
| Clarithromycin | Biaxin | |||
| Erythromycin | Erythocin, Erythroped | |||
| Roxithromycin | ||||
| Telithromycin | Ketek | Pneumonia | Visual disturbance, liver toxicity.[7] | |
| Spiramycin | Rovamycine | Mouth infections | ||
| Fidaxomicin | Dificid | Treatment of Clostridioides (formerly Clostridium) difficile infection.[8] May be more narrow-spectrum than vancomycin, resulting in less bowel microbiota alteration.[9] | Nausea (11%), vomiting, and abdominal pain.[10] | Bactericidal in susceptible organisms such as C. difficile by inhibiting RNA polymerase, thereby inhibiting protein synthesis.[10] |
| Monobactams | ||||
| Aztreonam | Azactam | Gram-negative bacteria | Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. | |
| Nitrofurans | ||||
| Furazolidone | Furoxone | Bacterial or protozoal diarrhea or enteritis | ||
| Nitrofurantoin(Bs) | Macrodantin, Macrobid | Urinary tract infections | ||
| Oxazolidinones(Bs) | ||||
| Linezolid | Zyvox | VRSA | Protein synthesis inhibitor; prevents the initiation step | |
| Posizolid | Phase II clinical trials | |||
| Radezolid | Phase II clinical trials | |||
| Tedizolid | Sivextro | |||
| Penicillins | ||||
| Amoxicillin | Novamox, Amoxil | Wide range of infections; penicillin used for streptococcal infections, syphilis, and Lyme disease |
|
Same mode of action as other beta-lactam antibiotics: disrupt the synthesis of the peptidoglycan layer of bacterial cell walls. |
| Ampicillin | Principen (discontinued) | |||
| Azlocillin | ||||
| Dicloxacillin | Dynapen (discontinued) | |||
| Flucloxacillin | Floxapen (Sold to European generics Actavis Group) | |||
| Mezlocillin | Mezlin (discontinued) | |||
| Methicillin | Staphcillin (discontinued) | |||
| Nafcillin | Unipen (discontinued) | |||
| Oxacillin | Prostaphlin (discontinued) | |||
| Penicillin G | Pentids (discontinued) | |||
| Penicillin V | Veetids (Pen-Vee-K) (discontinued) | |||
| Piperacillin | Pipracil (discontinued) | |||
| Penicillin G | Pfizerpen | |||
| Temocillin | Negaban (UK) (discontinued) | |||
| Ticarcillin | Ticar (discontinued) | |||
| Penicillin combinations | ||||
| Amoxicillin/clavulanate | Augmentin | Both Amoxicillin/clavulanate and Ampicillin/sulbactam are effective against non-recurrent acute otitis media.[11] Amoxicillin/clavulanate is one of the few oral antibiotics effective against skin and soft tissue infections. Can be given to children less than 40 kilograms in weight; for children heavier, the dosage is same as adults, twice daily.[12] | The second component reduces the effectiveness of some forms of bacterial resistance to the first component | |
| Ampicillin/sulbactam | Unasyn | |||
| Piperacillin/tazobactam | Zosyn | |||
| Ticarcillin/clavulanate | Timentin | |||
| Polypeptides | ||||
| Bacitracin | Eye, ear or bladder infections; usually applied directly to the eye or inhaled into the lungs; rarely given by injection, although the use of intravenous colistin is experiencing a resurgence due to the emergence of multi drug resistant organisms. | Kidney and nerve damage (when given by injection) | Inhibits isoprenyl pyrophosphate, a molecule that carries the building blocks of the peptidoglycan bacterial cell wall outside of the inner membrane[13] | |
| Colistin | Coly-Mycin-S | Interact with the Gram-negative bacterial outer membrane and cytoplasmic membrane, displacing bacterial counterions, which destabilizes the outer membrane. Act like a detergent against the cytoplasmic membrane, which alters its permeability. Polymyxin B and E are bactericidal even in an isosmotic solution. | ||
| Polymyxin B | ||||
| Quinolones/Fluoroquinolones | ||||
| Ciprofloxacin | Cipro, Ciproxin, Ciprobay | Urinary tract infections, bacterial prostatitis, community-acquired pneumonia, bacterial diarrhea, mycoplasmal infections, gonorrhea | Nausea (rare), irreversible damage to central nervous system (uncommon), tendinosis (rare) | Inhibits the bacterial DNA gyrase or the topoisomerase IV enzyme, thereby inhibiting DNA replication and transcription. |
| Enoxacin | Penetrex | |||
| Gatifloxacin | Tequin | |||
| Gemifloxacin | Factive[14] | |||
| Levofloxacin | Levaquin | |||
| Lomefloxacin | Maxaquin | |||
| Moxifloxacin | Avelox | |||
| Nadifloxacin | ||||
| Nalidixic acid | NegGram | |||
| Norfloxacin | Noroxin | |||
| Ofloxacin | Floxin (discontinued), Ocuflox | |||
| Trovafloxacin | Trovan | Withdrawn | ||
| Grepafloxacin | Raxar | Withdrawn | ||
| Sparfloxacin | Zagam | Withdrawn | ||
| Temafloxacin | Omniflox | Withdrawn | ||
| Sulfonamides(Bs) | ||||
| Mafenide | Sulfamylon | Urinary tract infections (except sulfacetamide, used for eye infections, and mafenide and silver sulfadiazine, used topically for burns) |
|
Folate synthesis inhibition. They are competitive inhibitors of the enzyme dihydropteroate synthetase, DHPS. DHPS catalyses the conversion of PABA (para-aminobenzoate) to dihydropteroate, a key step in folate synthesis. Folate is necessary for the cell to synthesize nucleic acids (nucleic acids are essential building blocks of DNA and RNA), and in its absence cells cannot divide. |
| Sulfacetamide | Sulamyd, Bleph-10 | |||
| Sulfadiazine | Micro-Sulfon | |||
| Silver sulfadiazine | Silvadene | |||
| Sulfadimethoxine | Di-Methox, Albon | |||
| Sulfamethizole | Thiosulfil Forte | |||
| Sulfamethoxazole | Gantanol | |||
| Sulfanilimide (archaic) | ||||
| Sulfasalazine | Azulfidine | |||
| Sulfisoxazole | Gantrisin | |||
| Trimethoprim-Sulfamethoxazole (Co-trimoxazole) (TMP-SMX) | Bactrim, Septra | |||
| Sulfonamidochrysoidine (archaic) | Prontosil | |||
| Tetracyclines(Bs) | ||||
| Demeclocycline | Declomycin | Syphilis, chlamydial infections, Lyme disease, mycoplasmal infections, acne rickettsial infections, malaria[note 1] |
|
Inhibits the binding of aminoacyl-tRNA to the mRNA-ribosome complex. They do so mainly by binding to the 30S ribosomal subunit in the mRNA translation complex. But Tetracycline cannot be taken together with all dairy products, aluminium, iron and zinc minerals. |
| Doxycycline | Vibramycin | |||
| Metacycline | ||||
| Minocycline | Minocin | |||
| Oxytetracycline | Terramycin | |||
| Tetracycline | Sumycin, Achromycin V, Steclin | |||
| Drugs against mycobacteria | ||||
| Clofazimine | Lamprene | Antileprotic | ||
| Dapsone | Avlosulfon | Antileprotic | ||
| Capreomycin | Capastat | Antituberculosis | ||
| Cycloserine | Seromycin | Antituberculosis, urinary tract infections | ||
| Ethambutol(Bs) | Myambutol | Antituberculosis | ||
| Ethionamide | Trecator | Antituberculosis | Inhibits peptide synthesis | |
| Isoniazid | I.N.H. | Antituberculosis | ||
| Pyrazinamide | Aldinamide | Antituberculosis | ||
| Rifampicin (Rifampin in US) | Rifadin, Rimactane | mostly Gram-positive and mycobacteria | Reddish-orange sweat, tears, and urine | Binds to the β subunit of RNA polymerase to inhibit transcription |
| Rifabutin | Mycobutin | Mycobacterium avium complex | Rash, discolored urine, GI symptoms | |
| Rifapentine | Priftin | Antituberculosis | ||
| Streptomycin | Antituberculosis | Neurotoxicity, ototoxicity | As other aminoglycosides | |
| Others | ||||
| Arsphenamine | Salvarsan | Spirochaetal infections (obsolete) | ||
| Chloramphenicol(Bs) | Chloromycetin | Meningitis, MRSA, topical use, or for low-cost internal treatment. Historic: typhus, cholera. Gram-negative, Gram-positive, anaerobes | Rarely: aplastic anemia. | Inhibits bacterial protein synthesis by binding to the 50S subunit of the ribosome |
| Fosfomycin | Monurol, Monuril | Acute cystitis in women | This antibiotic is not recommended for children and 75 and up of age | Inactivates enolpyruvyl transferase, thereby blocking cell wall synthesis |
| Fusidic acid | Fucidin | |||
| Metronidazole | Flagyl | Infections caused by anaerobic bacteria; also amoebiasis, trichomoniasis, giardiasis | Discolored urine, headache, metallic taste, nausea; alcohol is contraindicated | Produces toxic free radicals that disrupt DNA and proteins. This non-specific mechanism is responsible for its activity against a variety of bacteria, amoebae, and protozoa. |
| Mupirocin | Bactroban | Ointment for impetigo, cream for infected cuts | Inhibits isoleucine t-RNA synthetase (IleRS) causing inhibition of protein synthesis | |
| Platensimycin | ||||
| Quinupristin/Dalfopristin | Synercid | |||
| Thiamphenicol | Gram-negative, Gram-positive, anaerobes. Widely used in veterinary medicine. | Rash. Lacks known anemic side-effects. | A chloramphenicol analog. May inhibit bacterial protein synthesis by binding to the 50S subunit of the ribosome | |
| Tigecycline(Bs) | Tigacyl | Slowly Intravenous. Indicated for complicated skin/skin structure infections, soft tissue infections and complicated intra-abdominal infections. Effective for gram-positive, gram-negative, anaerobic, and against multi-antibiotic resistant bacteria (such as Staphylococcus aureus [MRSA] and Acinetobacter baumannii), but not effective for Pseudomonas spp. and Proteus spp. | Teeth discoloration and same side effects as tetracycline. Not to be given for children and pregnant or lactate women. Relatively safe and no need dose adjusted when be given for mild to moderate liver function or renal patients | Similar structure with tetracycline, but five times stronger, big volume distribution and long half-time in the body |
| Tinidazole | Tindamax Fasigyn | Protozoal infections | Upset stomach, bitter taste, and itchiness | |
| Trimethoprim(Bs) | Proloprim, Trimpex | Urinary tract infections | ||
| Generic Name | Brand Names | Common Uses[4] | Possible Side Effects[4] | Mechanism of action |
Note: (Bs): Bacteriostatic
Antibiotic candidates
These are antibiotic candidates, and known antibiotics that are not yet mass-produced.
| Generic name | Origin | Susceptible phyla | Stage of development | Mechanism of action |
|---|---|---|---|---|
| Unclassified | ||||
| Teixobactin | Eleftheria terrae | Gram-positive, including antibiotic resistant S. aureus and M. tuberculosis | No human trials scheduled | Binds fatty acid precursors to cell wall |
| Malacidins | Uncultured Bacterium | Gram-positive, including antibiotic resistant S. aureus | No human trials scheduled | Binds fatty acid precursors to cell wall |
| Halicin | Anti-diabetic drug | Clostridiodes difficile, Acinetobacter baumannii, and Mycobacterium tuberculosis | No human trials scheduled | Disrupts electrochemical gradient |
See also
- Timeline of antibiotics, listed by year of introduction
- Pathogenic bacteria
Notes
References
- ^ Pelczar, M. J.; Chan, E. C. S. and Krieg, N. R. (1999) "Host-Parasite Interaction; Nonspecific Host Resistance", In: Microbiology Concepts and Applications, 6th ed., McGraw-Hill Inc., New York pp. 478-479.
- ^ a b c d Aoki M (2015). レジデントのための感染症診療マニュアル. Japan: 医学書院. ISBN 978-4-260-02027-5.
- ^ Zhanel GG, Lam A, Schweizer F, Thomson K, Walkty A, Rubinstein E, Gin AS, Hoban DJ, Noreddin AM, Karlowsky JA (2008). "Ceftobiprole: a review of a broad-spectrum and anti-MRSA cephalosporin". American Journal of Clinical Dermatology. 9 (4): 245–54. doi:10.2165/00128071-200809040-00004. PMID 18572975. S2CID 24357533.
- ^ a b c d For common Uses and possible side effects reference is: Robert Berkow (ed.) The Merck Manual of Medical Information - Home Edition. Pocket (September 1999), ISBN 0-671-02727-1.
- ^ "Neomycin Drug Information". uptodate. Retrieved November 2, 2012.(subscription required)
- ^ Berger DS (2014-04-03). GIDEON Guide to Antimicrobial Agents (2014 ed.). GIDEON Informatics Inc. p. 221. ISBN 978-1-61755-839-9. Retrieved 4 February 2015.
- ^ Splete H, Kerri Wachter (March 2006). "Liver toxicity reported with Ketek". Internal Medicine News.
- ^ McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, Dubberke ER, Garey KW, Gould CV, Kelly C, Loo V, Shaklee Sammons J, Sandora TJ, Wilcox MH (March 2018). "Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA)". Clinical Infectious Diseases. 66 (7): e1–e48. doi:10.1093/cid/cix1085. PMC 6018983. PMID 29462280.
- ^ Tannock GW, Munro K, Taylor C, Lawley B, Young W, Byrne B, Emery J, Louie T (November 2010). "A new macrocyclic antibiotic, fidaxomicin (OPT-80), causes less alteration to the bowel microbiota of Clostridium difficile-infected patients than does vancomycin". Microbiology. 156 (Pt 11): 3354–9. doi:10.1099/mic.0.042010-0. PMID 20724385.
- ^ a b Dificid (fidaxomicin) [prescribing information] Whitehouse Station, NJ: Merck; December 2015.
- ^ Casellas JM, Israele V, Marín M, Ishida MT, Heguilen R, Soutric J, Arenoso H, Sibbald A, Stamboulian D (September 2005). "Amoxicillin-sulbactam versus amoxicillin-clavulanic acid for the treatment of non-recurrent-acute otitis media in Argentinean children". International Journal of Pediatric Otorhinolaryngology. 69 (9): 1225–33. doi:10.1016/j.ijporl.2005.03.016. PMID 16061111.
- ^ "APO-Amoxycillin and Clavulanic Acid 500mg/125 mg Tablets" (PDF). Retrieved November 27, 2014.
- ^ Mechanism of Action of Bacitracin: Complexation with Metal Ion and C55-Isoprenyl Pyrophosphate K. John Stone and Jack L. Strominger
- ^ "List of Antibiotics". Retrieved February 7, 2014.