User:QuackGuru/Sand A
https://commons.wikimedia.org/wiki/Special:Watchlist
Vaping can harm youth,[1] children, and non‐smokers.[2] Most vapes have nicotine in them, which is highly addictive.[1] Nicotine use in adolescence can harm brain development, which continues until about age 25, can impact attention, learning, mood, and impulse control, and may increase risk for future addiction to other drugs.[1]
In addition to nicotine, e-cigarette aerosol can contain other harmful and potentially harmful substances, including cancer-causing chemicals, volatile organic compounds, ultrafine particles, flavorings that have been linked to lung disease, and heavy metals such as nickel, tin, and lead.[1]
References
- ↑ 1.0 1.1 1.2 1.3 "What You Can Do to Protect Youth From the Harms of Vaping". Centers for Disease Control and Prevention. 18 September 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Banks E, AM; Yazidjoglou, A; Brown, S; Nguyen, M; Martin, M; Beckwith, K; Daluwatta, A; Campbell, S; Joshy, G (20 March 2023). "Electronic cigarettes and health outcomes: umbrella and systematic review of the global evidence". The Medical journal of Australia. doi:10.5694/mja2.51890. PMID 36939271.
https://pubmed.ncbi.nlm.nih.gov/?linkname=pubmed_pubmed_citedin&from_uid=34930765 Reasons for cannabis use during pregnancy and lactation: a qualitative study
Click below for reliable sources:
[1] Check for more content. https://nap.nationalacademies.org/catalog/24625/the-health-effects-of-cannabis-and-cannabinoids-the-current-state
Can you rewrite the following text?
|pmc=
https://drugpolicy.org/wp-content/uploads/2023/05/2023.04.10_syntheticcannabinoid_factsheet.pdf
https://www.cdc.gov/nceh/hsb/chemicals/sc/default.html
https://www.cdc.gov/nceh/hsb/chemicals/sc/healthcare.html
https://nida.nih.gov/research-topics/synthetic-cannabinoids
https://www.cdc.gov/nchs/data/nhcs/ED_Substance_Abuse_Factsheet.PDF https://www.cdc.gov/nchs/nhcs/
https://pubmed.ncbi.nlm.nih.gov/36626363/ Wait for review. Click on "Cited by" for reviews in the future.
https://pubmed.ncbi.nlm.nih.gov/?term=vaping+psychoactive+drug&filter=pubt.booksdocs&filter=pubt.meta-analysis&filter=pubt.review&filter=pubt.systematicreview&size=200 - vaping psychoactive drug
https://pubmed.ncbi.nlm.nih.gov/?term=marijuana+vaping&filter=pubt.booksdocs&filter=pubt.meta-analysis&filter=pubt.review&filter=pubt.systematicreview&size=200 - marijuana vaping
https://pubmed.ncbi.nlm.nih.gov/?term=marijuana+organizations&size=200 - marijuana organizations
https://nida.nih.gov/publications/drugfacts/cannabis-marijuana



The term vaping[note 1] refers to the usage of electronic cigarettes or other devices to inhale a range of heated and aerosolized substances.[4] Vaping or e-cigarette products can be used to deliver nicotine, flavorings, cannabis (marijuana[5]) and other chemicals.[4] The fundamental design of all vaping devices consists of three central components: a refillable or disposable lliquid reservoir, a heating element, and a power source.[4] Cannabis vaping is the process of using a battery-powered e-cigarette device or other vaporizer devices to heat and aerosolize cannabinoids, that are inhaled.[6] The heated cannabinoids are in a liquid solution such as a e-liquid or a solid such as a wax.[6] There are disposable and reusable devices.[6] The liquid solution can be made with nicotine, flavorings, propylene glycol and glycerin,[6] and polyethylene glycol or medium-chain triglycerides to replace or use with propylene glycol and glycerin,[7] various cannabinoid forms of tetrahydrocannabinol (THC), and cannabidiol.[6] The design of vaporizers has evolved to reflect the changing preferences of cannabis consumers.[8]
There is a connection between cannabis vaping and an array of unwanted health effects.[9] in contrast to cannabis smoking, suggestive evidence indicates that cannabis or THC vaping carries unique and overlapping potential health effects.[10] The potential long-term effects of cannabis vaping on youth are largely unknown.[9] This is due to it being a fairly new phenomenon, as of 2022.[9] In regard to the unwanted health effects associated with cannabis exposure, young individuals are a vulnerable group.[10] Compared with non-vaping users, youth cannabis vaping is tied to a 1.8-fold hike in respiratory problems like wheezing and dry coughing.[9] Although the association between vaping and the development of lung cancer is not well established, the carcinogenicity of breathing in of substances such as nitrosamine compounds, humectants (propylene glycol and glycerin), flavoring compounds, cannabis, and vitamin E acetate has been attributed to several possible mechanisms.[4] THC use may lead to death.[11] In 2019,[12] there had been a noteworthy upswing in vaping-induced lung illnesses among cannabinoid-based vaping users, characterized by acute lung injury or organizing pneumonia.[note 2][4]
There is limited clinical research on the medicinal use of cannabis and its efficacy and safety has not been substantiated.[19] There is also a lack of compelling evidence demonstrating the usefulness of using cannabis as medicine.[19] The flavorings in THC extracts are potentially harmful.[20] Cannabidiol or THC oil used in the vaping cartridges contain various harmful compounds, and this result largely depends on the type of extraction solvent used.[21] Cannabis is extremely addictive.[22] The particular patterns of addiction, tolerance, and withdrawal that has been seen in hard drugs such as heroin, is also being seen in people vaping THC.[20] The most common symptoms observed during cannabis withdrawal include irritability, anxiety, decreased appetite, restlessness, and sleep disturbances.[23] Treatment for cannabis use disorder may involve cognitive behavioral therapy integrated with motivational interviewing and/or motivational enhancement therapy.[24] Youth believe that cannabis is one of the least detrimental psychoactive drugs.[25] This is partly due to it as generally being seen as being more natural than other chemicals.[25] Youth often see content on cannabis vaping from non-credible internet sources and across social media.[25] Cannabis vaping devices are available at cannabis dispensaries, smoke shops,[10] and vape shops.[26]
In the 2010 decade, the sales of vaping products had grown exponentially, giving rise to health concerns regarding their exposure.[27] Despite prior gains in lowering smoking rates and nicotine usage, the current data, as of 2023, indicates an alarming rise in vaping among younger people, especially adolescents.[4] Vaping nicotine is more prevalent than vaping cannabis.[25] Youth are more likely to first experiment with combustible cigarettes and/or e-cigarettes than they are with cannabis.[10] As of 2020, the evidence indicates that the prevalence of cannabis vaping has grown among youth in Canada and the US.[9] Using e-cigarettes along with illicit chemicals is a cause for concern.[28] Concern exists that youth who use Juul may result in gateway effects, like initiating cannabis use.[29] There is a strong association with exposure to advertisements of vaping products and subsequent teenage vaping and cannabis consumption.[25] The increased use of e-cigarettes and cannabis vaping, especially among young individuals, females, and non-smokers, is a significant public health concern.[4] The legalizing of cannabis for recreational and medical purposes in numerous states in the US has resulted in a thriving cannabis industry.[30] While cannabis cultivation is harmful to the environment, abstaining from cannabis use is beneficial for the environment.[31]
Background
Terminology and overview




The term vaping refers to the usage of electronic cigarettes or other devices to inhale a range of heated and aerosolized substances.[4] Vaping or e-cigarette products can be used to deliver nicotine, flavorings, cannabis (marijuana[5]) and other chemicals.[4] The fundamental design of all vaping devices consists of three central components: a refillable or disposable liquid reservoir, a heating element, and a power source.[4] Vaping devices were manufactured as nicotine replacement products to facilitate smoking cessation and decrease the negative health impact of traditional nicotine smoking,[4] but clinical and experimental research has shown the potentially, lethal consequences of these devices.[33] E-cigarettes were initially advertised as a form of tobacco that could circumvent existing smoke-free legislation.[34]
Classically, e-cigarettes convert a liquid solution comprising nicotine, propylene glycol, glycerin, and flavors into aerosols,[4] although some e-liquids do not contain nicotine.[35] The amount of nicotine delivered varies.[36] The aerosols produced from e-cigarettes are not vapor.[37] There are many various designs and styles available in the market ranging from disposable devices that resemble cigarettes to pod mods that are refillable and rechargeable using a USB cable.[4] Prefilled pod cartridges can contain nicotine, tetrahydrocannabinol (THC), or cannabidiol with or without flavoring.[32] Recently, as of 2023, modern devices such as Juul have become more prestigious, rechargeable, stylized, controlled flavors, colorful, socially acceptable alternatives to conventional cigarettes, and equipped with attractive accessories.[4] Other prevalent vaping devices, as of 2023, include disposables such as Elf Bar.[38] Many e-cigarette devices can be modified to deliver other substances such as cannabis.[39] There are vaping devices that resemble ink pens, cup holders, and smart watches.[7]
Cannabis vaping is the process of using a battery-powered e-cigarette device or other vaporizer devices to heat and aerosolize cannabinoids, that are inhaled.[6] The heated cannabinoids are in a liquid solution such as a e-liquid or a solid such as a wax.[6] Cannabidiol and nicotine can be used interchangeably in some vaping devices.[26] There are numerous electronic vaping devices available such as disposable and reusable versions.[6] Reusable versions can be refilled using a cannabis-containing cartridge or a refillable e-liquid bottle.[6] The liquid solution can be made with nicotine, flavorings, propylene glycol, glycerin, various types of cannabinoids (i.e. delta-8-tetrahydrocannabinol, delta-9-tetrahydrocannabinol, and delta-10-tetrahydrocannabinol), and cannabidiol.[6] Vaping cannabis oil is convenient; it is discrete, affordable, and delivers the most amount of the compound compared with other routes of cannabis oil use.[21] Cannabis-containing e-liquids can be made with propylene glycol and glycerin, but because of their limited cannabinoid solubility, polyethylene glycol or medium-chain triglycerides are used to stabilize the cannabinoids more effectively.[7] This done prior to adding propylene glycol and glycerin, or without adding propylene glycol and glycerin.[7] The heating element of THC vaping devices is typically composed of ceramic, quartz, or glass.[40]
The design of vaporizers has evolved to reflect the changing preferences of cannabis consumers.[8] The earliest marketed vaporizer designed for dried flower was a portable, battery-powered desktop vaporizer.[8] Vaping cannabis oil using disposable or refillable cartridges has emerged more recently, as of 2022.[8] Cannabis vaping devices have been developed to facilitate vaping of 'solid' concentrates such as wax or shatter in which the concentrate is placed in a chamber or on a metal component that heats it.[8] Vaporizers can heat cannabis material to about 200 °C (392 °F) and can heat THC wax or oil to about 400 °C (752 °F).[41] Dabbing or dibbing is a process that allows the user to inhale a high concentration of THC by aerosolizing of a concentrate that has been placed on hot surface (the "nail").[32] Dabbing is also a term used when using THC concentrates and wax in a dab pen or a vaporizer.[32] With the rise in use of e-cigarettes, manufactures are producing products that allow consumption of both products, such as pen-sized vaporizers which are specially designed for dual use.[42]
The rising trend of vaping among the public could be based on perceptions of the safety of flavorants and inhaling aerosol substances.[4] The absence of the production of carbon monoxide or other combustion-related toxic substances during vaping might increase its use,[4] though later-generation and "tank-style" e-cigarettes with a higher voltage (5.0 V[43]) may generate equal or higher levels of formaldehyde compared to smoking.[44] A vast improvement in the palatability of e-liquids was observed; as nicotine-alone-based e-liquids have a bitter taste, there was a subsequent shift towards flavored e-liquids.[4] E-cigarette vaping devices can be used as illicit drug delivery devices and these devices are being used to inhale a range of substances including MDMA, cocaine powder, crack cocaine, synthetic cathinones, mephedrone, α-PVP, synthetic cannabinoids, opioids, heroin, fentanyl, tryptamines, ketamine,[3] lysergic acid diethylamide (LSD), and bath salts.[25] Oxycodone, a semi-synthetic opioid, can be breathing in by inhaling the vapors from the heated the tablet.[45] Drug users have discovered a method of adapting e-cigarettes to vaporize a potent hallucinogen known as N,N-Dimethyltryptamine.[2]
Detection of drugs of abuse
The majority of drugs of abuse can be observed at insignificant nanograms per milliliter (ng/ml) concentrations for up to two days in blood or plasma.[46] A one-time dose of a drug of abuse in the urine of users can be identified between one and a half to four days.[46] In a long-term user, it is possible to detect in the urine a drug of abuse for about seven days following the last time they used a drug.[46] In cocaine and cannabis users this could be longer.[46] Chidden exposed to cannabis had observable levels of delta-9-THC in their urine.[47]
The most commonly used emergency department method to screen for cannabis is a urine drug screen, which uses an immunoassay to detect the delta-9-THC metabolite 11-nor-delta-9-tetrahydrocannabinol-9-carboxylic acid (9-carboxy-THC).[48]
There is a limited availability of selective and sensitive rapid analytical methods to be able to screen test for synthetic cannabinoids.[49] Their consumption is often undetectable with available standard drug screening tests.[49] The use of highly specific and sensitive analytical methods is mandatory to be able to detect synthetic cannabinoid consumption.[50] The rapid development of new synthetic cannabinoids is a limitation even for targeted mass spectrometry screening methods, which can only detect the analytes they were designed for, and thus require continuous updating and validation.[50] Routine analytical approaches cannot monitor the new trends in the drug market because when a substance is finally identified and incorporated into an analytical panel, it is no longer used.[50] New approaches, such as high-resolution mass spectrometry, although expensive, can tentatively identify unknown substances without the need for reference standards.[50]
Since synthetic cannabinoids display a molecular structure different from that of delta-9-THC, their detection is often challenging, as they will not be spotted by the existing tests for screening of cannabis consumption.[51] Moreover, as they are generally extensively metabolized, the concentration of parent compound detected in urine after consumption is usually very low or absent.[51]
Basic e-cigarette operation

Examples of cannabis vaping devices and their different parts

Usage
Initiation

The initiation of cannabis use typically takes place in late adolescence.[52] Social factors in youth may determine the outcome between starting drug use and leading to more drug use.[6] Youth are more likely to first experiment with combustible cigarettes and/or e-cigarettes than they are with cannabis.[10] Cannabis initiation usually follows alcohol use though cannabis use can start before alcohol use.[53] African-Americans have an increased risk to experience this cannabis-first pattern compared to European-Americans.[53]
Risk factors leading to cannabis use in adolescence include influence by peers, home environment, parental history and monitoring, difficulties in school, personality traits, disinhibition of behavior, as well as externalizing behavior.[42]
Modes of cannabis consumption
People smoke cannabis in hand-rolled cigarettes (joints) or in pipes or water pipes (bongs).[54] They also smoke it in blunts—emptied cigars that have been partly or completely refilled with cannabis.[54] To avoid inhaling smoke, some people are using vaporizers.[54] These devices pull the active ingredients (including THC) from the cannabis and collect their aerosol in a storage unit.[54] A person then inhales the aerosol, not the smoke.[54] Some vaporizers use a liquid cannabis extract.[54] E-cigarettes are also used to inhale THC or cannabinoids.[2] Over-the-counter cannabidiol-based products include capsules, sprays, oil droppers, gummies, plant materials to be used for the inhalation of dry vaporizers, and e-liquid vaporizers.[55] A 2020 examination, of Reddit posts related to perceived therapeutic effects and popular modes of cannabidiol use, found that the most popular cannabidiol products were oil and tinctures ahead of vapes, edibles, pills, and topicals.[56] The most common ways of cannabis consumption among people with cancer and survivors in the US were external application at 80%, smoking at 73%, vaping at 12%, and eating edible products at 10%.[57] In contrast to other methods of use, cannabis vaping is correlated well with a higher uptake of cannabis.[25] The most recent method of use for cannabis consumption is vaping.[58]
Synthetic cannabinoids are used in a variety of ways.[59] They can be sprayed onto plant material and smoked, mixed into a liquid and vaped in electronic nicotine delivery devices (such as e-cigarettes), and added to herbal tea or to food and swallowed.[59]
Prevalence
In the 2010 decade, the sales of vaping products had grown exponentially, giving rise to health concerns regarding their exposure.[27] The widespread acceptance of medical and recreational cannabis usage in recent years leading up to 2023 has contributed to a surge in the drug's popularity in several countries.[60] In 2023, there was a growing popularity of e-cigarettes for recreational use in people who have not previously smoked combustible cigarettes.[12] Vaping nicotine is more prevalent than vaping cannabis.[25] Even though most e-liquids contain nicotine, cannabidiol and cannabinoid-based e-liquids consumption has increased significantly, especially among the younger population.[4] Cannabinoids are being consumed in varied formulations, and vaping is one such delivery method that has been increasingly used in the recent times, leading up to 2019.[21] Studies have shown that compared to nonusers, e-cigarette users were three times more likely to use cannabis.[42] A low percentage of cannabis vaping users are using cannabis for medical purposes.[20] The top three most observed substances misused by athletes are alcohol, cannabis, and nicotine vaping.[61]
Globally, there were about 193 million people using cannabis in 2018.[52] Cannabis is the most popular illegal drug worldwide,[62] in the US,[63] and the UK[19] and it is the most popular illicit drug among teens and young adults worldwide.[64] It is also the second most frequently used drug in the world, after alcohol.[65] Across studies, as of 2022, cannabis vaping was more common among males than females, and among older youth (e.g., high school compared to middle school students) in most studies, and among young adults compared to older adults.[66] Cannabis vaping was also more common among Hispanic youth compared with non-Hispanic White or Black, youth.[66] Some studies show that Black youths were more likely to vape cannabis relative to White youth, while other studies shows the reverse.[66] Greater socio-economic status may be a risk factor for cannabis vaping.[66] E-cigarette use with nicotine only or flavors, as well as use of cigarettes, cigars, hookah, and smokeless tobacco is associated with greater odds of cannabis vaping.[66] Former cannabis use, susceptibility to use cannabis, and peer use of cannabis, via vaping and other forms of cannabis consumption (e.g., ingesting, smoking), have also been shown to be related to greater odds of cannabis vaping.[66] Greater access to both e-cigarettes and cannabis; and parent, sibling, and peer cannabis vaping are associated with cannabis vaping.[66] Teens who use e-cigarettes or hookah are more than three times more likely to use cannabis.[10]
Other less studied correlations of cannabis vaping include alcohol use, non-medical prescription use, and illicit drug use; greater impulsivity and attention-related factors (e.g., inattention, perseverance); openness to new experiences and sensation seeking; psychiatric symptoms (e.g., depressive symptoms, conduct problems); delinquent behavior; low grade point average and skipping class; internalizing and externalizing problems; more exposure to e-cigarette marketing; school urbanicity (urban and suburban being greater risk versus rural); using cannabis in a vehicle; obtaining cannabis from dispensaries or recreational retailers versus from friends and family; low disapproval of nicotine vaping and of smoking cannabis regularly, lower perceived risk of cannabis use; lower perceived addictiveness of e-cigarettes; and earlier age of initiation of cannabis use, in any form.[66] The prevalence of dabbing is largely unknown.[67] Since the early 2000s, synthetic cannabinoid use has grown considerably.[68]
Impact of COVID-19 on prevalence
Lifestyle changes and mental stress and health were factors, in many studies, contributing to the rise in cannabis use during the COVID-19 pandemic.[69] As a consequence of various changes in lifestyle during the COVID-19 pandemic, boredom was one of the contributing factors to the rise in cannabis use.[69] Anxiety associated with being infected with COVID-19 was also one of the contributing factors to using cannabis.[69] Cannabis sales on illicit online markets have risen rapidly during the first 3 months of the COVID-19 pandemic.[70] This may represent an increase in personal use, which may correspond to greater rates of frequent use and cannabis use disorder.[70] The COVID-19 lockdowns resulted in a rise in vaping in the majority of reported respondents, whereas a drop or quitting of vaping was reported in the minority of reported respondents.[71] When vaping was temporarily banned in South Africa as a part of COVID-19 emergency response efforts, many vape shops circumvented this ban by switching their product offerings to include cannabidiol e-liquid and vapes.[26]
Pregnancy prevalence
Cannabis is commonly used during pregnancy, and breastfeeding mothers commonly use cannabis.[72] Around 50% of females reported to continue to use cannabis during pregnancy.[73] The most widely used illegal drug used among pregnant females is cannabis.[74]
Youth prevalence
Despite prior gains in lowering smoking rates and nicotine usage, the current data, as of 2023, indicates an alarming rise in vaping among younger people, especially adolescents.[4] The vaping of cannabis has picked up significantly as of 2020, especially among teenagers and millennials.[21] Many youths use cigars to make cannabis blunts (i.e., cigarillos with the tobacco removed and replaced with marijuana), and some use manufactured disposable cannabis products (e.g., vape pens, vaporizer cartridges, oils, and concentrates).[75] Youth tobacco smokers are more likely to use cannabis.[76] Teen targeted designs, vigorous marketing by e-cigarette and cannabis firms, easier availability as a consequence of pro-cannabis laws, and viewed as eliciting a minor potential risk are just a few of the reasons that may have caused a dramatic surge in demand for vaping cannabis products in underage minors.[25]
Using e-cigarettes at the age of 14 is linked to a nearly a four times hike in the chances of starting and continuing to use cannabis in the future in a couple of years.[77] Numerous underage minors are using vaping devices to inhale nicotine as well as cannabis.[25] Many newspaper stories associated with vaping opioids had discussed mainly youth who were vaping opioids during school.[78]
International prevalence
As of 2020, the lifetime and current prevalence of e-cigarettes vaping globally were 23% and 11%.[79] Lifetime and current prevalence of e-cigarettes vaping in women globally were 16% and 8%.[79] Also, lifetime and current prevalence of e-cigarettes vaping in men globally were 22% and 12%.[79] As of 2020, the current prevalence of e-cigarettes vaping in who had lifetime smoked conventional cigarettes globally was 39%, and in current smokers was 43%.[79] The lifetime prevalence of e-cigarettes vaping in the continents of America, Europe, Asia, and Oceania were 24%, 26%, 16%, and 25%.[79] The current prevalence of e-cigarettes vaping in the continents of America, Europe, Asia, and Oceania were 10%, 14%, 11%, and 6%.[79]
International prevalence among ex-smokers and current smokers
As of 2020, the current prevalence of e-cigarettes vaping in people who had lifetime used conventional cigarettes globally, and among current smokers globally were 39% and 43%.[79] In a 2019 study conducted in Malaysia, the current prevalence of e-cigarettes vaping in who had lifetime smoked conventional cigarettes, and in current smokers' conventional cigarettes were 4.3% and 8%.[79] In a 2016 study in the US, the current prevalence of e-cigarettes vaping among current smokers has been reported to be 24.1%.[79] One of the reasons for e-cigarettes vaping among current smoker’s conventional cigarettes is the curiosity to try it, helping to quit and reduce conventional cigarette smoking.[79] In a 2019 study conducted in Serbia, 12.8% of respondents reported that e-cigarettes vaping helped reduce their conventional cigarette smoking.[79]
International prevalence in college students
As of 2020, the lifetime and current prevalence of e-cigarettes in college students globally were 26% and 14%.[79] In a 2019 study conducted in five European countries including Slovakia, Belarus, Poland, Russia and Lithuania, the lifetime prevalence of e-cigarettes among college students were 34.4%, 42.7%, 45%, 33.4%, and 42.7%, and the current prevalence of e-cigarettes in these five countries were 2.3%, 2.7%, 2.8%, 4%, and 3.5%.[79] In a 2013 study conducted in the US, the lifetime and current prevalence of e-cigarettes vaping among college students were 9% and 30%.[79] In another 2019 study among health science students in Saudi Arabia, the lifetime prevalence of e-cigarettes vaping has been reported to be 27.7%.[79] In a 2018 study conducted in Pakistan on medical students, the prevalence of e-cigarettes vaping was 13.9%, while in another 2019 study, the current prevalence of e-cigarettes vaping was 4.4% on medical students and 12.4% on non-medical students.[79]
It has been reported in 2019 that the reason for the low prevalence among medical students maybe their high awareness of the dangers of e-cigarettes vaping during the period of their education course.[79] The lifetime prevalence of e-cigarettes in Malaysian college students has been reported to be 20.4% in 2018.[79] Differences prevalence of e-cigarettes vaping in studies can be due to the different target groups, differences in age groups, and method of conducted the studies.[79] According to the results of a 2022 review, the lifetime prevalence of e-cigarettes among college students showed increasing trend and the current prevalence of consumption has been decreasing.[79] The reasons for the declining trend of the current prevalence of e-cigarettes can be cultural differences and the creation of laws to monitor and prohibit the use of e-cigarettes.[79]
International prevalence in youth
As of 2020, the lifetime and current prevalence of e-cigarettes vaping among adolescents globally were 25%.[79] In a 2017 study conducted in Russia, the lifetime and current prevalence of e-cigarettes vaping among adolescents were 28.6% and 2.2%.[79] The current prevalence of e-cigarettes vaping among adolescents and school students is very wide in different countries, such as 1% in Mexico and 9.9% in the US.[79] In other countries such as China, the UK, Canada, and Poland, the current prevalence of e-cigarettes vaping among adolescents were reported 1.2%, 2.2%, 3.6% and 3.5%.[79]
According to the results, the trend of lifetime and current prevalence of e-cigarettes vaping in adolescents has been increasing, for example, the lifetime prevalence rate in the UK has increased from 22% in 2014 to 25% in 2016, also the current prevalence rate in the US has increased rapidly from 1.5% in 2011 to 20.8% in 2018.[79] In various studies, a positive relationship has been found between the amounts of monthly allowance given by parents to their adolescent children, so as much as the amount of money is higher, the probability of e-cigarettes vaping is also higher by children and this factor could have been a reason to increase e-cigarettes vaping.[79] Another reason for increasing the prevalence of e-cigarettes vaping could be the use of e-cigarettes to quitting conventional cigarette by adolescents.[79]
A 2021 meta-analysis found that among adolescents in the US and Canada, lifetime, past-12 month, and 30-day prevalence of cannabis vaping increased by two- to seven-fold, from 2013 to 2020.[66] Preference for cannabis products, therefore, may be shifting from dried herb to cannabis oil.[66]
Canada youth prevalence
As of 2020, the evidence indicates that the prevalence of cannabis vaping has grown among youth in Canada.[9] In Canada, one-third of youth e-cigarette users were also vaping cannabis.[25]
Unites Stated prevalence
The use of cannabis for recreational as well as medical use is on the rise recently, as of 2020, with more US states legalizing it.[21] Vaporizing cannabis oils is more prevalent in US states where it is legal.[20] There has been a rise in cases of cannabinoid hyperemesis syndrome because more US states have passed laws to make recreational and medicinal cannabis use legal.[80]
In the US, cannabis is the most widely used illegal substance used among pregnant females.[81] Among female participates in eight states in the US in 2017 who had a recent live birth, 9.8% reported using cannabis before pregnancy, 4.2% during pregnancy, and 5.5% after pregnancy.[82] The observed prevalence during pregnancy is similar to 2018 estimates from a national population-based survey, which found that 4.7% of pregnant women used cannabis in the past 30 days.[82] Among pregnant women in the US who reported drinking alcohol in the preceding 30 days, tobacco and cannabis were also commonly used.[82]
Unites Stated prevalence in new mothers
As of 2021, the use of cannabis has roughly increased by two-fold in US postnatal mothers since 2005.[47] Breastfeeding mothers tend to use cannabis less than non-breastfeeding mothers.[47] The evidence indicates that the majority of breastfeeding mothers using cannabis were also using it before they gave birth.[47]
Unites Stated prevalence in young adults and youth
As of 2020, the evidence indicates that the prevalence of cannabis vaping has grown among youth in the US.[9] Cannabis vaping is the most dominant way to use cannabis among youth and young adults in the US.[6] This is mainly due to the popularity of modifiable vaping devices along with new cannabis regulations and greater accessibility of cannabinoid products.[6] From 2017 to 2018, high school students' current usage of e-cigarettes increased from 11.7% to 20.8% and from 3.3% to 4.9% for middle school students in the US.[note 3][4] A 2020 survey in the US found 11.9% high-school seniors had used a cannabis vaporizer.[67] A 2019 US national study among high school students found that almost 40% of current users of e-cigarettes also used THC as an ingredient in their e-cigarettes.[42] In another study in 2015, up to 27% of high school e-cigarette users also were using the device to vape cannabis.[42]
Among young adults in the US, lifetime prevalence increased from 14.4% in 2017 to 34.6% in 2020.[66] Frequent vaping (defined as using more than 10 times in the last month) increased significantly among high school seniors from 2018 to 2019 in the US.[66] In the US, almost one-third of teenagers who vaped using an e-cigarette had also vaped cannabis, which frequently involved high concentrations of cannabis oils and concentrates.[83] In the US, past-year cannabis vaping was reported by 21% of adults 19 to 30 years old in 2022, the highest levels reported since the measure was first added in 2017 (12%), as well as a notable increase from the past year (19% in 2021) and five years ago (12% in 2017).[84] In the US, past-year nicotine vaping among this younger adult group also reached a historic high in 2022 (24%), nearly double the rate reported five years ago in 2017 (14%), when the measure was first added to the Monitoring the Future panel studies.[84]
Impact of legality of cannabis and subsequent cannabis initiation in Unites Stated youth
Youth who try an e-cigarette who live in US states that legalized recreational cannabis use have a greater likelihood of initiating cannabis use than youth who try an e-cigarette who live in other states where their use is illegal.[85]
France youth prevalence
After a dip in cannabis use in France, both cannabis experimentation and habitual use have been on the rise again since 2011, as of 2016.[86] Between 2011 and 2014, there was a noticeable rise in cannabis experimentation in youth in France.[86] In 2014, the rate of cannabis experimentation in youth was lowered (47.8% compared to 50.3%) than that of 2003 in France.[86] Between 2011 and 2014, the prevalence of habitual cannabis use in youth rose from 6.5% to 9.2% in France.[86] Between 2011 and 2014, the percentage of youth using cannabis daily rose from 3% to 4%.[86]
United Kingdom youth prevalence
Between 2016 and 2017, there was a 4% jump, from 7% to 11%, in 11–18-year-olds who had used an e-cigarette in the UK.[87]
A 2023 UK prospective cohort stud followed over 5,000 youth regarding the association between e-cigarette and subsequent cocaine use.[42] They found that youth who had used e-cigarettes before 14 years of age were two times more likely to use cocaine (7.6% versus 3.1%) when matched with non e-cigarette users.[42]
South Africa prevalence
Since its entrance into South African about 10 years ago, as of 2022, e-cigarette vaping has increased exponentially.[88] This has occurred without a proportional decline in cigarette smoking.[88] A 2017 national population-based survey found that almost one in ten participants aged 15 and older had used cannabis in the past 3 months in South Africa.[89] Dual use of vaping and cannabis use is widespread among high school students in South Africa.[90]
Co-use
Cannabis is often combined with consumption of alcohol or diazepam which increases cannabis sedative effects.[53] Addition of various other drugs enhances the euphoric effects.[53] For example, cannabis is often mixed with various drugs such as nicotine, cocaine, opioids, or hallucinogens such as LSD.[53] It is also mixed with drugs such as phencyclidine (PCP).[53] Such additions add to the complications of cannabis use.[53] Other additives include glutethimide and methaqualone, which have been popularized in the past.[53] Persons abusing cannabis who also take disulfiram due to alcohol abuse can develop increased psychoactive effects of cannabis due to THC blockage by the disulfiram.[53]
There is significant overlap between vaping cannabis and other methods of delivery, notably smoking.[9] Cannabis use is frequently associated with tobacco smoking.[11] Using e-cigarettes along with illicit chemicals is a cause for concern.[28] The large percentage of people experiencing cannabis use disorder in conjunction with experiencing other mental disorders is a cause for concern.[91]
A 2018 survey discovered that up to 11.7% of individuals who vaped have also vaped 3-4-methylenedioxymethamphetamine.[42] Up to 7.1% of e-cigarette users have been reported to have vaped α-PVP.[42] Up to 8.5% of e-cigarette users have reported vaping mephedrone.[42] Analysis of drug forums in 2018 has shown heroin in its free base form is also vaped via e-cigarette devices, and that more than 7% of electronic vaping users had vaped heroin through this method.[42] 7.3% of e-cigarette device users reported vaping fentanyl.[42]
Youth co-use
Youth cannabis vape users use other drugs such as vaping nicotine, drinking alcohol, and additionally use other drugs at greater percentages in comparison to non-cannabis vape users.[6] Teens who use e-cigarettes are more likely to use cannabis, not just in its traditionally combusted form, but also vaporized, as e-cigarette devices present opportunities for experimentation and customization.[34]
The increasing prevalence of e-cigarettes, particularly among youth and adolescents in the 2010 decade have led to an increase in the dual use of e-cigarettes with alcohol, cannabis, and other illicit drug use like heroin and 3-4-methylenedioxymethamphetamine.[42]
Subsequent other substances initiation in young adults and youth
Trying an e-cigarette once increases the chance for subsequent cannabis, alcohol, and non-prescribed Ritalin or Adderall use than in those who had never used an e-cigarette.[85] Nicotine use in youth can result to addiction to other chemicals, as it causes the brain to be more sensitive to the addictive properties of other psychoactive drugs.[85] Youth and young adults who have tried an e-cigarette is linked to a greater risk of later cannabis use and use of other illegal chemicals.[36]
Synthetic cannabinoids
Synthetic cannabinoids (e.g., Spice[note 4]) are often used as an alternative to cannabis.[92] Synthetic cannabinoids are popular because users often believe they are legal and relatively safe.[59] The frequency of synthetic cannabinoid use daily and weekly is distinctly higher among some vulnerable populations.[93] This includes teenagers and young adults, males, persons receiving mental health-related treatment, and persons using cannabis and other drugs.[93] Since these substances have a reputation of causing psychotropic effects at a relatively low cost, the increasing use of synthetic cannabinoids by vulnerable groups such as homeless people and prisoners has emerged as a particular area of concern.[51]
Motivation
Reasons for vaping cannabis include, to reduce or quit smoking cigarettes or other combustible tobacco products, as well as cannabis; to control dosage or amount of cannabis consumed and/or to maintain a sustained high; experimentation; mixing with flavors; friends' use; because it is enjoyable; stress relief; relaxation; sleep improvement; mood improvement; and its discreetness or ability to circumvent smoking bans.[66] The ability to regulate the evaporation temperature significantly magnifies the attractiveness of using e-cigarettes for vaping psychoactive drugs, such as THC.[2] Young adults like vaping and/or dabbing more than cannabis smoking.[94]
Some people have considered using medical cannabis as a substitute for prescription drugs.[95] The motivations for pursuing cannabis as alternative or complementary medicine include failure of conventional treatments, their unwelcome side effects, and a desire to find more natural solutions, often in a context of uncontrolled or terminal disease and severe pain, or for addiction to prescribed or illicit drugs.[56] This, coupled with the promotion of cannabis as natural and safe medicine, leads people to conclude that they have nothing to lose in trying cannabis.[56]
No legal ramifications, the ease of acquiring them, the fair cost, and the access online are the main reasons that appeal to users of synthetic cannabinoids and synthetic cathinones.[96]
Motivation in young adults and youth
Vaping cannabis among youth and young adults is typically more enticing.[6] This is because it is thought to be trendy and cool by users because of its ease of use, being simple to hide, and reduced irritation to the upper respiratory tract than smoking products, and its belief of being less harmful than combustible cannabis.[6]
Reasons for cannabis vaping, among youth and young adults, include that vaping cannabis is safer, healthier, and/or less physically irritating than cigarettes or combustible tobacco; to reduce or quit smoking cigarettes or other combustible tobacco products, as well as cannabis; to control dosage or amount of cannabis consumed and/or to maintain a sustained high; experimentation; mixing with flavors; friends' use; because it is enjoyable; stress relief; relaxation; sleep improvement; mood improvement; and its discreetness or ability to circumvent smoking bans.[66] A 2017 study reported a reason that may deter young adults from cannabis vaping, namely that vaping may be less safe than other forms of consuming cannabis.[66]
Motivation during pregnancy
The most common reasons for using cannabis during pregnancy among respondents in eight states in the US in 2017 were to relieve stress or anxiety, nausea or vomiting, and pain.[82]
Gateway theory
Youth exposure to nicotine can lead to subsequent abuse of nicotine and other substances, which is known as the gateway hypothesis.[10] Nicotine interacts with other neurotransmitter systems and as a result increases the rewarding effects of other drugs by enhanced activation of reward circuitry.[10] Developing brains are incredibly susceptible to long-lasting changes from perturbations during maturation, leading to behavioral changes that continue into adulthood.[10] Concern exists that youth who use Juul may result in gateway effects, like initiating cannabis use.[29]
Use of alcohol, tobacco, and cannabis are likely to come before use of other drugs.[54] Animal studies have shown that early exposure to addictive substances, including THC, may change how the brain responds to other drugs.[54] For example, when rodents are repeatedly exposed to THC when they're young, they later show an enhanced response to other addictive substances—such as morphine or nicotine—in the areas of the brain that control reward, and they're more likely to show addiction-like behaviors.[54] Early adolescent nicotine exposure in various rodent models increases the acquisition and intake of nicotine, alcohol, cocaine, and methamphetamine.[10] Early adolescent nicotine exposure in various rodent models also enhances the rewarding effects of nicotine, cocaine, methamphetamine, and opioids.[10] Adolescent susceptibility to co-use of nicotine and alcohol is reinforcing and leads to an increase in subsequent oral alcohol intake in rodents.[10]
Some research suggests that cannabis use is likely to precede use of other licit and illicit substances and the development of addiction to other substances.[97] For instance, a 2016 study using longitudinal data found that adults who reported cannabis use during the first wave of the survey were more likely than adults who did not use cannabis to develop an alcohol use disorder within three years.[97] People who used cannabis and already had an alcohol use disorder at the outset were at greater risk of their alcohol use disorder worsening.[97] Cannabis use is also linked to other substance use disorders including nicotine addiction.[97] There is concern that cannabis vaping may act as a gateway to experimentation with vaping of illicit and black-market products, especially amongst curious high-school students and young adults.[98] For decades, cannabis has been recognized as a gateway drug.[99]
Impact of marketing

There is a strong association with exposure to advertisements of vaping products and subsequent teenage vaping and cannabis consumption.[25] A growing body of literature shows e-cigarette marketing is prevalent, largely unregulated, and is an important risk factor for e-cigarette use among youth and young adults, especially.[66]
Most studies, as of 2022, descriptive content analyses of messaging about vaping cannabis on varied digital media platforms including e-liquid vendor online sites, the Google Play Store, YouTube, Instagram, and Twitter.[66] Together, these studies showed that content was primarily promotional, with very little prevention, cessation, or health messaging.[66] In 2020, in an effort to combat COVID-19, South Africa restricted tobacco and e-cigarette product sales over a 5-month period.[66] Studying this, a 2021 analysis shows that among 2661 e-liquids marketed by online vendors, about 29% were cannabidiol liquids, primarily fruit and tobacco-flavored.[66] During the restriction period, online vendors commonly promoted cannabidiol liquids instead of nicotine-containing e-liquid, salts, and concentrates.[66] Some research indicated advertising regarding the medicinal properties and cannabis consumption as a remedy to treating the COVID-19 virus was an extra incentive to using it.[69]
A 2020 review identified 79 Google Play Store applications that were related to vaping, three of which were specific to cannabis vaping, with the remaining specific to nicotine or unspecified.[66] Applications were commonly categorized as tools and lifestyle, health and fitness, and social and included do-it-yourself content for creating e-liquids and coils, games, social networking, purchasing e-cigarette products, smoking cessation services, pairing with e-cigarettes to adjust dosage and temperature, and e-cigarette cessation.[66] A 2018 study identified 214 YouTube videos over a one-year period in 2014–2015 related to cannabis vaping.[66] Most videos were generated and shared by lay persons and included personal experiences and tips, instructions, and product reviews related to cannabis vaping — although 21% of videos were clearly marketing a specific brand or product.[66]
—Nicholas Chadi and colleagues, Paediatrics & Child Health[25]
Reviewing content over a 4-month period in 2018, a study published in 2019 identified 18,200 stealth vaping YouTube videos that touted numerous discreetly designed e-cigarettes like Juul’s USB-like device, to enable discreet vaping of nicotine and cannabis, especially by youth.[66] E-cigarettes in these videos resembled pens, smart phones and other electronics, and even asthma inhalers.[66] Over a 2-week period in 2014, researchers identified over 400,000 Instagram posts with cannabis-related hashtags.[66] Of a random sample of 5000 of these posts, 2136 were explicitly about cannabis, in general.[66] About 9% (187/2136) of cannabis-related posts were advertisements, many of which (43%; 80/187) promoted devices or tools to use cannabis including advertising vape pens to use cannabis (13%; 10/80).[66]
A 2020 study identified 1775 Instagram posts with the hashtag #kandypens posted over a one-month period in 2018, and about 32% of these posts referenced using cannabis-related solutions in Kandy Pens.[66] These posts were made and distributed by laypersons, vendors, KandyPen’s official Instagram account, vaping advocates or enthusiasts, and influencers.[66] A 2020 study identified over 50,000 Juul-related Instagram posts over 2 ½ months in 2018, prior to Juul Lab’s voluntary actions limiting their own youth-oriented Instagram content in 2018, and over 6 months following these self-imposed restrictions in 2018.[66]
Cannabis-content in Juul-related posts was identified as a common theme, and one that grew in prominence over time in 2018.[66] A 2021 study identified cannabis vaping themes in Juul-related Instagram posts over 2 ½ months in 2018.[66] Cross-promotion of Juul with cannabis products was a prominent theme in commercial posts, and youth use of Juul with marijuana was a prominent theme in organic, non-commercial posts.[66] Two studies of e-cigarette-related tweets posted in 2019 identified cannabis vaping as a prominent theme, for example, cannabis vaping was discussed on Twitter as "the real problem" causing the vaping-induced lung injury outbreak.[66]

A 2019 study reported statistically significant longitudinal associations between marketing via numerous channels including digital media and cannabis vaping.[66] A 2019 study reported increased odds of using e-cigarette products with cannabis one-year later among 3720 college students who self-reported increased exposure to e-cigarette advertising via eight channels: gas/convenience stores, drug stores, grocery stores; liquor stores; bars or clubs; music events; radio or internet radio; online; magazines or newspapers; and billboards.[66]
Device selection
Vaping cannabis devices are offered in all generations of e-cigarettes.[7] Disposable cartridges are popular for vaping cannabis.[7] Pod mod devices are also popular for vaping cannabis.[7] About 27% of cannabis users vape using a pen or e-cigarette, while 15% of respondents use a vaporizer.[100]
Health concerns
Toxicology

Completely transparent labeling of every chemical found in cannabis vaping devices is not commonly practiced in the cannabis industry.[7] The specified percentage of cannabinoids in vaping products can be very different from what is claimed on the label.[7] 77.1% of the 70 e-liquids analyzed had underreported or overreported the concentrations of cannabidiol specified on the label.[101] Powder or liquid vaping formulations that contained synthetic cannabinoids have been falsely sold as delta-9-THC or cannabidiol.[102] Unclear or inaccurate labeling of cannabis products can lead to unexpected or adverse effects.[56] In addition to safety risks and unproven claims, the quality of many cannabidiol products may also be in question, according to the US FDA.[103] The US FDA is concerned that a lack of appropriate processing controls and practices can put consumers at additional risks.[103] For example, the US FDA has tested the chemical content of cannabinoid compounds in some of the products, and many were found to not contain the levels of cannabidiol they claimed.[103] Olivetol was identified in 22 out of 27 samples of vape products analyzed in 2022.[104] It may be irritating to the eye, skin, and respiratory system.[104]
There is extremely limited toxicological research on aerosols that were produced from THC or vitamin E acetate-containing e-liquids.[17] Cannabidiol, medium-chain triglycerides, and vitamin E acetate aerosols induce cytotoxicity, inflammation, and lung trauma, but the extent of these effects from each chemical varies.[17] In the aerosol that is generated, additional chemicals are detected in both nicotine- and cannabis-based e-liquids.[5] Dosages and potency of different cannabinoid preparations vary in strength and composition.[105] A 2018 study reported higher peak concentrations of THC in blood and stronger drug effects for pharmacodynamic outcomes (subjective drug effects, cognitive and psychomotor performance) by using vaporized cannabis as compared to equal doses of smoked cannabis.[66] The effects of inhaling chemical solutions of nicotine or cannabis vaping products vary considerably, and this depends on whether they are vaporized or heated.[20] Cannabidiol is less toxic than THC.[49]
Contaminants
One of the major safety concerns associated with cannabis use is the potential for contamination with biological, physical, or chemical contaminants.[60] Microbiological contaminants may be unsafe for cannabis users.[106]
Cannabis products and solvents may deliver an array of contaminants to the user.[67] Cannabis plants are sprayed multiple times throughout their lifetime.[107] This may lead to pesticides accumulation.[107] In immunocompromised people, bacteria and fungi could lead to infections.[106] Cannabis might be contaminated with microorganisms such as pathogenic bacteria, yeasts, and molds.[108] In an effort to curb microorganisms, pesticides may be used, which itself is a contaminant.[108] During the extraction process other substances may enter the e-liquid and cannabis extract preparations such as naphtha, ethanol, butane and petroleum ether, which might be detrimental to one's health.[108]
The US FDA has investigated reports of cannabidiol potentially containing unsafe levels of contaminants such as pesticides and heavy metals.[103] As of May 18, 2022, 36 US states and the District of Columbia listed a total of 679 cannabis contaminants as regulated in medical or recreational cannabis, including 551 pesticides, 74 solvents, 12 inorganics, 21 microbes, five mycotoxins, and 16 other contaminants.[95] A 2022 report shows that 5.1% of the cannabis samples for compliance testing exceeded California’s regulatory action levels of contaminants.[95]
Overconsumption of cannabis
One of the main risks associated with cannabis use is the potential for overconsumption, particularly when consuming edibles or other foods infused with cannabis.[60] This is because the effects of ingested cannabis can take longer to manifest and last longer as compared to when cannabis is smoked or vaporized, leading users to inadvertently consume more than intended.[60] For example, inhaled THC blood concentrations peak within 30 minutes, while ingestion takes approximately 2 to 4 hours or longer to peak after consumption.[109] Overconsumption of cannabis can cause severe side effects, including vomiting, nausea, anxiety, paranoia, and, in the extreme cases can lead to hospitalization.[60]
Cannabinoid intoxication, whether being used for medical or non-medical purposes, is more common via inhalation.[109] Cannabis toxicity in children can result in undesirable effects like poor muscle control, tiredness, seizures, and confusion.[109] Pharmacologic management for cannabis intoxication typically centers on use of benzodiazepines or atypical anti-psychotics.[53] Propranolol and rimonabant have been reported to be beneficial in management of acute, physiologic effects of cannabis intoxication.[53]
Adverse effects
There is an ongoing debate among experts regarding the safety of the cannabis plant.[60] The variety of products available as well as the ongoing modifications of e-cigarette and vaping devices makes it difficult to comprehensively evaluate the biological risk of vaping and the specific e-liquids.[12] The long-term implications of vaping are unknown.[110] The health consequences specific to vaping cannabis preparations remain largely unknown and speculative due to the absence of comprehensive, robust scientific studies.[2] The long-term implications of smoking cannabis compared to vaping cannabis among regular users is unclear.[111] Prolonged exposure to THC causes THC to accumulate in fat tissues.[109] Because cannabis can be used in different ways, with different levels of active compounds, it can affect each person differently.[112] Most of the documented unwanted effects of cannabinoids use, typically came from research involving recreational users.[113]
Unwanted effects of cannabinoid use vary from mild to deadly, and the risks involved depends on the method of consumption.[113] Short-term cannabinoid use raises the risk of adverse effects and major adverse effects.[114] Acute cannabinoid use seems to be related to increased blood pressure, tachycardia, and increased or decreased cardiac contractility.[105] Frequent undesirable effects of cannabinoid use include lost of strength, balance impairment, confusion, dizziness, disorientation, diarrhea, euphoria, hallucination, dry mouth, tiredness, sleepiness, drowsiness, nausea, and vomiting..[114] According to a 2014 study, long-term cannabis use can have unintended side effects such as stomach pain, thinning skin, depression, inability to work, and dropsy (a buildup of water in the body).[60] Exposure to high amounts of THC for recreational use has been found to negatively affect various physiological systems, including ophthalmological, gastrointestinal, respiratory, immunological, and hormonal systems.[60] The danger involved with cannabis vaporization devices and products vary.[108] The effects between the use of cannabis and other drugs are largely known.[52] The recent legalizing of cannabis use, as of 2019, around the world has generated concern with respect to its effects on the most-at-risk groups, including expecting mothers and teens.[72] Cannabis use is associated with a reduction of workplace productivity.[115] Using cannabis during work is connected to serious risks.[115] Cannabis impairment at work may lead to workplace accidents or death.[115]
There is a connection between cannabis vaping and an array of unwanted health effects.[9] in contrast to cannabis smoking, suggestive evidence indicates that cannabis or THC vaping carries unique and overlapping potential health effects.[10] Cannabis or THC vaping may result in an increased likelihood for acute lung damage, seizures, and acute psychiatric issues.[10] There is limited research in regard to the impact of cannabis vaping on cognition and behavior.[66] Cannabis vaping youth reported various physical health effects ranging from respiratory, oral, nausea, and headaches, in a 2021 qualitative study.[66]
Using cannabidiol products is not risk free.[116] It is unknown how cannabidiol use affects a person over time.[116] It is unknown how different modes of cannabidiol use (smoking, vaping, eating, applying to skin, etc.) affect a person.[116] There is a scarcity of clinical trials describing the long-term effects of using a minimal dose of cannabidiol.[101] As a result, cannabidiol-enriched e-liquids cannot be deemed to be safe.[101] Regulated cannabidiol products, including Epidiolex, have purported positive effects in a limited number of studies, but it is not possible to generalize and infer such findings to unregulated products.[101] Further, most of the US FDA-approved medications that contain cannabinoid derivative are not used as the first-line of treatment.[105] For example, a 2012 review states, "cannabinoids are not recommended as first-line treatment for the prevention of CINV [chemotherapy-induced nausea and vomiting]".[117] This is because, according to the same review, there are lower-risk and more effective approved medications.[117]
Synthetic cannabinoids
The exact mechanisms by which synthetic cannabinoids (such as AMB-FUBINACA and ADB-FUBINACA) produce their wide range of harmful effects, are not fully understood, and as of 2021, there are few preclinical assessments of their acute or chronic toxicological effects.[51] In addition, it is also unknown whether the toxicity of these compounds is caused by the parent compounds (which are rapidly metabolized) or by the action of metabolites and/or thermolytic products.[51]
Synthetic cannabinoids are dissolved in organic solvents and subsequently sprayed over dry plant matter to cause the misleading impression of being as natural as cannabis; or encapsulated for oral consumption.[51] The quality of synthetic cannabinoids often fails to meet pharmaceutical standards for purity or identification and labeling of all active ingredients, excipients, or impurities exceeding an acceptable standard percentage or estimated daily dose exposure.[118] In addition, most of the chemical ingredients are improperly identified on customs declarations, using a variety of inaccurate chemical descriptors or inappropriate descriptions (e.g., herbal incense).[118] The purity of these synthetic preparations varies widely and appears to be poorly controlled.[118] In some instances, seized bulk synthetic cannabinoid chemicals have been found to be contaminated with a variety of synthetic by-products and intermediates originating from the synthetic procedures employed, and a variety of structural analogs have been shown to degrade at commonly encountered room temperature exposures.[118]
Synthetic cannabinoid products are unsafe to use.[59] It is hard to know what the products contain or what the reaction to them will be.[59] There are no standards for making, packaging, or selling synthetic cannabinoid chemicals. That means that two packets of a brand-named product may have completely different chemicals.[59] The amount of the synthetic cannabinoid chemical(s) can vary between batches or even within the same batch.[59] Synthetic cannabinoid products may also be contaminated with other drugs or toxic chemicals, such as synthetic cathinones (e.g., bath salts or flakka).[59] Part of the potential danger is that they can contain various added but often unknown chemicals that are part of the manufacturing process.[53] However, some of the products found on the internet do not have significant amounts of impurities and adverse effects are due to the synthetic cannabinoids themselves and the potential additives.[53]
Synthetic cannabinoids can affect brain function.[59] Signs and symptoms include agitation and irritability, confusion and concentration problems, hallucinations, delusions, psychosis, suicidal thoughts, and violent behavior, seizures, sleepiness and dizziness.[59] Synthetic cannabinoids can cause other health problems such as breathing problems, gastrointestinal problems, heart attack, fast heart rate, high blood pressure, and stroke, Kidney failure, and muscle damage.[59] These health problems depend on many factors, including the specific synthetic cannabinoid, the dose (how much), and the duration of use (for how long).[59]
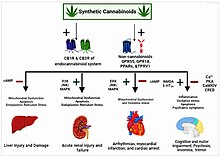
Evidence shows that using synthetic cannabinoids products leads to greater health risks than cannabis.[68] They have been associated with greater toxicity and higher addiction potential unrelated to the primary psychoactive component of cannabis, delta-9-THC.[68] Moreover, early cases of intoxication and death related to synthetic cannabinoids highlight the inherent danger that may accompany the use of these substances.[68] Synthetic cannabinoids are linked to a multitude of unwanted effects, such as cardiovascular and respiratory problems.[102] Synthetic cannabinoids target the endocannabinoid system in many body organs.[119] The specific mechanisms by the means of which synthetic cannabinoids generate their diverse effects and harms are not entirely clear.[120]
The long-term effects of using synthetic cannabinoids are not known.[67] The usefulness of their benefits outweighing their possible unwanted effects continues to be controversial.[121] The most common adverse effects of synthetic cannabinoids include agitation, drowsiness, dizziness, confusion, hallucinations, hypertension, tachycardia, chest pain, nausea, and vomiting, which typically have a short duration.[122] Synthetic cannabinoids can initiate pathophysiological changes in many tissues which can be severe enough to damage the normal functionality of human body systems.[119] The majority of synthetic cannabinoids-related side effects is mediated by activating both CB1 receptor and CB2 receptor.[119] The activation of these receptors can enkindle many downstream signaling pathways, including oxidative stress, inflammation, and apoptosis that ultimately can produce deleterious changes in many organs.[119]
Besides activating the cannabinoid receptors, synthetic cannabinoids can act on non-cannabinoid targets, such as the orphan G protein receptors GPR55 and GPR18, the peroxisome proliferator-activated receptors, and the transient receptor potential vanilloid 1, which are broadly expressed in the brain and the heart and their activation mediates many pharmacological effects of synthetic cannabinoids.[119] Generally, synthetic cannabinoids have lengthy half-lives, which can result in a longer mood-altering effect.[120] In 2021, it was reported of an accidental intoxication of a 16-year-old male after vaping with the use of the third generation synthetic cannabinoid, 5F-ADB.[123] The deaths and toxic effects linked to synthetic cannabinoids have led to concern worldwide.[68]
Interaction effects
Interaction effects have been observed between cannabis use and cigarette smoke.[124] Cannabis users report that nicotine enhances the pleasurable effects of THC.[10] Nicotine facilitates THC's hypothermic, antinociceptive, and hypolocomotive effects in mice.[10] Sub-chronic nicotine exposure in adolescent rats induces long-lasting effects in cannabinoid CB1 receptors, including increases in the hippocampus and decreases in the striatum.[10] The association between nicotine and cannabis use and the role of reward processing in both the cholinergic and endocannabinoid systems provides support to the hypothesis that nicotine may encourage and perpetuate cannabis use.[10]
As cannabis becomes more widely available with the adoption of US state medical cannabis laws, emergency department-related cannabis visits will likely rise.[48] Between 2004 to 2011, cannabis was the third most prevalent catalyst for drug-related emergency department visits in the US.[99]
Cannabis-involved emergency department visits among young persons were higher during the COVID-19 pandemic than during 2019.[125] Large increases in cannabis-involved emergency department visit rates occurred among children aged under 10 years, and among persons aged 11 to 14 years; rates among females aged 11 to 14 years increased more than they did among males.[125]
Past month cannabis use among adolescents aged 15 to 17 has increased steadily since 2006, and perception of great risk from smoking cannabis has decreased.[126] At the same time, the number of cannabis-related emergency department visits for adolescents aged 15 to 17 increased 50% between 2005 and 2010 (from 30,657 to 45,938 visits).[126] Population rates also increased during this period (from 232 per 100,000 population in 2005 to 355 per 100,000 population in 2010), which confirms that the increased number of visits cannot be attributed to population growth.[126]
These emergency department visits were for cannabis alone or in combination with other substances.[126] Data from the Drug Abuse Warning Network show that the increase in cannabis-related emergency department visits varied by gender.[126] Visits among males increased 54% (from 19,148 visits in 2005 to 29,424 visits in 2010).[126] While the number of visits among females appeared to also increase, the difference did not reach statistical significance.[126]
Acid-catalyzed ring closure of cannabidiol-delta-8-THC products
Over-the-counter cannabidiol-based products may be of questionable quality, are not subject to appropriate safety controls, and are characterized by unknown cannabidiol content.[55] Like other areas in the cannabis sector, there are quality control problems involving the acid-catalyzed ring closure of cannabidiol (ACRCC)-delta-8-THC products.[104] A more than negligible amount of the ACRCC-delta-8-THC is used in the vaping industry without information being made available about the safety of inhaling them into the lungs.[104] Consumer end products infused with ACRCC-delta-8-THC, which contain varying levels of the isomeric and breakdown by-products at levels above 30%, are being bought by people that are labeled as just being made with delta-8-THC.[104]
New psychoactive substances
The four classifications of new psychoactive substances (colloquially termed spice drugs,[128] designer drugs, new designer drugs,[96] research chemicals,[129] herbal highs,[128] or legal highs[102]) are synthetic stimulants, synthetic cannabinoids, synthetic hallucinogens, and synthetic depressants (such as opioids and benzodiazepines).[102] Synthetic cannabinoids are sold illegally, usually added to plant materials (crushed leaves), wrapped in aluminum foil—herbal mixtures—but can also be sold in a solid or oily form, if in their pure state.[45] Comparative to cannabis, these substances are essentially smoked, but oral use has been reported, and less commonly, injections.[45]
Recently as of 2022, e-liquids are also available.[45] It is common, in prison surroundings, to soak papers or tissues with synthetic cannabinoids, and then smoke them with tobacco or vape them using e-cigarettes.[45] Nowadays, it is possible to acquire these substances on online markets (darknet), through drug dealers, or even by exchanging products with other consumers.[45] New drugs are constantly appearing in recreational drug markets worldwide.[127] As soon as legislation makes a specific new psychoactive substance illegal, slightly different chemical versions can be made to evade the law.[127]
Misuse of new psychoactive substances remains a worldwide concern.[130] New psychoactive substance intoxication is often associated with serious and unpredictable adverse effects that can lead to hospitalization and even death.[127] For example, a stimulant-like new psychoactive substance can cause neurological symptoms like agitation, aggression, and psychosis.[127] An opioid-like new psychoactive substance can induce respiratory depression, which is a life-threatening condition when breathing becomes slow and shallow and may stop entirely.[127] The health risks of new synthetic cannabinoids are unknown.[59] Numerous deaths have been caused by taking designer opioids by themselves or taking them with other psychoactive chemicals.[122] In 2014, there were a total of 540 new psychoactive substances that were identified across the globe.[131] As of May 2023, 1,185 unique new psychoactive substances had been identified worldwide.[127]
Dabbing and dripping
Oils and concentrates used in vaping and dabbing (which is a specific method of inhaling THC concentrates) often have highly concentrated forms of THC and may contain additives or be contaminated with other substances.[132] The effects of using these more concentrated forms of THC are not well understood but may include a higher risk of developing cannabis use disorder.[132] Use of concentrates in vaping or dabbing devices may increase a number of health risks because of the concentration or strength of marijuana being used.[132] The health effects of dabbing and dripping are not well understood.[67] The act of direct dripping increases the exposure to toxicants and these users typically use modified devices.[20] Moreover, a modified device with higher-powered batteries that is used to increase the voltage leads to higher temperatures on the heating coils.[20]
Metal exposure
Increased use of e-cigarettes has raised numerous adverse health concerns involving the risks of heavy metals exposure via e-liquids and aerosols.[4] Studies, as of 2023, have confirmed that many heavy metals are present in both e-liquids and aerosols at potentially harmful levels, which endangers both user and exposure to passive vaping.[4]
Several metal levels have been detected in e-cigarettes, e-liquids, and human biological samples collected from vaping users.[4] The most commonly found metals were arsenic, copper, cadmium, chromium, lead, nickel, iron, and zinc.[4] The source of these metals is commonly from the metal coils incorporated in the clearomizer of the e-cigarettes device or from e-liquids.[4] A 2016 study found that the previous metal presence in nanoparticle size was less than 2.5 µm.[4] Hence, the ultrafine size range is more dangerous to the lungs than larger ones due to their ready access to the alveolar region and rapid absorption systemically.[4]
Respiratory and central nervous system

Vaping cannabinoid plants may lead to lung injury similar to that of smoking tobacco.[105] Vaping poses unique risks, as contaminants and additives to the vape medium may cause significant lung damage apart from cannabinoids.[105] These changes emerged even though cannabinoids are immune-inhibitory.[105] Inhaled cannabis products may directly impact the pulmonary immune system.[134]
The potential harmful consequences of e-cigarettes have been linked to respiratory system damage.[4] There is limited research on the consequences of vaping nicotine, e-liquids, or cannabis-enriched oils on the respiratory system.[135] With the wide variety of e-liquids available, as well as the potential combination of multiple e-liquids by users, the effect of individual or combinations of e-liquids and their ingredients on respiratory health is largely unknown.[12] Chemicals released from vaping of cannabis may damage the bronchial epithelium and disrupt alveolar surfactant thus interfering with gas exchange leading to respiratory failure.[21] The vaping of cannabis products (including cannabidiol) may lead to acute pulmonary toxicity.[55] Cannabis vaping has been linked to bronchitis in youth.[133] There are reports of acute lung injury associated with cannabinoid oil vaping with no clear mechanism of injury.[134]
Heavy metal exposure in e-cigarettes is linked to significant health threats, such as neurotoxic and carcinogenic effects.[4] Chronic inhalation of lead nanoparticles is linked with respiratory and central nervous system pathological changes.[4] Co-exposure to several heavy metals in e-cigarettes caused oxidative stress as indicated by increases in the generation of reactive oxygen species and the expression of ferritin light chain mRNA and heme oxygenase-1 mRNA and protein.[4] Heavy metals prompt apoptosis and evoke oxidative stress and DNA damage in lung cells.[4]
Cardiovascular effects
Cannabis was traditionally assumed to only have mild vegetative side effects.[11] There is no evidence that THC and other cannabinoids elicit a positive inotropic effect in the human heart.[11] Acute exposure to THC even of young healthy people to cannabis was reported to lead to severe cardiovascular events including myocardial infarction, sudden cardiac death, cardiomyopathy, transient ischemic attack, and stroke.[11] All the consequences of cannabinoid use on coronary circulation are not thoroughly known..[19] Cannabis use can negatively impact coronary artery disease.[60] Takotsubo is perhaps the most reported cardiomyopathy in cannabis users.[136] Cannabis use was found to be an independent predictor of transient ventricular regional ballooning, a marker of takotsubo cardiomyopathy.[136] There is a lack of studies investigating the pathophysiology of cannabis use and the development of takotsubo cardiomyopathy.[136]
As of 2022, an increasing number of studies showed serious cardiovascular effects, including acute myocardial infarction in healthy young people.[11] Myocardial infarction related to cannabis use is associated with tachycardia.[11] Tachycardia is the most reliable biomarker of cannabis use and occurs independent of the route of administration.[11] The reason why cannabis elicits tachycardia in humans but almost exclusively bradycardia in animals is unclear but may have to do with the relatively low heart rate level in humans.[11] Myocardial infarction can lead to life-threatening arrhythmias.[11] On February 28, 2024, the American Heart Association released a statement showing that a new study published in the Journal of the American Heart Association found a link between cannabis use, such as smoking, ingesting, or vaporization, and a substantially greater risk of heart attack and stroke.[137]
Inhaling THC can increase heart rate.[11] There is good evidence that the effect of THC on heart rate is the result of a combined action between central CB1 receptors in areas of the brain involved in cardiovascular regulation and peripheral presynaptic inhibitory CB1 receptors on sympathetic and/or parasympathetic nerve fibers.[11] Tachycardia can lead to complex adverse cardiac consequences such as a decrease in cardiac-stroke volume or a myocardial oxygen supply–demand imbalance.[11] Coronary flow is impaired by tachycardia, since blood supply to the coronary arteries can occur only during the diastole of the heart action.[11] Tachycardia, thrombus formation and/or coronary constriction have been discussed as factors involved in the development of acute myocardial infarction accompanying the use of THC or related compounds.[11]
Bone health effects
Cannabis use can negatively impacts bone functions.[60]
Brain effects
n the brain, CB1 receptors are extensively distributed in regions like the hippocampus, basal ganglia, cortex, amygdala, and cerebellum.[49] Cannabis induces dose-dependent toxicological changes in these brain regions.[49] There are changes in grey or white matter density in different regions of the brain including the frontal and parietal lobes and degenerative changes in the hippocampus and amygdala are reported more often.[49] These findings suggest that cannabis use leads to changes in the morphology and function of brain structures involved in learning and memory.[49] A 2014 study showed that there was a decrease in grey matter volume in regions, including the temporal cortex, temporal pole, parahippocampal gyrus, left insula, and orbitofrontal cortex in regular cannabis users as compared with occasional users.[49] The same results have been found in animal studies, which further corroborate that cannabis exposure results in volume reduction of CB1 rich regions.[49]
Functional magnetic resonance imaging studies also demonstrate that there are alterations in core regions of the brain including the ventromedial prefrontal cortex, insula, and orbitofrontal cortices, which are linked to motivation and decision making.[49] However, in addition to changes in the polar region of the brain, changes have also been noted in the medial temporal cortex.[49] The hypothesis of the reduction in grey matter volume suggests that it is due to abnormal pruning of the synaptic connections, which damages the brain maturation process.[49] The exogenous CBs interfere with the normal functioning process of the eCBs and alter the pruning activity of the synapses in brain regions including the cerebellum and prefrontal cortex.[49]
Cannabis arteritis
Cannabis use can cause cannabis arteritis (also known as limb arteritis[138] or juvenile arteritis[139]).[140] Cannabis arteritis has similar clinical and pathological manifestations as thromboangiitis obliterans (also known as or Buerger's disease).[141] As of 2007, there were about 55 cases documented in the literature since its initial description in 1960.[140]
This disease manifests mostly in young men.[140] Symptoms were claudication, acral pain, Raynaud syndrome, sub-acute distal ischemia of the lower legs, distal necrosis or gangrene of lower legs, early absence of distal pulses, and in some cases venous thrombosis.[140] Cannabis use can negatively impact cannabis arteritis.[60] Upper limb involvement is less frequently reported.[136] When initially diagnosed with cannabis arteritis, most people had experienced distressing distal necrosis of the lower and upper legs, following multiple months of claudication.[138] The mechanism causing the vasculitis in people diagnosed with cannabis arteritis is poorly understood.[99]
The pathophysiology of cannabis-associated arteritis is still under debate.[136] Vasoconstriction due to THC is often cited as the mechanism leading to cannabis arteritis.[136] Another hypothesis regarding the development of cannabis arteritis concerns arsenic as a contaminant.[136] Arsenic impairs angiogenesis by inhibiting vascular endothelial growth factor and inducing endothelial cell apoptosis.[136] The rare cases of cannabis arteritis could be associated with cannabis containing higher amounts of arsenic.[136] Migratory thrombophlebitis has also been reported as a possible complication of cannabis use.[136] The pro-coagulant effects of marijuana and platelet activation could explain these findings.[136]
Most cannabis arteritis cases have been reported in patients with concomitant tobacco use, raising the question of whether tobacco is the main substance behind the disease.[136] However, smoking cessation often does not impact disease progression, which refutes a diagnosis of thromboangiitis obliterans where it is expected that smoking cessation leads to an improvement of symptoms.[136] In contrast to thromboangiitis obliterans, the collateral arterial network is less developed in cannabis arteritis and proximal atheromatous lesions are sometimes seen.[136] An arterial biopsy in one case report found thrombosis with endarteritis associated with inflammation and fragmentation of the internal elastic lamina.[136]
The primary strategy for managing cannabis arteritis centers around discontinuing cannabis use.[140] Treatment may include aspirin and nifedipine.[141] Cannabis arteritis has a poor prognosis without cessation of the drug, with more than 50% of persons undergoing limb amputation due to worsening disease.[136] Tissue necrosis and gangrene seem to worsen during periods of heavy cannabis use, with remission noted after stopping use.[136]
Cannabinoid hyperemesis syndrome
Cannabinoid hyperemesis syndrome is a condition with recurrent vomiting due to high doses of cannabis.[49] It was initially described in 2004,[142] and a proposed a diagnostic criteria was published in 2009.[143] Though cannabinoids have been used to treat chronic nausea and emesis, a paradoxical effect on the gastrointestinal tract in noted in cannabis hyperemesis syndrome and three parts are described: prodromal, hyperemetic, and recovery phases.[53] In the initial prodromal phase, the individual experiences nausea upon waking, worrying about vomiting, and abdominal uneasiness.[86] This is followed by the hyperemetic phase, which involves severe nausea and excessive vomiting.[86]
It is difficult to understand the exact pathophysiology of cannabinoid hyperemesis syndrome, as some data suggest that it is due to dysregulation of the eCB receptors CB1 and CB2 in the brain and gastric system, while other data suggest that interaction of CBs with CB1 in gastrointestinal tract changes the gastric motility.[49] More than 80 cases have been described in the literature, as of 2013.[144] As of 2018, the persistent yearly growth in cannabis usage has led to an annual increase in the number of cannabinoid hyperemesis syndrome cases.[142] Widespread use of synthetic cannabinoids has increased the number of cannabinoid hyperemesis syndrome cases because they are potent against CB1 receptors.[49] Despite its widespread use, the factors leading to the development of cannabinoid hyperemesis syndrome in some people remains uncertain.[144]
Ceasing cannabis consumption is recognized as the most effective approach for treating cannabinoid hyperemesis syndrome.[145] Other treatments that show promise in relieving symptoms include hot water hydrotherapy, topical application of capsaicin, haloperidol, droperidol, benzodiazepines, propranolol, and aprepitant.[145] If cannabis use resumes, the hyperemesis phase of the disease may recur.[53]
and a proposed a diagnostic criteria was published in 2009:
Cause:
https://www.learnaboutcannabiswa.org/topics/health-effects/cannabis-hyperemesis-syndrome/
https://pubmed.ncbi.nlm.nih.gov/34227878/ Cannabinoid Hyperemesis Syndrome Survey and Genomic Investigation
https://pubmed.ncbi.nlm.nih.gov/?linkname=pubmed_pubmed_citedin&from_uid=34227878
Cannabis carcinogenicity
Reports have linked cannabis use to the growth of tumors, including in children whose mothers' used cannabis during pregnancy.[60] Depending on the dose and length of use, cannabis can also cause cancer and genetic changes.[60] The amount of time needed to cause an increased risk of cancer from cannabis use is uncertain.[124]
Cannabis use might carry a risk of cancers of the head, neck, and pharyngeal areas.[124] There appears to be a relationship between cannabis use and bladder cancer.[124] The available research suggests there is a relationship between cannabis use and testicular germ cell tumors.[124]
Dental effects
Cannabis users tend to have increased risks for dental cavities, oral infections, and periodontal disease.[53] Dysplastic changes and premalignant lesions can be identified in oral mucosa of cannabis users.[53] Use of local anesthetics in patients intoxicated with cannabis intensifies and prolongs pot-induced tachycardia.[53] Cannabis users often smoke tobacco and drink alcohol which increases carcinogen exposure and risk of oral squamous cell carcinoma which represent 95% of malignant lesions in the mouth.[53]
Kidney effects
Renal biopsy studies showed that people addicted to synthetic cannabinoids are afflicted with tubular necrosis and proximal tubular dilatation.[49] Long-term use of synthetic cannabinoids damages the kidney with abnormal urinalysis and increased levels of creatinine levels in blood.[49]
Lung cancer
Although the association between vaping and the development of lung cancer is not well established, the carcinogenicity of breathing in of substances such as nitrosamine compounds, humectants (propylene glycol and glycerin), flavoring compounds, cannabis and vitamin E acetate has been attributed to several possible mechanisms.[4]
The published data, as of 2023, regarding heavy metal exposure in e-cigarettes and the risk of lung cancer is scarce.[4] Because e-cigarette use is still relatively new, as of 2023, there may not have been enough opportunity to observe long-term impacts, including lung cancer.[4] Significantly, nickel is classified as a respiratory carcinogen, and the lung represents the most sensitive target of nickel toxicity.[4] A 2020 study identified chromium and nickel in e-liquids and aerosols and stated that prolonged exposure to nickel could substantially enhance the carcinogenesis process.[4] A 2017 study documented high levels of metal concentrations up to 400-fold in e-cigarettes, particularly cadmium, chromium, lead, and nickel in e-liquids.[4]
Mental disorder
There is emerging research suggesting cannabidiol, as a pharmacotherapy, has a possible role for treating neuropsychiatric problems, while THC is linked to short-term and neurodevelopmental propsychotic unwarned effects.[146] In comparison to smoking cannabis, emerging evidence indicates that cannabis vaping may be linked to increased behavioral and psychological problems.[27] Research suggests that certain genetic variants may increase the risk of mental health problems in individuals who use cannabis due to its impact on brain development, including neuroanatomical alterations, respiratory problems, metabolic and neurotransmitter functioning, and neuronal activation.[60]
Impact on a person's life
Cannabis use during youth may disrupt everyday life in a multitude of ways.[86] Compared to those who do not use cannabis, those who frequently use large amounts report lower life satisfaction, poorer mental health, poorer physical health, and more relationship problems.[54] People also report less academic and career success.[54] For example, cannabis use is linked to a higher likelihood of dropping out of school.[54] It is also linked to more job absences, accidents, and injuries.[54] Even occasional cannabis use has been linked to lower levels of educational attainment and a higher risk of escalation to the use of more illicit abused drugs.[42]
Dual use
E-cigarette use is a risk factor for downstream substance use, including cannabis initiation (the gateway hypothesis), which compounds health risks in dual users.[133] The use of more than one drug among adolescence has been linked to causing serious mental health issues such as becoming very depressed.[85] Users of both cannabis and tobacco is associated with a greater odds of having a mental health condition, as opposed to using any of them exclusively.[147]
Young adults and youth

The potential long-term effects of cannabis vaping on youth are largely unknown.[9] This is due to it being a fairly new phenomenon, as of 2022.[9] In regard to the unwanted health effects associated with cannabis exposure, young individuals are a vulnerable group.[10] As early as four years old, the effects of perinatal THC exposure can become evident.[149]
Compared with non-vaping users, youth cannabis vaping is tied to a 1.8-fold hike in respiratory problems like wheezing and dry coughing.[9] Prior research has shown a simultaneous rise of e-cigarette and/or cannabis use and mental problems, including depression and risk of suicide among youth.[17] A 2023 review does not recommend cannabis use for adolescents and young adults, as the development of the nervous system is continuing to occur.[150]
Brain and nervous system development
Nicotine use was associated with imbalances in brain development, whereby teens exposed to nicotine had less-developed regions in the prefrontal cortex responsible for inhibitory control, while the part of the brain responsible for the reward system (dopamine pathway) had been well matured as indicated on functional MRIs, which highlighted the imbalance in reward and control regions in the brain.[133] Nicotine affects the developing brain through its effect on cerebral cortex as well as in the hippocampus.[133] Nicotine uptake during teen brain development may induce neurotoxic modifications, including impaired memory, learning, and cognition.[35]
There is limited understanding of the effects of cannabis use on brain health.[151] Using cannabis during adolescence or young adulthood, before the brain is fully developed, may affect how the brain builds connections for functions like attention, memory, and learning.[152] These effects may last a long time or even be permanent.[152] Exposure to cannabis during the development of the nervous system may affect the endogenous endocannabinoid system that is vital for brain development.[72] Cannabis use is tied to a reduced cognitive development in youth.[9] Cannabis products of today contain a more potent amount of THC than they did fifty years ago, as of 2022, and as a result, they may elicit a more profound impact on the development of the nervous system.[note 5][9] The data suggests that THC-induced stimulation of the CB1 receptor can impede neuronal development, and this impacts the creation of synopses in teens.[153] Alterations in the specific areas with high densities of CB1 receptors in the hippocampal structure have been identified in adults who had started heavy cannabis use[note 6] in their teens.[153]
One of the ways the developing teen brain has a heightened vulnerability to the effects of cannabis is due its greater vulnerability to excitotoxicity from glutamate signaling.[153] Cannabis use can amplify this fragility through impeding GABAergic suppressive activity on glutaminergic neurons.[153] Moreover, cannabis use during teen years also can cause other structural changes such as modified grey matter volume and functional changes such as modified prefrontal cortex connectivity.[153] Because of the characteristics of the growing brain, neural changes happen at a faster pace among teens than adults.[153] Consequently, several of the brain's structural changes related to cannabis use are unique to this population.[153]
Surgery complications
There is a scarcity of information available in regard to recreational cannabis use in people receiving surgery.[154] Cannabis use can affect how the body responses to anesthesia, interfere with post-surgery treatment of pain, and amplify the threat of complications, while vaping can cause unwanted effects on the respiratory system and impede recovery following surgery.[155]
Male fertility complications
Cannabis use among males is correlated well with erectile dysfunction, spermatogenesis disorders, and a shrinkage in the size of both testes.[156]
Pregnancy complications

Evidence regarding the safety and health effects of cannabis use during pregnancy is largely inconclusive.[82] No safe level of cannabis use has been identified for use while pregnant.[73]
Prolonged maternal THC use can result in accumulation of THC in the developing fetus.[73] Cannabis use among females is correlated well with infertility and altered embryo implantation and growth.[156] Cannabis at any amount used during pregnancy or lactation is unsafe.[74] Using cannabis during pregnancy may increase a person's risk for pregnancy complications.[157] There is an association between the use of cannabis during pregnancy and a greater likelihood of unintentional preterm birth.[149] Babies exposed to THC via breast milk may show signs of sedation, poor feeding, and growth delays.[149]
The Centers for Disease Control and Prevention advises against the use of cannabis while pregnant.[158] The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics recommend refraining from cannabis use during pregnancy and lactation because evidence on safety and health effects are inconclusive or insufficient.[82]
Infant health
The health effects of a breastfeeding person's use of cannabis on their infant or baby are not fully known.[158] Breastfeeding mothers who use cannabis pass on THC into breast milk.[72] Consequently, this may be harmful to the baby.[72] Breastmilk can contain THC for up to six days after use.[159] This THC may affect a newborn's brain development and result in hyperactivity, poor cognitive function, and other long-term consequences.[159] Studies suggest that cannabis use by persons during pregnancy could be linked to problems with attention, memory, problem-solving skills, and behavior in their children later in life.[158]
The US FDA strongly advises against the use of cannabidiol, THC, and cannabis in any form during pregnancy or while breastfeeding.[159] Cannabidiol-containing products often make questionable health promises about cannabidiol.[159] Cannabis use during pregnancy may result in birth defects.[60]
There are many potential negative health effects from using cannabis and other products containing THC during pregnancy and while breastfeeding.[159] The US Surgeon General advised consumers that cannabis use during pregnancy may affect fetal brain development, because THC can enter the fetal brain from the mother’s bloodstream.[159] The US Surgeon General also advised that cannabis may increase the risk of a newborn with low birth weight.[159] Research also suggests that cannabis use during pregnancy increases the risk for premature birth.[159] Using cannabis during pregnancy potentially causes stillbirth.[159]
Direct exposure to vaping liquid

Young children could wrongly think cannabis vaping products are candies or toys.[25] There are non-negligible dangers of poisoning for children and teenagers via accidental or voluntary ingestion of e-liquids containing appetizing flavors, nicotine, and/or psychoactive drugs.[2] Young children have been hospitalized for cannabis toxicity due to being exposed to high potency products, such as vaping liquid.[160] The high potency products contain very high amounts of cannabinoids, and can result in ill effects such as sedation and hypoventilation.[160]
Second-hand exposure
An accurate evaluation of the overall health risks posed by passive exposure to vaped cannabis or THC aerosols, particularly on children's health, will require relevant human exposure data, which are lacking at present.[2]
Malfunctions and explosions
Vaping devices and vaporizers themselves pose a danger.[25] Vaping devices malfunctioning or exploding has led to injuries.[25]
When solvents are used to produce concentrates, the preparation process itself can be dangerous.[161] A number of people using butane to make extracts at home have caused fires and explosions and have been seriously burned.[161] A study conducted in 2015 looking at implications from cannabis legalization in Colorado reported that in a two-year period the University of Colorado Burn and Frostbite Center saw a substantial increase in the number of flash burns that occurred during amateur THC extraction using butane, some involving more than 70% of body surface area and most requiring skin grafting.[161]
Tourette's syndrome
Delta-9-THC has been proposed as the key therapeutic agent in treating Tourette's syndrome (also known as Tourette syndrome[162] and Gilles de la Tourette Syndrome[163]).[162] Preliminary evidence from case studies in adolescents and small randomized trials in adults suggests that THC may be effective in reducing tics.[162] However, high-quality studies in adolescents with Tourette's syndrome have not been conducted, as of 2023.[162]
A 2022 study compared the efficacy and tolerability of single doses of three vaporized medical cannabis products and placebo in reducing tics in adults with Tourette's syndrome.[163] Each participant received a vaporized single 0.25 g dose of delta-9-THC 10%, cannabidiol 13%, delta-9-THC/cannabidiol 9%/9%, and placebo at two-week intervals.[163] There were no statistically significant differences in tic severity for any of the cannabis-based medicine in primary outcome, but THC 10% was significantly better than placebo on the secondary outcome measures including assessments for premonitory urge, stress, and clinical global impression.[163]
A 2020 review does not recommend cannabis for reducing tics in children or adolescents.[164] There are a limited number of studies in this age bracket, and the prolonged neurologic outcome with cannabis use in youth remains a concern.[164]
COVID-19
Among the populations affected by COVID-19 are people engaged in substance use, such as people who smoke; vape (e-cigarette use); use opioids, cannabis, alcohol, or psychoactive prescription drugs; or have a substance use disorder.[70] Comorbid pathologies, such as those promoted by chronic vaping, negatively impact the integrity and function of the blood-brain barrier, which may facilitate virus entry into the central nervous system.[165] There may be a relationship between vaping and susceptibility to SARS-CoV-2 and COVID-19 complications.[70] People who vape nicotine or THC may be at risk for COVID-19.[70] Heavy cannabis use was linked to more severe COVID-19 symptoms and a greater chance of ending up in hospital.[69]
The evidence suggests that vape aerosols may damage lung tissue and reduce the lungs' ability to respond to infections.[70] Vaping cannabidiol was associated with severe COVID-19 problems.[55] A 2020 study suggests that nicotine-based e-cigarettes or vaping may contribute to the upregulation of ACE2 which may also play an important role in progression and outcome of COVID-19.[165] The impact of over-the-counter cannabidiol on the immunity of the SARS-CoV-2 infection is unclear.[55]
There were voiced concerns associated with the increased risk of becoming infected with the COVID-19 virus because of circumventing social distancing policies and sharing cannabis devices (e.g., vaporizers and hookahs) when used in close proximity to other people.[69] The method of using cannabis may increase the susceptivity to becoming infected with COVID-19 and also put one in jeopardy of the associated undesirable effects, like brain damage and death.[69] For example, people sharing paraphernalia (e.g., pipes, bongs, or vaporizers) when using cannabis had purportedly an increase in contracting COVID-19.[69] This was because of the inhaling of respiratory droplets that transported the virus.[69]
Most COVID-19 medicines could potentially interact with cannabis[69] THC, and cannabinoid.[166] As a consequence, cannabis users being treated for COVID-19 may experience unwanted adverse effects (i.e., nausea, diarrhea, or liver damage).[69] THC and cannabinoid are lipophilic, highly protein-bound molecules.[166] They have a long half-life, undergo bioaccumulation, and share metabolic pathways with cytochrome P450, drug transporters (e.g., breast cancer resistance protein), and substrates that bind to plasma proteins.[166] Furthermore, pharmacokinetic (e.g., warfarin and clobazam) and pharmacodynamic (e.g., valproic acid) interactions were described for THC and cannabidiol.[166] A 2020 investigation between cannabinoids and possible interactions with COVID-19 Drugs proposes that people diagnosed with COVID-19 should be asked about their use of substances containing cannabinoids, as these may significantly affect their reaction to the selected treatment method.[166]
Drug interactions
There is the potential for adverse medication interactions between cannabis and other medications, particularly those that are metabolized by the liver.[60] Cannabis can interact with certain medications, such as blood thinners and antidepressants, leading to unintended side effects or reduced effectiveness of these drugs.[60] Furthermore, there are concerns about the potential for cannabis to interact with other medications or supplements.[60] For example, a study found that consuming grapefruit juice with cannabis-containing products can increase the levels of THC in the blood, potentially leading to an increased risk of adverse effects.[60]
Harm reduction
Vaping cannabis can prevent the blending of cannabis with tobacco known as mulling (also called spliffs[65]) which may, as a result, decrease later tobacco use.[167] Although vaping cannabis may lower both tobacco use, and smoking cannabis and tobacco-associated respiratory and systemi disease, life-time use of recreational drugs was greater than one-third in UK adults and the continuous use of e-cigarette among underage minors demonstrates the misuse of vaping devices is potentially dangerous to public health.[167] As a result of the escalating cannabis use, practitioners and policymakers are urging for interventions aimed at reducing harm.[69]
Benefits
As of 2019, there has been increased interest in the role of cannabis for treating medical conditions.[168] The benefits related to cannabis use have been heavily debated.[167] Several putative health benefits of the main non-psychoactive cannabinoid, cannabidiol, have been under investigation.[2] Although cannabidiol is considered as a potential therapeutic drug because of its anti-inflammatory, neuroprotective, anti-psychotic, anxiolytic, anti-epileptic, and anti-cancer effects,[2] there are potential harms, side effects, as well as unknowns from their use.[103] Cannabinoids' beneficial or harmful effects are determined by how they act on the CB receptors and by their affinity for a particular receptor.[169] The cannabinoids can also interact with a multitude of other receptors, which explains the variety of effects encountered with these compounds.[169] Despite its long history of human use, issues of legality have contributed to significant gaps in the understanding of the efficacy of cannabis in alleviating symptoms of disease and the physiochemical properties of the more 500 chemicals that cannabis produces.[134]
While cannabis is generally well tolerated, it has been reported to have a potential for negative effects, particularly among older adults and people with chronic disease.[56] Cannabidiol can cause liver damage.[103] Cannabidiol can affect how other drugs a person takes work, potentially causing serious side effects.[103] Use of cannabidiol with alcohol or other drugs that slow brain activity, such as those used to treat anxiety, panic, stress, or sleep disorders, increases the risk of sedation and drowsiness, which can lead to injuries.[103] Male reproductive toxicity, or damage to fertility in males or male offspring of females who have been exposed, has been reported in studies of animals exposed to cannabidiol.[103] There is a poor understanding of the best-practice considerations for cannabidiol implementation, including an understanding of the efficacious dosages for cannabidiol-based opioid use disorder therapy as well as a lack of clearly defined tolerability and side-effect profiles.[170] While short-lasting side effects from cannabis use including drowsiness, loss of short-term memory, and dizziness are relatively well known and may be considered minor, other possible effects (e.g., psychosis, paranoia, anxiety, infection, and withdrawal) may be more harmful to people.[168] Mild harms were frequently reported, and it is possible the harms of cannabis-based medicines may outweigh benefits.[168]
Cannabidiol may be potentially helpful for treating epilepsy among different ages to decrease seizures.[150] Medical cannabis[note 7] may also be helpful for treating chronic pain amongst a variety of ailments (e.g., multiple sclerosis), for muscle stiffness and spasms in individuals with multiple sclerosis, for nausea and vomiting in individuals with more than one ailment, and for sleep with those who have cancer.[150] A potential therapeutic effect of cannabidiol is suggested for inflammatory and autoimmune diseases, anxiety disorders, schizophrenia, depression, Alzheimer's disease, Parkinson's disease, and diabetic complications.[55] There is limited clinical research on the medicinal use of cannabis and its efficacy and safety has not been substantiated.[19] There is also a lack of compelling evidence demonstrating the usefulness of using cannabis as medicine.[19] Medical cannabis contains unsafe levels of THC.[22]
Information on health effects, risk factors, and reasons associated with cannabis vaping among youth and young adults

Information on common additives and pollutants in vaping liquid and their effects

Driving under the influence of cannabis
Cannabis use may increase the likelihood of car collisions.[150] Driving under the influence of drugs, including cannabis, is dangerous.[173] Cannabis affects areas of the brain that control ones body's movements, balance, coordination, memory, and judgment.[173] Cannabis use can impair important skills required for safe driving by slowing one's reaction time and ability to make decisions, impairing coordination, and distorting perception.[173]
Gendered patterns of cannabis use likely influence the risk of driving under the influence with cannabis.[65] In one 2016 study, males were more likely to both vape and use cannabis edibles; and more frequent vaping was associated with driving under the influence.[65] In general, boys and young men tend to engage in riskier substance use behaviors.[65] Boys and men are also more likely to co-use cannabis and alcohol, which significantly increases impairment, driving errors, and accidents.[65] Further, compared to women, men tend to perceive lower harm with driving under the influence of cannabis, are less likely to believe that cannabis negatively affects their driving ability, are more likely to perceive their friends as approving of driving under the influence of cannabis, and are more likely to report an intention to drive after cannabis use in the future.[65]
Effects of vaping THC on simulated driving
As of 2021, only a few studies examined the effects of vaped THC on simulated driving.[100] In one 2019 study, participants vaped 11% THC.[100] Consistent with the smoked route, vaped THC increased Standard Deviation of Lateral (a measure of weaving), when required to follow and maintain a given distance to the car ahead.[100] In this same task, no effect on headway was found.[100] When instructed to follow GPS segments on highway and rural roads, no effects of THC were found.[100] In another study in 2018, participants vaped 12.9% THC and the only effect observed was on crash risk at one, three, and five hours post-cannabis use.[100] No effects were seen on braking reaction times, steering reaction time, lane-keeping speed control, intersection crossing, vigilance, obstacle avoidance accuracy, and obstacle avoidance crash risk.[100] Thus, the effects of vaped THC seem to vary depending on the task parameters.[100]
Nitrosamine compounds
Although vaping devices are marketed as safer than nicotine products, the correlation between e-cigarettes vaping and lung oncogenicity is still unknown.[4] It is documented that nitrosamine compounds attain adequate local concentrations within the distal bronchioles and alveoli, thus potentiating adduct formation and DNA damage.[4] The induced DNA methylation changes were supported by the findings in a 2018 study that e-cigarettes result from DNA adduct formation in murine bronchogenic tissues.[4] A 2019 study reported that mice exposed to e-cigarettes fumes for three months developed lung adenocarcinomas (9 of 40 mice, 22.5%); however, this tumor was particularly rare in mice exposed to filtered air or vehicle control.[4] They suggested that e-cigarettes induces DNA damage in the lungs and inhibits DNA repair in lung tissues, implicate e-cigarettes as a lung carcinogen in mice.[4] However, another study conducted in 1996 found that stream air-vaporized nicotine is not lung carcinogenic in rats.[4] This discrepancy in findings could be explained by the fact that the aerosol size of e-cigarettes is smaller than the aerosols generated in traditional tobacco, and the small size of e-cigarettes aerosol allows nicotine to penetrate deeply into bronchioloalveolar cells.[4] Moreover, e-cigarettes induce mutagenic DNA adducts (cyclic 1,N2-γ-hydroxy-propano-deoxyguanosine [γ-OH-PdG] and O6-methyl-dG) in the mice lungs resulting in DNA damage.[4]
It is suggested that tobacco smoke-generated reactive oxygen species may result in lung epithelial cells' DNA damage, prompting apoptosis and leading to the development of lung cancer.[4] It has been shown that e-cigarettes induce similar respiratory epithelial toxicity and oxidative stress, which play a chief role in malignant transformation.[4] This pathway appears to have multifactorial oncogenicity, with inflammation being directly associated with lung cancer and with the adverse inflammasome/macrophage activation inducing an overall immunosuppressive "cold" environment, hostile to T-Cells—proven to be important in lung cancer oncogenesis and malignant potential.[4] In addition, thermal breakdown of flavoring e-liquids creates carcinogenic organic aldehydes such as formaldehyde, acetaldehyde and acrolein.[4] It is recognized that formaldehyde, acrolein, and acetaldehyde are carcinogens.[4] Formaldehyde is a group 1 carcinogen that is associated with a five to 15 times greater lifetime chance of developing cancer.[20]
Compared to conventional smoking, e-cigarettes create lower levels of carcinogens and toxic elements such as nicotine, particulate matter, polycyclic aromatic hydrocarbons (PCA), formaldehyde nitrosamines, and heavy metals.[4] However, long-term exposure to low levels of the aforementioned elements poses serious health effects.[4] Moreover, vaping devices can deliver substantial nicotine levels that could become addictive.[4] Several potential carcinogenic mechanisms could play a role in lung cancer development, including increased DNA methylation, mutations, and binding to the nicotinic acetylcholine receptor that could induce tumorigenesis, survival, and invasion.[4] Furthermore, 80% of inhaled nicotine is metabolized into a nontoxic compound, cotinine which is excreted in urine.[4] At the same time, nearly 10% of inhaled nicotine undergoes endogenous conversion to nitrosamine compounds such as nitrosonornicotine and nitrosamine ketone.[4] These nitrosamine compounds are potent human carcinogens.[4] A 2017 study found substantial nitrosamine ketone derivative levels 4-(methylnitrosoamino)-4-(3-pyidyl)-1-butanol in pulmonary tissues.[4]
Propylene glycol and glycerin
Propylene glycol and glycerin are humectants commonly used in e-liquids with different ratios to produce aerosols that simulate traditional tobacco cigarette smoke.[4] The propylene glycol/glycerin ratio in the e-liquids is modified according to preferred plume (higher concentration of glycerin) or flavor (higher concentration of propylene glycol).[4] The US Food and Drug Administration (FDA) has approved the dermal or oral use of propylene glycol and glycerin in food, cosmetics and medications.[4] Although the US FDA has categorized these humectants as generally recognized as safe (GRAS), the safety data of inhalation exposure to these elements and their thermal degradation products in e-cigarettes is limited.[4] The heated propylene glycol and glycerin in e-cigarettes are known to undergo thermal degradation, producing pulmonary irritants, free radicals and suspected carcinogenic carbonyl compounds (acetaldehyde, formaldehyde, and acrolein).[4] Propylene glycol may create acetaldehyde and formaldehyde in cannabis vaping devices.[41]
It has been proposed that chronic propylene glycol/glycerin exposure damages epithelial barrier function by reducing lung cell volume and membrane fluidity, which could contribute to airway damage.[4] Many studies have observed that exposure to aerosols from propylene glycol and glycerin leads to an increase in pro-inflammatory and oxidative stress reactions.[4] A 2023 study found that propylene glycol is metabolized to methylglyoxal in airway epithelia leading to altering mucociliary function via reduction of Ca2+ activated and voltage-dependent K+ (BK) channels.[4] It is suggested that methylglyoxal is a potent glycation agent in the human body resulting glycation of proteins, DNA, and lipids and the gradual accumulation of advanced glycation end-products in cells and tissues.[4] Recently, as of 2023, emerging evidence indicated that methylglyoxal plays a role in cancer development and progression.[4] Furthermore, a 2020 study demonstrated the lung colonization-promoting effects of e-cigarettes on human breast cancer cells, indicating the risks of e-cigarettes on the lung metastasis of various cancers.[4]
Polyethylene glycol 400 and medium-chain triglycerides
Polyethylene glycol 400 (PEG 400) and medium-chain triglycerides are two agents that are commonly added to cannabis-based vaping products.[5] PEG 400 is a low-molecular-weight grade of polyethylene glycol that is widely used in cosmetics products and pharmaceutical formulations as a solvent/lubricant due to its low oral and dermal toxicity.[5] Medium-chain triglycerides is a fatty acid derived from coconut or palm that is often ingested as food or as a nutritional supplement.[5] Similar to propylene glycol and glycerin, both PEG 400 and medium-chain triglycerides are recognized by the US FDA as generally recognized as safe (GRAS).[5] However, the potential health effects of inhaling aerosols containing these compounds have not been investigated.[5]
A 2017 study conducted tests on thinning agents that are added to cannabis e-liquids.[41] Assessing the creation of harmful carbonyl compounds, propylene glycol, glycerin, and polyethylene glycol, polyethylene glycol 400, and medium-chain triglycerides were heated to a temperature of 230 °C.[41] PEG 400 and propylene glycol created formaldehyde and/or acetaldehyde at greater concentrations than glycerin and medium-chain triglycerides.[41]
Terpene
Most cannabis vaping cartridges contain a combination of cannabidiol and THC in different individual concentrations.[21] Along with the commonly used cannabidiol and THC, terpene is another compound that gained attention in recent times, leading up to 2020.[21] Terpenes are hydrocarbons compounds found naturally in the essential oils of plants, synthesized from trichomes of the plant.[21] It is presumed, according to a 2020 review, that terpenes aid in better absorption of cannabidiol and THC causing an entourage effect.[21] However, terpenes in the cannabis extract when heated to high temperatures during the vaping process degrade into methacrolein and benzene, which are known to cause acute lung injury and pulmonary edema leading to respiratory failure.[21]
Flavoring compounds
Vaping offers a diverse range of flavors, which is one of the main attractions to e-cigarettes among youth and non-smokers.[4] The traditional mint flavor was recently replaced by a wide range of artificial contaminants and flavoring liquids with a high risk of pulmonary toxicities.[4] Several flavoring additives are aldehydes, and recent studies have examined the impact of toxic aldehyde emissions on human health during vaping.[4] There are growing concerns regarding the safety profile of e-liquids flavors compounds.[4] The flavorings in THC extracts are potentially harmful.[20]
Importantly, e-cigarettes generate aerosols using a heating element, which can lead to the decomposition of e-liquids ingredients.[4] As coil temperatures rise, the liability of oxidation, pyrolysis, and thermal decomposition of organic aldehydes increases.[4] Thermal breakdown of flavoring e-liquids creates toxic organic aldehydes during vaping at high concentration levels that exceed occupational safety guidelines.[4] Numerous studies have exhibited the formation of toxic aldehydes, especially formaldehyde, in e-cigarettes aerosols during vaping.[4] A 2020 study discovered that the aldehyde emission levels in flavored e-liquids were 150–200% greater than those in unflavored e-liquids.[4] Many organic aldehyde derivatives are included (formaldehyde, acetaldehyde, acrolein, glyoxal, hexanaldehyde, and methanol).[4] There is a lack of data regarding the impact of e-liquid flavor mixtures on inhalation toxicity and lung oncogenesis.[4] Also, it is unclear whether the concentration limits are relevant to human exposure levels.[4] It is recognized that formaldehyde, acrolein, and acetaldehyde are carcinogens.[4]
Several mechanisms have been suggested by which flavoring compounds in e-cigarettes could contribute to lung cancer.[4] It is found that flavoring compounds in e-liquids induce intense toxic activity, an inflammatory response with macrophage activation and chemotaxis, vascular injury, dyslipidemia, and increased platelet reactivity).[4] These inflammatory and toxic processes lead to the formation of reactive oxygen species and encourage oxidative stress-induced lung tissue damage.[4] The reactive oxygen species could be generated intracellularly (via mitochondrial oxidative phosphorylation) or from exogenous sources (e-cigarette aerosols or cigarette smoke).[4] Reactive oxygen species plays a significant role in modulating the immune-inflammatory system and causes damage to DNA, cellular membranes, lipids, and proteins.[4] Raised reactive oxygen species levels could lead to the activation of polymorphonuclear neutrophils (PMNs), which generate further reactive oxygen species in lung tissue.[4]
A 2018 study demonstrated increased epithelial-mesenchymal transition (EMT) in A549 CCL-185 lung cancer cells, with resultant increased invasive/metastatic potential, on exposure to various flavored e-liquids including menthol-based.[4] Additionally, a 2020 study found that the pro-inflammatory effects of menthol were mediated directly via TRPM8, resulting in calcium influx in a BEAS-2B cell-line model.[4] Remarkably, altered intracellular calcium through TRPM8 has been previously shown to induce a neoplastic phenotype in lung cancer.[4] A possible adverse effect for e-cigarette users is a direct suppression on pulmonary epithelial cilia movement leading to impairment of clearance of toxic particles, which increases the risk of respiratory infections.[4]
Cannabis vaping products

Hemp Bombs CBD Oil https://commons.wikimedia.org/wiki/File:Hemp_Bombs_CBD_Oil.jpg
https://commons.wikimedia.org/wiki/File:Hemp_Bombs_CBD_Gummies.jpg
https://commons.wikimedia.org/wiki/File:Hemp_Bombs_CBD_syrup.jpg
https://commons.wikimedia.org/wiki/File:E-Juice_Bottles.jpg
https://commons.wikimedia.org/wiki/File:Hemp_Bombs_CBD_capsules.jpg
Not only nicotine is used in e-cigarettes, but other vaporized substances, especially cannabis derivatives, are widely used worldwide.[4] Cannabidiol vaping products have become extensively accessible in the US since their legalization in 2018.[4] However, data, as of 2023, are scarce on the relationship between lung cancer risk and vaping cannabis.[4] Other known risk factors for lung cancer, such as chronic tobacco use and flavoring compounds, could confound with cannabis and play a chief role in lung cancer carcinogenesis.[4]
The long-term effects of cannabis vaping are unclear.[6] Pertaining to cannabis exposure, youth are a vulnerable group to its unwanted adverse effects.[6] It is unclear how vaping cannabidiol negatively affects respiratory cell function.[4] Cannabis e-liquids are prone to thermal decomposition and pyrolysis, yielding diverse potentially toxic organic compounds.[4] Cannabidiol vaping products oxidized into a reactive cannabidiol quinone, which generates adducts with protein cysteine residues, altering protein function.[4] Cannabidiol quinone was found to induce cytotoxicity, apoptosis in specific cells, liver toxicity, and inhibit topoisomerase II and angiogenesis.[4] Thus, cannabidiol can potentially have harmful adverse effects on lung cells.[4] It has been shown that aerosolized cannabidiol induces apoptosis, pro-inflammatory reactions, reactive oxygen species generation, and enhanced cytotoxicity in bronchial epithelial cell lines.[4] The potential for cannabis oncogenicity could be attributed to toxic and pro-inflammatory effects on respiratory functions and can cause pulmonary irritation.[4] A study conducted in 2017 showed that synthetic cannabinoid-based e-cigarettes result in significant and relatively unpredictable pyrolytic organic reactions.[4]
Different oily substances were used in many e-liquids as thickening agents and diluents.[4] Vitamin E acetate was used as oil in e-cigarettes, mainly cannabinoid-based e-liquids.[4] Recent studies, as of 2023, show that pyrolysis of cannabinoid and nicotine e-cigarette mixtures can produce hazardous toxicants whose synergistic actions potentially drive acute lung injury upon inhalation.[4] Starting in 2019,[12] there had been a noteworthy upswing in vaping-induced lung illnesses among cannabinoid-based vaping users, characterized by acute lung injury or organizing pneumonia.[4] The vaping-induced lung illnesses were not restricted to users who vaped cannabinoids.[174] There were users of vaping products who were diagnosed with the vaping-induced lung illnesses who reported exclusively using nicotine products.[174]
Numerous cases of a vaping-induced lung illness had occurred prior to the outbreak of vaping-induced lung illnesses.[174] Similar cases of vaping-induced lung injuries were reported in the UK and Japan before the outbreak occurred.[note 8][176][177] This suggests the phenomenon has the possibility of being more pervasive.[176] However, the prevalence of lung injuries in various countries resulting from e-cigarette use is not clear.[note 9][176] Prior to February 2021, published case reports of vaping-induced lung injuries outside of the US was 17 from 13 countries.[174] There is probably under-reporting and possibly a lack of diagnosing of vaping-induced lung injuries outside of the US.[174]
—Antonella Marrocco and colleagues, Critical Reviews in Toxicology[17]
The severity of vaping-induced lung injuries varies, with the most severe cases leading to extended ICU stays, lung transplants, and death.[66] The majority of vaping-induced lung injury cases and death were related to young people vaping THC.[178] Patients in the Centers for Disease Control and Prevention investigation have reported symptoms such as cough, shortness of breath, chest pain, nausea, vomiting, diarrhea, fatigue, fever, or abdominal pain.[179] Some patients have reported that their symptoms developed over a few days, while others have reported that their symptoms developed over several weeks.[179] A lung infection does not appear to be causing the symptoms.[179] Fatalities were higher in non-Hispanic whites, those aged 35 years or older, and those with known histories of asthma, cardiac disease or a mental health condition.[48] Just over 50% of fatalities were in men and in obese individuals.[48] The most popular THC vape brands connected to the vaping-induced lung injury cases were Dank Vapes, proceeded by, Rove, Golden Gorilla, Smart Carts/Exotic Carts, Chronic Carts, and Cereal Carts.[17] As of 2023, a multitude of e-cigarettes such as cannabinoid vaping products, are readily accessible and mostly underregulated that are not covered under the jurisdiction of the US FDA, possibly enabling for the use of untested substances in e-liquids, which might trigger other vaping-induced lung injury outbreaks.[180]
The Centers for Disease Control and Prevention documented 2807 vaping-induced lung injury cases in hospitals and 68 deaths in the US.[4] Generally, vitamin E acetate is a relatively safe biologically inert compound; however, several vaping-induced lung injury cases have recently been documented.[4] Notably, vitamin E acetate has been determined in the bronchoalveolar lavage fluid of 29 persons diagnosed with vaping-induced lung injury.[4] It is suggested that vitamin E acetate and other e-cigarette compounds play a significant role in the pathogenesis of this injury.[4] A 2020 study proved that the thermal decomposition of vitamin E acetate produces highly toxic and irritant ketene gas (via elimination of the aryl acetate group) along with several other toxic reactive oxygen species with noticeable carcinogenic activity, including benzene and various alkenes.[4] The aforementioned thermal decomposition of vitamin E acetate plays an important role in lung carcinogenesis.[4] Wu and O'Shea's study demonstrated that vaping vitamin E acetate can lead to exposure to the toxic gas ketene.[4] In animal experiments, severe, acute lung damage was observed after 24 days of ketene exposure.[4] Because lung biopsies not commonly obtained in people diagnosed with a vaping-induced lung injury, the pathological drivers of symptoms and disease progression remain poorly understood.[12]
Two deaths were linked to vaping synthetic cannabinoids, one man died in 2017 and the other man in 2018.[181] Both were convicted and in jail in England.[181] A death was reported in the medical literature in 2020 of a 65-year-old woman who was vaping cannabinoids almost every day.[182]
What are the health risks of marijuana (THC)?
- Use of THC, which comes from marijuana, has been associated with a wide range of health effects, particularly with prolonged heavy use. The best way to avoid potentially harmful effects is not to use THC, including through e-cigarette, or vaping, products.
- Persons engaging in ongoing marijuana use that leads to significant impairment or distress should seek evidence-based treatment by a healthcare professional.
- The best way to avoid potentially harmful effects is to not use marijuana. For more information visit the CDC web page Marijuana and Public Health.
Cannabis vaping cartridges
Cannabidiol or THC oil used in the vaping cartridges contain various harmful compounds, and this result largely depends on the type of extraction solvent used.[21] Commonly used solvents are butane, propane, ethanol, and carbon dioxide.[21] Cannabis extracted using butane oil is called butane hash oil, contains a very high concentration of THC at 80% compared with only 10% to 25% with other extraction methods.[21] However, smoking butane hash oil that contains butane oil was linked to acute respiratory failure requiring intubation in a 19-year-old male in 2016 and the proposed mechanism was a direct injury resulted from inhalation of butane and/or other impurities.[21] In another case reported in 2019, an 18-year-old female was diagnosed with pneumonitis and respiratory failure secondary to using butane hash oil-processed cannabis.[21] People who use butane hash oil likely inhale some butane and other impurities along with the vaporized THC.[161]
Black market vaping products
Research shows use of illicit synthetic cannabinoids is associated with severe health problems and can be life-threatening.[183] Illicitly manufactured synthetic cannabinoids are typically added to liquid cartridges used in vaping devices or added to dried, shredded plant material so they can be smoked.[183]
Use of e-liquids via vaping devices may unintentionally expose underage minors to drugs that they did not want to inhale.[6] Non-reusable vaping devices, such as THC vape pens, are available on the black market from drug dealers.[6] These could contain undeclared chemicals, such as fentanyl, that were added on purpose during production.[6] Some of the black market disposable THC vape devices had been spiked with fentanyl, which can put the unknowing user in jeopardy of overdosing on opioid.[6] Nicotine and THC vaping are linked to other adverse effects in underage minors, such as seizures, cardiovascular and oral health complications, burns, and bodily harm from vaping device malfunctions, which were caused by devices that had exploded or became hot.[6]
Addictive properties
Nicotine and cannabis addiction have the same genetic risk factors, and the dual use of these two chemicals can exacerbate the degree of withdrawal symptoms which can hamper quitting efforts.[25] Nicotine is extremely addictive[35] and vaping nicotine can increase the addictive properties of cannabis and other chemicals.[25] This is because of its quick uptake and elevated stimulation of the brain's reward system.[25]
While the two main constituents of cannabis are THC and cannabidiol, THC seems to be responsible for cannabis' addictive potential due to its psychoactive properties and associated effects on brain dopaminergic function.[23] The evidence suggests that THC increases dopamine release similar to other drugs of abuse.[23]
Cannabis is extremely addictive.[22] Rapid drug delivery via vaporized forms of THC have been linked to greater reinforcement and addiction-related effects for example by promoting forms of neurobehavioural plasticity that contribute to compulsive drug-seeking.[184] The particular patterns of addiction, tolerance, and withdrawal that has been seen in hard drugs such as heroin, is also being seen in people vaping THC.[20]
Cannabis use disorder
Chronic cannabis use is associated with an increased risk of developing substance use disorders.[23] About 9% of those who use cannabis present with characteristic symptoms of dependence according to the DSM-IV criteria,[23] while up to 42% of heavy cannabis users have a dependency.[185] Children and young adults both have a greater likelihood of becoming cannabis dependence.[186] People who begin using cannabis before age 18 are four to seven times more likely than adults to develop a cannabis use disorder.[54] Being male and being a minority also increases the chance of becoming addicted to cannabis.[76]
Diagnoses of cannabis abuse and dependence in the DSM-IV did not include withdrawal due to uncertainty of its diagnostic features.[23] In the DSM-5, however, cannabis abuse and dependence fall under a diagnosis of cannabis use disorder (also known as marijuana use disorder[187] or cannabis addiction[188]) which now includes withdrawal from cannabis.[23] Another source states, at least 10% of those who are using cannabis have symptoms that conform to the specifications for a use disorder as described in the DSM-V and the International Statistical Classification of Diseases and Related Health Problems 10 or 11.[91] Using cannabis greatly improves the odds for addiction, and teens are four times as likely to become dependent on it in two years or less after initial use.[64] There is a dose-dependent, greater risk of developing a substance use disorder when using products that contain higher concentrations of THC.[64]
Some people who use cannabis will develop cannabis use disorder, meaning that they are unable to stop using cannabis even though it is causing health and social problems in their lives.[152] One study estimated that approximately 3 in 10 people who use cannabis have cannabis use disorder.[152] The risk of developing cannabis use disorder is stronger in people who start using cannabis during youth and who use cannabis more frequently.[152] A possible explanation for the rise in adolescent cannabis use disorder may be due the higher potency of THC found in products like vaping cannabis products offered in US states with legal recreational cannabis use.[189]
Cannabis use disorder withdrawal symptoms
A clinical diagnosis of cannabis withdrawal includes irritability, anger or aggression, nervousness or anxiety, sleep difficulty, decreased appetite or weight loss, restlessness, depressed mood, and physical symptoms causing significant discomfort such as shakiness or tremors, sweating, fever, chills, and headaches.[23] Typically, symptoms of cannabis withdrawal occur one to two days after cessation of heavy use and can last between seven and 14 days.[23]
The most common symptoms observed during cannabis withdrawal include irritability, anxiety, decreased appetite, restlessness, and sleep disturbances.[23] Sleep disturbances seem to be characterized by trouble falling asleep, decrease in total sleep time, and the presence of nightmares and strange dreams.[23] The severity of withdrawal symptoms was associated with greater negative impact on normal, daily activities suggesting that the effects of cannabis withdrawal seem to parallel withdrawal in other drugs of abuse.[23]
Many people who use cannabis long term and are trying to quit report mild withdrawal symptoms that make quitting difficult.[54] These include grouchiness, sleeplessness, decreased appetite, anxiety, and cravings.[54] Due to the concentrated strength of cannabis concentrates in dab pens and vaporizers, there is an increased likelihood of experiencing withdrawal symptoms following the discontinuation of use.[25]
Cannabis use disorder treatment
There has been a global increase in cannabis use disorder users seeking treatment.[24] Most people with cannabis use disorder treat their disorder and/or give up use in the absence of professional treatment.[24] Cannabis withdrawal symptoms greatly impact trying to quit.[24] Cannabis withdrawal symptoms are also correlated well with relapse.[24] Most adults and adolescents with cannabis use disorders relapse after therapeutic treatments.[190] Treatment of cannabis withdrawal and dependence is difficult.[53]
Cognitive behavioral therapy integrated with motivational interviewing is helpful for treating cannabis dependence.[24] Cognitive behavioral therapy can be used along with motivational enhancement therapy.[24] As of now, no scientifically validated pharmacotherapies are available to treat cannabis withdrawal or urges.[24] The drug buspirone has demonstrated some potential for helping with cannabis cessation.[191] Reasons for a large percentage of cannabis use combined with low rates for treating cannabis use disorder may be due to numerous people with this disorder do not get treated, have limited access and funds, and involve a stigma surrounding getting treated.[189] Other reasons that may contribute to not getting treatment include wish for relying on one's self, thinking that treatment is not needed, and limited understanding of the issue.[91] Individuals with co-occurrence of cannabis and tobacco use tend to have higher abstinence rates if treatment includes measures aimed at dual abstinence.[53]
Many different pharmacological treatments have been investigated for reduction of cannabis withdrawal symptoms, primarily through modulation of cannabinoid receptors but also through other neurotransmitter systems including glutamate, dopamine, norepinephrine, serotonin, and GABA.[23] A 2018 review of the different pharmacological treatments for cannabis use disorder and cannabis withdrawal concluded that therapies targeting specific symptoms of withdrawal (such as anxiety, irritability, sleep disturbances, and decreased appetite) should be administered in conjunction with treatments that target reduction in cannabis use and prevention of relapse.[23]
Promising candidates for treatment of cannabis use disorder that prevent relapse include naltrexone, gabapentin, and N-acetylcysteine.[23] The greatest reduction in multiple withdrawal symptoms has been shown with treatment using CB1R agonists such as dronabinol (oral THC), nabiximols (a combination of THC and CBD), and nabilone.[23] Surprisingly, previous studies have not shown cannabidiol as a potential treatment for cannabis withdrawal despite its anxiolytic effects.[23] With CB1R agonists as potential treatments, it is necessary to consider the abuse potential of these drugs, according to a 2018 review.[23] Dronabinol, nabilone, and nabiximols seem to have a lower abuse potential than smoked cannabis, but in one 2015 study of cannabinoid replacement therapy, dronabinol and nabixmol had higher self-reports of liking than placebo drugs.[23] Released in 2008, the Marijuana Anonymous World Service's 12-step workbook is designed to help people quit cannabis use.[186]
Synthetic cannabinoid use disorder
Synthetic cannabinoid use disorder is a clinically serious issue.[93] A handle of medical research illustrates a pattern of synthetic cannabinoid use that is in line with the existing criteria for diagnosing a substance use disorder.[93] This includes lack of control, tolerance, urges, and withdrawal symptoms.[93]
Synthetic cannabinoid use disorder withdrawal symptoms
Symptoms of withdrawal vary from mild to serious.[93] This includes seizures, psychosis, suicidal thoughts, and trying to kill oneself.[93] Synthetic cannabinoids may be addictive, since some people have reported withdrawal symptoms after heavy use over a long time.[59] If one suddenly stop using synthetic cannabinoids, they may develop symptoms such as headache, nausea and vomiting, severe anxiety, sweating, or trouble sleeping.[59] One may have more severe symptoms if they use synthetic cannabinoids frequently for a long time period and suddenly stop.[59] More severe symptoms include breathing problems, chest pain, palpitations, heart rate, and seizures.[59] Experts think that the severity of these symptoms is related to how much synthetic cannabinoid is used and for how long.[59]
Synthetic cannabinoid use disorder users initially experience pleasurable effects which is following by feeling of uneasiness and an intense urge to use the drug again.[93] Withdrawal symptoms from synthetic cannabinoid use develops quicker than that of cannabis use.[93]
Synthetic cannabinoid use disorder treatment
There is no specific antidote for synthetic cannabinoids, but health care professionals can provide supportive treatments, such as oxygen, intravenous fluids, and medications to control seizures, agitation, and nausea.[59] If one becomes sick after using synthetic cannabinoids, it is recommended by the Centers for Disease Control and Prevention to seek immediate medical attention such as calling 911 or going to the closest emergency room.[59]
The general treatment of acute poisoning by synthetic cannabinoids is often performed through supportive measures, namely by controlling signs and symptoms and fluid therapy to obviate electrolyte disturbances.[51] Persons experiencing irritability, agitation, anxiety and seizures, both associated with synthetic cannabinoid intoxication and withdrawal syndrome, are usually treated with benzodiazepines as the first-line approach.[51] Antipsychotics are also administered to manage psychotic symptoms.[51]
Treatment for synthetic cannabinoid use disorder tends to follow the interventions used for treating cannabis use disorder, which consist of motivational enhancement and cognitive behavioral therapy.[93] A 2019 review recommends approaches to minimize use and/or impact.[93] Reports suggest that diazepam and quetiapine may be used for treating transient withdrawal symptoms.[93] There may be a need for a more intensive treatment, because of the higher potency of synthetic cannabinoids causes a greater degree of dependence.[93]
Vaping cessation
Because of the rise in prevalence of e-cigarette vaping among children and youth worldwide in recent years leading up to 2023 as well as the growing evidence regarding the possible dangers of e-cigarettes among children and youth, prominent public health agencies have urged for strategies to combat the rise in e-cigarette vaping.[192] The evidence indicates, as of 2023, that e-cigarette users and dual users are trying to obtain information on how to stop vaping.[193] Interest in vaping cessation seemed to dramatically increase during the vaping-induced lung injury outbreak.[178] There are no evidence-based standards for treating nicotine addiction in children and adolescents.[34] The most compelling level of evidence to support treating nicotine addiction in youth is with the use of behavioral therapies.[83]
THC and synthetic cannabinoids yield

The rate at which a drug enters the brain largely determines its euphoric effects.[2] Recreational cannabis users will, therefore, prefer to achieve peak blood concentrations of THC by choosing e-cigarettes that are able to deliver a significant dose in a minimum amount of time.[2] To achieve these goals, two important parameters would need to be met.[2] First, the maximum THC blood level would need to be reached in a reasonable number of puffs (e.g., fewer than a dozen).[2] Second, the length of time required to reach this peak concentration would need to be as short as possible (e.g., a dozen of minutes).[2]
It is known that each puff consumes about 5 mg of e-liquid.[2] The maximum proportion of butane hash oil in e-liquids is about one third, but good quality butane hash oil (decarboxylated and purified) may contain 80% THC.[2] Therefore, 5 mg of butane hash oil e-liquid could contain 1.3 mg THC.[2] Using a bioavailability of just 30% and a minimum THC psychoactive IV dose of 1.5 mg, a mere four puffs could deliver about 4 × 0.4 mg THC = 1.6 mg THC into general blood circulation.[2] This is a high enough dose to produce a psychoactive effect.[2] Once in the bloodstream, 90% of THC (and cannabidiol) are distributed to the plasma, while the remaining 10% are distributed to red blood cells.[105]

The rapid absorption of THC from vaporized cannabis and the onset of intoxicating effects which parallel absorption from the lungs tend to limit an individual's THC intake.[194] Inhaling aerosolized cannabis is the fastest method of delivery and has more anticipated absorbability, with THC blood concentrations detectable within seconds to minutes, and peaks at 15 to 30 minutes.[195] Studies have shown that the vaporization of medical cannabis can produce similar blood concentrations of THC to those achieved by smoking conventional cannabis.[42]
A concern is the marked increase in concentrations of delta-9-delta-THC, the principal psychoactive agent contained in cannabis, since the 1970s and most specifically since the 2010s decade.[196] Concentrations of 9-delta-THC ranged between 0.5 and 4.0% in the 1970s, whereas contemporary strains from North America, Europe, and Australia attain concentrations of 15% and over.[196] In contrast to smoking cannabis, vaping THC absorbs faster and has greater THC blood concentrations.[27]
Tests conducted on first-generation synthetic cannabinoids on animals did not generate the cataleptic effect as THC does, but the dose tested may not have been high enough to cause this effect.[94] Extremely potent second-generation synthetic cannabinoids such as AB-CHMINACA and XLR-11, evoke strong behavioral changes in animals after intraperitoneal and inhalation exposure.[94] Synthetic cannabinoids[note 10] like Spice and K2 may have been chemically altered in such a way that makes them "potentially dangerous".[197] They could be 100 times more potent than THC and are associated with greater long-lasting and injurious downstream pharmacodynamic changes.[197] Chemically modifying the structure of psychoactive substances is a widely practiced technique in the illegal drugs market, to circumvent existing drug control laws.[198] New synthetic cannabinoids are emerging rapidly and continuously, as of 2022.[50]
Positions of professional organizations
General recommendations
Leading professional organizations, such as the American Academy of Pediatrics, the American Medical Association, the American Society of Addiction Medicine, and the American Academy of Child and Adolescent Psychiatry each have positions highlighting cannabis as a public health concern and are against additional activities that promote legalization.[199]
In 2022, the American Heart Association released a position statement that stated, "Public health efforts should be considered to raise awareness about the potential negative effects associated with the use of marijuana in the general population."[151] They also recommend the "use of standardized concentrations of biologically active components and health warning labels on available formulations. In addition, the use of marijuana should be individualized and closely monitored."[151]
In 2022, the American Association of Nurse Practitioners (AANP) released a position statement that stated, "AANP supports efforts for the continued scientific review of medicinal marijuana and cannabinoid use, the establishment of evidence-based therapeutic recommendations for marijuana and the inclusion of marijuana and cannabinoids in nursing education and continuing education. AANP supports policies that authorize NPs to discuss treatments and treatment alternatives in open and direct dialog with their patients. AANP believes that these conversations are essential to patient care and should be exempt from criminal or professional prosecution, such as loss of licensure."[200]
The American College of Obstetricians and Gynecologists has issued guidelines advising obstetrician and gynecologists to counsel women to avoid using cannabis while attempting to conceive, during pregnancy, and while breastfeeding.[73] According to American College of Obstetricians and Gynecologists Committee Opinion, there is a lack of data to fully comprehend the effects of cannabis use on babies during lactation.[73] As a result of the limited data currently available and until future research can provide clarity on the matter, the American College of Obstetricians and Gynecologists cautions against the use of cannabis during breastfeeding.[73]
The American Academy of Pediatrics realizes the limited data available to be able to provide clear guidance for clinicians.[73] A 2018 American Academy of Pediatrics statement recommended to avoid the use of cannabis during breastfeeding, due to the lack of evidence to assess its impact on the developing infant.[73] The Centers for Disease Control and Prevention in 2018 advised against the use of cannabis while pregnant because it may adversely affect the unborn baby's development.[73]
Public health
Several of the same public health concerns are being debated in relation to vaping with cannabis and the use of e-cigarettes.[201] The effect of vaping on public health remains unclear.[202] The increased use of e-cigarettes and cannabis vaping, especially among young individuals, females, and non-smokers, is a significant public health concern.[4] An area of public health concern is the use of vaping devises to inhale synthetic cannabinoids.[102] Vaping-related lung damage is a public health problem, which has been mostly associated with vaping THC, yet cases of damage with vaping only nicotine have been identified.[182] The most significant health concerns involve the vaping of cannabinoids by children and teenagers.[2] For North American youth, vaping THC and hashish is a serious public health dilemma.[202] Pro-cannabis recreational laws have led to public health concerns.[189]
The acceptance and use of cannabis as medicine has run ahead of research evidence.[56] The traditional requirements of drug trials, approvals, and post-licensure surveillance are either not applied or not consistently applied to medicinal cannabis.[56] Consequently, there is a public health concern that evidence for the efficacy and safety of medicinal cannabis is not fully established for a range of clinical contexts.[56]
By promoting e-cigarettes as the healthier option, tobacco companies are attempting to rebrand themselves.[34] A pressing concern stems from the repetitive efforts of tobacco companies to rebrand themselves to target vulnerable underage minors.[203] With regard to the tobacco industry's considerable investment in e-cigarettes globally, their intent "appears to be to sustain, rather than replace, cigarette sales, and to increase their influence and credibility with respect to e-cigarette policy and regulation".[34] A critical public health issue is the onset of using e-cigarettes in non-smoking youth, as it may induce damage to the respiratory system, yet also result in smoking cigarettes and vaping other chemicals, such as cannabis derivatives.[204]
Public perceptions
Cannabis remains a controversial drug, because its illegal US federal status places it in conflict with the popular notion that pot is a harmless chemical – a notion made fashionable or trendy by many media and Hollywood personalities who may promote its use to enhance their joie de vivre.[53] Although it is widely viewed as a safe drug, cannabis use has been strongly linked to various cardiovascular adverse events.[136] While in some parts of the world, it is viewed as a helpful medicine, in other parts it is seen as a dangerous substance if taken in large amounts, particularly when it comes to the consumption of cannabis-containing foods or beverages.[60]
Youth believe that cannabis is one of the least detrimental psychoactive drugs.[25] This is partly due to it as generally being seen as being more natural than other chemicals.[25] Particularly with the use of vaping devices, the perceptions of harm with utilizing cannabis is thought of as minimal.[25] Cannabis use using a vaping device is frequently seen as safer than other methods of delivery.[25] There is possibly that there is a misbelief among people under the age of 30 that cannabis is a benign substance.[19] Cannabis users may falsely assume that cannabis cannot cause a dependency or result in symptoms after discontinuing use.[52]
Despite the clear presence of nicotine in e-cigarettes, adolescents often do not recognize this fact, potentially fueling misperceptions about the health risks and addictive potential of e-cigarettes.[34] Adolescents perceive that e-cigarettes with flavors are less harmful than those with tobacco flavors.[34] A 2022 review states, "many adolescents believe that e-cigarettes do not contain nicotine, that the vapour contains only water, and that the products are safe with minimal health hazards. Similarly, many adolescents believe vaped or edible cannabis confers few health risks and is safer than combustible cannabis."[153] In England in 2018, numerous practitioners indicated they were uncertain about the safety and long-term effects of e-cigarette use.[87] Nearly 70% of females in the US think that cannabis use during pregnancy is harmless.[156]
A 2018 study reported that young adults perceived combustible (e.g., smoked, via a joint or pipe) cannabis as more harmful than vaporized cannabis; however, chemicals (e.g., butane) used make cannabis concentrates were thought to be a source of harm.[66] Another study reported that most participants perceived using e-cigarettes to vape cannabis to be just as harmful or more harmful than joint use.[66] Studies also reported uncertainty about the safety and harms of cannabis vaping compared to other forms of use.[66] One 2020 study reported that youth and young adult cannabis vapers had lower odds of perceiving harm from daily cannabis use in any form, when compared to never cannabis users.[66]
A 2015 qualitative content analysis of over 40,000 cannabis-related tweets found that cannabis was characterized as being substantially less harmful than conventional drugs for a variety of conditions such as sleep disorders, generalized anxiety, depression, and cancer.[56] Less than 1% of the tweets indicated any concern about cannabis use, and 43% of them were anecdotes and personal stories.[56] A 2020 analysis of vaping-related conversations found health discussions specifically on vape-administered cannabidiol as a treatment for COVID-19.[56] Although the investigations showed that discussions were mostly very positive toward cannabis as medicine, some of them noted negative consequences of cannabis use.[56] A 2018 quantitative analysis of 400,000 Reddit discussions about smoking, vaping, edibles, dabbing, and butane hash oil concentrate use found fewer adverse event mentions related to new modes of use. The most frequently mentioned adverse effects were anxiety-related, linked to smoking, edibles, and butane hash oil, and "cough" mentions related to vaping and dabbing.[56]
History

Norman Jacobson coined the term vaping, referring to a device for the purposes of quitting smoking in 1980.[7] The Oxford Dictionaries' 2014 word of the year was "vape".[205] Cannabis flower vaping can be traced back in the literature to 2001.[206] In 1963,[207] vaping was first invented by Pennsylvanian Herbert Gilbert who was a cigarette smoker.[20] His device was battery-powered and was used to inhale a liquid.[20] Hon Lik is credited with inventing the modern e-cigarette in 2003.[7] However, designs for a device to aerosolize nicotine may be traced back to the early 1960s, with the development of British American Tobacco's Project Ariel.[34] Despite two patents, Project Ariel never made it to the market; this was perhaps because the design was imperfect, and perhaps because—despite the science linking smoking with cancer—cigarette smoking was still immensely popular and unregulated.[34] As early as 1959, tobacco company research recognized (though not publicly acknowledged) nicotine's addictive nature and, therefore, the importance of nicotine in maintaining a customer base.[34]
By means of direct acquisitions, purchases, and takeovers, the mainstream tobacco industry had entered the e-cigarette market.[2] Meanwhile, e-cigarette and e-liquid technologies developed by small and innovative high-tech firms had evolved very quickly.[2] One challenge was to improve the performance and rate of nicotine delivery to the body.[2] With this goal, Pax Labs has substituted nicotine salts for free-base nicotine in an e-liquid and has developed a product called Juul.[2] The product is said to provide a blood nicotine absorption profile approaching that observed after regular tobacco cigarette smoking, unlike most e-cigarettes that were on the market in 2015.[2] By 2018, the popularity of Juul had led to a flood of other pod mod devices hitting the market.[208] There has been a proliferation of pod-based products with high nicotine concentration, triggered by Juul's financial success.[209] The majority of leading e-cigarette brands are owned by mainstream tobacco companies.[210]
Although the Trump administration originally announced a plan on September 11, 2019 to ban all flavored e-cigarettes from the US market,[211] the revised US FDA regulations, formulated under the Trump administration, did not include disposables.[212] This provoked numerous underage minors to shift from using Juul to using other flavored products.[212] At one point a niche market, disposable vapes accounted for 40% of the retail vaping marketplace in the US in 2022.[212] In 2023, Elf Bars became the most prevalent disposable vaping product worldwide.[38]




Cannabis is a genus of plants in the family Cannabaceae that has three common species: Cannabis sativa, Cannabis indica, and Cannabis ruderalis.[213] Natural compounds of the cannabis plant are referred to as phytocannabinoids to differentiate them from the synthetic cannabinoids and endocannabinoids.[213] The cannabis plant has been cultivated throughout the world since ancient civilizations and used for thousands of years for both medicinal and recreational applications.[31] Humans using cannabis can be traced back to around 11,700 years ago in Central Asia close to the Altai Mountains.[214] The first recorded use of cannabis as a medicinal drug was recorded in 2737 B.C. by the Chinese emperor Shen Nung in the world's oldest pharmacopoeia, the pen-ts'ao ching, who documented its effectiveness in the treatment of pain associated with rheumatism, intestinal disorders, gout and malaria, among others.[134] Other ancient Chinese texts describe cannabis as a hallucinogen in the context of shamanism, which was widespread in regions of Central and Western Asia, as well as India, leading to an increase in cannabis use in those regions.[134] Cannabis sativa is a flowering plant indigenous to eastern Asia but now is cultivated throughout the world due to its widespread industrial uses.[21] While cannabis has over a 100 active ingredients, most attention is drawn toward two main ingredients: THC and cannabidiol.[21] After other sedative and analgesic medications became available (e.g., aspirin), cannabis was displaced as a treatment option for a variety of medical conditions.[215] Elucidating the structure of THC in 1964 led to the development of THC analogues with similar activity, and this discovery also led to an increase in the production of synthetic cannabinoids.[49]
The psychoactive compound THC in cannabis creates a psychogenic effect.[31] It can be consumed through the respiratory tract and digestive tract through inhaling and oral ingesting.[31] In contrast, cannabidiol, another component derived from cannabis, is a non-psychoactive cannabinoid that has gained popularity for its medicinal values and as a supplement.[31] Because it is non-psychoactive, it does not produce the characteristic "high" associated with cannabis use.[216] Cannabidiol can also be derived from hemp.[32] This also includes cannabigerol and cannabichromene along with other non-cannabinoid compounds.[217] Cannabis contains significantly more THC than hemp, while hemp has more cannabidiol.[32] There have been remarkable increases in the average THC content percentage of cannabis (from 3% in the 1980s to 4% in 1995 to about 12% in 2012–2014) as well as hashish and hash oil.[48] These remarkable increases, in recent decades leading up to 2021, were probably due to selective breeding.[48] Cannabis oil in the form of butane honey oil, shatter, wax, or crumble can contain as high as 75% delta-9-THC whereas herb or resin contains from 5 to 20% delta-9-THC.[1]
Vaping devices were originally intended to provide nicotine as an alternative to traditional cigarettes.[9] However, they are now commonly used to provide psychoactive drugs, which includes cannabis and its derivatives.[9] Around the beginning of the 1990s, vaping became a new modality to use cannabis for recreational and medicinal purposes.[20] The original tabletop devices to aerosolize cannabinoids, called volcanoes or dab rigs, were bulky and heavy, and were not easy to use and were not discreet.[7] Grenco Science and Pax Labs introduced THC-based e-cigarettes which gave users an easy and discreet way to obtain THC.[7] The founder of Grenco Science,[7] Chris Folkerts,[218] purportedly engineered an e-cigarette specifically for delta-9-THC concentrates and e-liquids after not getting the expected delta-9-THC euphoric effect when he used an e-cigarette that contained delta-9-THC.[7] THC vape products include G Pen Micro+ Vaporizer, Utoya 1-Gram D8 THCP Vape, Boulder Viridian Vape Pod Starter Kit, Hypnos Zero Concentrate, Smok Morph 2 Starter Kit, Groove Cara Pen, and Innokin Endura Apex Vape Pen Kit.[219]
Sales of tobacco in Canada and the US have declined, while the cannabis industry has been characterized as a significant opportunity for mainstream tobacco companies.[220] Mainstream tobacco companies are making an effort to expand their product range not just by investing in alternatives to traditional cigarettes such as IQOS, which is owned by Philip Morris International, but also by offering new products like cannabis products to their customers.[221] Mainstream tobacco companies are considering investing or have invested in the cannabis industry during the past few years leading up to 2023.[222] Mainstream tobacco companies have also invested at the inception of cannabis space.[220] For instance, Altria spent $2.4 billion to obtain a 45% equity stake in Cronos, a cannabis company based in Canada.[220] Meanwhile, British American Tobacco obtained close to a 20% stake in Organigram, a cannabis company located in Canada.[220] In 2019, Imperial Brands invested $123 million for a 19.9% ownership in the Vancouver cannabis company, Auxly Cannabis.[223] The additional funds may help with Auxly Cannabis' intent of introducing later-generation cannabis vaping devices for the Canadian market.[223] In 2022, British American Tobacco invested £48.2 million ($57.4 million[224]) to acquire approximately a 19.99% share of Charlotte's Web,[225] which is a company that sells products that contain hemp extract.[224]
Lack of US federal policies overseeing the cannabis industry and different state-to-state policies has caused inferior quality products to penetrate the market.[7] There has been an emergence of a multitude of unregulated, adulterated cannabidiol products.[7] This includes synthetic cannabinoids, and various pharmacologically active chemicals, such as nuciferine and dextromethorphan.[7] Cannabis products such as dried cannabis flower that can be vaporized are sold at cannabis dispensaries and are unregulated by the US FDA.[226] The legalizing of cannabis for recreational and medical purposes in numerous states in the US has resulted in a thriving cannabis industry.[30]
Society and culture

Youth often see content on cannabis vaping from non-credible internet sources and across social media.[25] The increased mentioning of THC, CBD, or synthetic cannabinoids in online vaping posts went up from 14.5% in 2015 to 24.6% in 2019.[7] A 2017 Twitter analysis found that tweets on "social image and ENDS use" jumped from 21% in 2012 to 37% in 2015.[27]
Social media and the internet are used by the public to seek and share information about the medicinal use of cannabis.[56] People trying new formulations or experimenting with new modes of use found advice from other users rather than health professionals, and these sources were often found on the web.[56] Previous studies have found that consumers more frequently use the internet as their first source of information and consider the collective wisdom found on social media as a credible and accessible source of information.[56] Other studies have indicated that the growth in web-based cannabis resources is often accompanied by a lack of balanced information such as promotional articles, which purport to be scientific.[56] These resources have been shown to contain misleading information regarding the medical effects of cannabis.[56] Instead of learning about medicinal cannabis through structured training programs, physicians are obtaining fragmented knowledge about cannabis from fellow physicians, medical journals, news media, and even from their own patients.[56]
Lucy Popova, assistant professor at the School of Public Health at Georgia State University, was conducting research funded by the National Institutes of Health in 2020 that identified worrisome trends seen in popular YouTube vaping videos, like how to modify or "hack" a pre-packaged vape to include other substances or more cannabis or nicotine.[227] Social bots have been found to market unsubstantiated health claims on social media platforms and to spread low-credibility information.[56] A 2019 of data collected on cannabis-related tweets found 14.5% of the posts were generated by bots, with health and medical claims being the second most prevalent subject.[56] The emergence of a "new youth culture of vaping" could weaken the efficiency of anti-smoking campaigns and measures.[2] Further, vaping cannabis extracts could attract many young people and thwart cannabis use prevention efforts.[2] A 2020 cross-sectional analysis regarding tweets on social media on various cannabis networks found deliberate misinformation indicating that the consumption of cannabis is a therapy for COVID-19.[69]
A very large number of websites provide instructions on how to prepare cannabis-derived liquids for use in e-cigarette devices.[2] For example, a Google search in June 2015 of the terms "electronic cigarette" and "cannabis" obtained more than 250,000 results; searching for "electronic cigarette" and "BHO" obtained 72,000 results; and searching for ("electronic liquid" OR "e-liquid") AND "marijuana" obtained 420,000 results.[2] The same search, made with Google Scholar, provided a mere 384 results.[2] The majority of people who make extracts of THC oil at home figured out how to make them from information accessible online, and by viewing YouTube videos.[20]

There are dedicated magazines that publish buyer's guides for vape pens that review dozens of e-cigarette devices.[2] The dedicated magazines evaluate e-cigarettes that not only are able to vaporize wax or other hash-style concentrates, but also flower buds or even oil concentrates.[2] Many personal experiences about vaping crystal methamphetamine are discussed on the internet.[2] Similarly, the use of e-cigarettes as a means of administering numerous controlled substances is abundantly discussed on websites and forums.[2]
Cannabis vaping devices are available at cannabis dispensaries, smoke shops,[10] and vape shops.[26] Vape shops in the US are selling cannabiss or hemp-derived psychoactive delta-8-THC-containing vape cartridges since the passage of the 2018 Farm Bill.[228] Delta-8-THC is offered at convenience stores and gas stations.[6] Despite THC-based oils and waxes being illegal in most US states, they remain easily accessible.[98] Known as Weed day,[19] 4/20,[229] or 420,[230] April 20th is the day cannabis advocates celebrate cannabis in the US and across the world each year.[231]
Approximately in 2004 or earlier, websites and head shops started selling synthetic cannabinoids.[128] Synthetic cannabinoids, sold under various brand names such as Spice, are mostly available online, and in a handle of countries, specialty retailers sell them as legal substitutes to illegal drugs.[128] They can also be purchased in convenience stores and from individual drug dealers.[59] A person living in a country where synthetic cannabinoids are illegal to purchase can obtain them from another country.[128] Synthetic cannabinoids are sold over the internet, which enables very easy access to these compounds, and there is no age restrictions on purchasing them.[49]
Marketing
A typical marketing tactic is the promotion of so-called psychological health benefits related to use of a product.[232] THC-enriched cannabis products are being promoted and advertised as a way of alleviating psychological distress and mental issues in spite of scarcity of controlled clinical trials to verify such assertions.[232] The promotion of using THC-enriched cannabis for emotional health, irrespective of taking place in the farmwork of medical or recreational regulations, is a matter a great concern.[232] In regard to the therapeutic benefits of cannabis, cannabis retailers promote unfounded statements.[232] Cannabis retailers are also neglecting to disclose any warnings pertaining to health.[232] Cannabis vapor product producers are marketing specific devices to girls and women.[65]
Public interest in the use of cannabis for medical purposes is rising globally, as of 2023, which has resulted in some countries enacting legislation, leading to increased access to cannabis and cannabis-based products.[56] These legislative changes have generated public health concerns, as evidence for the efficacy and safety of cannabis is yet to be fully established, while cannabis products are increasingly being provided to consumers by a cannabis industry using sophisticated marketing strategies to influence public understanding of its benefits.[56] Medical cannabis companies, such Charlotte's Web, commonly cite University research to suggest that their products are safe and effective without supporting evidence.[233] This behavior may cause the public to misbelieve unverifiable claims about the safety and efficacy of cannabis-enriched products.[233] In 2022, Charlotte's Web announced a partnership with Major League Baseball.[234] The $30.5 million deal lasts for three years and makes them the "official CBD of Major League Baseball."[235]
The US FDA is aware that unapproved cannabis or cannabis-derived products are being used for the treatment of a number of medical conditions including, for example, AIDS wasting, epilepsy, neuropathic pain, spasticity associated with multiple sclerosis, and cancer and chemotherapy-induced nausea.[236]
To date, the US FDA has not approved a marketing application for cannabis for the treatment of any disease or condition and thus has not determined that cannabis is safe and effective for any particular disease or condition.[236] The agency has, however, approved one cannabis-derived and three cannabis-related drug products.[236]
Cannabidiol products are also being marketed for pets and other animals.[103] The US FDA has not approved cannabidiol for any use in animals and the concerns regarding cannabidiol products with unproven medical claims and of unknown quality equally apply to cannabidiol products marketed for animals.[103] The US FDA recommends pet owners talk with their veterinarians about appropriate treatment options for their pets.[103]
Synthetic cannabinoids are promoted as incense products, meditation potpourris, bath additives, or air fresheners.[128] They are also portrayed as natural herbs or a harmless incense blend.[128] They may be sold as incense, potpourri, or herbal supplements.[237] These drugs may be labeled as "not for human consumption" to circumvent drug control laws.[96]
Lobbying efforts
Mainstream tobacco companies are lobbying for pro-cannabis regulations in the US.[222] Altria has lobbied in Verginia[238] and the US Congress for pro-cannabis regulations.[239] The cannabis industry is lobbying in Canada[240] and the US.[241]
Legality and regulations
Frequently referring to the environmental cost of electronic waste, more governments are passing laws to prevent disposable vapes like Elf Bar from being used.[38] The available evidence generally fails to support a particular type of regulation for curbing youth vaping.[243] However, according to a 2024 review, introducing a variety of regulations may help with curbing youth vaping.[243] A 2022 review states, the prohibition of e-cigarettes vaping in the college can be effective in reducing e-cigarettes vaping.[79] The same 2022 review also states, banning the sale of e-cigarettes to people under 18 years may help reduce e-cigarettes vaping rates among adolescents and school students.[79]
In 2021, the United Nations Office on Drugs and Crime removed cannabis from Schedule IV, but it remains on the Schedule I list due to insufficient data on its effects.[60] A large number of countries have passed new cannabis laws, such as decriminalizing cannabis possession as well as legalizing cannabis for medical and recreational use;[244] however, using cannabis recreationally is still illegal in most countries, as of 2021.[62] Canada legalized cannabis for non-medical use in 2018.[8] Cannabis is categorized as a Schedule I drug by the US FDA[245] with no recognized medical use.[115]
As of May 2021, a total of 36 states and 4 US territories allows for medical use of cannabis products and 18 states, 2 US territories, and the District of Columbia have legalized adult-use (recreational) cannabis.[66] Of note, two states (South Dakota and Mississippi) passed ballot initiatives by popular vote to legalize cannabis use (medical and adult-use in South Dakota; medical-only in Mississippi) in 2020; however, these ballot initiatives were overturned by the State Supreme Court in each state.[66] Most states set no legal age restrictions for medical cannabis, though all require a prescription from a credentialed medical professional and for minors to use under the supervision of their guardian.[66] Legal age for purchase of adult-use cannabis is 21 years of age in all legalized states, territories, and the District of Columbia.[66] The use, sale, and possession of cannabis above 0.3% THC is a federal crime in the US.[67]
Cannabis is semi-legal in several countries.[65] For example, Argentina, South Africa, and Mexico have identified punishment for possession of cannabis for personal consumption as unconstitutional; the Netherlands tolerates public consumption and sale of cannabis in licensed coffee-shops; and in Spain personal consumption and cultivation of cannabis is tolerated.[65] Cannabis for medical use is legal in South Africa.[246] It is unlawful to possess, supply, produce, import or export cannabis from the UK except under a Home Office license.[247] In the UK, it is also an offence to cultivate any plant of the genus Cannabis except under a Home Office license..[247] The medical use of cannabis became legal in the UK in 2018.[248]
There is a lack of regulations for cannabis extracts used in vaping devices.[20] As of 2021, regulations that apply to nicotine e-liquids do not apply to cannabidiol products..[101] This has resulted in concerns regarding the quality of cannabidiol vaping devices.[101] It is against US federal law to manufacture butane hash oil, and even in some states where adult use of cannabis is legal, like Colorado and California, it is illegal to make hash oil using flammable liquids.[161] In Colorado, state officials recommend alternate methods using nonflammable dry ice (CO2), ice water, or purchasing the product from a licensed cannabis retail store.[161] The legal limit of THC in cannabidiol-based products varies among countries, starting from 0% to as high as 2%.[101] The legal limit for THC can change.[101] For example, the European Parliament changed the legal limit for THC from 0.2% to 0.3% in 2020.[101] The legal limit for THC among various regions include Hong Kong at 0%, Argentina at 0.2%, Canada at 0.3%, Paraguay at 0.5%, Italy at 0.6%, Switzerland at 1%, and New Zealand at 2%.[101]
The majority of the legal cannabis regulations in the US are not backed by evidence or aligned with public health.[232] To address this issue, various publications have provided evidence-backed approaches for public health-focused legal cannabis legislation.[232]
Although federal and US state laws prohibit general categories of substances related to synthetic cannabinoids, manufacturers of synthetic cannabinoids keep selling new products with modifications of said ingredients and state on products "not for human consumption" to circumvent these laws.[67] Clandestine laboratories synthesize synthetic cannabinoids and circumvent legal barriers by falsely marketing them as incense or herbal products.[50] Internet vendors may at least temporarily sell designer drugs (such as synthetic cannabinoids often referred to as Spice) without adhering to legal statutes or facing legal consequences.[122]
Environmental impact

Environmental effects from improper e-waste disposal and recycling are increasing worldwide, as of 2023.[4] Electronic waste handling and disposal exposes people to highly toxic compounds, such as heavy metals.[4]
Cannabis product waste represents an emerging issue, as of 2019.[75] Cannabis product waste can include plastics, metals, electronic components, and batteries.[75] A garbology study of environmental contamination including cannabis product waste was conducted at 12 public high schools in Alameda, Contra Costa, Marin, and San Francisco counties in California.[75] At each school, researchers systematically scanned the student parking lots and exterior school perimeter areas once during July 2018–April 2019 to collect all e-cigarette product waste, combustible tobacco product waste, and cannabis product waste found on the ground.[75] 14 cannabis product waste items were found, including vaporizer pens, cartridges, and packaging from high-potency pineapple- and lemon-flavored cannabis oil concentrate vaporizer cartridges.[75]
Interest in growing cannabis for medical and recreational purposes has increased worldwide.[31] Cannabis is a water- and nutrient-intensive crop.[31] The water demand for cannabis growing far exceeds the water needs of many commodity crops.[31] For example, cannabis in a growing season needs twice as much as the water required by maize, soybean, and wheat.[31] The high water demand presses the need for water sources.[31] Water diversion is a common practice, which removes or transfers the water from one watershed to another to meet irrigation requirements.[31] While the water diversion alleviates the water shortage problem for cannabis cultivation, it also presents new challenges. A 2015 study quantitatively showed that surface water diversions for irrigation led to reduced flows and dewatered streams.[31] Water demand and usage for cannabis continues to be a major concern.[31]
There is limited data on the impact of cannabis cultivation on water quality worldwide.[31] Water diversion and water pollution affect the water ecosystem.[31] The high demand for water due to cannabis cultivation in watersheds affects wildlife such as fish and amphibians in a significant way since cannabis cultivation is widespread within the boundaries of the watersheds, where the downstream water houses populations of sensitive aquatic species.[31] The diminished flows may be notably detrimental to salmonid fishes since they need clean, cold water and suitable flow regimes.[31] As the reduced streamflow has a strong positive correlation with increased water temperature, indirectly resulting in reduced growth rates in salmonids, lowered dissolved oxygen, increased predation risk, and increased susceptibility to disease.[31] It has been reported that there are 80%–116% increases in cannabis cultivation sites near high-quality habitats for threatened and endangered salmonid fish species.[31]
Cannabis cultivation, especially illegal cultivation, may deteriorate water quality.[31] Studies have suggested the considerable demands of nutrition such as nitrogen, phosphorous, and potassium for cannabis growth.[31] Based on a 2019 California survey, more than 30 different soil amendments and foliar nutrient sprays were used to maintain nutrition and fertility.[31] The applied pesticides (including herbicides, insecticides, fungicides, nematicides, and rodenticides), due to routine pest and disease controls, make their way into the water without restriction and therefore posing significant risks to the water environment.[31] The transport and fate of the applied fertilizers and pesticides vary.[31] For example, nitrogen and pesticides can get into runoff or leach into groundwater due to rainfall or excessive irrigation.[31] If the polluted water continues to be used, it would add contaminants into soil, surface water, and groundwater.[31] These chemicals may threaten humans and crops through the food chain.[31] The other major irrigated crops can also be significantly impacted since the placement of crops is subject to the environmental safety of runoff, groundwater contamination, and the poisoning of nearby bodies of water.[31] However, without the ability to sample water quality and assess the extent to which chemical inputs are entering adjacent water bodies, the ability to link cultivation practices to water pollution is greatly limited.[31] Few environmental clean-up and remediation efforts in the polluted watersheds are accessible due to a lack of resources and staff in state or US federal agencies.[31]
The plant requires increased levels of nitrogen, phosphorus, and potassium for optimal growth, but little research has been done on how this affects water quality globally.[60] The use of pesticides, such as herbicides, insecticides, fungicides, nematicides, and rodenticides, can also contribute to water contamination when not properly checked, posing a threat to the environment.[60] Illegal cannabis cultivation and improper operation may increase water pollution issues.[31] Studies on cannabis' physiological properties may provide guidance to determine water demand.[31] Identifying and applying best management practices, such as precision irrigation and enhanced climate control, may be helpful ways to minimize the environmental impacts on water.[31] Energy consumptions mainly come from the equipment operation of the indoor cultivations such as lighting, HVAC, and dehumidification.[31]
Outdoor cannabis cultivation greatly impacts water diversion, is linked to land clearing, contributes to chemical pollution, and represents a pervasive danger to wildlife.[249] Carbon footprint can be calculated both indoors and outdoors based on energy consumption.[31] Quantitatively accounting for the energy assumption across operations at scales is the key to better estimating the carbon footprint.[31] Techniques such as life cycle energy assessment and life cycle carbon emissions assessment would offer informative guidance to reduce the environmental impacts.[31] Few studies have focused on the impacts of cannabis cultivation on air quality.[31] Evidence has emerged that biologically generated volatile organic compounds (BVOCs) and fertilization may contribute to outdoor air quality issues.[31] Cannabis cultivation directly contributes to soil erosion.[31] The cutting down of trees and clearing of forests for cannabis cultivation exacerbates soil erosion.[60] However, durable greenhouses can help prevent soil erosion by avoiding the need for massive clearings that expose soil to erosion.[60] Cannabis also has a strong ability to absorb and store heavy metals in the soil.[31]
Cannabis waste may contain branches, leaves, and bush.[249] Cannabis biomass waste management utilizes disposal techniques such as incineration, aerobic or anaerobic digestion, composting, and shredding, that are environmentally unsustainable long-term.[249] Cannabis waste significantly contributes to rising global temperatures because of both incinerating it locally and disposing of it away from the local area.[249]
Although cannabis can be grown outdoors in many regions of the world, sizeable commercial cultivation can also occur indoors or in greenhouses.[31] Indoor air pollutants caused by indoor cannabis cultivation, i.e., BVOCs emission, mold, pesticide, and chemicals pose risks to one's health.[31] More than 350 distinct pesticides may be utilized on cannabis.[107] The American Herbal Pharmacopoeia created a list of the potential top 16 pesticides and potential top three plant growth regulators.[107] This compilation does not pertain to each individual country.[107] There may be differences in the availability of each pesticide in any given country and there may be different regulations on pesticides in any given country.[107] Several of the pesticides detected in the cannabis materials analyzed that were intended for consumption are categorized as moderately unsafe by the World Health Organization.[107] The energy use of indoor cannabis cultivation arises from a range of equipment, falling into two major categories: lighting and precise microclimate control.[31] For the cannabis plants to thrive and therefore make the growers a profit, several energy-intensive tools are regularly utilized.[31]
Other names
Electronic cigarettes
Electronic cigarettes are variously known as electronic-cigarettes,[250] e-cigarettes,[39] convection vaporisers,[108] cannabis vaporisers,[108] cannabis vaporisation devices,[108] vaporisation devices,[108] desktop vaporisers,[108] portable vaporisers,[108] vaporisers,[108] dried flower vaporisers,[108] personal aerosolizers,[27] electronic vaporizers,[251] table vaporizers,[2] marijuana leaf vaporizers,[252] marijuana vaporizers,[67] vaporizers,[203] vaping products,[133] disposable e-cigarettes,[38] disposable vapes,[38] disposable electronic vaping devices,[6] e-devices,[2] cannabis e-cigarettes (CECs),[206] electronic cannabis systems,[27] cannabidiol vapes,[101] THC vape pens,[40] vape pens,[27] dab pens,[32] oil pens,[135] weed pens,[40] or e-joints.[40] Youth sometimes call them e-cigs, e-hookahs, mods, nic sticks, or vape pens.[253] They also may refer to them by their brand names.[253]
Vaping
Other names for the term vaping include aerosolizing, cloud chasing, vapo, vaporisin,[7] electronic smoking,[254] e-cigarette smoking,[165] and e-smoking.[255] Vaping cannabinoids is also called dabbin, ride the mist, skitzin, vapindaganja, cold boxing, tankinista, tootle puffer, vooping, and vaples.[7] Cannabis vaping[5] is variously known as marijuana vaping,[256] or "cannavaping".[5]
E-liquids
E-liquids are also often known as cannabis oils or vape oils.[108]
Cannabis
Cannabis is variously known as marijuana, weed, pot, ganja,[257] Ganja, hash, BC Bud, smoke, doobs,[53] herb, grass, bud, Mary Jane, and many other names.[258]
Recreational cannabis
Recreational cannabis[259] is also known as recreational marijuana.[154]
Medical cannabis
Medical cannabis[110] is variously known as medical marijuana,[110] medicinal cannabis,[172] or medicinal marijuana.[154]
Tetrahydrocannabinol and cannabidiol
The abbreviation for tetrahydrocannabinol is "THC" and the abbreviation for cannabidiol is "CBD".[257]
Synthetic cannabinoids
Synthetic cannabinoids are variously known as AK-47 24-Karat Gold,[260] AK-47, Kush, Kronic,[59] K2,[261] K2 Summit, K2 Blonde, K2 Standard,[262] K-3,[263] 'K9, Spice, Youcatan, Chill, Black Mamba,[261] Smoke, Spice Gold, Banana Cream Nuke,[264] herbal incense, herbal smoking blends,[265] synthetic marijuana, herbal incense, potpourri, Phantom Wicked, Mr. Happy, Mad Monkey, Clown Loyal, Lava, Flame 2.0,[266] Cloud 9, Mojo,[49] Bliss, Blaze, Bombay Blue, Legal Weed, Scooby Snax, Red X Dawn,[267] RedX Dawn, Paradise, Demon, Black Magic, Spike, Mr. Nice Guy, Ninja, Zohai, Dream, Genie, Sence, Smoke, Skunk, Serenity, Yucatan, Fire, Crazy Clown,[268] Solar Flare, Genie PEP, Spice Fire "n" Ice, Zombie World, Bad-to-the-Bone, Dark Night, Earthquake, Berry Blend, The Moon, G-Force, Blueberry Haze, Dank Demon, Passion Smoke, Hawaiian Hybrid, Magma, Ninja, Ono Budz, Panama Red Ball, Puff Sativah, Herbal Smoke, Skunk Ultra, Chronic Voodoo, Spice Aroma,[262] King Krypto, Red Magic, Blueberry Medication, Super Skunk,[263] Spice Diamond, Arctic Spice, Silver, Scene, Yucatan Fire, Aroma, Lava Red, and other names.[128]
While ADB-FUBINACA was detected in samples of products labelled as Black Mamba, VaperFi,“Freeze, and Mojo, its AMB-FUBINACA analogue has been detected in products marketed under the name AK-47 Carat Gold, Train Wreck2 and Scooby Snax Limited Edition Blueberry Potpourri, which consist of mixtures of herbs ready to be used in vaporization devices, e-cigarettes, inhalers, or even orally ingested.[51] In addition, there are dozens of other street names for unspecific synthetic cannabinoid preparations, such as K2, K2XXX, barely legal, iBlaze, spice, herbal incense, Kush, and zombie, that contain one or more unidentified synthetic cannabinoids, including AMB-FUBINACA or ADB-FUBINACA.[51]
Related technologies
Philip Morris International planned to initially spend $120 million in 2023 to assist Syqe Medical in getting authorization from the US FDA for its cannabis-infused inhaler.[222] If the inhaler is cleared in clinical trials and gets FDA authorization, Philip Morris International would buy the remaining shares of Syqe Medical it does not own for $650 million.[222] Previously in 2019, Philip Morris International made an investment of $20 million in Syqe Medical.[269] This purchase would be finalized via its subsidiary, Vectura,[222] which offers inhalable medicines and devices[270] and was bought for $1.44 billion in 2021.[222]
Notes
- ↑ A 2018 review states, "The term 'vaping' is used both colloquially and in the literature to describe the through mouth inhalation of a vaporized product from a device that uses electrical power to heat the product to the point of vaporization. The product can refer to substances with desired inhalation effects such as nicotine dissolved in e-liquids (usually a mix of propylene glycol and glycerine); crushed plant material placed directly into the vaporizing device; concentrated extracts from plant materials in the form of thick waxes or oils either on their own or diluted in e-liquid; or substances directly dripped onto the hot coil to produce vapor."[3]
- ↑ While vitamin E acetate is strongly linked to this outbreak, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC or non-THC products, in some of the reported vaping-related lung injury cases.[13] There is likely more than one cause of the outbreak.[14] The majority of cases in Canada involving lung injuries do not seem to have been connected with the use of THC-infused products.[15] In 2019, some people diagnosed with a vaping-induced lung injury reported using only nicotine-containing products.[16] Nicotine e-cigarette use has been linked to the vaping-induced lung injury cases in a small subset of users.[17] In 2020, the first uptick in vaping-induced lung injury cases had occurred in Utah since the decline of 2019.[18] This research indicates the recurrent nature of the vaping-induced lung illness epidemic with new occurrences continuing to be reported.[18]
- ↑ Current use of e-cigarettes is defined as having vaped within the previous 30 days.[4]
- ↑ Synthetic cannabinoids are sprayed on natural harmless herbs with an aim to mimic the euphoric effect of cannabis.[49] They are sold under different brand names including Black mamba, spice, K2, and Bombay Blue.[49]
- ↑ During adolescence, the human brain undergoes substantial changes.[9] A 2015 study using female rats shows that high THC exposure during adolescence slows the development of the prefrontal cortex.[9]
- ↑ Heavy cannabis use is identified as using cannabis at a minimum of 20 days in a month.[153]
- ↑ The purpose of using cannabis recreationally is different than when it is used for medical reasons.[171] The term medical cannabis refers to using the whole, unprocessed cannabis plant or its basic extracts to treat symptoms of illness and other conditions.[168] Medical cannabis has received increased research attention over the recent years leading up to 2020 due to loosening global regulatory changes.[172]
- ↑ A 2020 review states that "The wide distribution of cases across the United States and reports of similar case presentations in other parts of the world support the possibility that other presentations of e-cigarette- or vaping product-associated lung injury existed prior to this outbreak, and vaping-associated lung injuries have been under-recognized by health care workers."[175]
- ↑ A 2019 review states that "similar cases have been found in the UK and Japan, suggesting that this has the potential to be a more widespread phenomenon, although the country to country variations in frequency remain to be determined."[176]
- ↑ Synthetic cannabinoids mimic the effects of delta-9-tetrahydrocannabinol (THC), but they are reported to have a higher potency.[45] Different groups exist within synthetic cannabinoids, and substances are categorized based on their chemical structure.[45] Further, illegal synthetic cannabinoids differ from that of cannabis or legal synthetic cannabinoids like dronabinol and nabilone.[67]
Further reading
- "What We Know About Marijuana". Centers for Disease Control and Prevention. 9 September 2021.
- "Marijuana and Public Health". Centers for Disease Control and Prevention. 21 September 2023.
- "Health Effects of Marijuana". Centers for Disease Control and Prevention. 2 June 2021.
- "Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products". Centers for Disease Control and Prevention. 3 August 2021.
- "Learn About Marijuana Risks". Drug Abuse Warning Network. Substance Abuse and Mental Health Services Administration. 28 February 2023.
- "Lung Illnesses Associated with Use of Vaping Products". United States Food and Drug Administration. 13 April 2020.
- "FDA and Cannabis: Research and Drug Approval Process". United States Food and Drug Administration. 27 February 2023.
- "Let's Talk Cannabis". California Tobacco Control Program. California Department of Public Health. 18 September 2019.
- Corum, Jonathan (13 January 2020). "Vaping Illness Tracker 2: 2,602 Cases and 59 Deaths". The New York Times.
- "Cannabis". TobaccoTactics. University of Bath. 31 March 2023.
References
- ↑ 1.0 1.1 The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies Press. 31 March 2017. doi:10.17226/24625. PMID 28182367.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 2.29 2.30 2.31 2.32 2.33 2.34 2.35 2.36 2.37 2.38 2.39 2.40 2.41 2.42 2.43 2.44 2.45 2.46 2.47 Giroud, Christian; de Cesare, Mariangela; Berthet, Aurélie; Varlet, Vincent; Concha-Lozano, Nicolas; Favrat, Bernard (2015). "E-Cigarettes: A Review of New Trends in Cannabis Use". International Journal of Environmental Research and Public Health. 12 (8): 9988–10008. doi:10.3390/ijerph120809988. ISSN 1660-4601. PMC 4555324. PMID 26308021.
 This article incorporates text by Christian Giroud, Mariangela de Cesare, Aurélie Berthet, Vincent Varlet, Nicolas Concha-Lozano, and Bernard Favrat available under the CC BY 4.0 license.
This article incorporates text by Christian Giroud, Mariangela de Cesare, Aurélie Berthet, Vincent Varlet, Nicolas Concha-Lozano, and Bernard Favrat available under the CC BY 4.0 license.
- ↑ 3.0 3.1 Breitbarth, Andreas K.; Morgan, Jody; Jones, Alison L. (November 2018). "E-cigarettes—An unintended illicit drug delivery system". Drug and Alcohol Dependence. 192: 98–111. doi:10.1016/j.drugalcdep.2018.07.031. ISSN 0376-8716. PMID 30245461.
- ↑ 4.000 4.001 4.002 4.003 4.004 4.005 4.006 4.007 4.008 4.009 4.010 4.011 4.012 4.013 4.014 4.015 4.016 4.017 4.018 4.019 4.020 4.021 4.022 4.023 4.024 4.025 4.026 4.027 4.028 4.029 4.030 4.031 4.032 4.033 4.034 4.035 4.036 4.037 4.038 4.039 4.040 4.041 4.042 4.043 4.044 4.045 4.046 4.047 4.048 4.049 4.050 4.051 4.052 4.053 4.054 4.055 4.056 4.057 4.058 4.059 4.060 4.061 4.062 4.063 4.064 4.065 4.066 4.067 4.068 4.069 4.070 4.071 4.072 4.073 4.074 4.075 4.076 4.077 4.078 4.079 4.080 4.081 4.082 4.083 4.084 4.085 4.086 4.087 4.088 4.089 4.090 4.091 4.092 4.093 4.094 4.095 4.096 4.097 4.098 4.099 4.100 4.101 4.102 4.103 4.104 4.105 4.106 4.107 4.108 4.109 4.110 4.111 4.112 4.113 4.114 4.115 4.116 4.117 4.118 4.119 4.120 4.121 Shehata, Shaimaa A.; Toraih, Eman A.; Ismail, Ezzat A.; Hagras, Abeer M.; Elmorsy, Ekramy; Fawzy, Manal S. (12 September 2023). "Vaping, Environmental Toxicants Exposure, and Lung Cancer Risk". Cancers. 15 (18): 4525. doi:10.3390/cancers15184525. PMC 10526315. PMID 37760496.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Shaimaa A Shehata, Eman A Toraih, Ezzat A Ismail, Abeer M Hagras, Ekramy Elmorsy, and Manal S Fawzy available under the CC BY 4.0 license.
This article incorporates text by Shaimaa A Shehata, Eman A Toraih, Ezzat A Ismail, Abeer M Hagras, Ekramy Elmorsy, and Manal S Fawzy available under the CC BY 4.0 license.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Traboulsi, Hussein; Cherian, Mathew; Abou Rjeili, Mira; Preteroti, Matthew; Bourbeau, Jean; Smith, Benjamin M.; Eidelman, David H.; Baglole, Carolyn J. (15 May 2020). "Inhalation Toxicology of Vaping Products and Implications for Pulmonary Health". International Journal of Molecular Sciences. 21 (10): 3495. doi:10.3390/ijms21103495. ISSN 1422-0067. PMC 7278963. PMID 32429092.
 This article incorporates text by Hussein Traboulsi, Mathew Cherian, Mira Abou Rjeili, Matthew Preteroti, Jean Bourbeau, Benjamin M. Smith, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
This article incorporates text by Hussein Traboulsi, Mathew Cherian, Mira Abou Rjeili, Matthew Preteroti, Jean Bourbeau, Benjamin M. Smith, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 6.19 6.20 6.21 6.22 6.23 6.24 Sharma, Pravesh; Mathews, Doug B; Nguyen, Quang Anh; Rossmann, Gillian L; A Patten, Christi; Hammond, Christopher J (January 2023). "Old Dog, New Tricks: A Review of Identifying and Addressing Youth Cannabis Vaping in the Pediatric Clinical Setting". Clinical Medicine Insights: Pediatrics. 17. doi:10.1177/11795565231162297. PMC 10041590. PMID 36993933.
{{cite journal}}: Check|pmc=value (help) - ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 7.15 7.16 7.17 7.18 7.19 7.20 Holt, Alaina K.; Poklis, Justin L.; Peace, Michelle R. (February 2023). "The history, evolution, and practice of cannabis and E-cigarette industries highlight necessary public health and public safety considerations". Journal of Safety Research. 84: 192–203. doi:10.1016/j.jsr.2022.10.019. PMID 36868647.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Lim, Carmen C. W.; Chan, Gary C. K.; Wadsworth, Elle; Stjepanović, Daniel; Chiu, Vivian; Chung, Jack Y. C.; Sun, Tianze; Connor, Jason; Leung, Janni; Gartner, Coral; Hall, Wayne; Hammond, David (3 November 2022). "Trends and Socio-Demographic Differences of Cannabis Vaping in the USA and Canada". International Journal of Environmental Research and Public Health. 19 (21): 14394. doi:10.3390/ijerph192114394. PMC 9659122. PMID 36361272.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Carmen C. W. Lim, Gary C. K. Chan, Elle Wadsworth, Daniel Stjepanović, Vivian Chiu, Jack Y. C. Chung, Tianze Sun, Jason Connor, Janni Leung, Coral Gartner, Wayne Hall, and David Hammond available under the CC BY 4.0 license.
This article incorporates text by Carmen C. W. Lim, Gary C. K. Chan, Elle Wadsworth, Daniel Stjepanović, Vivian Chiu, Jack Y. C. Chung, Tianze Sun, Jason Connor, Janni Leung, Coral Gartner, Wayne Hall, and David Hammond available under the CC BY 4.0 license.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 9.15 9.16 9.17 Lim, Carmen C. W.; Sun, Tianze; Leung, Janni; Chung, Jack Y. C.; Gartner, Coral; Connor, Jason; Hall, Wayne; Chiu, Vivian; Stjepanović, Daniel; Chan, Gary C. K. (1 January 2022). "Prevalence of Adolescent Cannabis Vaping: A Systematic Review and Meta-analysis of US and Canadian Studies". JAMA Pediatrics. 176 (1): 42. doi:10.1001/jamapediatrics.2021.4102. PMC 8546627. PMID 34694342.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 10.18 10.19 Ren, Michelle; Lotfipour, Shahrdad (20 August 2019). "Nicotine Gateway Effects on Adolescent Substance Use". Western Journal of Emergency Medicine. 20 (5): 696–709. doi:10.5811/westjem.2019.7.41661. PMC 6754186. PMID 31539325.
 This article incorporates text by Michelle Ren and Shahrdad Lotfipour available under the CC BY 4.0 license.
This article incorporates text by Michelle Ren and Shahrdad Lotfipour available under the CC BY 4.0 license.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 11.13 11.14 Weresa, Jolanta; Pędzińska-Betiuk, Anna; Mińczuk, Krzysztof; Malinowska, Barbara; Schlicker, Eberhard (28 March 2022). "Why Do Marijuana and Synthetic Cannabimimetics Induce Acute Myocardial Infarction in Healthy Young People?". Cells. 11 (7): 1142. doi:10.3390/cells11071142. PMC 8997492. PMID 35406706.
 This article incorporates text by Jolanta Weresa, Anna Pędzińska-Betiuk, Krzysztof Mińczuk, Barbara Malinowska, and Eberhard Schlickero available under the CC BY 4.0 license.
This article incorporates text by Jolanta Weresa, Anna Pędzińska-Betiuk, Krzysztof Mińczuk, Barbara Malinowska, and Eberhard Schlickero available under the CC BY 4.0 license.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 Hofmann, Joseph J.; Poulos, Victoria C.; Zhou, Jiahai; Sharma, Maksym; Parraga, Grace; McIntosh, Marrissa J. (24 January 2024). "Review of quantitative and functional lung imaging evidence of vaping-related lung injury". Frontiers in Medicine. 11. doi:10.3389/fmed.2024.1285361. PMC 10847544. PMID 38327710.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Joseph J. Hofmann, Victoria C. Poulos, Jiahai Zhou, Maksym Sharma, Grace Parraga, and Marrissa J. McIntosh available under the CC BY 4.0 license.
This article incorporates text by Joseph J. Hofmann, Victoria C. Poulos, Jiahai Zhou, Maksym Sharma, Grace Parraga, and Marrissa J. McIntosh available under the CC BY 4.0 license.
- ↑ "Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products". Centers for Disease Control and Prevention. 3 August 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ King, Brian A.; Jones, Christopher M.; Baldwin, Grant T.; Briss, Peter A. (2020). "The EVALI and Youth Vaping Epidemics — Implications for Public Health". New England Journal of Medicine. doi:10.1056/NEJMp1916171. ISSN 0028-4793. PMID 31951683.
- ↑ "Vaping-associated lung illness". Public Health Agency of Canada. 20 August 2020.
- ↑ Ghinai, Isaac; Navon, Livia; Gunn, Jayleen K.L.; Duca, Lindsey M.; Brister, Sarah; Love, Sarah; Brink, Rachel; Fajardo, Geroncio; Johnson, Jona; Saathoff-Huber, Lori; King, Brian A.; Jones, Christopher M.; Krishnasamy, Vikram P.; Layden, Jennifer E. (24 January 2020). "Characteristics of Persons Who Report Using Only Nicotine-Containing Products Among Interviewed Patients with E-cigarette, or Vaping, Product Use–Associated Lung Injury — Illinois, August–December 2019". MMWR. Morbidity and Mortality Weekly Report. 69 (3): 84–89. doi:10.15585/mmwr.mm6903e1. PMC 7367041. PMID 31971930.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 Marrocco, Antonella; Singh, Dilpreet; Christiani, David C.; Demokritou, Philip (16 March 2022). "E-cigarette vaping associated acute lung injury (EVALI): state of science and future research needs". Critical Reviews in Toxicology. 52 (3): 188–220. doi:10.1080/10408444.2022.2082918. PMC 9716650. PMID 35822508.
{{cite journal}}: Check|pmc=value (help) - ↑ 18.0 18.1 Smith, Maxwell L.; Gotway, Michael B.; Crotty Alexander, Laura E.; Hariri, Lida P. (2020). "Vaping-related lung injury". Virchows Archiv. 478 (1): 81–88. doi:10.1007/s00428-020-02943-0. ISSN 0945-6317. PMC 7590536. PMID 33106908.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 19.7 Ahmad, S; Hlaing, SW; Haris, M; Attar, N (April 2022). "Marijuana: cardiovascular effects and legal considerations. A clinical case-based review". The British journal of cardiology. 29 (2): 11. doi:10.5837/bjc.2022.011. PMC 9534111. PMID 36212793.
{{cite journal}}: Check|pmc=value (help) - ↑ 20.00 20.01 20.02 20.03 20.04 20.05 20.06 20.07 20.08 20.09 20.10 20.11 20.12 20.13 20.14 Laucks, P; Salzman, GA (March 2020). "The Dangers of Vaping". Missouri medicine. 117 (2): 159–164. PMC 7144697. PMID 32308243.
- ↑ 21.00 21.01 21.02 21.03 21.04 21.05 21.06 21.07 21.08 21.09 21.10 21.11 21.12 21.13 21.14 21.15 21.16 21.17 Adapa, Sreedhar; Gayam, Vijay; Konala, Venu Madhav; Annangi, Srinadh; Raju, Mina P.; Bezwada, Vishnu; McMillan, Christine; Dalal, Hussain; Mandal, Amrendra; Naramala, Srikanth (January 2020). "Cannabis Vaping–Induced Acute Pulmonary Toxicity: Case Series and Review of Literature". Journal of Investigative Medicine High Impact Case Reports. 8: 232470962094726. doi:10.1177/2324709620947267. PMC 7543135. PMID 32755249.
 This article incorporates text by Sreedhar Adapa, Vijay Gayam, Venu Madhav Konala, Srinadh Annangi, Mina P. Raju, Vishnu Bezwada, Christine McMillan, Hussain Dalal, Amrendra Mandal, and Srikanth Naramala available under the CC BY 4.0 license.
This article incorporates text by Sreedhar Adapa, Vijay Gayam, Venu Madhav Konala, Srinadh Annangi, Mina P. Raju, Vishnu Bezwada, Christine McMillan, Hussain Dalal, Amrendra Mandal, and Srikanth Naramala available under the CC BY 4.0 license.
- ↑ 22.0 22.1 22.2 Ford, Talitha C.; Hayley, Amie C.; Downey, Luke A.; Parrott, Andrew C. (11 June 2018). "Cannabis: An Overview of its Adverse Acute and Chronic Effects and its Implications". Current Drug Abuse Reviews. 10 (1): 6–18. doi:10.2174/1874473710666170712113042. PMID 28707583.
- ↑ 23.00 23.01 23.02 23.03 23.04 23.05 23.06 23.07 23.08 23.09 23.10 23.11 23.12 23.13 23.14 23.15 23.16 23.17 23.18 Zehra, Amna; Burns, Jamie; Liu, Christopher Kure; Manza, Peter; Wiers, Corinde E.; Volkow, Nora D.; Wang, Gene-Jack (December 2018). "Cannabis Addiction and the Brain: a Review". Journal of Neuroimmune Pharmacology. 13 (4): 438–452. doi:10.1007/s11481-018-9782-9. PMC 6223748. PMID 29556883.
 This article incorporates text by Amna Zehra, Jamie Burns, Christopher Kure Liu, Peter Manza, Corinde E. Wiers, Nora D. Volkow, and Gene-Jack Wang available under the CC BY 4.0 license.
This article incorporates text by Amna Zehra, Jamie Burns, Christopher Kure Liu, Peter Manza, Corinde E. Wiers, Nora D. Volkow, and Gene-Jack Wang available under the CC BY 4.0 license.
- ↑ 24.0 24.1 24.2 24.3 24.4 24.5 24.6 24.7 Copeland, J (December 2016). "Cannabis use and its associated disorders: Clinical care". Australian family physician. 45 (12): 874–877. PMID 27903036.
- ↑ 25.00 25.01 25.02 25.03 25.04 25.05 25.06 25.07 25.08 25.09 25.10 25.11 25.12 25.13 25.14 25.15 25.16 25.17 25.18 25.19 25.20 25.21 25.22 25.23 25.24 25.25 Chadi, Nicholas; Minato, Claudia; Stanwick, Richard (15 June 2020). "Cannabis vaping: Understanding the health risks of a rapidly emerging trend". Paediatrics & Child Health. 25 (Supplement_1): S16–S20. doi:10.1093/pch/pxaa016. PMC 7757764. PMID 33390752.
- ↑ 26.0 26.1 26.2 26.3 Leas, Eric C.; Moy, Natalie; McMenamin, Sara B.; Shi, Yuyan; Benmarhnia, Tarik; Stone, Matthew D.; Trinidad, Dennis R.; White, Martha (January 2021). "Availability and Promotion of Cannabidiol (CBD) Products in Online Vape Shops". International Journal of Environmental Research and Public Health. 18 (13): 6719. doi:10.3390/ijerph18136719. PMC 8295837. PMID 34206501.
 This article incorporates text by Eric C. Leas, Natalie Moy, Sara B. McMenamin, Yuyan Shi, Tarik Benmarhnia, Matthew D. Stone, Dennis R. Trinidad, and Martha White available under the CC BY 4.0 license.
This article incorporates text by Eric C. Leas, Natalie Moy, Sara B. McMenamin, Yuyan Shi, Tarik Benmarhnia, Matthew D. Stone, Dennis R. Trinidad, and Martha White available under the CC BY 4.0 license.
- ↑ 27.0 27.1 27.2 27.3 27.4 27.5 27.6 27.7 Bonner, Emily; Chang, Yvonne; Christie, Emerson; Colvin, Victoria; Cunningham, Brittany; Elson, Daniel; Ghetu, Christine; Huizenga, Juliana; Hutton, Sara J.; Kolluri, Siva K.; Maggio, Stephanie; Moran, Ian; Parker, Bethany; Rericha, Yvonne; Rivera, Brianna N.; Samon, Samantha; Schwichtenberg, Trever; Shankar, Prarthana; Simonich, Michael T.; Wilson, Lindsay B.; Tanguay, Robyn L. (September 2021). "The chemistry and toxicology of vaping". Pharmacology & Therapeutics. 225: 107837. doi:10.1016/j.pharmthera.2021.107837. ISSN 0163-7258. PMC 8263470. PMID 33753133.
- ↑ 28.0 28.1 28.2 Brown, Christopher J; Cheng, James M (2014). "Electronic cigarettes: product characterisation and design considerations". Tobacco Control. 23 (suppl 2): ii4–ii10. doi:10.1136/tobaccocontrol-2013-051476. ISSN 0964-4563. PMC 3995271. PMID 24732162.
- ↑ 29.0 29.1 Besaratinia, Ahmad; Tommasi, Stella (2021). "The consequential impact of JUUL on youth vaping and the landscape of tobacco products: The state of play in the COVID-19 era". Preventive Medicine Reports. 22: 101374. doi:10.1016/j.pmedr.2021.101374. ISSN 2211-3355. PMC 8207461. PMID 34168950.
- ↑ 30.0 30.1 Mullins, Mary Frances (May 2021). "Cannabis dabbing: An emerging trend". Nursing. 51 (5): 46–50. doi:10.1097/01.NURSE.0000743108.72528.d8. PMC 8078006. PMID 33871423.
- ↑ 31.00 31.01 31.02 31.03 31.04 31.05 31.06 31.07 31.08 31.09 31.10 31.11 31.12 31.13 31.14 31.15 31.16 31.17 31.18 31.19 31.20 31.21 31.22 31.23 31.24 31.25 31.26 31.27 31.28 31.29 31.30 31.31 31.32 31.33 31.34 31.35 31.36 31.37 31.38 31.39 31.40 31.41 31.42 31.43 31.44 31.45 Zheng, Zhonghua; Fiddes, Kelsey; Yang, Liangcheng (December 2021). "A narrative review on environmental impacts of cannabis cultivation". Journal of Cannabis Research. 3 (1). doi:10.1186/s42238-021-00090-0. PMC 8349047. PMID 34362475.
 This article incorporates text by Zhonghua Zheng, Kelsey Fiddes, and Liangcheng Yang available under the CC BY 4.0 license.
This article incorporates text by Zhonghua Zheng, Kelsey Fiddes, and Liangcheng Yang available under the CC BY 4.0 license.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 32.6 "E-Cigarette, or Vaping, Products Visual Dictionary" (PDF). Centers for Disease Control and Prevention. 24 September 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Pham, Kien; DeFina, Sam; Wang, He (24 February 2021). "E-Cigarettes Promote Macrophage-Tumor Cells Crosstalk: Focus on Breast Carcinoma Progression and Lung Metastasis". Exploratory Research and Hypothesis in Medicine. 000 (000): 000–000. doi:10.14218/erhm.2021.00002. PMC 9005083. PMID 35419501.
- ↑ 34.0 34.1 34.2 34.3 34.4 34.5 34.6 34.7 34.8 34.9 Jenssen, Brian P.; Boykan, Rachel (2019). "Electronic Cigarettes and Youth in the United States: A Call to Action (at the Local, National and Global Levels)". Children. 6 (2): 30. doi:10.3390/children6020030. ISSN 2227-9067. PMC 6406299. PMID 30791645.
 This article incorporates text by Brian P. Jenssen and Rachel Boykan available under the CC BY 4.0 license.
This article incorporates text by Brian P. Jenssen and Rachel Boykan available under the CC BY 4.0 license.
- ↑ 35.0 35.1 35.2 Feeney, Susan; Rossetti, Victoria; Terrien, Jill (29 March 2022). "E-Cigarettes—a review of the evidence—harm versus harm reduction". Tobacco use insights. SAGE Publications. 15: 1179173X2210875. doi:10.1177/1179173x221087524. ISSN 1179-173X. PMC 8968985. PMID 35370428.
- ↑ 36.0 36.1 Gupta, Priya Sarin; Kalagher, Kelly M. (2021). "Where There Is (No) Smoke, There Is Still Fire: a Review of Trends, Reasons for Use, Preferences and Harm Perceptions of Adolescent and Young Adult Electronic Cigarette Use". Current Pediatrics Reports. doi:10.1007/s40124-021-00240-1. ISSN 2167-4841. PMC 8107807. PMID 33996271.
- ↑ Cheng, T. (2014). "Chemical evaluation of electronic cigarettes". Tobacco Control. 23 (Supplement 2): ii11–ii17. doi:10.1136/tobaccocontrol-2013-051482. ISSN 0964-4563. PMC 3995255. PMID 24732157.
- ↑ 38.0 38.1 38.2 38.3 38.4 Perrone, Matthew (19 December 2023). "Elf Bar and other e-cigarette makers dodged US customs and taxes after China's ban on vaping flavors". AP News.
- ↑ 39.0 39.1 Grana, Rachel; Benowitz, Neal; Glantz, Stanton A. (13 May 2014). "E-Cigarettes: A Scientific Review". Circulation. 129 (19): 1972–1986. doi:10.1161/circulationaha.114.007667. PMC 4018182. PMID 24821826.
- ↑ 40.0 40.1 40.2 40.3 Cecchini, Matthew J.; Mukhopadhyay, Sanjay; Arrossi, Andrea V.; Beasley, Mary B.; Butt, Yasmeen M.; Jones, Kirk D.; Pambuccian, Stefan; Mehrad, Mitra; Monaco, Sara E.; Saqi, Anjali; Smith, Maxwell L.; Tazelaar, Henry D.; Larsen, Brandon T. (2020). "E-Cigarette or Vaping Product Use-Associated Lung Injury: A Review for Pathologists". Archives of Pathology & Laboratory Medicine. 144 (12): 1490–1500. doi:10.5858/arpa.2020-0024-RA. ISSN 1543-2165. PMID 32401055.
- ↑ 41.0 41.1 41.2 41.3 41.4 Stefaniak, Aleksandr B.; LeBouf, Ryan F.; Ranpara, Anand C.; Leonard, Stephen S. (2021). "Toxicology of flavoring- and cannabis-containing e-liquids used in electronic delivery systems". Pharmacology & Therapeutics. 224: 107838. doi:10.1016/j.pharmthera.2021.107838. ISSN 0163-7258. PMC 8251682. PMID 33746051.
- ↑ 42.00 42.01 42.02 42.03 42.04 42.05 42.06 42.07 42.08 42.09 42.10 42.11 42.12 42.13 42.14 Chen, Grace; Rahman, Shafiqur; Lutfy, Kabirullah (30 June 2023). "E-cigarettes may serve as a gateway to conventional cigarettes and other addictive drugs". Advances in Drug and Alcohol Research. 3. doi:10.3389/adar.2023.11345. PMC 10880776. PMID 38389821.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Grace Chen, Shafiqur Rahman, and Kabirullah Lutfy available under the CC BY 4.0 license.
This article incorporates text by Grace Chen, Shafiqur Rahman, and Kabirullah Lutfy available under the CC BY 4.0 license.
- ↑ Cooke, Andrew; Fergeson, Jennifer; Bulkhi, Adeeb; Casale, Thomas B. (2015). "The Electronic Cigarette: The Good, the Bad, and the Ugly". The Journal of Allergy and Clinical Immunology: In Practice. 3 (4): 498–505. doi:10.1016/j.jaip.2015.05.022. ISSN 2213-2198. PMID 26164573.
- ↑ Orellana-Barrios, Menfil A.; Payne, Drew; Mulkey, Zachary; Nugent, Kenneth (2015). "Electronic cigarettes-a narrative review for clinicians". The American Journal of Medicine. 128 (7): 674–81. doi:10.1016/j.amjmed.2015.01.033. ISSN 0002-9343. PMID 25731134.
- ↑ 45.0 45.1 45.2 45.3 45.4 45.5 45.6 45.7 Simão, Ana Y.; Antunes, Mónica; Cabral, Emanuel; Oliveira, Patrik; Rosendo, Luana M.; Brinca, Ana Teresa; Alves, Estefânia; Marques, Hernâni; Rosado, Tiago; Passarinha, Luís A.; Andraus, Maristela; Barroso, Mário; Gallardo, Eugenia (17 April 2022). "An Update on the Implications of New Psychoactive Substances in Public Health". International Journal of Environmental Research and Public Health. 19 (8): 4869. doi:10.3390/ijerph19084869. PMC 9028227. PMID 35457736.
 This article incorporates text by Ana Y. Simão, Mónica Antunes, Emanuel Cabral, Patrik Oliveira, Luana M. Rosendo, Ana Teresa Brinca, Estefânia Alves, Hernâni Marques, Tiago Rosado, Luís A. Passarinha, Maristela Andraus, Mário Barroso, and Eugenia Gallardo available under the CC BY 4.0 license.
This article incorporates text by Ana Y. Simão, Mónica Antunes, Emanuel Cabral, Patrik Oliveira, Luana M. Rosendo, Ana Teresa Brinca, Estefânia Alves, Hernâni Marques, Tiago Rosado, Luís A. Passarinha, Maristela Andraus, Mário Barroso, and Eugenia Gallardo available under the CC BY 4.0 license.
- ↑ 46.0 46.1 46.2 46.3 Verstraete, Alain G. (April 2004). "Detection Times of Drugs of Abuse in Blood, Urine, and Oral Fluid:". Therapeutic Drug Monitoring. 26 (2): 200–205. doi:10.1097/00007691-200404000-00020. PMID 15228165.
- ↑ 47.0 47.1 47.2 47.3 Alshaarawy, Omayma; Roskos, Steven E.; Meghea, Cristian I. (September 2021). "Tobacco cigarette and cannabis use among new mothers". Addiction. 116 (9): 2572–2576. doi:10.1111/add.15372. PMC 8192585. PMID 33314407.
- ↑ 48.0 48.1 48.2 48.3 48.4 48.5 Takakuwa, Kevin M.; Schears, Raquel M. (December 2021). "The emergency department care of the cannabis and synthetic cannabinoid patient: a narrative review". International Journal of Emergency Medicine. 14 (1). doi:10.1186/s12245-021-00330-3. PMC 7874647. PMID 33568074.
 This article incorporates text by Kevin M. Takakuwa and Raquel M. Schears available under the CC BY 4.0 license.
This article incorporates text by Kevin M. Takakuwa and Raquel M. Schears available under the CC BY 4.0 license.
- ↑ 49.00 49.01 49.02 49.03 49.04 49.05 49.06 49.07 49.08 49.09 49.10 49.11 49.12 49.13 49.14 49.15 49.16 49.17 49.18 49.19 49.20 49.21 49.22 49.23 Bukke, Vidyasagar Naik; Archana, Moola; Villani, Rosanna; Serviddio, Gaetano; Cassano, Tommaso (24 September 2021). "Pharmacological and Toxicological Effects of Phytocannabinoids and Recreational Synthetic Cannabinoids: Increasing Risk of Public Health". Pharmaceuticals. 14 (10): 965. doi:10.3390/ph14100965. PMC 8541640. PMID 34681189.
 This article incorporates text by Vidyasagar Naik Bukke, Moola Archana, Rosanna Villani, Gaetano Serviddio, and Tommaso Cassano available under the CC BY 4.0 license.
This article incorporates text by Vidyasagar Naik Bukke, Moola Archana, Rosanna Villani, Gaetano Serviddio, and Tommaso Cassano available under the CC BY 4.0 license.
- ↑ 51.00 51.01 51.02 51.03 51.04 51.05 51.06 51.07 51.08 51.09 51.10 Lobato-Freitas, Carolina; Brito-da-Costa, Andreia Machado; Dinis-Oliveira, Ricardo Jorge; Carmo, Helena; Carvalho, Félix; Silva, João Pedro; Dias-da-Silva, Diana (25 February 2021). "Overview of Synthetic Cannabinoids ADB-FUBINACA and AMB-FUBINACA: Clinical, Analytical, and Forensic Implications". Pharmaceuticals. 14 (3): 186. doi:10.3390/ph14030186. PMC 7996508. PMID 33669071.
 This article incorporates text by Carolina Lobato-Freitas, Andreia Machado Brito-da-Costa, Ricardo Jorge Dinis-Oliveira, Helena Carmo, Félix Carvalho, João Pedro Silva, and Diana Dias-da-Silva available under the CC BY 4.0 license.
This article incorporates text by Carolina Lobato-Freitas, Andreia Machado Brito-da-Costa, Ricardo Jorge Dinis-Oliveira, Helena Carmo, Félix Carvalho, João Pedro Silva, and Diana Dias-da-Silva available under the CC BY 4.0 license.
- ↑ 52.0 52.1 52.2 52.3 Connor, Jason P.; Stjepanović, Daniel; Le Foll, Bernard; Hoch, Eva; Budney, Alan J.; Hall, Wayne D. (25 February 2021). "Cannabis use and cannabis use disorder". Nature Reviews Disease Primers. 7 (1). doi:10.1038/s41572-021-00247-4. PMC 8655458. PMID 33627670.
- ↑ 53.00 53.01 53.02 53.03 53.04 53.05 53.06 53.07 53.08 53.09 53.10 53.11 53.12 53.13 53.14 53.15 53.16 53.17 53.18 53.19 53.20 53.21 53.22 Greydanus, Donald E.; Hawver, Elizabeth K.; Greydanus, Megan M.; Merrick, Joav (2013). "Marijuana: Current Concepts†". Frontiers in Public Health. 1. doi:10.3389/fpubh.2013.00042. PMC 3859982. PMID 24350211.
 This article incorporates text by Donald E Greydanus, Elizabeth K Hawver, Megan M Greydanus, and Joav Merrick available under the CC BY 4.0 license.
This article incorporates text by Donald E Greydanus, Elizabeth K Hawver, Megan M Greydanus, and Joav Merrick available under the CC BY 4.0 license.
- ↑ 54.00 54.01 54.02 54.03 54.04 54.05 54.06 54.07 54.08 54.09 54.10 54.11 54.12 54.13 54.14 54.15 "Cannabis (Marijuana) DrugFacts". National Institute on Drug Abuse. 24 December 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 55.0 55.1 55.2 55.3 55.4 55.5 Malinowska, Barbara; Baranowska-Kuczko, Marta; Kicman, Aleksandra; Schlicker, Eberhard (17 February 2021). "Opportunities, Challenges and Pitfalls of Using Cannabidiol as an Adjuvant Drug in COVID-19". International Journal of Molecular Sciences. 22 (4): 1986. doi:10.3390/ijms22041986. PMC 7922403. PMID 33671463.
 This article incorporates text by Barbara Malinowska, Marta Baranowska-Kuczko, Aleksandra Kicman, and Eberhard Schlicker available under the CC BY 4.0 license.
This article incorporates text by Barbara Malinowska, Marta Baranowska-Kuczko, Aleksandra Kicman, and Eberhard Schlicker available under the CC BY 4.0 license.
- ↑ 56.00 56.01 56.02 56.03 56.04 56.05 56.06 56.07 56.08 56.09 56.10 56.11 56.12 56.13 56.14 56.15 56.16 56.17 56.18 56.19 56.20 56.21 56.22 Khademi, Sedigh; Hallinan, Christine Mary; Conway, Mike; Bonomo, Yvonne (27 February 2023). "Using Social Media Data to Investigate Public Perceptions of Cannabis as a Medicine: Narrative Review". Journal of Medical Internet Research. 25: e36667. doi:10.2196/36667. PMC 10012004. PMID 36848191.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Sedigh Khademi, Christine Mary Hallinan, Mike Conway, and Yvonne Bonomo available under the CC BY 4.0 license.
This article incorporates text by Sedigh Khademi, Christine Mary Hallinan, Mike Conway, and Yvonne Bonomo available under the CC BY 4.0 license.
- ↑ Amin, Samia; Chae, Si Woo; Kawamoto, Crissy T; Phillips, Kristina T; Pokhrel, Pallav (30 January 2024). "Cannabis use among cancer patients and survivors in the United States: a systematic review". JNCI Cancer Spectrum. doi:10.1093/jncics/pkae004. PMID 38291891.
- ↑ Joseph, P; Vettraino, IM (September 2020). "Cannabis in Pregnancy and Lactation - A Review". Missouri medicine. 117 (5): 400–405. PMC 7723128. PMID 33311738.
- ↑ 59.00 59.01 59.02 59.03 59.04 59.05 59.06 59.07 59.08 59.09 59.10 59.11 59.12 59.13 59.14 59.15 59.16 59.17 59.18 59.19 59.20 59.21 "About synthetic cannabinoids". Centers for Disease Control and Prevention. 23 March 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 60.00 60.01 60.02 60.03 60.04 60.05 60.06 60.07 60.08 60.09 60.10 60.11 60.12 60.13 60.14 60.15 60.16 60.17 60.18 60.19 60.20 60.21 60.22 60.23 60.24 60.25 Fordjour, Eric; Manful, Charles F.; Sey, Albert A.; Javed, Rabia; Pham, Thu Huong; Thomas, Raymond; Cheema, Mumtaz (15 June 2023). "Cannabis: a multifaceted plant with endless potentials". Frontiers in Pharmacology. 14. doi:10.3389/fphar.2023.1200269. PMC 10308385. PMID 37397476.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Eric Fordjour, Charles F. Manful, Albert A. Sey, Rabia Javed, Thu Huong Pham, Raymond Thomas, and Mumtaz Cheema available under the CC BY 4.0 license.
This article incorporates text by Eric Fordjour, Charles F. Manful, Albert A. Sey, Rabia Javed, Thu Huong Pham, Raymond Thomas, and Mumtaz Cheema available under the CC BY 4.0 license.
- ↑ McDuff, David R.; Garvin, Michelle; Thompson, Donald (January 2024). "Substance Misuse in Elite Athletes". Clinics in Sports Medicine. 43 (1): 127–144. doi:10.1016/j.csm.2023.06.008. PMID 37949506.
- ↑ 62.0 62.1 Žigić, N; Hasanović, M; Pajević, I; Jakovljević, M (2021). "Possible Consequences of Cannabis Legalization - What Do Research Show?". Psychiatria Danubina. 33 (Suppl 4): 1184–1195. PMID 35354186.
- ↑ "Data and Statistics". Centers for Disease Control and Prevention. 8 June 2021.
- ↑ 64.0 64.1 64.2 Fischer, Adina S.; Tapert, Susan F.; Louie, Dexter Lee; Schatzberg, Alan F.; Singh, Manpreet K. (June 2020). "Cannabis and the Developing Adolescent Brain". Current Treatment Options in Psychiatry. 7 (2): 144–161. doi:10.1007/s40501-020-00202-2. PMC 7380653. PMID 32714742.
- ↑ 65.0 65.1 65.2 65.3 65.4 65.5 65.6 65.7 65.8 65.9 Greaves, Lorraine; Hemsing, Natalie (14 January 2020). "Sex and Gender Interactions on the Use and Impact of Recreational Cannabis". International Journal of Environmental Research and Public Health. 17 (2): 509. doi:10.3390/ijerph17020509. PMC 7014129. PMID 31947505.
 This article incorporates text by Lorraine Greaves and Natalie Hemsing available under the CC BY 4.0 license.
This article incorporates text by Lorraine Greaves and Natalie Hemsing available under the CC BY 4.0 license.
- ↑ 66.00 66.01 66.02 66.03 66.04 66.05 66.06 66.07 66.08 66.09 66.10 66.11 66.12 66.13 66.14 66.15 66.16 66.17 66.18 66.19 66.20 66.21 66.22 66.23 66.24 66.25 66.26 66.27 66.28 66.29 66.30 66.31 66.32 66.33 66.34 66.35 66.36 66.37 66.38 66.39 66.40 66.41 66.42 66.43 66.44 66.45 66.46 66.47 66.48 66.49 66.50 66.51 Harrell, Melissa B.; Clendennen, Stephanie L.; Sumbe, Aslesha; Case, Kathleen R.; Mantey, Dale S.; Swan, Sunaina (7 May 2022). "Cannabis Vaping Among Youth and Young Adults: a Scoping Review". Current Addiction Reports. 9 (3): 217–234. doi:10.1007/s40429-022-00413-y. PMC 9078633. PMID 35573056.
 This article incorporates text by Melissa B. Harrell, Stephanie L. Clendennen, Aslesha Sumbe, Kathleen R. Case, Dale S. Mantey, and Sunaina Swan available under the CC BY 4.0 license.
This article incorporates text by Melissa B. Harrell, Stephanie L. Clendennen, Aslesha Sumbe, Kathleen R. Case, Dale S. Mantey, and Sunaina Swan available under the CC BY 4.0 license.
- ↑ 67.0 67.1 67.2 67.3 67.4 67.5 67.6 67.7 67.8 Choi, Humberto; Lin, Yu; Race, Elliot; Macmurdo, Maeve G. (February 2021). "Electronic Cigarettes and Alternative Methods of Vaping". Annals of the American Thoracic Society. 18 (2): 191–199. doi:10.1513/AnnalsATS.202005-511CME. PMID 33052707.
- ↑ 68.0 68.1 68.2 68.3 68.4 de Oliveira, Mariana Campello; Vides, Mariana Capelo; Lassi, Dângela Layne Silva; Torales, Julio; Ventriglio, Antonio; Bombana, HenriqueSilva; Leyton, Vilma; Périco, Cintia de Azevedo-Marques; Negrão, André Brooking; Malbergier, André; Castaldelli-Maia, João Maurício (24 June 2023). "Toxicity of Synthetic Cannabinoids in K2/Spice: A Systematic Review". Brain Sciences. 13 (7): 990. doi:10.3390/brainsci13070990. PMC 10377539. PMID 37508922.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Mariana Campello de Oliveira, Mariana Capelo Vides, Dângela Layne Silva Lassi, Julio Torales, Antonio Ventriglio, Henrique Silva Bombana, Vilma Leyton, Cintia de Azevedo-Marques Périco, André Brooking Negrão, André Malbergier, and João Maurício Castaldelli-Maia available under the CC BY 4.0 license.
This article incorporates text by Mariana Campello de Oliveira, Mariana Capelo Vides, Dângela Layne Silva Lassi, Julio Torales, Antonio Ventriglio, Henrique Silva Bombana, Vilma Leyton, Cintia de Azevedo-Marques Périco, André Brooking Negrão, André Malbergier, and João Maurício Castaldelli-Maia available under the CC BY 4.0 license.
- ↑ 69.00 69.01 69.02 69.03 69.04 69.05 69.06 69.07 69.08 69.09 69.10 69.11 69.12 Chong, Wendy Wing-Yee; Acar, Zeynep Ilgaz; West, Meghan Lee; Wong, Francis (1 October 2022). "A Scoping Review on the Medical and Recreational Use of Cannabis During the COVID-19 Pandemic". Cannabis and Cannabinoid Research. 7 (5): 591–602. doi:10.1089/can.2021.0054. PMC 9587770. PMID 34981958.
{{cite journal}}: Check|pmc=value (help) - ↑ 70.0 70.1 70.2 70.3 70.4 70.5 Kumar, Navin; Janmohamed, Kamila; Nyhan, Kate; Martins, Silvia S.; Cerda, Magdalena; Hasin, Deborah; Scott, Jenny; Pates, Richard; Ghandour, Lilian; Wazaify, Mayyada; Khoshnood, Kaveh (December 2021). "Substance use and substance use disorder, in relation to COVID-19: protocol for a scoping review". Systematic Reviews. 10 (1). doi:10.1186/s13643-021-01605-9. PMC 7857102. PMID 33536070.
 This article incorporates text by Navin Kumar, Kamila Janmohamed, Kate Nyhan, Silvia S. Martins, Magdalena Cerda, Deborah Hasin, Jenny Scott, Richard Pates, Lilian Ghandour, Mayyada Wazaify, and Kaveh Khoshnood available under the CC BY 4.0 license.
This article incorporates text by Navin Kumar, Kamila Janmohamed, Kate Nyhan, Silvia S. Martins, Magdalena Cerda, Deborah Hasin, Jenny Scott, Richard Pates, Lilian Ghandour, Mayyada Wazaify, and Kaveh Khoshnood available under the CC BY 4.0 license.
- ↑ Bakaloudi, Dimitra Rafailia; Evripidou, Kleo; Siargkas, Antonios; Breda, Joao; Chourdakis, Michail (May 2023). "Impact of COVID-19 lockdown on smoking and vaping: systematic review and meta-analysis". Public Health. 218: 160–172. doi:10.1016/j.puhe.2023.02.007. PMC 9939396. PMID 37043948.
{{cite journal}}: Check|pmc=value (help) - ↑ 72.0 72.1 72.2 72.3 72.4 Hurd, Yasmin L.; Manzoni, Olivier J.; Pletnikov, Mikhail V.; Lee, Francis S.; Bhattacharyya, Sagnik; Melis, Miriam (16 October 2019). "Cannabis and the Developing Brain: Insights into Its Long-Lasting Effects". The Journal of Neuroscience. 39 (42): 8250–8258. doi:10.1523/JNEUROSCI.1165-19.2019. PMC 6794936. PMID 31619494.
- ↑ 73.0 73.1 73.2 73.3 73.4 73.5 73.6 73.7 73.8 Thompson, Rebecca; DeJong, Katherine; Lo, Jamie (July 2019). "Marijuana Use in Pregnancy: A Review". Obstetrical & Gynecological Survey. 74 (7): 415–428. doi:10.1097/OGX.0000000000000685. PMC 7090387. PMID 31343707.
- ↑ 74.0 74.1 Badowski, S; Smith, G (February 2020). "Cannabis use during pregnancy and postpartum". Canadian family physician Medecin de famille canadien. 66 (2): 98–103. PMC 7021337. PMID 32060189.
- ↑ 75.0 75.1 75.2 75.3 75.4 75.5 Mock, Jeremiah (2019). "Notes from the Field: Environmental Contamination from E-cigarette, Cigarette, Cigar, and Cannabis Products at 12 High Schools — San Francisco Bay Area, 2018–2019". MMWR Morb Mortal Wkly Rep. 68 (40): 897–899. doi:10.15585/mmwr.mm6840a4. PMC 6788397. PMID 31600185.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 76.0 76.1 Dharmapuri, Sadhana; Miller, Kathleen; Klein, Jonathan D. (1 August 2020). "Marijuana and the Pediatric Population". Pediatrics. 146 (2). doi:10.1542/peds.2019-2629. PMID 32661188.
- ↑ Fadus, Matthew C.; Smith, Tracy T.; Squeglia, Lindsay M. (2019). "The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects". Drug and Alcohol Dependence. 201: 85–93. doi:10.1016/j.drugalcdep.2019.04.011. ISSN 0376-8716. PMID 31200279.
- ↑ Morris, James D.; Pebley, Kinsey; Little, Melissa A. (November 2023). "Vaping Opioids: Should We Be Worried?". American Journal of Health Promotion. 37 (8): 1171–1173. doi:10.1177/08901171231193785. PMID 37547936.
- ↑ 79.00 79.01 79.02 79.03 79.04 79.05 79.06 79.07 79.08 79.09 79.10 79.11 79.12 79.13 79.14 79.15 79.16 79.17 79.18 79.19 79.20 79.21 79.22 79.23 79.24 79.25 79.26 79.27 79.28 79.29 Tehrani, Hadi; Rajabi, Abdolhalim; Ghelichi-Ghojogh, Mousa; Nejatian, Mahbobeh; Jafari, Alireza (21 November 2022). "The prevalence of electronic cigarettes vaping globally: a systematic review and meta-analysis". Archives of Public Health. 80 (1). doi:10.1186/s13690-022-00998-w. PMC 9682677. PMID 36415010.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Hadi Tehrani, Abdolhalim Rajabi, Mousa Ghelichi-Ghojogh, Mahbobeh Nejatian, and Alireza Jafari available under the CC BY 4.0 license.
This article incorporates text by Hadi Tehrani, Abdolhalim Rajabi, Mousa Ghelichi-Ghojogh, Mahbobeh Nejatian, and Alireza Jafari available under the CC BY 4.0 license.
- ↑ Stubbs, Justin Joe; McCallum, Richard (February 2024). "Cannabinoid hyperemesis syndrome: prevalence and management in an era of cannabis legalization". Journal of Investigative Medicine. 72 (2): 171–177. doi:10.1177/10815589231217495. PMID 37997432.
- ↑ "Marijuana and Pregnancy". Substance Abuse and Mental Health Services Administration. 14 February 2024.
- ↑ 82.0 82.1 82.2 82.3 82.4 82.5 Ko, Jean Y.; Coy, Kelsey C.; Haight, Sarah C.; Haegerich, Tamara M.; Williams, Letitia; Cox, Shanna; Njai, Rashid; Grant, Althea M. (14 August 2020). "Characteristics of Marijuana Use During Pregnancy — Eight States, Pregnancy Risk Assessment Monitoring System, 2017". MMWR. Morbidity and Mortality Weekly Report. 69 (32): 1058–1063. doi:10.15585/mmwr.mm6932a2. PMC 7440118. PMID 32790656.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 83.0 83.1 Chadi, Nicholas; Hadland, Scott E.; Harris, Sion K. (January 2019). "Understanding the Implications of the "Vaping Epidemic" among Adolescents and Young Adults: A Call for Action". Substance Abuse. 40 (1): 7–10. doi:10.1080/08897077.2019.1580241. PMC 6583912. PMID 30883295.
- ↑ 84.0 84.1 "Marijuana and hallucinogen use, binge drinking reached historic highs among adults 35 to 50". National Institutes of Health. 17 August 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 85.0 85.1 85.2 85.3 Lau, Lucinda; Conti, Aldo Alberto; Hemmati, Zeynab; Baldacchino, Alex (October 2023). "The prospective association between the use of E-cigarettes and other psychoactive substances in young people: A systematic review and meta-analysis". Neuroscience & Biobehavioral Reviews. 153: 105392. doi:10.1016/j.neubiorev.2023.105392. PMID 37714228.
- ↑ 86.0 86.1 86.2 86.3 86.4 86.5 86.6 86.7 Desjardins, N.; Stheneur, C. (June 2016). "Syndrome d'hyperémèse cannabique: revue de la littérature" [Cannabinoid hyperemesis syndrome: A review of the literature]. Archives de Pédiatrie (in French). 23 (6): 619–623. doi:10.1016/j.arcped.2016.01.016. PMID 27017363.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ 87.0 87.1 Aladeokin, Adewale; Haighton, Catherine (22 April 2019). "Is adolescent e-cigarette use associated with smoking in the United Kingdom?: A systematic review with meta-analysis". Tobacco Prevention & Cessation. 5 (April). doi:10.18332/tpc/108553. PMC 7205081. PMID 32411879.
- ↑ 88.0 88.1 Ayo-Yusuf, Olalekan; Nkosi, Lungile; Agaku, Israel (9 November 2022). "E-cigarette Use and Regulation in South Africa: a Synthesis of Evidence in Response to Industry Efforts to Undermine Product Regulation". Current Addiction Reports. 9 (4): 363–372. doi:10.1007/s40429-022-00451-6.
- ↑ Ramlagan, Shandir; Peltzer, Karl; Pengpid, Supa (December 2021). "Prevalence and correlates of non-daily and daily cannabis use among persons 15 years and older in South Africa: results of a national survey in 2017". Substance Abuse Treatment, Prevention, and Policy. 16 (1). doi:10.1186/s13011-021-00364-z. PMC 7980317. PMID 33743758.
 This article incorporates text by Shandir Ramlagan, Karl Peltzer, and Supa Pengpid available under the CC BY 4.0 license.
This article incorporates text by Shandir Ramlagan, Karl Peltzer, and Supa Pengpid available under the CC BY 4.0 license.
- ↑ Soin, G.K.; Filby, S.; van Zyl-Smit, R.N. (May 2023). "The Nature and Extent of Vaping and Tobacco Use Amongst South African High School Learners": A2611–A2611. doi:10.1164/ajrccm-conference.2023.207.1_MeetingAbstracts.A2611.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 91.0 91.1 91.2 Budney, Alan J.; Sofis, Michael J.; Borodovsky, Jacob T. (February 2019). "An update on cannabis use disorder with comment on the impact of policy related to therapeutic and recreational cannabis use". European Archives of Psychiatry and Clinical Neuroscience. 269 (1): 73–86. doi:10.1007/s00406-018-0976-1. PMC 6397057. PMID 30604051.
- ↑ Dresen, Sebastian; Ferreirós, Nerea; Pütz, Michael; Westphal, Folker; Zimmermann, Ralf; Auwärter, Volker (October 2010). "Monitoring of herbal mixtures potentially containing synthetic cannabinoids as psychoactive compounds". Journal of Mass Spectrometry. 45 (10): 1186–1194. doi:10.1002/jms.1811. PMID 20857386.
- ↑ 93.00 93.01 93.02 93.03 93.04 93.05 93.06 93.07 93.08 93.09 93.10 93.11 93.12 Grigg, Jasmin; Manning, Victoria; Arunogiri, Shalini; Lubman, Dan I (June 2019). "Synthetic cannabinoid use disorder: an update for general psychiatrists". Australasian Psychiatry. 27 (3): 279–283. doi:10.1177/1039856218822749. PMID 30663326.
- ↑ 94.0 94.1 94.2 Miliano, Cristina; Scott, E. Reilly; Murdaugh, Laura B.; Gnatowski, Emma R.; Faunce, Christine L.; Anderson, Megan S.; Reyes, Malissa M.; Gregus, Ann M.; Buczynski, Matthew W. (January 2020). "Modeling drug exposure in rodents using e-cigarettes and other electronic nicotine delivery systems". Journal of Neuroscience Methods. 330: 108458. doi:10.1016/j.jneumeth.2019.108458. PMID 31614162.
- ↑ 95.0 95.1 95.2 95.3 95.4 Jameson, Laura E.; Conrow, Kendra D.; Pinkhasova, Dorina V.; Boulanger, Haleigh L.; Ha, Hyunji; Jourabchian, Negar; Johnson, Steven A.; Simeone, Michael P.; Afia, Iniobong A.; Cahill, Thomas M.; Orser, Cindy S.; Leung, Maxwell C.K. (September 2022). "Comparison of State-Level Regulations for Cannabis Contaminants and Implications for Public Health". Environmental Health Perspectives. 130 (9). doi:10.1289/EHP11206. PMC 9472674. PMID 36102653.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 96.0 96.1 96.2 Cottencin, Olivier; Rolland, Benjamin; Karila, Laurent (December 2014). "New Designer Drugs (Synthetic Cannabinoids and Synthetic Cathinones): Review of Literature". Current Pharmaceutical Design. 20 (25): 4106–4111. doi:10.2174/13816128113199990622. PMID 24001292.
- ↑ 97.0 97.1 97.2 97.3 "Is marijuana a gateway drug?". National Institute on Drug Abuse. July 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 98.0 98.1 O'Callaghan, Marissa; Boyle, Niamh; Fabre, Aurelie; Keane, Michael P.; McCarthy, Cormac (10 March 2022). "Vaping-Associated Lung Injury: A Review". Medicina (Kaunas, Lithuania). MDPI AG. 58 (3): 412. doi:10.3390/medicina58030412. ISSN 1648-9144. PMC 8949983. PMID 35334588.}
 This article incorporates text by Marissa O’Callaghan, Niamh Boyle, Aurelie Fabre, Michael P. Keane, and Cormac McCarthy available under the CC BY 4.0 license.
This article incorporates text by Marissa O’Callaghan, Niamh Boyle, Aurelie Fabre, Michael P. Keane, and Cormac McCarthy available under the CC BY 4.0 license.
- ↑ 99.0 99.1 99.2 Subramaniam, VN; Menezes, AR; DeSchutter, A; Lavie, CJ (March 2019). "The Cardiovascular Effects of Marijuana: Are the Potential Adverse Effects Worth the High?". Missouri medicine. 116 (2): 146–153. PMC 6461323. PMID 31040502.
- ↑ 100.0 100.1 100.2 100.3 100.4 100.5 100.6 100.7 100.8 Brands, Bruna; Di Ciano, Patricia; Mann, Robert E. (19 August 2021). "Cannabis, Impaired Driving, and Road Safety: An Overview of Key Questions and Issues". Frontiers in Psychiatry. 12. doi:10.3389/fpsyt.2021.641549. PMC 8416748. PMID 34489746.
 This article incorporates text by Bruna Brands, Patricia Di Ciano, and Robert E Mann available under the CC BY 4.0 license.
This article incorporates text by Bruna Brands, Patricia Di Ciano, and Robert E Mann available under the CC BY 4.0 license.
- ↑ 101.00 101.01 101.02 101.03 101.04 101.05 101.06 101.07 101.08 101.09 101.10 Dunn, Keeley; Taylor, Amelia; Turfus, Sophie (August 2021). "A review of cannabidiol‐containing electronic liquids—Current regulations and labelling accuracy". Drug Testing and Analysis. 13 (8): 1490–1498. doi:10.1002/dta.3102. PMID 34022104.
- ↑ 102.0 102.1 102.2 102.3 102.4 Shafi, Abu; Berry, Alex J.; Sumnall, Harry; Wood, David M.; Tracy, Derek K. (January 2020). "New psychoactive substances: a review and updates". Therapeutic Advances in Psychopharmacology. 10: 204512532096719. doi:10.1177/2045125320967197. PMC 7750892. PMID 33414905.
- ↑ 103.00 103.01 103.02 103.03 103.04 103.05 103.06 103.07 103.08 103.09 103.10 103.11 "What You Need to Know (And What We're Working to Find Out) About Products Containing Cannabis or Cannabis-derived Compounds, Including CBD". United States Food and Drug Administration. 5 March 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 104.0 104.1 104.2 104.3 104.4 Geci, Michael; Scialdone, Mark; Tishler, Jordan (April 2023). "The Dark Side of Cannabidiol: The Unanticipated Social and Clinical Implications of Synthetic Δ8-THC". Cannabis and Cannabinoid Research. 8 (2): 270–282. doi:10.1089/can.2022.0126. PMC 10061328. PMID 36264171.
{{cite journal}}: Check|pmc=value (help) - ↑ 105.0 105.1 105.2 105.3 105.4 105.5 105.6 Laudanski, Krzysztof; Wain, Justin (22 January 2022). "Considerations for Cannabinoids in Perioperative Care by Anesthesiologists". Journal of Clinical Medicine. 11 (3): 558. doi:10.3390/jcm11030558. PMC 8836924. PMID 35160010.
 This article incorporates text by Krzysztof Laudanski and Justin Wain2 available under the CC BY 4.0 license.
This article incorporates text by Krzysztof Laudanski and Justin Wain2 available under the CC BY 4.0 license.
- ↑ 106.0 106.1 McPartland, John M.; McKernan, Kevin J. (2017). "Contaminants of Concern in Cannabis: Microbes, Heavy Metals and Pesticides". Cannabis sativa L. - Botany and Biotechnology: 457–474. doi:10.1007/978-3-319-54564-6_22.
- ↑ 107.0 107.1 107.2 107.3 107.4 107.5 107.6 Taylor, Amelia; Birkett, Jason W. (February 2020). "Pesticides in cannabis: A review of analytical and toxicological considerations". Drug Testing and Analysis. 12 (2): 180–190. doi:10.1002/dta.2747. PMID 31834671.
- ↑ 108.00 108.01 108.02 108.03 108.04 108.05 108.06 108.07 108.08 108.09 108.10 108.11 108.12 MacCallum, Caroline A.; Lo, Lindsay A.; Pistawka, Carly A.; Christiansen, April; Boivin, Michael (20 December 2023). "Cannabis vaporisation: Understanding products, devices and risks". Drug and Alcohol Review. doi:10.1111/dar.13800. PMID 38124429.
- ↑ 109.0 109.1 109.2 109.3 Kelly, Brian F.; Nappe, Thomas M. (January 2024). "Cannabinoid Toxicity". StatPearls. StatPearls Publishing. PMID 29489164/.
{{cite book}}: Check|pmid=value (help) - ↑ 110.0 110.1 110.2 Ebbert, Jon O.; Scharf, Eugene L.; Hurt, Ryan T. (December 2018). "Medical Cannabis". Mayo Clinic Proceedings. 93 (12): 1842–1847. doi:10.1016/j.mayocp.2018.09.005. PMID 30522595.
- ↑ Spindle, Tory R; Bonn-Miller, Marcel O; Vandrey, Ryan (December 2019). "Changing landscape of cannabis: novel products, formulations, and methods of administration". Current Opinion in Psychology. 30: 98–102. doi:10.1016/j.copsyc.2019.04.002. PMID 31071592.
- ↑ "Cancer". Centers for Disease Control and Prevention. 19 October 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 113.0 113.1 Sheikh, NK; Dua, A (January 2024). "Cannabinoids.". StatPearls. StatPearls Publishing. PMID 32310522.
- ↑ 114.0 114.1 Whiting, Penny F.; Wolff, Robert F.; Deshpande, Sohan; Di Nisio, Marcello; Duffy, Steven; Hernandez, Adrian V.; Keurentjes, J.Christiaan; Lang, Shona; Misso, Kate; Ryder, Steve; Schmidlkofer, Simone; Westwood, Marie; Kleijnen, Jos (23 June 2015). "Cannabinoids for Medical Use: A Systematic Review and Meta-analysis". JAMA. 313 (24): 2456. doi:10.1001/jama.2015.6358. PMID 26103030.
- ↑ 115.0 115.1 115.2 115.3 Hazle, Mia C.; Hill, Kevin P.; Westreich, Laurence M. (1 February 2022). "Workplace Cannabis Policies: A Moving Target". Cannabis and Cannabinoid Research. 7 (1): 16–23. doi:10.1089/can.2020.0095. PMC 8864412. PMID 33998870.
- ↑ 116.0 116.1 116.2 "CBD: What You Need to Know". Centers for Disease Control and Prevention. 8 August 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 117.0 117.1 Todaro, Barbara (April 2012). "Cannabinoids in the Treatment of Chemotherapy-Induced Nausea and Vomiting". Journal of the National Comprehensive Cancer Network. 10 (4): 487–492. doi:10.6004/jnccn.2012.0048. PMID 22491047.
- ↑ 118.0 118.1 118.2 118.3 Howlett, Allyn C.; Thomas, Brian F.; Huffman, John W. (14 October 2021). "The Spicy Story of Cannabimimetic Indoles". Molecules. 26 (20): 6190. doi:10.3390/molecules26206190. PMC 8538531. PMID 34684770.
 This article incorporates text by Allyn C. Howlett, Brian F. Thomas, and John W. Huffman available under the CC BY 4.0 license.
This article incorporates text by Allyn C. Howlett, Brian F. Thomas, and John W. Huffman available under the CC BY 4.0 license.
- ↑ 119.0 119.1 119.2 119.3 119.4 119.5 119.6 Alzu'bi, A; Almahasneh, F; Khasawneh, R; Abu-El-Rub, E; Baker, WB; Al-Zoubi, RM (12 January 2024). "The synthetic cannabinoids menace: a review of health risks and toxicity". European journal of medical research. 29 (1): 49. doi:10.1186/s40001-023-01443-6. PMC 10785485. PMID 38216984.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Ayman Alzu'bi, Fatimah Almahasneh, Ramada Khasawneh, Ejlal Abu-El-Rub, Worood Bani Baker, and Raed M Al-Zoubi available under the CC BY 4.0 license.
This article incorporates text by Ayman Alzu'bi, Fatimah Almahasneh, Ramada Khasawneh, Ejlal Abu-El-Rub, Worood Bani Baker, and Raed M Al-Zoubi available under the CC BY 4.0 license.
- ↑ 120.0 120.1 Alves, Vera L.; Gonçalves, João L.; Aguiar, Joselin; Teixeira, Helena M.; Câmara, José S. (27 May 2020). "The synthetic cannabinoids phenomenon: from structure to toxicological properties. A review". Critical Reviews in Toxicology. 50 (5): 359–382. doi:10.1080/10408444.2020.1762539. PMID 32530350.
- ↑ Goyal, Hemant; Awad, Hamza H.; Ghali, Jalal K. (July 2017). "Role of cannabis in cardiovascular disorders". Journal of Thoracic Disease. 9 (7): 2079–2092. doi:10.21037/jtd.2017.06.104. PMC 5542986. PMID 28840009.
- ↑ 122.0 122.1 122.2 Luethi, Dino; Liechti, Matthias E. (April 2020). "Designer drugs: mechanism of action and adverse effects". Archives of Toxicology. 94 (4): 1085–1133. doi:10.1007/s00204-020-02693-7. PMC 7225206. PMID 32249347.
 This article incorporates text by Dino Luethi and Matthias E. Liechti available under the CC BY 4.0 license.
This article incorporates text by Dino Luethi and Matthias E. Liechti available under the CC BY 4.0 license.
- ↑ Salle, Sophie; Sevestre, Christelle; Richeval, Camille; Hakim, Florian; Allorge, Delphine; Gaulier, Jean-michel (July 2021). "Involuntary 5F-ADB-related intoxication following e-cigarette use". International Journal of Legal Medicine. 135 (4): 1467–1470. doi:10.1007/s00414-021-02561-8. PMID 33765158.
- ↑ 124.0 124.1 124.2 124.3 124.4 Gordon, Adam J.; Conley, James W.; Gordon, Joanne M. (December 2013). "Medical Consequences of Marijuana Use: A Review of Current Literature". Current Psychiatry Reports. 15 (12). doi:10.1007/s11920-013-0419-7. PMID 24234874.
- ↑ 125.0 125.1 Roehler, Douglas R.; Smith, Herschel; Radhakrishnan, Lakshmi; Holland, Kristin M.; Gates, Abigail L.; Vivolo-Kantor, Alana M.; Hoots, Brooke E. (14 July 2023). "Cannabis-Involved Emergency Department Visits Among Persons Aged". MMWR. Morbidity and Mortality Weekly Report. 72 (28): 758–765. doi:10.15585/mmwr.mm7228a1. PMC 10360609. PMID 37440436.
{{cite journal}}: Check|pmc=value (help) This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 126.0 126.1 126.2 126.3 126.4 126.5 126.6 "Emergency Department Visits Involving Marijuana among Adolescents Aged 15 to 17: Increase from 2005 to 2010 Varied by Gender" (PDF). Drug Abuse Warning Network. Substance Abuse and Mental Health Services Administration. 13 November 2012. p. 1.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 127.0 127.1 127.2 127.3 127.4 127.5 127.6 127.7 127.8 Lu, Stacy (23 October 2023). "Can science keep up with designer drugs?". National Institute on Drug Abuse.
- ↑ 128.0 128.1 128.2 128.3 128.4 128.5 128.6 128.7 Fattore, Liana; Fratta, Walter (2011). "Beyond THC: The New Generation of Cannabinoid Designer Drugs". Frontiers in Behavioral Neuroscience. 5. doi:10.3389/fnbeh.2011.00060. ISSN 1662-5153. PMC 3187647. PMID 2200716.
- ↑ Sajwani, Hawraa Sameer (March 2023). "The dilemma of new psychoactive substances: A growing threat". Saudi Pharmaceutical Journal. 31 (3): 348–350. doi:10.1016/j.jsps.2023.01.002. PMC 10071313. PMID 37026049.
{{cite journal}}: Check|pmc=value (help) - ↑ Feng, Ling-Yi; Li, Jih-Heng (July 2020). "New psychoactive substances in Taiwan: challenges and strategies". Current Opinion in Psychiatry. 33 (4): 306–311. doi:10.1097/YCO.0000000000000604. PMID 32167950.
- ↑ Baumann, MH (January 2016). "The Changing Face of Recreational Drug Use". Cerebrum : the Dana forum on brain science. 2016. PMC 4938259. PMID 27408674.
- ↑ 132.0 132.1 132.2 "Frequently Asked Questions - How is Marijuana Used?". Centers for Disease Control and Prevention. 11 June 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 133.0 133.1 133.2 133.3 133.4 133.5 Lyzwinski, Lynnette Nathalie; Naslund, John A.; Miller, Christopher J.; Eisenberg, Mark J. (11 April 2022). "Global youth vaping and respiratory health: epidemiology, interventions, and policies". npj Primary Care Respiratory Medicine. 32 (1): 14. doi:10.1038/s41533-022-00277-9. PMC 9001701. PMID 35410990.
 This article incorporates text by Lynnette Nathalie Lyzwinski, John A. Naslund, Christopher J. Miller, and Mark J. Eisenberg available under the CC BY 4.0 license.
This article incorporates text by Lynnette Nathalie Lyzwinski, John A. Naslund, Christopher J. Miller, and Mark J. Eisenberg available under the CC BY 4.0 license.
- ↑ 134.0 134.1 134.2 134.3 134.4 134.5 134.6 Preteroti, Matthew; Wilson, Emily T.; Eidelman, David H.; Baglole, Carolyn J. (28 March 2023). "Modulation of pulmonary immune function by inhaled cannabis products and consequences for lung disease". Respiratory Research. 24 (1). doi:10.1186/s12931-023-02399-1. PMC 10043545. PMID 36978106.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Matthew Preteroti, Emily T. Wilson, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
This article incorporates text by Matthew Preteroti, Emily T. Wilson, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
- ↑ 135.0 135.1 Henry, Travis S.; Kligerman, Seth J.; Raptis, Constantine A.; Mann, Howard; Sechrist, Jacob W.; Kanne, Jeffrey P. (2019). "Imaging Findings of Vaping-Associated Lung Injury". American Journal of Roentgenology: 1–8. doi:10.2214/AJR.19.22251. ISSN 0361-803X. PMID 31593518. S2CID 203985885.
- ↑ 136.00 136.01 136.02 136.03 136.04 136.05 136.06 136.07 136.08 136.09 136.10 136.11 136.12 136.13 136.14 136.15 136.16 136.17 Latif, Zara; Garg, Nadish (19 June 2020). "The Impact of Marijuana on the Cardiovascular System: A Review of the Most Common Cardiovascular Events Associated with Marijuana Use". Journal of Clinical Medicine. 9 (6): 1925. doi:10.3390/jcm9061925. PMC 7355963. PMID 32575540.
 This article incorporates text by Zara Latif and Nadish Garg available under the CC BY 4.0 license.
This article incorporates text by Zara Latif and Nadish Garg available under the CC BY 4.0 license.
- ↑ "Cannabis use linked to increase in heart attack and stroke risk". American Heart Association. 28 February 2024.
- ↑ 138.0 138.1 Desbois, Anne Claire; Cacoub, Patrice (October 2013). "Cannabis-Associated Arterial Disease". Annals of Vascular Surgery. 27 (7): 996–1005. doi:10.1016/j.avsg.2013.01.002. PMID 23850313.
- ↑ Fiessinger, Jean-Noel (2002). "Juvenile arteritis revisited". Pathophysiology of Haemostasis and Thrombosis. 32 (5–6): 295–298. doi:10.1159/000073584. PMID 13679660.
- ↑ 140.0 140.1 140.2 140.3 140.4 Peyrot, I; Garsaud, A‐M; Saint‐Cyr, I; Quitman, O; Sanchez, B; Quist, D (March 2007). "Cannabis arteritis: a new case report and a review of literature". Journal of the European Academy of Dermatology and Venereology. 21 (3): 388–391. doi:10.1111/j.1468-3083.2006.01947.x. PMID 17309465.
- ↑ 141.0 141.1 Pilitsi, Eleni; Kennamer, Brooke; Trepanowski, Nicole; Gonzalez, Reina; Trojanowski, Marcin; Phillips, Tania; Lam, Christina S. (July 2023). "Cannabis arteritis presenting with Raynaud's and digital ulcerations: a case-based review of a controversial thromboangiitis obliterans-like condition". Clinical Rheumatology. 42 (7): 1981–1985. doi:10.1007/s10067-023-06603-x. PMID 37097526.
- ↑ 142.0 142.1 Khattar, Neera; Routsolias, Joanne C. (May 2018). "Emergency Department Treatment of Cannabinoid Hyperemesis Syndrome: A Review". American Journal of Therapeutics. 25 (3): e357–e361. doi:10.1097/MJT.0000000000000655. PMID 28953512.
- ↑ Sontineni, Siva-P (2009). "Cannabinoid hyperemesis syndrome: Clinical diagnosis of an underrecognised manifestation of chronic cannabis abuse". World Journal of Gastroenterology. 15 (10): 1264. doi:10.3748/wjg.15.1264. PMC 2658859. PMID 19291829.
- ↑ 144.0 144.1 Sorensen, Cecilia J.; DeSanto, Kristen; Borgelt, Laura; Phillips, Kristina T.; Monte, Andrew A. (March 2017). "Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment—a Systematic Review". Journal of Medical Toxicology. 13 (1): 71–87. doi:10.1007/s13181-016-0595-z. PMC 5330965. PMID 28000146.
- ↑ 145.0 145.1 Senderovich, Helen; Patel, Preet; Jimenez Lopez, Briam; Waicus, Sarah (November 2022). "A Systematic Review on Cannabis Hyperemesis Syndrome and Its Management Options". Medical Principles and Practice. 31 (1): 29–38. doi:10.1159/000520417. PMC 8995641. PMID 34724666.
- ↑ Hudson, Roger; Rushlow, Walter; Laviolette, Steven R. (February 2018). "Phytocannabinoids modulate emotional memory processing through interactions with the ventral hippocampus and mesolimbic dopamine system: implications for neuropsychiatric pathology". Psychopharmacology. 235 (2): 447–458. doi:10.1007/s00213-017-4766-7. PMID 29063964.
- ↑ Meier, Ellen; Hatsukami, Dorothy K. (September 2016). "A review of the additive health risk of cannabis and tobacco co-use". Drug and Alcohol Dependence. 166: 6–12. doi:10.1016/j.drugalcdep.2016.07.013. PMID 27476751.
- ↑ 148.0 148.1 "U.S. Surgeon General's Advisory: Marijuana Use and the Developing Brain". United States Department of Health and Human Services. Surgeon General of the United States. 29 August 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 149.0 149.1 149.2 Shukla, Samarth; Doshi, Harshit (January 2024). "Marijuana and Maternal, Perinatal, and Neonatal Outcomes". StatPearls. StatPearls Publishing.
- ↑ 150.0 150.1 150.2 150.3 Solmi, Marco; De Toffol, Marco; Kim, Jong Yeob; Choi, Min Je; Stubbs, Brendon; Thompson, Trevor; Firth, Joseph; Miola, Alessandro; Croatto, Giovanni; Baggio, Francesca; Michelon, Silvia; Ballan, Luca; Gerdle, Björn; Monaco, Francesco; Simonato, Pierluigi; Scocco, Paolo; Ricca, Valdo; Castellini, Giovanni; Fornaro, Michele; Murru, Andrea; Vieta, Eduard; Fusar-Poli, Paolo; Barbui, Corrado; Ioannidis, John P A; Carvalho, Andrè F; Radua, Joaquim; Correll, Christoph U; Cortese, Samuele; Murray, Robin M; Castle, David; Shin, Jae Il; Dragioti, Elena (30 August 2023). "Balancing risks and benefits of cannabis use: umbrella review of meta-analyses of randomised controlled trials and observational studies". BMJ: e072348. doi:10.1136/bmj-2022-072348. PMC 10466434. PMID 37648266.
{{cite journal}}: Check|pmc=value (help) - ↑ 151.0 151.1 151.2 Testai, Fernando D.; Gorelick, Philip B.; Aparicio, Hugo J.; Filbey, Francesca M.; Gonzalez, Raul; Gottesman, Rebecca F.; Melis, Miriam; Piano, Mariann R.; Rubino, Tiziana; Song, Sarah Y. (April 2022). "Use of Marijuana: Effect on Brain Health: A Scientific Statement From the American Heart Association". Stroke. 53 (4). doi:10.1161/STR.0000000000000396. PMID 35142225.
- ↑ 152.0 152.1 152.2 152.3 152.4 "What We Know about Marijuana". Centers for Disease Control and Prevention. 1 March 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 153.0 153.1 153.2 153.3 153.4 153.5 153.6 153.7 153.8 Dash, Genevieve F; Holt, Laura; Kenyon, Emily A; Carter, Emily K; Ho, Diana; Hudson, Karen A; Feldstein Ewing, Sarah W (November 2022). "Detection of vaping, cannabis use, and hazardous prescription opioid use among adolescents". The Lancet Child & Adolescent Health. 6 (11): 820–828. doi:10.1016/S2352-4642(22)00212-7. PMC 9588707. PMID 36030794.
{{cite journal}}: Check|pmc=value (help) - ↑ 154.0 154.1 154.2 Bakshi, Chetna; Barrett, Allison M. (April 2019). "Impact of recreational and medicinal marijuana on surgical patients: A review". The American Journal of Surgery. 217 (4): 783–786. doi:10.1016/j.amjsurg.2018.10.053. PMID 30471810.
- ↑ Kallurkar, Anusha; Kaye, Alan D.; Shekoohi, Sahar (March 2024). "Marijuana Use, Vaping, and Preoperative Anesthetic and Surgical Considerations in Clinical Practice". Anesthesiology Clinics. 42 (1): 53–63. doi:10.1016/j.anclin.2023.09.001. PMID 38278592.
- ↑ 156.0 156.1 156.2 Lo, Jamie O.; Hedges, Jason C.; Girardi, Guillermina (October 2022). "Impact of cannabinoids on pregnancy, reproductive health, and offspring outcomes". American Journal of Obstetrics and Gynecology. 227 (4): 571–581. doi:10.1016/j.ajog.2022.05.056. PMC 9530020. PMID 35662548.
{{cite journal}}: Check|pmc=value (help) - ↑ "Marijuana Use Disorder/Cannabis Use Disorder". Centers for Disease Control and Prevention. 5 April 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 158.0 158.1 158.2 "Marijuana Use Disorder/Cannabis Use Disorder". Centers for Disease Control and Prevention. 19 October 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 159.0 159.1 159.2 159.3 159.4 159.5 159.6 159.7 159.8 "What You Should Know About Using Cannabis, Including CBD, When Pregnant or Breastfeeding". United States Food and Drug Administration. 16 October 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 160.0 160.1 Blohm, Eike; Sell, Peter; Neavyn, Mark (April 2019). "Cannabinoid toxicity in pediatrics". Current Opinion in Pediatrics. 31 (2): 256–261. doi:10.1097/MOP.0000000000000739. PMID 30694824.
- ↑ 161.0 161.1 161.2 161.3 161.4 161.5 "Cannabis (Marijuana) Concentrates DrugFacts". National Institute on Drug Abuse. 25 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 162.0 162.1 162.2 162.3 Efron, Daryl; Taylor, Kaitlyn (7 April 2023). "Medicinal Cannabis for Paediatric Developmental, Behavioural and Mental Health Disorders". International Journal of Environmental Research and Public Health. 20 (8): 5430. doi:10.3390/ijerph20085430. PMC 10138057. PMID 37107712.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Daryl Efron and Kaitlyn Taylor available under the CC BY 4.0 license.
This article incorporates text by Daryl Efron and Kaitlyn Taylor available under the CC BY 4.0 license.
- ↑ 163.0 163.1 163.2 163.3 Hartmann, Andreas; Andrén, Per; Atkinson-Clément, Cyril; Czernecki, Virginie; Delorme, Cécile; Monique Debes, Nanette Marinette; Müller-Vahl, Kirsten; Paschou, Peristera; Szejko, Natalia; Topaloudi, Apostolia; Ueda, Keisuke; Black, Kevin J. (23 October 2023). "Tourette syndrome research highlights from 2022". F1000Research. 12: 826. doi:10.12688/f1000research.135702.2. PMC 10483181. PMID 37691732.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Andreas Hartmann, Per Andrén, Cyril Atkinson-Clément, Virginie Czernecki, Cécile Delorme, Nanette Marinette Monique Debes, Kirsten Müller-Vahl, Peristera Paschou, Natalia Szejko, Apostolia Topaloudi, Keisuke Ueda, Kevin J Black available under the CC BY 4.0 license.
This article incorporates text by Andreas Hartmann, Per Andrén, Cyril Atkinson-Clément, Virginie Czernecki, Cécile Delorme, Nanette Marinette Monique Debes, Kirsten Müller-Vahl, Peristera Paschou, Natalia Szejko, Apostolia Topaloudi, Keisuke Ueda, Kevin J Black available under the CC BY 4.0 license.
- ↑ 164.0 164.1 Seideman, Mary F.; Seideman, Travis A. (1 June 2020). "A Review of the Current Treatment of Tourette Syndrome". The Journal of Pediatric Pharmacology and Therapeutics. 25 (5): 401–412. doi:10.5863/1551-6776-25.5.401. PMC 7337131. PMID 32641910.
- ↑ 165.0 165.1 165.2 165.3 165.4 165.5 165.6 165.7 165.8 Archie, Sabrina Rahman; Cucullo, Luca (30 May 2020). "Cerebrovascular and Neurological Dysfunction under the Threat of COVID-19: Is There a Comorbid Role for Smoking and Vaping?". International Journal of Molecular Sciences. 21 (11): 3916. doi:10.3390/ijms21113916. PMC 7312781. PMID 32486196.
 This article incorporates text by Sabrina Rahman Archie and Luca Cucullo available under the CC BY 4.0 license.
This article incorporates text by Sabrina Rahman Archie and Luca Cucullo available under the CC BY 4.0 license.
- ↑ 166.0 166.1 166.2 166.3 166.4 Zielińska, Aleksandra; Eder, Piotr; Karczewski, Jacek; Szalata, Marlena; Hryhorowicz, Szymon; Wielgus, Karolina; Szalata, Milena; Dobrowolska, Agnieszka; Atanasov, Atanas G.; Słomski, Ryszard; Souto, Eliana B. (22 March 2023). "Tocilizumab-coated solid lipid nanoparticles loaded with cannabidiol as a novel drug delivery strategy for treating COVID-19: A review". Frontiers in Immunology. 14. doi:10.3389/fimmu.2023.1147991. PMC 10073701. PMID 37033914.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Aleksandra Zielińska, Piotr Eder, Jacek Karczewski, Marlena Szalata, Szymon Hryhorowicz, Karolina Wielgus, Milena Szalata, Agnieszka Dobrowolska, Atanas G. Atanasov, Ryszard Słomski, and Eliana B. Souto available under the CC BY 4.0 license.
This article incorporates text by Aleksandra Zielińska, Piotr Eder, Jacek Karczewski, Marlena Szalata, Szymon Hryhorowicz, Karolina Wielgus, Milena Szalata, Agnieszka Dobrowolska, Atanas G. Atanasov, Ryszard Słomski, and Eliana B. Souto available under the CC BY 4.0 license.
- ↑ 167.0 167.1 167.2 Blundell, M S; Dargan, P I; Wood, D M (1 March 2018). "The dark cloud of recreational drugs and vaping". QJM: An International Journal of Medicine. 111 (3): 145–148. doi:10.1093/qjmed/hcx049. PMID 28339800.
- ↑ 168.0 168.1 168.2 168.3 Pratt, Misty; Stevens, Adrienne; Thuku, Micere; Butler, Claire; Skidmore, Becky; Wieland, L. Susan; Clemons, Mark; Kanji, Salmaan; Hutton, Brian (December 2019). "Benefits and harms of medical cannabis: a scoping review of systematic reviews". Systematic Reviews. 8 (1). doi:10.1186/s13643-019-1243-x. PMC 6905063. PMID 31823819.
 This article incorporates text by Misty Pratt, Adrienne Stevens, Micere Thuku, Claire Butler, Becky Skidmore, L Susan Wieland, Mark Clemons, Salmaan Kanji, and Brian Hutton available under the CC BY 4.0 license.
This article incorporates text by Misty Pratt, Adrienne Stevens, Micere Thuku, Claire Butler, Becky Skidmore, L Susan Wieland, Mark Clemons, Salmaan Kanji, and Brian Hutton available under the CC BY 4.0 license.
- ↑ 169.0 169.1 Filipiuc, Silviu-Iulian; Neagu, Anca-Narcisa; Uritu, Cristina Mariana; Tamba, Bogdan-Ionel; Filipiuc, Leontina-Elena; Tudorancea, Ivona Maria; Boca, Andreea Nicoleta; Hâncu, Mădălina Florina; Porumb, Vlad; Bild, Walther (24 July 2023). "The Skin and Natural Cannabinoids–Topical and Transdermal Applications". Pharmaceuticals. 16 (7): 1049. doi:10.3390/ph16071049. PMC 10386449. PMID 37513960.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Silviu-Iulian Filipiuc, Anca-Narcisa Neagu, Cristina Mariana Uritu, Bogdan-Ionel Tamba, Leontina-Elena Filipiuc, Ivona Maria Tudorancea, Andreea Nicoleta Boca, Mădălina Florina Hâncu, Vlad Porumb, and Walther Bild available under the CC BY 4.0 license.
This article incorporates text by Silviu-Iulian Filipiuc, Anca-Narcisa Neagu, Cristina Mariana Uritu, Bogdan-Ionel Tamba, Leontina-Elena Filipiuc, Ivona Maria Tudorancea, Andreea Nicoleta Boca, Mădălina Florina Hâncu, Vlad Porumb, and Walther Bild available under the CC BY 4.0 license.
- ↑ Le, Kelvin; Au, Joanne; Hua, Jean; Le, Khang Duy Ricky (16 December 2023). "The Therapeutic Potential of Cannabidiol in Revolutionising Opioid Use Disorder Management". Cureus. doi:10.7759/cureus.50634. PMC 10789504. PMID 38226097.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Kelvin Le, Joanne Au, Jean Hua, and Khang Duy Ricky Le available under the CC BY 4.0 license.
This article incorporates text by Kelvin Le, Joanne Au, Jean Hua, and Khang Duy Ricky Le available under the CC BY 4.0 license.
- ↑ Joshi, Manish; Joshi, Anita; Bartter, Thaddeus (March 2014). "Marijuana and lung diseases:". Current Opinion in Pulmonary Medicine. 20 (2): 173–179. doi:10.1097/MCP.0000000000000026. PMID 24384575.
- ↑ 172.0 172.1 Sarris, Jerome; Sinclair, Justin; Karamacoska, Diana; Davidson, Maggie; Firth, Joseph (December 2020). "Medicinal cannabis for psychiatric disorders: a clinically-focused systematic review". BMC Psychiatry. 20 (1). doi:10.1186/s12888-019-2409-8. PMC 6966847. PMID 31948424.
 This article incorporates text by Jerome Sarris, Justin Sinclair, Diana Karamacoska, Maggie Davidson, and Joseph Firth available under the CC BY 4.0 license.
This article incorporates text by Jerome Sarris, Justin Sinclair, Diana Karamacoska, Maggie Davidson, and Joseph Firth available under the CC BY 4.0 license.
- ↑ 173.0 173.1 173.2 "Driving". Centers for Disease Control and Prevention. 19 October 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 174.0 174.1 174.2 174.3 174.4 Sund, Lachlan J.; Dargan, Paul I.; Archer, John R. H.; Wood, David M. (1 February 2023). "E-cigarette or vaping-associated lung injury (EVALI): a review of international case reports from outside the United States of America". Clinical Toxicology. 61 (2): 91–97. doi:10.1080/15563650.2022.2160342. PMID 36636876.
- ↑ Cherian, Sujith V.; Kumar, Anupam; Estrada-Y-Martin, Rosa M. (2020). "E-Cigarette or Vaping Product-Associated Lung Injury: A Review". The American Journal of Medicine. 133 (6): 657–663. doi:10.1016/j.amjmed.2020.02.004. ISSN 0002-9343. PMID 32179055.
- ↑ 176.0 176.1 176.2 176.3 Gotts, Jeffrey E; Jordt, Sven-Eric; McConnell, Rob; Tarran, Robert (2019). "What are the respiratory effects of e-cigarettes?". BMJ. 366: l5275. doi:10.1136/bmj.l5275. ISSN 0959-8138. PMID 31570493.
- ↑ Schupp, J. C.; Prasse, A.; Erythropel, H. C. (February 2020). "E-Zigaretten – Funktionsweise, Inhaltsstoffe und die Vaping-assoziierte akute Lungenschädigung" [E-Cigarettes - Operating Principle, Ingredients, and Associated Acute Lung Injury]. Pneumologie (in Deutsch). 74 (02): 77–87. doi:10.1055/a-1078-8126. ISSN 0934-8387. PMC 7366312. PMID 32016924.
- ↑ 178.0 178.1 Striley, Catherine W.; Nutley, Sara K. (July 2020). "World vaping update". Current Opinion in Psychiatry. 33 (4): 360–368. doi:10.1097/YCO.0000000000000617. PMID 32398544.
- ↑ 179.0 179.1 179.2 179.3 179.4 "Frequently Asked Questions". Centers for Disease Control and Prevention. 1 December 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Rebuli, Meghan E.; Rose, Jason J.; Noël, Alexandra; Croft, Daniel P.; Benowitz, Neal L.; Cohen, Alan H.; Goniewicz, Maciej L.; Larsen, Brandon T.; Leigh, Noel; McGraw, Matthew D.; Melzer, Anne C.; Penn, Arthur L.; Rahman, Irfan; Upson, Dona; Crotty Alexander, Laura E.; Ewart, Gary; Jaspers, Ilona; Jordt, Sven Eric; Kligerman, Seth; Loughlin, Ceila E.; McConnell, Rob; Neptune, Enid R.; Nguyen, Tran B.; Pinkerton, Kent E.; Witek, Theodore J. (January 2023). "The E-cigarette or Vaping Product Use–Associated Lung Injury Epidemic: Pathogenesis, Management, and Future Directions: An Official American Thoracic Society Workshop Report". Annals of the American Thoracic Society. 20 (1): 1–17. doi:10.1513/AnnalsATS.202209-796ST. PMC 9819258. PMID 36584985.
{{cite journal}}: Check|pmc=value (help) - ↑ 181.0 181.1 Roberts, Emmert; Copeland, Caroline; Robson, Deborah; McNeill, Ann (October 2021). "Drug‐related deaths associated with vaping product use in the United Kingdom". Addiction. 116 (10): 2908–2911. doi:10.1111/add.15468. PMID 33751729.
- ↑ 182.0 182.1 Priemer, David S.; Gravenmier, Curtis; Batouli, Amir; Hooper, Jody E. (1 November 2020). "Overview of Pathologic Findings of Vaping in the Context of an Autopsy Patient With Chronic Injury". Archives of Pathology & Laboratory Medicine. 144 (11): 1408–1413. doi:10.5858/arpa.2019-0637-RA. PMID 32383974.
- ↑ 183.0 183.1 "Synthetic Cannabinoids". National Institute on Drug Abuse. October 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Schlag, Anne K; Hindocha, Chandni; Zafar, Rayyan; Nutt, David J; Curran, H Valerie (July 2021). "Cannabis based medicines and cannabis dependence: A critical review of issues and evidence". Journal of Psychopharmacology. 35 (7): 773–785. doi:10.1177/0269881120986393. PMC 8278552. PMID 33593117.
 This article incorporates text by Anne K Schlag, Chandni Hindocha, Rayyan Zafar, David J Nutt, and H Valerie Curran3 available under the CC BY 4.0 license.
This article incorporates text by Anne K Schlag, Chandni Hindocha, Rayyan Zafar, David J Nutt, and H Valerie Curran3 available under the CC BY 4.0 license.
- ↑ Sherman, Brian J.; McRae‐Clark, Aimee L. (May 2016). "Treatment of Cannabis Use Disorder: Current Science and Future Outlook". Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 36 (5): 511–535. doi:10.1002/phar.1747. PMC 4880536. PMID 27027272.
- ↑ 186.0 186.1 Danovitch, Itai; Gorelick, David A. (June 2012). "State of the Art Treatments for Cannabis Dependence". Psychiatric Clinics of North America. 35 (2): 309–326. doi:10.1016/j.psc.2012.03.003. PMC 3371269. PMID 22640758.
- ↑ "Is marijuana addictive?". National Institute on Drug Abuse. July 2020.
- ↑ Curran, H. Valerie; Freeman, Tom P.; Mokrysz, Claire; Lewis, David A.; Morgan, Celia J. A.; Parsons, Loren H. (May 2016). "Keep off the grass? Cannabis, cognition and addiction". Nature Reviews Neuroscience. 17 (5): 293–306. doi:10.1038/nrn.2016.28. PMID 27052382.
- ↑ 189.0 189.1 189.2 Aletraris, Lydia; Graves, Brian D.; Ndung’u, Joyce J. (10 April 2023). "Assessing the Impact of Recreational Cannabis Legalization on Cannabis Use Disorder and Admissions to Treatment in the United States". Current Addiction Reports. 10 (2): 198–209. doi:10.1007/s40429-023-00470-x. PMC 10088679. PMID 37266190.
{{cite journal}}: Check|pmc=value (help) - ↑ Vandrey, Ryan; Haney, Margaret (July 2009). "Pharmacotherapy for Cannabis Dependence: How Close Are We?". CNS Drugs. 23 (7): 543–553. doi:10.2165/00023210-200923070-00001. PMC 2729499. PMID 19552483.
- ↑ Benyamina, Amine; Lecacheux, Marie; Blecha, Lisa; Reynaud, Michel; Lukasiewcz, Michael (March 2008). "Pharmacotherapy and psychotherapy in cannabis withdrawal and dependence". Expert Review of Neurotherapeutics. 8 (3): 479–491. doi:10.1586/14737175.8.3.479. PMID 18345976.
- ↑ Barnes, Courtney; Turon, Heidi; McCrabb, Sam; Hodder, Rebecca K; Yoong, Sze Lin; Stockings, Emily; Hall, Alix E; Bialek, Caitlin; Morrison, Jacob L; Wolfenden, Luke (15 November 2023). "Interventions to prevent or cease electronic cigarette use in children and adolescents". Cochrane Database of Systematic Reviews. 2023 (12). doi:10.1002/14651858.CD015511.pub2. PMC 10646968. PMID 37965949.
{{cite journal}}: Check|pmc=value (help) - ↑ Kundu, Anasua; Kouzoukas, Erika; Zawertailo, Laurie; Fougere, Chantal; Dragonetti, Rosa; Selby, Peter; Schwartz, Robert (March 2023). "Scoping review of guidance on cessation interventions for electronic cigarettes and dual electronic and combustible cigarettes use". CMAJ Open. 11 (2): E336–E344. doi:10.9778/cmajo.20210325. PMC 10118292. PMID 37072138.
{{cite journal}}: Check|pmc=value (help) - ↑ Skolnick, Phil; Crystal, Roger (February 2020). "Cannabinoid1 (CB-1) receptor antagonists: a molecular approach to treating acute cannabinoid overdose". Journal of Neural Transmission. 127 (2): 279–286. doi:10.1007/s00702-019-02132-7. PMID 31893308.
 This article incorporates text by Phil Skolnick and Roger Crystal available under the CC BY 4.0 license.
This article incorporates text by Phil Skolnick and Roger Crystal available under the CC BY 4.0 license.
- ↑ Ghosh, Moyukh; Naderi, Sahar (June 2019). "Cannabis and Cardiovascular Disease". Current Atherosclerosis Reports. 21 (6). doi:10.1007/s11883-019-0783-9. PMID 30980200.
- ↑ 196.0 196.1 Bourque, Josiane; Potvin, Stéphane (10 June 2021). "Cannabis and Cognitive Functioning: From Acute to Residual Effects, From Randomized Controlled Trials to Prospective Designs". Frontiers in Psychiatry. 12. doi:10.3389/fpsyt.2021.596601. PMC 8222623. PMID 34177633.
 This article incorporates text by Josiane Bourque1 and Stéphane Potvin available under the CC BY 4.0 license.
This article incorporates text by Josiane Bourque1 and Stéphane Potvin available under the CC BY 4.0 license.
- ↑ 197.0 197.1 DeFilippis, Ersilia M.; Bajaj, Navkaranbir S.; Singh, Amitoj; Malloy, Rhynn; Givertz, Michael M.; Blankstein, Ron; Bhatt, Deepak L.; Vaduganathan, Muthiah (January 2020). "Marijuana Use in Patients With Cardiovascular Disease". Journal of the American College of Cardiology. 75 (3): 320–332. doi:10.1016/j.jacc.2019.11.025. PMID 31976871.
- ↑ Nieddu, Maria; Baralla, Elena; Pasciu, Valeria; Rimoli, Maria Grazia; Boatto, Gianpiero (September 2022). "Cross-reactivity of commercial immunoassays for screening of new amphetamine designer drugs. A review". Journal of Pharmaceutical and Biomedical Analysis. 218: 114868. doi:10.1016/j.jpba.2022.114868. PMID 35688007.
- ↑ Hadland, Scott E.; Harris, Sion K. (August 2014). "Youth marijuana use: state of the science for the practicing clinician". Current Opinion in Pediatrics. 26 (4): 420–427. doi:10.1097/MOP.0000000000000114. PMC 4138809. PMID 24914878.
- ↑ "Therapeutic Use of Marijuana". American Association of Nurse Practitioners. 2022.
- ↑ Budney, Alan J.; Sargent, James D.; Lee, Dustin C. (November 2015). "Vaping cannabis (marijuana): parallel concerns to e‐cigs?". Addiction. 110 (11): 1699–1704. doi:10.1111/add.13036. PMC 4860523. PMID 26264448.
- ↑ 202.0 202.1 Gilley, Meghan; Beno, Suzanne (June 2020). "Vaping implications for children and youth". Current Opinion in Pediatrics. 32 (3): 343–348. doi:10.1097/MOP.0000000000000889. ISSN 1040-8703. PMID 32332326.
- ↑ 203.0 203.1 Civiletto, Cody W.; Hutchison, Julia (January 2024). "Electronic Vaping Delivery Of Cannabis And Nicotine". StatPearls. StatPearls Publishing. PMID 31424744.
- ↑ Thirión-Romero, Ireri; Pérez-Padilla, Rogelio; Zabert, Gustavo; Barrientos-Gutiérrez, Inti (2019). "Respiratory Impact of Electronic Cigarettes and Low-Risk Tobacco". Revista de Investigación Clínica. 71 (1). doi:10.24875/RIC.18002616. ISSN 0034-8376. PMID 30810544.
- ↑ Poole, Steven (25 November 2014). "Vape is the new selfie: what the 2014 word of the year says about our times". The Guardian.
- ↑ 206.0 206.1 Meehan-Atrash, Jiries; Rahman, Irfan (18 October 2021). "Cannabis Vaping: Existing and Emerging Modalities, Chemistry, and Pulmonary Toxicology". Chemical Research in Toxicology. 34 (10): 2169–2179. doi:10.1021/acs.chemrestox.1c00290. PMC 8882064. PMID 34622654.
- ↑ Noah Charney (7 December 2014). "America's vaping revolution: How suspicious should we really be of the e-cigarette craze?". Salon (website).
- ↑ "JUUL copycats are flooding the e-cigarette market". Truth Initiative. August 8, 2018.
- ↑ Jackler, Robert K; Ramamurthi, Divya (2019). "Nicotine arms race: JUUL and the high-nicotine product market". Tobacco Control. 28 (6): tobaccocontrol–2018–054796. doi:10.1136/tobaccocontrol-2018-054796. ISSN 0964-4563. PMID 30733312.
- ↑ Walley, Susan C.; Wilson, Karen M.; Winickoff, Jonathan P.; Groner, Judith (2019). "A Public Health Crisis: Electronic Cigarettes, Vape, and JUUL". Pediatrics. 143 (6): e20182741. doi:10.1542/peds.2018-2741. ISSN 0031-4005. PMID 31122947.
- ↑ "Trump Administration Combating Epidemic of Youth E-Cigarette Use with Plan to Clear Market of Unauthorized, Non-Tobacco-Flavored E-Cigarette Products". United States Food and Drug Administration. 11 September 2019.
- ↑ 212.0 212.1 212.2 Perrone, Matthew (26 June 2023). "Thousands of unauthorized vapes are pouring into the US despite the FDA crackdown on fruity flavors". AP News.
- ↑ 213.0 213.1 213.2 Mannekote Thippaiah, Srinagesh; Iyengar, Sloka S.; Vinod, K. Yaragudri (23 April 2021). "Exo- and Endo-cannabinoids in Depressive and Suicidal Behaviors". Frontiers in Psychiatry. 12. doi:10.3389/fpsyt.2021.636228. PMC 8102729. PMID 33967855.
 This article incorporates text by Srinagesh Mannekote Thippaiah, Sloka S. Iyengar, and K. Yaragudri Vinod available under the CC BY 4.0 license.
This article incorporates text by Srinagesh Mannekote Thippaiah, Sloka S. Iyengar, and K. Yaragudri Vinod available under the CC BY 4.0 license.
- ↑ Pisanti, S.; Bifulco, M. (June 2019). "Medical Cannabis : A plurimillennial history of an evergreen". Journal of Cellular Physiology. 234 (6): 8342–8351. doi:10.1002/jcp.27725. PMID 30417354.
- ↑ Crocq, Marc-Antoine (30 September 2020). "History of cannabis and the endocannabinoid system". Dialogues in Clinical Neuroscience. 22 (3): 223–228. doi:10.31887/DCNS.2020.22.3/mcrocq. PMC 7605027. PMID 33162765.
- ↑ Singh, Kuldeep; Bhushan, Bharat; Chanchal, Dilip Kumar; Sharma, Satish Kumar; Rani, Ketki; Yadav, Manoj Kumar; Porwal, Prateek; Kumar, Shivendra; Sharma, Ashwani; Virmani, Tarun; Kumar, Girish; Noman, Abdullah Al (12 October 2023). "Emerging Therapeutic Potential of Cannabidiol (CBD) in Neurological Disorders: A Comprehensive Review". Behavioural Neurology. 2023: 1–17. doi:10.1155/2023/8825358. PMC 10586905. PMID 37868743.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Kuldeep Singh, Bharat Bhushan, Dilip Kumar Chanchal, Satish Kumar Sharma, Ketki Rani, Manoj Kumar Yadav, Prateek Porwal, Shivendra Kumar, Ashwani Sharma, Tarun Virmani, Girish Kumar, and Abdullah Al Noman available under the CC BY 4.0 license.
This article incorporates text by Kuldeep Singh, Bharat Bhushan, Dilip Kumar Chanchal, Satish Kumar Sharma, Ketki Rani, Manoj Kumar Yadav, Prateek Porwal, Shivendra Kumar, Ashwani Sharma, Tarun Virmani, Girish Kumar, and Abdullah Al Noman available under the CC BY 4.0 license.
- ↑ Krüger, Marlize; van Eeden, Tertia; Beswa, Daniso (1 December 2022). "Cannabis sativa Cannabinoids as Functional Ingredients in Snack Foods—Historical and Developmental Aspects". Plants. 11 (23): 3330. doi:10.3390/plants11233330. PMC 9739163. PMID 36501366.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Marlize Krüger, Tertia van Eeden, and Daniso Beswa available under the CC BY 4.0 license.
This article incorporates text by Marlize Krüger, Tertia van Eeden, and Daniso Beswa available under the CC BY 4.0 license.
- ↑ Bobrow, Warren (13 August 2019). "Chris Folkerts, CEO Of Grenco Science Digs Deeply Into Five Questions". Forbes.
- ↑ Khan, Jamila (29 December 2023). "7 Best THC Vape Pens in 2024: Shop Refillable & Disposable Weed Pens". The Sacramento Bee.
- ↑ 220.0 220.1 220.2 220.3 Dewhirst, Timothy (May 2023). "'Beyond nicotine' marketing strategies: Big Tobacco diversification into the vaping and cannabis product sectors". Tobacco Control. 32 (3): 402–404. doi:10.1136/tobaccocontrol-2021-056798. PMID 34511407.
- ↑ Sabaghi, Dario (2 August 2021). "Why Cannabis Is Part Of The Future Of Big Tobacco". Forbes.
- ↑ 222.0 222.1 222.2 222.3 222.4 222.5 Sabaghi, Dario (20 July 2023). "Philip Morris To Acquire Israeli Cannabis Inhaler Company Syqe Medical For Up To $650 Million". Forbes.
- ↑ 223.0 223.1 "Auxly Cannabis signs $123M deal with tobacco giant Imperial Brands". CBC.ca. The Canadian Press. 25 July 2019.
- ↑ 224.0 224.1 "BAT Invests in Charlotte's Web". Tobacco Reporter. 14 November 2022.
- ↑ Gelsi, Steve (November 2022). "Charlotte's Web gets investment from British American Tobacco". MarketWatch.
- ↑ Boehnke, Kevin F.; Wu, Christopher L.; Clauw, Daniel J. (January 2024). "Thoughtfully Integrating Cannabis Products Into Chronic Pain Treatment". Anesthesia & Analgesia. 138 (1): 5–15. doi:10.1213/ANE.0000000000005904. PMC 10730114. PMID 38100797.
{{cite journal}}: Check|pmc=value (help) - ↑ "Under the influence: NIH research shows teen vaping, social pressure on the rise". NIH MedlinePlus Magazine. National Institute on Drug Abuse. United States National Library of Medicine. 5 November 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Tadlock, Collin (7 April 2023). "Cannabis sales have buyers, sellers on a different high". The Charlotte Post.
- ↑ Lopez, German (19 April 2019). "4/20, the marijuana holiday, explained". Vox.
- ↑ Hughes, Mark (20 April 2022). "The 20 Best Films To Celebrate 420 With On April 20". Forbes.
- ↑ Kaufman, Anna (19 April 2023). "Happy 4/20! How a group of teens getting high spawned a global cannabis-lovers event". USA Today.
- ↑ 232.0 232.1 232.2 232.3 232.4 232.5 232.6 Borodovsky, Jacob T.; Sofis, Michael J.; Grucza, Richard A.; Budney, Alan J. (February 2021). "The importance of psychology for shaping legal cannabis regulation". Experimental and Clinical Psychopharmacology. 29 (1): 99–115. doi:10.1037/pha0000362. PMC 7679279. PMID 32437193.
- ↑ 233.0 233.1 Caputi, Theodore L. (January 2022). "The Use of Academic Research in Medical Cannabis Marketing: A Qualitative and Quantitative Review of Company Websites". Journal of Studies on Alcohol and Drugs. 83 (1): 5–17. doi:10.15288/jsad.2022.83.5. PMID 35040755.
- ↑ Adams, Benjamin (9 November 2022). "Charlotte's Web Scores Pivotal CBD Deal With Major League Baseball". Forbes.
- ↑ Brooks, Khristopher J. (12 October 2022). "Major League Baseball teams with CBD company in $30 million partnership". CBS News.
- ↑ 236.0 236.1 236.2 "FDA Regulation of Cannabis and Cannabis-Derived Products, Including Cannabidiol (CBD)". United States Food and Drug Administration. 28 September 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Vashi, Sonam (26 September 2012). "K2 Trend Not Slowing Down". Eyewitness News. WebMD.
- ↑ Martin, Alyson (7 February 2021). "Altria, Maker of Marlboro Cigarettes, Is Lobbying on Cannabis Sales in Virginia". Cannabis Wire.
- ↑ Roberts, Chris (9 February 2021). "How Tobacco Giant Altria Is Becoming A Cannabis Company". Forbes.
- ↑ George-Cosh, David (28 January 2022). "Cannabis Canada Weekly: Lobbying Ottawa ahead of the Cannabis Act review; Stocks suffer decline". BNN Bloomberg.
- ↑ Kerr, Andrew (2 August 2022). "Green industry: Inside the big business of marijuana legalization". Washington Examiner.
- ↑ Powell, Anita (16 November 2018). "South Africa Cannabis Ruling Leads to Pot-Themed Products". VOA News.
- ↑ 243.0 243.1 Reiter, Anna; Hébert-Losier, Andréa; Mylocopos, Genevieve; Filion, Kristian B.; Windle, Sarah B.; O'Loughlin, Jennifer L.; Grad, Roland; Eisenberg, Mark J. (January 2024). "Regulatory Strategies for Preventing and Reducing Nicotine Vaping Among Youth: A Systematic Review". American Journal of Preventive Medicine. 66 (1): 169–181. doi:10.1016/j.amepre.2023.08.002. PMID 37553038.
- ↑ Hill, Kevin P.; Palastro, Matthew D. (25 October 2017). "Medical cannabis for the treatment of chronic pain and other disorders: misconceptions and facts". Polish Archives of Internal Medicine. doi:10.20452/pamw.4123. PMID 29067992.
- ↑ Patel, J; Marwaha, R (January 2024). Cannabis Use Disorder. StatPearls Publishing. PMID 30844158.
- ↑ Kitchen, Chenai; Kabba, John Alimamy; Fang, Yu (1 June 2022). "Status and Impacts of Recreational and Medicinal Cannabis Policies in Africa: A Systematic Review and Thematic Analysis of Published and "Gray" Literature". Cannabis and Cannabinoid Research. 7 (3): 239–261. doi:10.1089/can.2021.0110. PMC 9225416. PMID 34986005.
- ↑ 247.0 247.1 "Drug licensing factsheet: cannabis, CBD and other cannabinoids". UK government. 17 June 2020.
 Text was copied from this source, which is available under an Open Government Licence v3.0. © Crown copyright.
Text was copied from this source, which is available under an Open Government Licence v3.0. © Crown copyright.
- ↑ Schlag, Anne Katrin; Baldwin, David S; Barnes, Michael; Bazire, Steve; Coathup, Rachel; Curran, HValerie; McShane, Rupert; Phillips, LawrenceD; Singh, Ilina; Nutt, David J (September 2020). "Medical cannabis in the UK: From principle to practice". Journal of Psychopharmacology. 34 (9): 931–937. doi:10.1177/0269881120926677. PMC 7436434. PMID 32522058.
- ↑ 249.0 249.1 249.2 249.3 Brar, Kamalpreet Kaur; Raheja, Yashika; Chadha, Bhupinder Singh; Magdouli, Sara; Brar, Satinder Kaur; Yang, Yung-Hun; Bhatia, Shashi Kant; Koubaa, Ahmed (February 2024). "A paradigm shift towards production of sustainable bioenergy and advanced products from Cannabis/hemp biomass in Canada". Biomass Conversion and Biorefinery. 14 (3): 3161–3182. doi:10.1007/s13399-022-02570-6. PMC 8934023. PMID 35342682.
- ↑ Hendlin, Yogi Hale; Bialous, Stella A. (January 2020). "The environmental externalities of tobacco manufacturing: A review of tobacco industry reporting". Ambio. 49 (1): 17–34. doi:10.1007/s13280-019-01148-3. PMC 6889105. PMID 30852780.
- ↑ Jones, Nicole S.; Comparin, Jeffrey H. (2020). "Interpol review of controlled substances 2016–2019". Forensic Science International: Synergy. 2: 608–669. doi:10.1016/j.fsisyn.2020.01.019. PMC 7770462. PMID 33385148.
- ↑ Liu, Jiangtao; Nabavizadeh, Pooneh; Rao, Poonam; Derakhshandeh, Ronak; Han, Daniel D.; Guo, Raymond; Murphy, Morgan B.; Cheng, Jing; Schick, Suzaynn F.; Springer, Matthew L. (5 December 2023). "Impairment of Endothelial Function by Aerosol From Marijuana Leaf Vaporizers". Journal of the American Heart Association. 12 (23). doi:10.1161/JAHA.123.032969. PMC 10727338. PMID 38014661.
{{cite journal}}: Check|pmc=value (help) - ↑ 253.0 253.1 "Understanding Vaping and Other Tobacco Product Use Among Youth" (PDF). Centers for Disease Control and Prevention. September 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Virgili, Fabrizio; Nenna, Raffaella; Ben David, Shira; Mancino, Enrica; Di Mattia, Greta; Matera, Luigi; Petrarca, Laura; Midulla, Fabio (December 2022). "E-cigarettes and youth: an unresolved Public Health concern". Italian Journal of Pediatrics. 48 (1): 97. doi:10.1186/s13052-022-01286-7. PMC 9194784. PMID 35701844.
- ↑ Jankowski, Mateusz; Brożek, Grzegorz; Lawson, Joshua; Skoczyński, Szymon; Zejda, Jan (2017). "E-smoking: Emerging public health problem?". International Journal of Occupational Medicine and Environmental Health. 30 (3): 329–344. doi:10.13075/ijomeh.1896.01046. ISSN 1232-1087. PMID 28481369.
- ↑ Besaratinia, Ahmad; Tommasi, Stella (July 2020). "Vaping epidemic: challenges and opportunities". Cancer Causes & Control. 31 (7): 663–667. doi:10.1007/s10552-020-01307-y. ISSN 0957-5243. PMC 7274878. PMID 32363571.
- ↑ 257.0 257.1 Rei, Joshua L. (March 2020). "The nephrologist's guide to cannabis and cannabinoids". Current Opinion in Nephrology and Hypertension. 29 (2): 248–257. doi:10.1097/MNH.0000000000000590. PMC 7012334. PMID 31972598.
- ↑ "What is marijuana". National Institute on Drug Abuse. July 2020.
- ↑ Ladha, Karim S.; Manoo, Varuna; Virji, Ali-Faizan; Hanlon, John G.; Mclaren-Blades, Alexander; Goel, Akash; Wijeysundera, Duminda N.; Kotra, Lakshmi P.; Ibarra, Carlos; Englesakis, Marina; Clarke, Hance (1 December 2019). "The Impact of Perioperative Cannabis Use: A Narrative Scoping Review". Cannabis and Cannabinoid Research. 4 (4): 219–230. doi:10.1089/can.2019.0054. PMC 6922064. PMID 31872058.
- ↑ Hourani, Wafa; Alexander, Stephen P. H. (January 2018). "Cannabinoid ligands, receptors and enzymes: Pharmacological tools and therapeutic potential". Brain and Neuroscience Advances. 2: 239821281878390. doi:10.1177/2398212818783908. PMC 7058259. PMID 32166144.
- ↑ 261.0 261.1 de Oliveira, Mariana Campello; Vides, Mariana Capelo; Lassi, Dângela Layne Silva; Torales, Julio; Ventriglio, Antonio; Bombana, Henrique Silva; Leyton, Vilma; Périco, Cintia de Azevedo-Marques; Negrão, André Brooking; Malbergier, André; Castaldelli-Maia, João Maurício (24 June 2023). "Toxicity of Synthetic Cannabinoids in K2/Spice: A Systematic Review". Brain Sciences. 13 (7): 990. doi:10.3390/brainsci13070990. PMC 10377539. PMID 37508922.
{{cite journal}}: Check|pmc=value (help) - ↑ 262.0 262.1 Tatusov, Michael; Mazer-Amirshahi, Maryann; Nelson, Lewis; Pines, Jesse (23 October 2015). "6 Things Every EP Needs to Know About K2/Spice & the Synthetic Cannabinoid Epidemic". Emergency Physicians Monthly.
- ↑ 263.0 263.1 "Synthetic Marijuana – K2 or Spice Fact Sheet" (PDF). Michigan Department of Health and Human Services.
- ↑ Seely, Kathryn A.; Lapoint, Jeff; Moran, Jeffery H.; Fattore, Liana (December 2012). "Spice drugs are more than harmless herbal blends: A review of the pharmacology and toxicology of synthetic cannabinoids". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 39 (2): 234–243. doi:10.1016/j.pnpbp.2012.04.017. PMC 3936256. PMID 22561602.
- ↑ Kumar, Sachil; Baggi, Tulsidas R. (March 2022). "Analytical Methods for Herbal Products Containing Synthetic Cannabinoids: A Review". Forensic Chemistry. 27: 100396. doi:10.1016/j.forc.2021.100396.
- ↑ "Acute kidney injury associated with synthetic cannabinoid use--multiple states, 2012". MMWR. Morbidity and mortality weekly report. 62 (6): 93–8. 15 February 2013. PMC 4604808. PMID 23407124.
- ↑ "What You Should Knowe about K2/Spice" (PDF). Drug Enforcement Administration. January 2014.
- ↑ "Drug Fact Sheet: K2/Spice" (PDF). Drug Enforcement Administration. April 2020.
- ↑ Shulman, Sophie (18 July 2023). "Philip Morris acquiring Cannabis inhaler developer Syqe Medical for up to $650 million". Calcalist.
- ↑ "Vectura: Marlboro giant seals takeover of UK inhaler firm". BBC News. 16 September 2021.
External links
- Pages using duplicate arguments in template calls
- Pages with broken file links
- Pages using image frame with unknown parameters
- Cannabis and health
- Cannabis cultivation
- Cannabis industry
- Tobacco industry
- Environmental impact of agriculture
- Electronic cigarettes
- Cigarette types
- Chinese inventions
- Smoking cessation
- Effects of psychoactive drugs
- Substance dependence
- Substance-related disorders
- Non-tobacco nicotine products
- Electronic cigarette aerosol carcinogens
- IARC Group 1 carcinogens
- Articles containing video clips


