Postherpetic neuralgia
| Postherpetic neuralgia | |
|---|---|
| Other names: Postherpetic trigeminal neuralgia[1][2] | |
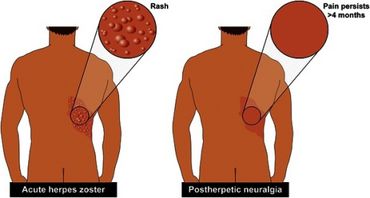 | |
| Left Presentation of acute herpes zoster Right postherpetic neuralgia, with pain persisting more than 4 months after the acute rash | |
| Symptoms | burning or stabbing pain, pain doesn't end after the shingles subsides. |
| Duration | lifelong |
Postherpetic neuralgia (PHN) is neuropathic pain that occurs due to damage to a peripheral nerve caused by the reactivation of the varicella zoster virus (herpes zoster, also known as shingles). Typically, the nerve pain (neuralgia) is confined to an area of skin innervated by a single sensory nerve, which is known as a dermatome. PHN is defined as dermatomal nerve pain that persists for more than 90 days after an outbreak of herpes zoster affecting the same dermatome.[3] Several types of pain may occur with PHN including continuous burning pain, episodes of severe shooting or electric-like pain, and a heightened sensitivity to gentle touch which would not otherwise cause pain (mechanical allodynia) or to painful stimuli (hyperalgesia).[3] Abnormal sensations and itching may also occur.[3]
The nerve pain of PHN is thought to result from damage in a peripheral nerve that was affected by the reactivation of the varicella zoster virus or troubles after chemotherapy. PHN typically begins when the herpes zoster vesicles have crusted over and begun to heal, but can begin in the absence of herpes zoster—a condition called zoster sine herpete.[4]
There is no treatment that modifies the disease course of PHN; therefore, controlling the affected person's symptoms is the main goal of treatment. Medications applied to the skin such as capsaicin or topical anesthetics (e.g., lidocaine) are used for mild pain and can be used in combination with oral medications for moderate to severe pain.[3] Oral anticonvulsant medications such as gabapentin and pregabalin are also approved for treatment of PHN.[3] Tricyclic antidepressants reduce PHN pain, but their use is limited by side effects.[3] Opioid medications are not generally recommended for treatment except in specific circumstances. Such cases should involve a pain specialist in patient care due to mixed evidence of efficacy and concerns about potential for abuse and addiction.[3]
PHN is the most common long-term complication of herpes zoster.[3] The incidence and prevalence of PHN are uncertain due to varying definitions. Approximately 20% of people affected by herpes zoster report pain in the affected area three months after the initial episode of herpes zoster, and 15% of people similarly report this pain two years after the herpes zoster rash.[3] Since herpes zoster occurs due to reactivation of the varicella zoster virus, which is more likely to occur with a weakened immune system, both herpes zoster and PHN occur more often in the elderly and in people with diabetes mellitus.[3] Risk factors for PHN include older age, a severe herpes-zoster rash, and pain during the herpes zoster episode.[3] PHN is often very painful and can be quite debilitating. Affected individuals often experience a decrease in their quality of life.[3]
Signs and symptoms
Symptoms:[citation needed]
- With resolution of the herpes zoster eruption, pain that continues for three months or more is defined as postherpetic neuralgia.
- Pain is variable, from discomfort to very severe, and may be described as burning, stabbing, or gnawing.
Signs:[citation needed]
- Area of previous herpes zoster may show evidence of cutaneous scarring.
- Sensation may be altered over the areas involved, in the form of either hypersensitivity or decreased sensation.
- In rare cases, the patient might also experience muscle weakness, tremor, or paralysis if the nerves involved also control muscle movement.
Pathophysiology

Postherpetic neuralgia is thought to be due to nerve damage caused by herpes zoster. The damage causes nerves in the affected dermatomic area of the skin to send abnormal electrical signals to the brain. These signals may convey excruciating pain, and may persist or recur for months, years, or for life.[5]
A key factor in the neural plasticity underlying neuropathic pain is altered gene expression in sensory dorsal root ganglia neurons. Injury to sensory nerves induces neurochemical, physiological, and anatomical modifications to afferent and central neurons, such as afferent terminal sprouting and inhibitory interneuron loss.[5]
Following nerve damage, NaCl channel accumulation causes hyperexcitability, and downregulation of the TTX-resistant Nav1.8 (sensory neuron specific, SNS1) channel and upregulation of TTX-sensitive Nav1.3 (brain type III) and TRPV1 channels. These changes contribute to increased NMDA glutamate receptor-dependent excitability of spinal dorsal horn neurons and are restricted to the ipsilateral (injured) side. A combination of these factors could contribute to the neuropathic pain state of postherpetic neuralgia.[citation needed]
Diagnosis
Lab Studies:[citation needed]
- No laboratory work is usually necessary.
- Results of cerebrospinal fluid evaluation are abnormal in 61%.
- Pleocytosis is observed in 46%, elevated protein in 26%, and VZV DNA in 22%.
- These findings are not predictive of the clinical course of postherpetic neuralgia.
- Viral culture or immunofluorescence staining may be used to differentiate herpes simplex from herpes zoster in cases that are difficult to distinguish clinically.
- Antibodies to herpes zoster can be measured. A 4-fold increase has been used to support the diagnosis of subclinical herpes zoster (zoster sine herpete). However, a rising titer secondary to viral exposure rather than reactivation cannot be ruled out.
Imaging studies:[citation needed]
- Magnetic resonance imaging lesions attributable to herpes zoster were seen in the brain stem and cervical cord in 56% (9/16) of patients.
- At three months after onset of herpes zoster, 56% (5/9) of patients with an abnormal magnetic resonance image had developed postherpetic neuralgia.
- Of the seven patients who had no herpes-zoster-related lesions on the magnetic resonance image, none had residual pain.
Prevention
Primary prevention
In 1995, the Food and Drug Administration (FDA) approved the Varicella vaccine to prevent chickenpox. Its effect on postherpetic neuralgia is still unknown. The vaccine—made from a weakened form of the varicella-zoster virus—may keep chickenpox from occurring in nonimmune children and adults, or at least lessen the risk of the varicella zoster virus lying dormant in the body and reactivating later as shingles. If shingles could be prevented, postherpetic neuralgia could be completely avoided.[citation needed]
In May 2006 the Advisory Committee on Immunization Practices approved a new vaccine by Merck (Zostavax) against shingles. This vaccine is a more potent version of the chickenpox vaccine, and evidence shows that it reduces the incidence of postherpetic neuralgia.[7] The CDC recommends use of this vaccine in all persons over 60 years old.[8]
The most effective means of preventing PHN from a herpes zoster infection is prior vaccination with the varicella vaccine. Vaccination decreases the overall incidence of virus reactivation but also decreases the severity of disease development and incidence of PHN if reactivation does occur.[9]
Secondary prevention
A 2013 Cochrane meta-analysis of 6 randomized controlled trials (RCTs) investigating oral antiviral medications given within 72 hours after the onset of herpes zoster rash in immunocompetent people for preventing postherpetic neuralgia (PHN) found no significant difference between placebo and acyclovir. Additionally, there was no significant difference in preventing the incidence of PHN found in the one RCT included in the meta-analysis that compared placebo to oral famciclovir treatment within 72 hours of HZ rash onset. Studies using valacyclovir treatment were not included in the meta-analysis. PHN was defined as pain at the site of the dermatomic rash at 120 days after the onset of rash, and incidence was evaluated at 1, 4, and 6 months after rash onset. Patients who are prescribed oral antiviral agents after the onset of rash should be informed that their chances of developing PHN are no different than those not taking oral antiviral agents.[10]
Treatment
The pain from postherpetic neuralgia can be very severe and requires immediate treatment. There is no treatment which modifies the course of the disease and management primarily aims to control symptoms.[3]
Medications
Topical medications
Medications applied to the skin can be used alone if the pain from PHN is mild or in combination with oral medications if the pain is moderate to severe.[3] Topical medications for PHN include low-dose (0.075%) and high-dose (8%) capsaicin and anesthetics such as lidocaine patches.[3] Lidocaine patches (5% concentration) are approved in the United States and Europe to treat PHN though evidence supporting their use is limited.[3] A meta-analysis of multiple small placebo-controlled randomized controlled trials found that for every two people treated with topical lidocaine, one person experienced at least a 50% reduction in their PHN-associated pain (number needed to treat (NNT)=2).[11]
Low-dose capsaicin may be useful for reducing PHN-associated pain but is limited by side effects (redness and a burning or stinging sensation with application) and the need to apply it four times daily.[3] Approximately three people must be treated with low-dose capsaicin cream for one person to experience significant pain relief (number needed to treat =3.3).[3][11] A single topical application of a high-dose capsaicin patch over the affected area after numbing the area with a topical anesthetic has also been found to relieve PHN-associated pain.[3] For every eleven people treated with a high-dose capsaicin patch for up to 12 weeks, one person experienced a significant improvement in their pain. (number needed to treat=11).[12] Due to the need for topical anesthesia before application of the high-dose capsaicin patch, referral to a pain specialist is generally recommended if this approach is being considered.[3]
Oral medications
Multiple oral medications have demonstrated efficacy in relieving postherpetic neuralgia pain. Tricyclic antidepressants (TCAs), such as nortriptyline or desipramine, are effective in reducing postherpetic neuralgia pain but are limited by their numerous side effects. For every three people treated with a tricyclic antidepressant, one person is expected to have a clinically significant reduction in their pain (NNT=3).[3] Additionally, of every sixteen people treated with a TCA, one person is expected to stop the medication due to a bothersome side effect, such as dry mouth, constipation, or urinary retention (number needed to harm=16).[3] The anticonvulsant medications pregabalin and gabapentin also effectively relieve postherpetic neuralgia pain. Treatment with pregabalin leads to a reduction in pain intensity of 50% or more in one person out of every 4–5 people treated (NNT=4–5).[13] Similarly, treatment with gabapentin also leads to a 50% reduction in pain intensity in one person out of every 7-8 people treated (NNT=7.5).[13]
Opioids such as tramadol, methadone, oxycodone, and morphine have not been well-studied for postherpetic neuralgia treatment.[14][15][16][17] Acetaminophen and nonsteroidal anti-inflammatory drugs are thought to be ineffective and have not undergone rigorous study for PHN.[3][18]
Prognosis
The natural history of postherpetic neuralgia involves slow resolution of the pain syndrome. A subgroup of affected individuals may develop severe, long-lasting pain that does not respond to medical therapy.[citation needed]
Epidemiology
In the United States each year approximately 1,000,000 individuals develop herpes zoster.[19] Of those individuals, approximately 10–18% develop postherpetic neuralgia.[20]
Fewer than 10 percent of people younger than 60 develop postherpetic neuralgia after a bout of herpes zoster, while about 40 percent of people older than 60 do.[citation needed]
References
- ↑ Suen, James Y.; Petersen, Erika (20 July 2018). Diagnosis and Management of Head and Face Pain: A Practical Approach. Springer. p. 40. ISBN 978-3-319-90999-8. Archived from the original on 2 April 2024. Retrieved 1 April 2024.
- ↑ 2.0 2.1 Niemeyer, Christy S.; Harlander-Locke, Michael; Bubak, Andrew N.; Rzasa-Lynn, Rachael; Birlea, Marius (1 April 2024). "Trigeminal Postherpetic Neuralgia: From Pathophysiology to Treatment". Current Pain and Headache Reports. 28 (4): 295–306. doi:10.1007/s11916-023-01209-z. ISSN 1534-3081. Retrieved 31 March 2024.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 Johnson RW, Rice AS (October 2014). "Clinical practice. Postherpetic neuralgia". The New England Journal of Medicine (Review). 371 (16): 1526–33. doi:10.1056/NEJMcp1403062. PMID 25317872.
- ↑ Rissardo, JamirPitton; Caprara, AnaLetícia Fornari (2020). "Postherpetic neuralgia and varicella-zoster virus". Current Medical Issues. 18 (4): 340. doi:10.4103/cmi.cmi_94_20. ISSN 0973-4651. Archived from the original on 2020-12-11. Retrieved 2022-03-17.
- ↑ 5.0 5.1 Gharibo C, Kim C (December 2011). "Neuropathic Pain of Postherpetic Neuralgia" (PDF). Pain Medicine News. McMahon Publishing. Archived (PDF) from the original on 21 October 2014. Retrieved 6 October 2014.
- ↑ Devulder, J. E. R. (2002). "Postherpetic ophthalmic neuralgia". Bulletin De La Societe Belge D'ophtalmologie (285): 19–23. ISSN 0081-0746. Retrieved 11 December 2022.
- ↑ Chen N, Li Q, Zhang Y, Zhou M, Zhou D, He L (March 2011). He L (ed.). "Vaccination for preventing postherpetic neuralgia". The Cochrane Database of Systematic Reviews (3): CD007795. doi:10.1002/14651858.CD007795.pub2. PMID 21412911.
- ↑ "Shingles (Herpes Zoster) Vaccination". U.S. Centers for Disease Control and Prevention (CDC). 25 March 2021. Archived from the original on 31 October 2021. Retrieved 15 November 2021.
- ↑ Benzon H, Raja SN, Fishman S, Liu S, Cohen (2011). Essentials of pain medicine (3rd ed.). St. Louis, Mo.: Elsevier/Saunders. ISBN 978-1-4377-2242-0.
- ↑ Chen N, Li Q, Yang J, Zhou M, Zhou D, He L (February 2014). He L (ed.). "Antiviral treatment for preventing postherpetic neuralgia". The Cochrane Database of Systematic Reviews. 2 (2): CD006866. doi:10.1002/14651858.CD006866.pub3. PMID 24500927.
- ↑ 11.0 11.1 Hempenstall K, Nurmikko TJ, Johnson RW, A'Hern RP, Rice AS (July 2005). "Analgesic therapy in postherpetic neuralgia: a quantitative systematic review". PLOS Medicine (Systematic Review and Meta-Analysis). 2 (7): e164. doi:10.1371/journal.pmed.0020164. PMC 1181872. PMID 16013891.
- ↑ Derry S, Rice AS, Cole P, Tan T, Moore RA (January 2017). "Topical capsaicin (high concentration) for chronic neuropathic pain in adults". The Cochrane Database of Systematic Reviews (Systematic Review and Meta-Analysis). 1 (7): CD007393. doi:10.1002/14651858.CD007393.pub4. PMC 6464756. PMID 28085183.
- ↑ 13.0 13.1 Wiffen PJ, Derry S, Moore RA, Aldington D, Cole P, Rice AS, et al. (November 2013). "Antiepileptic drugs for neuropathic pain and fibromyalgia - an overview of Cochrane reviews". The Cochrane Database of Systematic Reviews (Systematic Review and Meta-Analysis). 11 (11): CD010567. doi:10.1002/14651858.CD010567.pub2. PMC 6469538. PMID 24217986.
- ↑ Duehmke RM, Derry S, Wiffen PJ, Bell RF, Aldington D, Moore RA (June 2017). "Tramadol for neuropathic pain in adults". The Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 6 (CD003726): CD003726. doi:10.1002/14651858.CD003726.pub4. PMC 6481580. PMID 28616956.
- ↑ McNicol ED, Ferguson MC, Schumann R (May 2017). "Methadone for neuropathic pain in adults". The Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 5 (CD012499): CD012499. doi:10.1002/14651858.CD012499.pub2. PMC 6353163. PMID 28514508.
- ↑ Cooper TE, Chen J, Wiffen PJ, Derry S, Carr DB, Aldington D, et al. (May 2017). "Morphine for chronic neuropathic pain in adults". The Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 5 (CD011669): CD011669. doi:10.1002/14651858.CD011669.pub2. PMC 6481499. PMID 28530786.
- ↑ Gaskell H, Derry S, Stannard C, Moore RA (July 2016). "Oxycodone for neuropathic pain in adults". The Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 7 (CD010692): CD010692. doi:10.1002/14651858.CD010692.pub3. PMC 6457997. PMID 27465317.
- ↑ Wiffen PJ, Knaggs R, Derry S, Cole P, Phillips T, Moore RA (December 2016). "Paracetamol (acetaminophen) with or without codeine or dihydrocodeine for neuropathic pain in adults". The Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 12 (CD012227): CD012227. doi:10.1002/14651858.CD012227.pub2. PMC 6463878. PMID 28027389.
- ↑ Sayaprakash A, Ravanfar P, Tyring SK (2010). "Dermatological Virology". In Hall BJ, Hall JC (eds.). Sauer's manual of skin diseases (10th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 232. ISBN 978-1-60547-077-1.
- ↑ Weaver BA (June 2009). "Herpes zoster overview: natural history and incidence" (PDF). The Journal of the American Osteopathic Association. 109 (6 Suppl 2): S2-6. PMID 19553632. Retrieved 6 October 2014.
{{cite journal}}: CS1 maint: url-status (link)
Further reading
- Hempenstall K, Nurmikko TJ, Johnson RW, A'Hern RP, Rice AS (July 2005). "Analgesic therapy in postherpetic neuralgia: a quantitative systematic review". PLOS Medicine. 2 (7): e164. doi:10.1371/journal.pmed.0020164. PMC 1181872. PMID 16013891.
External links
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- CS1 maint: url-status
- Articles with hatnote templates targeting a nonexistent page
- Missing redirects
- All articles with unsourced statements
- Articles with unsourced statements from December 2020
- Articles with invalid date parameter in template
- Virus-related cutaneous conditions
- Neurological disorders
- Pain
- Varicella zoster virus-associated diseases