Erectile dysfunction
| Erectile dysfunction | |
|---|---|
| Other names: Impotence | |
 | |
| Cross-section of a flaccid penis | |
| Specialty | Urology |
| Symptoms | Inability to gain or maintain an erection[1] |
| Complications | Depression, anxiety, infertility[1] |
| Risk factors | Diabetes, heart disease, being overweight, kidney problems, smoking, alcohol,, anxiety, certain medications[2] |
| Diagnostic method | Based on symptoms and examination[3] |
| Treatment | Lifestyle changes, counselling, medication, surgery[4] |
| Medication | Sildenafil, alprostadil[4] |
| Prognosis | Depends on the cause[5] |
| Frequency | Very common (>150 million people globally)[1][5] |
Erectile dysfunction (ED), also called impotence, is the type of sexual dysfunction in which the penis fails to become sufficiently erect for satisfactory sexual activity.[1] It can be a short or long term issue.[1] It can affect quality of life and result in depression, anxiety, or infertility.[1]
Risk factors include diabetes, heart disease, being overweight, kidney problems, smoking, alcohol,, anxiety, and certain medications.[2] Medications that may be involved include blood pressure medication, antiandrogens, benzodiazepines, and antidepressants.[2] It can also occur after certain procedures such as prostate surgery.[2] Diagnosis is based on symptoms and examination.[3]
Treatment may involve addressing the underlying causes, lifestyle changes, and counselling.[4] Medications such as sildenafil (a PDE5 inhibitor) may be used.[4] Other options may include alprostadil or penis pump. If these measures are not effective surgery, in the form of a penile implants or vascular reconstructive, may be an option.[4] Outcomes depend on the cause.[5]
Erectile dysfunction is very common, affecting about 30 million males in the United States.[1] While it becomes more common with age, it is not a normal part of aging.[1] Up to half of men over the age of 40 may be affected.[5] People all over the world are affected.[5]
Signs and symptoms
ED is characterized by the regular or repeated inability to achieve or maintain an erection of sufficient rigidity to accomplish sexual activity. It is defined as the "persistent or recurrent inability to achieve and maintain a penile erection of sufficient rigidity to permit satisfactory sexual activity for at least 3 months."[6]
Psychological
ED often has an impact on the emotional well-being of both men and their partners. Many men do not seek treatment due to feelings of embarrassment. About 75% of diagnosed cases of ED go untreated.[7]
Causes
Causes of or contributors to ED include the following:
- Diets high in saturated fat are linked to heart disease and men with heart disease are more likely to experience ED.[8][9] By contrast, plant-based diets show a lower risk for ED.[10][11][12]
- Prescription drugs (e.g., SSRIs,[13] beta blockers, alpha-2 adrenergic receptor agonists, thiazides, hormone modulators, and 5α-reductase inhibitors)[14][6]
- Neurogenic disorders (e.g., diabetic neuropathy, temporal lobe epilepsy, multiple sclerosis, Parkinson's disease, multiple system atrophy)[14][6][15]
- Cavernosal disorders (e.g., Peyronie's disease)[14][16]
- Hyperprolactinemia (e.g., due to a prolactinoma)[14]
- Psychological causes: performance anxiety, stress, and mental disorders[17]
- Surgery (e.g., radical prostatectomy)[18]
- Aging: after age 40 years, aging itself is a risk factor for ED, although numerous other pathologies that may occur with aging, such as testosterone deficiency, cardiovascular diseases, or diabetes, among others, appear to have interacting effects[19][20]
- Kidney disease: ED and chronic kidney disease have pathological mechanisms in common, including vascular and hormonal dysfunction, and may share other comorbidities, such as hypertension and diabetes mellitus that can contribute to ED[21]
- Lifestyle habits, particularly smoking, which is a key risk factor for ED as it promotes arterial narrowing.[22][23][24]
- COVID-19: preliminary research indicates that COVID-19 viral infection may affect sexual and reproductive health[25][26]
Surgical intervention for a number of conditions may remove anatomical structures necessary to erection, damage nerves, or impair blood supply.[18] ED is a common complication of treatments for prostate cancer, including prostatectomy and destruction of the prostate by external beam radiation, although the prostate gland itself is not necessary to achieve an erection. As far as inguinal hernia surgery is concerned, in most cases, and in the absence of postoperative complications, the operative repair can lead to a recovery of the sexual life of people with preoperative sexual dysfunction, while, in most cases, it does not affect people with a preoperative normal sexual life.[27]
ED can also be associated with bicycling due to both neurological and vascular problems due to compression.[28] The increased risk appears to be about 1.7-fold.[29]
Concerns that use of pornography can cause ED[30] have little support[31][32][33] According to Gunter de Win, a Belgian professor and sex researcher, "Put simply, respondents who watch 60 minutes a week and think they're addicted were more likely to report sexual dysfunction than those who watch a care-free 160 minutes weekly."[34][35]
Pathophysiology
Penile erection is managed by two mechanisms: the reflex erection, which is achieved by directly touching the penile shaft, and the psychogenic erection, which is achieved by erotic or emotional stimuli. The former involves the peripheral nerves and the lower parts of the spinal cord, whereas the latter involves the limbic system of the brain. In both cases, an intact neural system is required for a successful and complete erection. Stimulation of the penile shaft by the nervous system leads to the secretion of nitric oxide (NO), which causes the relaxation of the smooth muscles of the corpora cavernosa (the main erectile tissue of the penis), and subsequently penile erection. Additionally, adequate levels of testosterone (produced by the testes) and an intact pituitary gland are required for the development of a healthy erectile system. As can be understood from the mechanisms of a normal erection, impotence may develop due to hormonal deficiency, disorders of the neural system, lack of adequate penile blood supply or psychological problems.[36] Spinal cord injury causes sexual dysfunction, including ED. Restriction of blood flow can arise from impaired endothelial function due to the usual causes associated with coronary artery disease, but can also be caused by prolonged exposure to bright light.[citation needed]
Diagnosis
In many cases, the diagnosis can be made based on the person's history of symptoms. In other cases, a physical examination and laboratory investigations are done to rule out more serious causes such as hypogonadism or prolactinoma.[6]
One of the first steps is to distinguish between physiological and psychological ED. Determining whether involuntary erections are present is important in eliminating the possibility of psychogenic causes for ED.[6] Obtaining full erections occasionally, such as nocturnal penile tumescence when asleep (that is, when the mind and psychological issues, if any, are less present), tends to suggest that the physical structures are functionally working.[37][38] Similarly, performance with manual stimulation, as well as any performance anxiety or acute situational ED, may indicate a psychogenic component to ED.[6]
Another factor leading to ED is diabetes mellitus, a well known cause of neuropathy).[6] ED is also related to generally poor physical health, poor dietary habits, obesity, and most specifically cardiovascular disease, such as coronary artery disease and peripheral vascular disease.[6] Screening for cardiovascular risk factors, such as smoking, dyslipidemia, hypertension, and alcoholism, is helpful.[6]
In some cases, the simple search for a previously undetected groin hernia can prove useful since it can affect sexual functions in men and is relatively easily curable.[27]
The current diagnostic and statistical manual of mental diseases (DSM-IV) lists ED.
Ultrasonography

Penile ultrasonography with doppler can be used to examine the erect penis. Most cases of ED of organic causes are related to changes in blood flow in the corpora cavernosa, represented by occlusive artery disease (in which less blood is allowed to enter the penis), most often of atherosclerotic origin, or due to failure of the veno-occlusive mechanism (in which too much blood circulates back out of the penis). Before the Doppler sonogram, the penis should be examined in B mode, in order to identify possible tumors, fibrotic plaques, calcifications, or hematomas, and to evaluate the appearance of the cavernous arteries, which can be tortuous or atheromatous.[39]
Erection can be induced by injecting 10–20 µg of prostaglandin E1, with evaluations of the arterial flow every five minutes for 25–30 min (see image). The use of prostaglandin E1 is contraindicated in patients with predisposition to priapism (e.g., those with sickle cell anemia), anatomical deformity of the penis, or penile implants. Phentolamine (2 mg) is often added. Visual and tactile stimulation produces better results. Some authors recommend the use of sildenafil by mouth to replace the injectable drugs in cases of contraindications, although the efficacy of such medication is controversial.[39]
Before the injection of the chosen drug, the flow pattern is monophasic, with low systolic velocities and an absence of diastolic flow. After injection, systolic and diastolic peak velocities should increase, decreasing progressively with vein occlusion and becoming negative when the penis becomes rigid (see image below). The reference values vary across studies, ranging from > 25 cm/s to > 35 cm/s. Values above 35 cm/s indicate the absence of arterial disease, values below 25 cm/s indicate arterial insufficiency, and values of 25–35 cm/s are indeterminate because they are less specific (see image below). The data obtained should be correlated with the degree of erection observed. If the peak systolic velocities are normal, the final diastolic velocities should be evaluated, those above 5 cm/s being associated with venogenic ED.[39]
-
Graphs representing the color Doppler spectrum of the flow pattern of the cavernous arteries during the erection phases. A: Single-phase flow with minimal or absent diastole when the penis is flaccid. B: Increased systolic flow and reverse diastole 25 min after injection of prostaglandin.[39]
-
Longitudinal, ventral ultrasound of the penis, with pulsed mode and color Doppler. Flow of the cavernous arteries at 5, 15, and 25 min after prostaglandin injection (A, B, and C, respectively). The cavernous artery flow remains below the expected levels (at least 25–35 cm/s), which indicates ED due to arterial insufficiency.[39]
Other workup
- Penile nerves function
- Tests such as the bulbocavernosus reflex test are used to ascertain whether there is enough nerve sensation in the penis. The physician squeezes the glans (head) of the penis, which immediately causes the anus to contract if nerve function is normal. A physician measures the latency between squeeze and contraction by observing the anal sphincter or by feeling it with a gloved finger in the anus.[40]
- Nocturnal penile tumescence (NPT)
- It is normal for a man to have five to six erections during sleep, especially during rapid eye movement (REM). Their absence may indicate a problem with nerve function or blood supply in the penis. There are two methods for measuring changes in penile rigidity and circumference during nocturnal erection: snap gauge and strain gauge. A significant proportion [give us the percentage] of men who have no sexual dysfunction nonetheless do not have regular nocturnal erections.[citation needed]
- Penile biothesiometry
- This test uses electromagnetic vibration to evaluate sensitivity and nerve function in the glans and shaft of the penis.[citation needed]
- Dynamic infusion cavernosometry (DICC)
- Technique in which fluid is pumped into the penis at a known rate and pressure. It gives a measurement of the vascular pressure in the corpus cavernosum during an erection.[citation needed]
- Corpus cavernosometry
- Cavernosography measurement of the vascular pressure in the corpus cavernosum. Saline is infused under pressure into the corpus cavernosum with a butterfly needle, and the flow rate needed to maintain an erection indicates the degree of venous leakage. The leaking veins responsible may be visualized by infusing a mixture of saline and x-ray contrast medium and performing a cavernosogram.[41] In Digital Subtraction Angiography (DSA), the images are acquired digitally.[citation needed]
- Magnetic resonance angiography (MRA)
- This is similar to magnetic resonance imaging. Magnetic resonance angiography uses magnetic fields and radio waves to provide detailed images of the blood vessels. The doctor may inject into the patient's bloodstream a contrast agent, which causes vascular tissues to stand out against other tissues, so that information about blood supply and vascular anomalies is easier to gather.[citation needed]
Treatment
Treatment depends on the underlying cause. In general, exercise, particularly of the aerobic type, is effective for preventing ED during midlife.[44]: 6, 18–19 Counseling can be used if the underlying cause is psychological, including how to lower stress or anxiety related to sex.[45] Medications by mouth and vacuum erection devices are first-line treatments,[44]: 20, 24 followed by injections of drugs into the penis, as well as penile implants.[44]: 25–26 Vascular reconstructive surgeries are beneficial in certain groups.[46] Treatments, other than surgery, do not fix the underlying physiological problem, but are used as needed before sex.[47]
Medications
The PDE5 inhibitors sildenafil (Viagra), vardenafil (Levitra) and tadalafil (Cialis) are prescription drugs which are taken by mouth.[44]: 20–21 As of 2018, sildenafil is available in the UK without a prescription.[48] Additionally, a cream combining alprostadil with the permeation enhancer DDAIP has been approved in Canada as a first line treatment for ED.[49] Penile injections, on the other hand, can involve one of the following medications: papaverine, phentolamine, and prostaglandin E1, also known as alprostadil.[44] In addition to injections, there is an alprostadil suppository that can be inserted into the urethra. Once inserted, an erection can begin within 10 minutes and last up to an hour.[45] Medications to treat ED may cause a side effect called priapism.[45]
Testosterone
Men with low levels of testosterone can experience ED. Taking testosterone may help maintain an erection.[50] Men with type 2 diabetes are twice as likely to have lower levels of testosterone, and are three times more likely to experience ED than non-diabetic men.[50]
Pumps
A vacuum erection device helps draw blood into the penis by applying negative pressure. This type of device is sometimes referred to as penis pump and may be used just prior to sexual intercourse. Several types of FDA approved vacuum therapy devices are available under prescription. When pharmacological methods fail, a purpose-designed external vacuum pump can be used to attain erection, with a separate compression ring fitted to the base of the penis to maintain it. These pumps should be distinguished from other penis pumps (supplied without compression rings) which, rather than being used for temporary treatment of impotence, are claimed to increase penis length if used frequently, or vibrate as an aid to masturbation. More drastically, inflatable or rigid penile implants may be fitted surgically.[51]
Shockwave therapy
Focused shockwave therapy is supported by tentative evidence.[52][53]
Surgery
Often, as a last resort, if other treatments have failed, the most common procedure is prosthetic implants which involves the insertion of artificial rods into the penis.[44]: 26 Some sources show that vascular reconstructive surgeries are viable options for some people.[46]
Alternative medicine
The Food and Drug Administration (FDA) does not recommend alternative therapies to treat sexual dysfunction.[54] Many products are advertised as "herbal viagra" or "natural" sexual enhancement products, but no clinical trials or scientific studies support the effectiveness of these products for the treatment of ED, and synthetic chemical compounds similar to sildenafil have been found as adulterants in many of these products.[55][56][57][58][59] The FDA has warned consumers that any sexual enhancement product that claims to work as well as prescription products is likely to contain such a contaminant.[60] A 2021 review indicated that ginseng had "only trivial effects on erectile function or satisfaction with intercourse compared to placebo".[61]
History

Attempts to treat ED date back well over 1,000 years. In the 8th century, men of Ancient Rome and Greece wore talismans of rooster and goat genitalia, believing these talismans would serve as an aphrodisiac and promote sexual function.[62] In the 13th century Albertus Magnus recommended ingesting roasted wolf penis as a remedy for impotence.[62]
During the late 16th and 17th centuries in France, male impotence was considered a crime, as well as legal grounds for a divorce. The practice, which involved inspection of the complainants by court experts, was declared obscene in 1677.[63][64]
The first successful vacuum erection device, or penis pump, was developed by Vincent Marie Mondat in the early 1800s.[62] A more advanced device, based on a bicycle pump, was developed by Geddings Osbon, a Pentecostal preacher, in the 1970s. In 1982, he received FDA approval to market the product as the ErecAid®.[65]
John R. Brinkley initiated a boom in male impotence cures in the U.S. in the 1920s and 1930s. His radio programs recommended expensive goat gland implants and "mercurochrome" injections as the path to restored male virility, including operations by surgeon Serge Voronoff.
Modern drug therapy for ED made a significant advance in 1983, when British physiologist Giles Brindley dropped his trousers and demonstrated to a shocked Urodynamics Society audience his papaverine-induced erection.[66] The drug Brindley injected into his penis was a non-specific vasodilator, an alpha-blocking agent, and the mechanism of action was clearly corporal smooth muscle relaxation. The effect that Brindley discovered established the fundamentals for the later development of specific, safe, and orally effective drug therapies.[67][68]
The current first-line treatment for ED, the oral PDE5 inhibitor, was introduced by Pfizer in 1999.[69]
Society and culture
Anthropology
Anthropological research presents ED not as a disorder but, as a normal, and sometimes even welcome sign of healthy aging. Wentzell's study of 250 Mexican men in their 50's and 60's found that “most simply did not see decreasing erectile function as a biological pathology”.[70] The men interviewed described the decrease in erectile function “as an aid for aging in socially appropriate ways”.[70] A common theme amongst the interviewees showed that respectable older men shifted their focus toward the domestic sphere into a “second stage of life”.[70] The Mexican men of this generation often pursued sex outside of marriage; decreasing erectile function acted as an aid to overcoming infidelity thus helping to attain the ideal “second stage” of life.[70] A 56-year-old about to retire from the public health service said he would now "dedicate myself to my wife, the house, gardening, caring for the grandchildren—the Mexican classic".[70] Wentzell found that treating ED as a pathology was antithetical to the social view these men held of themselves, and their purpose at this stage of their lives.
In the 20th and 21st centuries, anthropologists investigated how common treatments for ED are built upon assumptions of institutionalized social norms. In offering a range of clinical treatments to ‘correct’ a person's ability to produce an erection, biomedical institutions encourage the public to strive for prolonged sexual function. Anthropologists argue that a biomedical focus places emphasis on the biological processes of fixing the body thereby disregarding holistic ideals of health and aging.[71] By relying on a wholly medical approach, Western biomedicine can become blindsided by bodily dysfunctions which can be understood as appropriate functions of age, and not as a medical problem.[72] Anthropologists understand that a biosocial approach to ED considers a person's decision to undergo clinical treatment more likely a result of "society, political economy, history, and culture" than a matter of personal choice.[71] In rejecting biomedical treatment for ED, men can challenge common forms of medicalized social control by deviating from what is considered the normal approach to dysfunction.
Terminology
The Latin term impotentia coeundi describes simple inability to insert the penis into the vagina; it is now mostly replaced by more precise terms, such as erectile dysfunction (ED). The study of ED within medicine is covered by andrology, a sub-field within urology. Research indicates that ED is common, and it is suggested that approximately 40% of males experience symptoms compatible with ED, at least occasionally.[73] The condition is also on occasion called phallic impotence.[74] Its antonym, or opposite condition, is priapism.[75][76]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 "Definition & Facts for Erectile Dysfunction | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 1 February 2022. Retrieved 4 February 2022.
- ↑ 2.0 2.1 2.2 2.3 "Symptoms & Causes of Erectile Dysfunction | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 19 November 2021. Retrieved 4 February 2022.
- ↑ 3.0 3.1 "Diagnosis of Erectile Dysfunction | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 19 November 2021. Retrieved 4 February 2022.
- ↑ 4.0 4.1 4.2 4.3 4.4 "Treatment for Erectile Dysfunction | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 22 February 2021. Retrieved 4 February 2022.
- ↑ 5.0 5.1 5.2 5.3 5.4 Sooriyamoorthy, Thushanth; Leslie, Stephen W. (2022). "Erectile Dysfunction". StatPearls. StatPearls Publishing. Archived from the original on 21 January 2022. Retrieved 4 February 2022.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Chowdhury SH, Cozma AI, Chowdhury JH. Erectile Dysfunction. Essentials for the Canadian Medical Licensing Exam: Review and Prep for MCCQE Part I. 2nd edition. Wolters Kluwer. Hong Kong. 2017.
- ↑ Frederick LR, Cakir OO, Arora H, Helfand BT, McVary KT (October 2014). "Undertreatment of erectile dysfunction: claims analysis of 6.2 million patients". The Journal of Sexual Medicine. 11 (10): 2546–53. doi:10.1111/jsm.12647. PMID 25059314.
- ↑ "Can Your Diet Cause Erectile Dysfunction?". Cleveland Clinic. 2021-01-20. Archived from the original on 2022-01-04. Retrieved 2022-01-04.
- ↑ "Erectile Dysfunction & Heart Disease". Cleveland Clinic. Archived from the original on 2022-01-04. Retrieved 2022-01-04.
- ↑ Bauer, Scott R.; Breyer, Benjamin N.; Stampfer, Meir J.; Rimm, Eric B.; Giovannucci, Edward L.; Kenfield, Stacey A. (2020-11-02). "Association of Diet With Erectile Dysfunction Among Men in the Health Professionals Follow-up Study". JAMA Network Open. 3 (11): e2021701. doi:10.1001/jamanetworkopen.2020.21701. ISSN 2574-3805. PMC 7666422. PMID 33185675.
- ↑ Lu, Yi; Kang, Jiaqi; Li, Zhongjia; Wang, Xiao; Liu, Kang; Zhou, Kechong; Wang, Wei; Shen, Chen (2021-05-13). "The association between plant-based diet and erectile dysfunction in Chinese men". Basic and Clinical Andrology. 31 (1): 11. doi:10.1186/s12610-021-00129-5. ISSN 2051-4190. PMC 8117588. PMID 33980148.
- ↑ Russo, Giorgio Ivan; Broggi, Giuseppe; Cocci, Andrea; Capogrosso, Paolo; Falcone, Marco; Sokolakis, Ioannis; Gül, Murat; Caltabiano, Rosario; Di Mauro, Marina (2021-11-19). "Relationship between Dietary Patterns with Benign Prostatic Hyperplasia and Erectile Dysfunction: A Collaborative Review". Nutrients. 13 (11): 4148. doi:10.3390/nu13114148. ISSN 2072-6643. PMC 8618879. PMID 34836403.
- ↑ Delgado PL, Brannan SK, Mallinckrodt CH, Tran PV, McNamara RK, Wang F, Watkin JG, Detke MJ (2005). "Sexual functioning assessed in 4 double-blind placebo- and paroxetine-controlled trials of duloxetine for major depressive disorder". The Journal of Clinical Psychiatry. 66 (6): 686–92. doi:10.4088/JCP.v66n0603. PMID 15960560.
- ↑ 14.0 14.1 14.2 14.3 Cunningham GR, Rosen RC. Overview of male sexual dysfunction. In: UpToDate, Martin KA (Ed), UpToDate, Waltham, MA, 2018.
- ↑ Azadzoi, Kazem M.; Siroky, Mike B. (2006). "Neurogenic Sexual Dysfunction in Men and Women". Male Sexual Function: A Guide to Clinical Management. pp. 195–226. doi:10.1007/978-1-59745-155-0_9. ISBN 978-1-59745-155-0. S2CID 35058570.
- ↑ "Male Sexual Dysfunction Epidemiology". Erectile dysfunction. Armenian Health Network, Health.am. 2006. Archived from the original on 2021-02-22. Retrieved 2007-10-07.
- ↑ Lue TF (2006). "Causes of Erectile Dysfunction". Erectile dysfunction. Armenian Health Network, Health.am. Archived from the original on 2021-02-22. Retrieved 2007-10-07.
- ↑ 18.0 18.1 "Erectile Dysfunction Causes". Erectile Dysfunction. Healthcommunities.com. 1998. Archived from the original on 2007-10-09. Retrieved 2007-10-07.
- ↑ Gökçe Mİ, Yaman Ö (September 2017). "Erectile dysfunction in the elderly male". Turkish Journal of Urology. 43 (3): 247–251. doi:10.5152/tud.2017.70482. PMC 5562240. PMID 28861293.
- ↑ Meldrum DR, Morris MA, Gambone JC, Esposito K (December 2020). "Aging and erectile function". The Aging Male. 23 (5): 1115–1124. doi:10.1080/13685538.2019.1686756. PMID 31724458. S2CID 208018226.
- ↑ Papadopoulou E, Varouktsi A, Lazaridis A, Boutari C, Doumas M (July 2015). "Erectile dysfunction in chronic kidney disease: From pathophysiology to management". World Journal of Nephrology. 4 (3): 379–387. doi:10.5527/wjn.v4.i3.379. PMC 4491929. PMID 26167462.
- ↑ Peate I (2005). "The effects of smoking on the reproductive health of men". Br J Nurs. 14 (7): 362–66. doi:10.12968/bjon.2005.14.7.17939. PMID 15924009.
- ↑ Korenman SG (2004). "Epidemiology of erectile dysfunction". Endocrine. 23 (2–3): 87–91. doi:10.1385/ENDO:23:2-3:087. PMID 15146084. S2CID 29133230.
- ↑ Kendirci M, Nowfar S, Hellstrom WJ (2005). "The impact of vascular risk factors on erectile function". Drugs Today (Barc). 41 (1): 65–74. doi:10.1358/dot.2005.41.1.875779. PMID 15753970.
- ↑ Sansone A, Mollaioli D, Ciocca G, Limoncin E, Colonnello E, Vena W, Jannini EA (February 2021). "Addressing male sexual and reproductive health in the wake of COVID-19 outbreak". Journal of Endocrinological Investigation. 44 (2): 223–231. doi:10.1007/s40618-020-01350-1. PMC 7355084. PMID 32661947.
- ↑ Tian Y, Zhou LQ (February 2021). "Evaluating the impact of COVID-19 on male reproduction". Reproduction. 161 (2): R37–R44. doi:10.1530/rep-20-0523. PMID 33434886. S2CID 229455124.
- ↑ 27.0 27.1 Zieren J, Menenakos C, Paul M, Müller JM (2005). "Sexual function before and after mesh repair of inguinal hernia". Journal of Pharmaceutical and Biomedical Analysis. 12 (1): 35–38. doi:10.1111/j.1442-2042.2004.00983.x. PMID 15661052. S2CID 30209465.
- ↑ Sommer F, Goldstein I, Korda JB (July 2010). "Bicycle riding and erectile dysfunction: a review". The Journal of Sexual Medicine. 7 (7): 2346–58. doi:10.1111/j.1743-6109.2009.01664.x. PMID 20102446. S2CID 34409059.
- ↑ Huang V, Munarriz R, Goldstein I (September 2005). "Bicycle riding and erectile dysfunction: an increase in interest (and concern)". The Journal of Sexual Medicine. 2 (5): 596–604. doi:10.1111/j.1743-6109.2005.00099.x. PMID 16422816.
- ↑ Robinson M, Wilson G (July 11, 2011). "Porn-Induced Sexual Dysfunction: A Growing Problem". Psychology Today.
- ↑ Whelan, Georgina; Brown, Jac (September 2021). "Pornography Addiction: An Exploration of the Association Between Use, Perceived Addiction, Erectile Dysfunction, Premature (Early) Ejaculation, and Sexual Satisfaction in Males Aged 18-44 Years". The Journal of Sexual Medicine. 18 (9): 1582–1591. doi:10.1016/j.jsxm.2021.06.014. ISSN 1743-6109. PMID 34400111. Archived from the original on 2021-12-30. Retrieved 2022-01-30.
There was no evidence for an association between internet pornography use with erectile dysfunction, premature ejaculation, or sexual satisfaction. However, there were small to moderate positive correlations between self-perceived internet pornography addiction and erectile dysfunction, premature ejaculation or sexual dissatisfaction.
- ↑ Grubbs, Joshua B.; Gola, Mateusz (January 2019). "Is Pornography Use Related to Erectile Functioning? Results From Cross-Sectional and Latent Growth Curve Analyses". The Journal of Sexual Medicine. 16 (1): 111–125. doi:10.1016/j.jsxm.2018.11.004. ISSN 1743-6109. PMID 30621919. S2CID 58592884. Archived from the original on 30 December 2021. Retrieved 30 December 2021.
there was evidence of a positive, cross-sectional association between self-reported problematic use and ED, but no consistent association between mere use itself and ED.
- ↑ Landripet I, Štulhofer A (May 2015). "Is Pornography Use Associated with Sexual Difficulties and Dysfunctions among Younger Heterosexual Men?". The Journal of Sexual Medicine. 12 (5): 1136–1139. doi:10.1111/jsm.12853. PMID 25816904.
- ↑ Van Boom D (1 December 2020). "Porn addiction is ruining lives, but scientists aren't convinced it's real". CNET. Archived from the original on 3 November 2021. Retrieved 2 October 2021.
- ↑ Jacobs T, Geysemans B, Van Hal G, Glazemakers I, Fog-Poulsen K, Vermandel A, et al. (September 2021). "Is online pornography consumption linked to offline sexual dysfunction in young men? A multivariate analysis based on an international web-based survey". JMIR Public Health and Surveillance. JMIR Publications Inc. 7 (10): e32542. doi:10.2196/32542. PMC 8569536. PMID 34534092.
Conclusions: This prevalence of ED in young men is alarmingly high and the results of presented study suggest a significant association with PPC.
- ↑ Shamloul R, Bella AJ (2014-03-01). Erectile Dysfunction. Biota Publishing. pp. 6–. ISBN 978-1-61504-653-9. Archived from the original on 2021-02-22. Retrieved 2022-01-30.
- ↑ Levine LA, Lenting EL (1995). "Use of nocturnal penile tumescence and rigidity in the evaluation of male erectile dysfunction". Urol. Clin. North Am. 22 (4): 775–88. PMID 7483128.
- ↑ "Tests for Erection Problems". WebMD, Inc. Archived from the original on 2018-03-08. Retrieved 2007-03-03.
- ↑ 39.0 39.1 39.2 39.3 39.4 39.5 Originally copied from:
Fernandes MA, de Souza LR, Cartafina LP (2018). "Ultrasound evaluation of the penis". Radiologia Brasileira. 51 (4): 257–261. doi:10.1590/0100-3984.2016.0152. PMC 6124582. PMID 30202130.
CC-BY license - ↑ Vodušek DB, Deletis V (January 2002). "Intraoperative Neurophysiological Monitoring of the Sacral Nervous System". Neurophysiology in Neurosurgery, A Modern Intraoperative Approach: 153–165. doi:10.1016/B978-012209036-3/50011-1. ISBN 9780122090363.
- ↑ Dawson C, Whitfield H (April 1996). "ABC of urology. Subfertility and male sexual dysfunction". BMJ. 312 (7035): 902–05. doi:10.1136/bmj.312.7035.902. PMC 2350600. PMID 8611887.
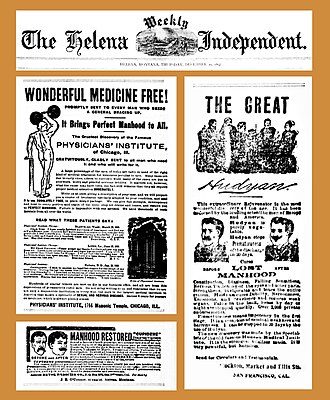
- ↑ 42.0 42.1 "Wonderful Medicine Free / Manhood Restored / The Great Hudyan". The Helena Weekly Independent. Helena, Montana, U.S. December 30, 1897. pp. 7–8. Archived from the original on February 3, 2022. Retrieved January 30, 2022. (and page 8 Archived 2022-02-03 at the Wayback Machine)
- ↑ "Phony Cures for Erectile Dysfunction". ftc.gov. U.S. Federal Trade Commission. Archived from the original on April 30, 2020.
- ↑ 44.0 44.1 44.2 44.3 44.4 44.5 Wespes E (chair), et al. Guidelines on Male Sexual Dysfunction: Erectile dysfunction and premature ejaculation. European Association of Urology 2013
- ↑ 45.0 45.1 45.2 "Treatment for erectile dysfunction |". US National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 2021-02-22. Retrieved 2019-08-04.
- ↑ 46.0 46.1 "Encyclopedia of Reproduction - 2nd Edition". www.elsevier.com. Archived from the original on 2021-02-22. Retrieved 2019-01-17.
- ↑ "What is Erectile Dysfunction? - Urology Care Foundation". www.urologyhealth.org. Archived from the original on 2019-08-05. Retrieved 2019-08-05.
- ↑ "Viagra can be sold over the counter". BBC News. 28 November 2017. Archived from the original on 22 February 2021. Retrieved 5 April 2018.
- ↑ Bujdos B. "New Topical Erectile Dysfunction Drug Vitaros Approved in Canada; Approved Topical Drug Testim Proves Helpful for Erectile Dysfunction". Archived from the original on 13 May 2011. Retrieved 15 April 2011.
- ↑ 50.0 50.1 "Men and diabetes". US Centers for Disease Control and Prevention. 2019-04-01. Archived from the original on 2021-02-22. Retrieved 2019-08-04.
- ↑ "Erectile Dysfunction". The Lecturio Medical Concept Library. Archived from the original on 21 July 2021. Retrieved 21 July 2021.
- ↑ Man L, Li G (September 2018). "Low-intensity Extracorporeal Shock Wave Therapy for Erectile Dysfunction: A Systematic Review and Meta-analysis". Urology. 119: 97–103. doi:10.1016/j.urology.2017.09.011. PMID 28962876. S2CID 7048621.
- ↑ Clavijo RI, Kohn TP, Kohn JR, Ramasamy R (January 2017). "Effects of Low-Intensity Extracorporeal Shockwave Therapy on Erectile Dysfunction: A Systematic Review and Meta-Analysis". The Journal of Sexual Medicine. 14 (1): 27–35. doi:10.1016/j.jsxm.2016.11.001. PMID 27986492.
- ↑ "Dangers of Sexual Enhancement Supplements". Medscape. Archived from the original on 2021-02-22. Retrieved 2022-01-30.
- ↑ Gryniewicz CM, Reepmeyer JC, Kauffman JF, Buhse LF (2009). "Detection of undeclared erectile dysfunction drugs and analogues in dietary supplements by ion mobility spectrometry". Journal of Pharmaceutical and Biomedical Analysis. 49 (3): 601–06. doi:10.1016/j.jpba.2008.12.002. PMID 19150190.
- ↑ Choi DM, Park S, Yoon TH, Jeong HK, Pyo JS, Park J, Kim D, Kwon SW (2008). "Determination of analogs of sildenafil and vardenafil in foods by column liquid chromatography with a photodiode array detector, mass spectrometry, and nuclear magnetic resonance spectrometry". Journal of AOAC International. 91 (3): 580–88. doi:10.1093/jaoac/91.3.580. PMID 18567304.
- ↑ Reepmeyer JC, Woodruff JT (2007). "Use of liquid chromatography-mass spectrometry and a chemical cleavage reaction for the structure elucidation of a new sildenafil analogue detected as an adulterant in an herbal dietary supplement". Journal of Pharmaceutical and Biomedical Analysis. 44 (4): 887–93. doi:10.1016/j.jpba.2007.04.011. PMID 17532168. Archived from the original on 2020-01-28. Retrieved 2022-01-30.
- ↑ Reepmeyer JC, Woodruff JT, d'Avignon DA (2007). "Structure elucidation of a novel analogue of sildenafil detected as an adulterant in an herbal dietary supplement". Journal of Pharmaceutical and Biomedical Analysis. 43 (5): 1615–21. doi:10.1016/j.jpba.2006.11.037. PMID 17207601. Archived from the original on 2021-10-09. Retrieved 2022-01-30.
- ↑ Enforcement Report for June 30, 2010 Archived June 25, 2016, at the Wayback Machine, United States Food and Drug Administration
- ↑ Hidden Risks of Erectile Dysfunction "Treatments" Sold Online Archived 2019-04-23 at the Wayback Machine, United States Food and Drug Administration, February 21, 2009
- ↑ Lee HW, Lee MS, Kim TH, Alraek T, Zaslawski C, Kim JW, Moon DG (April 2021). "Ginseng for erectile dysfunction". The Cochrane Database of Systematic Reviews. 2021 (4): CD012654. doi:10.1002/14651858.cd012654.pub2. PMC 8094213. PMID 33871063.
- ↑ 62.0 62.1 62.2 McLaren A (2007). Impotence: A Cultural History. University of Chicago Press. ISBN 978-0226500768.
- ↑ Roach M (2009). Bonk: The Curious Coupling of Science and Sex. New York: W.W. Norton & Co. pp. 149–52. ISBN 9780393334791.
- ↑ Darmon P (1985). Trial by Impotence: Virility and Marriage in Pre-Revolutionary France. Vintage/Ebury. ISBN 978-0701129156.
- ↑ Hoyland K, Vasdev N, Adshead J (2013). "The use of vacuum erection devices in erectile dysfunction after radical prostatectomy". Reviews in Urology. 15 (2): 67–71. PMC 3784970. PMID 24082845.
- ↑ Klotz L (November 2005). "How (not) to communicate new scientific information: a memoir of the famous Brindley lecture". BJU International. 96 (7): 956–7. doi:10.1111/j.1464-410X.2005.05797.x. PMID 16225508. S2CID 38931340.
- ↑ Brindley GS (October 1983). "Cavernosal alpha-blockade: a new technique for investigating and treating erectile impotence". The British Journal of Psychiatry. 143 (4): 332–7. doi:10.1192/bjp.143.4.332. PMID 6626852.
- ↑ Helgason AR, Adolfsson J, Dickman P, Arver S, Fredrikson M, Göthberg M, Steineck G (July 1996). "Sexual desire, erection, orgasm and ejaculatory functions and their importance to elderly Swedish men: a population-based study" (PDF). Age and Ageing. 25 (4): 285–91. doi:10.1093/ageing/25.4.285. PMID 8831873. Archived (PDF) from the original on 2022-01-21. Retrieved 2022-01-30.
- ↑ Valiquette L (February 2003). "A historical review of erectile dysfunction". The Canadian Journal of Urology. 10 (Suppl 1): 7–11. PMID 12625844. Archived from the original on 2022-02-03. Retrieved 2022-01-30.
- ↑ 70.0 70.1 70.2 70.3 70.4 Wentzell E, Labuski C (2020). "Role of Medical Anthropology in Understanding Cultural Differences in Sexuality". Cultural Differences and the Practice of Sexual Medicine. Trends in Andrology and Sexual Medicine. Cham: Springer International Publishing. pp. 23–35. doi:10.1007/978-3-030-36222-5_2. ISBN 978-3-030-36221-8. S2CID 214042890. Archived from the original on 3 February 2022. Retrieved 28 August 2021.
- ↑ 71.0 71.1 Farmer P, Kleinman A, Kim J, Basilico M (2013). Reimagining Global Health: An Introduction. Berkeley: University of California Press. pp. 17–20. ISBN 978-0-520-27197-5. Retrieved 28 August 2021.[permanent dead link]
- ↑ Wentzell E, Salmerón J (2009). "Prevalence of erectile dysfunction and its treatment in a Mexican population: distinguishing between erectile function change and dysfunction". Journal of Men's Health. 6 (1): 56–62. doi:10.1016/j.jomh.2008.09.009.
- ↑ Schouten BW, Bohnen AM, Groeneveld FP, Dohle GR, Thomas S, Bosch JL (July 2010). "Erectile dysfunction in the community: trends over time in incidence, prevalence, GP consultation and medication use – the Krimpen study: trends in ED". J Sex Med. 7 (7): 2547–53. doi:10.1111/j.1743-6109.2010.01849.x. PMID 20497307.
- ↑ Kahane C (20 September 2011). "Bad Timing: The Problematics of Intimacy in On Chesil Beach". PsyArt. Archived from the original on 19 October 2021. Retrieved 30 January 2022.
- ↑ Allgeier A (1995). Sexual interactions. D.C. Heath. p. 243.
- ↑ Grimes J (2013). Sexually Transmitted Disease: An Encyclopedia of Diseases, Prevention, Treatment and Issues. p. 496.
External links
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- CS1: Julian–Gregorian uncertainty
- Webarchive template wayback links
- All articles with dead external links
- Articles with dead external links from March 2022
- Articles with invalid date parameter in template
- Articles with permanently dead external links
- All articles with unsourced statements
- Articles with unsourced statements from January 2020
- Articles with unsourced statements from March 2021
- Articles with unsourced statements from December 2020
- Articles with hatnote templates targeting a nonexistent page
- Articles with Curlie links
- Portal templates with all redlinked portals
- Portal-inline template with redlinked portals
- Non-sexuality
- Penis disorders
- Sexual dysfunctions
- Penile erection
- Men's health
- RTT
![Graphs representing the color Doppler spectrum of the flow pattern of the cavernous arteries during the erection phases. A: Single-phase flow with minimal or absent diastole when the penis is flaccid. B: Increased systolic flow and reverse diastole 25 min after injection of prostaglandin.[39]](https://upload.wikimedia.org/wikipedia/commons/thumb/e/e0/Doppler_ultrasonography_of_cavernous_artery_flow_in_flaccid_and_erected_state.jpg/569px-Doppler_ultrasonography_of_cavernous_artery_flow_in_flaccid_and_erected_state.jpg)
![Longitudinal, ventral ultrasound of the penis, with pulsed mode and color Doppler. Flow of the cavernous arteries at 5, 15, and 25 min after prostaglandin injection (A, B, and C, respectively). The cavernous artery flow remains below the expected levels (at least 25–35 cm/s), which indicates ED due to arterial insufficiency.[39]](https://upload.wikimedia.org/wikipedia/commons/thumb/6/6b/Doppler_ultrasonography_of_cavernous_arterial_insufficiency.jpg/401px-Doppler_ultrasonography_of_cavernous_arterial_insufficiency.jpg)