COVID-19
| Coronavirus disease 2019 (COVID-19) | |
|---|---|
| Other names: COVID, Covid, (the) coronavirus | |
 | |
Transmission and life-cycle of SARS-CoV-2 causing COVID-19. | |
| Pronunciation | |
| Specialty | Infectious disease |
| Symptoms | Fever, cough, shortness of breath, tiredness, loss of smell;[2] some are asymptomatic[3] |
| Complications | Blood clots, heart disease, kidney problems, multisystem inflammatory syndrome in children, chronic COVID syndrome[4] |
| Usual onset | 2–14 days (typically 5) from infection[2][5] |
| Diagnostic method | Rapid antigen test, PCR test[5] |
| Prevention | Physical distancing, face masks, ventilation, quarantine, vaccination[5][6][7] |
| Treatment | Supportive and symptomatic[8] |
| Medication | Non-hospitalized: Nirmatrelvir/ritonavir, sotrovimab, molnupiravir[8] Severe: Oxygen therapy, dexamethasone, remdesivir[8] Critical care: Tocilizumab, sarilumab[8] |
| Prognosis | 20% require hospitalization[5] |
| Frequency | 676,609,955[9] |
| Deaths | ~20 million (as of Dec 31, 2021)[10] |
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).[5] Symptoms often include fever, cough, breathing difficulties, tiredness, headache, loss of smell and taste, sore throat, vomiting, and diarrhea.[2] Onset is usually two to fourteen days after exposure to the virus.[2] Some people; however, develop no symptoms.[3]
Spread occurs mainly when an infected person is in close contact with another person.[11] This may occur by either airborne transmission or small droplets containing the virus.[12][13] Less commonly, the virus may spread via contaminated surfaces.[11] People can transmit the virus two days before they show symptoms, and generally remain infectious for up to 10 days, though those with severe disease maybe infectious longer.[12][14] Diagnosis is generally by polymerase chain reaction (PCR) or rapid antigen test from a nose or throat swab.[5]
Preventive measures include physical distancing, use of a high quality face mask, ventilation of indoor spaces, and quarantine.[5][6][15] Several vaccines also decrease the risk.[7] Much of treatment is symptomatic and supportive.[8] In those who do not require hospitalization, but are at high risk, nirmatrelvir/ritonavir, sotrovimab, or molnupiravir may be used.[8] For those who require oxygen therapy, dexamethasone and remdesivir may be used.[8] For those who required critical care tocilizumab or sarilumab may be added.[8]
Of those people who develop symptoms, around 80% recover without needing hospitalization, 15% require oxygen therapy, and 5% require intensive care.[5] Older people and those with other health problems are at a higher risk.[5] While most get better after a few weeks, some continue to experience a range of effects (long COVID) for months.[16] As of 24 April 2024, at least 676 million cases have been confirmed, which has resulted in more than 6.88 million deaths.[9] The actual number of deaths was; however, estimated at nearly 20 million as of December 31st 2021.[10] The first known case was identified in Wuhan, China, in December 2019.[17] The disease has since spread worldwide, leading to an ongoing pandemic.[18]
Signs and symptoms

Symptoms of COVID-19 are variable, ranging from mild symptoms to severe illness.[19][20] Common symptoms include headache,[21] loss of smell[22] and taste,[23] nasal congestion and runny nose, cough, muscle pain, sore throat, fever,[24] diarrhea, and breathing difficulties.[25] People with the same infection may have different symptoms, and their symptoms may change over time. Three common clusters of symptoms have been identified: one respiratory symptom cluster with cough, sputum, shortness of breath, and fever; a musculoskeletal symptom cluster with muscle and joint pain, headache, and fatigue; a cluster of digestive symptoms with abdominal pain, vomiting, and diarrhea.[25] In people without prior ear, nose, and throat disorders, loss of taste combined with loss of smell is associated with COVID-19.[26]
Most people (81%) develop mild to moderate symptoms (up to mild pneumonia), while 14% develop severe symptoms (dyspnea, hypoxia, or more than 50% lung involvement on imaging) and 5% of patients suffer critical symptoms (respiratory failure, shock, or multiorgan dysfunction).[27] At least a third of the people who are infected with the virus do not develop noticeable symptoms at any point in time.[28][29][30][31] These asymptomatic carriers tend not to get tested and can spread the disease.[31][32][33][34] Other infected people will develop symptoms later, called "pre-symptomatic", or have very mild symptoms and can also spread the virus.[34]
As is common with infections, there is a delay between the moment a person first becomes infected and the appearance of the first symptoms. The median delay for COVID-19 is four to five days.[35] Most symptomatic people experience symptoms within two to seven days after exposure, and almost all will experience at least one symptom within 12 days.[35][36]
Most people recover from the acute phase of the disease. However, some people continue to experience a range of effects for months after recovery—named long COVID—and damage to organs has been observed. Multi-year studies are underway to further investigate the long-term effects of the disease.[37]-
Suspected COVID-19 rash
-
Suspected COVID-19 rash
-
Rash on feet associated with COVID-19
-
Exanthem associated with COVID-19
-
A red face and neck associated with COVID-19
-
Hand dermatitis in a patient with COVID-19 infection
Cause
COVID-19 is caused by infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus strain.
Transmission

The virus is transmitted mainly through the respiratory route after an infected person coughs, sneezes, sings, talks, or breathes. A new infection occurs when virus-containing particles exhaled by an infected person, either respiratory droplets or aerosols, get into the mouth, nose, or eyes of other people who are in close contact with the infected person.[38] During human-to-human transmission, an average 1000 infectious SARS-CoV-2 virions are thought to initiate a new infection.
The closer people interact, and the longer they interact, the more likely they are to transmit COVID-19. Closer distances can involve larger droplets (which fall to the ground) and aerosols, whereas longer distances only involve aerosols. Larger droplets can also turn into aerosols (known as droplet nuclei) through evaporation. The relative importance of the larger droplets and the aerosols is not clear as of November 2020; however, the virus is not known to spread between rooms over long distances such as through air ducts. Airborne transmission is able to particularly occur indoors, in high risk locations such as restaurants, choirs, gyms, nightclubs, offices, and religious venues, often when they are crowded or less ventilated. It also occurs in healthcare settings, often when aerosol-generating medical procedures are performed on COVID-19 patients.
The number of people generally infected by one infected person varies; as of September 2020 it was estimated that one infected person will, on average, infect between two and three other people. This is more infectious than influenza, but less so than measles. It often spreads in clusters, where infections can be traced back to an index case or geographical location. There is a major role of "super-spreading events", where many people are infected by one person. A person who is infected can transmit the virus to others up to two days before they themselves show symptoms, and even if symptoms never appear.[38] People remain infectious in moderate cases for 7–12 days, and up to two weeks in severe cases. In October 2020, medical scientists reported evidence of reinfection in one patient.Virology

Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel severe acute respiratory syndrome coronavirus. It was first isolated from three people with pneumonia connected to the cluster of acute respiratory illness cases in Wuhan.[39] All structural features of the novel SARS-CoV-2 virus particle occur in related coronaviruses in nature.[40]
Outside the body, the virus is destroyed by household soap, which bursts its protective bubble.[41]
SARS-CoV-2 is closely related to the original SARS-CoV.[42] It is thought to have an animal (zoonotic) origin. Genetic analysis has revealed that the coronavirus genetically clusters with the genus Betacoronavirus, in subgenus Sarbecovirus (lineage B) together with two bat-derived strains. It is 96% identical at the whole genome level to other bat coronavirus samples (BatCov RaTG13).[43][44] The structural proteins of SARS-CoV-2 include membrane glycoprotein (M), envelope protein (E), nucleocapsid protein (N), and the spike protein (S). The M protein of SARS-CoV-2 is about 98% similar to the M protein of bat SARS-CoV, maintains around 98% homology with pangolin SARS-CoV, and has 90% homology with the M protein of SARS-CoV; whereas, the similarity is only around 38% with the M protein of MERS-CoV. The structure of the M protein resembles the sugar transporter SemiSWEET.[45]
The many thousands of SARS-CoV-2 variants are grouped into clades.[46] Several different clade nomenclatures have been proposed. Nextstrain divides the variants into five clades (19A, 19B, 20A, 20B, and 20C), while GISAID divides them into seven (L, O, V, S, G, GH, and GR).[47]
Several notable variants of SARS-CoV-2 emerged in late 2020. Cluster 5 emerged among minks and mink farmers in Denmark. After strict quarantines and a mink euthanasia campaign, it is believed to have been eradicated. The Variant of Concern 202012/01 (VOC 202012/01) is believed to have emerged in the United Kingdom in September. The 501Y.V2 Variant, which has the same N501Y mutation, arose independently in South Africa.[48][49]
Variants
Three known variants of SARS-CoV-2 are spreading among global populations As of January 2021[update], including the UK Variant (referred to as B.1.1.7) first found in London and Kent, a variant discovered in South Africa (referred to as 1.351), and a variant discovered in Brazil (referred to as P.1).[50]
Using whole genome sequencing, epidemiology and modelling suggest the new UK variant VUI-202012/01 (the first variant under investigation in December 2020) transmits more easily than other strains.[51]
Pathophysiology

The SARS-CoV-2 virus can infect a wide range of cells and systems of the body. COVID‑19 is most known for affecting the upper respiratory tract (sinuses, nose, and throat) and the lower respiratory tract (windpipe and lungs).[52] The lungs are the organs most affected by COVID‑19 because the virus accesses host cells via the receptor for the enzyme angiotensin-converting enzyme 2 (ACE2), which is most abundant on the surface of type II alveolar cells of the lungs.[53] The virus uses a special surface glycoprotein called a "spike" to connect to the ACE2 receptor and enter the host cell.[54]
Respiratory
Following viral entry, COVID‑19 infects the ciliated epithelium of the nasopharynx and upper airways.[55]
Nervous system

One common symptom, loss of smell, results from infection of the support cells of the olfactory epithelium, with subsequent damage to the olfactory neurons.[56] The involvement of both the central and peripheral nervous system in COVID‑19 has been reported in many medical publications.[57] It is clear that many people with COVID-19 exhibit neurological or mental health issues. The virus is not detected in the CNS of the majority of COVID-19 patients with neurological issues. However, SARS-CoV-2 has been detected at low levels in the brains of those who have died from COVID‑19, but these results need to be confirmed.[58] While virus has been detected in cerebrospinal fluid of autopsies, the exact mechanism by which it invades the CNS remains unclear and may first involve invasion of peripheral nerves given the low levels of ACE2 in the brain.[59][60][61] The virus may also enter the bloodstream from the lungs and cross the blood-brain barrier to gain access to the CNS, possibly within an infected white blood cell.[58]
Gastrointestinal
The virus also affects gastrointestinal organs as ACE2 is abundantly expressed in the glandular cells of gastric, duodenal and rectal epithelium[62] as well as endothelial cells and enterocytes of the small intestine.[63]
Cardiovascular
The virus can cause acute myocardial injury and chronic damage to the cardiovascular system.[64] An acute cardiac injury was found in 12% of infected people admitted to the hospital in Wuhan, China,[65] and is more frequent in severe disease.[66] Rates of cardiovascular symptoms are high, owing to the systemic inflammatory response and immune system disorders during disease progression, but acute myocardial injuries may also be related to ACE2 receptors in the heart.[64] ACE2 receptors are highly expressed in the heart and are involved in heart function.[64][67] A high incidence of thrombosis and venous thromboembolism have been found in people transferred to Intensive care units (ICU) with COVID‑19 infections, and may be related to poor prognosis.[68] Blood vessel dysfunction and clot formation (as suggested by high D-dimer levels caused by blood clots) are thought to play a significant role in mortality, incidences of clots leading to pulmonary embolisms, and ischaemic events within the brain have been noted as complications leading to death in people infected with SARS-CoV-2. Infection appears to set off a chain of vasoconstrictive responses within the body, constriction of blood vessels within the pulmonary circulation has also been posited as a mechanism in which oxygenation decreases alongside the presentation of viral pneumonia.[69] Furthermore, microvascular (arterioles and capillaries) blood vessel damage has been reported in a small number of tissue samples of the brains – without detected SARS-CoV-2 – and the olfactory bulbs from those who have died from COVID‑19.[70][71][72] COVID‑19 was also found to cause substantial – including morphological and mechanical – changes to blood cells – such as increased sizes – sometimes persisting for months after hospital discharge.[73][74]
Other organs
Another common cause of death is complications related to the kidneys.[69] Early reports show that up to 30% of hospitalized patients both in China and in New York have experienced some injury to their kidneys, including some persons with no previous kidney problems.[75]
Autopsies of people who died of COVID‑19 have found diffuse alveolar damage, and lymphocyte-containing inflammatory infiltrates within the lung.[76]
Immunopathology
Although SARS-CoV-2 has a tropism for ACE2-expressing epithelial cells of the respiratory tract, people with severe COVID‑19 have symptoms of systemic hyperinflammation. Clinical laboratory findings of elevated IL‑2, IL‑7, IL‑6, granulocyte-macrophage colony-stimulating factor (GM‑CSF), interferon gamma-induced protein 10 (IP‑10), monocyte chemoattractant protein 1 (MCP1), macrophage inflammatory protein 1‑alpha (MIP‑1‑alpha), and tumour necrosis factor (TNF‑α) indicative of cytokine release syndrome (CRS) suggest an underlying immunopathology.[65]
Additionally, people with COVID‑19 and acute respiratory distress syndrome (ARDS) have classical serum biomarkers of CRS, including elevated C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, and ferritin.[77]
Systemic inflammation results in vasodilation, allowing inflammatory lymphocytic and monocytic infiltration of the lung and the heart. In particular, pathogenic GM-CSF-secreting T cells were shown to correlate with the recruitment of inflammatory IL-6-secreting monocytes and severe lung pathology in people with COVID‑19.[78] Lymphocytic infiltrates have also been reported at autopsy.[76]
-
Role of B cells in COVID-19 infection/re-infection- Naïve B cells are activated via the help of folliculat T cells after the invasion of SARS-CoV-2 virus[79]
-
Key components of the adaptive immune response to SARS-CoV-2
Viral and host factors
Virus proteins

Multiple viral and host factors affect the pathogenesis of the virus. The S-protein, otherwise known as the spike protein, is the viral component that attaches to the host receptor via the ACE2 receptors. It includes two subunits: S1 and S2. S1 determines the virus-host range and cellular tropism via the receptor-binding domain. S2 mediates the membrane fusion of the virus to its potential cell host via the H1 and HR2, which are heptad repeat regions. Studies have shown that S1 domain induced IgG and IgA antibody levels at a much higher capacity. It is the focus spike proteins expression that are involved in many effective COVID‑19 vaccines.[80]
The M protein is the viral protein responsible for the transmembrane transport of nutrients. It is the cause of the bud release and the formation of the viral envelope.[81] The N and E protein are accessory proteins that interfere with the host's immune response.[81]
Host factors
Human angiotensin converting enzyme 2 (hACE2) is the host factor that SARS-COV2 virus targets causing COVID‑19. Theoretically, the usage of angiotensin receptor blockers (ARB) and ACE inhibitors upregulating ACE2 expression might increase morbidity with COVID‑19, though animal data suggest some potential protective effect of ARB; however no clinical studies have proven susceptibility or outcomes. Until further data is available, guidelines and recommendations for hypertensive patients remain.[82]
The effect of the virus on ACE2 cell surfaces leads to leukocytic infiltration, increased blood vessel permeability, alveolar wall permeability, as well as decreased secretion of lung surfactants. These effects cause the majority of the respiratory symptoms. However, the aggravation of local inflammation causes a cytokine storm eventually leading to a systemic inflammatory response syndrome.[83]
Among healthy adults not exposed to SARS-CoV-2, about 35% have CD4+ T cells that recognize the SARS-CoV-2 S protein (particularly the S2 subunit) and about 50% react to other proteins of the virus, suggesting cross-reactivity from previous common colds caused by other coronaviruses.[84]
It is unknown whether different persons use similar antibody genes in response to COVID‑19.[85]
Host cytokine response

The severity of the inflammation can be attributed to the severity of what is known as the cytokine storm.[86] Levels of interleukin 1B, interferon-gamma, interferon-inducible protein 10, and monocyte chemoattractant protein 1 were all associated with COVID‑19 disease severity. Treatment has been proposed to combat the cytokine storm as it remains to be one of the leading causes of morbidity and mortality in COVID‑19 disease.[87]
A cytokine storm is due to an acute hyperinflammatory response that is responsible for clinical illness in an array of diseases but in COVID‑19, it is related to worse prognosis and increased fatality. The storm causes acute respiratory distress syndrome, blood clotting events such as strokes, myocardial infarction, encephalitis, acute kidney injury, and vasculitis. The production of IL-1, IL-2, IL-6, TNF-alpha, and interferon-gamma, all crucial components of normal immune responses, inadvertently become the causes of a cytokine storm. The cells of the central nervous system, the microglia, neurons, and astrocytes, are also involved in the release of pro-inflammatory cytokines affecting the nervous system, and effects of cytokine storms toward the CNS are not uncommon.[88]
Pregnancy response
There are many unknowns for pregnant women during the COVID‑19 pandemic. Given that they are prone to suffering from complications and severe disease infection with other types of coronaviruses, they have been identified as a vulnerable group and advised to take supplementary preventive measures.[89]
Physiological responses to pregnancy can include:
- Immunological: The immunological response to COVID-19, like other viruses, depends on a working immune system. It adapts during pregnancy to allow the development of the fetus whose genetic load is only partially shared with their mother, leading to a different immunological reaction to infections during the course of pregnancy.[89]
- Respiratory: Many factors can make pregnant women more vulnerable to hard respiratory infections. One of them is the total reduction of the lungs' capacity and inability to clear secretions.[89]
- Coagulation: During pregnancy, there are higher levels of circulating coagulation factors, and the pathogenesis of SARS-CoV-2 infection can be implicated. The thromboembolic events with associated mortality are a risk for pregnant women.[89]
However, from the evidence base, it is difficult to conclude whether pregnant women are at increased risk of grave consequences of this virus.[89]
In addition to the above, other clinical studies have proved that SARS-CoV-2 can affect the period of pregnancy in different ways. On the one hand, there is little evidence of its impact up to 12 weeks gestation. On the other hand, COVID-19 infection may cause increased rates of unfavorable outcomes in the course of the pregnancy. Some examples of these could be fetal growth restriction, preterm birth, and perinatal mortality, which refers to the fetal death past 22 or 28 completed weeks of pregnancy as well as the death among live-born children up to seven completed days of life.[89]
Unvaccinated women in later stages of pregnancy with COVID-19 are more likely than other patients to need very intensive care. Babies born to mothers with COVID-19 are more likely to have breathing problems. Pregnant women are strongly encouraged to get vaccinated.[90]
Diagnosis
COVID-19 can provisionally be diagnosed on the basis of symptoms and confirmed using reverse transcription polymerase chain reaction (RT-PCR) or other nucleic acid testing of infected secretions.[91][92] Along with laboratory testing, chest CT scans may be helpful to diagnose COVID-19 in individuals with a high clinical suspicion of infection.[93] Detection of a past infection is possible with serological tests, which detect antibodies produced by the body in response to the infection.[91]
Viral testing

The standard methods of testing for presence of SARS-CoV-2 are nucleic acid tests,[91][94] which detects the presence of viral RNA fragments.[95] As these tests detect RNA but not infectious virus, its "ability to determine duration of infectivity of patients is limited."[96] The test is typically done on respiratory samples obtained by a nasopharyngeal swab; however, a nasal swab or sputum sample may also be used.[97][98] Results are generally available within hours.[91] The WHO has published several testing protocols for the disease.[99]

Several laboratories and companies have developed serological tests, which detect antibodies produced by the body in response to infection. Several have been evaluated by Public Health England and approved for use in the UK.[100]
The University of Oxford's CEBM has pointed to mounting evidence[101][102] that "a good proportion of 'new' mild cases and people re-testing positives after quarantine or discharge from hospital are not infectious, but are simply clearing harmless virus particles which their immune system has efficiently dealt with" and have called for "an international effort to standardize and periodically calibrate testing"[103] On 7 September, the UK government issued "guidance for procedures to be implemented in laboratories to provide assurance of positive SARS-CoV-2 RNA results during periods of low prevalence, when there is a reduction in the predictive value of positive test results".[104]
Imaging
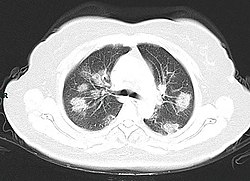
Chest CT scans may be helpful to diagnose COVID-19 in individuals with a high clinical suspicion of infection but are not recommended for routine screening.[93][105] Bilateral multilobar ground-glass opacities with a peripheral, asymmetric, and posterior distribution are common in early infection.[93][106] Subpleural dominance, crazy paving (lobular septal thickening with variable alveolar filling), and consolidation may appear as the disease progresses.[93][107] Characteristic imaging features on chest radiographs and computed tomography (CT) of people who are symptomatic include asymmetric peripheral ground-glass opacities without pleural effusions.[108]
Many groups have created COVID-19 datasets that include imagery such as the Italian Radiological Society which has compiled an international online database of imaging findings for confirmed cases.[109] Due to overlap with other infections such as adenovirus, imaging without confirmation by rRT-PCR is of limited specificity in identifying COVID-19.[108] A large study in China compared chest CT results to PCR and demonstrated that though imaging is less specific for the infection, it is faster and more sensitive.[92]
-
A CT scan of a person with COVID-19 shows lesions (bright regions) in the lungs
-
Chest X-ray showing COVID-19 pneumonia
Pathology
The main pathological findings at autopsy are:
- Macroscopy: pericarditis, lung consolidation and pulmonary oedema[76]
- Lung findings:
- minor serous exudation, minor fibrin exudation[76]
- pulmonary oedema, pneumocyte hyperplasia, large atypical pneumocytes, interstitial inflammation with lymphocytic infiltration and multinucleated giant cell formation[76]
- diffuse alveolar damage (DAD) with diffuse alveolar exudates. DAD is the cause of acute respiratory distress syndrome (ARDS) and severe hypoxemia.[76]
- organisation of exudates in alveolar cavities and pulmonary interstitial fibrosis[76]
- plasmocytosis in BAL[110]
- Blood and vessels: disseminated intravascular coagulation (DIC);[111] leukoerythroblastic reaction,[112] endotheliitis,[113] hemophagocytosis[113]
- Heart: cardiac muscle cell necrosis[113]
- Liver: microvesicular steatosis[76]
- Nose: shedding of olfactory epithelium[56]
- Brain: infarction[113]
- Kidneys: acute tubular damage.[113]
- Spleen: white pulp depletion.[113]
Prevention
Preventive measures to reduce the chances of infection include getting vaccinated, staying at home, wearing a mask in public, avoiding crowded places, keeping distance from others, ventilating indoor spaces, managing potential exposure durations,[115] washing hands with soap and water often and for at least twenty seconds, practising good respiratory hygiene, and avoiding touching the eyes, nose, or mouth with unwashed hands.[116][117]
Those diagnosed with COVID‑19 or who believe they may be infected are advised by the CDC to stay home except to get medical care, call ahead before visiting a healthcare provider, wear a face mask before entering the healthcare provider's office and when in any room or vehicle with another person, cover coughs and sneezes with a tissue, regularly wash hands with soap and water and avoid sharing personal household items.[118][119]
The first COVID‑19 vaccine was granted regulatory approval on 2 December 2020 by the UK medicines regulator MHRA.[120] It was evaluated for emergency use authorization (EUA) status by the US FDA, and in several other countries.[121] Initially, the US National Institutes of Health guidelines do not recommend any medication for prevention of COVID‑19, before or after exposure to the SARS-CoV-2 virus, outside the setting of a clinical trial.[122][123] Without a vaccine, other prophylactic measures, or effective treatments, a key part of managing COVID‑19 is trying to decrease and delay the epidemic peak, known as "flattening the curve".[124] This is done by slowing the infection rate to decrease the risk of health services being overwhelmed, allowing for better treatment of active cases, and delaying additional cases until effective treatments or a vaccine become available.[124][125]
Vaccine
A COVID‑19 vaccine is a vaccine intended to provide acquired immunity against severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2), the virus that causes coronavirus disease 2019 (COVID‑19).
Prior to the COVID‑19 pandemic, an established body of knowledge existed about the structure and function of coronaviruses causing diseases like severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). This knowledge accelerated the development of various vaccine platforms during early 2020.[126] The initial focus of SARS-CoV-2 vaccines was on preventing symptomatic, often severe illness.[127] On 10 January 2020, the SARS-CoV-2 genetic sequence data was shared through GISAID, and by 19 March, the global pharmaceutical industry announced a major commitment to address COVID‑19.[128]
The COVID‑19 vaccines are widely credited for their role in reducing the severity and death caused by COVID‑19.[129][130] Many countries have implemented phased distribution plans that prioritize those at highest risk of complications, such as the elderly, and those at high risk of exposure and transmission, such as healthcare workers.[131]
As of 17 January 2022[update], 9.68 billion doses of COVID‑19 vaccines have been administered worldwide based on official reports from national public health agencies.[132] By December 2020, more than 10 billion vaccine doses had been preordered by countries,[133] with about half of the doses purchased by high-income countries comprising 14% of the world's population.[134]
-
COVID-19 Vaccination Center of the Medical University of Gdańsk, Poland
-
Different vaccine candidate types in development for SARS-CoV-2
Respiratory hygiene

The WHO and the US CDC recommend individuals wear non-medical face coverings in public settings where there is an increased risk of transmission and where social distancing measures are difficult to maintain.[135][136] This recommendation is meant to reduce the spread of the disease by asymptomatic and pre-symptomatic individuals and is complementary to established preventive measures such as social distancing.[136][137] Face coverings limit the volume and travel distance of expiratory droplets dispersed when talking, breathing, and coughing.[136][137] A face covering without vents or holes will also filter out particles containing the virus from inhaled and exhaled air, reducing the chances of infection.[138] But, if the mask include an exhalation valve, a wearer that is infected (maybe without having noticed that, and asymptomatic) would transmit the virus outwards through it, despite any certification they can have. So the masks with exhalation valve are not for the infected wearers, and are not reliable to stop the pandemic in a large scale. Many countries and local jurisdictions encourage or mandate the use of face masks or cloth face coverings by members of the public to limit the spread of the virus.[139]
Masks are also strongly recommended for those who may have been infected and those taking care of someone who may have the disease.[140] When not wearing a mask, the CDC recommends covering the mouth and nose with a tissue when coughing or sneezing and recommends using the inside of the elbow if no tissue is available. Proper hand hygiene after any cough or sneeze is encouraged. Healthcare professionals interacting directly with people who have COVID‑19 are advised to use respirators at least as protective as NIOSH-certified N95 or equivalent, in addition to other personal protective equipment.[141]
Indoor ventilation
The CDC recommends that crowded indoor spaces should be avoided.[142] When indoors, increasing the rate of air change, decreasing recirculation of air and increasing the use of outdoor air can reduce transmission.[142][143] The WHO recommends ventilation and air filtration in public spaces to help clear out infectious aerosols.[144][145][146]
Exhaled respiratory particles can build-up within enclosed spaces with inadequate ventilation. The risk of COVID‑19 infection increases especially in spaces where people engage in physical exertion or raise their voice (e.g., exercising, shouting, singing) as this increases exhalation of respiratory droplets. Prolonged exposure to these conditions, typically more than 15 minutes, leads to higher risk of infection.[142]
Displacement ventilation with large natural inlets can move stale air directly to the exhaust in laminar flow while significantly reducing the concentration of droplets and particles. Passive ventilation reduces energy consumption and maintenance costs but may lack controllability and heat recovery. Displacement ventilation can also be achieved mechanically with higher energy and maintenance costs. The use of large ducts and openings helps to prevent mixing in closed environments. Recirculation and mixing should be avoided because recirculation prevents dilution of harmful particles and redistributes possibly contaminated air, and mixing increases the concentration and range of infectious particles and keeps larger particles in the air.[147]
Hand-washing

Thorough hand hygiene after any cough or sneeze is required.[148] The WHO also recommends that individuals wash hands often with soap and water for at least twenty seconds, especially after going to the toilet or when hands are visibly dirty, before eating and after blowing one's nose.[149] When soap and water are not available, the CDC recommends using an alcohol-based hand sanitiser with at least 60% alcohol.[150] For areas where commercial hand sanitisers are not readily available, the WHO provides two formulations for local production. In these formulations, the antimicrobial activity arises from ethanol or isopropanol. Hydrogen peroxide is used to help eliminate bacterial spores in the alcohol; it is "not an active substance for hand antisepsis." Glycerol is added as a humectant.[151]
Social distancing
Social distancing (also known as physical distancing) includes infection control actions intended to slow the spread of the disease by minimising close contact between individuals. Methods include quarantines; travel restrictions; and the closing of schools, workplaces, stadiums, theatres, or shopping centres. Individuals may apply social distancing methods by staying at home, limiting travel, avoiding crowded areas, using no-contact greetings, and physically distancing themselves from others.[152] Many governments are now mandating or recommending social distancing in regions affected by the outbreak.[153]
Outbreaks have occurred in prisons due to crowding and an inability to enforce adequate social distancing.[154][155] In the United States, the prisoner population is aging and many of them are at high risk for poor outcomes from COVID‑19 due to high rates of coexisting heart and lung disease, and poor access to high-quality healthcare.[154]
Surface cleaning
After being expelled from the body, coronaviruses can survive on surfaces for hours to days. If a person touches the dirty surface, they may deposit the virus at the eyes, nose, or mouth where it can enter the body and cause infection.[156] Evidence indicates that contact with infected surfaces is not the main driver of COVID‑19,[157][158][159] leading to recommendations for optimised disinfection procedures to avoid issues such as the increase of antimicrobial resistance through the use of inappropriate cleaning products and processes.[160][161] Deep cleaning and other surface sanitation has been criticized as hygiene theater, giving a false sense of security against something primarily spread through the air.[162][163]
The amount of time that the virus can survive depends significantly on the type of surface, the temperature, and the humidity.[164] Coronaviruses die very quickly when exposed to the UV light in sunlight.[164] Like other enveloped viruses, SARS-CoV-2 survives longest when the temperature is at room temperature or lower, and when the relative humidity is low (<50%).[164]
On many surfaces, including glass, some types of plastic, stainless steel, and skin, the virus can remain infective for several days indoors at room temperature, or even about a week under ideal conditions.[164][165] On some surfaces, including cotton fabric and copper, the virus usually dies after a few hours.[164] The virus dies faster on porous surfaces than on non-porous surfaces due to capillary action within pores and faster aerosol droplet evaporation.[166][159][164] However, of the many surfaces tested, two with the longest survival times are N95 respirator masks and surgical masks, both of which are considered porous surfaces.[164]
The CDC says that in most situations, cleaning surfaces with soap or detergent, not disinfecting, is enough to reduce risk of transmission.[167][168] The CDC recommends that if a COVID‑19 case is suspected or confirmed at a facility such as an office or day care, all areas such as offices, bathrooms, common areas, shared electronic equipment like tablets, touch screens, keyboards, remote controls, and ATM machines used by the ill persons should be disinfected.[169] Surfaces may be decontaminated with 62–71 percent ethanol, 50–100 percent isopropanol, 0.1 percent sodium hypochlorite, 0.5 percent hydrogen peroxide, and 0.2–7.5 percent povidone-iodine. Other solutions, such as benzalkonium chloride and chlorhexidine gluconate, are less effective. Ultraviolet germicidal irradiation may also be used.[144] A datasheet comprising the authorised substances to disinfection in the food industry (including suspension or surface tested, kind of surface, use dilution, disinfectant and inocuylum volumes) can be seen in the supplementary material of.[160]
Self-isolation
Self-isolation at home has been recommended for those diagnosed with COVID‑19 and those who suspect they have been infected. Health agencies have issued detailed instructions for proper self-isolation.[170] Many governments have mandated or recommended self-quarantine for entire populations. The strongest self-quarantine instructions have been issued to those in high-risk groups.[171] Those who may have been exposed to someone with COVID‑19 and those who have recently travelled to a country or region with the widespread transmission have been advised to self-quarantine for 14 days from the time of last possible exposure.[172]
Diet and lifestyle
The Harvard T.H. Chan School of Public Health recommends a healthy diet, being physically active, managing psychological stress, and getting enough sleep.[173]
Consistently meeting scientific guidelines of 150+ minutes per week of exercise or similar physical activity was shown to be associated with a smaller risk of hospitalisation and death due to COVID‑19, even when considering likely risk factors such as elevated Body mass index (BMI).[174][175]
A meta-analysis, published online in October 2021, concluded that “Vitamin D supplementation in SARS-CoV-2 positive patients has the potential to positively impact patients with both mild and severe symptoms.”[176] The largest observational study on the subject using online questionnaires, with over 6 000 participants and a dosage regime near the RDI, is set to conclude in July 2021.[177][178] One of the collaborators in the study is Synergy Biologics Ltd, a manufacturer of vitamin D3 supplements.[178]
A 2021 Cochrane rapid review found that based upon low-certainty evidence, international travel-related control measures such as restricting cross-border travel may help to contain the spread of COVID‑19.[179] Additionally, symptom/exposure-based screening measures at borders may miss many positive cases.[179] While test-based border screening measures may be more effective, it could also miss many positive cases if only conducted upon arrival without follow-up. The review concluded that a minimum 10-day quarantine may be beneficial in preventing the spread of COVID‑19 and may be more effective if combined with an additional control measure like border screening.[179]
Treatment

There is no specific, effective treatment or cure for coronavirus disease 2019 (COVID-19), the disease caused by the SARS-CoV-2 virus.[180][needs update][181] Thus, the cornerstone of management of COVID-19 is supportive care, which includes treatment to relieve symptoms, fluid therapy, oxygen support and prone positioning as needed, and medications or devices to support other affected vital organs.[182][183][184]
Most cases of COVID-19 are mild. In these, supportive care includes medication such as paracetamol or NSAIDs to relieve symptoms (fever, body aches, cough), proper intake of fluids, rest, and nasal breathing.[185][181][186][187] Good personal hygiene and a healthy diet are also recommended.[188] The U.S. Centers for Disease Control and Prevention (CDC) recommend that those who suspect they are carrying the virus isolate themselves at home and wear a face mask.[189]
People with more severe cases may need treatment in hospital. In those with low oxygen levels, use of the glucocorticoid dexamethasone is strongly recommended, as it can reduce the risk of death.[190][191][192] Noninvasive ventilation and, ultimately, admission to an intensive care unit for mechanical ventilation may be required to support breathing.[193] Extracorporeal membrane oxygenation (ECMO) has been used to address the issue of respiratory failure, but its benefits are still under consideration.[194][195]
Several experimental treatments are being actively studied in clinical trials.[180] Others were thought to be promising early in the pandemic, such as hydroxychloroquine and lopinavir/ritonavir, but later research found them to be ineffective or even harmful.[180][196][197] Despite ongoing research, there is still not enough high-quality evidence to recommend so-called early treatment.[196][197] Nevertheless, in the United States, two monoclonal antibody-based therapies are available for early use in cases thought to be at high risk of progression to severe disease.[197] The antiviral remdesivir is available in the U.S., Canada, Australia, and several other countries, with varying restrictions; however, it is not recommended for people needing mechanical ventilation, and is discouraged altogether by the World Health Organization (WHO),[198] due to limited evidence of its efficacy.[180]Prognosis

The severity of COVID-19 varies. The disease may take a mild course with few or no symptoms, resembling other common upper respiratory diseases such as the common cold. In 3–4% of cases (7.4% for those over age 65) symptoms are severe enough to cause hospitalization.[200] Mild cases typically recover within two weeks, while those with severe or critical diseases may take three to six weeks to recover. Among those who have died, the time from symptom onset to death has ranged from two to eight weeks.[43] The Italian Istituto Superiore di Sanità reported that the median time between the onset of symptoms and death was twelve days, with seven being hospitalised. However, people transferred to an ICU had a median time of ten days between hospitalisation and death.[201] Prolonged prothrombin time and elevated C-reactive protein levels on admission to the hospital are associated with severe course of COVID-19 and with a transfer to ICU.[202][203]
Some early studies suggest 10% to 20% of people with COVID-19 will experience symptoms lasting longer than a month.[204][205] A majority of those who were admitted to hospital with severe disease report long-term problems including fatigue and shortness of breath.[206] On 30 October 2020 WHO chief Tedros Adhanom warned that "to a significant number of people, the COVID virus poses a range of serious long-term effects." He has described the vast spectrum of COVID-19 symptoms that fluctuate over time as "really concerning". They range from fatigue, a cough and shortness of breath, to inflammation and injury of major organs – including the lungs and heart, and also neurological and psychologic effects. Symptoms often overlap and can affect any system in the body. Infected people have reported cyclical bouts of fatigue, headaches, months of complete exhaustion, mood swings, and other symptoms. Tedros has concluded that therefore herd immunity is "morally unconscionable and unfeasible".[207]
In terms of hospital readmissions about 9% of 106,000 individuals had to return for hospital treatment within two months of discharge. The average to readmit was eight days since first hospital visit. There are several risk factors that have been identified as being a cause of multiple admissions to a hospital facility. Among these are advanced age (above 65 years of age) and presence of a chronic condition such as diabetes, COPD, heart failure or chronic kidney disease.[208][209]
According to scientific reviews smokers are more likely to require intensive care or die compared to non-smokers,[210][211] air pollution is similarly associated with risk factors,[211] and pre-existing heart and lung diseases[212] and also obesity contributes to an increased health risk of COVID-19.[211][213][214]
It is also assumed that those that are immunocompromised are at higher risk of getting severely sick from SARS-CoV-2.[215] One research that looked into the COVID-19 infections in hospitalized kidney transplant recipients found a mortality rate of 11%.[216]
Genetics also plays an important role in the ability to fight off the disease.[217] For instance, those that do not produce detectable type I interferons or produce auto-antibodies against these may get much sicker from COVID-19.[218][219] Genetic screening is able to detect interferon effector genes.[220]
Pregnant women may be at higher risk of severe COVID-19 infection based on data from other similar viruses, like SARS and MERS, but data for COVID-19 is lacking.
Children
While very young children have experienced lower rates of infection, older children have a rate of infection that is similar to the population as a whole.[221][222] Children are likely to have milder symptoms and are at lower risk of severe disease than adults. The CDC reports that in the US roughly a third of hospitalized children were admitted to the ICU,[223] while a European multinational study of hospitalized children from June 2020 found that about 8% of children admitted to a hospital needed intensive care.[224] Four of the 582 children (0.7%) in the European study died, but the actual mortality rate could be "substantially lower" since milder cases that did not seek medical help were not included in the study.[225][226]
Complications

Complications may include pneumonia, acute respiratory distress syndrome (ARDS), multi-organ failure, septic shock, and death.[227][228][229][230] Cardiovascular complications may include heart failure, arrhythmias, heart inflammation, and blood clots.[231][232][233][234] Approximately 20–30% of people who present with COVID-19 have elevated liver enzymes, reflecting liver injury.[235][123]
Neurologic manifestations include seizure, stroke, encephalitis, and Guillain–Barré syndrome (which includes loss of motor functions).[236][237] Following the infection, children may develop paediatric multisystem inflammatory syndrome, which has symptoms similar to Kawasaki disease, which can be fatal.[238][239] In very rare cases, acute encephalopathy can occur, and it can be considered in those who have been diagnosed with COVID-19 and have an altered mental status.[240]
In the case of pregnant women, it is important to note that, according to the Centers for Disease Control and Prevention, pregnant women are at increased risk of becoming seriously ill from COVID-19.[241] This is because pregnant women with COVID-19 appear to be more likely to develop respiratory and obstetric complications that can lead to miscarriage, premature delivery and intrauterine growth restriction.[241]
Longer-term effects
Some early studies suggest that that ten to twenty percent of people with COVID-19 will experience symptoms lasting longer than a month.[242][243] A majority of those who were admitted to hospital with severe disease report long-term problems, including fatigue and shortness of breath.[244] About 5-10% of patients admitted to hospital progress to severe or critical disease, including pneumonia and acute respiratory failure.[245]
By a variety of mechanisms, the lungs are the organs most affected in COVID-19.[246] The majority of CT scans performed show lung abnormalities in people tested after 28 days of illness.[247]
People with advanced age, severe disease, prolonged ICU stays, or who smoke are more likely to have long-lasting effects, including pulmonary fibrosis.[248] Overall, approximately one-third of those investigated after four weeks will have findings of pulmonary fibrosis or reduced lung function as measured by DLCO, even in asymptomatic people, but with the suggestion of continuing improvement with the passing of more time.[246]
Immunity

The immune response by humans to CoV-2 virus occurs as a combination of the cell-mediated immunity and antibody production,[249] just as with most other infections.[250] Since SARS-CoV-2 has been in the human population only since December 2019, it remains unknown if the immunity is long-lasting in people who recover from the disease.[251] The presence of neutralizing antibodies in blood strongly correlates with protection from infection, but the level of neutralizing antibody declines with time. Those with asymptomatic or mild disease had undetectable levels of neutralizing antibody two months after infection. In another study, the level of neutralizing antibodies fell four-fold one to four months after the onset of symptoms. However, the lack of antibodies in the blood does not mean antibodies will not be rapidly produced upon reexposure to SARS-CoV-2. Memory B cells specific for the spike and nucleocapsid proteins of SARS-CoV-2 last for at least six months after the appearance of symptoms.[251] Nevertheless, 15 cases of reinfection with SARS-CoV-2 have been reported using stringent CDC criteria requiring identification of a different variant from the second infection. There are likely to be many more people who have been reinfected with the virus. Herd immunity will not eliminate the virus if reinfection is common.[251] Some other coronaviruses circulating in people are capable of reinfection after roughly a year.[252] Nonetheless, on 3 March 2021, scientists reported that a much more contagious COVID-19 variant, Lineage P.1, first detected in Japan, and subsequently found in Brazil, as well as in several places in the United States, may be associated with COVID-19 disease reinfection after recovery from an earlier COVID-19 infection.[253][254]
Mortality
Several measures are commonly used to quantify mortality.[255] These numbers vary by region and over time and are influenced by the volume of testing, healthcare system quality, treatment options, time since the initial outbreak, and population characteristics such as age, sex, and overall health.[256] Data has changed throughout the course of the pandemic, as much within as between countries. However, what has remained constant is the prevalence of women affected by Covid in contrast to men, although the fatalities have not been as high as theirs. This was especially so at the beginning of the pandemic. This might be due to the fact that both professional and home care affairs have been an area relegated to women in history. These are obviously closer to the virus than other areas of work.[257] Regarding age and sex, in India, for instance, COVID-19 cases between men and women did not represent a uniform ratio among different age groups. Mortality rates were higher in women, especially in the 40-49 year age group. The socioeconomic status can also affect the number of people affected by COVID-19. We do not own precise data about this factor, but in other national contexts it has been found that marginalised groups are at higher risk of infection and death.[258] The mortality rate reflects the number of deaths within a specific demographic group divided by the population of that demographic group. Consequently, the mortality rate reflects the prevalence as well as the severity of the disease within a given population. Mortality rates are highly correlated to age, with relatively low rates for young people and relatively high rates among the elderly.[259][260][261] In fact, one relevant factor of mortality rates is the age structure of the countries’ populations. For example, the case fatality rate for COVID-19 is lower in India than in the US since India's younger population represents a larger percentage than in the US.[258]
The case fatality rate (CFR) reflects the number of deaths divided by the number of diagnosed cases within a given time interval. Based on Johns Hopkins University statistics, the global death-to-case ratio is 1.02% (6,881,955/676,609,955) as of 10 March 2023.[9] The number varies by region.[262][263] The CFR may not reflect the true severity of the disease, because some infected individuals remain asymptomatic or experience only mild symptoms, and hence such infections may not be included in official case reports. Moreover, the CFR may vary markedly over time and across locations due to the availability of live virus tests.
Infection fatality rate


A key metric in gauging the severity of COVID-19 is the infection fatality rate (IFR), also referred to as the infection fatality ratio or infection fatality risk.[265][266][267] This metric is calculated by dividing the total number of deaths from the disease by the total number of infected individuals; hence, in contrast to the CFR, the IFR incorporates asymptomatic and undiagnosed infections as well as reported cases.[268]
A December 2020 systematic review and meta-analysis estimated that population IFR during the first wave of the pandemic was about 0.5% to 1% in many locations (including France, Netherlands, New Zealand, and Portugal), 1% to 2% in other locations (Australia, England, Lithuania, and Spain), and exceeded 2% in Italy.[264] That study also found that most of these differences in IFR reflected corresponding differences in the age composition of the population and age-specific infection rates; in particular, the metaregression estimate of IFR is very low for children and younger adults (e.g., 0.002% at age 10 and 0.01% at age 25) but increases progressively to 0.4% at age 55, 1.4% at age 65, 4.6% at age 75, and 15% at age 85.[264] These results were also highlighted in a December 2020 report issued by the WHO.[269]
Earlier estimates
At an early stage of the pandemic, the World Health Organization reported estimates of IFR between 0.3% and 1%.[270][271] On 2 July, The WHO's chief scientist reported that the average IFR estimate presented at a two-day WHO expert forum was about 0.6%.[272][273] In August, the WHO found that studies incorporating data from broad serology testing in Europe showed IFR estimates converging at approximately 0.5–1%.[274] Firm lower limits of IFRs have been established in a number of locations such as New York City and Bergamo in Italy since the IFR cannot be less than the population fatality rate. As of 10 July, in New York City, with a population of 8.4 million, 23,377 individuals (18,758 confirmed and 4,619 probable) have died with COVID-19 (0.3% of the population).[275] Antibody testing in New York City suggested an IFR of ~0.9%,[276] and ~1.4%.[277] In Bergamo province, 0.6% of the population has died.[278] In September 2020 the U.S. Center for Disease Control & Prevention reported preliminary estimates of age-specific IFRs for public health planning purposes.[279]
Sex differences
| Percentage of infected people who are hospitalized | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.1 (0.07–0.2) |
0.5 (0.3–0.8) |
0.9 (0.5–1.5) |
1.3 (0.7–2.1) |
2.6 (1.5–4.2) |
5.1 (2.9–8.3) |
7.8 (4.4–12.8) |
19.3 (10.9–31.6) |
2.6 (1.5–4.3) |
| Male | 0.2 (0.08–0.2) |
0.6 (0.3–0.9) |
1.2 (0.7–1.9) |
1.6 (0.9–2.6) |
3.2 (1.8–5.2) |
6.7 (3.7–10.9) |
11.0 (6.2–17.9) |
37.6 (21.1–61.3) |
3.3 (1.8–5.3) |
| Total | 0.1 (0.08–0.2) |
0.5 (0.3–0.8) |
1.1 (0.6–1.7) |
1.4 (0.8–2.3) |
2.9 (1.6–4.7) |
5.8 (3.3–9.5) |
9.3 (5.2–15.1) |
26.2 (14.8–42.7) |
2.9 (1.7–4.8) |
| Percentage of hospitalized people who go to Intensive Care Unit | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 16.7 (14.3–19.3) |
8.7 (7.5–9.9) |
11.9 (10.9–13.0) |
16.6 (15.6–17.7) |
20.7 (19.8–21.6) |
23.1 (22.2–24.0) |
18.7 (18.0–19.5) |
4.2 (4.0–4.5) |
14.3 (13.9–14.7) |
| Male | 26.9 (23.1–31.1) |
14.0 (12.2–16.0) |
19.2 (17.6–20.9) |
26.9 (25.4–28.4) |
33.4 (32.0–34.8) |
37.3 (36.0–38.6) |
30.2 (29.1–31.3) |
6.8 (6.5–7.2) |
23.1 (22.6–23.6) |
| Total | 22.2 (19.1–25.7) |
11.6 (10.1–13.2) |
15.9 (14.5–17.3) |
22.2 (21.0–23.5) |
27.6 (26.5–28.7) |
30.8 (29.8–31.8) |
24.9 (24.1–25.8) |
5.6 (5.3–5.9) |
19.0 (18.7–19.44) |
| Percent of hospitalized people who die | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.5 (0.2–1.0) |
0.9 (0.5–1.3) |
1.5 (1.2–1.9) |
2.6 (2.3–3.0) |
5.2 (4.8–5.6) |
10.1 (9.5–10.6) |
16.7 (16.0–17.4) |
25.2 (24.4–26.0) |
14.4 (14.0–14.8) |
| Male | 0.7 (0.3–1.5) |
1.3 (0.8–1.9) |
2.2 (1.7–2.7) |
3.8 (3.3–4.4) |
7.6 (7.0–8.2) |
14.8 (14.1–15.6) |
24.6 (23.7–25.6) |
37.1 (36.1–38.2) |
21.2 (20.8–21.7) |
| Total | 0.6 (0.2–1.3) |
1.1 (0.7–1.6) |
1.9 (1.5–2.3) |
3.3 (2.9–3.8) |
6.5 (6.0–7.0) |
12.6 (12.0–13.2) |
21.0 (20.3–21.7) |
31.6 (30.9–32.4) |
18.1 (17.8–18.4) |
| Percent of infected people who die – infection fatality rate (IFR) | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.001 (<0.001–0.002) |
0.004 (0.002–0.007) |
0.01 (0.007–0.02) |
0.03 (0.02–0.06) |
0.1 (0.08–0.2) |
0.5 (0.3–0.8) |
1.3 (0.7–2.1) |
4.9 (2.7–8.0) |
0.4 (0.2–0.6) |
| Male | 0.001 (<0.001–0.003) |
0.007 (0.003–0.01) |
0.03 (0.02–0.05) |
0.06 (0.03–0.1) |
0.2 (0.1–0.4) |
1.0 (0.6–1.6) |
2.7 (1.5–1.4) |
14.0 (7.9–22.7) |
0.7 (0.4–1.1) |
| Total | 0.001 (<0.001–0.002) |
0.005 (0.003–0.01) |
0.02 (0.01–0.03) |
0.05 (0.03–0.08) |
0.2 (0.1–0.3) |
0.7 (0.4–1.2) |
1.9 (1.1–3.2) |
8.3 (4.7–13.5) |
0.5 (0.3–0.9) |
| Numbers in parentheses are 95% credible intervals for the estimates. | |||||||||
Early reviews of epidemiologic data showed gendered impact of the pandemic and a higher mortality rate in men in China and Italy.[281][282][283] According to global data, COVID-19 case fatality rates are higher among men than women in most countries. However, in a few countries like India, Nepal, Vietnam, and Slovenia the fatality cases are higher in women than men.[258] This might be due to the fact that both professional and home care affairs have been an area relegated to women in history. These are obviously closer to the virus than other areas of work. For example, in Spain since the sanitary crisis began, healthcare workers have been more affected than anyone else. Almost 50,000 of them have been affected, of whom a 66% are women.[257]
The Chinese Center for Disease Control and Prevention reported the death rate was 2.8% for men and 1.7% for women.[284] Later reviews in June 2020 indicated that there is no significant difference in susceptibility or in CFR between genders.[285][286] One review acknowledges the different mortality rates in Chinese men, suggesting that it may be attributable to lifestyle choices such as smoking and drinking alcohol rather than genetic factors.[287] Smoking, which in some countries like China is mainly a male activity, is a habit that contributes to increasing significantly the case fatality rates among men.[258] Sex-based immunological differences, lesser prevalence of smoking in women and men developing co-morbid conditions such as hypertension at a younger age than women could have contributed to the higher mortality in men.[288] In Europe, 57% of the infected people were men and 72% of those died with COVID-19 were men.[289] The fact that women boast a longer life expectancy than men also makes a bigger group of female population at risk of contracting the disease. Not only that, it also creates an ageist dynamic that can end up in discrimination for being both a woman and old.[257] As of April 2020, the US government is not tracking sex-related data of COVID-19 infections.[290] Research has shown that viral illnesses like Ebola, HIV, influenza and SARS affect men and women differently.[290] The WHO issued a report in 2007 that showed that more than half the SARS cases at the beginning of 2000 were women.[257]
Regarding the spread of information about COVID-19, many researchers and experts agreed that data on COVID-19 infection should be sex-disaggregated. This would allow researchers to develop solutions to the pandemic from a gender-equitable perspective, given sex differences in fatality rates. Also, this would allow experts to deliver high-quality data separately to men and women.[258]
Ethnic differences
In the US, a greater proportion of deaths due to COVID-19 have occurred among African Americans and other minority groups.[291] Structural factors that prevent them from practicing social distancing include their concentration in crowded substandard housing and in "essential" occupations such as retail grocery workers, public transit employees, health-care workers and custodial staff. Greater prevalence of lacking health insurance and care of underlying conditions such as diabetes, hypertension, and heart disease also increase their risk of death.[292] Similar issues affect Native American and Latino communities.[291] On the one hand, in the Dominican Republic there is a clear example of both gender and ethnic inequality. In this Latin American territory, there is great inequality and precariousness that especially affects Dominican women, with greater emphasis on those of Haitian descent.[293] According to a US health policy non-profit, 34% of American Indian and Alaska Native People (AIAN) non-elderly adults are at risk of serious illness compared to 21% of white non-elderly adults.[294] The source attributes it to disproportionately high rates of many health conditions that may put them at higher risk as well as living conditions like lack of access to clean water.[295] Leaders have called for efforts to research and address the disparities.[296] In the U.K., a greater proportion of deaths due to COVID-19 have occurred in those of a Black, Asian, and other ethnic minority background.[297][298][299] More severe impacts upon victims including the relative incidence of the necessity of hospitalization requirements, and vulnerability to the disease has been associated via DNA analysis to be expressed in genetic variants at chromosomal region 3, features that are associated with European Neanderthal heritage. That structure imposes greater risks that those affected will develop a more severe form of the disease.[300] The findings are from Professor Svante Pääbo and researchers he leads at the Max Planck Institute for Evolutionary Anthropology and the Karolinska Institutet.[300] This admixture of modern human and Neanderthal genes is estimated to have occurred roughly between 50,000 and 60,000 years ago in Southern Europe.[300]
Comorbidities
Biological factors (immune response) and the general behaviour (habits) can strongly determine the consequences of COVID-19.[258] Most of those who die of COVID-19 have pre-existing (underlying) conditions, including hypertension, diabetes mellitus, and cardiovascular disease.[301] According to March data from the United States, 89% of those hospitalised had preexisting conditions.[302] The Italian Istituto Superiore di Sanità reported that out of 8.8% of deaths where medical charts were available, 96.1% of people had at least one comorbidity with the average person having 3.4 diseases.[201] According to this report the most common comorbidities are hypertension (66% of deaths), type 2 diabetes (29.8% of deaths), Ischemic Heart Disease (27.6% of deaths), atrial fibrillation (23.1% of deaths) and chronic renal failure (20.2% of deaths).
Most critical respiratory comorbidities according to the CDC, are: moderate or severe asthma, pre-existing COPD, pulmonary fibrosis, cystic fibrosis.[303] Evidence stemming from meta-analysis of several smaller research papers also suggests that smoking can be associated with worse outcomes.[304][305] When someone with existing respiratory problems is infected with COVID-19, they might be at greater risk for severe symptoms.[306] COVID-19 also poses a greater risk to people who misuse opioids and methamphetamines, insofar as their drug use may have caused lung damage.[307]
In August 2020 the CDC issued a caution that tuberculosis (TB) infections could increase the risk of severe illness or death. The WHO recommended that people with respiratory symptoms be screened for both diseases, as testing positive for COVID-19 could not rule out co-infections. Some projections have estimated that reduced TB detection due to the pandemic could result in 6.3 million additional TB cases and 1.4 million TB-related deaths by 2025.[308]
History
The virus is thought to be natural and of an animal origin,[40] through spillover infection.[309] There are several theories about where the first case (the so-called patient zero) originated.[310] Phylogenetics estimates that SARS-CoV-2 arose in October or November 2019.[311][312][313] Evidence suggests that it descends from a coronavirus that infects wild bats, and spread to humans through an intermediary wildlife host.[314][315]
The first known human infections were in Wuhan, Hubei, China. A study of the first 41 cases of confirmed COVID-19, published in January 2020 in The Lancet, reported the earliest date of onset of symptoms as 1 December 2019.[316][317][318] Official publications from the WHO reported the earliest onset of symptoms as 8 December 2019.[319] Human-to-human transmission was confirmed by the WHO and Chinese authorities by 20 January 2020.[320][321] According to official Chinese sources, these were mostly linked to the Huanan Seafood Wholesale Market, which also sold live animals.[322] In May 2020 George Gao, the director of the CDC, said animal samples collected from the seafood market had tested negative for the virus, indicating that the market was the site of an early superspreading event, but that it was not the site of the initial outbreak.[323] Traces of the virus have been found in wastewater samples that were collected in Milan and Turin, Italy, on 18 December 2019.[324]
By December 2019, the spread of infection was almost entirely driven by human-to-human transmission.[325][326] The number of coronavirus cases in Hubei gradually increased, reaching sixty by 20 December,[327] and at least 266 by 31 December.[328] On 24 December, Wuhan Central Hospital sent a bronchoalveolar lavage fluid (BAL) sample from an unresolved clinical case to sequencing company Vision Medicals. On 27 and 28 December, Vision Medicals informed the Wuhan Central Hospital and the Chinese CDC of the results of the test, showing a new coronavirus.[329] A pneumonia cluster of unknown cause was observed on 26 December and treated by the doctor Zhang Jixian in Hubei Provincial Hospital, who informed the Wuhan Jianghan CDC on 27 December.[330] On 30 December, a test report addressed to Wuhan Central Hospital, from company CapitalBio Medlab, stated an erroneous positive result for SARS, causing a group of doctors at Wuhan Central Hospital to alert their colleagues and relevant hospital authorities of the result. The Wuhan Municipal Health Commission issued a notice to various medical institutions on "the treatment of pneumonia of unknown cause" that same evening.[331] Eight of these doctors, including Li Wenliang (punished on 3 January),[332] were later admonished by the police for spreading false rumours and another, Ai Fen, was reprimanded by her superiors for raising the alarm.[333]
The Wuhan Municipal Health Commission made the first public announcement of a pneumonia outbreak of unknown cause on 31 December, confirming 27 cases[334][335][336] – enough to trigger an investigation.[337]
During the early stages of the outbreak, the number of cases doubled approximately every seven and a half days.[338] In early and mid-January 2020, the virus spread to other Chinese provinces, helped by the Chinese New Year migration and Wuhan being a transport hub and major rail interchange.[43] On 20 January, China reported nearly 140 new cases in one day, including two people in Beijing and one in Shenzhen.[339] Later official data shows 6,174 people had already developed symptoms by then,[340] and more may have been infected.[341] A report in The Lancet on 24 January indicated human transmission, strongly recommended personal protective equipment for health workers, and said testing for the virus was essential due to its "pandemic potential".[65][342] On 30 January, the WHO declared the coronavirus a Public Health Emergency of International Concern.[341] By this time, the outbreak spread by a factor of 100 to 200 times.[343]
Italy had its first confirmed cases on 31 January 2020, two tourists from China.[344] As of 13 March 2020 the WHO considered Europe the active centre of the pandemic.[345][unreliable source] Italy overtook China as the country with the most deaths on 19 March 2020 .[346] By 26 March the United States had overtaken China and Italy with the highest number of confirmed cases in the world.[347] Research on coronavirus genomes indicates the majority of COVID-19 cases in New York came from European travellers, rather than directly from China or any other Asian country.[348] Retesting of prior samples found a person in France who had the virus on 27 December 2019,[349][350] and a person in the United States who died from the disease on 6 February 2020.[351]
RT-PCR testing of untreated wastewater samples from Brazil and Italy have suggested detection of SARS-CoV-2 as early as November and December 2019, respectively, but the methods of such sewage studies have not been optimised, many have not been peer-reviewed, details are often missing, and there is a risk of false positives due to contamination or if only one gene target is detected.[352] A September 2020 review journal article said, "The possibility that the COVID-19 infection had already spread to Europe at the end of last year is now indicated by abundant, even if partially circumstantial, evidence," including pneumonia case numbers and radiology in France and Italy in November and December.[353]
Society and culture
Name
During the initial outbreak in Wuhan, China, the virus and disease were commonly referred to as "coronavirus" and "Wuhan coronavirus",[354][355][356] with the disease sometimes called "Wuhan pneumonia".[357][358] In the past, many diseases have been named after geographical locations, such as the Spanish flu,[359] Middle East Respiratory Syndrome, and Zika virus.[360] In January 2020, the WHO recommended 2019-nCov[361] and 2019-nCoV acute respiratory disease[362] as interim names for the virus and disease per 2015 guidance and international guidelines against using geographical locations (e.g. Wuhan, China), animal species, or groups of people in disease and virus names in part to prevent social stigma.[363][364][365] The official names COVID-19 and SARS-CoV-2 were issued by the WHO on 11 February 2020.[366] Tedros Adhanom explained: CO for corona, VI for virus, D for disease and 19 for when the outbreak was first identified (31 December 2019).[367] The WHO additionally uses "the COVID-19 virus" and "the virus responsible for COVID-19" in public communications.[366]
Pharmacy trade
There was a report[368] on 3 March 2021, that social distancing and common wearing of surgical masks and similar as a common precaution against COVID-19 caused such a drop in the spread rate of the common cold and flu that in Britain the sale of cough liquids and throat lozenges and decongestants from 30 November 2020 to 21 February 2021, was about a half of the sale a year earlier, and that Public Health England reported no cases of flu in the year 2021 to date, and that there was an 89% rise in sales of Vitamin D to try to boost immunity.
Misinformation
After the initial outbreak of COVID-19, misinformation and disinformation regarding the origin, scale, prevention, treatment, and other aspects of the disease rapidly spread online.[369][370][371]
In September 2020, the U.S. CDC published preliminary estimates of the risk of death by age groups in the United States, but those estimates were widely misreported and misunderstood.[372][373]
Other animals
Humans appear to be capable of spreading the virus to some other animals, a type of disease transmission referred to as zooanthroponosis.
Some pets, especially cats and ferrets, can catch this virus from infected humans.[374][375] Symptoms in cats include respiratory (such as a cough) and digestive symptoms.[374] Cats can spread the virus to other cats, and may be able to spread the virus to humans, but cat-to-human transmission of SARS-CoV-2 has not been proven.[374][376] Compared to cats, dogs are less susceptible to this infection.[376] Behaviors which increase the risk of transmission include kissing, licking, and petting the animal.[376]
The virus does not appear to be able to infect pigs, ducks, or chickens at all.[374] Mice, rats, and rabbits, if they can be infected at all, are unlikely to be involved in spreading the virus.[376]
Tigers and lions in zoos have become infected as a result of contact with infected humans.[376] As expected, monkeys and great ape species such as orangutans can also be infected with the COVID-19 virus.[376]
Minks, which are in the same family as ferrets, have been infected.[376] Minks may be asymptomatic, and can also spread the virus to humans.[376] Multiple countries have identified infected animals in mink farms.[377] Denmark, a major producer of mink pelts, ordered the slaughter of all minks over fears of viral mutations.[377] A vaccine for mink and other animals is being researched.[377]
Research
International research on vaccines and medicines in COVID-19 is underway by government organisations, academic groups, and industry researchers.[378][379] The CDC has classified it to require a BSL3 grade laboratory.[380] There has been a great deal of COVID-19 research, involving accelerated research processes and publishing shortcuts to meet the global demand.[381]
As of December 2020[update], hundreds of clinical trials have been undertaken, with research happening on every continent except Antarctica.[382] As of November 2020[update], more than 200 possible treatments had been studied in humans so far.[383]
Spread and prevention
Modelling research has been conducted with several objectives, including predictions of the dynamics of transmission,[384] diagnosis and prognosis of infection,[385][needs update] estimation of the impact of interventions,[386][387] or allocation of resources.[388] Modelling studies are mostly based on epidemiological models,[389] estimating the number of infected people over time under given conditions. Several other types of models have been developed and used during the COVID-19 including computational fluid dynamics models to study the flow physics of COVID-19,[390] retrofits of crowd movement models to study occupant exposure,[391] mobility-data based models to investigate transmission,[392] or the use of macroeconomic models to assess the economic impact of the pandemic.[393] Further, conceptual frameworks from crisis management research have been applied to better understand the effects of COVID-19 on organizations worldwide.[394][395]
Treatment

Repurposed antiviral drugs make up most of the research into COVID-19 treatments.[396][397] Other candidates in trials include vasodilators, corticosteroids, immune therapies, lipoic acid, bevacizumab, and recombinant angiotensin-converting enzyme 2.[397]
In March 2020, the World Health Organization (WHO) initiated the Solidarity trial to assess the treatment effects of some promising drugs: an experimental drug called remdesivir; anti-malarial drugs chloroquine and hydroxychloroquine; two anti-HIV drugs, lopinavir/ritonavir; and interferon-beta.[398][399] More than 300 active clinical trials are underway as of April 2020.[123]
Research on the antimalarial drugs hydroxychloroquine and chloroquine showed that they were ineffective at best,[400][401] and that they may reduce the antiviral activity of remdesivir.[402] By May 2020[update], France, Italy, and Belgium had banned the use of hydroxychloroquine as a COVID-19 treatment.[403]
In June, initial results from the randomised RECOVERY Trial in the United Kingdom showed that dexamethasone reduced mortality by one third for people who are critically ill on ventilators and one fifth for those receiving supplemental oxygen.[404] Because this is a well-tested and widely available treatment, it was welcomed by the WHO, which is in the process of updating treatment guidelines to include dexamethasone and other steroids.[405][406] Based on those preliminary results, dexamethasone treatment has been recommended by the NIH for patients with COVID-19 who are mechanically ventilated or who require supplemental oxygen but not in patients with COVID-19 who do not require supplemental oxygen.[407]
In September 2020, the WHO released updated guidance on using corticosteroids for COVID-19.[408] The WHO recommends systemic corticosteroids rather than no systemic corticosteroids for the treatment of people with severe and critical COVID-19 (strong recommendation, based on moderate certainty evidence).[408] The WHO suggests not to use corticosteroids in the treatment of people with non-severe COVID-19 (conditional recommendation, based on low certainty evidence).[408] The updated guidance was based on a meta-analysis of clinical trials of critically ill COVID-19 patients.[409][410]
In September 2020, the European Medicines Agency (EMA) endorsed the use of dexamethasone in adults and adolescents from twelve years of age and weighing at least 40 kilograms (88 lb) who require supplemental oxygen therapy.[411][412] Dexamethasone can be taken by mouth or given as an injection or infusion (drip) into a vein.[411]
In November 2020, the U.S. Food and Drug Administration (FDA) issued an emergency use authorization for the investigational monoclonal antibody therapy bamlanivimab for the treatment of mild-to-moderate COVID-19.[413] Bamlanivimab is authorized for people with positive results of direct SARS-CoV-2 viral testing who are twelve years of age and older weighing at least 40 kilograms (88 lb), and who are at high risk for progressing to severe COVID-19 or hospitalization.[413] This includes those who are 65 years of age or older, or who have chronic medical conditions.[413]
In February 2021, the FDA issued an emergency use authorization (EUA) for bamlanivimab and etesevimab administered together for the treatment of mild to moderate COVID‑19 in people twelve years of age or older weighing at least 40 kilograms (88 lb) who test positive for SARS‑CoV‑2 and who are at high risk for progressing to severe COVID‑19. The authorized use includes treatment for those who are 65 years of age or older or who have certain chronic medical conditions.[414]
In April 2021, the FDA revoked the emergency use authorization (EUA) that allowed for the investigational monoclonal antibody therapy bamlanivimab, when administered alone, to be used for the treatment of mild-to-moderate COVID-19 in adults and certain pediatric patients.[415]
See also
- Coronavirus diseases, a group of closely related syndromes
- Disease X, a WHO term
References
- ↑ "Covid-19". Oxford English Dictionary (3rd ed.). Oxford University Press. April 2020. Retrieved 15 April 2020. (Subscription or UK public library membership required.)
- ↑ 2.0 2.1 2.2 2.3 "Coronavirus Disease 2019 (COVID-19) – Symptoms". Centers for Disease Control and Prevention. 22 February 2021. Archived from the original on 30 January 2020. Retrieved 19 January 2022.
- ↑ 3.0 3.1 Ma, Q; Liu, J; Liu, Q; Kang, L; Liu, R; Jing, W; Wu, Y; Liu, M (1 December 2021). "Global Percentage of Asymptomatic SARS-CoV-2 Infections Among the Tested Population and Individuals With Confirmed COVID-19 Diagnosis: A Systematic Review and Meta-analysis". JAMA network open. 4 (12): e2137257. doi:10.1001/jamanetworkopen.2021.37257. PMID 34905008.
- ↑ "Coronavirus disease 2019 (COVID-19) - Complications | BMJ Best Practice US". bestpractice.bmj.com. Archived from the original on 19 January 2022. Retrieved 19 January 2022.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 "Coronavirus disease (COVID-19)". www.who.int. Archived from the original on 31 March 2020. Retrieved 19 January 2022.
- ↑ 6.0 6.1 "Quarantine & Isolation". Centers for Disease Control and Prevention. 9 January 2022. Archived from the original on 17 January 2022. Retrieved 19 January 2022.
- ↑ 7.0 7.1 "COVID-19 and Your Health". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 28 December 2021. Retrieved 19 January 2022.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 "Clinical Management Summary". COVID-19 Treatment Guidelines. Archived from the original on 5 November 2021. Retrieved 19 January 2022.
- ↑ 9.0 9.1 9.2 "COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)". ArcGIS. Johns Hopkins University. Retrieved 10 March 2023.
- ↑ 10.0 10.1 Wang, Haidong; Paulson, Katherine R; Pease, Spencer A; Watson, Stefanie; Comfort, Haley; Zheng, Peng; Aravkin, Aleksandr Y; Bisignano, Catherine; Barber, Ryan M; Alam, Tahiya; Fuller, John E; May, Erin A; Jones, Darwin Phan; Frisch, Meghan E; Abbafati, Cristiana; Adolph, Christopher; Allorant, Adrien; Amlag, Joanne O; Bang-Jensen, Bree; Bertolacci, Gregory J; Bloom, Sabina S; Carter, Austin; Castro, Emma; Chakrabarti, Suman; Chattopadhyay, Jhilik; Cogen, Rebecca M; Collins, James K; Cooperrider, Kimberly; Dai, Xiaochen; Dangel, William James; Daoud, Farah; Dapper, Carolyn; Deen, Amanda; Duncan, Bruce B; Erickson, Megan; Ewald, Samuel B; Fedosseeva, Tatiana; Ferrari, Alize J; Frostad, Joseph Jon; Fullman, Nancy; Gallagher, John; Gamkrelidze, Amiran; Guo, Gaorui; He, Jiawei; Helak, Monika; Henry, Nathaniel J; Hulland, Erin N; Huntley, Bethany M; Kereselidze, Maia; Lazzar-Atwood, Alice; LeGrand, Kate E; Lindstrom, Akiaja; Linebarger, Emily; Lotufo, Paulo A; Lozano, Rafael; Magistro, Beatrice; Malta, Deborah Carvalho; Månsson, Johan; Mantilla Herrera, Ana M; Marinho, Fatima; Mirkuzie, Alemnesh H; Misganaw, Awoke Temesgen; Monasta, Lorenzo; Naik, Paulami; Nomura, Shuhei; O'Brien, Edward G; O'Halloran, James Kevin; Olana, Latera Tesfaye; Ostroff, Samuel M; Penberthy, Louise; Reiner Jr, Robert C; Reinke, Grace; Ribeiro, Antonio Luiz P; Santomauro, Damian Francesco; Schmidt, Maria Inês; Shaw, David H; Sheena, Brittney S; Sholokhov, Aleksei; Skhvitaridze, Natia; Sorensen, Reed J D; Spurlock, Emma Elizabeth; Syailendrawati, Ruri; Topor-Madry, Roman; Troeger, Christopher E; Walcott, Rebecca; Walker, Ally; Wiysonge, Charles Shey; Worku, Nahom Alemseged; Zigler, Bethany; Pigott, David M; Naghavi, Mohsen; Mokdad, Ali H; Lim, Stephen S; Hay, Simon I; Gakidou, Emmanuela; Murray, Christopher J L (April 2022). "Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21". The Lancet. 399 (10334): 1513–1536. doi:10.1016/S0140-6736(21)02796-3.
- ↑ 11.0 11.1 "COVID-19 and Your Health". Centers for Disease Control and Prevention. 14 July 2021. Archived from the original on 3 April 2020. Retrieved 19 January 2022.
- ↑ 12.0 12.1 "Coronavirus disease (COVID-19): How is it transmitted?". World Health Organization (WHO). Archived from the original on 15 October 2020. Retrieved 6 December 2020.
- ↑ "Transmission of COVID-19". European Centre for Disease Prevention and Control. Archived from the original on 14 September 2020. Retrieved 6 December 2020.
- ↑ "Healthcare Workers". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 6 June 2021. Retrieved 19 January 2022.
- ↑ "Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis". BMJ (Clinical research ed.). 375: n2997. 3 December 2021. doi:10.1136/bmj.n2997. PMID 34862160.
- ↑ "COVID-19 and Your Health". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 14 January 2022. Retrieved 19 January 2022.
- ↑ Page J, Hinshaw D, McKay B (26 February 2021). "In Hunt for Covid-19 Origin, Patient Zero Points to Second Wuhan Market – The man with the first confirmed infection of the new coronavirus told the WHO team that his parents had shopped there". The Wall Street Journal. Archived from the original on 24 May 2021. Retrieved 27 February 2021.
- ↑ Zimmer C (26 February 2021). "The Secret Life of a Coronavirus – An oily, 100-nanometer-wide bubble of genes has killed more than two million people and reshaped the world. Scientists don't quite know what to make of it". Archived from the original on 27 February 2021. Retrieved 28 February 2021.
- ↑ "Symptoms of Coronavirus". U.S. Centers for Disease Control and Prevention (CDC). 2021-02-22. Archived from the original on 2021-03-04. Retrieved 2021-03-04.
- ↑ Grant MC, Geoghegan L, Arbyn M, Mohammed Z, McGuinness L, Clarke EL, Wade RG (23 June 2020). "The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries". PLOS ONE. 15 (6): e0234765. Bibcode:2020PLoSO..1534765G. doi:10.1371/journal.pone.0234765. PMC 7310678. PMID 32574165. S2CID 220046286.
- ↑ Islam MA (November 2020). "Prevalence of Headache in Patients With Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis of 14,275 Patients". Frontiers in Neurology. 11: 562634. doi:10.3389/fneur.2020.562634. PMC 7728918. PMID 33329305.
- ↑ Saniasiaya J, Islam MA (April 2021). "Prevalence of Olfactory Dysfunction in Coronavirus Disease 2019 (COVID-19): A Meta-analysis of 27,492 Patients". The Laryngoscope. 131 (4): 865–878. doi:10.1002/lary.29286. PMC 7753439. PMID 33219539.
- ↑ Saniasiaya J, Islam MA (November 2020). "Prevalence and Characteristics of Taste Disorders in Cases of COVID-19: A Meta-analysis of 29,349 Patients". Otolaryngology–Head and Neck Surgery: 1–10. doi:10.1177/0194599820981018. PMID 33320033.
- ↑ Islam MA (April 2021). "Prevalence and characteristics of fever in adult and paediatric patients with coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis of 17515 patients". PLOS ONE. 16 (4): e0249788. doi:10.1371/journal.pone.0249788. PMC 8023501. PMID 33822812.
- ↑ 25.0 25.1 "Clinical characteristics of COVID-19". European Centre for Disease Prevention and Control. Archived from the original on 2020-12-29. Retrieved 2020-12-29.
- ↑ Niazkar HR, Zibaee B, Nasimi A, Bahri N (July 2020). "The neurological manifestations of COVID-19: a review article". Neurological Sciences. 41 (7): 1667–1671. doi:10.1007/s10072-020-04486-3. PMC 7262683. PMID 32483687.
- ↑ "Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 6 April 2020. Archived from the original on 2 March 2020. Retrieved 19 April 2020.
- ↑ Oran DP, Topol EJ (January 2021). "The Proportion of SARS-CoV-2 Infections That Are Asymptomatic : A Systematic Review". Annals of Internal Medicine. doi:10.7326/M20-6976. PMC 7839426. PMID 33481642.
- ↑ "Transmission of COVID-19". European Centre for Disease Prevention and Control. Archived from the original on 2020-09-14. Retrieved 2020-12-06.
- ↑ Nogrady B (November 2020). "What the data say about asymptomatic COVID infections". Nature. 587 (7835): 534–535. Bibcode:2020Natur.587..534N. doi:10.1038/d41586-020-03141-3. PMID 33214725.
- ↑ 31.0 31.1 Gao Z, Xu Y, Sun C, Wang X, Guo Y, Qiu S, Ma K (February 2021). "A systematic review of asymptomatic infections with COVID-19". Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. 54 (1): 12–16. doi:10.1016/j.jmii.2020.05.001. PMC 7227597. PMID 32425996.
- ↑ Oran, Daniel P., and Eric J. Topol. “Prevalence of Asymptomatic SARS-CoV-2 Infection : A Narrative Review.” Annals of Internal Medicine. vol. 173,5 (2020): 362-367. doi:10.7326/M20-3012 PMID 32491919 Archived 2020-12-03 at the Wayback Machine Retrieved 14 January 2021.
- ↑ Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, et al. (June 2020). "Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths". Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. 53 (3): 404–412. doi:10.1016/j.jmii.2020.02.012. PMC 7128959. PMID 32173241.
- ↑ 34.0 34.1 Furukawa NW, Brooks JT, Sobel J (July 2020). "Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic". Emerging Infectious Diseases. 26 (7). doi:10.3201/eid2607.201595. PMC 7323549. PMID 32364890.
- ↑ 35.0 35.1 Gandhi RT, Lynch JB, Del Rio C (October 2020). "Mild or Moderate Covid-19". The New England Journal of Medicine. 383 (18): 1757–1766. doi:10.1056/NEJMcp2009249. PMID 32329974.
- ↑ Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC (August 2020). "Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review". JAMA. 324 (8): 782–793. doi:10.1001/jama.2020.12839. PMID 32648899. S2CID 220465311.
- ↑ CDC (2020-02-11). "COVID-19 and Your Health". Centers for Disease Control and Prevention. Archived from the original on 2021-05-13. Retrieved 2021-01-23.
- ↑ 38.0 38.1 "Transmission of COVID-19". www.ecdc.europa.eu. 7 September 2020. Archived from the original on 14 September 2020. Retrieved 14 October 2020.
- ↑ "Outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): increased transmission beyond China – fourth update" (PDF). European Centre for Disease Prevention and Control. 14 February 2020. Archived (PDF) from the original on 30 April 2020. Retrieved 8 March 2020.
- ↑ 40.0 40.1 Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF (April 2020). "The proximal origin of SARS-CoV-2". Nature Medicine. 26 (4): 450–452. doi:10.1038/s41591-020-0820-9. PMC 7095063. PMID 32284615.
- ↑ Gibbens S (18 March 2020). "Why soap is preferable to bleach in the fight against coronavirus". National Geographic. Archived from the original on 2 April 2020. Retrieved 2 April 2020.
- ↑ Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. (February 2020). "A Novel Coronavirus from Patients with Pneumonia in China, 2019". The New England Journal of Medicine. 382 (8): 727–733. doi:10.1056/NEJMoa2001017. PMC 7092803. PMID 31978945.
- ↑ 43.0 43.1 43.2 Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) (PDF) (Report). World Health Organization (WHO). February 2020. Archived (PDF) from the original on 29 February 2020. Retrieved 21 March 2020.
- Lay summary in: Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) (Report).
- ↑ Rathore JS, Ghosh C (August 2020). "Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), a newly emerged pathogen: an overview". Pathogens and Disease. 78 (6). doi:10.1093/femspd/ftaa042. OCLC 823140442. PMC 7499575. PMID 32840560.
- ↑ Thomas S (2020). "The Structure of the Membrane Protein of SARS-CoV-2 Resembles the Sugar Transporter SemiSWEET". Pathogens & Immunity. 5 (1): 342–363. doi:10.20411/pai.v5i1.377. PMC 7608487. PMID 33154981.
- ↑ Koyama T, Platt D, Parida L (July 2020). "Variant analysis of SARS-CoV-2 genomes". Bulletin of the World Health Organization. 98 (7): 495–504. doi:10.2471/BLT.20.253591. PMC 7375210. PMID 32742035.
We detected in total 65776 variants with 5775 distinct variants.
- ↑ Alm E, Broberg EK, Connor T, Hodcroft EB, Komissarov AB, Maurer-Stroh S, et al. (August 2020). "Geographical and temporal distribution of SARS-CoV-2 clades in the WHO European Region, January to June 2020". Euro Surveillance. 25 (32). doi:10.2807/1560-7917.ES.2020.25.32.2001410. PMC 7427299. PMID 32794443.
- ↑ "Emerging SARS-CoV-2 Variants". Centers for Disease Control and Prevention. 30 December 2020. Archived from the original on 15 May 2021. Retrieved 30 December 2020.
- ↑ "Implications of Emerging SARS-CoV-2 Variant VOC 202012/01 in the UK". Centers for Disease Control and Prevention. 29 December 2020. Archived from the original on 22 January 2021. Retrieved 30 December 2020.
- ↑ "New COVID-19 Variants". Centers for Disease Control and Prevention. Archived from the original on 23 January 2021. Retrieved 24 January 2021.
- ↑ Mahase E (December 2020). "Covid-19: What have we learnt about the new variant in the UK?". BMJ. 371: m4944. doi:10.1136/bmj.m4944. PMID 33361120.
- ↑ Harrison AG, Lin T, Wang P (December 2020). "Mechanisms of SARS-CoV-2 Transmission and Pathogenesis". Trends in Immunology. 41 (12): 1100–1115. doi:10.1016/j.it.2020.10.004. PMC 7556779. PMID 33132005.
- ↑ Verdecchia P, Cavallini C, Spanevello A, Angeli F (June 2020). "The pivotal link between ACE2 deficiency and SARS-CoV-2 infection". European Journal of Internal Medicine. 76: 14–20. doi:10.1016/j.ejim.2020.04.037. PMC 7167588. PMID 32336612.
- ↑ Letko M, Marzi A, Munster V (April 2020). "Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses". Nature Microbiology. 5 (4): 562–569. doi:10.1038/s41564-020-0688-y. PMC 7095430. PMID 32094589.
- ↑ Marik PE, Iglesias J, Varon J, Kory P (1 January 2021). "A scoping review of the pathophysiology of COVID-19". International Journal of Immunopathology and Pharmacology. 35: 20587384211048026. doi:10.1177/20587384211048026. PMC 8477699. PMID 34569339.
- ↑ 56.0 56.1 Meunier N, Briand L, Jacquin-Piques A, Brondel L, Pénicaud L (June 2020). "COVID 19-Induced Smell and Taste Impairments: Putative Impact on Physiology". Frontiers in Physiology. 11: 625110. doi:10.3389/fphys.2020.625110. PMC 7870487. PMID 33574768.
- ↑ Juan IG, et al. (2021). "Central and peripheral nervous system involvement by COVID-19: a systematic review of the pathophysiology, clinical manifestations, neuropathology, neuroimaging, electrophysiology, and cerebrospinal fluid findings". BMC Infectious Diseases. 21 (1): 515. doi:10.1186/s12879-021-06185-6. PMC 8170436. PMID 34078305.
- ↑ 58.0 58.1 Pezzini A, Padovani A (November 2020). "Lifting the mask on neurological manifestations of COVID-19". Nature Reviews. Neurology. 16 (11): 636–644. doi:10.1038/s41582-020-0398-3. PMC 7444680. PMID 32839585.
- ↑ Li YC, Bai WZ, Hashikawa T (June 2020). "The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients". Journal of Medical Virology. 92 (6): 552–555. doi:10.1002/jmv.25728. PMC 7228394. PMID 32104915.
- ↑ Baig AM, Khaleeq A, Ali U, Syeda H (April 2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chemical Neuroscience. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. PMC 7094171. PMID 32167747.
- ↑ Yavarpour-Bali H, Ghasemi-Kasman M (September 2020). "Update on neurological manifestations of COVID-19". Life Sciences. 257: 118063. doi:10.1016/j.lfs.2020.118063. PMC 7346808. PMID 32652139.
- ↑ Gu J, Han B, Wang J (May 2020). "COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission". Gastroenterology. 158 (6): 1518–1519. doi:10.1053/j.gastro.2020.02.054. PMC 7130192. PMID 32142785.
- ↑ Mönkemüller K, Fry L, Rickes S (May 2020). "COVID-19, coronavirus, SARS-CoV-2 and the small bowel". Revista Espanola de Enfermedades Digestivas. 112 (5): 383–388. doi:10.17235/reed.2020.7137/2020. PMID 32343593. S2CID 216645754.
- ↑ 64.0 64.1 64.2 Zheng YY, Ma YT, Zhang JY, Xie X (May 2020). "COVID-19 and the cardiovascular system". Nature Reviews. Cardiology. 17 (5): 259–260. doi:10.1038/s41569-020-0360-5. PMC 7095524. PMID 32139904.
- ↑ 65.0 65.1 65.2 Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. (February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299. PMID 31986264.
- ↑ "Coronavirus disease 2019 (COVID-19): Myocardial infarction and other coronary artery disease issues". UpToDate. Archived from the original on 17 October 2020. Retrieved 28 September 2020.
- ↑ Turner AJ, Hiscox JA, Hooper NM (June 2004). "ACE2: from vasopeptidase to SARS virus receptor". Trends in Pharmacological Sciences. 25 (6): 291–4. doi:10.1016/j.tips.2004.04.001. PMC 7119032. PMID 15165741.
- ↑ Abou-Ismail MY, Diamond A, Kapoor S, Arafah Y, Nayak L (October 2020). "The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management". Thrombosis Research. Elsevier BV. 194: 101–115. doi:10.1016/j.thromres.2020.06.029. PMC 7305763. PMID 32788101.
- ↑ 69.0 69.1 Wadman M (April 2020). "How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes". Science. doi:10.1126/science.abc3208.
- ↑ "NIH study uncovers blood vessel damage and inflammation in COVID-19 patients' brains but no infection". National Institutes of Health (NIH). 30 December 2020. Archived from the original on 17 January 2021. Retrieved 17 January 2021.
- ↑ Celine T (8 January 2021). "COVID-19's Severe Damage to Brain Tissues Found Through Studying Autopsies". Science Times. Archived from the original on 9 January 2021. Retrieved 17 January 2021.
- ↑ Lee MH, Perl DP, Nair G, Li W, Maric D, Murray H, et al. (February 2021). "Microvascular Injury in the Brains of Patients with Covid-19". The New England Journal of Medicine. 384 (5): 481–483. doi:10.1056/nejmc2033369. PMC 7787217. PMID 33378608.
- ↑ "How a COVID-19 infection changes blood cells in the long run". phys.org. Archived from the original on 31 October 2021. Retrieved 10 July 2021.
- ↑ Kubánková M, Hohberger B, Hoffmanns J, Fürst J, Herrmann M, Guck J, Kräter M (July 2021). "Physical phenotype of blood cells is altered in COVID-19". Biophysical Journal. 120 (14): 2838–2847. Bibcode:2021BpJ...120.2838K. doi:10.1016/j.bpj.2021.05.025. PMC 8169220. PMID 34087216.
- ↑ Coronavirus: Kidney Damage Caused by COVID‑19 Coronavirus: Kidney Damage Caused by COVID-19 at the Wayback Machine (archived 2021-05-06)(Positional parameters ignored), Johns Hopkins Medicine, C. John Sperati, updated 14 May 2020.
- ↑ 76.0 76.1 76.2 76.3 76.4 76.5 76.6 76.7 Eketunde AO, Mellacheruvu SP, Oreoluwa P (July 2020). "A Review of Postmortem Findings in Patients With COVID-19". Cureus. Cureus, Inc. 12 (7): e9438. doi:10.7759/cureus.9438. PMC 7451084. PMID 32864262. S2CID 221352704.
- ↑ Zhang C, Wu Z, Li JW, Zhao H, Wang GQ (May 2020). "Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality". International Journal of Antimicrobial Agents. 55 (5): 105954. doi:10.1016/j.ijantimicag.2020.105954. PMC 7118634. PMID 32234467.
- ↑ Gómez-Rial J, Rivero-Calle I, Salas A, Martinón-Torres F (2020). "Role of Monocytes/Macrophages in Covid-19 Pathogenesis: Implications for Therapy". Infection and Drug Resistance. 13: 2485–2493. doi:10.2147/IDR.S258639. PMC 7383015. PMID 32801787.
- ↑ Chen, Shiru; Guan, Fei; Candotti, Fabio; Benlagha, Kamel; Camara, Niels Olsen Saraiva; Herrada, Andres A.; James, Louisa K.; Lei, Jiahui; Miller, Heather; Kubo, Masato; Ning, Qin; Liu, Chaohong (2022). "The role of B cells in COVID-19 infection and vaccination". Frontiers in Immunology. 13: 988536. doi:10.3389/fimmu.2022.988536. ISSN 1664-3224. Archived from the original on 19 September 2022. Retrieved 11 May 2023.
- ↑ Dai L, Gao GF (February 2021). "Viral targets for vaccines against COVID-19". Nature Reviews. Immunology. 21 (2): 73–82. doi:10.1038/s41577-020-00480-0. ISSN 1474-1733. PMC 7747004. PMID 33340022.
- ↑ 81.0 81.1 Boopathi S, Poma AB, Kolandaivel P (April 2020). "Novel 2019 coronavirus structure, mechanism of action, antiviral drug promises and rule out against its treatment". Journal of Biomolecular Structure & Dynamics. 39 (9): 3409–3418. doi:10.1080/07391102.2020.1758788. PMC 7196923. PMID 32306836.
- ↑ Kai H, Kai M (July 2020). "Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors-lessons from available evidence and insights into COVID-19". Hypertension Research. 43 (7): 648–654. doi:10.1038/s41440-020-0455-8. PMC 7184165. PMID 32341442.
- ↑ Chen HX, Chen ZH, Shen HH (October 2020). "[Structure of SARS-CoV-2 and treatment of COVID-19]". Sheng Li Xue Bao. 72 (5): 617–630. PMID 33106832.
- ↑ Jeyanathan M, Afkhami S, Smaill F, Miller MS, Lichty BD, Xing Z (4 September 2020). "Immunological considerations for COVID-19 vaccine strategies". Nature Reviews Immunology. 20 (10): 615–632. doi:10.1038/s41577-020-00434-6. ISSN 1474-1741. PMC 7472682. PMID 32887954.
- ↑ Zhang Q, Ju B, Ge J, Chan JF, Cheng L, Wang R, et al. (July 2021). "Potent and protective IGHV3-53/3-66 public antibodies and their shared escape mutant on the spike of SARS-CoV-2". Nature Communications. 12 (1): 4210. Bibcode:2021NatCo..12.4210Z. doi:10.1038/s41467-021-24514-w. PMC 8270942. PMID 34244522. S2CID 235786394.
- ↑ Soy M, Keser G, Atagündüz P, Tabak F, Atagündüz I, Kayhan S (July 2020). "Cytokine storm in COVID-19: pathogenesis and overview of anti-inflammatory agents used in treatment". Clinical Rheumatology. 39 (7): 2085–2094. doi:10.1007/s10067-020-05190-5. PMC 7260446. PMID 32474885.
- ↑ Quirch M, Lee J, Rehman S (August 2020). "Hazards of the Cytokine Storm and Cytokine-Targeted Therapy in Patients With COVID-19: Review". Journal of Medical Internet Research. 22 (8): e20193. doi:10.2196/20193. PMC 7428145. PMID 32707537.
- ↑ Bhaskar S, Sinha A, Banach M, Mittoo S, Weissert R, Kass JS, et al. (2020). "Cytokine Storm in COVID-19-Immunopathological Mechanisms, Clinical Considerations, and Therapeutic Approaches: The REPROGRAM Consortium Position Paper". Frontiers in Immunology. 11: 1648. doi:10.3389/fimmu.2020.01648. PMC 7365905. PMID 32754159.
- ↑ 89.0 89.1 89.2 89.3 89.4 89.5 Wastnedge EA, Reynolds RM, van Boeckel SR, Stock SJ, Denison FC, Maybin JA, Critchley HO (January 2021). "Pregnancy and COVID-19". Physiological Reviews. 101 (1): 303–318. doi:10.1152/physrev.00024.2020. PMC 7686875. PMID 32969772.
- ↑ One in six most critically ill NHS patients are unvaccinated pregnant women with Covid One in six most critically ill NHS Covid patients are unvaccinated pregnant women at the Wayback Machine (archived 2021-11-04)(Positional parameters ignored) The Guardian
- ↑ 91.0 91.1 91.2 91.3 Li C, Zhao C, Bao J, Tang B, Wang Y, Gu B (November 2020). "Laboratory diagnosis of coronavirus disease-2019 (COVID-19)". Clinica Chimica Acta; International Journal of Clinical Chemistry. 510: 35–46. doi:10.1016/j.cca.2020.06.045. PMC 7329657. PMID 32621814.
- ↑ 92.0 92.1 Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. (August 2020). "Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases". Radiology. 296 (2): E32–E40. doi:10.1148/radiol.2020200642. PMC 7233399. PMID 32101510.
- ↑ 93.0 93.1 93.2 93.3 Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A (July 2020). "Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients". AJR. American Journal of Roentgenology. 215 (1): 87–93. doi:10.2214/AJR.20.23034. PMID 32174129.
- ↑ "2019 Novel Coronavirus (2019-nCoV) Situation Summary". U.S. Centers for Disease Control and Prevention (CDC). 30 January 2020. Archived from the original on 26 January 2020. Retrieved 30 January 2020.
- ↑ "Coronavirus disease (COVID-19) technical guidance: Laboratory testing for 2019-nCoV in humans". World Health Organization (WHO). Archived from the original on 15 March 2020. Retrieved 14 March 2020.
- ↑ Bullard J, Dust K, Funk D, Strong JE, Alexander D, Garnett L, et al. (December 2020). "Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic Samples". Clinical Infectious Diseases. 71 (10): 2663–2666. doi:10.1093/cid/ciaa638. PMC 7314198. PMID 32442256.
- ↑ "Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Persons for Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 4 March 2020. Retrieved 26 March 2020.
- ↑ "Real-Time RT-PCR Panel for Detection 2019-nCoV". U.S. Centers for Disease Control and Prevention (CDC). 29 January 2020. Archived from the original on 30 January 2020. Retrieved 1 February 2020.
- ↑ "Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases". World Health Organization (WHO). Archived from the original on 17 March 2020. Retrieved 13 March 2020.
- ↑ "NHS staff will be first to get new coronavirus antibody test, medical chief promises". The Independent. 14 May 2020. Archived from the original on 18 May 2020. Retrieved 14 May 2020.
- ↑ Heneghan C, Jefferson T (1 September 2020). "Virological characterization of COVID-19 patients that test re-positive for SARS-CoV-2 by RT-PCR". CEBM. Archived from the original on 18 June 2021. Retrieved 19 September 2020.
- ↑ Lu J, Peng J, Xiong Q, Liu Z, Lin H, Tan X, et al. (September 2020). "Clinical, immunological and virological characterization of COVID-19 patients that test re-positive for SARS-CoV-2 by RT-PCR". EBioMedicine. 59: 102960. doi:10.1016/j.ebiom.2020.102960. PMC 7444471. PMID 32853988.
- ↑ Spencer E, Jefferson T, Brassey J, Heneghan C (11 September 2020). "When is Covid, Covid?". The Centre for Evidence-Based Medicine. Archived from the original on 18 June 2021. Retrieved 19 September 2020.
- ↑ "SARS-CoV-2 RNA testing: assurance of positive results during periods of low prevalence". GOV.UK. Archived from the original on 6 May 2021. Retrieved 19 September 2020.
- ↑ "ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection". American College of Radiology. 22 March 2020. Archived from the original on 28 March 2020.
- ↑ Pormohammad A, Ghorbani S, Khatami A, Razizadeh MH, Alborzi E, Zarei M, et al. (October 2020). "Comparison of influenza type A and B with COVID-19: A global systematic review and meta-analysis on clinical, laboratory and radiographic findings". Reviews in Medical Virology: e2179. doi:10.1002/rmv.2179. PMC 7646051. PMID 33035373. S2CID 222255245.
- ↑ Lee EY, Ng MY, Khong PL (April 2020). "COVID-19 pneumonia: what has CT taught us?". The Lancet. Infectious Diseases. 20 (4): 384–385. doi:10.1016/S1473-3099(20)30134-1. PMC 7128449. PMID 32105641.
- ↑ 108.0 108.1 Li Y, Xia L (June 2020). "Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management". AJR. American Journal of Roentgenology. 214 (6): 1280–1286. doi:10.2214/AJR.20.22954. PMID 32130038. S2CID 212416282.
- ↑ "COVID-19 Database". Società Italiana di Radiologia Medica e Interventistica (in italiano). Archived from the original on 7 December 2020. Retrieved 11 March 2020.
- ↑ Giani M, Seminati D, Lucchini A, Foti G, Pagni F (May 2020). "Exuberant Plasmocytosis in Bronchoalveolar Lavage Specimen of the First Patient Requiring Extracorporeal Membrane Oxygenation for SARS-CoV-2 in Europe". Journal of Thoracic Oncology. 15 (5): e65–e66. doi:10.1016/j.jtho.2020.03.008. PMC 7118681. PMID 32194247.
- ↑ Lillicrap D (April 2020). "Disseminated intravascular coagulation in patients with 2019-nCoV pneumonia". Journal of Thrombosis and Haemostasis. 18 (4): 786–787. doi:10.1111/jth.14781. PMC 7166410. PMID 32212240.
- ↑ Mitra A, Dwyre DM, Schivo M, Thompson GR, Cohen SH, Ku N, Graff JP (August 2020). "Leukoerythroblastic reaction in a patient with COVID-19 infection". American Journal of Hematology. 95 (8): 999–1000. doi:10.1002/ajh.25793. PMC 7228283. PMID 32212392.
- ↑ 113.0 113.1 113.2 113.3 113.4 113.5 Satturwar, Swati; Fowkes, Mary; Farver, Carol; Wilson, Allecia M.; Eccher, Albino; Girolami, Ilaria; Pujadas, Elisabet; Bryce, Clare; Salem, Fadi; El Jamal, Siraj M.; Paniz-Mondolfi, Alberto; Petersen, Bruce; Gordon, Ronald E.; Reidy, Jason; Fraggetta, Filippo; Marshall, Desiree A.; Pantanowitz, Liron (2021). "Postmortem Findings Associated With SARS-CoV-2". American Journal of Surgical Pathology. Publish Ahead of Print (5): 587–603. doi:10.1097/PAS.0000000000001650. ISSN 0147-5185. PMID 33481385. S2CID 231679276.
- ↑ Maier BF, Brockmann D (May 2020). "Effective containment explains subexponential growth in recent confirmed COVID-19 cases in China". Science. 368 (6492): 742–746. arXiv:2002.07572. Bibcode:2020Sci...368..742M. doi:10.1126/science.abb4557. PMC 7164388. PMID 32269067. ("... initial exponential growth expected for an unconstrained outbreak.")
- ↑ "Viral Load Exposure Factors". ReallyCorrect.com. Archived from the original on 2021-05-06. Retrieved 2021-05-08.
- ↑ "Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission". U.S. Centers for Disease Control and Prevention (CDC). 28 June 2020. Archived from the original on 19 May 2020. Retrieved 8 May 2021.
- ↑ "Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission". COVID-19 Published Science and Research. U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 5 October 2020. Retrieved 30 October 2020.
- ↑ Centers for Disease Control and Prevention (5 April 2020). "What to Do if You Are Sick". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 14 February 2020. Retrieved 24 April 2020.
- ↑ "Coronavirus Disease 2019 (COVID-19) – Prevention & Treatment". U.S. Centers for Disease Control and Prevention (CDC). 10 March 2020. Archived from the original on 11 March 2020. Retrieved 11 March 2020.
- ↑ "UK medicines regulator gives approval for first UK COVID-19 vaccine". Medicines and Healthcare Products Regulatory Agency, Government of the UK. 2 December 2020. Archived from the original on 17 March 2021. Retrieved 2 December 2020.
- ↑ Mueller B (2 December 2020). "U.K. Approves Pfizer Coronavirus Vaccine, a First in the West". The New York Times. Archived from the original on 28 January 2021. Retrieved 2 December 2020.
- ↑ "COVID-19 Treatment Guidelines". nih.gov. National Institutes of Health. Archived from the original on 11 October 2020. Retrieved 21 April 2020.
- ↑ 123.0 123.1 123.2 Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB (May 2020). "Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review". JAMA. 323 (18): 1824–1836. doi:10.1001/jama.2020.6019. PMID 32282022.
- ↑ 124.0 124.1 Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (March 2020). "How will country-based mitigation measures influence the course of the COVID-19 epidemic?". Lancet. 395 (10228): 931–934. doi:10.1016/S0140-6736(20)30567-5. PMC 7158572. PMID 32164834.
A key issue for epidemiologists is helping policy makers decide the main objectives of mitigation – e.g. minimising morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the effects on the economy within manageable levels, and flattening the epidemic curve to wait for vaccine development and manufacture on scale and antiviral drug therapies.
- ↑ Wiles S (14 March 2020). "After 'Flatten the Curve', we must now 'Stop the Spread'. Here's what that means". The Spinoff. Archived from the original on 26 March 2020. Retrieved 13 March 2020.
- ↑ Li YD, Chi WY, Su JH, Ferrall L, Hung CF, Wu TC (December 2020). "Coronavirus vaccine development: from SARS and MERS to COVID-19". Journal of Biomedical Science. 27 (1): 104. doi:10.1186/s12929-020-00695-2. PMC 7749790. PMID 33341119.
- ↑ Subbarao K (July 2021). "The success of SARS-CoV-2 vaccines and challenges ahead". Cell Host & Microbe. 29 (7): 1111–1123. doi:10.1016/j.chom.2021.06.016. PMC 8279572. PMID 34265245.
- ↑ Padilla TB (24 February 2021). "No one is safe unless everyone is safe". BusinessWorld. Archived from the original on 23 February 2021. Retrieved 24 February 2021.
- ↑ Vergano D (5 June 2021). "COVID-19 Vaccines Work Way Better Than We Had Ever Expected. Scientists Are Still Figuring Out Why". BuzzFeed News. Archived from the original on 6 October 2021. Retrieved 24 June 2021.
- ↑ Mallapaty S, Callaway E, Kozlov M, Ledford H, Pickrell J, Van Noorden R (16 December 2021). "How COVID vaccines shaped 2021 in eight powerful charts". Nature. 600 (7890): 580–583. Bibcode:2021Natur.600..580M. doi:10.1038/d41586-021-03686-x. PMID 34916666. S2CID 245262732.
- ↑ Beaumont P (18 November 2020). "Covid-19 vaccine: who are countries prioritising for first doses?". The Guardian. ISSN 0261-3077. Archived from the original on 18 January 2021. Retrieved 26 December 2020.
- ↑ Richie H, Ortiz-Ospina E, Beltekian D, Methieu E, Hasell J, Macdonald B, et al. (5 March 2020). "Coronavirus (COVID-19) Vaccinations – Statistics and Research". Our World in Data. Archived from the original on 10 March 2021. Retrieved 7 February 2021.
- ↑ Mullard A (November 2020). "How COVID vaccines are being divvied up around the world". Nature. doi:10.1038/d41586-020-03370-6. PMID 33257891. S2CID 227246811.
- ↑ So AD, Woo J (December 2020). "Reserving coronavirus disease 2019 vaccines for global access: cross sectional analysis". BMJ. 371: m4750. doi:10.1136/bmj.m4750. PMC 7735431. PMID 33323376.
- ↑ "Wear masks in public says WHO, in update of COVID-19 advice". Reuters. 5 June 2020. Archived from the original on 23 July 2020. Retrieved 3 July 2020.
- ↑ 136.0 136.1 136.2 "Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 19 May 2020. Retrieved 17 April 2020.
- ↑ 137.0 137.1 "Using face masks in the community – Technical Report" (PDF). ECDC. 8 April 2020. Archived (PDF) from the original on 8 April 2020. Retrieved 8 May 2021.
- ↑ "Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2". U.S. Centers for Disease Control and Prevention (CDC). 10 November 2020. Archived from the original on 10 November 2020. Retrieved 8 May 2021.
- ↑ Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L (April 2020). "Face masks for the public during the covid-19 crisis". BMJ. 369: m1435. doi:10.1136/bmj.m1435. PMID 32273267. S2CID 215516381.
- ↑ "Caring for Someone Sick at Home". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 19 March 2020. Retrieved 3 July 2020.
- ↑ "Using Personal Protective Equipment (PPE)". U.S. Centers for Disease Control and Prevention (CDC). 11 June 2020. Archived from the original on 4 April 2020. Retrieved 4 July 2020.
- ↑ 142.0 142.1 142.2 CDC (11 February 2020). "Scientific Brief: SARS-CoV-2 Transmission". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 15 November 2021. Retrieved 10 May 2021.
- ↑ "Transmission of COVID-19". www.ecdc.europa.eu. 7 September 2020. Archived from the original on 14 September 2020. Retrieved 14 October 2020.
- ↑ 144.0 144.1 National Center for Immunization and Respiratory Diseases (NCIRD) (9 July 2020). "COVID-19 Employer Information for Office Buildings". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 17 July 2020. Retrieved 9 July 2020.
- ↑ World Health Organization (29 October 2020). WHO's Science in 5 on COVID-19 – Ventilation. Archived from the original on 24 September 2021. Retrieved 2 November 2020 – via YouTube.
- ↑ Somsen GA, van Rijn C, Kooij S, Bem RA, Bonn D (July 2020). "Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission". The Lancet. Respiratory Medicine. Elsesier. 8 (7): 658–659. doi:10.1016/S2213-2600(20)30245-9. PMC 7255254. PMID 32473123.
- ↑ Lipinski T, Ahmad D, Serey N, Jouhara H (1 November 2020). "Review of ventilation strategies to reduce the risk of disease transmission in high occupancy buildings". International Journal of Thermofluids. 7–8: 100045. doi:10.1016/j.ijft.2020.100045. ISSN 2666-2027. S2CID 221642242. Archived from the original on 13 February 2021. Retrieved 15 March 2022.
- ↑ "Social distancing: what you need to do – Coronavirus (COVID-19)". nhs.uk. 2 June 2020. Archived from the original on 2 June 2020. Retrieved 18 August 2020.
- ↑ "Advice for the public on COVID-19 – World Health Organization". World Health Organization (WHO). Archived from the original on 26 January 2020. Retrieved 18 August 2020.
- ↑ "COVID-19 and Your Health". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 23 March 2021. Retrieved 23 March 2021.
To prevent the spread of germs, including COVID-19, CDC recommends washing hands with soap and water whenever possible because it reduces the amount of many types of germs and chemicals on hands. But if soap and water are not readily available, using a hand sanitizer with at least 60% alcohol can help you avoid getting sick and spreading germs to others.
- ↑ "WHO-recommended handrub formulations". WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care. World Health Organization (WHO). 19 March 2009. Archived from the original on 21 March 2020. Retrieved 19 March 2020.
- ↑ Nussbaumer-Streit B, Mayr V, Dobrescu AI, Chapman A, Persad E, Klerings I, et al. (April 2020). "Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review". The Cochrane Database of Systematic Reviews. 4: CD013574. doi:10.1002/14651858.CD013574. PMC 7141753. PMID 32267544.
- ↑ Qian M, Jiang J (May 2020). "COVID-19 and social distancing". Zeitschrift für Gesundheitswissenschaften = Journal of Public Health. 30: 259–261. doi:10.1007/s10389-020-01321-z. PMC 7247774. PMID 32837835.
- ↑ 154.0 154.1 Hawks L, Woolhandler S, McCormick D (August 2020). "COVID-19 in Prisons and Jails in the United States". JAMA Internal Medicine. 180 (8): 1041–1042. doi:10.1001/jamainternmed.2020.1856. PMID 32343355.
- ↑ Waldstein D (6 May 2020). "To Fight Virus in Prisons, C.D.C. Suggests More Screenings". The New York Times. Archived from the original on 8 May 2020. Retrieved 14 May 2020.
- ↑ "How COVID-19 Spreads". U.S. Centers for Disease Control and Prevention (CDC). 18 September 2020. Archived from the original on 19 September 2020. Retrieved 20 September 2020.
- ↑ Goldman E (August 2020). "Exaggerated risk of transmission of COVID-19 by fomites". The Lancet. Infectious Diseases. 20 (8): 892–893. doi:10.1016/S1473-3099(20)30561-2. PMC 7333993. PMID 32628907.
- ↑ Weixel N (5 April 2021). "CDC says risk of COVID-19 transmission on surfaces 1 in 10,000". TheHill. Archived from the original on 8 December 2021. Retrieved 19 December 2021.
- ↑ 159.0 159.1 "Science Brief: SARS-CoV-2 and Surface (Fomite) Transmission for Indoor Community Environments". U.S. Centers for Disease Control and Prevention (CDC). 5 April 2021. Archived from the original on 5 April 2021. Retrieved 8 May 2021.
- ↑ 160.0 160.1 Pedreira A, Taşkın Y, García MR (January 2021). "A Critical Review of Disinfection Processes to Control SARS-CoV-2 Transmission in the Food Industry". Foods. 10 (2): 283. doi:10.3390/foods10020283. PMC 7911259. PMID 33572531. S2CID 231900820.
- ↑ Rezasoltani S, Yadegar A, Hatami B, Asadzadeh Aghdaei H, Zali MR (2020). "Antimicrobial Resistance as a Hidden Menace Lurking Behind the COVID-19 Outbreak: The Global Impacts of Too Much Hygiene on AMR". Frontiers in Microbiology. 11: 590683. doi:10.3389/fmicb.2020.590683. PMC 7769770. PMID 33384670.
- ↑ Thompson D (8 February 2021). "Hygiene Theater Is Still a Huge Waste of Time". The Atlantic. Archived from the original on 26 February 2021. Retrieved 27 February 2021.
- ↑ Thompson D (27 July 2020). "Hygiene Theater Is a Huge Waste of Time". The Atlantic. Archived from the original on 26 April 2021. Retrieved 27 February 2021.
- ↑ 164.0 164.1 164.2 164.3 164.4 164.5 164.6 Bueckert M, Gupta R, Gupta A, Garg M, Mazumder A (November 2020). "Infectivity of SARS-CoV-2 and Other Coronaviruses on Dry Surfaces: Potential for Indirect Transmission". Materials. 13 (22): 5211. Bibcode:2020Mate...13.5211B. doi:10.3390/ma13225211. PMC 7698891. PMID 33218120.
- ↑ Bhardwaj R, Agrawal A (November 2020). "How coronavirus survives for days on surfaces". Physics of Fluids. 32 (11): 111706. Bibcode:2020PhFl...32k1706B. doi:10.1063/5.0033306. PMC 7713872. PMID 33281435.
- ↑ Chatterjee S, Murallidharan JS, Agrawal A, Bhardwaj R (February 2021). "Why coronavirus survives longer on impermeable than porous surfaces". Physics of Fluids. 33 (2): 021701. Bibcode:2021PhFl...33b1701C. doi:10.1063/5.0037924. PMC 7978145. PMID 33746485.
- ↑ CDC (11 February 2020). "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 5 April 2021. Retrieved 12 April 2021.
- ↑ Anthes E (8 April 2021). "Has the Era of Overzealous Cleaning Finally Come to an End?". The New York Times. Archived from the original on 12 April 2021. Retrieved 12 April 2021.
- ↑ "Interim Recommendations for US Community Facilities with Suspected/Confirmed Coronavirus Disease 2019". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 20 May 2020. Retrieved 4 April 2020.
- ↑ Patiño-Lugo DF, Vélez M, Velásquez Salazar P, Vera-Giraldo CY, Vélez V, Marín IC, et al. (June 2020). "Non-pharmaceutical interventions for containment, mitigation and suppression of COVID-19 infection". Colombia Medica. 51 (2): e4266. doi:10.25100/cm.v51i2.4266. PMC 7518730. PMID 33012884.
- ↑ "COVID-19 Informational Resources for High-Risk Groups | Keeping Education ACTIVE | Partnership to Fight Chronic Disease". fightchronicdisease.org. Archived from the original on 10 June 2020. Retrieved 31 May 2020.
- ↑ "Quarantine and Isolation". U.S. Centers for Disease Control and Prevention (CDC). 29 July 2021. Archived from the original on 16 November 2020. Retrieved 12 August 2021.
- ↑ "Food safety, nutrition, and wellness during COVID-19". The Nutrition Source. Harvard T.H. Chan School of Public Health. 29 May 2020. Archived from the original on 14 November 2020. Retrieved 8 November 2020.
- ↑ Reynolds G (14 April 2021). "Regular Exercise May Help Protect Against Severe COVID". The New York Times. Archived from the original on 26 October 2021. Retrieved 10 May 2021.
- ↑ Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, Li Q, et al. (April 2021). "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients". British Journal of Sports Medicine. 55 (19): 1099–1105. doi:10.1136/bjsports-2021-104080. PMC 8050880. PMID 33849909.
- ↑ Szarpak L, Filipiak KJ, Gasecka A, Gawel W, Koziel D, Jaguszewski MJ, et al. (October 2021). "Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis". Cardiology Journal. doi:10.5603/CJ.a2021.0122. PMID 34642923. S2CID 238746984.
- ↑ "Trial to test if Vitamin D protects against Covid". BBC News. 13 October 2020. Archived from the original on 26 October 2021. Retrieved 10 November 2020.
- ↑ 178.0 178.1 "Trial of Vitamin D to Reduce Risk and Severity of COVID-19 and Other Acute Respiratory Infections - Full Text View - ClinicalTrials.gov". clinicaltrials.gov. Archived from the original on 19 November 2021. Retrieved 10 November 2020.
- ↑ 179.0 179.1 179.2 Burns J, Movsisyan A, Stratil JM, Biallas RL, Coenen M, Emmert-Fees KM, et al. (Cochrane Public Health Group) (March 2021). "International travel-related control measures to contain the COVID-19 pandemic: a rapid review". The Cochrane Database of Systematic Reviews. 2021 (3): CD013717. doi:10.1002/14651858.CD013717.pub2. PMC 8406796. PMID 33763851. S2CID 232356197.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ↑ 180.0 180.1 180.2 180.3 Siemieniuk RA, Bartoszko JJ, Ge L, Zeraatkar D, Izcovich A, Kum E, et al. (July 2020). "Drug treatments for covid-19: living systematic review and network meta-analysis". BMJ. 370: m2980. doi:10.1136/bmj.m2980. PMC 7390912. PMID 32732190.
- ↑ 181.0 181.1 "Coronavirus". WebMD. Archived from the original on 2020-02-01. Retrieved 2020-02-01.
- ↑ Fisher D, Heymann D (February 2020). "Q&A: The novel coronavirus outbreak causing COVID-19". BMC Medicine. 18 (1): 57. doi:10.1186/s12916-020-01533-w. PMC 7047369. PMID 32106852.
- ↑ Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, et al. (May 2020). "Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province". Chinese Medical Journal. 133 (9): 1025–1031. doi:10.1097/CM9.0000000000000744. PMC 7147277. PMID 32044814.
- ↑ Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, Jiang B (March 2020). "Comorbidities and multi-organ injuries in the treatment of COVID-19". Lancet. Elsevier BV. 395 (10228): e52. doi:10.1016/s0140-6736(20)30558-4. PMC 7270177. PMID 32171074.
- ↑ Wang Y, Wang Y, Chen Y, Qin Q (March 2020). "Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures". Journal of Medical Virology. 92 (6): 568–576. doi:10.1002/jmv.25748. PMC 7228347. PMID 32134116.
- ↑ Martel J, Ko YF, Young JD, Ojcius DM (May 2020). "Could nasal breathing help to mitigate the severity of COVID-19". Microbes and Infection. 22 (4–5): 168–171. doi:10.1016/j.micinf.2020.05.002. PMC 7200356. PMID 32387333.
- ↑ "Coronavirus recovery: breathing exercises". www.hopkinsmedicine.org. Johns Hopkins Medicine. Archived from the original on 11 October 2020. Retrieved 30 July 2020.
- ↑ Wang L, Wang Y, Ye D, Liu Q (March 2020). "Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence". International Journal of Antimicrobial Agents. 55 (6): 105948. doi:10.1016/j.ijantimicag.2020.105948. PMC 7156162. PMID 32201353. Archived from the original on 27 March 2020. Retrieved 27 March 2020.
- ↑ U.S. Centers for Disease Control and Prevention (5 April 2020). "What to Do if You Are Sick". Centers for Disease Control and Prevention (CDC). Archived from the original on 14 February 2020. Retrieved 24 April 2020.
- ↑ "Update to living WHO guideline on drugs for covid-19". BMJ (Clinical Research Ed.). 371: m4475. November 2020. doi:10.1136/bmj.m4475. ISSN 1756-1833. PMID 33214213. S2CID 227059995.
- ↑ "Q&A: Dexamethasone and COVID-19". World Health Organization (WHO). Archived from the original on 2020-10-11. Retrieved 2020-07-11.
- ↑ "Home". National COVID-19 Clinical Evidence Taskforce. Archived from the original on 2020-10-11. Retrieved 2020-07-11.
- ↑ "COVID-19 Treatment Guidelines". www.nih.gov. National Institutes of Health. Archived from the original on 2021-01-19. Retrieved 2021-01-18.
- ↑ Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. (April 2020). "Clinical Characteristics of Coronavirus Disease 2019 in China". The New England Journal of Medicine. Massachusetts Medical Society. 382 (18): 1708–1720. doi:10.1056/nejmoa2002032. PMC 7092819. PMID 32109013.
- ↑ Henry BM (April 2020). "COVID-19, ECMO, and lymphopenia: a word of caution". The Lancet. Respiratory Medicine. Elsevier BV. 8 (4): e24. doi:10.1016/s2213-2600(20)30119-3. PMC 7118650. PMID 32178774.
- ↑ 196.0 196.1 Kim PS, Read SW, Fauci AS (December 2020). "Therapy for Early COVID-19: A Critical Need". JAMA. American Medical Association (AMA). 324 (21): 2149–2150. doi:10.1001/jama.2020.22813. PMID 33175121.
- ↑ 197.0 197.1 197.2 "COVID-19 Treatment Guidelines". www.nih.gov. National Institutes of Health. Archived from the original on 2021-01-19. Retrieved 2021-01-18./
- ↑ Hsu, Jeremy (2020-11-19). "Covid-19: What now for remdesivir?". BMJ. 371: m4457. doi:10.1136/bmj.m4457. ISSN 1756-1833. PMID 33214186.
- ↑ Roser M, Ritchie H, Ortiz-Ospina E (4 March 2020). "Coronavirus Disease (COVID-19)". Our World in Data. Archived from the original on 19 March 2020. Retrieved 12 March 2020.
- ↑ Doshi P (October 2020). "Will covid-19 vaccines save lives? Current trials aren't designed to tell us". BMJ. 371: m4037. doi:10.1136/bmj.m4037. PMID 33087398. S2CID 224817161.
- ↑ 201.0 201.1 Palmieri L, Andrianou X, Barbariol P, Bella A, Bellino S, Benelli E, et al. (22 July 2020). Characteristics of SARS-CoV-2 patients dying in Italy Report based on available data on July 22nd, 2020 (PDF) (Report). Istituto Superiore di Sanità. Archived (PDF) from the original on 23 September 2020. Retrieved 4 October 2020.
- ↑ Baranovskii DS, Klabukov ID, Krasilnikova OA, Nikogosov DA, Polekhina NV, Baranovskaia DR, et al. (December 1975). "Letter: Acid secretion by gastric mucous membrane". The American Journal of Physiology. 229 (6): 21–25. doi:10.1080/03007995.2020.1853510. PMC 7738209. PMID 33210948. S2CID 227065216.
- ↑ Christensen B, Favaloro EJ, Lippi G, Van Cott EM (October 2020). "Hematology Laboratory Abnormalities in Patients with Coronavirus Disease 2019 (COVID-19)". Seminars in Thrombosis and Hemostasis. 46 (7): 845–849. doi:10.1055/s-0040-1715458. PMC 7645834. PMID 32877961.
- ↑ "Living with Covid19". NIHR Themed Reviews. National Institute for Health Research. 15 October 2020. doi:10.3310/themedreview_41169. Archived (PDF) from the original on 18 October 2020. Retrieved 8 May 2021.
- ↑ "How long does COVID-19 last?". UK COVID Symptom Study. 6 June 2020. Archived from the original on 10 October 2020. Retrieved 15 October 2020.
- ↑ "Summary of COVID-19 Long Term Health Effects: Emerging evidence and Ongoing Investigation" (PDF). University of Washington. 1 September 2020. Archived from the original (PDF) on 18 December 2020. Retrieved 15 October 2020.
- ↑ "Long-term symptoms of COVID-19 'really concerning', says WHO chief". UN News. 30 October 2020. Archived from the original on 18 January 2021. Retrieved 7 March 2021.
- ↑ "Coronavirus disease 2019 (COVID-19) – Prognosis | BMJ Best Practice US". BMJ. Archived from the original on 22 October 2020. Retrieved 15 November 2020.
- ↑ Lavery AM, Preston LE, Ko JY, Chevinsky JR, DeSisto CL, Pennington AF, et al. (November 2020). "Characteristics of Hospitalized COVID-19 Patients Discharged and Experiencing Same-Hospital Readmission – United States, March-August 2020". MMWR. Morbidity and Mortality Weekly Report. 69 (45): 1695–1699. doi:10.15585/mmwr.mm6945e2. PMC 7660660. PMID 33180754.
- ↑ Vardavas CI, Nikitara K (March 2020). "COVID-19 and smoking: A systematic review of the evidence". Tobacco Induced Diseases. 18: 20. doi:10.18332/tid/119324. PMC 7083240. PMID 32206052.
- ↑ 211.0 211.1 211.2 Engin AB, Engin ED, Engin A (August 2020). "Two important controversial risk factors in SARS-CoV-2 infection: Obesity and smoking". Environmental Toxicology and Pharmacology. 78: 103411. doi:10.1016/j.etap.2020.103411. PMC 7227557. PMID 32422280.
- ↑ "COVID-19: Who's at higher risk of serious symptoms?". Mayo Clinic. Archived from the original on 2021-05-13. Retrieved 2021-05-08.
- ↑ Tamara A, Tahapary DL (July 2020). "Obesity as a predictor for a poor prognosis of COVID-19: A systematic review". Diabetes & Metabolic Syndrome. 14 (4): 655–659. doi:10.1016/j.dsx.2020.05.020. PMC 7217103. PMID 32438328.
- ↑ Petrakis D, Margină D, Tsarouhas K, Tekos F, Stan M, Nikitovic D, et al. (July 2020). "Obesity – A risk factor for increased COVID-19 prevalence, severity and lethality (Review)". Molecular Medicine Reports. 22 (1): 9–19. doi:10.3892/mmr.2020.11127. PMC 7248467. PMID 32377709.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 6 May 2021. Retrieved 8 May 2021.
- ↑ Devresse A, Belkhir L, Vo B, Ghaye B, Scohy A, Kabamba B, et al. (November 2020). "COVID-19 Infection in Kidney Transplant Recipients: A Single-Center Case Series of 22 Cases From Belgium". Kidney Medicine. 2 (4): 459–466. doi:10.1016/j.xkme.2020.06.001. PMC 7295531. PMID 32775986.
- ↑ Shelton JF, Shastri AJ, Ye C, Weldon CH, Filshtein-Sonmez T, Coker D; et al. (2021). "Trans-ancestry analysis reveals genetic and nongenetic associations with COVID-19 susceptibility and severity". Nat Genet. doi:10.1038/s41588-021-00854-7. PMID 33888907. Archived from the original on 2021-08-28. Retrieved 2022-03-15.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Wallis C. "One in Seven Dire COVID Cases May Result from a Faulty Immune Response". Scientific American. Archived from the original on 2021-08-28. Retrieved 2021-05-08.
- ↑ Bastard P, Rosen LB, Zhang Q, Michailidis E, Hoffmann HH, Zhang Y, et al. (October 2020). "Autoantibodies against type I IFNs in patients with life-threatening COVID-19". Science. 370 (6515): eabd4585. doi:10.1126/science.abd4585. PMC 7857397. PMID 32972996. S2CID 221914095.
- ↑ Fusco DN, Brisac C, John SP, Huang YW, Chin CR, Xie T, et al. (June 2013). "A genetic screen identifies interferon-α effector genes required to suppress hepatitis C virus replication". Gastroenterology. 144 (7): 1438–49, 1449.e1-9. doi:10.1053/j.gastro.2013.02.026. PMC 3665646. PMID 23462180.
- ↑ "COVID-19 in children and the role of school settings in transmission – first update". European Centre for Disease Prevention and Control. 23 December 2020. Archived from the original on 1 April 2021. Retrieved 6 April 2021.
- ↑ "Estimated Disease Burden of COVID-19". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 5 April 2021. Retrieved 6 April 2021.
- ↑ "Information for Pediatric Healthcare Providers". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 6 April 2021. Retrieved 6 April 2021.
- ↑ Götzinger, Florian; Santiago-García, Begoña; Noguera-Julián, Antoni (1 September 2020). "COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study". The Lancet Child & Adolescent Health. 4 (9): 653–661. doi:10.1016/S2352-4642(20)30177-2. ISSN 2352-4642. PMC 7316447. PMID 32593339. Archived from the original on 9 April 2021. Retrieved 6 April 2021.
- ↑ Fang L, Karakiulakis G, Roth M (April 2020). "Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?". The Lancet. Respiratory Medicine. 8 (4): e21. doi:10.1016/S0140-6736(20)30311-1. PMC 7118626. PMID 32171062.
- ↑ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 2 March 2020. Retrieved 2 March 2020.
- ↑ Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, et al. (February 2020). "The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – The latest 2019 novel coronavirus outbreak in Wuhan, China". International Journal of Infectious Diseases. 91: 264–266. doi:10.1016/j.ijid.2020.01.009. PMC 7128332. PMID 31953166.
- ↑ Murthy S, Gomersall CD, Fowler RA (April 2020). "Care for Critically Ill Patients With COVID-19". JAMA. 323 (15): 1499–1500. doi:10.1001/jama.2020.3633. PMID 32159735.
- ↑ Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R (2020). "Features, Evaluation and Treatment Coronavirus (COVID-19)". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32150360. Archived from the original on 6 April 2020. Retrieved 18 March 2020.
- ↑ Heymann DL, Shindo N, et al. (WHO Scientific and Technical Advisory Group for Infectious Hazards) (February 2020). "COVID-19: what is next for public health?". Lancet. 395 (10224): 542–545. doi:10.1016/s0140-6736(20)30374-3. PMC 7138015. PMID 32061313.
- ↑ Long B, Brady WJ, Koyfman A, Gottlieb M (July 2020). "Cardiovascular complications in COVID-19". The American Journal of Emergency Medicine. 38 (7): 1504–1507. doi:10.1016/j.ajem.2020.04.048. PMC 7165109. PMID 32317203.
- ↑ Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. (November 2020). "Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. 5 (11): 1265–1273. doi:10.1001/jamacardio.2020.3557. PMC 7385689. PMID 32730619.
- Lay summary in: "Covid-19 infections leave an impact on the heart, raising concerns about lasting damage".
{{cite journal}}: Cite journal requires|journal=(help)
- Lay summary in: "Covid-19 infections leave an impact on the heart, raising concerns about lasting damage".
- ↑ Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, et al. (November 2020). "Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases". JAMA Cardiology. 5 (11): 1281–1285. doi:10.1001/jamacardio.2020.3551. PMC 7385672. PMID 32730555.
{{cite journal}}: CS1 maint: PMC embargo expired (link)- Lay summary in: "Covid-19 infections leave an impact on the heart, raising concerns about lasting damage".
{{cite journal}}: Cite journal requires|journal=(help)
- Lay summary in: "Covid-19 infections leave an impact on the heart, raising concerns about lasting damage".
- ↑ Siripanthong B, Nazarian S, Muser D, Deo R, Santangeli P, Khanji MY, et al. (September 2020). "Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management". Heart Rhythm. 17 (9): 1463–1471. doi:10.1016/j.hrthm.2020.05.001. PMC 7199677. PMID 32387246.
- ↑ Xu L, Liu J, Lu M, Yang D, Zheng X (May 2020). "Liver injury during highly pathogenic human coronavirus infections". Liver International. 40 (5): 998–1004. doi:10.1111/liv.14435. PMC 7228361. PMID 32170806.
- ↑ Carod-Artal FJ (May 2020). "Neurological complications of coronavirus and COVID-19". Revista de Neurologia. 70 (9): 311–322. doi:10.33588/rn.7009.2020179. PMID 32329044.
- ↑ Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, Cuzzoni MG, et al. (June 2020). "Guillain-Barré Syndrome Associated with SARS-CoV-2". The New England Journal of Medicine. 382 (26): 2574–2576. doi:10.1056/NEJMc2009191. PMC 7182017. PMID 32302082.
- ↑ "Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19". World Health Organization (WHO). 15 May 2020. Archived from the original on 15 May 2020. Retrieved 20 May 2020.
- ↑ HAN Archive – 00432. U.S. Centers for Disease Control and Prevention (CDC) (Report). 15 May 2020. Archived from the original on 15 May 2020. Retrieved 20 May 2020.
- ↑ Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B (August 2020). "COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: Imaging Features". Radiology. 296 (2): E119–E120. doi:10.1148/radiol.2020201187. PMC 7233386. PMID 32228363.
- ↑ 241.0 241.1 Córdoba-Vives S, Peñaranda G (April 2020). "COVID-19 y Embarazo". Medical Journal of Costa Rica: 629. Archived from the original on 2021-05-06. Retrieved 2021-05-08.
- ↑ "Living with Covid19". NIH Themed Review. National Institute for Health Research. 15 October 2020. doi:10.3310/themedreview_41169. Archived (PDF) from the original on 18 October 2020. Retrieved 8 May 2021.
- ↑ "How long does COVID-19 last?". UK COVID Symptom Study. 6 June 2020. Archived from the original on 10 October 2020. Retrieved 15 October 2020.
- ↑ "Summary of COVID-19 Long Term Health Effects: Emerging evidence and Ongoing Investigation" (PDF). University of Washington. 1 September 2020. Archived (PDF) from the original on 8 November 2020. Retrieved 15 October 2020.
- ↑ Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. (February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299. PMID 31986264.
- ↑ 246.0 246.1 Torres-Castro R, Vasconcello-Castillo L, Alsina-Restoy X, Solis-Navarro L, Burgos F, Puppo H, Vilaró J (November 2020). "Respiratory function in patients post-infection by COVID-19: a systematic review and meta-analysis". Pulmonology. Elsevier BV. doi:10.1016/j.pulmoe.2020.10.013. PMC 7687368. PMID 33262076. S2CID 227162748.
- ↑ Shaw B, Daskareh M, Gholamrezanezhad A (January 2021). "The lingering manifestations of COVID-19 during and after convalescence: update on long-term pulmonary consequences of coronavirus disease 2019 (COVID-19)". La Radiologia Medica. 126 (1): 40–46. doi:10.1007/s11547-020-01295-8. PMC 7529085. PMID 33006087.
- ↑ Zhao YM, Shang YM, Song WB, Li QQ, Xie H, Xu QF, et al. (August 2020). "Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery". EClinicalMedicine. 25: 100463. doi:10.1016/j.ijtb.2020.11.003. PMC 7654356. PMID 32838236.
- ↑ Immune responses and immunity to SARS-CoV-2[permanent dead link], by European Centre for Disease Prevention and Control
- ↑ Vabret N, Britton GJ, Gruber C, Hegde S, Kim J, Kuksin M, et al. (June 2020). "Immunology of COVID-19: Current State of the Science". Immunity. 52 (6): 910–941. doi:10.1016/j.immuni.2020.05.002. PMC 7200337. PMID 32505227.
- ↑ 251.0 251.1 251.2 Cohen JI, Burbelo PD (December 2020). "Reinfection with SARS-CoV-2: Implications for Vaccines". Clinical Infectious Diseases. doi:10.1093/cid/ciaa1866. PMC 7799323. PMID 33338197. S2CID 229323810.
- ↑ "What if immunity to covid-19 doesn't last?". MIT Technology Review. Archived from the original on 28 August 2021. Retrieved 1 May 2020.
- ↑ Andreoni M, Londoño E, Casado L (3 March 2021). "Brazil's Covid Crisis Is a Warning to the Whole World, Scientists Say – Brazil is seeing a record number of deaths, and the spread of a more contagious coronavirus variant that may cause reinfection". The New York Times. Archived from the original on 3 March 2021. Retrieved 3 March 2021.
- ↑ Zimmer C (1 March 2021). "Virus Variant in Brazil Infected Many Who Had Already Recovered From Covid-19 – The first detailed studies of the so-called P.1 variant show how it devastated a Brazilian city. Now scientists want to know what it will do elsewhere". The New York Times. Archived from the original on 3 March 2021. Retrieved 3 March 2021.
- ↑ Centers for Disease Control and Prevention (May 2012). "Lesson 3: Measures of Risk Section 3: Mortality Frequency Measures". Principles of Epidemiology in Public Health Practice (Third ed.). U.S. Centers for Disease Control and Prevention (CDC). No. SS1978. Archived from the original on 28 February 2020. Retrieved 28 March 2020.
- ↑ Ritchie H, Roser M (25 March 2020). Chivers T (ed.). "What do we know about the risk of dying from COVID-19?". Our World in Data. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
- ↑ 257.0 257.1 257.2 257.3 Suarez, Alejandro Ivan (6 March 2021). "Mujeres mayores y pandemia por COVID-19". THE CONVERSATION. Archived from the original on 22 April 2021. Retrieved 22 April 2021.
- ↑ 258.0 258.1 258.2 258.3 258.4 258.5 Dehingia, Nabamallika (5 November 2020). "Sex differences in COVID-19 case fatality: do we know enough?". THE LANCET: GLOBAL HEALTH. Archived from the original on 28 April 2021. Retrieved 22 April 2021.
- ↑ Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, et al. (September 2020). "Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review". JAMA Pediatrics. 174 (9): 882–889. doi:10.1001/jamapediatrics.2020.1467. PMID 32320004.
- ↑ Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, et al. (April 2020). "SARS-CoV-2 Infection in Children". The New England Journal of Medicine. Massachusetts Medical Society. 382 (17): 1663–1665. doi:10.1056/nejmc2005073. PMC 7121177. PMID 32187458.
- ↑ Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S (June 2020). "Epidemiology of COVID-19 Among Children in China". Pediatrics. 145 (6): e20200702. doi:10.1542/peds.2020-0702. PMID 32179660. S2CID 219118986.
- ↑ Lazzerini M, Putoto G (May 2020). "COVID-19 in Italy: momentous decisions and many uncertainties". The Lancet. Global Health. 8 (5): e641–e642. doi:10.1016/S2214-109X(20)30110-8. PMC 7104294. PMID 32199072.
- ↑ "What do we know about the risk of dying from COVID-19?". Our World in Data. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
- ↑ 264.0 264.1 264.2 Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G (December 2020). "Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications". European Journal of Epidemiology. 35 (12): 1123–1138. doi:10.1007/s10654-020-00698-1. PMC 7721859. PMID 33289900.
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License Creative Commons — Attribution 4.0 International — CC BY 4.0 at the Wayback Machine (archived 2017-10-16).
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License Creative Commons — Attribution 4.0 International — CC BY 4.0 at the Wayback Machine (archived 2017-10-16).
- ↑ Mallapaty S (June 2020). "How deadly is the coronavirus? Scientists are close to an answer". Nature. 582 (7813): 467–468. Bibcode:2020Natur.582..467M. doi:10.1038/d41586-020-01738-2. PMID 32546810. S2CID 219726496.
- ↑ Alwan NA, Burgess RA, Ashworth S, Beale R, Bhadelia N, Bogaert D, et al. (October 2020). "Scientific consensus on the COVID-19 pandemic: we need to act now". Lancet. 396 (10260): e71–e72. doi:10.1016/S0140-6736(20)32153-X. PMC 7557300. PMID 33069277.
- ↑ Meyerowitz-Katz G, Merone L (December 2020). "A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates". International Journal of Infectious Diseases. 101: 138–148. doi:10.1016/j.ijid.2020.09.1464. PMC 7524446. PMID 33007452.
- ↑ Zhang D, Hu M, Ji Q (October 2020). "Financial markets under the global pandemic of COVID-19". Finance Research Letters. 36: 101528. Bibcode:2020CSFX....500043D. doi:10.1016/j.csfx.2020.100043. PMC 7402242. PMID 32837360.
- ↑ "Background paper on Covid-19 disease and vaccines: prepared by the Strategic Advisory Group of Experts (SAGE) on immunization working group on COVID-19 vaccines". World Health Organization. 22 December 2020. hdl:10665/338095. Archived from the original on 11 January 2021. Retrieved 8 May 2021.
- ↑ "Coronavirus disease 2019 (COVID-19) Situation Report – 30" (PDF). 19 February 2020. Archived (PDF) from the original on 2 March 2020. Retrieved 3 June 2020.
- ↑ "Coronavirus disease 2019 (COVID-19) Situation Report – 31" (PDF). 20 February 2020. Archived (PDF) from the original on 14 April 2020. Retrieved 23 April 2020.
- ↑ McNeil Jr DG (4 July 2020). "The Pandemic's Big Mystery: How Deadly Is the Coronavirus? – Even with more than 500,000 dead worldwide, scientists are struggling to learn how often the virus kills. Here's why". The New York Times. Archived from the original on 5 July 2020. Retrieved 6 July 2020.
- ↑ "Global Research and Innovation Forum on COVID-19: Virtual Press Conference" (PDF). World Health Organization. 2 July 2020. Archived (PDF) from the original on 4 May 2021. Retrieved 8 May 2021.
- ↑ "Estimating mortality from COVID-19". World Health Organization (WHO). Archived from the original on 23 January 2021. Retrieved 21 September 2020.
- ↑ "COVID-19: Data". City of New York. Archived from the original on 2020-06-05. Retrieved 2021-05-08.
- ↑ Wilson L (May 2020). "SARS-CoV-2, COVID-19, Infection Fatality Rate (IFR) Implied by the Serology, Antibody, Testing in New York City". SSRN 3590771.
- ↑ Yang W, Kandula S, Huynh M, Greene SK, Van Wye G, Li W, et al. (February 2021). "Estimating the infection-fatality risk of SARS-CoV-2 in New York City during the spring 2020 pandemic wave: a model-based analysis". The Lancet. Infectious Diseases. 21 (2): 203–212. doi:10.1016/s1473-3099(20)30769-6. PMC 7572090. PMID 33091374.
- ↑ Modi C (21 April 2020). "How deadly is COVID-19? Data Science offers answers from Italy mortality data". Medium. Archived from the original on 24 April 2020. Retrieved 23 April 2020.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 10 September 2020. Archived from the original on 11 January 2021. Retrieved 9 December 2020.
- ↑ Salje H, Tran Kiem C, Lefrancq N, Courtejoie N, Bosetti P, Paireau J, et al. (July 2020). "Estimating the burden of SARS-CoV-2 in France". Science. 369 (6500): 208–211. Bibcode:2020Sci...369..208S. doi:10.1126/science.abc3517. PMC 7223792. PMID 32404476.
- ↑ Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. (February 2020). "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study". Lancet. 395 (10223): 507–513. doi:10.1016/S0140-6736(20)30211-7. PMC 7135076. PMID 32007143.
- ↑ Wenham C, Smith J, Morgan R (March 2020). "COVID-19: the gendered impacts of the outbreak". Lancet. 395 (10227): 846–848. doi:10.1016/S0140-6736(20)30526-2. PMC 7124625. PMID 32151325.
- ↑ Epidemiology Working Group For Ncip Epidemic Response, Chinese Center for Disease Control Prevention (February 2020). "[The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]". Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi (in 中文). 41 (2): 145–151. doi:10.3760/cma.j.issn.0254-6450.2020.02.003. PMID 32064853. S2CID 211133882.
- ↑ "The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19)". China CDC Weekly. 2 (8): 113–122. February 2020. doi:10.46234/ccdcw2020.032. ISSN 2096-7071. Archived from the original on 19 February 2020. Retrieved 15 June 2020.
- ↑ Hu Y, Sun J, Dai Z, Deng H, Li X, Huang Q, et al. (June 2020). "Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis". Journal of Clinical Virology. 127: 104371. doi:10.1016/j.jcv.2020.104371. PMC 7195434. PMID 32315817.
- ↑ Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. (June 2020). "Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis". The Journal of Infection. 80 (6): 656–665. doi:10.1016/j.jinf.2020.03.041. PMC 7151416. PMID 32283155.
- ↑ Yuki K, Fujiogi M, Koutsogiannaki S (June 2020). "COVID-19 pathophysiology: A review". Clinical Immunology. 215: 108427. doi:10.1016/j.clim.2020.108427. PMC 7169933. PMID 32325252. S2CID 216028003.
- ↑ Rabin RC (20 March 2020). "In Italy, Coronavirus Takes a Higher Toll on Men". The New York Times. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- ↑ "COVID-19 weekly surveillance report". World Health Organization (WHO). Archived from the original on 15 March 2020. Retrieved 7 April 2020.
- ↑ 290.0 290.1 Gupta AH (3 April 2020). "Does Covid-19 Hit Women and Men Differently? U.S. Isn't Keeping Track". The New York Times. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- ↑ 291.0 291.1 Dorn AV, Cooney RE, Sabin ML (April 2020). "COVID-19 exacerbating inequalities in the US". Lancet. 395 (10232): 1243–1244. doi:10.1016/S0140-6736(20)30893-X. PMC 7162639. PMID 32305087.
- ↑ Adams ML, Katz DL, Grandpre J (August 2020). "Population-Based Estimates of Chronic Conditions Affecting Risk for Complications from Coronavirus Disease, United States". Emerging Infectious Diseases. 26 (8): 1831–1833. doi:10.3201/eid2608.200679. PMC 7392427. PMID 32324118.
- ↑ Batthyány, Karina. "Coronavirus y Desigualdades preexistentes: Género y Cuidados". CLACSO (Consejo Latinoamericano de Ciencias Sociales). Archived from the original on 19 April 2021. Retrieved 22 April 2021.
- ↑ "COVID-19 Presents Significant Risks for American Indian and Alaska Native People". 14 May 2020. Archived from the original on 11 May 2021. Retrieved 8 May 2021.
- ↑ "COVID-19 Presents Significant Risks for American Indian and Alaska Native People". 14 May 2020. Archived from the original on 11 May 2021. Retrieved 8 May 2021.
- ↑ Laurencin CT, McClinton A (June 2020). "The COVID-19 Pandemic: a Call to Action to Identify and Address Racial and Ethnic Disparities". Journal of Racial and Ethnic Health Disparities. 7 (3): 398–402. doi:10.1007/s40615-020-00756-0. PMC 7166096. PMID 32306369.
- ↑ "How coronavirus deaths in the UK compare by race and ethnicity". The Independent. 9 June 2020. Archived from the original on 10 June 2020. Retrieved 10 June 2020.
- ↑ "Emerging findings on the impact of COVID-19 on black and minority ethnic people". The Health Foundation. Archived from the original on 10 June 2020. Retrieved 10 June 2020.
- ↑ Butcher B, Massey J (9 June 2020). "Why are more BAME people dying from coronavirus?". BBC News. Archived from the original on 9 June 2020. Retrieved 10 June 2020.
- ↑ 300.0 300.1 300.2 The ancient Neanderthal in severe COVID-19 The ancient Neanderthal hand in severe COVID-19 -- ScienceDaily at the Wayback Machine (archived 2021-05-04), Science News, 30 September 2020. Retrieved 13 December 2020.
- ↑ "WHO Director-General's statement on the advice of the IHR Emergency Committee on Novel Coronavirus". World Health Organization (WHO). Archived from the original on 2020-01-27. Retrieved 2021-05-08.
- ↑ Garg S, Kim L, Whitaker M, O'Halloran A, Cummings C, Holstein R, et al. (April 2020). "Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 – COVID-NET, 14 States, March 1-30, 2020". MMWR. Morbidity and Mortality Weekly Report. 69 (15): 458–464. doi:10.15585/mmwr.mm6915e3. PMC 7755063. PMID 32298251.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 19 June 2020. Retrieved 19 June 2020.
- ↑ Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, et al. (October 2020). "The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis". Journal of Medical Virology. 92 (10): 1915–1921. doi:10.1002/jmv.25889. PMC 7262275. PMID 32293753.
- ↑ "Smoking and COVID-19". World Health Organization (WHO). Archived from the original on 23 August 2020. Retrieved 19 June 2020.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 19 June 2020. Retrieved 4 May 2020.
- ↑ DeRobertis J (3 May 2020). "People who use drugs are more vulnerable to coronavirus. Here's what clinics are doing to help". The Advocate (Louisiana). Archived from the original on 6 May 2020. Retrieved 4 May 2020.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 7 May 2021. Retrieved 8 May 2021.
- ↑ Berger K (12 March 2020). "The Man Who Saw the Pandemic Coming". Nautilus. Archived from the original on 15 March 2020. Retrieved 16 March 2020.
- ↑ Duarte F (24 February 2020). "As the cases of coronavirus increase in China and around the world, the hunt is on to identify "patient zero"". BBC News. Archived from the original on 8 March 2020. Retrieved 22 March 2020.
- ↑ Li X, Zai J, Zhao Q, Nie Q, Li Y, Foley BT, Chaillon A (June 2020). "Evolutionary history, potential intermediate animal host, and cross-species analyses of SARS-CoV-2". Journal of Medical Virology. 92 (6): 602–611. doi:10.1002/jmv.25731. PMC 7228310. PMID 32104911.
- ↑ Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF (April 2020). "The proximal origin of SARS-CoV-2". Nature Medicine. 26 (4): 450–452. doi:10.1038/s41591-020-0820-9. PMC 7095063. PMID 32284615.
- ↑ van Dorp L, Acman M, Richard D, Shaw LP, Ford CE, Ormond L, et al. (September 2020). "Emergence of genomic diversity and recurrent mutations in SARS-CoV-2". Infection, Genetics and Evolution. 83: 104351. doi:10.1016/j.meegid.2020.104351. PMC 7199730. PMID 32387564.
- ↑ Shield C (26 March 2020). "Coronavirus: From bats to pangolins, how do viruses reach us?". Deutsche Welle. Archived from the original on 4 June 2020. Retrieved 1 December 2020.
- ↑ "WHO Points To Wildlife Farms In Southern China As Likely Source Of Pandemic". NPR. 15 March 2021. Archived from the original on 28 August 2021. Retrieved 8 May 2021.
- ↑ Wu YC, Chen CS, Chan YJ (March 2020). "The outbreak of COVID-19: An overview". Journal of the Chinese Medical Association. 83 (3): 217–220. doi:10.1097/JCMA.0000000000000270. PMC 7153464. PMID 32134861.
- ↑ Wang C, Horby PW, Hayden FG, Gao GF (February 2020). "A novel coronavirus outbreak of global health concern". Lancet. 395 (10223): 470–473. doi:10.1016/S0140-6736(20)30185-9. PMC 7135038. PMID 31986257.
- ↑ Cohen J (January 2020). "Wuhan seafood market may not be source of novel virus spreading globally". Science. doi:10.1126/science.abb0611. Archived from the original on 2020-01-27. Retrieved 2021-05-08.
- ↑ "Novel Coronavirus – China". World Health Organization (WHO). 12 January 2020. Archived from the original on 14 January 2020. Retrieved 8 May 2021.
- ↑ Kessler G (17 April 2020). "Trump's false claim that the WHO said the coronavirus was 'not communicable'". The Washington Post. Archived from the original on 17 April 2020. Retrieved 17 April 2020.
- ↑ Kuo L (21 January 2020). "China confirms human-to-human transmission of coronavirus". The Guardian. Archived from the original on 22 March 2020. Retrieved 18 April 2020.
- ↑ Epidemiology Working Group For Ncip Epidemic Response, Chinese Center for Disease Control Prevention (February 2020). "[The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]". Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi (in 中文). 41 (2): 145–151. doi:10.3760/cma.j.issn.0254-6450.2020.02.003. PMID 32064853. S2CID 211133882.
- ↑ Areddy JT (26 May 2020). "China Rules Out Animal Market and Lab as Coronavirus Origin". The Wall Street Journal. Archived from the original on 17 February 2021. Retrieved 29 May 2020.
- ↑ Kelland K (19 June 2020). "Italy sewage study suggests COVID-19 was there in December 2019". Reuters. Archived from the original on 24 June 2020. Retrieved 23 June 2020.
- ↑ Yanping Z, et al. (The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team) (February 2020). "The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) – China, 2020". China CDC Weekly. Chinese Center for Disease Control and Prevention. 2 (8): 113–122. doi:10.46234/ccdcw2020.032. Archived from the original on 19 February 2020. Retrieved 18 March 2020.
- ↑ Heymann DL, Shindo N (February 2020). "COVID-19: what is next for public health?". Lancet. 395 (10224): 542–545. doi:10.1016/S0140-6736(20)30374-3. PMC 7138015. PMID 32061313.
- ↑ March 2020, Jeanna Bryner-Live Science Editor-in-Chief 14. "1st known case of coronavirus traced back to November in China". livescience.com. Archived from the original on 14 March 2020. Retrieved 31 May 2020.
- ↑ Politics, Canadian (8 April 2020). "The birth of a pandemic: How COVID-19 went from Wuhan to Toronto | National Post". Archived from the original on 28 August 2021. Retrieved 31 May 2020.
- ↑ 高昱 (26 February 2020). "独家 | 新冠病毒基因测序溯源:警报是何时拉响的" [Exclusive | Tracing the New Coronavirus gene sequencing: when did the alarm sound]. Caixin (in 中文). Archived from the original on 27 February 2020. Retrieved 1 March 2020.
- ↑ 路子康. "最早上报疫情的她,怎样发现这种不一样的肺炎". 中国网新闻 (in 中文(中国大陆)). 北京. Archived from the original on 2 March 2020. Retrieved 11 February 2020.
- ↑ "Undiagnosed pneumonia – China (HU): RFI". ProMED Mail. ProMED. Archived from the original on 18 May 2020. Retrieved 7 May 2020.
- ↑ "'Hero who told the truth': Chinese rage over coronavirus death of whistleblower doctor". The Guardian. 7 February 2020. Archived from the original on 11 May 2020. Retrieved 8 May 2021.
- ↑ Kuo L (11 March 2020). "Coronavirus: Wuhan doctor speaks out against authorities". The Guardian. London. Archived from the original on 11 May 2020. Retrieved 8 May 2021.
- ↑ "Novel Coronavirus". World Health Organization (WHO). Archived from the original on 2 February 2020. Retrieved 6 February 2020.
- ↑ "武汉现不明原因肺炎 官方确认属实:已经做好隔离". Xinhua Net 新華網. 31 December 2019. Archived from the original on 22 April 2020. Retrieved 31 March 2020.
- ↑ 武汉市卫健委关于当前我市肺炎疫情的情况通报. WJW.Wuhan.gov.cn (in 中文). Wuhan Municipal Health Commission. 31 December 2019. Archived from the original on 9 January 2020. Retrieved 8 February 2020.
- ↑ "Mystery pneumonia virus probed in China". BBC News. 3 January 2020. Archived from the original on 5 January 2020. Retrieved 29 January 2020.
- ↑ Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. (March 2020). "Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia". The New England Journal of Medicine. 382 (13): 1199–1207. doi:10.1056/NEJMoa2001316. PMC 7121484. PMID 31995857.
- ↑ "China confirms sharp rise in cases of SARS-like virus across the country". 20 January 2020. Archived from the original on 20 January 2020. Retrieved 20 January 2020.
- ↑ The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (February 2020). "The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) – China, 2020". China CDC Weekly. 2 (8): 113–122. doi:10.46234/ccdcw2020.032. Archived from the original on 19 February 2020. Retrieved 18 March 2020.
- ↑ 341.0 341.1 "Flattery and foot dragging: China's influence over the WHO under scrutiny". The Globe and Mail. 25 April 2020. Archived from the original on 27 April 2020. Retrieved 8 May 2021.
- ↑ Horton R (18 March 2020). "Scientists have been sounding the alarm on coronavirus for months. Why did Britain fail to act?". The Guardian. Archived from the original on 18 March 2020. Retrieved 23 April 2020.
- ↑ "China delayed releasing coronavirus info, frustrating WHO". AP NEWS. 2 June 2020. Archived from the original on 2 June 2020. Retrieved 3 June 2020.
- ↑ "Coronavirus: Primi due casi in Italia" [Coronavirus: First two cases in Italy]. Corriere della sera (in italiano). 31 January 2020. Archived from the original on 13 April 2020. Retrieved 31 January 2020.
- ↑ Fredericks B (13 March 2020). "WHO says Europe is new epicenter of coronavirus pandemic". New York Post. Archived from the original on 14 March 2020. Retrieved 9 May 2020.
- ↑ "Coronavirus: Number of COVID-19 deaths in Italy surpasses China as total reaches 3,405". Sky News. Archived from the original on 29 April 2020. Retrieved 7 May 2020.
- ↑ McNeil Jr DG (26 March 2020). "The U.S. Now Leads the World in Confirmed Coronavirus Cases". The New York Times. Archived from the original on 11 May 2020. Retrieved 27 March 2020.
- ↑ "Studies Show N.Y. Outbreak Originated in Europe". The New York Times. 8 April 2020. Archived from the original on 14 May 2020. Retrieved 8 May 2021.
- ↑ Irish J (4 May 2020). Lough RM, Graff P (eds.). "After retesting samples, French hospital discovers COVID-19 case from December". Reuters. Archived from the original on 18 May 2020. Retrieved 4 May 2020.
- ↑ Deslandes A, Berti V, Tandjaoui-Lambotte Y, Alloui C, Carbonnelle E, Zahar JR, et al. (June 2020). "SARS-CoV-2 was already spreading in France in late December 2019". International Journal of Antimicrobial Agents. 55 (6): 106006. doi:10.1016/j.ijantimicag.2020.106006. PMC 7196402. PMID 32371096.
- ↑ "2 died with coronavirus weeks before 1st U.S. virus death". PBS NewsHour. 22 April 2020. Archived from the original on 19 May 2020. Retrieved 23 April 2020.
- ↑ Michael-Kordatou I, Karaolia P, Fatta-Kassinos D (October 2020). "Sewage analysis as a tool for the COVID-19 pandemic response and management: the urgent need for optimised protocols for SARS-CoV-2 detection and quantification". Journal of Environmental Chemical Engineering. 8 (5): 104306. doi:10.1016/j.jece.2020.104306. PMC 7384408. PMID 32834990.
- ↑ Platto S, Xue T, Carafoli E (September 2020). "COVID19: an announced pandemic". Cell Death & Disease. 11 (9): 799. doi:10.1038/s41419-020-02995-9. PMC 7513903. PMID 32973152.
- ↑ "2nd U.S. Case Of Wuhan Coronavirus Confirmed". NPR. Archived from the original on 24 January 2020. Retrieved 4 April 2020.
- ↑ McNeil Jr DG (2 February 2020). "Wuhan Coronavirus Looks Increasingly Like a Pandemic, Experts Say". The New York Times. ISSN 0362-4331. Archived from the original on 15 January 2021. Retrieved 4 April 2020.
- ↑ Griffiths J. "Wuhan coronavirus deaths spike again as outbreak shows no signs of slowing". CNN. Archived from the original on 20 December 2020. Retrieved 4 April 2020.
- ↑ Jiang S, Xia S, Ying T, Lu L (May 2020). "A novel coronavirus (2019-nCoV) causing pneumonia-associated respiratory syndrome". Cellular & Molecular Immunology. 17 (5): 554. doi:10.1038/s41423-020-0372-4. PMC 7091741. PMID 32024976.
- ↑ Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. (February 2020). "A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster". Lancet. 395 (10223): 514–523. doi:10.1016/S0140-6736(20)30154-9. PMC 7159286. PMID 31986261.
- ↑ Shablovsky S (September 2017). "The legacy of the Spanish flu". Science. 357 (6357): 1245. Bibcode:2017Sci...357.1245S. doi:10.1126/science.aao4093. ISSN 0036-8075. S2CID 44116811. Archived from the original on 2020-10-19. Retrieved 2021-05-08.
- ↑ "Stop the coronavirus stigma now". Nature. 7 April 2020. p. 165. doi:10.1038/d41586-020-01009-0. Archived from the original on 12 May 2020. Retrieved 16 April 2020.
- ↑ "Novel Coronavirus (2019-nCoV) Situation Report – 1" (PDF). World Health Organization (WHO). 21 January 2020. Archived (PDF) from the original on 8 January 2021. Retrieved 8 May 2021.
- ↑ "Novel Coronavirus(2019-nCoV) Situation Report – 10" (PDF). World Health Organization (WHO). 30 January 2020. Archived (PDF) from the original on 30 January 2020. Retrieved 8 May 2021.
- ↑ "Novel coronavirus named 'Covid-19': WHO". Today. Singapore. Archived from the original on 21 March 2020. Retrieved 11 February 2020.
- ↑ "The coronavirus spreads racism against – and among – ethnic Chinese". The Economist. 17 February 2020. Archived from the original on 17 February 2020. Retrieved 17 February 2020.
- ↑ World Health Organization Best Practices for the Naming of New Human Infectious Diseases (PDF) (Report). World Health Organization (WHO). May 2015. hdl:10665/163636. Archived (PDF) from the original on 2020-02-12. Retrieved 2021-05-08.
- ↑ 366.0 366.1 "Naming the coronavirus disease (COVID-19) and the virus that causes it". World Health Organization (WHO). Archived from the original on 28 February 2020. Retrieved 13 March 2020.
- ↑ Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK – eighth update (PDF) (Report). ecdc. Archived (PDF) from the original on 14 March 2020. Retrieved 19 April 2020.
- ↑ Uttley H (2 March 2021). "Pandemic sends demand for cold and flu remedies to record low". The Telegraph. Archived from the original on 2 March 2021. Retrieved 28 March 2021.
- ↑ "China coronavirus: Misinformation spreads online about origin and scale". BBC News. 30 January 2020. Archived from the original on 4 February 2020. Retrieved 10 February 2020.
- ↑ Taylor J (31 January 2020). "Bat soup, dodgy cures and 'diseasology': the spread of coronavirus misinformation". The Guardian. Archived from the original on 2 February 2020. Retrieved 3 February 2020.
- ↑ "Here's A Running List Of Disinformation Spreading About The Coronavirus". Buzzfeed News. Archived from the original on 6 February 2020. Retrieved 8 February 2020.
- ↑ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 11 January 2021. Retrieved 10 October 2020.
- ↑ "Misleading claim circulates online about infection fatality ratio of Covid-19 in the US". Fact Check. 8 October 2020. Archived from the original on 28 November 2020. Retrieved 10 October 2020.
- ↑ 374.0 374.1 374.2 374.3 Kampf G, Brüggemann Y, Kaba HE, Steinmann J, Pfaender S, Scheithauer S, Steinmann E (December 2020). "Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2". The Journal of Hospital Infection. 106 (4): 678–697. doi:10.1016/j.jhin.2020.09.022. PMC 7500278. PMID 32956786.
- ↑ Shi, Jianzhong; Wen, Zhiyuan; Zhong, Gongxun; Yang, Huanliang; Wang, Chong; Huang, Baoying; Liu, Renqiang; He, Xijun; Shuai, Lei; Sun, Ziruo; Zhao, Yubo; Liu, Peipei; Liang, Libin; Cui, Pengfei; Wang, Jinliang; Zhang, Xianfeng; Guan, Yuntao; Tan, Wenjie; Wu, Guizhen; Chen, Hualan; Bu, Zhigao (2020). "Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2". Science. 368 (6494): 1016–1020. doi:10.1126/science.abb7015. PMC 7164390. PMID 32269068.
- ↑ 376.0 376.1 376.2 376.3 376.4 376.5 376.6 376.7 Salajegheh Tazerji S, Magalhães Duarte P, Rahimi P, Shahabinejad F, Dhakal S, Singh Malik Y, et al. (September 2020). "Transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to animals: an updated review". Journal of Translational Medicine. 18 (1): 358. doi:10.1186/s12967-020-02534-2. PMC 7503431. PMID 32957995.
- ↑ 377.0 377.1 377.2 Gorman J (22 January 2021). "The Coronavirus Kills Mink, So They Too May Get a Vaccine". The New York Times. ISSN 0362-4331. Archived from the original on 24 February 2021. Retrieved 24 February 2021.
- ↑ Dhama K, Sharun K, Tiwari R, Dadar M, Malik YS, Singh KP, Chaicumpa W (June 2020). "COVID-19, an emerging coronavirus infection: advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics". Human Vaccines & Immunotherapeutics. 16 (6): 1232–1238. doi:10.1080/21645515.2020.1735227. PMC 7103671. PMID 32186952.
- ↑ Zhang L, Liu Y (May 2020). "Potential interventions for novel coronavirus in China: A systematic review". Journal of Medical Virology. 92 (5): 479–490. doi:10.1002/jmv.25707. PMC 7166986. PMID 32052466.
- ↑ "Interim Laboratory Biosafety Guidelines for Handling and Processing Specimens Associated with Coronavirus Disease 2019 (COVID-19)". Coronavirus Disease 2019 (COVID-19) Lab Biosafety Guidelines. Centers for Disease Control and Prevention. Archived from the original on 16 February 2021. Retrieved 1 April 2020.
- ↑ Aristovnik A, Ravšelj D, Umek L (November 2020). "A Bibliometric Analysis of COVID-19 across Science and Social Science Research Landscape". Sustainability. 12 (21): 9132. doi:10.3390/su12219132.
- ↑ Kupferschmidt K (3 December 2020). "First-of-its-kind African trial tests common drugs to prevent severe COVID-19". Science. Archived from the original on 3 December 2020. Retrieved 10 December 2020.
- ↑ Reardon S (13 November 2020). "For COVID Drugs, Months of Frantic Development Lead to Few Outright Successes". Scientific American. Archived from the original on 13 November 2020. Retrieved 10 December 2020.
- ↑ Kucharski AJ, Russell TW, Diamond C, Liu Y, Edmunds J, Funk S, Eggo RM (May 2020). "Early dynamics of transmission and control of COVID-19: a mathematical modelling study". The Lancet. Infectious Diseases. 20 (5): 553–558. doi:10.1016/S1473-3099(20)30144-4. PMC 7158569. PMID 32171059.
- ↑ Wynants L, Van Calster B, Collins GS, Riley RD, Heinze G, Schuit E, et al. (April 2020). "Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal". BMJ. 369: m1328. doi:10.1136/bmj.m1328. PMC 7222643. PMID 32265220.
- ↑ Giordano G, Blanchini F, Bruno R, Colaneri P, Di Filippo A, Di Matteo A, Colaneri M (June 2020). "Modelling the COVID-19 epidemic and implementation of population-wide interventions in Italy". Nature Medicine. 26 (6): 855–860. doi:10.1038/s41591-020-0883-7. PMC 7175834. PMID 32322102.
- ↑ Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, et al. (May 2020). "The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study". The Lancet. Public Health. 5 (5): e261–e270. doi:10.1016/S2468-2667(20)30073-6. PMC 7158905. PMID 32220655.
- ↑ Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. (May 2020). "Fair Allocation of Scarce Medical Resources in the Time of Covid-19". The New England Journal of Medicine. 382 (21): 2049–2055. doi:10.1056/NEJMsb2005114. PMID 32202722.
- ↑ Kermack WO, McKendrick AG (1927). "A contribution to the mathematical theory of epidemics". Proceedings of the Royal Society of London. Series A, Containing Papers of a Mathematical and Physical Character. 115 (772): 700–721. Bibcode:1927RSPSA.115..700K. doi:10.1098/rspa.1927.0118.
- ↑ Mittal R, Ni R, Seo JH (2020). "The flow physics of COVID-19". Journal of Fluid Mechanics. 894: –2. arXiv:2004.09354. Bibcode:2020JFM...894F...2M. doi:10.1017/jfm.2020.330.
- ↑ Ronchi E, Lovreglio R (October 2020). "EXPOSED: An occupant exposure model for confined spaces to retrofit crowd models during a pandemic". Safety Science. 130: 104834. arXiv:2005.04007. doi:10.1016/j.ssci.2020.104834. PMC 7373681. PMID 32834509.
- ↑ Badr HS, Du H, Marshall M, Dong E, Squire MM, Gardner LM (November 2020). "Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study". The Lancet Infectious Diseases. 20 (11): 1247–1254. doi:10.1016/S1473-3099(20)30553-3. PMC 7329287. PMID 32621869.
- ↑ McKibbin W, Roshen F (2020). "The global macroeconomic impacts of COVID-19: Seven scenarios" (PDF). CAMA Working Paper. doi:10.2139/ssrn.3547729. S2CID 216307705. Archived (PDF) from the original on 2021-05-06. Retrieved 2021-05-08.
- ↑ Bundy J, Pfarrer MD, Short CE, Coombs WT (July 2017). "Crises and crisis management: Integration, interpretation, and research development". Journal of Management. 43 (6): 1661–92. doi:10.1177/0149206316680030. S2CID 152223772.
- ↑ Kraus S, Clauss T, Breier M, Gast J, Zardini A, Tiberius V (2020). "The economics of COVID-19: initial empirical evidence on how family firms in five European countries cope with the corona crisis". International Journal of Entrepreneurial Behavior & Research. 26 (5): 1067–1092. doi:10.1108/IJEBR-04-2020-0214. ISSN 1355-2554. S2CID 219144929. Archived from the original on 2021-08-28. Retrieved 2021-05-08.
- ↑ "COVID-19 treatment and vaccine tracker" (PDF). Milken Institute. 21 April 2020. Archived (PDF) from the original on 22 April 2020. Retrieved 21 April 2020.
- Lay summary in: https://milkeninstitute.org/covid-19-tracker.
{{cite web}}: Missing or empty|title=(help)
- Lay summary in: https://milkeninstitute.org/covid-19-tracker.
- ↑ 397.0 397.1 Koch S, Pong W (13 March 2020). "First up for COVID-19: nearly 30 clinical readouts before end of April". BioCentury Inc. Archived from the original on 3 April 2020. Retrieved 1 April 2020.
- ↑ Kupferschmidt K, Cohen J (March 2020). "WHO launches global megatrial of the four most promising coronavirus treatments". Science. doi:10.1126/science.abb8497.
- ↑ "UN health chief announces global 'solidarity trial' to jumpstart search for COVID-19 treatment". UN News. 18 March 2020. Archived from the original on 23 March 2020. Retrieved 23 March 2020.
- ↑ "Citing safety concerns, the W.H.O. paused tests of a drug Trump said he had taken". The New York Times. 26 May 2020. Archived from the original on 6 May 2021. Retrieved 8 May 2021.
- ↑ "Hydroxychloroquine does not benefit adults hospitalized with COVID-19". National Institutes of Health (NIH) (Press release). 9 November 2020. Archived from the original on 9 November 2020. Retrieved 9 November 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Coronavirus (COVID-19) Update: FDA Warns of Newly Discovered Potential Drug Interaction That May Reduce Effectiveness of a COVID-19 Treatment Authorized for Emergency Use". U.S. Food and Drug Administration (FDA) (Press release). 15 June 2020. Archived from the original on 13 October 2020. Retrieved 15 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "France bans use of hydroxychloroquine, drug touted by Trump, in coronavirus patients". CBS News. 27 May 2020. Archived from the original on 6 May 2021. Retrieved 8 May 2021.
- ↑ Boseley S (16 June 202). "Recovery trial for Covid-19 treatments: what we know so far". The Guardian. Archived from the original on 20 June 2020. Retrieved 21 June 2020.
- ↑ "WHO welcomes preliminary results about dexamethasone use in treating critically ill COVID-19 patients". World Health Organization (WHO) (Press release). 16 June 2020. Archived from the original on 17 June 2020. Retrieved 21 June 2020.
- ↑ "Q&A: Dexamethasone and COVID-19". World Health Organization (WHO) (Press release). Archived from the original on 11 October 2020. Retrieved 12 July 2020.
- ↑ "Corticosteroids". COVID-19 Treatment Guidelines. National Institutes of Health. Archived from the original on 19 July 2020. Retrieved 12 July 2020.
- ↑ 408.0 408.1 408.2 World Health Organization (2020). Corticosteroids for COVID-19: living guidance, 2 September 2020 (Report). hdl:10665/334125. WHO/2019-nCoV/Corticosteroids/2020.1.
- Lay summary in: WHO updates clinical care guidance with corticosteroid recommendations (Report).
- ↑ Sterne JA, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, et al. (The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group) (October 2020). "Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis". JAMA. 324 (13): 1330–1341. doi:10.1001/jama.2020.17023. PMC 7489434. PMID 32876694. S2CID 221467783.
- ↑ Prescott HC, Rice TW (October 2020). "Corticosteroids in COVID-19 ARDS: Evidence and Hope During the Pandemic". JAMA. 324 (13): 1292–1295. doi:10.1001/jama.2020.16747. PMID 32876693. S2CID 221468015.
- ↑ 411.0 411.1 "EMA endorses use of dexamethasone in COVID-19 patients on oxygen or mechanical ventilation". European Medicines Agency (EMA) (Press release). 18 September 2020. Archived from the original on 14 February 2021. Retrieved 21 September 2020. Text was copied from this source which is European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ↑ "Archive copy" (PDF). Archived (PDF) from the original on 2021-05-06. Retrieved 2021-05-08.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ 413.0 413.1 413.2 "Coronavirus (COVID-19) Update: FDA Authorizes Monoclonal Antibody for Treatment of COVID-19". U.S. Food and Drug Administration (FDA) (Press release). 9 November 2020. Archived from the original on 11 January 2021. Retrieved 9 November 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "FDA Authorizes Monoclonal Antibodies for Treatment of COVID-19". U.S. Food and Drug Administration (FDA) (Press release). 10 February 2021. Archived from the original on 10 February 2021. Retrieved 9 February 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Monoclonal Antibody Bamlanivimab". U.S. Food and Drug Administration (FDA) (Press release). 16 April 2021. Archived from the original on 16 April 2021. Retrieved 16 April 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
External links
Health agencies
- Coronavirus disease (COVID-19) Archived 2020-01-30 at the Wayback Machine FACTS Archived 2020-02-06 at the Wayback Machine by the World Health Organization (WHO)
- Coronavirus 2019 (COVID-19) Archived 2020-01-20 at the Wayback Machine by the US Centers for Disease Control and Prevention (CDC)
- Coronavirus (COVID-19) Archived 2020-03-02 at the Wayback Machine by the UK National Health Service (NHS)
Directories
- Coronavirus Resource Center Archived 2021-05-15 at the Wayback Machine at the Center for Inquiry
- COVID-19 at Curlie
- COVID-19 Resource Directory on OpenMD Archived 2021-05-06 at the Wayback Machine
- COVID-19 Information on FireMountain.net Archived 2021-05-08 at the Wayback Machine
Medical journals
- Coronavirus Disease 2019 (COVID-19) Archived 2021-05-08 at the Wayback Machine by JAMA
- BMJ's Coronavirus (covid-19) Hub Archived 2021-05-06 at the Wayback Machine by the BMJ
- Novel Coronavirus Information Center Archived 2020-01-30 at the Wayback Machine by Elsevier
- COVID-19 Resource Centre Archived 2020-02-23 at the Wayback Machine by The Lancet
- Coronavirus (COVID-19) Research Highlights Archived 2020-08-02 at the Wayback Machine by Springer Nature
- Coronavirus (Covid-19) Archived 2021-05-07 at the Wayback Machine by The New England Journal of Medicine
- Covid-19: Novel Coronavirus Archived 2020-09-24 at the Wayback Machine by Wiley Publishing
Treatment guidelines
- WHO living guideline Archived 2022-11-04 at the Wayback Machine
- "JHMI Clinical Recommendations for Available Pharmacologic Therapies for COVID-19" (PDF). The Johns Hopkins University. Archived from the original on 2021-08-28. Retrieved 2021-05-08.
- "Bouncing Back From COVID-19: Your Guide to Restoring Movement" (PDF). The Johns Hopkins School of Medicine. Archived (PDF) from the original on 2021-02-15. Retrieved 2021-05-08.
- "Guidelines on the Treatment and Management of Patients with COVID-19" (PDF). Infectious Diseases Society of America. Archived (PDF) from the original on 2021-04-05. Retrieved 2021-05-08. Lay summary.
{{cite web}}: Cite uses deprecated parameter|lay-url=(help) - "Coronavirus Disease 2019 (COVID-19) Treatment Guidelines" (PDF). National Institutes of Health. Archived (PDF) from the original on 2021-05-06. Retrieved 2021-05-08. Lay summary.
{{cite web}}: Cite uses deprecated parameter|lay-url=(help) - World Health Organization (2020). Therapeutics and COVID-19: living guideline, 17 December 2020 (Report). hdl:10665/337876. WHO/2019-nCoV/therapeutics/2020.1. Lay summary.
{{cite report}}: Cite uses deprecated parameter|lay-url=(help) - NHS England and NHS Improvement. National Guidance for post-COVID syndrome assessment clinics (PDF) (Report). Archived from the original (PDF) on 2021-03-29. Retrieved 2021-05-08. Lay summary.
{{cite report}}: Cite uses deprecated parameter|lay-url=(help)
| Classification |
|---|
- Pages with script errors
- Webarchive template wayback links
- Webarchive template warnings
- CS1 italiano-language sources (it)
- CS1: long volume value
- CS1 maint: PMC embargo expired
- CS1 maint: multiple names: authors list
- CS1 errors: missing periodical
- All articles with dead external links
- Articles with dead external links from April 2021
- Articles with invalid date parameter in template
- Articles with permanently dead external links
- CS1 中文-language sources (zh)
- CS1 中文(中国大陆)-language sources (zh)
- CS1 uses 中文-language script (zh)
- CS1 errors: missing title
- CS1 errors: bare URL
- Wikipedia articles incorporating the PD-notice template
- CS1 maint: archived copy as title
- Articles with hatnote templates targeting a nonexistent page
- Missing redirects
- Portal templates with all redlinked portals
- Portal-inline template with redlinked portals
- Articles with excerpts
- Articles containing potentially dated statements from January 2021
- All articles containing potentially dated statements
- Articles containing potentially dated statements from January 2022
- All articles lacking reliable references
- Articles lacking reliable references from May 2021
- Articles containing potentially dated statements from December 2020
- Articles containing potentially dated statements from November 2020
- Wikipedia articles in need of updating from March 2021
- All Wikipedia articles in need of updating
- Articles containing potentially dated statements from May 2020
- Articles with Curlie links
- CS1 errors: deprecated parameters
- COVID-19
- Occupational safety and health
- Viral respiratory tract infections
- Zoonoses
- Public health
- RTT
- RTTCovid






![Role of B cells in COVID-19 infection/re-infection- Naïve B cells are activated via the help of folliculat T cells after the invasion of SARS-CoV-2 virus[79]](https://nccommons.org/media/thumb/c/cb/Fimmu-13-988536-g001.jpg/710px-Fimmu-13-988536-g001.jpg)