Viral hemorrhagic fever
| Viral hemorrhagic fever | |
|---|---|
| Other names: viral haemorrhagic fever | |
 | |
| Two nurses standing near Mayinga N'Seka, a nurse with Ebola virus disease in the 1976 outbreak in Zaire. N'Seka died a few days later due to severe internal hemorrhage. | |
| Specialty | Infectious disease |
Viral hemorrhagic fevers (VHFs) are a diverse group of animal and human illnesses in which fever and hemorrhage are caused by a viral infection.[1] VHFs may be caused by four distinct families of RNA viruses: the families Filoviridae, Flaviviridae, Bunyavirales and Arenaviridae.[2] All types of VHF are characterized by fever and bleeding disorders and all can progress to high fever, shock and death in many cases. Some of the VHF agents cause relatively mild illnesses, while others, such as Ebola virus, can cause severe, life-threatening disease.[2]
Signs and symptoms
Signs and symptoms of VHFs include, by definition fever and bleeding:[2][3]
- Flushing of the face and chest, small red or purple spots (petechiae), bleeding, and circulatory shock.
- Malaise, muscle pain, headache, vomiting, and diarrhea occur frequently.
The severity of symptoms varies with the type of virus. Capillary leak, bleeding diathesis, and circulatory compromise leading to shock, appears in a majority of people with filoviral hemorrhagic fevers , Crimean–Congo hemorrhagic fever , and the South American hemorrhagic fevers caused by arenaviruses.[2][4]
Causes
Four families of RNA viruses have been recognised as being able to cause hemorrhagic fevers.[2]
- Flaviviridae family
- Dengue virus - Dengue fever
- Kyasanur forest disease virus - Kyasanur forest disease
- Omsk hemorrhagic fever virus - Omsk hemorrhagic fever
- Yellow fever virus - Yellow fever
- Arenaviridae family
- Guanarito virus - Venezuelan hemorrhagic fever
- Lassa virus - Lassa fever
- Lymphocytic choriomeningitis virus - Lymphocytic choriomeningitis
- Machupo virus - Bolivian hemorrhagic fever

- Bunyaviridae family
- Crimean-Congo hemorrhagic virus - Crimean-Congo hemorrhagic fever
- Dobrava-Belgrade virus - Hemorrhagic fever with renal syndrome
- Hantaan virus - Hemorrhagic fever with renal syndrome
- Rift Valley fever virus - Rift Valley fever
- Saaremaa virus - Hemorrhagic fever with renal syndrome
- Sin Nombre virus - Hantavirus pulmonary syndrome
- Filoviridae family
- Bundibugyo ebolavirus - EVD
- Marburg marburgvirus - Marburg hemorrhagic fever
- Sudan ebolavirus - EVD
- Taï Forest ebolavirus - EVD
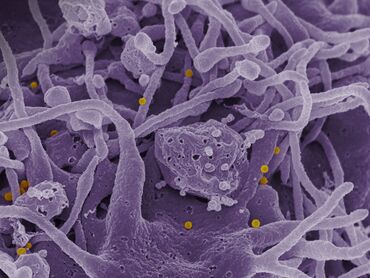
- Zaire ebolavirus - EVD
The pathogen that caused the cocoliztli epidemics in Mexico of 1545 and 1576 is still unknown, and the 1545 epidemic may have been bacterial rather than viral.[5][6]
Pathophysiology
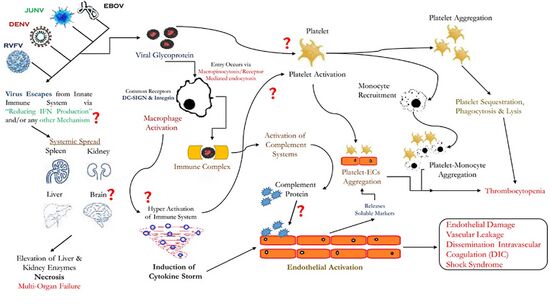
Different hemorrhagic fever viruses act on the body in different ways, resulting in different symptoms. In most VHFs, it is likely that several mechanisms contribute to symptoms, including liver damage, disseminated intravascular coagulation , and bone marrow dysfunction. In DIC, small blood clots form in blood vessels throughout the body, removing platelets necessary for clotting from the bloodstream and reducing clotting ability. [8][9]
DIC is thought to cause bleeding in Rift Valley, Marburg, and Ebola fevers. For filoviral hemorrhagic fevers, there are four general mechanisms of pathogenesis. The first mechanism is dissemination of virus due to suppressed responses by macrophages and dendritic cell. The second mechanism is prevention of antigen specific immune response. The third mechanism is apoptosis of lymphocytes. The fourth mechanism is when infected macrophages interact with toxic cytokines, leading to diapedesis and coagulation deficiency. From the vascular perspective, the virus will infect vascular endothelial cells, leading to the reorganization of the VE-cadherin catenin complex. This reorganization creates intercellular gaps in endothelial cells. The gaps lead to increased endothelial permeability and allow blood to escape from the vascular circulatory system.[10][4][11][12]
The reasons for variation among people infected with the same virus are unknown but stem from a complex system of virus-host interactions. Dengue fever becomes more virulent during a second infection by means of antibody-dependent enhancement. After the first infection, macrophages display antibodies on their cell membranes specific to the dengue virus. By attaching to these antibodies, dengue viruses from a second infection are better able to infect the macrophages, thus reducing the immune system's ability to fight off infection.[10][2][13]
Diagnosis
Definitive diagnosis is usually made at a reference laboratory with advanced biocontainment capabilities. The findings of laboratory investigation vary somewhat between the viruses, in some cases, there is a decrease in the total white cell count, a decrease in the platelet count, an increase in the blood serum liver enzymes.[2][14][15] Additionally there is a reduced blood clotting ability measured as an increase in both the prothrombin (PT) and activated partial thromboplastin times (PTT). The serum urea and creatine may be raised but this is dependent on the hydration status of the patient. The bleeding time tends to be prolonged.[16][2][14]
Prevention

With the exception of yellow fever vaccine and Ebola vaccines, vaccines for VHF-associated viruses are generally not available. Post-exposure prophylactic (preventive) ribavirin may be effective for some bunyavirus and arenavirus infections.[17][18]
VHF isolation guidelines dictate that all VHF patients (with the exception of dengue patients) should be cared for using strict contact precautions, including hand hygiene, double gloves, gowns, shoe and leg coverings, and face shield or goggles. Lassa, CCHF, Ebola, and Marburg viruses may be particularly prone to nosocomial (hospital-based) spread. Airborne precautions should be utilized including, at a minimum, a fit-tested, HEPA filter-equipped respirator (such as an N-95 mask), a battery-powered, air-purifying respirator, or a positive pressure supplied air respirator to be worn by personnel coming within 1,8 meter (six feet) of a VHF patient. Groups of patients should be cohorted (sequestered) to a separate building or a ward with an isolated air-handling system. Environmental decontamination is typically accomplished with hypochlorite (e.g. bleach) or phenolic disinfectants.[19]
Management
In 2020, the FDA approved Inmazeb a combination of three monoclonal antibodies and Ebanga a single monoclonal antibody for treating Zaire ebolavirus (disease infection)[20] Medical management of VHF patients may require intensive supportive care. Antiviral therapy with intravenous ribavirin may be useful in Bunyaviridae and Arenaviridae infections,[21] specifically, Lassa fever, RVF,and CCHF and can be used only under an experimental protocol as IND approved by the U.S. Food and Drug Administration (FDA).[21][2][22]
Epidemiology

The epidemiology of viral hemorrhagic fevers have been shown to be as follows:
- Cocoliztli in Mexico 1545 and 1576.[5]
- The Great Yellow Fever Epidemic of 1793 in Philadelphia, PA, US. Nearly 10% of the population of 50,000 succumbed to the disease.[23]
- Mékambo in Gabon is the site of several outbreaks of Ebola virus disease.[24]
- Orientale Province, Democratic Republic of the Congo villages of Durba and Watsa were the epicenter of the 1998–2000 outbreak of Marburg virus disease.[25]
- Uíge Province in Angola was the site of another outbreak of Marburg virus disease in 2005, the largest one to date of this disease.[26]
- A VHF outbreak in the village of Mweka, Democratic Republic of the Congo (DRC) that started in August 2007, and that has killed 103 people (100 adults and three children), has been shown to be caused (at least partially) by Ebola virus.[27]
- A viral hemorrhagic fever is a possible cause of the Plague of Athens during the Peloponnesian War.[28]
- The initial, and currently only, outbreak of Lujo virus in September–October 2008 left 4/5 patients dead.[29]
- The 2014 West Africa Ebola outbreak, which was the biggest outbreak in history.[30]
Society and culture
Biowarfare potential
The VHF viruses are spread in a variety of ways. Some may be transmitted to humans through a respiratory route.[31] The virus is considered by military medical planners to have a potential for aerosol dissemination, weaponization, or likelihood for confusion with similar agents that might be weaponized.[32][33]
See also
References
- ↑ "What are VHFs? | Viral Hemorrhagic Fevers (VHFs) | CDC". www.cdc.gov. 3 September 2021. Archived from the original on 17 January 2022. Retrieved 26 February 2022.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Mangat, Rupinder; Louie, Ted (2022). "Viral Hemorrhagic Fevers". StatPearls. StatPearls Publishing. Archived from the original on 11 January 2022. Retrieved 27 February 2022.
- ↑ "Hemorrhagic Fevers". medlineplus.gov. Archived from the original on 30 December 2021. Retrieved 27 February 2022.
- ↑ 4.0 4.1 Basler, Christopher F. (2017). "Molecular Pathogenesis of Viral Hemorrhagic Fever". Seminars in immunopathology. 39 (5): 551–561. doi:10.1007/s00281-017-0637-x. ISSN 1863-2297. Archived from the original on 3 March 2022. Retrieved 3 March 2022.
- ↑ 5.0 5.1 Acuna-Soto R, Stahle DW, Cleaveland MK, Therrell MD (April 2002). "Megadrought and megadeath in 16th century Mexico". Emerging Infect. Dis. 8 (4): 360–62. doi:10.3201/eid0804.010175. PMC 2730237. PMID 11971767.
- ↑ France-Presse, Agence (2018-01-16). "500 years later, scientists discover what probably killed the Aztecs". The Guardian. Archived from the original on 2021-11-11. Retrieved 2021-11-17.
- ↑ Mariappan, Vignesh; Pratheesh, Pooja; Shanmugam, Lokesh; Rao, S. R.; Pillai, Agieshkumar Balakrishna (1 January 2021). "Viral hemorrhagic fever: Molecular pathogenesis and current trends of disease management-an update". Current Research in Virological Science. 2: 100009. doi:10.1016/j.crviro.2021.100009. ISSN 2666-478X.
- ↑ Paessler, Slobodan; Walker, David H. (24 January 2013). "Pathogenesis of the viral hemorrhagic fevers". Annual Review of Pathology. 8: 411–440. doi:10.1146/annurev-pathol-020712-164041. ISSN 1553-4014. Archived from the original on 3 March 2022. Retrieved 4 March 2022.
- ↑ "Disseminated Intravascular Coagulation | NHLBI, NIH". www.nhlbi.nih.govNIH.gov. Archived from the original on 17 April 2021. Retrieved 7 March 2022.
- ↑ 10.0 10.1 Marty, Aileen M.; Jahrling, Peter B.; Geisbert, Thomas W. (June 2006). "Viral hemorrhagic fevers". Clinics in Laboratory Medicine. 26 (2): 345–386, viii. doi:10.1016/j.cll.2006.05.001. ISSN 0272-2712. Archived from the original on 2021-10-21. Retrieved 2022-03-01.
- ↑ Mahanty, Siddhartha; Bray, Mike (August 2004). "Pathogenesis of filoviral haemorrhagic fevers". The Lancet. Infectious Diseases. 4 (8): 487–498. doi:10.1016/S1473-3099(04)01103-X. ISSN 1473-3099. Archived from the original on 9 March 2022. Retrieved 10 March 2022.
- ↑ Srikiatkhachorn, Anon; Spiropoulou, Christina F. (2014). "Vascular events in viral hemorrhagic fevers: a comparative study of dengue and hantaviruses". Cell and Tissue Research. 355 (3): 621–633. doi:10.1007/s00441-014-1841-9. ISSN 0302-766X. Archived from the original on 10 March 2022. Retrieved 10 March 2022.
- ↑ Soo, Kuan-Meng; Khalid, Bahariah; Ching, Siew-Mooi; Chee, Hui-Yee (23 May 2016). "Meta-Analysis of Dengue Severity during Infection by Different Dengue Virus Serotypes in Primary and Secondary Infections". PLoS ONE. 11 (5): e0154760. doi:10.1371/journal.pone.0154760. ISSN 1932-6203. Archived from the original on 13 March 2022. Retrieved 12 March 2022.
- ↑ 14.0 14.1 Racsa, Lori D.; Kraft, Colleen S.; Olinger, Gene G.; Hensley, Lisa E. (15 January 2016). "Viral Hemorrhagic Fever Diagnostics". Clinical Infectious Diseases. 62 (2): 214–219. doi:10.1093/cid/civ792. Archived from the original on 21 January 2022. Retrieved 2 March 2022.
- ↑ Singh, Sunit K.; Ruzek, Daniel (19 April 2016). Viral Hemorrhagic Fevers. CRC Press. p. 407. ISBN 978-1-4398-8431-7. Archived from the original on 5 March 2022. Retrieved 5 March 2022.
- ↑ "Viral Hemorrhagic Fevers - Chapter 4 - 2020 Yellow Book | Travelers' Health | CDC". wwwnc.cdc.gov. Archived from the original on 2 February 2022. Retrieved 28 February 2022.
- ↑ Ergönül Ö, Keske Ş, Çeldir MG, Kara İA, Pshenichnaya N, Abuova G; et al. (2018). "Systematic Review and Meta-analysis of Postexposure Prophylaxis for Crimean-Congo Hemorrhagic Fever Virus among Healthcare Workers". Emerg Infect Dis. 24 (9): 1642–1648. doi:10.3201/eid2409.171709. PMC 6106438. PMID 30124196. Archived from the original on 2023-04-13. Retrieved 2021-11-17.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Hadi CM, Goba A, Khan SH, Bangura J, Sankoh M, Koroma S; et al. (2010). "Ribavirin for Lassa fever postexposure prophylaxis". Emerg Infect Dis. 16 (12): 2009–11. doi:10.3201/eid1612.100994. PMC 3294560. PMID 21122249. Archived from the original on 2023-04-13. Retrieved 2021-11-17.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Woods, Lt Col Jon B., ed. (2005). USAMRIID's Medical Management of Biological Casualties Handbook (PDF) (6th ed.). Fort Detrick MA: U.S. Army Medical Institute of Infectious Diseases. pp. 143–44. Archived from the original (PDF) on 2007-06-09. Retrieved 2007-06-09.
- ↑ "Treatment | Ebola (Ebola Virus Disease) | CDC". www.cdc.gov. 26 February 2021. Archived from the original on 22 January 2019. Retrieved 27 February 2022.
- ↑ 21.0 21.1 "Viral hemorrhagic fevers". webwiser.nlm.nih.gov. Archived from the original on 1 January 2022. Retrieved 1 March 2022.
- ↑ "Management of Patients With Suspected Viral Hemorrhagic Fever". www.cdc.gov. Archived from the original on 24 January 2022. Retrieved 8 March 2022.
- ↑ Smith, Mark A. (October 1996). "Andrew Brown's "Earnest Endeavor": The Federal Gazette's Role in Philadelphia's Yellow Fever Epidemic of 1793". Pennsylvania Magazine of History and Biography. University of Pennsylvania Press. 120 (4): 321–342. Archived from the original on October 24, 2019. Retrieved October 24, 2019 – via Pennsylvania State University Libraries.
- ↑ Nkoghe, D.; Formenty, P.; Leroy, E. M.; Nnegue, S.; Edou, S. Y. Obame; Ba, J. Iba; Allarangar, Y.; Cabore, J.; Bachy, C.; Andraghetti, R.; de Benoist, A. C.; Galanis, E.; Rose, A.; Bausch, D.; Reynolds, M.; Rollin, P.; Choueibou, C.; Shongo, R.; Gergonne, B.; Koné, L. M.; Yada, A.; Roth, C.; Mve, M. Toung (September 2005). "[Multiple Ebola virus haemorrhagic fever outbreaks in Gabon, from October 2001 to April 2002]". Bulletin De La Societe De Pathologie Exotique (1990). 98 (3): 224–229. ISSN 0037-9085. Archived from the original on 27 February 2021. Retrieved 3 March 2022.
- ↑ "Outbreak Table | Marburg Hemorrhagic Fever | CDC". www.cdc.gov. Archived from the original on 21 January 2015. Retrieved 3 March 2022.
- ↑ Towner, J. S.; Khristova, M. L.; Sealy, T. K.; Vincent, M. J.; Erickson, B. R.; Bawiec, D. A.; Hartman, A. L.; Comer, J. A.; Zaki, S. R.; Ströher, U.; Gomes Da Silva, F.; Del Castillo, F.; Rollin, P. E.; Ksiazek, T. G.; Nichol, S. T. (2006). "Marburgvirus Genomics and Association with a Large Hemorrhagic Fever Outbreak in Angola". Journal of Virology. 80 (13): 6497–516. doi:10.1128/JVI.00069-06. PMC 1488971. PMID 16775337.
- ↑ Leroy, Eric M.; Epelboin, Alain; Mondonge, Vital; Pourrut, Xavier; Gonzalez, Jean-Paul; Muyembe-Tamfum, Jean-Jacques; Formenty, Pierre (December 2009). "Human Ebola outbreak resulting from direct exposure to fruit bats in Luebo, Democratic Republic of Congo, 2007". Vector Borne and Zoonotic Diseases (Larchmont, N.Y.). 9 (6): 723–728. doi:10.1089/vbz.2008.0167. ISSN 1557-7759. Archived from the original on 26 November 2021. Retrieved 2 March 2022.
- ↑ Olson PE, Hames CS, Benenson AS, Genovese EN (1996). "The Thucydides syndrome: Ebola déjà vu? (or Ebola reemergent?)". Emerging Infect. Dis. 2 (2): 155–56. doi:10.3201/eid0202.960220. PMC 2639821. PMID 8964060.
- ↑ Briese, T.; Paweska, J.T.; McMullan, L.K.; Hutchison, S.K.; Street, C.; Palacios, G.; Khristova, M.L.; Weyer, J.; Swanepoel, R.; Engholm, M.; Nichol, S.T.; Lipkin, W.I. (2009). "Genetic Detection and Characterization of Lujo Virus, a New Hemorrhagic Fever–Associated Arenavirus from Southern Africa". PLOS Pathog. 5 (5): e1000455. doi:10.1371/journal.ppat.1000455. PMC 2680969. PMID 19478873.
- ↑ "Ebola virus disease". www.who.int. Archived from the original on 18 April 2018. Retrieved 3 March 2022.
- ↑ Christian, Michael D. (2013). "Biowarfare and Bioterrorism". Critical Care Clinics. 29 (3): 717–756. doi:10.1016/j.ccc.2013.03.015. ISSN 0749-0704. Archived from the original on 2 March 2022. Retrieved 1 March 2022.
- ↑ Woods 2005, p. 145
- ↑ Peters, C. (2000). "Are Hemorrhagic Fever Viruses Practical Agents for Biological Terrorism?". In Scheld, W. M.; Craig, W. A.; Hughes, J. M. (eds.). Emerging Infections. Vol. 4. Washington, D.C.: ASM Press. pp. 201–09. ISBN 978-1555811976.
External links
- "Viral Haemorrhagic Fever". The National Archives of United Kingdom. Public Health England (PHE). Archived from the original on 2014-07-14.
- "Viral Haemorrhagic Fevers". World Health Organization (WHO). United Nations (UN). Archived from the original on 2019-07-27. Retrieved 2021-11-17.
- "Viral Hemorrhagic Fevers (VHFs) Virus Families". National Center for Emerging and Zoonotic Infectious Diseases (NCEZID). U.S. Centers for Disease Control and Prevention (CDC). 2019-09-24. Archived from the original on 2014-10-29. Retrieved 2021-11-17.
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- CS1 maint: multiple names: authors list
- Articles with hatnote templates targeting a nonexistent page
- Missing redirects
- Use American English from March 2019
- Articles with invalid date parameter in template
- All Wikipedia articles written in American English
- Hemorrhagic fevers
- Animal viral diseases
- Neglected tropical diseases
- Tropical diseases