Obesity
| Obesity | |
|---|---|
 | |
| Silhouettes and waist circumferences representing optimal, overweight, and obese | |
| Specialty | Endocrinology |
| Symptoms | Increased fat[1] |
| Complications | Cardiovascular diseases, type 2 diabetes, obstructive sleep apnea, certain types of cancer, osteoarthritis, depression[2][3] |
| Causes | Excessive food, lack of exercise, genetics[1][4] |
| Diagnostic method | BMI > 30 kg/m2[1] |
| Prevention | Societal changes, personal choices[1] |
| Treatment | Diet, exercise, medications, surgery[1][5][6] |
| Medication | GLP-1-RAs, orlistat, naltrexone/bupropion[5] |
| Prognosis | Reduced life expectancy[2] |
| Frequency | >1 billion / 12.5% (2022)[7] |
Obesity is a medical condition in which excess body fat has accumulated to an extent that it may have a negative effect on health.[1] People are generally considered obese when their body mass index (BMI), a measurement obtained by dividing a person's weight by the square of the person's height, is over 30 kg/m2; the range 25–30 kg/m2 is defined as overweight.[1] Some East Asian countries use lower values.[8] Obesity increases the likelihood of various diseases and conditions, particularly cardiovascular diseases, type 2 diabetes, obstructive sleep apnea, certain types of cancer, osteoarthritis, and depression.[2][3]
Obesity is most commonly caused by a combination of excessive food intake, lack of physical activity, and genetic susceptibility.[1][4] A few cases are caused primarily by genes, endocrine disorders, medications, or mental disorder.[9] The view that obese people eat little yet gain weight due to a slow metabolism is not medically supported.[10] On average, obese people have a greater energy expenditure than their normal counterparts due to the energy required to maintain an increased body mass.[10][11]
Obesity is mostly preventable through a combination of social changes and personal choices.[1] Changes to diet and exercising are the main treatments.[2] Diet quality can be improved by reducing the energy-dense foods, such as those high in fat or sugars, and by increasing dietary fiber.[1] Medications, such as GLP-1-RAs, orlistat, or naltrexone/bupropion, may be used with lifestyle changes.[5] If diet, exercise, and medication are not effective, a gastric balloon or surgery may be performed to reduce stomach volume or length of the intestines, leading to feeling full earlier or a reduced ability to absorb nutrients from food.[6][12]
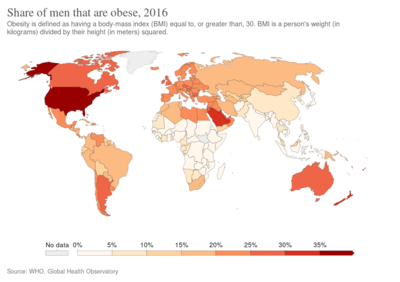
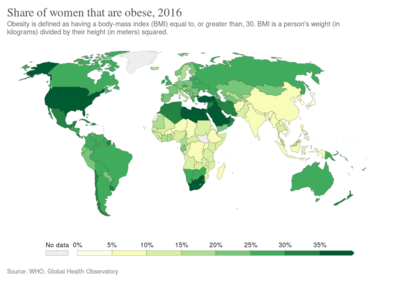
Obesity is a leading preventable cause of death worldwide, with increasing rates in adults and children.[1][13] In 2015, 600 million adults (12%) and 100 million children were obese in 195 countries.[14] Obesity is more common in women than men.[1] Authorities view it as one of the most serious public health problems of the 21st century.[15] Obesity is stigmatized in much of the modern world (particularly in the Western world), though it was seen as a symbol of wealth and fertility at other times in history and still is in some parts of the world.[2][16] In 2013, several medical societies, including the American Medical Association and the American Heart Association, classified obesity as a disease.[17][18][19]
Classification
| BMI (kg/m2) | Classification[20] | |
|---|---|---|
| from | up to | |
| 18.5 | underweight | |
| 18.5 | 25.0 | normal weight |
| 25.0 | 30.0 | overweight |
| 30.0 | 35.0 | class I obesity |
| 35.0 | 40.0 | class II obesity |
| 40.0 | class III obesity | |

Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health.[21] It is defined by body mass index (BMI) and further evaluated in terms of fat distribution via the waist–hip ratio and total cardiovascular risk factors.[22][23] BMI is closely related to both percentage body fat and total body fat.[24] In children, a healthy weight varies with age and sex. Obesity in children and adolescents is defined not as an absolute number but in relation to a historical normal group, such that obesity is a BMI greater than the 95th percentile.[25] The reference data on which these percentiles were based date from 1963 to 1994, and thus have not been affected by the recent increases in weight.[26] BMI is defined as the subject's weight divided by the square of their height and is calculated as follows.
- ,
- where m and h are the subject's weight and height respectively.
BMI is usually expressed in kilograms of weight per metre squared of height. To convert from pounds per inch squared multiply by 703 (kg/m2)/(lb/sq in).[27]
The most commonly used definitions, established by the World Health Organization (WHO) in 1997 and published in 2000, provide the values listed in the table.[28][29]
Some modifications to the WHO definitions have been made by particular organizations.[30] The surgical literature breaks down class II and III obesity into further categories whose exact values are still disputed.[31]
- Any BMI ≥ 35 or 40 kg/m2 is severe obesity.
- A BMI of ≥ 35 kg/m2 and experiencing obesity-related health conditions or ≥40–44.9 kg/m2 is morbid obesity.
- A BMI of ≥ 45 or 50 kg/m2 is super obesity.
As Asian populations develop negative health consequences at a lower BMI than Caucasians, some nations have redefined obesity; Japan has defined obesity as any BMI greater than 25 kg/m2[8] while China uses a BMI of greater than 28 kg/m2.[30]
Effects on health
Excessive body weight is associated with various diseases and conditions, particularly cardiovascular diseases, diabetes mellitus type 2, obstructive sleep apnea, certain types of cancer, osteoarthritis,[2] and asthma.[2][32] As a result, obesity has been found to reduce life expectancy.[2]
Mortality
| Relative risk of death over 10 years in white people who have never smoked in the United States by BMI. The BMI range 22.5 to 24.9 is set as the reference.[33] | |
Obesity is one of the leading preventable causes of death worldwide.[34][35][36] A number of reviews have found that mortality risk is lowest at a BMI of 20–25 kg/m2[37][38][39] in non-smokers and at 24–27 kg/m2 in current smokers, with risk increasing along with changes in either direction.[40][41] This appears to apply in at least four continents.[39] In contrast, a 2013 review found that grade 1 obesity (BMI 30–35) was not associated with higher mortality than normal weight, and that overweight (BMI 25–30) was associated with "lower" mortality than was normal weight (BMI 18.5–25).[42] Other evidence suggests that the association of BMI and waist circumference with mortality is U- or J-shaped, while the association between waist-to-hip ratio and waist-to-height ratio with mortality is more positive.[43] In Asians the risk of negative health effects begins to increase between 22–25 kg/m2.[44] A BMI above 32 kg/m2 has been associated with a doubled mortality rate among women over a 16-year period.[45] In the United States, obesity is estimated to cause 111,909 to 365,000 deaths per year,[2][36] while 1 million (7.7%) of deaths in Europe are attributed to excess weight.[46][47] On average, obesity reduces life expectancy by six to seven years,[2][48] a BMI of 30–35 kg/m2 reduces life expectancy by two to four years,[38] while severe obesity (BMI > 40 kg/m2) reduces life expectancy by ten years.[38] Sumo wrestlers have a shorter life expectancy at 60 to 65, being particularly low in those with a higher BMI compared to the average Japanese male of 81.[49][50]
Morbidity
Obesity increases the risk of many physical and mental conditions. These comorbidities are most commonly shown in metabolic syndrome,[2] a combination of medical disorders which includes: diabetes mellitus type 2, high blood pressure, high blood cholesterol, and high triglyceride levels.[51]
Complications are either directly caused by obesity or indirectly related through mechanisms sharing a common cause such as a poor diet or a sedentary lifestyle. The strength of the link between obesity and specific conditions varies. One of the strongest is the link with type 2 diabetes. Excess body fat underlies 64% of cases of diabetes in men and 77% of cases in women.[52]
Health consequences fall into two broad categories: those attributable to the effects of increased fat mass (such as osteoarthritis, obstructive sleep apnea, social stigmatization) and those due to the increased number of fat cells (diabetes, cancer, cardiovascular disease, non-alcoholic fatty liver disease).[2][53] Increases in body fat alter the body's response to insulin, potentially leading to insulin resistance. Increased fat also creates a proinflammatory state,[54][55] and a prothrombotic state.[53][56]
Obesity increases the risk of developing serious illness from coronavirus disease 2019.[57]
| Medical field | Condition | Medical field | Condition |
|---|---|---|---|
| Cardiology | Dermatology | ||
| Endocrinology and Reproductive medicine | Gastroenterology | ||
| Neurology | Oncology[70] | ||
| Psychiatry |
|
Respirology |
|
| Rheumatology and Orthopedics |
|
Urology and Nephrology |
Survival paradox
Although the negative health consequences of obesity in the general population are well supported by the available evidence, health outcomes in certain subgroups seem to be improved at an increased BMI, a phenomenon known as the obesity survival paradox.[79] The paradox was first described in 1999 in overweight and obese people undergoing hemodialysis,[79] and has subsequently been found in those with heart failure and peripheral artery disease (PAD).[80]
In people with heart failure, those with a BMI between 30.0 and 34.9 had lower mortality than those with a normal weight. This has been attributed to the fact that people often lose weight as they become progressively more ill.[81] Similar findings have been made in other types of heart disease. People with class I obesity and heart disease do not have greater rates of further heart problems than people of normal weight who also have heart disease. In people with greater degrees of obesity, however, the risk of further cardiovascular events is increased.[82][83] Even after cardiac bypass surgery, no increase in mortality is seen in the overweight and obese.[84] One study found that the improved survival could be explained by the more aggressive treatment obese people receive after a cardiac event.[85] Another study found that if one takes into account chronic obstructive pulmonary disease (COPD) in those with PAD, the benefit of obesity no longer exists.[80]
Causes
At an individual level, a combination of excessive food energy intake and a lack of physical activity is thought to explain most cases of obesity.[86] A limited number of cases are due primarily to genetics, medical reasons, or psychiatric illness.[9] In contrast, increasing rates of obesity at a societal level are felt to be due to an easily accessible and palatable diet,[87] increased reliance on cars, and mechanized manufacturing.[88][89]
A 2006 review identified ten other possible contributors to the recent increase of obesity: (1) insufficient sleep, (2) endocrine disruptors (environmental pollutants that interfere with lipid metabolism), (3) decreased variability in ambient temperature, (4) decreased rates of smoking, because smoking suppresses appetite, (5) increased use of medications that can cause weight gain (e.g., atypical antipsychotics), (6) proportional increases in ethnic and age groups that tend to be heavier, (7) pregnancy at a later age (which may cause susceptibility to obesity in children), (8) epigenetic risk factors passed on generationally, (9) natural selection for higher BMI, and (10) assortative mating leading to increased concentration of obesity risk factors (this would increase the number of obese people by increasing population variance in weight).[90] According to the Endocrine Society, there is "growing evidence suggesting that obesity is a disorder of the energy homeostasis system, rather than simply arising from the passive accumulation of excess weight".[91]
Diet
|
no data
<1,600 (<6,700)
1,600–1,800 (6,700–7,500)
1,800–2,000 (7,500–8,400)
2,000–2,200 (8,400–9,200)
2,200–2,400 (9,200–10,000)
2,400–2,600 (10,000–10,900)
|
2,600–2,800 (10,900–11,700)
2,800–3,000 (11,700–12,600)
3,000–3,200 (12,600–13,400)
3,200–3,400 (13,400–14,200)
3,400–3,600 (14,200–15,100)
>3,600 (>15,100)
|

A 2016 review supported excess food as the primary factor.[93][94] Dietary energy supply per capita varies markedly between different regions and countries. It has also changed significantly over time.[92] From the early 1970s to the late 1990s the average food energy available per person per day (the amount of food bought) increased in all parts of the world except Eastern Europe. The United States had the highest availability with 3,654 calories (15,290 kJ) per person in 1996.[92] This increased further in 2003 to 3,754 calories (15,710 kJ).[92] During the late 1990s Europeans had 3,394 calories (14,200 kJ) per person, in the developing areas of Asia there were 2,648 calories (11,080 kJ) per person, and in sub-Saharan Africa people had 2,176 calories (9,100 kJ) per person.[92][95] Total food energy consumption has been found to be related to obesity.[96]
The widespread availability of nutritional guidelines[97] has done little to address the problems of overeating and poor dietary choice.[98] From 1971 to 2000, obesity rates in the United States increased from 14.5% to 30.9%.[99] During the same period, an increase occurred in the average amount of food energy consumed. For women, the average increase was 335 calories (1,400 kJ) per day (1,542 calories (6,450 kJ) in 1971 and 1,877 calories (7,850 kJ) in 2004), while for men the average increase was 168 calories (700 kJ) per day (2,450 calories (10,300 kJ) in 1971 and 2,618 calories (10,950 kJ) in 2004). Most of this extra food energy came from an increase in carbohydrate consumption rather than fat consumption.[100] The primary sources of these extra carbohydrates are sweetened beverages, which now account for almost 25 percent of daily food energy in young adults in America,[101] and potato chips.[102] Consumption of sweetened drinks such as soft drinks, fruit drinks, iced tea, and energy and vitamin water drinks is believed to be contributing to the rising rates of obesity[103][104] and to an increased risk of metabolic syndrome and type 2 diabetes.[105] Vitamin D deficiency is related to diseases associated with obesity.[106]
As societies become increasingly reliant on energy-dense, big-portions, and fast-food meals, the association between fast-food consumption and obesity becomes more concerning.[107] In the United States consumption of fast-food meals tripled and food energy intake from these meals quadrupled between 1977 and 1995.[108]
Agricultural policy and techniques in the United States and Europe have led to lower food prices. In the United States, subsidization of corn, soy, wheat, and rice through the U.S. farm bill has made the main sources of processed food cheap compared to fruits and vegetables.[109] Calorie count laws and nutrition facts labels attempt to steer people toward making healthier food choices, including awareness of how much food energy is being consumed.
Obese people consistently under-report their food consumption as compared to people of normal weight.[110] This is supported both by tests of people carried out in a calorimeter room[111] and by direct observation.
Sedentary lifestyle
A sedentary lifestyle plays a significant role in obesity.[112] Worldwide there has been a large shift towards less physically demanding work,[113][114][115] and currently at least 30% of the world's population gets insufficient exercise.[114] This is primarily due to increasing use of mechanized transportation and a greater prevalence of labor-saving technology in the home.[113][114][115] In children, there appear to be declines in levels of physical activity due to less walking and physical education.[116] World trends in active leisure time physical activity are less clear. The World Health Organization indicates people worldwide are taking up less active recreational pursuits, while a study from Finland[117] found an increase and a study from the United States found leisure-time physical activity has not changed significantly.[118] A 2011 review of physical activity in children found that it may not be a significant contributor.[119]
In both children and adults, there is an association between television viewing time and the risk of obesity.[120][121][122] A review found 63 of 73 studies (86%) showed an increased rate of childhood obesity with increased media exposure, with rates increasing proportionally to time spent watching television.[123]
Genetics

Like many other medical conditions, obesity is the result of an interplay between genetic and environmental factors.[125] Polymorphisms in various genes controlling appetite and metabolism predispose to obesity when sufficient food energy is present. As of 2006, more than 41 of these sites on the human genome have been linked to the development of obesity when a favorable environment is present.[126] People with two copies of the FTO gene (fat mass and obesity associated gene) have been found on average to weigh 3–4 kg more and have a 1.67-fold greater risk of obesity compared with those without the risk allele.[127] The differences in BMI between people that are due to genetics varies depending on the population examined from 6% to 85%.[128]
Obesity is a major feature in several syndromes, such as Prader–Willi syndrome, Bardet–Biedl syndrome, Cohen syndrome, and MOMO syndrome. (The term "non-syndromic obesity" is sometimes used to exclude these conditions.)[129] In people with early-onset severe obesity (defined by an onset before 10 years of age and body mass index over three standard deviations above normal), 7% harbor a single point DNA mutation.[130]
Studies that have focused on inheritance patterns rather than on specific genes have found that 80% of the offspring of two obese parents were also obese, in contrast to less than 10% of the offspring of two parents who were of normal weight.[131] Different people exposed to the same environment have different risks of obesity due to their underlying genetics.[132]
The thrifty gene hypothesis postulates that, due to dietary scarcity during human evolution, people are prone to obesity. Their ability to take advantage of rare periods of abundance by storing energy as fat would be advantageous during times of varying food availability, and individuals with greater adipose reserves would be more likely to survive famine. This tendency to store fat, however, would be maladaptive in societies with stable food supplies.[133] This theory has received various criticisms, and other evolutionarily-based theories such as the drifty gene hypothesis and the thrifty phenotype hypothesis have also been proposed.[134][135]
Other illnesses
Certain physical and mental illnesses and the pharmaceutical substances used to treat them can increase risk of obesity. Medical illnesses that increase obesity risk include several rare genetic syndromes (listed above) as well as some congenital or acquired conditions: hypothyroidism, Cushing's syndrome, growth hormone deficiency,[136] and some eating disorders such as binge eating disorder and night eating syndrome.[2] However, obesity is not regarded as a psychiatric disorder, and therefore is not listed in the DSM-IVR as a psychiatric illness.[137] The risk of overweight and obesity is higher in patients with psychiatric disorders than in persons without psychiatric disorders.[138]
Certain medications may cause weight gain or changes in body composition; these include insulin, sulfonylureas, thiazolidinediones, atypical antipsychotics, antidepressants, steroids, certain anticonvulsants (phenytoin and valproate), pizotifen, and some forms of hormonal contraception.[2]
Social determinants


While genetic influences are important to understanding obesity, they cannot explain the current dramatic increase seen within specific countries or globally.[139] Though it is accepted that energy consumption in excess of energy expenditure leads to obesity on an individual basis, the cause of the shifts in these two factors on the societal scale is much debated. There are a number of theories as to the cause but most believe it is a combination of various factors.
The correlation between social class and BMI varies globally. A review in 1989 found that in developed countries women of a high social class were less likely to be obese. No significant differences were seen among men of different social classes. In the developing world, women, men, and children from high social classes had greater rates of obesity.[140] An update of this review carried out in 2007 found the same relationships, but they were weaker. The decrease in strength of correlation was felt to be due to the effects of globalization.[141] Among developed countries, levels of adult obesity, and percentage of teenage children who are overweight, are correlated with income inequality. A similar relationship is seen among US states: more adults, even in higher social classes, are obese in more unequal states.[142]
Many explanations have been put forth for associations between BMI and social class. It is thought that in developed countries, the wealthy are able to afford more nutritious food, they are under greater social pressure to remain slim, and have more opportunities along with greater expectations for physical fitness. In undeveloped countries the ability to afford food, high energy expenditure with physical labor, and cultural values favoring a larger body size are believed to contribute to the observed patterns.[141] Attitudes toward body weight held by people in one's life may also play a role in obesity. A correlation in BMI changes over time has been found among friends, siblings, and spouses.[143] Stress and perceived low social status appear to increase risk of obesity.[142][144][145]
Smoking has a significant effect on an individual's weight. Those who quit smoking gain an average of 4.4 kilograms (9.7 lb) for men and 5.0 kilograms (11.0 lb) for women over ten years.[146] However, changing rates of smoking have had little effect on the overall rates of obesity.[147]
In the United States the number of children a person has is related to their risk of obesity. A woman's risk increases by 7% per child, while a man's risk increases by 4% per child.[148] This could be partly explained by the fact that having dependent children decreases physical activity in Western parents.[149]
In the developing world urbanization is playing a role in increasing rate of obesity. In China overall rates of obesity are below 5%; however, in some cities rates of obesity are greater than 20%.[150]
Malnutrition in early life is believed to play a role in the rising rates of obesity in the developing world.[151] Endocrine changes that occur during periods of malnutrition may promote the storage of fat once more food energy becomes available.[151]
Consistent with cognitive epidemiological data, numerous studies confirm that obesity is associated with cognitive deficits.[152][153]
Whether obesity causes cognitive deficits, or vice versa is unclear at present.
Gut bacteria
The study of the effect of infectious agents on metabolism is still in its early stages. Gut flora has been shown to differ between lean and obese people. There is an indication that gut flora can affect the metabolic potential. This apparent alteration is believed to confer a greater capacity to harvest energy contributing to obesity. Whether these differences are the direct cause or the result of obesity has yet to be determined unequivocally.[154] The use of antibiotics among children has also been associated with obesity later in life.[155][156]
An association between viruses and obesity has been found in humans and several different animal species. The amount that these associations may have contributed to the rising rate of obesity is yet to be determined.[157]
Other factors
A number of reviews have found an association between short duration of sleep and obesity.[158][159] Whether one causes the other is unclear.[158] Even if shorts sleep does increase weight gain it is unclear if this is to a meaningful degree or increasing sleep would be of benefit.[160]
Certain aspects of personality are associated with being obese.[161] Neuroticism, impulsivity, and sensitivity to reward are more common in people who are obese while conscientiousness and self-control are less common in people who are obese.[161][162] Loneliness is also a risk factor.[163]
Pathophysiology

There are many possible pathophysiological mechanisms involved in the development and maintenance of obesity.[164] This field of research had been almost unapproached until the leptin gene was discovered in 1994 by J. M. Friedman's laboratory.[165] While leptin and ghrelin are produced peripherally, they control appetite through their actions on the central nervous system. In particular, they and other appetite-related hormones act on the hypothalamus, a region of the brain central to the regulation of food intake and energy expenditure. There are several circuits within the hypothalamus that contribute to its role in integrating appetite, the melanocortin pathway being the most well understood.[164] The circuit begins with an area of the hypothalamus, the arcuate nucleus, that has outputs to the lateral hypothalamus (LH) and ventromedial hypothalamus (VMH), the brain's feeding and satiety centers, respectively.[166]
The arcuate nucleus contains two distinct groups of neurons.[164] The first group coexpresses neuropeptide Y (NPY) and agouti-related peptide (AgRP) and has stimulatory inputs to the LH and inhibitory inputs to the VMH. The second group coexpresses pro-opiomelanocortin (POMC) and cocaine- and amphetamine-regulated transcript (CART) and has stimulatory inputs to the VMH and inhibitory inputs to the LH. Consequently, NPY/AgRP neurons stimulate feeding and inhibit satiety, while POMC/CART neurons stimulate satiety and inhibit feeding. Both groups of arcuate nucleus neurons are regulated in part by leptin. Leptin inhibits the NPY/AgRP group while stimulating the POMC/CART group. Thus a deficiency in leptin signaling, either via leptin deficiency or leptin resistance, leads to overfeeding and may account for some genetic and acquired forms of obesity.[164]
Public health
The World Health Organization (WHO) predicts that overweight and obesity may soon replace more traditional public health concerns such as undernutrition and infectious diseases as the most significant cause of poor health.[167] Obesity is a public health and policy problem because of its prevalence, costs, and health effects.[168] The United States Preventive Services Task Force recommends screening for all adults followed by behavioral interventions in those who are obese.[169] Public health efforts seek to understand and correct the environmental factors responsible for the increasing prevalence of obesity in the population. Solutions look at changing the factors that cause excess food energy consumption and inhibit physical activity. Efforts include federally reimbursed meal programs in schools, limiting direct junk food marketing to children,[170] and decreasing access to sugar-sweetened beverages in schools.[171] The World Health Organization recommends the taxing of sugary drinks.[172] When constructing urban environments, efforts have been made to increase access to parks and to develop pedestrian routes.[173] There is low quality evidence that nutritional labelling with energy information on menus can help to reduce energy intake while dining in restaurants.[174]
Reports
Many organizations have published reports pertaining to obesity. In 1998, the first US Federal guidelines were published, titled "Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report".[175] In 2006 the Canadian Obesity Network, now known as Obesity Canada published the "Canadian Clinical Practice Guidelines (CPG) on the Management and Prevention of Obesity in Adults and Children". This is a comprehensive evidence-based guideline to address the management and prevention of overweight and obesity in adults and children.[86]
In 2004, the United Kingdom Royal College of Physicians, the Faculty of Public Health and the Royal College of Paediatrics and Child Health released the report "Storing up Problems", which highlighted the growing problem of obesity in the UK.[176] The same year, the House of Commons Health Select Committee published its "most comprehensive inquiry [...] ever undertaken" into the impact of obesity on health and society in the UK and possible approaches to the problem.[177] In 2006, the National Institute for Health and Clinical Excellence (NICE) issued a guideline on the diagnosis and management of obesity, as well as policy implications for non-healthcare organizations such as local councils.[178] A 2007 report produced by Derek Wanless for the King's Fund warned that unless further action was taken, obesity had the capacity to cripple the National Health Service financially.[179]
Comprehensive approaches are being looked at to address the rising rates of obesity. The Obesity Policy Action (OPA) framework divides measure into 'upstream' policies, 'midstream' policies, 'downstream' policies. 'Upstream' policies look at changing society, 'midstream' policies try to alter individuals' behavior to prevent obesity, and 'downstream' policies try to treat currently afflicted people.[180]
Management
The main treatment for obesity consists of weight loss via calorie restricted dieting and physical exercise.[17][86][181][182] Dieting, as part of a lifestyle change, produces sustained weight loss, despite slow weight regain over time.[17][183][184][185] Although 87% of participants in the National Weight Control Registry were able to maintain 10% body weight loss for 10 years,[186] the most appropriate dietary approach for long term weight loss maintenance is still unknown.[187] Intensive behavioral interventions combining both dietary changes and exercise are recommended.[17][181][188] Intermittent fasting has no additional benefit of weight loss compared to continuous energy restriction.[187] Adherence is a more important factor in weight loss success than whatever kind of diet an individual undertakes.[187][189]
Several hypo-caloric diets are effective.[17] In the short-term low carbohydrate diets appear better than low fat diets for weight loss.[190] In the long term, however, all types of low-carbohydrate and low-fat diets appear equally beneficial.[190][191] A 2014 review found that the heart disease and diabetes risks associated with different diets appear to be similar.[192] Promotion of the Mediterranean diets among the obese may lower the risk of heart disease.[190] Decreased intake of sweet drinks is also related to weight-loss.[190] Success rates of long-term weight loss maintenance with lifestyle changes are low, ranging from 2–20%.[193] Dietary and lifestyle changes are effective in limiting excessive weight gain in pregnancy and improve outcomes for both the mother and the child.[194] Intensive behavioral counseling is recommended in those who are both obese and have other risk factors for heart disease.[195]
Medications
Five medications have evidence for long-term use orlistat, lorcaserin, liraglutide, phentermine–topiramate, and naltrexone–bupropion as of 2017.[196] They result in weight loss after one year ranged from 3.0 to 6.7 kg (6.6-14.8 lbs) over placebo.[196] Orlistat, liraglutide, and naltrexone–bupropion are available in both the United States and Europe, whereas phentermine–topiramate are available only in the United States.[197] European regulatory authorities rejected the latter two drugs in part because of associations of heart valve problems with lorcaserin and more general heart and blood vessel problems with phentermine–topiramate.[197] Lorcaserin was available in the United States and than removed from the market in 2020 due to its association with cancer.[198] Orlistat use is associated with high rates of gastrointestinal side effects[199] and concerns have been raised about negative effects on the kidneys.[200] There is no information on how these drugs affect longer-term complications of obesity such as cardiovascular disease or death.[201]
Surgery
The most effective treatment for obesity is bariatric surgery.[6][17] The types of procedures include laparoscopic adjustable gastric banding, Roux-en-Y gastric bypass, vertical-sleeve gastrectomy, and biliopancreatic diversion.[196] Surgery for severe obesity is associated with long-term weight loss, improvement in obesity-related conditions, and decreased overall mortality.[202][203] One study found a weight loss of between 14% and 25% (depending on the type of procedure performed) at 10 years, and a 29% reduction in all cause mortality when compared to standard weight loss measures.[204] Complications occur in about 17% of cases and reoperation is needed in 7% of cases.[203] Due to its cost and risks, researchers are searching for other effective yet less invasive treatments including devices that occupy space in the stomach.[205] For adults who have not responded to behavioral treatments with or without medication, the US guidelines on obesity recommend informing them about bariatric surgery.[181]
Epidemiology
In earlier historical periods obesity was rare, and achievable only by a small elite, although already recognised as a problem for health. But as prosperity increased in the Early Modern period, it affected increasingly larger groups of the population.[206]
In 1997 the WHO formally recognized obesity as a global epidemic.[101] As of 2008 the WHO estimates that at least 500 million adults (greater than 10%) are obese, with higher rates among women than men.[207] The percentage of adults affected in the United States as of 2015–2016 is about 39.6% overall (37.9% of males and 41.1% of females).[208]
The rate of obesity also increases with age at least up to 50 or 60 years old[209] and severe obesity in the United States, Australia, and Canada is increasing faster than the overall rate of obesity.[31][210][211] The OECD has projected an increase in obesity rates until at least 2030, especially in the United States, Mexico and England with rates reaching 47%, 39% and 35% respectively.[212]
Once considered a problem only of high-income countries, obesity rates are rising worldwide and affecting both the developed and developing world.[46] These increases have been felt most dramatically in urban settings.[207] The only remaining region of the world where obesity is not common is sub-Saharan Africa.[2]
History
Etymology
Obesity is from the Latin obesitas, which means "stout, fat, or plump". Ēsus is the past participle of edere (to eat), with ob (over) added to it.[213] The Oxford English Dictionary documents its first usage in 1611 by Randle Cotgrave.[214]
Historical attitudes


Ancient Greek medicine recognizes obesity as a medical disorder, and records that the Ancient Egyptians saw it in the same way.[206] Hippocrates wrote that "Corpulence is not only a disease itself, but the harbinger of others".[2] The Indian surgeon Sushruta (6th century BCE) related obesity to diabetes and heart disorders.[216] He recommended physical work to help cure it and its side effects.[216] For most of human history mankind struggled with food scarcity.[217] Obesity has thus historically been viewed as a sign of wealth and prosperity. It was common among high officials in Europe in the Middle Ages and the Renaissance[215] as well as in Ancient East Asian civilizations.[218] In the 17th century, English medical author Tobias Venner is credited with being one of the first to refer to the term as a societal disease in a published English language book.[206][219]
With the onset of the Industrial Revolution it was realized that the military and economic might of nations were dependent on both the body size and strength of their soldiers and workers.[101] Increasing the average body mass index from what is now considered underweight to what is now the normal range played a significant role in the development of industrialized societies.[101] Height and weight thus both increased through the 19th century in the developed world. During the 20th century, as populations reached their genetic potential for height, weight began increasing much more than height, resulting in obesity.[101] In the 1950s increasing wealth in the developed world decreased child mortality, but as body weight increased heart and kidney disease became more common.[101][220] During this time period, insurance companies realized the connection between weight and life expectancy and increased premiums for the obese.[2]
Many cultures throughout history have viewed obesity as the result of a character flaw. The obesus or fat character in Ancient Greek comedy was a glutton and figure of mockery. During Christian times the food was viewed as a gateway to the sins of sloth and lust.[16] In modern Western culture, excess weight is often regarded as unattractive, and obesity is commonly associated with various negative stereotypes. People of all ages can face social stigmatization, and may be targeted by bullies or shunned by their peers.[221]
Public perceptions in Western society regarding healthy body weight differ from those regarding the weight that is considered ideal – and both have changed since the beginning of the 20th century. The weight that is viewed as an ideal has become lower since the 1920s. This is illustrated by the fact that the average height of Miss America pageant winners increased by 2% from 1922 to 1999, while their average weight decreased by 12%.[222] On the other hand, people's views concerning healthy weight have changed in the opposite direction. In Britain, the weight at which people considered themselves to be overweight was significantly higher in 2007 than in 1999.[223] These changes are believed to be due to increasing rates of adiposity leading to increased acceptance of extra body fat as being normal.[223]
Obesity is still seen as a sign of wealth and well-being in many parts of Africa. This has become particularly common since the HIV epidemic began.[2]
The arts
The first sculptural representations of the human body 20,000–35,000 years ago depict obese females. Some attribute the Venus figurines to the tendency to emphasize fertility while others feel they represent "fatness" in the people of the time.[16] Corpulence is, however, absent in both Greek and Roman art, probably in keeping with their ideals regarding moderation. This continued through much of Christian European history, with only those of low socioeconomic status being depicted as obese.[16]
During the Renaissance some of the upper class began flaunting their large size, as can be seen in portraits of Henry VIII of England and Alessandro dal Borro.[16] Rubens (1577–1640) regularly depicted full-bodied women in his pictures, from which derives the term Rubenesque. These women, however, still maintained the "hourglass" shape with its relationship to fertility.[224] During the 19th century, views on obesity changed in the Western world. After centuries of obesity being synonymous with wealth and social status, slimness began to be seen as the desirable standard.[16]
Society and culture
Economic impact
In addition to its health impacts, obesity leads to many problems including disadvantages in employment[225][226] and increased business costs. These effects are felt by all levels of society from individuals, to corporations, to governments.
In 2005, the medical costs attributable to obesity in the US were an estimated $190.2 billion or 20.6% of all medical expenditures,[227][228][229] while the cost of obesity in Canada was estimated at CA$2 billion in 1997 (2.4% of total health costs).[86] The total annual direct cost of overweight and obesity in Australia in 2005 was A$21 billion. Overweight and obese Australians also received A$35.6 billion in government subsidies.[230] The estimate range for annual expenditures on diet products is $40 billion to $100 billion in the US alone.[231]
The Lancet Commission on Obesity in 2019 called for a global treaty — modelled on the WHO Framework Convention on Tobacco Control — committing countries to address obesity and undernutrition, explicitly excluding the food industry from policy development. They estimate the global cost of obesity $2 trillion a year, about or 2.8% of world GDP.[232]
Obesity prevention programs have been found to reduce the cost of treating obesity-related disease. However, the longer people live, the more medical costs they incur. Researchers, therefore, conclude that reducing obesity may improve the public's health, but it is unlikely to reduce overall health spending.[233]

Obesity can lead to social stigmatization and disadvantages in employment.[225] When compared to their normal weight counterparts, obese workers on average have higher rates of absenteeism from work and take more disability leave, thus increasing costs for employers and decreasing productivity.[235] A study examining Duke University employees found that people with a BMI over 40 kg/m2 filed twice as many workers' compensation claims as those whose BMI was 18.5–24.9 kg/m2. They also had more than 12 times as many lost work days. The most common injuries in this group were due to falls and lifting, thus affecting the lower extremities, wrists or hands, and backs.[236] The Alabama State Employees' Insurance Board approved a controversial plan to charge obese workers $25 a month for health insurance that would otherwise be free unless they take steps to lose weight and improve their health. These measures started in January 2010 and apply to those state workers whose BMI exceeds 35 kg/m2 and who fail to make improvements in their health after one year.[237]
Some research shows that obese people are less likely to be hired for a job and are less likely to be promoted.[221] Obese people are also paid less than their non-obese counterparts for an equivalent job; obese women on average make 6% less and obese men make 3% less.[238]
Specific industries, such as the airline, healthcare and food industries, have special concerns. Due to rising rates of obesity, airlines face higher fuel costs and pressures to increase seating width.[239] In 2000, the extra weight of obese passengers cost airlines US$275 million.[240] The healthcare industry has had to invest in special facilities for handling severely obese patients, including special lifting equipment and bariatric ambulances.[241] Costs for restaurants are increased by litigation accusing them of causing obesity.[242] In 2005 the US Congress discussed legislation to prevent civil lawsuits against the food industry in relation to obesity; however, it did not become law.[242]
With the American Medical Association's 2013 classification of obesity as a chronic disease,[18] it is thought that health insurance companies will more likely pay for obesity treatment, counseling and surgery, and the cost of research and development of fat treatment pills or gene therapy treatments should be more affordable if insurers help to subsidize their cost.[243] The AMA classification is not legally binding, however, so health insurers still have the right to reject coverage for a treatment or procedure.[243]
In 2014, The European Court of Justice ruled that morbid obesity is a disability. The Court said that if an employee's obesity prevents him from "full and effective participation of that person in professional life on an equal basis with other workers", then it shall be considered a disability and that firing someone on such grounds is discriminatory.[244]
Size acceptance

The principal goal of the fat acceptance movement is to decrease discrimination against people who are overweight and obese.[245][246] However, some in the movement are also attempting to challenge the established relationship between obesity and negative health outcomes.[247]
A number of organizations exist that promote the acceptance of obesity. They have increased in prominence in the latter half of the 20th century.[248] The US-based National Association to Advance Fat Acceptance (NAAFA) was formed in 1969 and describes itself as a civil rights organization dedicated to ending size discrimination.[249]
The International Size Acceptance Association (ISAA) is a non-governmental organization (NGO) which was founded in 1997. It has more of a global orientation and describes its mission as promoting size acceptance and helping to end weight-based discrimination.[250] These groups often argue for the recognition of obesity as a disability under the US Americans With Disabilities Act (ADA). The American legal system, however, has decided that the potential public health costs exceed the benefits of extending this anti-discrimination law to cover obesity.[247]
Industry influence
In 2015 the New York Times published an article on the Global Energy Balance Network, a nonprofit founded in 2014 that advocated for people to focus on increasing exercise rather than reducing calorie intake to avoid obesity and to be healthy. The organization was founded with at least $1.5M in funding from the Coca-Cola Company, and the company has provided $4M in research funding to the two founding scientists Gregory A. Hand and Steven N. Blair since 2008.[251][252]
Childhood obesity
The healthy BMI range varies with the age and sex of the child. Obesity in children and adolescents is defined as a BMI greater than the 95th percentile.[25] The reference data that these percentiles are based on is from 1963 to 1994 and thus has not been affected by the recent increases in rates of obesity.[26] Childhood obesity has reached epidemic proportions in the 21st century, with rising rates in both the developed and the developing world. Rates of obesity in Canadian boys have increased from 11% in the 1980s to over 30% in the 1990s, while during this same time period rates increased from 4 to 14% in Brazilian children.[253] In the UK, there were 60% more obese children in 2005 compared to 1989.[254] In the US, the percentage of overweight and obese children increased to 16% in 2008, a 300% increase over the prior 30 years.[255]
As with obesity in adults, many factors contribute to the rising rates of childhood obesity. Changing diet and decreasing physical activity are believed to be the two most important causes for the recent increase in the incidence of child obesity.[256] Antibiotics in the first 6 months of life have been associated with excess weight at age seven to twelve years of age.[156] Because childhood obesity often persists into adulthood and is associated with numerous chronic illnesses, children who are obese are often tested for hypertension, diabetes, hyperlipidemia, and fatty liver disease.[86] Treatments used in children are primarily lifestyle interventions and behavioral techniques, although efforts to increase activity in children have had little success.[257] In the United States, medications are not FDA approved for use in this age group.[253] Multi-component behaviour change interventions that include changes to dietary and physical activity may reduce BMI in the short term in children aged 6 to 11 years, although the benefits are small and quality of evidence is low.[258]
Other animals
Obesity in pets is common in many countries. In the United States, 23–41% of dogs are overweight, and about 5.1% are obese.[259] The rate of obesity in cats was slightly higher at 6.4%.[259] In Australia the rate of obesity among dogs in a veterinary setting has been found to be 7.6%.[260] The risk of obesity in dogs is related to whether or not their owners are obese; however, there is no similar correlation between cats and their owners.[261]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 "Obesity and overweight Fact sheet N°311". WHO. January 2015. Archived from the original on 22 April 2018. Retrieved 2 February 2016.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 2.29 2.30 2.31 2.32 2.33 2.34 Haslam DW, James WP (October 2005). "Obesity". Lancet (Review). 366 (9492): 1197–209. doi:10.1016/S0140-6736(05)67483-1. PMID 16198769.
- ↑ 3.0 3.1 Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG (March 2010). "Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies". Archives of General Psychiatry. 67 (3): 220–9. doi:10.1001/archgenpsychiatry.2010.2. PMID 20194822.
- ↑ 4.0 4.1 Yazdi FT, Clee SM, Meyre D (2015). "Obesity genetics in mouse and human: back and forth, and back again". PeerJ. 3: e856. doi:10.7717/peerj.856. PMC 4375971. PMID 25825681.
- ↑ 5.0 5.1 5.2 Ryan, DH (2022). "Drugs for Treating Obesity". Handbook of experimental pharmacology. 274: 387–414. doi:10.1007/164_2021_560. PMID 34783910.
- ↑ 6.0 6.1 6.2 Colquitt JL, Pickett K, Loveman E, Frampton GK (August 2014). "Surgery for weight loss in adults". The Cochrane Database of Systematic Reviews (Meta-analysis, Review). 8 (8): CD003641. doi:10.1002/14651858.CD003641.pub4. PMID 25105982.
- ↑ "Homepage > NCD-RisC". ncdrisc.org. Archived from the original on 15 May 2023. Retrieved 2 March 2024.
- ↑ 8.0 8.1 Kanazawa M, Yoshiike N, Osaka T, Numba Y, Zimmet P, Inoue S (2005). "Criteria and Classification of Obesity in Japan and Asia-Oceania". Nutrition and Fitness: Obesity, the Metabolic Syndrome, Cardiovascular Disease, and Cancer. World Review of Nutrition and Dietetics. Vol. 94. pp. 1–12. doi:10.1159/000088200. ISBN 978-3-8055-7944-5. PMID 16145245. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ 9.0 9.1 Bleich S, Cutler D, Murray C, Adams A (2008). "Why is the developed world obese?". Annual Review of Public Health (Research Support). 29: 273–95. doi:10.1146/annurev.publhealth.29.020907.090954. PMID 18173389.
- ↑ 10.0 10.1 Oxford Handbook of Medical Sciences (2nd ed.). Oxford: OUP Oxford. 2011. p. 180. ISBN 9780191652295. Archived from the original on 7 August 2020. Retrieved 4 August 2020.
- ↑ Kushner, Robert (2007). Treatment of the Obese Patient (Contemporary Endocrinology). Totowa, NJ: Humana Press. p. 158. ISBN 978-1-59745-400-1. Retrieved 5 April 2009.
- ↑ Imaz I, Martínez-Cervell C, García-Alvarez EE, Sendra-Gutiérrez JM, González-Enríquez J (July 2008). "Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis". Obesity Surgery. 18 (7): 841–6. doi:10.1007/s11695-007-9331-8. PMID 18459025.
- ↑ Encyclopedia of Mental Health (2 ed.). Academic Press. 2015. p. 158. ISBN 9780123977533. Archived from the original on 18 August 2020. Retrieved 4 August 2020.
- ↑ Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, Salama JS, Vos T, Abate KH, Abbafati C, Ahmed MB, Al-Aly Z, Alkerwi A, Al-Raddadi R, Amare AT, Amberbir A, Amegah AK, Amini E, Amrock SM, Anjana RM, Ärnlöv J, Asayesh H, Banerjee A, Barac A, Baye E, Bennett DA, Beyene AS, Biadgilign S, Biryukov S, Bjertness E, Boneya DJ, Campos-Nonato I, Carrero JJ, Cecilio P, Cercy K, Ciobanu LG, Cornaby L, Damtew SA, Dandona L, Dandona R, Dharmaratne SD, Duncan BB, Eshrati B, Esteghamati A, Feigin VL, Fernandes JC, Fürst T, Gebrehiwot TT, Gold A, Gona PN, Goto A, Habtewold TD, Hadush KT, Hafezi-Nejad N, Hay SI, Horino M, Islami F, Kamal R, Kasaeian A, Katikireddi SV, Kengne AP, Kesavachandran CN, Khader YS, Khang YH, Khubchandani J, Kim D, Kim YJ, Kinfu Y, Kosen S, Ku T, Defo BK, Kumar GA, Larson HJ, Leinsalu M, Liang X, Lim SS, Liu P, Lopez AD, Lozano R, Majeed A, Malekzadeh R, Malta DC, Mazidi M, McAlinden C, McGarvey ST, Mengistu DT, Mensah GA, Mensink GB, Mezgebe HB, Mirrakhimov EM, Mueller UO, Noubiap JJ, Obermeyer CM, Ogbo FA, Owolabi MO, Patton GC, Pourmalek F, Qorbani M, Rafay A, Rai RK, Ranabhat CL, Reinig N, Safiri S, Salomon JA, Sanabria JR, Santos IS, Sartorius B, Sawhney M, Schmidhuber J, Schutte AE, Schmidt MI, Sepanlou SG, Shamsizadeh M, Sheikhbahaei S, Shin MJ, Shiri R, Shiue I, Roba HS, Silva DA, Silverberg JI, Singh JA, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tegegne BS, Terkawi AS, Thakur JS, Tonelli M, Topor-Madry R, Tyrovolas S, Ukwaja KN, Uthman OA, Vaezghasemi M, Vasankari T, Vlassov VV, Vollset SE, Weiderpass E, Werdecker A, Wesana J, Westerman R, Yano Y, Yonemoto N, Yonga G, Zaidi Z, Zenebe ZM, Zipkin B, Murray CJ (July 2017). "Health Effects of Overweight and Obesity in 195 Countries over 25 Years". The New England Journal of Medicine. 377 (1): 13–27. doi:10.1056/NEJMoa1614362. PMC 5477817. PMID 28604169.
- ↑ 15.0 15.1 15.2 15.3 15.4 Dibaise JK, Foxx-Orenstein AE (July 2013). "Role of the gastroenterologist in managing obesity". Expert Review of Gastroenterology & Hepatology (Review). 7 (5): 439–51. doi:10.1586/17474124.2013.811061. PMID 23899283.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 Woodhouse R (2008). "Obesity in Art – A Brief Overview". Obesity in art: a brief overview. Frontiers of Hormone Research. Vol. 36. pp. 271–86. doi:10.1159/000115370. ISBN 978-3-8055-8429-6. PMID 18230908.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 Jensen, MD; Ryan, DH; Apovian, CM; Ard, JD; Comuzzie, AG; Donato, KA; Hu, FB; Hubbard, VS; Jakicic, JM; Kushner, RF; Loria, CM; Millen, BE; Nonas, CA; Pi-Sunyer, FX; Stevens, J; Stevens, VJ; Wadden, TA; Wolfe, BM; Yanovski, SZ; Jordan, HS; Kendall, KA; Lux, LJ; Mentor-Marcel, R; Morgan, LC; Trisolini, MG; Wnek, J; Anderson, JL; Halperin, JL; Albert, NM; Bozkurt, B; Brindis, RG; Curtis, LH; DeMets, D; Hochman, JS; Kovacs, RJ; Ohman, EM; Pressler, SJ; Sellke, FW; Shen, WK; Smith SC, Jr; Tomaselli, GF; American College of Cardiology/American Heart Association Task Force on Practice, Guidelines.; Obesity, Society. (24 June 2014). "2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society". Circulation. 129 (25 Suppl 2): S102-38. doi:10.1161/01.cir.0000437739.71477.ee. PMC 5819889. PMID 24222017.
- Lay summary in: "Doctors urged to treat obesity as a disease under new guidelines".
{{cite journal}}: Cite journal requires|journal=(help)
- Lay summary in: "Doctors urged to treat obesity as a disease under new guidelines".
- ↑ 18.0 18.1 Pollack, Andrew (18 June 2013). "A.M.A. Recognizes Obesity as a Disease". New York Times. Archived from the original on 24 June 2013.
- ↑ Weinstock, Matthew (21 June 2013). "The Facts About Obesity". H&HN. American Hospital Association. Archived from the original on 9 September 2013. Retrieved 24 June 2013.
- ↑ "BMI classification". World Health Organization. Archived from the original on 9 May 2009. Retrieved 15 February 2014.
- ↑ WHO 2000 p.6
- ↑ Sweeting HN (October 2007). "Measurement and definitions of obesity in childhood and adolescence: a field guide for the uninitiated". Nutrition Journal. 6 (1): 32. doi:10.1186/1475-2891-6-32. PMC 2164947. PMID 17963490.
- ↑ NHLBI p.xiv
- ↑ Gray DS, Fujioka K (1991). "Use of relative weight and Body Mass Index for the determination of adiposity". Journal of Clinical Epidemiology. 44 (6): 545–50. doi:10.1016/0895-4356(91)90218-X. PMID 2037859.
- ↑ 25.0 25.1 "Healthy Weight: Assessing Your Weight: BMI: About BMI for Children and Teens". Center for disease control and prevention. Archived from the original on 29 October 2013. Retrieved 6 April 2009.
- ↑ 26.0 26.1 Flegal KM, Ogden CL, Wei R, Kuczmarski RL, Johnson CL (June 2001). "Prevalence of overweight in US children: comparison of US growth charts from the Centers for Disease Control and Prevention with other reference values for body mass index". The American Journal of Clinical Nutrition. 73 (6): 1086–93. doi:10.1093/ajcn/73.6.1086. PMID 11382664.
- ↑ 1 (lb/sq in) is more precisely 703.06957964 (kg/m2).
- ↑ WHO 2000 p.9
- ↑ Nikcevic, Ana V.; Kuczmierczyk, Andrzej R.; Bruch, Michael (2009). Formulation and Treatment in Clinical Health Psychology. Routledge. ISBN 9781135452087. Archived from the original on 7 August 2020. Retrieved 4 August 2020.
- ↑ 30.0 30.1 Bei-Fan Z (December 2002). "Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut-off points of body mass index and waist circumference in Chinese adults". Asia Pac J Clin Nutr. 11 (Suppl 8): S685–93. doi:10.1046/j.1440-6047.11.s8.9.x.; Originally printed as Zhou BF (March 2002). "Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults". Biomedical and Environmental Sciences. 15 (1): 83–96. PMID 12046553.
- ↑ 31.0 31.1 Sturm R (July 2007). "Increases in morbid obesity in the USA: 2000–2005". Public Health. 121 (7): 492–6. doi:10.1016/j.puhe.2007.01.006. PMC 2864630. PMID 17399752.
- ↑ 32.0 32.1 32.2 32.3 Poulain M, Doucet M, Major GC, Drapeau V, Sériès F, Boulet LP, Tremblay A, Maltais F (April 2006). "The effect of obesity on chronic respiratory diseases: pathophysiology and therapeutic strategies". CMAJ. 174 (9): 1293–9. doi:10.1503/cmaj.051299. PMC 1435949. PMID 16636330.
- ↑ Berrington de Gonzalez, A; Hartge, P; Cerhan, JR; Flint, AJ; Hannan, L; MacInnis, RJ; Moore, SC; Tobias, GS; Anton-Culver, H; Freeman, LB; Beeson, WL; Clipp, SL; English, DR; Folsom, AR; Freedman, DM; Giles, G; Hakansson, N; Henderson, KD; Hoffman-Bolton, J; Hoppin, JA; Koenig, KL; Lee, IM; Linet, MS; Park, Y; Pocobelli, G; Schatzkin, A; Sesso, HD; Weiderpass, E; Willcox, BJ; Wolk, A; Zeleniuch-Jacquotte, A; Willett, WC; Thun, MJ (2 December 2010). "Body-mass index and mortality among 1.46 million white adults". The New England Journal of Medicine. 363 (23): 2211–9. doi:10.1056/NEJMoa1000367. PMC 3066051. PMID 21121834.: Supp.Table3
- ↑ Barness LA, Opitz JM, Gilbert-Barness E (December 2007). "Obesity: genetic, molecular, and environmental aspects". American Journal of Medical Genetics. Part A. 143A (24): 3016–34. doi:10.1002/ajmg.a.32035. PMID 18000969.
- ↑ Mokdad AH, Marks JS, Stroup DF, Gerberding JL (March 2004). "Actual causes of death in the United States, 2000". JAMA. 291 (10): 1238–45. doi:10.1001/jama.291.10.1238. PMID 15010446. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ 36.0 36.1 Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB (October 1999). "Annual deaths attributable to obesity in the United States". JAMA. 282 (16): 1530–8. doi:10.1001/jama.282.16.1530. PMID 10546692.
- ↑ Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, Romundstad P, Vatten LJ (May 2016). "BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants". BMJ. 353: i2156. doi:10.1136/bmj.i2156. PMC 4856854. PMID 27146380.
- ↑ 38.0 38.1 38.2 Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R (March 2009). "Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies". Lancet. 373 (9669): 1083–96. doi:10.1016/S0140-6736(09)60318-4. PMC 2662372. PMID 19299006.
- ↑ 39.0 39.1 Di Angelantonio E, Bhupathiraju S, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, et al. (The Global BMI Mortality Collaboration) (August 2016). "Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents". Lancet. 388 (10046): 776–86. doi:10.1016/S0140-6736(16)30175-1. PMC 4995441. PMID 27423262.
- ↑ Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW (October 1999). "Body-mass index and mortality in a prospective cohort of U.S. adults". The New England Journal of Medicine. 341 (15): 1097–105. doi:10.1056/NEJM199910073411501. PMID 10511607.
- ↑ Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, van der Schouw YT, Spencer E, Moons KG, Tjønneland A, Halkjaer J, Jensen MK, Stegger J, Clavel-Chapelon F, Boutron-Ruault MC, Chajes V, Linseisen J, Kaaks R, Trichopoulou A, Trichopoulos D, Bamia C, Sieri S, Palli D, Tumino R, Vineis P, Panico S, Peeters PH, May AM, Bueno-de-Mesquita HB, van Duijnhoven FJ, Hallmans G, Weinehall L, Manjer J, Hedblad B, Lund E, Agudo A, Arriola L, Barricarte A, Navarro C, Martinez C, Quirós JR, Key T, Bingham S, Khaw KT, Boffetta P, Jenab M, Ferrari P, Riboli E (November 2008). "General and abdominal adiposity and risk of death in Europe". The New England Journal of Medicine. 359 (20): 2105–20. doi:10.1056/NEJMoa0801891. PMID 19005195. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ Flegal KM, Kit BK, Orpana H, Graubard BI (January 2013). "Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis". JAMA. 309 (1): 71–82. doi:10.1001/jama.2012.113905. PMC 4855514. PMID 23280227.
- ↑ Carmienke S, Freitag MH, Pischon T, Schlattmann P, Fankhaenel T, Goebel H, Gensichen J (June 2013). "General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis". European Journal of Clinical Nutrition. 67 (6): 573–85. doi:10.1038/ejcn.2013.61. PMID 23511854.
- ↑ WHO Expert Consultation (January 2004). "Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies". Lancet. 363 (9403): 157–63. doi:10.1016/s0140-6736(03)15268-3. PMID 14726171.
- ↑ Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE (September 1995). "Body weight and mortality among women". The New England Journal of Medicine. 333 (11): 677–85. doi:10.1056/NEJM199509143331101. PMID 7637744.
- ↑ 46.0 46.1 Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, Micic D, Maislos M, Roman G, Schutz Y, Toplak H, Zahorska-Markiewicz B (April 2008). "Management of obesity in adults: European clinical practice guidelines" (PDF). Obesity Facts. 1 (2): 106–16. doi:10.1159/000126822. PMC 6452117. PMID 20054170. Archived from the original (PDF) on 26 April 2012.
- ↑ Fried M, Hainer V, Basdevant A, Buchwald H, Deitel M, Finer N, Greve JW, Horber F, Mathus-Vliegen E, Scopinaro N, Steffen R, Tsigos C, Weiner R, Widhalm K (April 2007). "Inter-disciplinary European guidelines on surgery of severe obesity". International Journal of Obesity. 31 (4): 569–77. doi:10.1038/sj.ijo.0803560. PMID 17325689.
- ↑ Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L (January 2003). "Obesity in adulthood and its consequences for life expectancy: a life-table analysis" (PDF). Annals of Internal Medicine. 138 (1): 24–32. doi:10.7326/0003-4819-138-1-200301070-00008. hdl:1765/10043. PMID 12513041. Archived (PDF) from the original on 10 September 2016. Retrieved 4 August 2020.
- ↑ Hoshi, A; Inaba, Y (August 1995). "[Risk factors for mortality and mortality rate of sumo wrestlers]". Nihon eiseigaku zasshi. Japanese journal of hygiene. 50 (3): 730–6. doi:10.1265/jjh.50.730. PMID 7474495.
- ↑ Okumura, Kaki (9 December 2021). "How Do Retired Sumo Wrestlers Lose Weight?". Medium. Archived from the original on 30 January 2023. Retrieved 16 May 2023.
- ↑ Grundy SM (June 2004). "Obesity, metabolic syndrome, and cardiovascular disease". The Journal of Clinical Endocrinology and Metabolism. 89 (6): 2595–600. doi:10.1210/jc.2004-0372. PMID 15181029.
- ↑ Seidell 2005 p.9
- ↑ 53.0 53.1 Bray GA (June 2004). "Medical consequences of obesity". The Journal of Clinical Endocrinology and Metabolism. 89 (6): 2583–9. doi:10.1210/jc.2004-0535. PMID 15181027.
- ↑ Shoelson SE, Herrero L, Naaz A (May 2007). "Obesity, inflammation, and insulin resistance". Gastroenterology. 132 (6): 2169–80. doi:10.1053/j.gastro.2007.03.059. PMID 17498510.
- ↑ Shoelson SE, Lee J, Goldfine AB (July 2006). "Inflammation and insulin resistance". The Journal of Clinical Investigation. 116 (7): 1793–801. doi:10.1172/JCI29069. PMC 1483173. PMID 16823477.
- ↑ Dentali F, Squizzato A, Ageno W (July 2009). "The metabolic syndrome as a risk factor for venous and arterial thrombosis". Seminars in Thrombosis and Hemostasis. 35 (5): 451–7. doi:10.1055/s-0029-1234140. PMID 19739035.
- ↑ "People with Certain Medical Conditions". Centers For Diseases Control and Prevention. 30 July 2020. Archived from the original on 18 March 2021. Retrieved 2 August 2020.
- ↑ Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G (March 2014). "Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants". Lancet. 383 (9921): 970–83. doi:10.1016/S0140-6736(13)61836-X. PMC 3959199. PMID 24269108.
- ↑ Aune D, Sen A, Norat T, Janszky I, Romundstad P, Tonstad S, Vatten LJ (February 2016). "Body Mass Index, Abdominal Fatness, and Heart Failure Incidence and Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies". Circulation. 133 (7): 639–49. doi:10.1161/CIRCULATIONAHA.115.016801. PMID 26746176.
- ↑ Darvall KA, Sam RC, Silverman SH, Bradbury AW, Adam DJ (February 2007). "Obesity and thrombosis". European Journal of Vascular and Endovascular Surgery. 33 (2): 223–33. doi:10.1016/j.ejvs.2006.10.006. PMID 17185009.
- ↑ 61.0 61.1 61.2 61.3 61.4 Yosipovitch G, DeVore A, Dawn A (June 2007). "Obesity and the skin: skin physiology and skin manifestations of obesity". Journal of the American Academy of Dermatology. 56 (6): 901–16, quiz 917–20. doi:10.1016/j.jaad.2006.12.004. PMID 17504714.
- ↑ Hahler B (June 2006). "An overview of dermatological conditions commonly associated with the obese patient". Ostomy/Wound Management. 52 (6): 34–6, 38, 40 passim. PMID 16799182.
- ↑ 63.0 63.1 63.2 Arendas K, Qiu Q, Gruslin A (June 2008). "Obesity in pregnancy: pre-conceptional to postpartum consequences". Journal of Obstetrics and Gynaecology Canada. 30 (6): 477–488. doi:10.1016/s1701-2163(16)32863-8. PMID 18611299.
- ↑ Harney D, Patijn J (2007). "Meralgia paresthetica: diagnosis and management strategies". Pain Medicine (Review). 8 (8): 669–77. doi:10.1111/j.1526-4637.2006.00227.x. PMID 18028045.
- ↑ Bigal ME, Lipton RB (January 2008). "Obesity and chronic daily headache". Current Pain and Headache Reports (Review). 12 (1): 56–61. doi:10.1007/s11916-008-0011-8. PMID 18417025.
- ↑ Sharifi-Mollayousefi A, Yazdchi-Marandi M, Ayramlou H, Heidari P, Salavati A, Zarrintan S, Sharifi-Mollayousefi A (February 2008). "Assessment of body mass index and hand anthropometric measurements as independent risk factors for carpal tunnel syndrome". Folia Morphologica. 67 (1): 36–42. PMID 18335412.
- ↑ Beydoun MA, Beydoun HA, Wang Y (May 2008). "Obesity and central obesity as risk factors for incident dementia and its subtypes: a systematic review and meta-analysis". Obesity Reviews (Meta-analysis). 9 (3): 204–18. doi:10.1111/j.1467-789X.2008.00473.x. PMC 4887143. PMID 18331422.
- ↑ Wall M (March 2008). "Idiopathic intracranial hypertension (pseudotumor cerebri)". Current Neurology and Neuroscience Reports (Review). 8 (2): 87–93. doi:10.1007/s11910-008-0015-0. PMID 18460275.
- ↑ Munger KL, Chitnis T, Ascherio A (November 2009). "Body size and risk of MS in two cohorts of US women". Neurology (Comparative Study). 73 (19): 1543–50. doi:10.1212/WNL.0b013e3181c0d6e0. PMC 2777074. PMID 19901245.
- ↑ Basen-Engquist K, Chang M (February 2011). "Obesity and cancer risk: recent review and evidence". Current Oncology Reports. 13 (1): 71–6. doi:10.1007/s11912-010-0139-7. PMC 3786180. PMID 21080117.
- ↑ Aune D, Norat T, Vatten LJ (December 2014). "Body mass index and the risk of gout: a systematic review and dose-response meta-analysis of prospective studies". European Journal of Nutrition. 53 (8): 1591–601. doi:10.1007/s00394-014-0766-0. PMID 25209031.
- ↑ Tukker A, Visscher TL, Picavet HS (March 2009). "Overweight and health problems of the lower extremities: osteoarthritis, pain and disability". Public Health Nutrition (Research Support). 12 (3): 359–68. doi:10.1017/S1368980008002103. PMID 18426630.
- ↑ Molenaar EA, Numans ME, van Ameijden EJ, Grobbee DE (November 2008). "[Considerable comorbidity in overweight adults: results from the Utrecht Health Project]". Nederlands Tijdschrift voor Geneeskunde (English abstract) (in Dutch). 152 (45): 2457–63. PMID 19051798.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Corona G, Rastrelli G, Filippi S, Vignozzi L, Mannucci E, Maggi M (2014). "Erectile dysfunction and central obesity: an Italian perspective". Asian Journal of Andrology. 16 (4): 581–91. doi:10.4103/1008-682X.126386. PMC 4104087. PMID 24713832.
- ↑ Hunskaar S (2008). "A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women". Neurourology and Urodynamics (Review). 27 (8): 749–57. doi:10.1002/nau.20635. PMID 18951445. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ Ejerblad E, Fored CM, Lindblad P, Fryzek J, McLaughlin JK, Nyrén O (June 2006). "Obesity and risk for chronic renal failure". Journal of the American Society of Nephrology (Research Support). 17 (6): 1695–702. doi:10.1681/ASN.2005060638. PMID 16641153.
- ↑ Makhsida N, Shah J, Yan G, Fisch H, Shabsigh R (September 2005). "Hypogonadism and metabolic syndrome: implications for testosterone therapy". The Journal of Urology (Review). 174 (3): 827–34. CiteSeerX 10.1.1.612.1060. doi:10.1097/01.ju.0000169490.78443.59. PMID 16093964.
- ↑ Pestana IA, Greenfield JM, Walsh M, Donatucci CF, Erdmann D (October 2009). "Management of "buried" penis in adulthood: an overview". Plastic and Reconstructive Surgery (Review). 124 (4): 1186–95. doi:10.1097/PRS.0b013e3181b5a37f. PMID 19935302.
- ↑ 79.0 79.1 Schmidt DS, Salahudeen AK (2007). "Obesity-survival paradox-still a controversy?". Seminars in Dialysis (Review). 20 (6): 486–92. doi:10.1111/j.1525-139X.2007.00349.x. PMID 17991192.
- ↑ 80.0 80.1 U.S. Preventive Services Task Force (June 2003). "Behavioral counseling in primary care to promote a healthy diet: recommendations and rationale". American Family Physician (Review). 67 (12): 2573–6. PMID 12825847.
- ↑ Habbu A, Lakkis NM, Dokainish H (October 2006). "The obesity paradox: fact or fiction?". The American Journal of Cardiology (Review). 98 (7): 944–8. doi:10.1016/j.amjcard.2006.04.039. PMID 16996880.
- ↑ Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, Mookadam F, Lopez-Jimenez F (August 2006). "Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies". Lancet (Review). 368 (9536): 666–78. doi:10.1016/S0140-6736(06)69251-9. PMID 16920472.
- ↑ Oreopoulos A, Padwal R, Kalantar-Zadeh K, Fonarow GC, Norris CM, McAlister FA (July 2008). "Body mass index and mortality in heart failure: a meta-analysis". American Heart Journal (Meta-analysis, Review). 156 (1): 13–22. doi:10.1016/j.ahj.2008.02.014. PMID 18585492. Archived from the original on 24 December 2020. Retrieved 4 August 2020.
- ↑ Oreopoulos A, Padwal R, Norris CM, Mullen JC, Pretorius V, Kalantar-Zadeh K (February 2008). "Effect of obesity on short- and long-term mortality postcoronary revascularization: a meta-analysis". Obesity (Meta-analysis). 16 (2): 442–50. doi:10.1038/oby.2007.36. PMID 18239657. Archived from the original on 5 August 2020. Retrieved 4 August 2020.
- ↑ Diercks DB, Roe MT, Mulgund J, Pollack CV, Kirk JD, Gibler WB, Ohman EM, Smith SC, Boden WE, Peterson ED (July 2006). "The obesity paradox in non-ST-segment elevation acute coronary syndromes: results from the Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the American College of Cardiology/American Heart Association Guidelines Quality Improvement Initiative". American Heart Journal (Research Support). 152 (1): 140–8. doi:10.1016/j.ahj.2005.09.024. PMID 16824844.
- ↑ 86.0 86.1 86.2 86.3 86.4 Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E (April 2007). "2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]". CMAJ (Practice Guideline, Review). 176 (8): S1–13. doi:10.1503/cmaj.061409. PMC 1839777. PMID 17420481.
- ↑ Drewnowski A, Specter SE (January 2004). "Poverty and obesity: the role of energy density and energy costs". The American Journal of Clinical Nutrition (Review). 79 (1): 6–16. doi:10.1093/ajcn/79.1.6. PMID 14684391.
- ↑ Nestle M, Jacobson MF (2000). "Halting the obesity epidemic: a public health policy approach". Public Health Reports (Research Support). 115 (1): 12–24. doi:10.1093/phr/115.1.12. PMC 1308552. PMID 10968581.
- ↑ James WP (March 2008). "The fundamental drivers of the obesity epidemic". Obesity Reviews (Review). 9 Suppl 1 (Suppl 1): 6–13. doi:10.1111/j.1467-789X.2007.00432.x. PMID 18307693. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ Keith SW, Redden DT, Katzmarzyk PT, Boggiano MM, Hanlon EC, Benca RM, Ruden D, Pietrobelli A, Barger JL, Fontaine KR, Wang C, Aronne LJ, Wright SM, Baskin M, Dhurandhar NV, Lijoi MC, Grilo CM, DeLuca M, Westfall AO, Allison DB (November 2006). "Putative contributors to the secular increase in obesity: exploring the roads less traveled". International Journal of Obesity (Review). 30 (11): 1585–94. doi:10.1038/sj.ijo.0803326. PMID 16801930.
- ↑ Schwartz, MW; Seeley, RJ; Zeltser, LM; Drewnowski, A; Ravussin, E; Redman, LM; Leibel, RL (1 August 2017). "Obesity Pathogenesis: An Endocrine Society Scientific Statement". Endocrine Reviews (Professional society guidelines). 38 (4): 267–296. doi:10.1210/er.2017-00111. PMC 5546881. PMID 28898979.
- ↑ 92.0 92.1 92.2 92.3 92.4 92.5 "EarthTrends: Nutrition: Calorie supply per capita". World Resources Institute. Archived from the original on 11 June 2011. Retrieved 18 October 2009.
- ↑ Bojanowska E, Ciosek J (15 February 2016). "Can We Selectively Reduce Appetite for Energy-Dense Foods? An Overview of Pharmacological Strategies for Modification of Food Preference Behavior". Current Neuropharmacology. 14 (2): 118–42. doi:10.2174/1570159X14666151109103147. PMC 4825944. PMID 26549651.
- ↑ Levitsky, DA; Sewall, A; Zhong, Y; Barre, L; Shoen, S; Agaronnik, N; LeClair, JL; Zhuo, W; Pacanowski, C (1 February 2019). "Quantifying the imprecision of energy intake of humans to compensate for imposed energetic errors: A challenge to the physiological control of human food intake". Appetite. 133: 337–343. doi:10.1016/j.appet.2018.11.017. PMID 30476522.
- ↑ "USDA: frsept99b". United States Department of Agriculture. Archived from the original on 3 June 2010. Retrieved 10 January 2009.
- ↑ "Diet composition and obesity among Canadian adults". Statistics Canada. Archived from the original on 22 April 2018.
- ↑ National Control for Health Statistics. "Nutrition For Everyone". Centers for Disease Control and Prevention. Archived from the original on 21 August 2008. Retrieved 9 July 2008.
- ↑ Marantz PR, Bird ED, Alderman MH (March 2008). "A call for higher standards of evidence for dietary guidelines". American Journal of Preventive Medicine. 34 (3): 234–40. doi:10.1016/j.amepre.2007.11.017. PMID 18312812.
- ↑ Flegal KM, Carroll MD, Ogden CL, Johnson CL (October 2002). "Prevalence and trends in obesity among US adults, 1999–2000". JAMA. 288 (14): 1723–7. doi:10.1001/jama.288.14.1723. PMID 12365955.
- ↑ Centers for Disease Control Prevention (CDC) (February 2004). "Trends in intake of energy and macronutrients—United States, 1971–2000". MMWR. Morbidity and Mortality Weekly Report. 53 (4): 80–2. PMID 14762332. Archived from the original on 20 June 2019. Retrieved 4 August 2020.
- ↑ 101.0 101.1 101.2 101.3 101.4 101.5 Caballero B (2007). "The global epidemic of obesity: an overview". Epidemiologic Reviews. 29: 1–5. doi:10.1093/epirev/mxm012. PMID 17569676.
- ↑ Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB (June 2011). "Changes in diet and lifestyle and long-term weight gain in women and men". The New England Journal of Medicine (Meta-analysis). 364 (25): 2392–404. doi:10.1056/NEJMoa1014296. PMC 3151731. PMID 21696306.
- ↑ Malik VS, Schulze MB, Hu FB (August 2006). "Intake of sugar-sweetened beverages and weight gain: a systematic review". The American Journal of Clinical Nutrition (Review). 84 (2): 274–88. doi:10.1093/ajcn/84.2.274. PMC 3210834. PMID 16895873.
- ↑ Olsen NJ, Heitmann BL (January 2009). "Intake of calorically sweetened beverages and obesity". Obesity Reviews (Review). 10 (1): 68–75. doi:10.1111/j.1467-789X.2008.00523.x. PMID 18764885.
- ↑ Malik VS, Popkin BM, Bray GA, Després JP, Willett WC, Hu FB (November 2010). "Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis". Diabetes Care (Meta-analysis, Review). 33 (11): 2477–83. doi:10.2337/dc10-1079. PMC 2963518. PMID 20693348.
- ↑ Wamberg L, Pedersen SB, Rejnmark L, Richelsen B (December 2015). "Causes of Vitamin D Deficiency and Effect of Vitamin D Supplementation on Metabolic Complications in Obesity: a Review". Current Obesity Reports. 4 (4): 429–40. doi:10.1007/s13679-015-0176-5. PMID 26353882.
- ↑ Rosenheck R (November 2008). "Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk". Obesity Reviews (Review). 9 (6): 535–47. doi:10.1111/j.1467-789X.2008.00477.x. PMID 18346099.
- ↑ Lin BH, Guthrie J, Frazao E (1999). "Nutrient contribution of food away from home". In Frazão E (ed.). Agriculture Information Bulletin No. 750: America's Eating Habits: Changes and Consequences. Washington, DC: US Department of Agriculture, Economic Research Service. pp. 213–39. Archived from the original on 8 July 2012.
- ↑ Pollan, Michael (22 April 2007). "You Are What You Grow". New York Times. Archived from the original on 17 July 2019. Retrieved 30 July 2007.
- ↑ Kopelman and Caterson 2005:324.
- ↑ Metabolism alone doesn't explain how thin people stay thin. John Schieszer. The Medical Post.
- ↑ Seidell 2005 p. 10
- ↑ 113.0 113.1 "Obesity and overweight". World Health Organization. Archived from the original on 18 December 2008. Retrieved 10 January 2009.
- ↑ 114.0 114.1 114.2 "WHO | Physical Inactivity: A Global Public Health Problem". World Health Organization. Archived from the original on 13 February 2014. Retrieved 22 February 2009.
- ↑ 115.0 115.1 Ness-Abramof R, Apovian CM (February 2006). "Diet modification for treatment and prevention of obesity". Endocrine (Review). 29 (1): 5–9. doi:10.1385/ENDO:29:1:135. PMID 16622287.
- ↑ Salmon J, Timperio A (2007). "Prevalence, Trends and Environmental Influences on Child and Youth Physical Activity". Pediatric Fitness (Review). Medicine and Sport Science. Vol. 50. pp. 183–99. doi:10.1159/000101391. ISBN 978-3-318-01396-2. PMID 17387258.
- ↑ Borodulin K, Laatikainen T, Juolevi A, Jousilahti P (June 2008). "Thirty-year trends of physical activity in relation to age, calendar time and birth cohort in Finnish adults". European Journal of Public Health (Research Support). 18 (3): 339–44. doi:10.1093/eurpub/ckm092. PMID 17875578.
- ↑ Brownson RC, Boehmer TK, Luke DA (2005). "Declining rates of physical activity in the United States: what are the contributors?". Annual Review of Public Health (Review). 26: 421–43. doi:10.1146/annurev.publhealth.26.021304.144437. PMID 15760296. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ Wilks DC, Sharp SJ, Ekelund U, Thompson SG, Mander AP, Turner RM, Jebb SA, Lindroos AK (February 2011). "Objectively measured physical activity and fat mass in children: a bias-adjusted meta-analysis of prospective studies". PLOS One. 6 (2): e17205. Bibcode:2011PLoSO...617205W. doi:10.1371/journal.pone.0017205. PMC 3044163. PMID 21383837.
- ↑ Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH (April 1996). "Television viewing as a cause of increasing obesity among children in the United States, 1986–1990". Archives of Pediatrics & Adolescent Medicine (Review). 150 (4): 356–62. doi:10.1001/archpedi.1996.02170290022003. PMID 8634729.
- ↑ Vioque J, Torres A, Quiles J (December 2000). "Time spent watching television, sleep duration and obesity in adults living in Valencia, Spain". International Journal of Obesity and Related Metabolic Disorders (Research Support). 24 (12): 1683–8. doi:10.1038/sj.ijo.0801434. PMID 11126224.
- ↑ Tucker LA, Bagwell M (July 1991). "Television viewing and obesity in adult females". American Journal of Public Health. 81 (7): 908–11. doi:10.2105/AJPH.81.7.908. PMC 1405200. PMID 2053671.
- ↑ Emanuel, Ezekiel J. (2008). "Media + Child and Adolescent Health: A Systematic Review" (PDF). Common Sense Media. Archived (PDF) from the original on 22 November 2012. Retrieved 6 April 2009.
- ↑ Mary Jones. "Case Study: Cataplexy and SOREMPs Without Excessive Daytime Sleepiness in Prader Willi Syndrome. Is This the Beginning of Narcolepsy in a Five Year Old?". European Society of Sleep Technologists. Archived from the original on 13 April 2009. Retrieved 6 April 2009.
- ↑ Albuquerque D, Nóbrega C, Manco L, Padez C (September 2017). "The contribution of genetics and environment to obesity". British Medical Bulletin. 123 (1): 159–173. doi:10.1093/bmb/ldx022. PMID 28910990.
- ↑ Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH (May 2006). "Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss". Arteriosclerosis, Thrombosis, and Vascular Biology (Review). 26 (5): 968–76. CiteSeerX 10.1.1.508.7066. doi:10.1161/01.ATV.0000216787.85457.f3. PMID 16627822.
- ↑ Loos RJ, Bouchard C (May 2008). "FTO: the first gene contributing to common forms of human obesity". Obesity Reviews (Review). 9 (3): 246–50. doi:10.1111/j.1467-789X.2008.00481.x. PMID 18373508.
- ↑ Yang W, Kelly T, He J (2007). "Genetic epidemiology of obesity". Epidemiologic Reviews (Review). 29: 49–61. doi:10.1093/epirev/mxm004. PMID 17566051.
- ↑ Walley AJ, Asher JE, Froguel P (July 2009). "The genetic contribution to non-syndromic human obesity". Nature Reviews. Genetics (Review). 10 (7): 431–42. doi:10.1038/nrg2594. PMID 19506576.
- ↑ Farooqi S, O'Rahilly S (December 2006). "Genetics of obesity in humans". Endocrine Reviews (Review). 27 (7): 710–18. doi:10.1210/er.2006-0040. PMID 17122358. Archived from the original on 10 July 2010. Retrieved 4 August 2020.
- ↑ Kolata, Gina (2007). Rethinking thin: The new science of weight loss – and the myths and realities of dieting. Picador. p. 122. ISBN 978-0-312-42785-6.
- ↑ Walley AJ, Asher JE, Froguel P (July 2009). "The genetic contribution to non-syndromic human obesity". Nature Reviews. Genetics (Review). 10 (7): 431–42. doi:10.1038/nrg2594. PMID 19506576.
However, it is also clear that genetics greatly influences this situation, giving individuals in the same 'obesogenic' environment significantly different risks of becoming obese.
- ↑ Chakravarthy MV, Booth FW (January 2004). "Eating, exercise, and "thrifty" genotypes: connecting the dots toward an evolutionary understanding of modern chronic diseases". Journal of Applied Physiology (Review). 96 (1): 3–10. doi:10.1152/japplphysiol.00757.2003. PMID 14660491. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ Wells JC (December 2009). "Thrift: a guide to thrifty genes, thrifty phenotypes and thrifty norms". International Journal of Obesity (Review). 33 (12): 1331–8. doi:10.1038/ijo.2009.175. PMID 19752875.
- ↑ Wells JC (2011). "The thrifty phenotype: An adaptation in growth or metabolism?". American Journal of Human Biology (Review). 23 (1): 65–75. doi:10.1002/ajhb.21100. PMID 21082685.
- ↑ Rosén T, Bosaeus I, Tölli J, Lindstedt G, Bengtsson BA (January 1993). "Increased body fat mass and decreased extracellular fluid volume in adults with growth hormone deficiency". Clinical Endocrinology. 38 (1): 63–71. doi:10.1111/j.1365-2265.1993.tb00974.x. PMID 8435887.
- ↑ Zametkin AJ, Zoon CK, Klein HW, Munson S (February 2004). "Psychiatric aspects of child and adolescent obesity: a review of the past 10 years". Journal of the American Academy of Child and Adolescent Psychiatry (Review). 43 (2): 134–50. doi:10.1097/00004583-200402000-00008. PMID 14726719.
- ↑ Chiles C, van Wattum PJ (2010). "Psychiatric aspects of the obesity crisis". Psychiatr Times. 27 (4): 47–51.
- ↑ Yach D, Stuckler D, Brownell KD (January 2006). "Epidemiologic and economic consequences of the global epidemics of obesity and diabetes". Nature Medicine. 12 (1): 62–6. doi:10.1038/nm0106-62. PMID 16397571.
- ↑ Sobal J, Stunkard AJ (March 1989). "Socioeconomic status and obesity: a review of the literature". Psychological Bulletin (Review). 105 (2): 260–75. doi:10.1037/0033-2909.105.2.260. PMID 2648443.
- ↑ 141.0 141.1 McLaren L (2007). "Socioeconomic status and obesity". Epidemiologic Reviews (Review). 29: 29–48. doi:10.1093/epirev/mxm001. PMID 17478442.
- ↑ 142.0 142.1 Wilkinson, Richard; Pickett, Kate (2009). The Spirit Level: Why More Equal Societies Almost Always Do Better. London: Allen Lane. pp. 91–101. ISBN 978-1-84614-039-6.
- ↑ Christakis NA, Fowler JH (July 2007). "The spread of obesity in a large social network over 32 years". The New England Journal of Medicine (Research Support). 357 (4): 370–9. CiteSeerX 10.1.1.581.4893. doi:10.1056/NEJMsa066082. PMID 17652652.
- ↑ Björntorp P (May 2001). "Do stress reactions cause abdominal obesity and comorbidities?". Obesity Reviews. 2 (2): 73–86. doi:10.1046/j.1467-789x.2001.00027.x. PMID 12119665.
- ↑ Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM (August 2003). "Impact of objective and subjective social status on obesity in a biracial cohort of adolescents". Obesity Research (Research Support). 11 (8): 1018–26. doi:10.1038/oby.2003.140. PMID 12917508.
- ↑ Flegal KM, Troiano RP, Pamuk ER, Kuczmarski RJ, Campbell SM (November 1995). "The influence of smoking cessation on the prevalence of overweight in the United States". The New England Journal of Medicine. 333 (18): 1165–70. doi:10.1056/NEJM199511023331801. PMID 7565970.
- ↑ Chiolero A, Faeh D, Paccaud F, Cornuz J (April 2008). "Consequences of smoking for body weight, body fat distribution, and insulin resistance". The American Journal of Clinical Nutrition (Review). 87 (4): 801–9. doi:10.1093/ajcn/87.4.801. PMID 18400700.
- ↑ Weng HH, Bastian LA, Taylor DH, Moser BK, Ostbye T (2004). "Number of children associated with obesity in middle-aged women and men: results from the health and retirement study". Journal of Women's Health (Comparative Study). 13 (1): 85–91. doi:10.1089/154099904322836492. PMID 15006281.
- ↑ Bellows-Riecken KH, Rhodes RE (February 2008). "A birth of inactivity? A review of physical activity and parenthood". Preventive Medicine (Review). 46 (2): 99–110. doi:10.1016/j.ypmed.2007.08.003. PMID 17919713.
- ↑ "Obesity and Overweight" (PDF). World Health Organization. Archived (PDF) from the original on 13 July 2017. Retrieved 22 February 2009.
- ↑ 151.0 151.1 Caballero B (March 2001). "Introduction. Symposium: Obesity in developing countries: biological and ecological factors". The Journal of Nutrition (Review). 131 (3): 866S–870S. doi:10.1093/jn/131.3.866s. PMID 11238776.
- ↑ Smith E, Hay P, Campbell L, Trollor JN (September 2011). "A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment". Obesity Reviews (Review). 12 (9): 740–55. doi:10.1111/j.1467-789X.2011.00920.x. PMID 21991597.
- ↑ Farruggia MC, Small DM (September 2019). "Effects of adiposity and metabolic dysfunction on cognition: a review". Physiology & Behavior (Review). 208: 112578. doi:10.1016/j.physbeh.2019.112578. PMID 31194997.
- ↑ DiBaise JK, Zhang H, Crowell MD, Krajmalnik-Brown R, Decker GA, Rittmann BE (April 2008). "Gut microbiota and its possible relationship with obesity". Mayo Clinic Proceedings (Review). 83 (4): 460–9. doi:10.4065/83.4.460. PMID 18380992.
- ↑ "Antibiotics: repeated treatments before the age of two could be a factor in obesity". Prescrire International. 2018. Archived from the original on 2 July 2018. Retrieved 2 July 2018.
- ↑ 156.0 156.1 Cox LM, Blaser MJ (March 2015). "Antibiotics in early life and obesity". Nature Reviews. Endocrinology. 11 (3): 182–90. doi:10.1038/nrendo.2014.210. PMC 4487629. PMID 25488483.
- ↑ Falagas ME, Kompoti M (July 2006). "Obesity and infection". The Lancet. Infectious Diseases (Review). 6 (7): 438–46. doi:10.1016/S1473-3099(06)70523-0. PMID 16790384.
- ↑ 158.0 158.1 Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA (May 2008). "Meta-analysis of short sleep duration and obesity in children and adults". Sleep. 31 (5): 619–26. doi:10.1093/sleep/31.5.619. PMC 2398753. PMID 18517032.
- ↑ Miller MA, Kruisbrink M, Wallace J, Ji C, Cappuccio FP (April 2018). "Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies". Sleep. 41 (4). doi:10.1093/sleep/zsy018. PMID 29401314.
- ↑ Horne, J (May 2011). "Obesity and short sleep: unlikely bedfellows?". Obesity Reviews. 12 (5): e84–94. doi:10.1111/j.1467-789X.2010.00847.x. PMID 21366837.
- ↑ 161.0 161.1 Gerlach G, Herpertz S, Loeber S (January 2015). "Personality traits and obesity: a systematic review". Obesity Reviews. 16 (1): 32–63. doi:10.1111/obr.12235. PMID 25470329.
- ↑ Jokela M, Hintsanen M, Hakulinen C, Batty GD, Nabi H, Singh-Manoux A, Kivimäki M (April 2013). "Association of personality with the development and persistence of obesity: a meta-analysis based on individual-participant data". Obesity Reviews. 14 (4): 315–23. doi:10.1111/obr.12007. PMC 3717171. PMID 23176713.
- ↑ Cacioppo, J.; Hawkley, L. (2010). "Loneliness Matters: A Theorectical and Empirical Review of Consequences and Mechanisms". Annals of Behavioral Medicine. 40 (2): 218–227. doi:10.1007/s12160-010-9210-8. PMC 3874845. PMID 20652462.
- ↑ 164.0 164.1 164.2 164.3 Flier JS (January 2004). "Obesity wars: molecular progress confronts an expanding epidemic". Cell (Review). 116 (2): 337–50. doi:10.1016/S0092-8674(03)01081-X. PMID 14744442.
- ↑ Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM (December 1994). "Positional cloning of the mouse obese gene and its human homologue". Nature (Research Support). 372 (6505): 425–32. Bibcode:1994Natur.372..425Z. doi:10.1038/372425a0. PMID 7984236.
- ↑ Boulpaep, Emile L.; Boron, Walter F. (2003). Medical physiology: A cellular and molecular approach. Philadelphia: Saunders. p. 1227. ISBN 978-0-7216-3256-8.
- ↑ World Health Organization (2000). Obesity: preventing and managing the global epidemic (Report). World Health Organization. pp. 1–2. Archived from the original on 28 August 2021. Retrieved 1 February 2014.
- ↑ Satcher D (2001). The Surgeon General's Call to Action to Prevent and Decrease Overweight and Obesity. Publications and Reports of the Surgeon General. U.S. Dept. of Health and Human Services, Public Health Service, Office of Surgeon General. ISBN 978-0-16-051005-2. Archived from the original on 7 June 2010. Retrieved 4 August 2020.
- ↑ Moyer VA (September 2012). "Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine (Practice Guideline). 157 (5): 373–8. doi:10.7326/0003-4819-157-5-201209040-00475. PMID 22733087.
- ↑ Brook Barnes (18 July 2007). "Limiting Ads of Junk Food to Children". New York Times. Archived from the original on 18 September 2019. Retrieved 24 July 2008.
- ↑ "Fewer Sugary Drinks Key to Weight Loss". U.S. Department of Health and Human Services. Archived from the original on 16 November 2012. Retrieved 18 October 2009.
- ↑ "WHO urges global action to curtail consumption and health impacts of sugary drinks". WHO. Archived from the original on 12 October 2016. Retrieved 13 October 2016.
- ↑ Brennan Ramirez LK, Hoehner CM, Brownson RC, Cook R, Orleans CT, Hollander M, Barker DC, Bors P, Ewing R, Killingsworth R, Petersmarck K, Schmid T, Wilkinson W (December 2006). "Indicators of activity-friendly communities: an evidence-based consensus process". American Journal of Preventive Medicine (Research Support). 31 (6): 515–24. doi:10.1016/j.amepre.2006.07.026. PMID 17169714.
- ↑ Crockett RA, King SE, Marteau TM, Prevost AT, Bignardi G, Roberts NW, Stubbs B, Hollands GJ, Jebb SA (27 February 2018). "Nutritional Labelling for Healthier Food or Non-Alcoholic Drink Purchasing and Consumption". Cochrane Database of Systematic Reviews (2): CD009315. doi:10.1002/14651858.CD009315.pub2. PMC 5846184. PMID 29482264.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ National Heart, Lung, and Blood Institute (1998). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults (PDF). International Medical Publishing, Inc. ISBN 978-1-58808-002-8. Archived (PDF) from the original on 21 June 2014. Retrieved 4 August 2020.
- ↑ Storing up problems; the medical case for a slimmer nation. London: Royal College of Physicians. 11 February 2004. ISBN 978-1-86016-200-8.
- ↑ Great Britain Parliament House of Commons Health Committee (May 2004). Obesity – Volume 1 – HCP 23-I, Third Report of session 2003–04. Report, together with formal minutes. London: TSO (The Stationery Office). ISBN 978-0-215-01737-6. Archived from the original on 29 June 2019. Retrieved 17 December 2007.
- ↑ "Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children" (PDF). National Institute for Health and Clinical Excellence(NICE). National Health Services (NHS). 2006. Archived (PDF) from the original on 6 December 2013. Retrieved 8 April 2009.
- ↑ Wanless, Derek; Appleby, John; Harrison, Anthony; Patel, Darshan (2007). Our Future Health Secured? A review of NHS funding and performance. London: The King's Fund. ISBN 978-1-85717-562-2.
- ↑ Sacks G, Swinburn B, Lawrence M (January 2009). "Obesity Policy Action framework and analysis grids for a comprehensive policy approach to reducing obesity". Obesity Reviews. 10 (1): 76–86. doi:10.1111/j.1467-789X.2008.00524.X. PMID 18761640. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ 181.0 181.1 181.2 US Department of Health and Human Services. (2017). "2015–2020 Dietary Guidelines for Americans - health.gov". health.gov. Skyhorse Publishing Inc. Archived from the original on 6 November 2019. Retrieved 30 September 2019.
- ↑ Arnett, Donna K.; Blumenthal, Roger S.; Albert, Michelle A.; Buroker, Andrew B.; Goldberger, Zachary D.; Hahn, Ellen J.; Himmelfarb, Cheryl D.; Khera, Amit; Lloyd-Jones, Donald; McEvoy, J. William; Michos, Erin D.; Miedema, Michael D.; Muñoz, Daniel; Smith, Sidney C.; Virani, Salim S.; Williams, Kim A.; Yeboah, Joseph; Ziaeian, Boback (17 March 2019). "2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease". Circulation. 140 (11): e596–e646. doi:10.1161/CIR.0000000000000678. PMID 30879355.
- ↑ Strychar I (January 2006). "Diet in the management of weight loss". CMAJ (Review). 174 (1): 56–63. doi:10.1503/cmaj.045037. PMC 1319349. PMID 16389240.
- ↑ Shick SM, Wing RR, Klem ML, McGuire MT, Hill JO, Seagle H (April 1998). "Persons successful at long-term weight loss and maintenance continue to consume a low-energy, low-fat diet". Journal of the American Dietetic Association. 98 (4): 408–13. doi:10.1016/S0002-8223(98)00093-5. PMID 9550162.
- ↑ Tate DF, Jeffery RW, Sherwood NE, Wing RR (April 2007). "Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain?". The American Journal of Clinical Nutrition (Randomized Controlled Trial). 85 (4): 954–9. doi:10.1093/ajcn/85.4.954. PMID 17413092.
- ↑ Thomas JG, Bond DS, Phelan S, Hill JO, and Wing RR (January 1, 2014). "Weight-Loss Maintenance for 10 Years in the National Weight Control Registry". American Journal of Preventive Medicine. 46 (1): 17–23. doi:10.1016/j.amepre.2013.08.019. PMID 24355667.
- ↑ 187.0 187.1 187.2 Yannakoulia M, Poulimeneas D, Mamalaki E, Anastasiou CA (March 1, 2019). "Dietary modifications for weight loss and weight loss maintenance". Metabolism. 92: 153–162. doi:10.1016/j.metabol.2019.01.001. PMID 30625301.
- ↑ US Preventive Services Task Force (2018). "Behavioral Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults US Preventive Services Task Force Recommendation Statement". JAMA. 320 (11): 1163–1171. doi:10.1001/jama.2018.13022. PMID 30326502.
- ↑ Gibson AA, Sainsbury A (July 11, 2017). "Strategies to Improve Adherence to Dietary Weight Loss Interventions in Research and Real-World Settings". Behav Sci (Basel). 7 (3): 44. doi:10.3390/bs7030044. PMID 28696389.
- ↑ 190.0 190.1 190.2 190.3 Services, Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU) (1987). "Dietary treatment of obesity". Annals of the New York Academy of Sciences. 499 (1): 250–263. Bibcode:1987NYASA.499..250B. doi:10.1111/j.1749-6632.1987.tb36216.x. PMID 3300485. Archived from the original on 26 March 2016. Retrieved 17 June 2016.
- ↑ Johnston BC, Kanters S, Bandayrel K, Wu P, Naji F, Siemieniuk RA, Ball GD, Busse JW, Thorlund K, Guyatt G, Jansen JP, Mills EJ (September 2014). "Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis". JAMA. 312 (9): 923–33. doi:10.1001/jama.2014.10397. PMID 25182101.
- ↑ Naude CE, Schoonees A, Senekal M, Young T, Garner P, Volmink J (2014). "Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis". PLOS One (Research Support). 9 (7): e100652. Bibcode:2014PLoSO...9j0652N. doi:10.1371/journal.pone.0100652. PMC 4090010. PMID 25007189.
- ↑ Wing RR, Phelan S (July 2005). "Long-term weight loss maintenance". The American Journal of Clinical Nutrition (Review). 82 (1 Suppl): 222S–225S. doi:10.1093/ajcn/82.1.222S. PMID 16002825.
- ↑ Thangaratinam S, Rogozinska E, Jolly K, Glinkowski S, Roseboom T, Tomlinson JW, Kunz R, Mol BW, Coomarasamy A, Khan KS (May 2012). "Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence". BMJ (Meta-analysis). 344: e2088. doi:10.1136/bmj.e2088. PMC 3355191. PMID 22596383.
- ↑ LeFevre ML (October 2014). "Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 161 (8): 587–93. doi:10.7326/M14-1796. PMID 25155419.
- ↑ 196.0 196.1 196.2 Heymsfield SB, Wadden TA (January 2017). "Mechanisms, Pathophysiology, and Management of Obesity". The New England Journal of Medicine. 376 (3): 254–266. doi:10.1056/NEJMra1514009. PMID 28099824.
- ↑ 197.0 197.1 Wolfe SM (August 2013). "When EMA and FDA decisions conflict: differences in patients or in regulation?". BMJ. 347: f5140. doi:10.1136/bmj.f5140. PMID 23970394. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ "Belviq, Belviq XR (lorcaserin) by Eisai: Drug Safety Communication - FDA Requests Withdrawal of Weight-Loss Drug". FDA. 13 February 2020. Archived from the original on 24 February 2020. Retrieved 18 February 2020.
- ↑ Rucker D, Padwal R, Li SK, Curioni C, Lau DC (December 2007). "Long term pharmacotherapy for obesity and overweight: updated meta-analysis". BMJ (Meta-analysis). 335 (7631): 1194–9. doi:10.1136/bmj.39385.413113.25. PMC 2128668. PMID 18006966.
- ↑ Wood, Shelley. "Diet Drug Orlistat Linked to Kidney, Pancreas Injuries". Medscape. Medscape News. Archived from the original on 10 May 2012. Retrieved 26 April 2011.
- ↑ Yanovski SZ, Yanovski JA (January 2014). "Long-term drug treatment for obesity: a systematic and clinical review". JAMA (Review). 311 (1): 74–86. doi:10.1001/jama.2013.281361. PMC 3928674. PMID 24231879.
- ↑ Wiggins, T; Guidozzi, N; Welbourn, R; Ahmed, AR; Markar, SR (July 2020). "Association of bariatric surgery with all-cause mortality and incidence of obesity-related disease at a population level: A systematic review and meta-analysis". PLoS medicine. 17 (7): e1003206. doi:10.1371/journal.pmed.1003206. PMID 32722673.
- ↑ 203.0 203.1 Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA (March 2014). "The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012". JAMA Surgery (Meta-analysis, Review). 149 (3): 275–87. doi:10.1001/jamasurg.2013.3654. PMC 3962512. PMID 24352617.
- ↑ Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, Lystig T, Sullivan M, Bouchard C, Carlsson B, Bengtsson C, Dahlgren S, Gummesson A, Jacobson P, Karlsson J, Lindroos AK, Lönroth H, Näslund I, Olbers T, Stenlöf K, Torgerson J, Agren G, Carlsson LM (August 2007). "Effects of bariatric surgery on mortality in Swedish obese subjects". The New England Journal of Medicine (Research Support). 357 (8): 741–52. doi:10.1056/NEJMoa066254. PMID 17715408. Archived from the original on 28 August 2021. Retrieved 4 August 2020.
- ↑ Weintraub, Karen. "New allies in war on weight". The Boston Globe. The Boston Globe. Archived from the original on 30 June 2014. Retrieved 30 June 2014.
- ↑ 206.0 206.1 206.2 Haslam D (March 2007). "Obesity: a medical history". Obesity Reviews (Review). 8 Suppl 1: 31–6. doi:10.1111/j.1467-789X.2007.00314.x. PMID 17316298.
- ↑ 207.0 207.1 "Obesity and overweight". World Health Organization. Archived from the original on 10 April 2009. Retrieved 8 April 2009.
- ↑ Hales CM, Carroll MD, Fryar CD, Ogden CL (October 2017). "Prevalence of Obesity Among Adults and Youth: United States, 2015–2016". NCHS Data Brief (288): 1–8. PMID 29155689.
- ↑ Seidell 2005 p.5
- ↑ Howard NJ, Taylor AW, Gill TK, Chittleborough CR (March 2008). "Severe obesity: Investigating the socio-demographics within the extremes of body mass index". Obesity Research & Clinical Practice. 2 (1): I–II. doi:10.1016/j.orcp.2008.01.001. PMID 24351678.
- ↑ Tjepkema M (6 July 2005). "Measured Obesity–Adult obesity in Canada: Measured height and weight". Nutrition: Findings from the Canadian Community Health Survey. Ottawa, Ontario: Statistics Canada. Archived from the original on 8 November 2016. Retrieved 4 August 2020.
- ↑ "Obesity Update 2017" (PDF). Organisation for Economic Co-operation and Development. Archived (PDF) from the original on 15 October 2018. Retrieved 6 October 2018.
- ↑ "Online Etymology Dictionary: Obesity". Douglas Harper. Archived from the original on 6 September 2017. Retrieved 31 December 2008.
- ↑ "Obesity, n". Oxford English Dictionary 2008. Archived from the original on 11 January 2008. Retrieved 21 March 2009.
- ↑ 215.0 215.1 Bloomgarden ZT (November 2003). "Prevention of obesity and diabetes". Diabetes Care (Review). 26 (11): 3172–8. doi:10.2337/diacare.26.11.3172. PMID 14578257. Archived from the original on 27 June 2017. Retrieved 4 August 2020.
- ↑ 216.0 216.1 "History of Medicine: Sushruta – the Clinician – Teacher par Excellence" (PDF). Dwivedi, Girish & Dwivedi, Shridhar. 2007. Archived from the original (PDF) on 10 October 2008. Retrieved 19 September 2008.
- ↑ Theodore Mazzone; Giamila Fantuzzi (2006). Adipose Tissue And Adipokines in Health And Disease (Nutrition and Health). Totowa, NJ: Humana Press. p. 222. ISBN 978-1-58829-721-1.
- ↑ Keller p. 49
- ↑ Gilman, Sander L (2004). Fat Boys: A Slim Book. University of Nebraska Press. p. 18. ISBN 978-0803221833.
tobias venner obesity.
- ↑ Breslow L (September 1952). "Public health aspects of weight control". American Journal of Public Health and the Nation's Health. 42 (9): 1116–20. doi:10.2105/AJPH.42.9.1116. PMC 1526346. PMID 12976585.
- ↑ 221.0 221.1 Puhl R, Brownell KD (December 2001). "Bias, discrimination, and obesity". Obesity Research (Review). 9 (12): 788–805. doi:10.1038/oby.2001.108. PMID 11743063.
- ↑ Rubinstein S, Caballero B (2000). "Is Miss America an undernourished role model?". JAMA (Letter). 283 (12): 1569. doi:10.1001/jama.283.12.1569. PMID 10735392.
- ↑ 223.0 223.1 Johnson F, Cooke L, Croker H, Wardle J (July 2008). "Changing perceptions of weight in Great Britain: comparison of two population surveys". BMJ. 337: a494. doi:10.1136/bmj.a494. PMC 2500200. PMID 18617488. Archived from the original on 22 February 2009. Retrieved 4 August 2020.
- ↑ Fumento, Michael (1997). The Fat of the Land: Our Health Crisis and How Overweight Americans Can Help Themselves. Penguin (Non-Classics). p. 126. ISBN 978-0-14-026144-8.
- ↑ 225.0 225.1 Puhl R., Henderson K., and Brownell K. 2005 p.29
- ↑ Johansson E, Böckerman P, Kiiskinen U, Heliövaara M (March 2009). "Obesity and labour market success in Finland: the difference between having a high BMI and being fat". Economics and Human Biology. 7 (1): 36–45. doi:10.1016/j.ehb.2009.01.008. PMID 19249259.
- ↑ Cawley J, Meyerhoefer C (January 2012). "The medical care costs of obesity: an instrumental variables approach". Journal of Health Economics. 31 (1): 219–30. doi:10.1016/j.jhealeco.2011.10.003. PMID 22094013.
- ↑ Finkelstein EA, Fiebelkorn IA, Wang G (1 January 2003). "National medical spending attributable to overweight and obesity: How much, and who's paying". Health Affairs. Online (May): W3–219–W3–226. doi:10.1377/hlthaff.w3.219. PMID 14527256. Archived from the original on 25 November 2010. Retrieved 4 August 2020.
- ↑ "Obesity and overweight: Economic consequences". Centers for Disease Control and Prevention. 22 May 2007. Archived from the original on 23 August 2017. Retrieved 5 September 2007.
- ↑ Colagiuri S, Lee CM, Colagiuri R, Magliano D, Shaw JE, Zimmet PZ, Caterson ID (March 2010). "The cost of overweight and obesity in Australia". The Medical Journal of Australia (Comparative Study). 192 (5): 260–4. doi:10.5694/j.1326-5377.2010.tb03503.x. PMID 20201759. Archived from the original on 19 August 2011. Retrieved 4 August 2020.
- ↑ Cummings, Laura (5 February 2003). "The diet business: Banking on failure". BBC News. Archived from the original on 16 March 2019. Retrieved 25 February 2009.
- ↑ "Public health experts call for global food treaty". Financial Times. 27 January 2019. Archived from the original on 8 March 2019. Retrieved 7 March 2019.
- ↑ van Baal PH, Polder JJ, de Wit GA, Hoogenveen RT, Feenstra TL, Boshuizen HC, Engelfriet PM, Brouwer WB (February 2008). "Lifetime medical costs of obesity: prevention no cure for increasing health expenditure". PLOS Medicine (Comparative Study). 5 (2): e29. doi:10.1371/journal.pmed.0050029. PMC 2225430. PMID 18254654.
- ↑ Bakewell J (2007). "Bariatric furniture: Considerations for use". Int J Ther Rehabil. 14 (7): 329–33. doi:10.12968/ijtr.2007.14.7.23858. Archived from the original on 8 October 2011.
- ↑ Neovius K, Johansson K, Kark M, Neovius M (January 2009). "Obesity status and sick leave: a systematic review". Obesity Reviews (Review). 10 (1): 17–27. doi:10.1111/j.1467-789X.2008.00521.x. PMID 18778315.
- ↑ Ostbye T, Dement JM, Krause KM (April 2007). "Obesity and workers' compensation: results from the Duke Health and Safety Surveillance System". Archives of Internal Medicine (Research Support). 167 (8): 766–73. doi:10.1001/archinte.167.8.766. PMID 17452538.
- ↑ "Alabama "Obesity Penalty" Stirs Debate". Don Fernandez. Archived from the original on 17 July 2019. Retrieved 5 April 2009.
- ↑ Puhl R., Henderson K., and Brownell K. 2005 p.30
- ↑ Lisa DiCarlo (24 October 2002). "Why Airlines Can't Cut The Fat". Forbes.com. Archived from the original on 17 July 2019. Retrieved 23 July 2008.
- ↑ Dannenberg AL, Burton DC, Jackson RJ (October 2004). "Economic and environmental costs of obesity: the impact on airlines". American Journal of Preventive Medicine (Letter). 27 (3): 264. doi:10.1016/j.amepre.2004.06.004. PMID 15450642. Archived from the original on 6 August 2020. Retrieved 4 August 2020.
- ↑ Lauren Cox (2 July 2009). "Who Should Pay for Obese Health Care?". ABC News. Archived from the original on 17 July 2019. Retrieved 6 August 2012.
- ↑ 242.0 242.1 "109th U.S. Congress (2005–2006) H.R. 554: 109th U.S. Congress (2005–2006) H.R. 554: Personal Responsibility in Food Consumption Act of 2005". GovTrack.us. Archived from the original on 1 November 2008. Retrieved 24 July 2008.
- ↑ 243.0 243.1 Basulto, Dominic (20 June 2013). "A changing battlefield in the fight against fat". The Washington Post. Archived from the original on 2 September 2014. Retrieved 20 June 2013.
- ↑ "Obesity can be deemed a disability at work – EU court". Reuters. 18 December 2014. Archived from the original on 21 November 2015. Retrieved 18 December 2014.
- ↑ "What is NAAFA". National Association to Advance Fat Acceptance. Archived from the original on 12 March 2009. Retrieved 17 February 2009.
- ↑ "ISAA Mission Statement". International Size Acceptance Association. Archived from the original on 25 February 2009. Retrieved 17 February 2009.
- ↑ 247.0 247.1 Pulver, Adam (2007). An Imperfect Fit: Obesity, Public Health, and Disability Anti-Discrimination Law. Social Science Electronic Publishing. SSRN 1316106.
- ↑ Neumark-Sztainer D (March 1999). "The weight dilemma: a range of philosophical perspectives". International Journal of Obesity and Related Metabolic Disorders (Review). 23 Suppl 2: S31–7. doi:10.1038/sj.ijo.0800857. PMID 10340803.
- ↑ National Association to Advance Fat Acceptance (2008). "We come in all sizes". NAAFA. Archived from the original on 26 December 2018. Retrieved 29 July 2008.
- ↑ "International Size Acceptance Association – ISAA". International Size Acceptance Association. Archived from the original on 5 January 2009. Retrieved 13 January 2009.
- ↑ O’Connor, Anahad (9 August 2015). "Coca-Cola Funds Scientists Who Shift Blame for Obesity Away From Bad Diets". New York Times. Archived from the original on 26 October 2020. Retrieved 4 August 2020.
- ↑ Nestle M (November 2016). "Food Industry Funding of Nutrition Research: The Relevance of History for Current Debates". JAMA Internal Medicine. 176 (11): 1685–1686. doi:10.1001/jamainternmed.2016.5400. PMID 27618496. Archived from the original on 29 August 2021. Retrieved 4 August 2020.
- ↑ 253.0 253.1 Flynn MA, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, Tough SC (February 2006). "Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with 'best practice' recommendations". Obesity Reviews (Review). 7 Suppl 1: 7–66. doi:10.1111/j.1467-789X.2006.00242.x. PMID 16371076.
- ↑ Lawrence, Justin (February 2005). "Childhood Obesity". British Journal of Perioperative Nursing (United Kingdom). 15 (2): 84–90. doi:10.1177/175045890501500204. ISSN 1467-1026. PMID 15736809.
- ↑ Brownback, Sam (January 2008). "Confronting Childhood Obesity". The Annals of the American Academy of Political and Social Science. 615 (1): 219–221. doi:10.1177/0002716207308894. ISSN 0002-7162.
- ↑ Dollman J, Norton K, Norton L (December 2005). "Evidence for secular trends in children's physical activity behaviour". British Journal of Sports Medicine (Review). 39 (12): 892–7, discussion 897. doi:10.1136/bjsm.2004.016675. PMC 1725088. PMID 16306494.
- ↑ Metcalf B, Henley W, Wilkin T (September 2012). "Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54)". BMJ (Review, Meta-analysis). 345: e5888. doi:10.1136/bmj.e5888. PMID 23044984.
- ↑ Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, Olajide J, Mainardi GM, Corpeleijn E, O'Malley C, Beardsmore E, Al-Khudairy L, Baur L, Metzendorf MI, Demaio A, Ells LJ (June 2017). "Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years" (PDF). The Cochrane Database of Systematic Reviews. 6: CD012651. doi:10.1002/14651858.CD012651. PMC 6481885. PMID 28639319. Archived (PDF) from the original on 6 August 2020. Retrieved 4 August 2020.
- ↑ 259.0 259.1 Lund, Elizabeth M. (2006). "Prevalence and Risk Factors for Obesity in Adult Dogs from Private US Veterinary Practices" (PDF). Intern J Appl Res Vet Med. 4 (2): 177–86. Archived (PDF) from the original on 1 June 2019. Retrieved 4 August 2020.
- ↑ McGreevy PD, Thomson PC, Pride C, Fawcett A, Grassi T, Jones B (May 2005). "Prevalence of obesity in dogs examined by Australian veterinary practices and the risk factors involved". The Veterinary Record. 156 (22): 695–702. doi:10.1136/vr.156.22.695. PMID 15923551.
- ↑ Nijland ML, Stam F, Seidell JC (January 2010). "Overweight in dogs, but not in cats, is related to overweight in their owners". Public Health Nutrition. 13 (1): 102–6. doi:10.1017/S136898000999022X. PMID 19545467.
Cited sources
- Bhargava A, Guthrie JF (December 2002). "Unhealthy eating habits, physical exercise and macronutrient intakes are predictors of anthropometric indicators in the Women's Health Trial: Feasibility Study in Minority Populations". The British Journal of Nutrition (Randomized Controlled Trial). 88 (6): 719–28. doi:10.1079/BJN2002739. PMID 12493094.
- Bhargava A (August 2006). "Fiber intakes and anthropometric measures are predictors of circulating hormone, triglyceride, and cholesterol concentrations in the women's health trial". The Journal of Nutrition (Research Support). 136 (8): 2249–54. doi:10.1093/jn/136.8.2249. PMID 16857849.
- Jebb S. and Wells J. Measuring body composition in adults and children In:Peter G. Kopelman; Ian D. Caterson; Michael J. Stock; William H. Dietz (2005). Clinical obesity in adults and children: In Adults and Children. Blackwell Publishing. pp. 12–28. ISBN 978-1-4051-1672-5.
- Kopelman P., Caterson I. An overview of obesity management In:Peter G. Kopelman; Ian D. Caterson; Michael J. Stock; William H. Dietz (2005). Clinical obesity in adults and children: In Adults and Children. Blackwell Publishing. pp. 319–26. ISBN 978-1-4051-1672-5.
- National Heart, Lung, and Blood Institute (NHLBI) (1998). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults (PDF). International Medical Publishing, Inc. ISBN 978-1-58808-002-8. Archived (PDF) from the original on 21 June 2014. Retrieved 4 August 2020.
- "Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children" (PDF). National Institute for Health and Clinical Excellence(NICE). National Health Services (NHS). 2006. Archived (PDF) from the original on 6 December 2013. Retrieved 8 April 2009.
- Puhl R., Henderson K., and Brownell K. Social consequences of obesity In:Peter G. Kopelman; Ian D. Caterson; Michael J. Stock; William H. Dietz (2005). Clinical obesity in adults and children: In Adults and Children. Blackwell Publishing. pp. 29–45. ISBN 978-1-4051-1672-5.
- Seidell JC. Epidemiology – definition and classification of obesity In:Peter G. Kopelman; Ian D. Caterson; Michael J. Stock; William H. Dietz (2005). Clinical obesity in adults and children: In Adults and Children. Blackwell Publishing. pp. 3–11. ISBN 978-1-4051-1672-5.
- World Health Organization (WHO) (2000). Technical report series 894: Obesity: Preventing and managing the global epidemic (PDF). Geneva: World Health Organization. ISBN 978-92-4-120894-9. Archived from the original (PDF) on 1 May 2015. Retrieved 10 May 2006.
Further reading
- Obesity at Curlie
- "Obesity 2015". The Lancet. 2015. Archived from the original on 13 August 2020. Retrieved 4 August 2020.
- Keller, Kathleen (2008). Encyclopedia of Obesity. Thousand Oaks, Calif: Sage Publications, Inc. ISBN 978-1-4129-5238-5.
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- Pages with obsolete Vega graphs
- Pages with graphs
- CS1 errors: missing periodical
- CS1 maint: unrecognized language
- CS1: long volume value
- CS1 maint: multiple names: authors list
- Articles with hatnote templates targeting a nonexistent page
- Good articles
- Articles with medical app sidebar
- Articles with Curlie links
- Subject bar templates with redlinked portals
- Obesity
- Bariatrics
- Body shape
- Nutrition
- RTT(full)
- RTTNEURO
- Amphetamine
- RTT