Myocarditis
| Myocarditis | |
|---|---|
| Other names: Inflammatory cardiomyopathy | |
 | |
| A microscope image of myocarditis at autopsy in a person with acute onset of heart failure | |
| Specialty | Cardiology |
| Symptoms | Shortness of breath, chest pain, decreased ability to exercise, irregular heartbeat[1] |
| Complications | Heart failure due to dilated cardiomyopathy, cardiac arrest[1] |
| Duration | Hours to months[1] |
| Causes | Usually viral infection, also bacterial infections, certain medications, toxins, autoimmune disorders[1][2] |
| Diagnostic method | Electrocardiogram, blood troponin, heart MRI, heart biopsy[1][2] |
| Treatment | Medications, implantable cardiac defibrillator, heart transplant[1][2] |
| Medication | ACE inhibitors, beta blockers, diuretics, corticosteroids, intravenous immunoglobulin[1][2] |
| Prognosis | Variable[3] |
| Frequency | 2.5 million with cardiomyopathy (2015)[4] |
| Deaths | 354,000 with cardiomyopathy (2015)[5] |
Myocarditis, also known as inflammatory cardiomyopathy, is inflammation of the heart muscle.[1] Symptoms can include shortness of breath, chest pain, decreased ability to exercise, and an irregular heartbeat.[1] The duration of problems can vary from hours to months.[1] Complications may include heart failure due to dilated cardiomyopathy or cardiac arrest.[1]
Myocarditis is most often due to a viral infection.[1] Other causes include bacterial infections, certain medications, toxins, and autoimmune disorders.[1][2] A diagnosis may be supported by an electrocardiogram (ECG), increased troponin, heart MRI, and occasionally a heart biopsy.[1][2] An ultrasound of the heart is important to rule out other potential causes such as heart valve problems.[2]
Treatment depends on both the severity and the cause.[1][2] Medications such as ACE inhibitors, beta blockers, and diuretics are often used.[1][2] A period of no exercise is typically recommended during recovery.[1][2] Corticosteroids or intravenous immunoglobulin (IVIG) may be useful in certain cases.[1][2] In severe cases an implantable cardiac defibrillator or heart transplant may be recommended.[1][2]
In 2013, about 1.5 million cases of acute myocarditis occurred.[6] While people of all ages are affected, the young are most often affected.[7] It is slightly more common in males than females.[1] Most cases are mild.[2] In 2015 cardiomyopathy, including myocarditis, resulted in 354,000 deaths up from 294,000 in 1990.[8][9] The initial descriptions of the condition are from the mid-1800s.[10]
Signs and symptoms
The signs and symptoms associated with myocarditis are varied, and relate either to the actual inflammation of the myocardium or to the weakness and dysfunction of the heart muscle that is secondary to the inflammation. While myocarditis may develop over periods ranging from hours to months, patients typically present with signs and symptoms that resemble heart failure, including the following:[1][11]
| Symptoms | Notes | Signs | Notes |
|---|---|---|---|
| Chest pain | Often described as sharp or stabbing in nature | Fever | Especially when infectious, e.g., from parvovirus B19 |
| Shortness of breath | Worse when lying down or in a prone position | Dull heart sounds | Muffling occurs with inflammation, especially with pericarditis |
| Palpitations | Feeling like one's heart is beating forcefully | Abnormal heart rhythm | Determined using an electrocardiogram |
| Dizziness or fainting | Can reflect inadequate blood flow to the brain | Damage to heart cells | Seen as elevated troponin and inflammation on imaging |
Since myocarditis is often due to a viral illness, many patients experience symptoms consistent with a recent viral infection including a fever, rash, loss of appetite, abdominal pain, vomiting, diarrhea, joint pains, and easily becoming tired.[12] Additionally, myocarditis is often associated with pericarditis, and many people with myocarditis present with signs and symptoms that suggest myocarditis and pericarditis at the same time.[13][12]
Children primarily present with the aforementioned symptoms associated with a viral infection.[11] Since they overlap with many other illnesses, this can make it more challenging to diagnose myocarditis in younger patients.[14] Later stages of the illness can involve the respiratory system and lead to increased work of breathing. These are often mistaken for asthma.[11][14]
Myocarditis can be distinguished as either fulminant or acute based on the severity of symptoms on presentation, as well as the time course over which symptoms develop and persist. This categorization can help predict the treatment, outcomes, and complications of myocarditis.
Fulminant myocarditis is defined as sudden and severe myocarditis that is associated with signs and symptoms of heart failure while at rest.[15] More specifically, fulminant myocarditis is characterized by a distinct, rapid onset of severe heart failure symptoms, such as shortness of breath and chest pain, that develop over the course of hours to days. Additionally, treatment requires the use of medications or mechanical devices to improve heart function.[15][16]
Acute non-fulminant myocarditis has a less distinct onset in contrast to fulminant myocarditis, and evolves over days to months.[16][17] While the symptoms of acute myocarditis overlap with those of fulminant myocarditis, they do not typically occur at rest, and treatment does not require the use of mechanical circulatory support.[17]
Causes
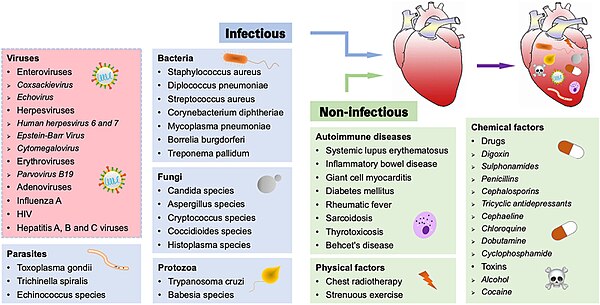
A large number of causes of myocarditis have been identified, but often a cause cannot be found. In Europe and North America, viruses are common culprits. Worldwide, however, the most common cause is Chagas' disease, an illness endemic to Central and South America that is due to infection by the protozoan Trypanosoma cruzi.[11] In viral myocarditis, the Coxsackie B family of the single-stranded RNA viruses, in particular the plus-strand RNA virus Coxsackievirus B3 and Coxsackievirus B5 are the most frequent cause.[18] Many of the causes listed below, particularly those involving protozoa, fungi, parasites, allergy, autoimmune disorders, and drugs are also causes of eosinophilic myocarditis.
Infections
- Viral (adenovirus, parvovirus B19, coxsackie virus, rubella virus, polio virus, Epstein-Barr virus, hepatitis C, and severe acute respiratory syndrome coronavirus 2)[19][20]
- Protozoan (Trypanosoma cruzi causing Chagas disease and Toxoplasma gondii)
- Bacterial (Brucella, Corynebacterium diphtheriae, gonococcus, Haemophilus influenzae, Actinomyces, Tropheryma whipplei, Vibrio cholerae, Borrelia burgdorferi, leptospirosis, and Rickettsia, Mycoplasma pneumoniae)
- Fungal (Aspergillus)
- Parasitic (ascaris, Echinococcus granulosus, Paragonimus westermani, schistosoma, Taenia solium, Trichinella spiralis, visceral larva migrans, and Wuchereria bancrofti)
Bacterial myocarditis is rare in patients without immunodeficiency.
Toxins
- Drugs, including alcohol, anthracyclines and some other forms of chemotherapy, and antipsychotics, e.g., clozapine, also some designer drugs such as mephedrone[21]
Immunologic
- Allergic (acetazolamide, amitriptyline)
- Rejection after a heart transplant
- Autoantigens (scleroderma, systemic lupus erythematosus, sarcoidosis, systemic vasculitis such as eosinophilic granulomatosis with polyangiitis, and granulomatosis with polyangiitis, Kawasaki disease, idiopathic hypereosinophilic syndrome)[22]
- Toxins (arsenic, toxic shock syndrome toxin, carbon monoxide, or snake venom)
- Heavy metals (copper or iron)
Physical agents
Mechanism
Most forms of myocarditis involve the infiltration of heart tissues by one or two types of pro-inflammatory blood cells, lymphocytes and macrophages plus two respective descendants of these cells, NK cells and macrophages. Eosinophilic myocarditis is a subtype of myocarditis in which cardiac tissue is infiltrated by another type of pro-inflammatory blood cell, the eosinophil. Eosinophilic myocarditis is further distinguished from non-eosinophilic myocarditis by having a different set of causes and recommended treatments.[24][25]
Coxsackie B, specifically B3 and B5, has been found to interact with coxsackievirus-adenovirus receptor (CAR) and decay-accelerating factor (DAF). However, other proteins have also been identified that allow Coxsackieviruses to bind to cardiac cells. The natural function of CAR and mechanism that the Coxsackievirus uses to infect the cardiac muscle is still unknown.[18] The mechanism by which coxsackie B viruses (CBVs) trigger inflammation is believed to be through the recognition of CBV virions by Toll-like receptors.[18]
Diagnosis


Myocarditis refers to an underlying process that causes inflammation and injury of the heart. It does not refer to inflammation of the heart as a consequence of some other insult. Many secondary causes, such as a heart attack, can lead to inflammation of the myocardium and therefore the diagnosis of myocarditis cannot be made by evidence of inflammation of the myocardium alone.[26][27]
Myocardial inflammation can be suspected on the basis of electrocardiographic (ECG) results, elevated C-reactive protein (CRP) and/or erythrocyte sedimentation rate (ESR), and increased IgM (serology) against viruses known to affect the myocardium. Markers of myocardial damage (troponin or creatine kinase cardiac isoenzymes) are elevated.[11]
The ECG findings most commonly seen in myocarditis are diffuse T wave inversions; saddle-shaped ST-segment elevations may be present (these are also seen in pericarditis).[11]
The gold standard is the biopsy of the myocardium, in general done in the setting of angiography. A small tissue sample of the endocardium and myocardium is taken and investigated. The cause for the myocarditis can be only diagnosed by a biopsy. Endomyocardial biopsy samples are assessed for histopathology (how the tissue looks like under the microscope: myocardial interstitium may show abundant edema and inflammatory infiltrate, rich in lymphocytes and macrophages. Focal destruction of myocytes explains the myocardial pump failure.[11] In addition samples may be assessed with immunohistochemistry to determine which types of immune cells are involved in the reaction and how they are distributed. Furthermore, PCR and/or RT-PCR may be performed to identify particular viruses. Finally, further diagnostic methods like microRNA assays and gene-expression profile may be performed.[citation needed]
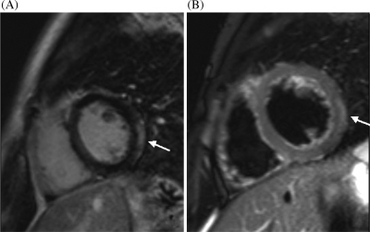
Cardiac magnetic resonance imaging (cMRI or CMR) has been shown to be very useful in diagnosing myocarditis by visualizing markers for inflammation of the myocardium.[28] Recently, consensus criteria for the diagnosis of myocarditis by CMR have been published.[29]
-
Ultrasound showing cardiogenic shock due to myocarditis[30]
-
Ultrasound showing cardiogenic shock due to myocarditis[30]
-
Ultrasound showing cardiogenic shock due to myocarditis[30]
Treatment
As with most viral infections, symptomatic treatment is the only form of therapy for most forms of myocarditis.[31] In the acute phase, supportive therapy, including bed rest, is indicated.
Medication
In people with symptoms, digoxin and diuretics may help. For people with moderate to severe dysfunction, cardiac function can be supported by use of inotropes such as milrinone in the acute phase, followed by oral therapy with ACE inhibitors when tolerated.
Systemic corticosteroids may have beneficial effects in people with proven myocarditis.[32] However, data on the usefulness of corticosteroids should be interpreted with caution, since 58% of adults recover spontaneously, while most studies on children lack control groups.[31]
A 2015 Cochrane review found no evidence of benefit of using intravenous immunoglobulin (IVIG) in adults and tentative benefit in certain children.[33] It is not recommended routinely until there is better evidence.[33]
Surgery
People who do not respond to conventional therapy may be candidates for bridge therapy with left ventricular assist devices. Heart transplantation is reserved for people who fail to improve with conventional therapy.[32]
Extracorporeal membrane oxygenation may be used in those who are about to go into cardiac arrest.[34]
Alternative medicine
Studies have shown no benefit for the use of herbal medicine on all cause mortality in viral myocarditis.[35]
Epidemiology
The exact incidence of myocarditis is unknown. However, in series of routine autopsies, 1–9% of all patients had evidence of myocardial inflammation. In young adults, up to 20% of all cases of sudden death are due to myocarditis.[11]
Among patients with HIV, myocarditis is the most common cardiac pathological finding at autopsy, with a prevalence of 50% or more.[36]
History
Cases of myocarditis have been documented as early as the 1600s,[37] but the term "myocarditis", implying an inflammatory process of the myocardium, was introduced by German physician Joseph Friedrich Sobernheim in 1837.[38] However, the term has been confused with other cardiovascular conditions, such as hypertension and ischemic heart disease.[39] Following admonition regarding the indiscriminate use of myocarditis as a diagnosis from authorities such as British cardiologist Sir Thomas Lewis and American cardiologist and a co-founder of the American Heart Association Paul White, myocarditis was under-diagnosed.[39]
Although myocarditis is clinically and pathologically clearly defined as "inflammation of the myocardium", its definition, classification, diagnosis, and treatment are subject to continued controversy, but endomyocardial biopsy has helped define the natural history of myocarditis and clarify clinicopathological correlations.[40]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 Cooper LT, Jr (9 April 2009). "Myocarditis". The New England Journal of Medicine. 360 (15): 1526–38. doi:10.1056/nejmra0800028. PMC 5814110. PMID 19357408.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Kindermann, I; Barth, C; Mahfoud, F; Ukena, C; Lenski, M; Yilmaz, A; Klingel, K; Kandolf, R; Sechtem, U; Cooper, LT; Böhm, M (28 February 2012). "Update on myocarditis". Journal of the American College of Cardiology. 59 (9): 779–92. doi:10.1016/j.jacc.2011.09.074. PMID 22361396.
- ↑ Stouffer, George; Runge, Marschall S.; Patterson, Cam (2010). Netter's Cardiology E-Book. Elsevier Health Sciences. p. 181. ISBN 9781437736502. Archived from the original on 2020-08-04. Retrieved 2019-05-21.
- ↑ GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ↑ GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ Global Burden of Disease Study 2013, Collaborators (22 August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMC 4561509. PMID 26063472.
- ↑ Willis, Monte; Homeister, Jonathon W.; Stone, James R. (2013). Cellular and Molecular Pathobiology of Cardiovascular Disease. Academic Press. p. 135. ISBN 9780124055254. Archived from the original on 2017-11-05.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ Cunha, Burke A. (2009). Infectious Diseases in Critical Care Medicine. CRC Press. p. 263. ISBN 9781420019605. Archived from the original on 2017-11-05.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 Feldman AM, McNamara D (November 2000). "Myocarditis". The New England Journal of Medicine. 343 (19): 1388–98. doi:10.1056/NEJM200011093431908. PMID 11070105.
- ↑ 12.0 12.1 "Myocarditis". The Lecturio Medical Concept Library. Archived from the original on 11 August 2021. Retrieved 11 August 2021.
- ↑ "Pericarditis". Lecturio. 23 July 2020. Archived from the original on 11 August 2021. Retrieved 11 August 2021.
- ↑ 14.0 14.1 Bejiqi, Ramush; Retkoceri, Ragip; Maloku, Arlinda; Mustafa, Aferdita; Bejiqi, Hana; Bejiqi, Rinor (4 January 2019). "The Diagnostic and Clinical Approach to Pediatric Myocarditis: A Review of the Current Literature". Open Access Macedonian Journal of Medical Sciences. 7 (1): 162–173. doi:10.3889/oamjms.2019.010. ISSN 1857-9655. PMC 6352488. PMID 30740183.
- ↑ 15.0 15.1 Sharma AN, Stultz JR, Bellamkonda N, Amsterdam EA (December 2019). "Fulminant Myocarditis: Epidemiology, Pathogenesis, Diagnosis, and Management". The American Journal of Cardiology. 124 (12): 1954–1960. doi:10.1016/j.amjcard.2019.09.017. PMID 31679645. S2CID 204061292.
- ↑ 16.0 16.1 Hang, Weijian; Chen, Chen; Seubert, John M.; Wang, Dao Wen (11 December 2020). "Fulminant myocarditis: a comprehensive review from etiology to treatments and outcomes". Signal Transduction and Targeted Therapy. 5 (1): 287. doi:10.1038/s41392-020-00360-y. ISSN 2059-3635. PMC 7730152. PMID 33303763.
- ↑ 17.0 17.1 Ammirati, Enrico; Veronese, Giacomo; Bottiroli, Maurizio; Wang, Dao Wen; Cipriani, Manlio; Garascia, Andrea; Pedrotti, Patrizia; Adler, Eric D.; Frigerio, Maria (August 2021). "Update on acute myocarditis". Trends in Cardiovascular Medicine. 31 (6): 370–379. doi:10.1016/j.tcm.2020.05.008. ISSN 1873-2615. PMC 7263216. PMID 32497572.
- ↑ 18.0 18.1 18.2 Marín-García, José (2007). Post-Genomic Cardiology. Academic Press. p. 416. ISBN 978-0123736987.
- ↑ Sheppard, Mary (2011). Practical Cardiovascular Pathology, 2nd edition. CRC Press. p. 197. ISBN 9780340981931. Archived from the original on 2018-09-17. Retrieved 2018-09-17.
- ↑ Kolata, Gina (27 March 2020). "A Heart Attack? No, It Was the Coronavirus". New York Times. Archived from the original on 4 April 2020. Retrieved 5 April 2020.
- ↑ Nicholson PJ, Quinn MJ, Dodd JD (December 2010). "Headshop heartache: acute mephedrone 'meow' myocarditis". Heart. 96 (24): 2051–2. doi:10.1136/hrt.2010.209338. PMID 21062771.
- ↑ Dinis, Paulo; Teixeira, Rogério; Puga, Luís; Lourenço, Carolina; Cachulo, Maria Carmo; Gonçalves, Lino (2018). "Eosinophilic Myocarditis: Clinical Case and Literature Review". Arquivos Brasileiros de Cardiologia. 110 (6): 597–599. doi:10.5935/abc.20180089. PMC 6023626. PMID 30226920.
- ↑ Zhang, Yue; Zhou, Xiaobin; Chen, Shuyi; Sun, Xinchen; Zhou, Chenglin. "Immune mechanisms of group B coxsackievirus induced viral myocarditis". Virulence. 14 (1): 2180951. doi:10.1080/21505594.2023.2180951. ISSN 2150-5594.
- ↑ Séguéla PE, Iriart X, Acar P, Montaudon M, Roudaut R, Thambo JB (2015). "Eosinophilic cardiac disease: Molecular, clinical and imaging aspects". Archives of Cardiovascular Diseases. 108 (4): 258–68. doi:10.1016/j.acvd.2015.01.006. PMID 25858537.
- ↑ Rose NR (2016). "Viral myocarditis". Current Opinion in Rheumatology. 28 (4): 383–9. doi:10.1097/BOR.0000000000000303. PMC 4948180. PMID 27166925.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; & Mitchell, Richard N. (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 414-416 ISBN 978-1-4160-2973-1
- ↑ Kenneth L. Baughman, Special Report: Diagnosis of Myocarditis; Death of Dallas Criteria. Circulation. 2006;113:593-595 Archived 2009-07-20 at the Wayback Machine
- ↑ Skouri HN, Dec GW, Friedrich MG, Cooper LT (2006). "Noninvasive imaging in myocarditis". J. Am. Coll. Cardiol. 48 (10): 2085–93. doi:10.1016/j.jacc.2006.08.017. PMID 17112998.
- ↑ Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, White JA, Abdel-Aty H, Gutberlet M, Prasad S, Aletras AH, Laissy JP, Paterson I, Filipchuk NG, Kumar A, Pauschinger M, Liu P (2009). "Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper". J. Am. Coll. Cardiol. 53 (17): 1475–87. doi:10.1016/j.jacc.2009.02.007. PMC 2743893. PMID 19389557.
- ↑ 30.0 30.1 30.2 "UOTW #7 - Ultrasound of the Week". Ultrasound of the Week. 30 June 2014. Archived from the original on 8 May 2017. Retrieved 27 May 2017.
- ↑ 31.0 31.1 Hia, CP; Yip, WC; Tai, BC; Quek, SC (June 2004). "Immunosuppressive therapy in acute myocarditis: an 18 year systematic review". Archives of Disease in Childhood. 89 (6): 580–4. doi:10.1136/adc.2003.034686. PMC 1719952. PMID 15155409.
- ↑ 32.0 32.1 Aziz, KU; Patel, N; Sadullah, T; Tasneem, H; Thawerani, H; Talpur, S (October 2010). "Acute viral myocarditis: role of immunosuppression: a prospective randomised study". Cardiology in the Young. 20 (5): 509–15. doi:10.1017/S1047951110000594. PMID 20584348.
- ↑ 33.0 33.1 Robinson, J; Hartling, L; Vandermeer, B; Klassen, TP (20 May 2015). "Intravenous immunoglobulin for presumed viral myocarditis in children and adults". The Cochrane Database of Systematic Reviews. 5 (5): CD004370. doi:10.1002/14651858.CD004370.pub3. PMID 25992494.
- ↑ de Caen, AR; Berg, MD; Chameides, L; Gooden, CK; Hickey, RW; Scott, HF; Sutton, RM; Tijssen, JA; Topjian, A; van der Jagt, ÉW; Schexnayder, SM; Samson, RA (3 November 2015). "Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S526–42. doi:10.1161/cir.0000000000000266. PMC 6191296. PMID 26473000.
- ↑ Liu, ZL; Liu, ZJ; Liu, JP; Kwong, JS (28 August 2013). "Herbal medicines for viral myocarditis". The Cochrane Database of Systematic Reviews. 8 (8): CD003711. doi:10.1002/14651858.CD003711.pub5. PMID 23986406.
- ↑ Cooper LT (April 2009). "Myocarditis". N. Engl. J. Med. 360 (15): 1526–35. doi:10.1056/NEJMra0800028. PMC 5814110. PMID 19357408.
- ↑ P. Schölmerich. (1983.) "Myocarditis — Cardiomyopathy Historic Survey and Definition", International Boehringer Mannheim Symposia, 1:5.
- ↑ Joseph Friedrich Sobernheim. (1837.) Praktische Diagnostik der inneren Krankheiten mit vorzueglicher Ruecksicht auf pathologische Anatomic. Hirschwald, Berlin, 117.
- ↑ 39.0 39.1 Eckhardt G. J. Olsen. (1985.) "What is myocarditis?" Archived 2018-06-03 at the Wayback Machine, Heart and Vessels, 1(1):S1-3.
- ↑ Jared W. Magnani; G. William Dec. (2006.) "Myocarditis" Archived 2013-12-16 at the Wayback Machine, Circulation, 113:876-890.
External links
| Classification | |
|---|---|
| External resources |
- Myocarditis on emedicine Archived 2009-02-04 at the Wayback Machine