Retinal migraine
| Retinal migraine | |
|---|---|
| Other names: Ophthalmic migraine, ocular migraine, ophthalmic megrim, anterior visual pathway migraine[1] | |
 | |
| Example of a scintillating scotoma that some may experience | |
| Specialty | Neurology, ophthalmology |
| Symptoms | Episodes of vision problems, headache[1] |
| Complications | Permanent vision loss[2] |
| Duration | Less than an hour[2] |
| Causes | Unclear[2] |
| Risk factors | Stress, smoking, high blood pressure, birth control pills, exercise, high altitude, dehydration, low blood sugar, dehydration[2] |
| Differential diagnosis | Migraine with aura, increase intracranial pressure, amaurosis fugax, optic neuritis, giant cell arteritis[2] |
| Treatment | Avoiding risk factors, nifedipine, aspirin[2] |
| Frequency | Rare[2] |
Retinal migraine is a type of headache disorder with episodes of vision problems in one eye followed by a migraine headache.[1] Vision problems may vary from a complete loss, to blurring, to flashing lights, to a scotoma and typically last less than an hour.[2] Most people develop a headache on the same side as the vision problems.[2] Complications may include permanent vision loss.[2]
Half of those affected have a family history of migraines and a third have a personal history of migraines.[2] Risk factors for an episode include stress, smoking, high blood pressure, birth control pills, exercise, high altitude, dehydration, low blood sugar, and dehydration.[2] The underlying mechanism is unclear with theories including spasm of blood vessels supplying the eye and spreading depression of the neurons in the retina.[2][1] Diagnosis requires ruling out other possible causes.[2] It is differentiated from the aura during the early phase of a migraine with aura, as that generally occurs in both eyes.[2]
Management involves avoiding risk factors for episodes.[2] If this is not sufficient, aspirin or a calcium channel blocker, such as nifedipine may be used.[2] Triptans, dihydroergotamine, and beta-blockers should be avoided.[2] Retinal migraine is rare.[2] While cases may start as early as 7 years of age, most people are first affected in their 20s.[2] It occurs more commonly in women.[1] The condition was first described in 1882 by Galezowski.[1]
Signs and symptoms
Retinal migraine results in temporary visual scotoma or loss in one eye lasting less than one hour.[1] During some episodes, the visual loss may occur with no headache and at other times throbbing headache on the same side of the head as the visual loss may occur, accompanied by severe light sensitivity and/or nausea. Visual loss tends to affect the entire monocular visual field of one eye, not both eyes. After each episode, normal vision returns.
It may be difficult to read and dangerous to drive a vehicle while retinal migraine symptoms are present.
Retinal migraine is a different disease than scintillating scotoma, which is a visual anomaly caused by spreading depression in the occipital cortex at the back of the brain, not in the eyes nor any component thereof.[3] Unlike in retinal migraine, a scintillating scotoma involves repeated bouts of temporary diminished vision or blindness and affects vision from both eyes, upon which sufferers may see flashes of light, zigzagging patterns, blind spots, or shimmering spots or stars.[4]
Causes
Retinal migraine is caused by the blood vessels (that leads to the eye) suddenly narrowing, reducing blood flow to the eye, which causes aura in vision.
It may be triggered by:
- Stress
- Smoking
- High blood pressure
- Oral contraceptive pill
- Exercise
- Bending over
- High altitude
- Dehydration
- Low blood sugar
- Excessive heat
Retinal migraine tends to be more common in:
- Women
- People aged under 40
- People with a personal or family history of migraines or other headaches
- People with an underlying disease (lupus, hardening of the arteries, sickle cell disease, epilepsy, antiphospholipid syndrome, and giant cell arteritis)[5]
Diagnosis
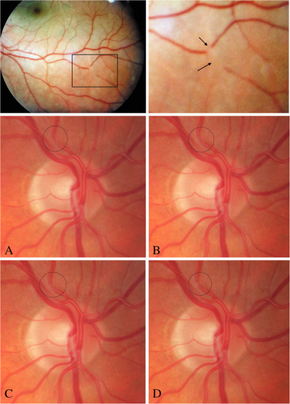
The medical exam should rule out any underlying causes, such as blood clot, stroke, pituitary tumor, or detached retina. A normal retina exam is consistent with retinal migraine.[6]
Treatment
Treatment depends on identifying behavior that triggers migraine such as stress, sleep deprivation, skipped meals, food sensitivities, or specific activities. Medicines used to treat retinal migraines include aspirin, other NSAIDS, and medicines that reduce high blood pressure.[6]
Prognosis
In general, the prognosis for retinal migraine is similar to that of migraine headache with typical aura. As the true incidence of retinal migraine is unknown, it is uncertain whether there is a higher incidence of permanent neuroretinal injury. The visual field data suggests that there is a higher incidence of end arteriolar distribution infarction and a higher incidence of permanent visual field defects in retinal migraine than in clinically manifest cerebral infarctions in migraine with aura. One study suggests that more than half of reported recurrent cases of retinal migraine subsequently experienced permanent visual loss in that eye from infarcts,[1] but more recent studies suggest such loss is a relatively rare side effect.[7]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Grosberg BM, Solomon S, Lipton RB (August 2005). "Retinal migraine". Curr Pain Headache Rep. 9 (4): 268–71. doi:10.1007/s11916-005-0035-2. PMID 16004843.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 Al Khalili, Y; Jain, S; King, KC (January 2020). "Retinal Migraine Headache". PMID 29939547.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "imigraine.net". Archived from the original on July 19, 2009. Retrieved 24 June 2015.
- ↑ "https://www.ohiohealth.com/theme_of_focus/clinical_focus_concept/ocular_migraine__when_to_seek_help/". Ohio Health. Archived from the original on 27 January 2016. Retrieved 12 February 2015.
{{cite web}}: External link in|title= - ↑ "Retinal migraine - NHS". Archived from the original on 26 April 2020. Retrieved 29 Nov 2019.
- ↑ 6.0 6.1 "Ocular Migraines - All About Retinal and Ocular Migraines". About.com Headaches & Migraines. Archived from the original on 24 September 2015. Retrieved 24 June 2015.
- ↑ Choices, NHS. "Retinal migraine - NHS Choices". www.nhs.uk. Archived from the original on 29 November 2016. Retrieved 17 November 2016.
External links
| Classification |
|---|