Opioid overdose
| Opioid overdose | |
|---|---|
| Other names: Narcotic overdose, opioid poisoning | |
 | |
| A naloxone kit as distributed in British Columbia, Canada | |
| Specialty | Emergency medicine |
| Symptoms | Insufficient breathing, small pupils, unconsciousness[1] |
| Complications | Rhabdomyolysis, pulmonary edema, compartment syndrome, permanent brain damage[2][3] |
| Causes | Opioids (morphine, heroin, fentanyl, tramadol, methadone)[1][4] |
| Risk factors | Opioid dependence, use of high doses of opioids, injection of opioids, use with alcohol, benzodiazepines, or cocaine.[1][5] |
| Diagnostic method | Based on symptoms[3] |
| Differential diagnosis | Low blood sugar, alcohol intoxication, head trauma, stroke[6] |
| Prevention | Improved access to naloxone, treatment of opioid dependence[1] |
| Treatment | Supporting a person's breathing, naloxone[7] |
| Deaths | 122,100 (2015)[8] |
An opioid overdose is toxicity due to excessive opioids.[9][3] Examples of opioids include morphine, heroin, fentanyl, tramadol, and methadone.[1][4] Symptoms include insufficient breathing, small pupils, and unconsciousness.[1] Onset of symptoms depends in part on the route by which the opioids are taken.[10] Among those who initially survive, complications can include rhabdomyolysis, pulmonary edema, compartment syndrome, and permanent brain damage.[2][3]
Risk factors for opioid overdose include opioid dependence, use of opioids by injection, use of high doses of opioids, mental disorders, and use of opioids together with alcohol, benzodiazepines, or cocaine.[1][11][5] Risk of overdose is particularly high following detoxification.[1] Dependence on prescription opioids can occur from their use to treat chronic pain.[1] Diagnosis of an opioid overdose is based on symptoms and examination.[3]
Initial treatment involves supporting the person's breathing and providing oxygen.[7] Naloxone is then recommended among those who are not breathing to reverse the opioid's effects.[7][3] Giving naloxone into the nose or as an injection into a muscle appear to be equally effective.[12] Among those who refuse to go to hospital following reversal, the risks of a poor outcome in the short term appear to be low.[12] Efforts to prevent deaths from overdose include improving access to naloxone and treatment for opioid dependence.[1]
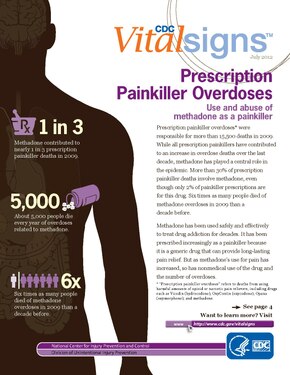
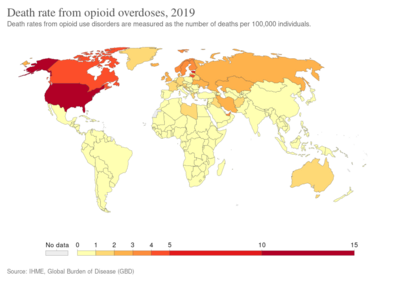
Opioid use disorders resulted in 122,000 deaths globally in 2015, up from 18,000 deaths in 1990.[8][13] In the United States, over 49,000 deaths involved opioids in 2017.[5] Of those, about 20,000 involved prescription opioids and 16,000 involved heroin.[5] In 2017, opioid deaths represented more than 65% of all drug overdose related deaths in the United States.[5] The opioid epidemic is believed to be in part due to assurances in the 1990s by the pharmaceutical industry that prescription opioids were safe.[4]
Signs and symptoms
Because of their effect on the part of the brain that regulates breathing, opioids can lead to a person having very slow or stopped breathing during overdoses and therefore result in death if left untreated.[1] Opiate overdose symptoms and signs can be referred to as the "opioid overdose triad": decreased level of consciousness, pinpoint pupils and respiratory depression. Other symptoms include seizures and muscle spasms. Sometimes an opiate overdose can lead to such a decreased level of consciousness such that the person will not wake up.
Prolonged lack of oxygenation from respiratory depression can also lead to detrimental damage to the brain and spinal cord and can leave the person unable to walk or function normally, even if treatment with naloxone is given.
Alcohol also causes respiratory depression and therefore when taken with opioids can increase the risk of respiratory depression and death.[1]
In young children, opioid overdose may not be apparent right away. This is due to absorption, distribution, and metabolism differences between young children and adults, and the higher amount of opioid ingestion per kilogram of body weight.[3]
Cause

Risk factors for opioid overdose include opioid dependence, injecting opioids, using high doses of opioids, and use together with alcohol, benzodiazepines, or cocaine.[1][5] The risk is particularly high following detoxification.[1] Dependence on prescription opioids can occur from their use to treat chronic pain.[1] In young children an overdose is usually due to opioids that are intended for their parents, older siblings, or grandparents.[15] In mothers who take codeine during breastfeeding, opioid overdoses have occurred in their baby.[16] Codeine is therefore not recommended in those who are breastfeeding.[16]
Co-ingestion
Opioid overdoses are often associated with benzodiazepines or alcohol use.[17][18] Other CNS depressants, muscle relaxers, pain relievers, anti-convulsants, anxiolytics, treatment drugs of a psychoactive or epileptic variety or any other such drug with its active function meant to calm or mitigate neuronal signaling (barbiturates, etc.) can additionally cause a worsened condition with less likelihood of recovery cumulative to each added drug. This includes drugs less immediately classed to a slowing of the metabolism such as with GABAergics like GHB or glutamatergic antagonists like PCP or ketamine.
-
The top line represents the yearly number of benzodiazepine deaths that involved opioids in the US. The bottom line represents benzodiazepine deaths that did not involve opioids.[5]
-
Opioid involvement in cocaine overdose deaths. Green line is cocaine and any opioid. Gray line is cocaine without any opioids. Yellow line is cocaine and other synthetic opioids.[5]
Risk factors
Opioids are metabolized by the liver before they are excreted in the urine and each opioid may be metabolized by different cytochrome P450 (CYP) enzymes.[3] Polymorphisms in CYP superfamily of genes vary by individual and can account for differences in therapeutic response to drugs.[19] This biotransformation of opioids by the liver can either lead to the inactivation or activation of the drug.[20] For example, methadone is converted primarily by CYP3A4 liver enzyme to an inactive metabolite.[20] In contrast, codeine is an initially inactive prodrug that is metabolized by CYP2D6 to its active form morphine to exert its analgesic effects.[21] An individual who has a poor metabolizer phenotype of CYP2D6 may experience weak analgesic effects with codeine while someone who has the ultra-rapid metabolizer phenotype would experience greater side effects.[21]
Mechanism
Permanent brain damage may occur due to cerebral hypoxia or opioid-induced neurotoxicity.[2][22] Opioids inhibit the medulla's chemoreceptors through the mu and delta receptors.[23] Opioids bind to receptors that are part of the endogenous opioid system as well as other central nervous neurotransmitter systems, binding to excitatory neurotransmitters like dopamine or glutamate, or inhibitory neurotransmitters like GABA. The main excitatory chemoreceptor, glutamate, and main inhibitory chemoreceptor, GABA, are the main neurotransmitters that control respiration.[24] Because of its fatal consequences, opioid induced respiratory depression is one of the major limiting factors of its analgesic effects.[25] Opioids vary in the rate of metabolism amongst individuals. The rate of metabolism of opiates vary due to genetic factors while tolerance of the opiates can determine risk.[26]
Prevention
Opioid overdoses can often be prevented.[27][28] Clear protocols for staff at emergency departments and urgent care centers can reduce opioid prescriptions for individuals presenting in these settings who engage in drug seeking behaviors or who have a history of substance abuse.[29] Drug seeking behaviors include but are not limited to obsessiveness or impatience when it comes to attaining medications, seeking multiple pain adjunct medications, and inconsistent physiological presentation.[30] A prescription monitoring program may help determine if an individual is receiving a high doses of opioids or combinations of medications such as benzodiazepines and opioids that put them at high risk.[31] Limited amount of evidence suggests opioid therapy with extended-release or long-acting formulations may increase the risk of an unintentional overdose compared to shorter-acting agents.[32] Routinely screening using tools such as the CAGE-AID and the Drug Abuse Screening Test (DAST-10) in adults and the CRAFFT in those aged 14–18 years is recommended.[27] Other “drug seeking” behaviors and physical indications of drug use should be used as clues to perform formal screenings.[27]
There are several medication-assisted treatments available for people with opioid use disorder or opioid dependence, who are at higher risk for opioid overdose.[33][34] The selection of treatment depends on various factors, such as a person's preference, accessibility, and history of treatment.[34] Examples of medication-assisted treatments are buprenorphine (with or without naloxone), naltrexone, and methadone.[35][36] Peer support groups have tentative evidence of benefit.[37] There is also some evidence indicating benefits in community-based overdose education and naloxone distribution programs.[38] Buprenorphine and methadone can help decrease drug cravings.[34] Combining pharmacologic treatments with behavioral therapy, such as support or recovery groups, can increase likelihood of overcoming addiction and reduce the risk of an opioid overdose.
Individuals diagnosed with opioid dependence should be prescribed naloxone to prevent overdose and should be directed to one of treatment options available, such as needle exchange programs and treatment centers.[27][28] A naloxone prescription is also recommended when risk factors for opioid overdose are present such as history of overdose, substance use disorder, or higher doses of opioids.[31] Brief motivational interviewing can also be performed and has been shown to improve people's motivation to change their behavior.[27][39] Despite these opportunities, the dissemination of prevention interventions in the US has been hampered by the lack of coordination and sluggish federal government response.[28]
In the United States, 49 states and the District of Columbia have expanded naloxone access at a pharmacy level via standing order, protocol order, naloxone-specific collaborative practice agreement, or pharmacist prescriptive authority.[40]
Treatment
In people who have overdosed on opioids, basic life support and naloxone are recommended as soon as possible. Naloxone is effective at reversing the cause, rather than just the symptoms, of an opioid overdose.[41] Compared to adults, children often need larger doses of naloxone per kilogram of body weight.[3]
Programs to provide drug users and their caregivers with naloxone are recommended.[42] In the United States, as of 2014, more than 25,000 overdoses have been reversed.[43][44] Programs training police and fire personnel in opioid overdose response using naloxone have also shown promise.[45] Programs have been developed in cities, such as San Francisco, to increase community awareness and engagement in prevention of opioid overdose.[46]
Epidemiology
In 2016, the World Health Organization estimates 34 million people used opioids and 19 million used opiates.[47] Of these, about 27 million people had opioid dependence, with the majority—but a decreasing number—using illicit heroin.[47] In 2015, 118,000 people died from opioid use disorders, causing almost one third of all drug related deaths.[47]
United States of America
Of the 70,200 overdose deaths in the US in 2017, opioids were involved in 47,600.[5] This is an increase from 2016 where over 64,000 died from drug overdose, and opioids were involved in over 42,000.[48] In 2017, the five states with the highest rates of death due to drug overdose were West Virginia (57.8 per 100,000), Ohio (46.3 per 100,000), Pennsylvania (44.3 per 100,000), Kentucky (37.2 per 100,000), and New Hampshire (37.0 per 100,000).[49]
Concerning the 2017 data in the charts below, deaths from the various drugs add up to more than 70,200 because multiple drugs are involved in many of the deaths.[5] According to the National Safety Council, the lifetime odds of dying from an overdose in the United States is 1 in 96.[50]
- Charts of deaths involving specific opioids and classes of opioids
-
Drug overdose deaths in the US per 100,000 people by state.[49]
-
US yearly deaths from all opioid drugs. Included in this number are opioid analgesics, along with heroin and illicit synthetic opioids.[5]
-
US yearly deaths involving other synthetic opioids, predominately Fentanyl.[5]
-
US yearly deaths involving prescription opioids. Non-methadone synthetics is a category dominated by illegally acquired fentanyl, and has been excluded.[5]
-
US yearly overdose deaths involving heroin.[5]
-
US yearly overdose deaths, and the drugs involved. Among the 70,200 deaths estimated in 2017, the sharpest increase occurred among deaths related to fentanyl and synthetic opioids (28,466 deaths).[5]
Awareness
The Substance Abuse and Mental Health Services Administration hosts an annual health observance known as National Prevention Week. Every third week of May, they encourage communities across the country to unite to share stories about positive mental and behavioral health and the importance of implementing prevention methods.[51] They also sponsor recovery Month every September. Recovery Month aims to raise awareness about mental and substance use disorders and to honor individuals who recover, promoting the positive message that prevention works and that treatment is effective.[52]
International Overdose Awareness Day is on August 31st to remember those who have lost their lives to overdose, to decrease stigma of drug-related deaths, and to promote prevention of overdose.[53]
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 "Information sheet on opioid overdose". WHO. November 2014. Archived from the original on 2014-12-01. Retrieved 2018-10-12.
- ↑ 2.0 2.1 2.2 "Heroin". National Institute on Drug Abuse. July 2017. Archived from the original on 19 October 2016. Retrieved 29 November 2017.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Boyer EW (July 2012). "Management of opioid analgesic overdose". The New England Journal of Medicine. 367 (2): 146–55. doi:10.1056/NEJMra1202561. PMC 3739053. PMID 22784117.
- ↑ 4.0 4.1 4.2 "Opioid Overdose Crisis". National Institute on Drug Abuse. 1 June 2017. Archived from the original on 9 June 2020. Retrieved 29 November 2017.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 Overdose Death Rates Archived 2015-11-28 at the Wayback Machine. By National Institute on Drug Abuse (NIDA).
- ↑ Adams, James G. (2008). Emergency Medicine: Expert Consult -- Online. Elsevier Health Sciences. p. PT4876. ISBN 978-1437721294. Archived from the original on 2020-01-26. Retrieved 2017-11-29.
- ↑ 7.0 7.1 7.2 de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, et al. (November 2015). "Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S526–42. doi:10.1161/cir.0000000000000266. PMC 6191296. PMID 26473000.
- ↑ 8.0 8.1 GBD 2015 Mortality and Causes of Death Collaborators (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ "Commonly Used Terms Drug Overdose". www.cdc.gov. 29 August 2017. Archived from the original on 10 December 2019. Retrieved 29 November 2017.
- ↑ Malamed, Stanley F. (2007). Medical Emergencies in the Dental Office - E-Book. Elsevier Health Sciences. p. 387. ISBN 978-0323075947. Archived from the original on 2020-01-26. Retrieved 2017-11-29.
- ↑ Park TW, Lin LA, Hosanagar A, Kogowski A, Paige K, Bohnert AS (2016). "Understanding Risk Factors for Opioid Overdose in Clinical Populations to Inform Treatment and Policy". Journal of Addiction Medicine. 10 (6): 369–381. doi:10.1097/ADM.0000000000000245. PMID 27525471.
- ↑ 12.0 12.1 Chou R, Korthuis PT, McCarty D, Coffin PO, Griffin JC, Davis-O'Reilly C, et al. (December 2017). "Management of Suspected Opioid Overdose With Naloxone in Out-of-Hospital Settings: A Systematic Review". Annals of Internal Medicine. 167 (12): 867–875. doi:10.7326/M17-2224. PMID 29181532.
- ↑ GBD 2013 Mortality and Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ Fentanyl Archived 2021-01-26 at the Wayback Machine. Image 4 of 17. US DEA (Drug Enforcement Administration).
- ↑ Boyer EW, McCance-Katz EF, Marcus S (January 2010). "Methadone and buprenorphine toxicity in children". The American Journal on Addictions. 19 (1): 89–95. doi:10.1111/j.1521-0391.2009.00002.x. PMID 20132125.
- ↑ 16.0 16.1 Lazaryan M, Shasha-Zigelman C, Dagan Z, Berkovitch M (June 2015). "Codeine should not be prescribed for breastfeeding mothers or children under the age of 12". Acta Paediatrica. 104 (6): 550–6. doi:10.1111/apa.13012. PMID 25809057.
- ↑ "BestBets: Concomitant use of benzodiazepines in opiate overdose and the association with a poorer outcome". Archived from the original on 2019-06-29. Retrieved 2008-12-20.
- ↑ "BestBets: Concomitant use of alcohol in opiate overdose and the association with a poorer outcome". Archived from the original on 2019-06-29. Retrieved 2008-12-20.
- ↑ Zhou SF, Liu JP, Chowbay B (2009). "Polymorphism of human cytochrome P450 enzymes and its clinical impact". Drug Metabolism Reviews. 41 (2): 89–295. doi:10.1080/03602530902843483. PMID 19514967.
- ↑ 20.0 20.1 Ferrari A, Coccia CP, Bertolini A, Sternieri E (December 2004). "Methadone--metabolism, pharmacokinetics and interactions". Pharmacological Research. 50 (6): 551–9. doi:10.1016/j.phrs.2004.05.002. PMID 15501692.
- ↑ 21.0 21.1 Kirchheiner J, Schmidt H, Tzvetkov M, Keulen JT, Lötsch J, Roots I, Brockmöller J (August 2007). "Pharmacokinetics of codeine and its metabolite morphine in ultra-rapid metabolizers due to CYP2D6 duplication". The Pharmacogenomics Journal. 7 (4): 257–65. doi:10.1038/sj.tpj.6500406. PMID 16819548.
- ↑ Cunha-Oliveira T, Rego AC, Oliveira CR (June 2008). "Cellular and molecular mechanisms involved in the neurotoxicity of opioid and psychostimulant drugs". Brain Research Reviews. 58 (1): 192–208. doi:10.1016/j.brainresrev.2008.03.002. hdl:10316/4676. PMID 18440072.
Since morphine can induce neurotoxicity (Hu et al., 2002; Mao et al., 2002; Lim et al., 2005), it may contribute to the neurotoxic effects of heroin. However, we showed that 6-MAM and morphine do not contribute to street heroin neurotoxicity in cultured cortical neurons (Cunha-Oliveira et al., 2007). In accordance, a recent study suggests that heroin has a higher neurotoxic potential in comparison with morphine (Tramullas et al., 2008).
- ↑ White JM, Irvine RJ (July 1999). "Mechanisms of fatal opioid overdose". Addiction. 94 (7): 961–72. doi:10.1046/j.1360-0443.1999.9479612.x. PMID 10707430.
- ↑ Watson SJ, Akil H, Khachaturian H, et al. Opioid systems: Anatomical, physiological and clinical perspectives. In: Opioids Past, Present and Future, Hughes J, Collier HO, Rance MJ, Tyers MB (Eds), Taylor & Francis, London 1984. p.145.
- ↑ Pattinson KT (June 2008). "Opioids and the control of respiration". British Journal of Anaesthesia. 100 (6): 747–58. doi:10.1093/bja/aen094. PMID 18456641. Archived from the original on 2018-11-20. Retrieved 2018-11-20.
- ↑ Smith HS (July 2009). "Opioid metabolism". Mayo Clinic Proceedings. 84 (7): 613–24. doi:10.4065/84.7.613. PMC 2704133. PMID 19567715.
- ↑ 27.0 27.1 27.2 27.3 27.4 Bowman S, Eiserman J, Beletsky L, Stancliff S, Bruce RD (July 2013). "Reducing the health consequences of opioid addiction in primary care". The American Journal of Medicine. 126 (7): 565–71. doi:10.1016/j.amjmed.2012.11.031. PMID 23664112.In press
- ↑ 28.0 28.1 28.2 Beletsky L, Rich JD, Walley AY (November 2012). "Prevention of fatal opioid overdose". JAMA. 308 (18): 1863–4. doi:10.1001/jama.2012.14205. PMC 3551246. PMID 23150005.
- ↑ "Emergency Department and Urgent Care Clinicians Use Protocol To Reduce Opioid Prescriptions for Patients Suspected of Abusing Controlled Substances". Agency for Healthcare Research and Quality. 2014-03-12. Archived from the original on 2017-12-02. Retrieved 2014-03-14.
- ↑ Pretorius RW, Zurick GM (April 2008). "A systematic approach to identifying drug-seeking patients". Family Practice Management. 15 (4): A3-5. PMID 18444310.
- ↑ 31.0 31.1 Dowell D, Haegerich TM, Chou R (April 2016). "CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016". JAMA. 315 (15): 1624–45. doi:10.1001/jama.2016.1464. PMC 6390846. PMID 26977696.
- ↑ Miller M, Barber CW, Leatherman S, Fonda J, Hermos JA, Cho K, Gagnon DR (April 2015). "Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy". JAMA Internal Medicine. 175 (4): 608–15. doi:10.1001/jamainternmed.2014.8071. PMID 25686208.
- ↑ "Information sheet on opioid overdose". World Health Organization. Archived from the original on 2014-12-01. Retrieved 2018-11-01.
- ↑ 34.0 34.1 34.2 "ASAM National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use" (PDF). Archived from the original (PDF) on 2019-04-07. Retrieved 2018-11-01.
- ↑ "Current and Emerging Options to Combat the Opioid Epidemic". AJMC. Archived from the original on 2018-11-03. Retrieved 2018-11-01.
- ↑ Mattick RP, Breen C, Kimber J, Davoli M (February 2014). "Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence" (PDF). The Cochrane Database of Systematic Reviews (2): CD002207. doi:10.1002/14651858.CD002207.pub4. PMID 24500948. Archived (PDF) from the original on 2019-04-07. Retrieved 2018-12-28.
- ↑ Tracy K, Wallace SP (September 2016). "Benefits of peer support groups in the treatment of addiction". Substance Abuse and Rehabilitation. 7: 143–154. doi:10.2147/SAR.S81535. PMC 5047716. PMID 27729825.
- ↑ Mueller SR, Walley AY, Calcaterra SL, Glanz JM, Binswanger IA (2015-03-16). "A Review of Opioid Overdose Prevention and Naloxone Prescribing: Implications for Translating Community Programming Into Clinical Practice". Substance Abuse. 36 (2): 240–53. doi:10.1080/08897077.2015.1010032. PMC 4470731. PMID 25774771.
- ↑ Zahradnik A, Otto C, Crackau B, Löhrmann I, Bischof G, John U, Rumpf HJ (January 2009). "Randomized controlled trial of a brief intervention for problematic prescription drug use in non-treatment-seeking patients". Addiction. 104 (1): 109–17. doi:10.1111/j.1360-0443.2008.02421.x. PMID 19133895.
- ↑ "PDAPS - Naloxone Overdose Prevention Laws". pdaps.org. Archived from the original on 2019-10-23. Retrieved 2019-10-23.
- ↑ Etherington J, Christenson J, Innes G, Grafstein E, Pennington S, Spinelli JJ, et al. (July 2000). "Is early discharge safe after naloxone reversal of presumed opioid overdose?". Canadian Journal of Emergency Medicine. 2 (3): 156–62. doi:10.1017/s1481803500004863. PMID 17621393. Archived from the original on 2015-05-10. Retrieved 2012-11-02.
- ↑ Community management of opioid overdose (PDF). World Health Organization. 2014. ISBN 9789241548816. Archived (PDF) from the original on 2016-11-08. Retrieved 2014-11-21.
- ↑ Wheeler E, Jones TS, Gilbert MK, Davidson PJ (June 2015). "Opioid Overdose Prevention Programs Providing Naloxone to Laypersons - United States, 2014". MMWR. Morbidity and Mortality Weekly Report. 64 (23): 631–5. PMC 4584734. PMID 26086633.
- ↑ Beletsky L, Burris S, Kral AH (July 21, 2009). "Closing Death's Door: Action Steps to Facilitate Emergency Opioid Drug Overdose Reversal in the United States". doi:10.2139/ssrn.1437163. SSRN 1437163.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Lavoie D (April 2012). "Naloxone: Drug-Overdose Antidote Is Put In Addicts' Hands". Huffington Post. Archived from the original on 2012-05-18. Retrieved 2012-05-12.
- ↑ "Archive copy". Archived from the original on 2019-10-31. Retrieved 2019-10-31.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ 47.0 47.1 47.2 "WHO | Information sheet on opioid overdose". WHO. Archived from the original on 2014-12-01. Retrieved 2019-10-23.
- ↑ National Center for Health Statistics. "Provisional Counts of Drug Overdose Deaths, as of 8/6/2017" (PDF). United States: Centers for Disease Control and Prevention. Archived (PDF) from the original on 2017-12-09. Retrieved 2018-10-12. Source lists US totals for 2015 and 2016 and statistics by state.
- ↑ 49.0 49.1 Drug Overdose Deaths Archived 2019-09-20 at the Wayback Machine. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Click on a map year. The data table is below the map. Number of deaths for each state, and the age-adjusted rates of death for each state. Also, place cursor on map states to get data.
- ↑ "Odds of Dying". Injury Facts. Archived from the original on 23 March 2018. Retrieved 31 January 2019.
- ↑ carley.heslin (2013-11-08). "About National Prevention Week". www.samhsa.gov. Archived from the original on 2018-11-03. Retrieved 2018-11-01.
- ↑ "Home | RecoveryMonth.gov". www.recoverymonth.gov. Archived from the original on 2018-11-30. Retrieved 2018-11-20.
- ↑ "International Overdose Awareness Day - August 31, 2019". MMWR. Morbidity and Mortality Weekly Report. 68 (34): 737. August 2019. doi:10.15585/mmwr.mm6834a1. PMC 6715257. PMID 31466079.
External links
- WHO Community Management of Opioid Overdose, 2014 Archived 2016-11-08 at the Wayback Machine
| Classification | |
|---|---|
| External resources |
![The top line represents the yearly number of benzodiazepine deaths that involved opioids in the US. The bottom line represents benzodiazepine deaths that did not involve opioids.[5]](https://upload.wikimedia.org/wikipedia/commons/thumb/c/ce/US_timeline._Opioid_involvement_in_benzodiazepine_overdose.jpg/360px-US_timeline._Opioid_involvement_in_benzodiazepine_overdose.jpg)
![Opioid involvement in cocaine overdose deaths. Green line is cocaine and any opioid. Gray line is cocaine without any opioids. Yellow line is cocaine and other synthetic opioids.[5]](https://upload.wikimedia.org/wikipedia/commons/thumb/d/df/US_timeline._Opioid_involvement_in_cocaine_overdose.jpg/360px-US_timeline._Opioid_involvement_in_cocaine_overdose.jpg)
![Drug overdose deaths in the US per 100,000 people by state.[49]](https://upload.wikimedia.org/wikipedia/commons/thumb/7/71/2016_US_map_of_drug_overdose_deaths_per_100%2C000_population_by_state.gif/424px-2016_US_map_of_drug_overdose_deaths_per_100%2C000_population_by_state.gif)
![US yearly deaths from all opioid drugs. Included in this number are opioid analgesics, along with heroin and illicit synthetic opioids.[5]](https://upload.wikimedia.org/wikipedia/commons/thumb/8/87/US_timeline._Opioid_deaths.jpg/360px-US_timeline._Opioid_deaths.jpg)
![US yearly deaths involving other synthetic opioids, predominately Fentanyl.[5]](https://upload.wikimedia.org/wikipedia/commons/thumb/3/3e/US_timeline._Deaths_involving_other_synthetic_opioids%2C_predominately_Fentanyl.jpg/369px-US_timeline._Deaths_involving_other_synthetic_opioids%2C_predominately_Fentanyl.jpg)
![US yearly deaths involving prescription opioids. Non-methadone synthetics is a category dominated by illegally acquired fentanyl, and has been excluded.[5]](https://upload.wikimedia.org/wikipedia/commons/thumb/c/c1/US_timeline._Prescription_opioid_pain_reliever_deaths.jpg/360px-US_timeline._Prescription_opioid_pain_reliever_deaths.jpg)
![US yearly overdose deaths involving heroin.[5]](https://upload.wikimedia.org/wikipedia/commons/thumb/8/8d/Timeline_of_US_overdose_deaths_involving_heroin%2C_by_other_opioid_involvement.jpg/360px-Timeline_of_US_overdose_deaths_involving_heroin%2C_by_other_opioid_involvement.jpg)
![US yearly overdose deaths, and the drugs involved. Among the 70,200 deaths estimated in 2017, the sharpest increase occurred among deaths related to fentanyl and synthetic opioids (28,466 deaths).[5]](https://upload.wikimedia.org/wikipedia/commons/thumb/f/fa/US_timeline._Drugs_involved_in_overdose_deaths.jpg/360px-US_timeline._Drugs_involved_in_overdose_deaths.jpg)
