Colorado tick fever
| Colorado tick fever | |
|---|---|
| Other names: Mountain tick fever, American tick fever, American mountain tick fever | |
| |
| Specialty | Infectious disease |
| Symptoms | Fever, chills, headache, body aches[1] |
| Causes | Colorado tick fever virus[2] |
| Diagnostic method | History of exposure to ticks (that carry CTF virus), blood test[1] |
| Differential diagnosis | Lyme disease,Rocky Mountain spotted fever[3] |
| Prevention | Treat clothing with products containing 0.5% permethrin[4] |
| Treatment | Rest, fluids[1] |
| Medication | None[1] |
Colorado tick fever (CTF) or Mountain tick fever[5] is a viral infection (Coltivirus) transmitted from the bite of an infected Rocky Mountain wood tick (Dermacentor andersoni). It should not be confused with the bacterial tick-borne infection, Rocky Mountain spotted fever. Colorado tick fever is probably the same disease that American pioneers referred to as "mountain fever".[6][7]
Colorado tick fever virus (CTFV) infects haemopoietic cells, particularly erythrocytes, which explains how the virus is transmitted by ticks and also accounts for the incidence of transmission by blood transfusion.[8][9][10]
Signs and symptoms
First signs or symptoms can occur within a week after the initial tick bite, although it can have incubation periods of up to 20 days. Patients usually experience a two-staged fever and illness which can continue for three days, diminish, and then return for another episode of one to three days. The virus has the ability to live in the bloodstream for several months; therefore, coming in contact without proper precautions is prohibited.[11][1][3][12]
Initial symptoms include fever, chills, headaches, pain behind the eyes, light sensitivity, muscle pain, generalized malaise, abdominal pain, hepatosplenomegaly, nausea and vomiting, and a flat or pimply rash.[13]
During the second phase of the virus, a high fever can return with an increase in symptoms. CTF can be very severe in cases involving children and require hospitalization. [12] [3]
Complications
Complications with this disease have included aseptic meningitis,as well as encephalitis.[14]
Cause
Virology
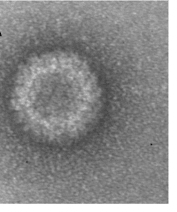
The virus particle, like other coltiviruses, is about 80 nm in diameter and is generally not enveloped. The double-stranded RNA viral genome is about 20,000 bp long and is divided into 12 segments, which are termed Seg-1 to Seg-12. Viral replication in infected cells is associated with characteristic cytoplasmic granular matrices. Evidence suggests the viral presence in mature erythrocytes is a result of replication of the virus in hematopoetic erythrocyte precursor cells and simultaneous maturation of the infected immature cells rather than of direct entry and replication of CTFV in mature erythrocytes.[15]
Trasmission

Tick
The Rocky Mountain wood tick is usually found attached to a host, but when it is without a host, it hides in cracks and crevices, as well as soil. If for some reason the tick is not able to find a host before the winter, it will stay under groundcover until spring, when it can resume its search. The wood tick does not typically seek hosts in the hottest summer months. Adult ticks tend to climb to the tops of grasses or low shrubs, attaching themselves to a host wandering by; they secure the attachment by secreting a substance from their mouths, inserting it into the host.[16][17][18][19]
Blood transfusion
Colorado tick fever is acquired by tick bite, no evidence of natural person-to-person transmission has been found. However, rare cases of transmission from blood transfusions have been reported. The virus which causes Colorado tick fever may stay in the blood for as long as four months after onset of the illness.[10][1]
Diagnosis
A combination of clinical signs, symptoms, and laboratory tests can confirm the likelihood of having CTF. Some tests include complement fixation to Colorado tick virus, immunofluorescence for Colorado tick fever, and some other common laboratory findings suggestive of CTF, including leucopenia, thrombocytopenia, and mildly elevated liver enzyme levels.[1][20]
The diagnostic detection of viral antibodies on red blood cells is possible.[21]
Prevention

Contracting the CTF virus is thought to provide long-lasting immunity against reinfection. However, it is always wise to be on the safe side and try to prevent tick bites.[13]
To avoid tick bites and infection, experts advise:[3][22]
- Avoid tick-infested areas, especially during the warmer months.
- Wear light-colored clothing so ticks can be easily seen; wear a long sleeved shirt, hat, long pants, and tuck pant legs into socks.
- Clothing and body parts should be checked every few hours for ticks when spending time outdoors in tick-infested areas. Ticks are most often found on the thigh, arms, underarms, and legs.
- The use of insect repellents containing DEET on skin or permethrin on clothing can be effective.
Treatment
No specific treatment for CTF is yet available. The first action is to make sure the tick is fully removed from the skin, then acetaminophen and analgesics can be used to help relieve the fever and pain. Aspirin is not recommended for children, as it has been linked to Reye’s syndrome in some viral illnesses. Salicylates should not be used because of thrombocytopenia, and the rare occurrence of bleeding disorders. People who suspect they have been bitten by a tick or are starting to show signs of CTF should contact their physicians immediately.[14]
Tick removal

Ticks should be removed promptly and carefully with tweezers and by applying gentle, steady traction. The tick's body should not be crushed when it is removed and the tweezers should be placed as close to the skin as possible to avoid leaving tick mouthparts in the skin; mouthparts left in the skin can allow secondary infections. Ticks should not be removed with bare hands. Hands should be protected by gloves or tissues and thoroughly washed with soap and water after the removal process.[23][24][25]
A match or flame should not be used to remove a tick; this method, once thought safe, can cause the tick to regurgitate expelling any disease it may be carrying into the bite wound.[23][25]
Epidemiology
The disease develops from March to September, with the highest infections occurring in June.[14]
The disease is found almost exclusively in the western United States and Canada, mostly in high mountain areas such as Colorado and Idaho. The CTFV was first isolated from human blood in 1944.[13][26]
CTF is seasonal, mostly occurring in the Rocky Mountain region of the United States and usually in altitudes from 4,000 to 10,000 feet (1.600 to 3.000 meters).[13] [27]
Patients with CTF are mostly campers and young males, who most likely have been bitten because of their activities.[28]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 "Symptoms & Treatment | Colorado Tick Fever | CDC". www.cdc.gov. 31 October 2022. Archived from the original on 8 June 2023. Retrieved 21 August 2023.
- ↑ "Virus | Colorado Tick Fever | CDC". www.cdc.gov. 16 April 2021. Archived from the original on 13 May 2023. Retrieved 21 August 2023.
- ↑ 3.0 3.1 3.2 3.3 "Colorado Tick Fever - Symptoms, Causes, Treatment | NORD". rarediseases.org. Archived from the original on 24 June 2023. Retrieved 26 August 2023.
- ↑ "Preventing tick bites on people | CDC". Centers for Disease Control and Prevention. 1 July 2020. Archived from the original on 29 July 2021. Retrieved 21 August 2023.
- ↑ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Colorado tick fever". www.orpha.net. Archived from the original on 23 August 2023. Retrieved 21 August 2023.
- ↑ Aldous JA, Nicholes PS. (1997). "What Is Mountain Fever?". Overland Journal. 15 (Spring): 18–23.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Aldous JA. (1997). "Mountain Fever in the 1847 Mormon Pioneer Companies" (PDF). Nauvoo Journal. 9 (Fall): 52–59. Archived (PDF) from the original on 2020-09-29. Retrieved 2022-09-12.
- ↑ Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Volume 2 (Eighth ed.). Philadelphia, PA: Elsevier Saunders. 2015. p. 1161. ISBN 978-1455748013. Retrieved 25 August 2023.
- ↑ Beckham, J. David; Tyler, Kenneth L. (1 January 2015). "91 - Encephalitis". Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases (Eighth Edition). W.B. Saunders. pp. 1144–1163.e3. ISBN 978-1-4557-4801-3. Retrieved 27 August 2023.
- ↑ 10.0 10.1 Giménez-Richarte, Á; Ortiz de Salazar, MI; Giménez-Richarte, MP; Collado, M; Fernández, PL; Clavijo, C; Navarro, L; Arbona, C; Marco, P; Ramos-Rincon, JM (October 2022). "Transfusion-transmitted arboviruses: Update and systematic review". PLOS Neglected Tropical Diseases. 16 (10): e0010843. doi:10.1371/journal.pntd.0010843. PMID 36201547.
- ↑ Klasco, Richard (March 2002). "Colorado tick fever". The Medical Clinics of North America. 86 (2): 435–440, ix. doi:10.1016/s0025-7125(03)00096-8. PMID 11982311. Archived from the original on 21 October 2021. Retrieved 22 August 2023.
- ↑ 12.0 12.1 Emmons, R W (October 1988). "Ecology of Colorado Tick Fever". Annual Review of Microbiology. 42 (1): 49–64. doi:10.1146/annurev.mi.42.100188.000405. Archived from the original on 29 August 2023. Retrieved 28 August 2023.
- ↑ 13.0 13.1 13.2 13.3 "Colorado Tick Fever". Archived from the original on 2009-02-13. Retrieved 2009-01-20.
- ↑ 14.0 14.1 14.2 "Colorado tick fever". MedlinePlus. Archived from the original on 2017-06-25. Retrieved 2017-07-10.
- ↑ Philipp CS, Callaway C, Chu MC, et al. (1 April 1993). "Replication of Colorado tick fever virus within human hematopoietic progenitor cells". J. Virol. 67 (4): 2389–95. doi:10.1128/JVI.67.4.2389-2395.1993. PMC 240408. PMID 8445735.
- ↑ Eisen, Lars; Ibarra-Juarez, Luis A.; Eisen, Rebecca J.; Piesman, Joseph (June 2008). "Indicators for elevated risk of human exposure to host-seeking adults of the Rocky Mountain wood tick (Dermacentor andersoni) in Colorado". Journal of Vector Ecology: Journal of the Society for Vector Ecology. 33 (1): 117–128. doi:10.3376/1081-1710(2008)33[117:iferoh]2.0.co;2. ISSN 1081-1710. PMID 18697314. S2CID 20648305. Archived from the original on 26 August 2023. Retrieved 23 August 2023.
- ↑ "Colorado Tick Fever: Background, Pathophysiology and Etiology, Epidemiology". Medscape. 26 April 2022. Archived from the original on 22 January 2019. Retrieved 28 August 2023.
- ↑ "CDC - DPDx - Ticks". www.cdc.gov. 23 January 2019. Archived from the original on 18 March 2021. Retrieved 29 August 2023.
- ↑ Diaz, James H. (1 January 2015). "298 - Ticks, Including Tick Paralysis". Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases (Eighth Edition). W.B. Saunders. pp. 3266–3279.e1. ISBN 978-1-4557-4801-3.
- ↑ "Diagnostic Testing | Colorado Tick Fever | CDC". www.cdc.gov. 7 March 2023. Archived from the original on 13 May 2023. Retrieved 24 August 2023.
- ↑ Mohd Jaafar F, Attoui H, Gallian P, et al. (May 2003). "Recombinant VP7-based enzyme-linked immunosorbent assay for detection of immunoglobulin G antibodies to Colorado tick fever virus". J. Clin. Microbiol. 41 (5): 2102–5. doi:10.1128/JCM.41.5.2102-2105.2003. PMC 154693. PMID 12734255.
- ↑ "Prevention | Colorado Tick Fever | CDC". www.cdc.gov. 26 February 2021. Archived from the original on 9 June 2023. Retrieved 25 August 2023.
- ↑ 23.0 23.1 "Tick removal | CDC". Centers for Disease Control and Prevention. 13 May 2022. Archived from the original on 16 January 2017. Retrieved 27 August 2023.
- ↑ "How to remove a tick". NIH MedlinePlus Magazine. Archived from the original on 28 May 2023. Retrieved 24 August 2023.
- ↑ 25.0 25.1 Benzoni, Thomas; Cooper, Jeffrey S. (2023). "Tick Removal". StatPearls. StatPearls Publishing. Archived from the original on 2023-09-01. Retrieved 2023-08-29.
- ↑ Medicine, Institute of; Practice, Board on Population Health and Public Health; Science, Committee on Lyme Disease and Other Tick-Borne Diseases: The State of the (31 May 2011). Critical Needs and Gaps in Understanding Prevention, Amelioration, and Resolution of Lyme and Other Tick-Borne Diseases: The Short-Term and Long-Term Outcomes: Workshop Report. National Academies Press. p. 223. ISBN 978-0-309-21112-3. Archived from the original on 29 August 2023. Retrieved 28 August 2023.
- ↑ Padgett, Kerry A.; Kjemtrup, Anne; Novak, Mark; Velez, Jason O.; Panella, Nicholas (1 August 2022). "Colorado Tick Fever Virus in the Far West: Forgotten, but Not Gone". Vector Borne and Zoonotic Diseases. 22 (8): 443–448. doi:10.1089/vbz.2022.0018. ISSN 1530-3667. Archived from the original on 29 August 2023. Retrieved 26 August 2023.
- ↑ Yendell, Stephanie J.; Fischer, Marc; Staples, J. Erin (May 2015). "Colorado tick fever in the United States, 2002-2012". Vector Borne and Zoonotic Diseases (Larchmont, N.Y.). 15 (5): 311–316. doi:10.1089/vbz.2014.1755. ISSN 1557-7759. PMC 6909933. PMID 25988440.
External links
| Classification | |
|---|---|
| External resources |

