Paresthesia
| Paresthesia | |
|---|---|
| Other names: Paraesthesia, pins and needles, numbness and tingling | |
| Pronunciation | |
| Specialty | Neurology |
| Symptoms | Tingling, pricking, burning, numbness[1] |
| Causes | Nerve compression, carpal tunnel syndrome, stroke, multiple sclerosis, transverse myelitis, tumors, vitamin B12 deficiency, lead toxicity, diabetes, Guillain-Barre syndrome, encephalitis[1][2] |
| Treatment | Depends on cause[1] |
| Frequency | Common[1] |
Paresthesia, also known as pins and needles, is a feeling of tingling, pricking, burning, or numbness.[1] Less common it may be described as coldness or a crawling feeling.[3] It occurs without the skin being touched.[3] While it can occur anywhere on the body, most commonly the arms and legs are affected.[1] It may be of a brief or prolonged duration.[1]
A common cause of brief episodes is pressure on a nerve.[1] Long term cases may occur due to a carpal tunnel syndrome, stroke, multiple sclerosis, transverse myelitis, tumors, vitamin B12 deficiency, lead toxicity, diabetes, Guillain-Barre syndrome, or encephalitis.[1][2] Diagnosis is based on the symptoms, examination, and further testing.[1]
Treatment depends on the underlying cause.[1] Efforts to improve the severity may include capsaicin creams, carbamazepine, or gabapentin.[4] The term is derived from the Greek "para" meaning beside and "aesthesis" meaning sensation.[3] The term dysesthesia has a similar meaning; however, some use it only when being touched results in the abnormal sensation.[5]
Signs and symptoms
The individual would feel, anywhere on the body (though most likely the extremeties) a type of burning or prickling sensation[6]
Causes
Brief episodes
Paresthesias of the hands, feet, legs and arms are common, transient symptoms. The briefest, electric shock type of paresthesia can be caused by tweaking the ulnar nerve near the elbow. Similar brief shocks can be experienced when any other nerve is tweaked (a tweaked neck nerve may cause a brief shock-like paresthesia toward the scalp). In the older age group, spinal column irregularities may tweak the spinal cord briefly when the head or back is turned, flexed, or extended into brief uncommon positions (Lhermitte's sign).
The most common, everyday cause is temporary restriction of nerve impulses to an area of nerves, commonly caused by leaning or resting on parts of the body such as the legs (often followed by a pins and needles tingling sensation). Other causes include conditions such as hyperventilation syndrome and panic attacks. A cold sore outside the mouth (not a canker sore inside the mouth) can be preceded by tingling because a cold sore is caused by herpes simplex virus. The varicella zoster virus (shingles) also notably may cause recurring pain and tingling in skin or tissue along the distribution path of that nerve (most commonly in the skin, along a dermatome pattern, but sometimes feeling like a headache, chest or abdominal pain, or pelvic pain).
Other common examples occur when sustained pressure has been applied over a nerve, inhibiting or stimulating its function. Removing the pressure typically results in gradual relief of these paresthesias.[7] Most pressure-induced paraesthesia results from awkward posture, such as engaging in cross-legged sitting for prolonged periods of time.
Reactive hyperaemia, which occurs when blood flow is restored after a period of ischemia, such as on rewarming after a cold episode in patients with Raynaud's disease, may be accompanied by paresthesia.[8]
Long term
Chronic paresthesia (Berger's paresthesia,[9] Sinagesia[10] or Bernhardt paresthesia[11]) indicates a problem with the functioning of neurons or poor circulation.
In older individuals, paresthesia is often the result of poor circulation in the limbs (such as in peripheral vascular disease), most often caused by atherosclerosis, the build up of plaque within artery walls, over decades, with eventual plaque ruptures, internal clots over the ruptures and subsequent clot healing but leaving behind narrowing of the artery openings or closure, both locally and in downstream smaller branches. Without a proper supply of blood and nutrients, nerve cells can no longer adequately send signals to the brain. Because of this, paresthesia can also be a symptom of vitamin deficiency and malnutrition, as well as metabolic disorders like diabetes, hypothyroidism, and hypoparathyroidism. It can also be a symptom of mercury poisoning.
Irritation to the nerve can also come from inflammation to the tissue. Joint conditions such as rheumatoid arthritis, psoriatic arthritis, and carpal tunnel syndrome are common sources of paresthesia. Nerves below the head may be compressed where chronic neck and spine problems exist and can be caused by, among other things, muscle cramps that may be a result of clinical anxiety or excessive mental stress,[citation needed] bone disease, poor posture, unsafe heavy lifting practices or physical trauma such as whiplash. Paresthesia can also be caused simply by putting pressure on a nerve by applying weight (or pressure) to the limb for extended periods of time.
Another cause of paresthesia may be direct damage to the nerves themselves, i.e., neuropathy, which itself can stem from injury, such as frostbite, or infection, such as Lyme disease, or may be indicative of a current neurological disorder. Neuropathy is also a side effect of some chemotherapies (see chemotherapy-induced peripheral neuropathy).[12] Benzodiazepine withdrawal may also cause paresthesia as the drug removal leaves the GABA receptors stripped bare and possibly malformed.[citation needed] Chronic paresthesia can sometimes be symptomatic of serious conditions, such as a transient ischemic attack, or autoimmune diseases such as multiple sclerosis, Complex Regional Pain Syndrome or lupus erythematosus.[citation needed] The use of fluoroquinolones can also cause paresthesia.[13] Stroke survivors and those with traumatic brain injury (TBI) may experience paresthesia from damage to the central nervous system.
The varicella zoster virus disease (shingles) can attack nerves causing numbness instead of pain commonly associated with shingles.[citation needed]
Acroparesthesia
Acroparesthesia is severe pain in the extremities, and may be caused by Fabry disease, a type of sphingolipidosis.[14]
It can also be a sign of hypocalcemia.
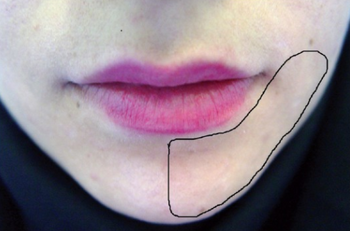
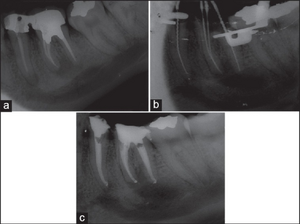
Dentistry
Paresthesia or "persistent anesthesia" is a transient or potentially permanent condition of extended numbness after administration of local anesthesia and the injected anesthetic has terminated.[15]
Potential causes include trauma introduced to the nerve sheath during administration of the injection, hemorrhage about the sheath, type of anesthetic used, or administration of anesthetic potentially contaminated with alcohol or sterilizing solutions.[16]
Other
Other causes may include:
- Anticonvulsant pharmaceutical drugs, such as topiramate, sultiame, and acetazolamide
- Anxiety or panic disorder[17]
- Autonomous sensory meridian response ("ASMR")[18]
- Benzodiazepine withdrawal syndrome
- Beta alanine
- Blood pressure medications
- Carpal tunnel syndrome
- Cerebral amyloid angiopathy
- Chiari malformation
- Coeliac disease (celiac disease)
- Complex regional pain syndrome
- Decompression sickness
- Dehydration
- Dextromethorphan (recreational use)
- Fabry disease
- Erythromelalgia
- Fibromyalgia
- Fluoroquinolone toxicity
- Guillain–Barré syndrome (GBS)
- Heavy metals
- Herpes zoster
- Hydroxy alpha sanshool, a component of Sichuan peppers
- Hyperglycemia (high blood sugar)
- Hyperkalemia
- Hyperventilation
- Hypoglycemia (low blood sugar)
- Hypocalcemia, and in turn:
- Hypermagnesemia, a condition in which hypocalcemia itself is typically observed as a secondary symptom
- Hypothyroidism
- Immunodeficiency, such as chronic inflammatory demyelinating polyneuropathy (CIDP)
- Intravenous administering of strong pharmaceutical drugs acting on the central nervous system (CNS), mainly opioids, opiates, narcotics; especially in non-medical use (drug abuse)
- Ketorolac
- Lidocaine poisoning
- Lomotil
- Lupus erythematosus
- Lyme disease
- Magnesium deficiency, often as a result of long term proton-pump inhibitor use
- Menopause
- Mercury poisoning
- Migraines
- Multiple sclerosis
- Nerve compression syndrome
- Nitrous oxide, long-term exposure[19]
- Obdormition
- Oxygen toxicity, especially, breathing oxygen under pressure, such as in scuba diving.
- Pyrethrum and pyrethroid (pesticide)[20]
- Rabies
- Radiation poisoning
- Sarcoidosis
- Scorpion stings
- Spinal disc herniation or injury
- Spinal stenosis
- Stinging nettles
- Syringomyelia
- Transverse myelitis
- Vitamin B5 deficiency
- Variant Creutzfeldt–Jakob disease
- Vitamin B12 deficiency
- Withdrawal from certain selective serotonin reuptake inhibitors (or serotonin-specific reuptake inhibitors) (SSRIs), such as paroxetine or serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine
Diagnosis
The nerve conduction study usually provides useful information for making diagnosis. A MRI or a CT scan is sometimes used to rule out some causes from the central nervous system.
Treatment
Medications offered can include the immunosuppressant prednisone, intravenous gamma globulin (IVIG), anticonvulsants such as gabapentin or Gabitril and antiviral medication, depending on the underlying cause.[medical citation needed]
In addition to treatment of the underlying disorder, palliative care can include the use of topical numbing creams, such as lidocaine or prilocaine. Care must be taken to apply only the necessary amount, as excess can contribute to the condition. Otherwise, these products offer extremely effective, but short-lasting, relief from the condition. Paresthesia caused by stroke may receive some temporary benefit from high doses of Baclofen multiple times a day[citation needed]. HIV patients who self-medicate with cannabis report that it reduces their symptoms.[21]
Paresthesia caused by shingles is treated with appropriate antiviral medication.[22]
Etymology
The word paresthesia (/ˌpærɪsˈθiːziə, -ʒə/; British English paraesthesia; plural paraesthesiae /-zii/ or paraesthesias), comes from the Greek para ("beside", i.e., abnormal) and aisthesia ("sensation").[23]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 "Paresthesia Information Page". National Institutes of Health. National Institute of Neurological Disorders and Stroke. 14 June 2018. Archived from the original on 2020. Retrieved 3 October 2018.
- ↑ 2.0 2.1 FACP, Fred F. Ferri, MD (2011). Ferri's Differential Diagnosis: A Practical Guide to the Differential Diagnosis of Symptoms, Signs, and Clinical Disorders. Elsevier Health Sciences. p. 374. ISBN 978-0-323-07699-9. Archived from the original on 2021-08-28. Retrieved 2020-12-02.
- ↑ 3.0 3.1 3.2 Loring, David W.; Bowden, Stephen (2015). INS Dictionary of Neuropsychology and Clinical Neurosciences. Oxford University Press. p. 279. ISBN 978-0-19-536645-7. Archived from the original on 2021-08-28. Retrieved 2020-12-02.
- ↑ Braddom, Randall L. (2010). Physical Medicine and Rehabilitation E-Book. Elsevier Health Sciences. p. 1092. ISBN 978-1-4377-3563-5. Archived from the original on 2021-08-28. Retrieved 2020-12-02.
- ↑ Larner, A. J. (2006). A Dictionary of Neurological Signs. Springer Science & Business Media. p. 101. ISBN 978-0-387-26214-7. Archived from the original on 2021-08-29. Retrieved 2020-12-02.
- ↑ "Paresthesia | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on 17 May 2022. Retrieved 25 May 2022.
- ↑ "Paresthesia Information Page: National Institute of Neurological Disorders and Stroke. (NINDS)". Archived from the original on 2020-11-11. Retrieved 2018-02-02.
- ↑ Belch JJ, McCollum PT, Walker WF, Stonebridge PA (1996). Color atlas of peripheral vascular diseases. Mosby-Wolfe. p. 77. ISBN 978-0-7234-2074-3.
- ↑ [ICD-10: R20.2]
- ↑ [ICD-10: R25.1]
- ↑ [ICD-10: G57.1]
- ↑ "Chemotherapy-induced Peripheral Neuropathy". National Cancer Institute. Archived from the original on 11 December 2011. Retrieved 1 December 2011.
- ↑ "FDA Drug Safety Communication: FDA requires label changes to warn of risk for possibly permanent nerve damage from antibacterial fluoroquinolone drugs taken by mouth or by injection". Food & Drug Administration. Archived from the original on 28 May 2016. Retrieved 28 May 2016.
- ↑ Marks, Dawn B.; Swanson, Todd; Kim, Sandra I.; Glucksman, Marc (2007). Biochemistry and Molecular biology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 978-0-7817-8624-9.
- ↑ "Paresthesia dental definition: The Free Dictionary. (TheFreeDictionary)". Archived from the original on 2017-06-09. Retrieved 2013-05-02.
- ↑ Garisto, G; Gaffen, A; Lawrence, H; Tenenbaum, H; Haas, D (Jul 2010). "Occurrence of Paresthesia After Dental Local Anesthetic Administration in the United States". The Journal of the American Dental Association. 141 (7): 836–844. doi:10.14219/jada.archive.2010.0281. PMID 20592403. Archived from the original on 2012-08-20. Retrieved 2013-05-02.
- ↑ Ietsugu, T; Sukigara, M; Furukawa, TA (Dec 2007). "Evaluation of diagnostic criteria for panic attack using item response theory: findings from the National Comorbidity Survey in USA". Journal of Affective Disorders. 104 (1–3): 197–201. doi:10.1016/j.jad.2007.03.005. PMID 17434598.
- ↑ Tihanyi, Benedek T.; Ferentzi, Eszter; Beissner, Florian; Köteles, Ferenc (1 February 2018). "The neuropsychophysiology of tingling" (PDF). Consciousness and Cognition. 58: 97–110. doi:10.1016/j.concog.2017.10.015. ISSN 1053-8100. Retrieved 28 November 2019.
{{cite journal}}: CS1 maint: url-status (link) - ↑ "Nitrous Oxide". Archived from the original on 2013-05-13. Retrieved 2016-03-05.
- ↑ Vijverberg, H.P., van den Bercken, J. Crit. Rev. Toxicol. (1990) Neurotoxicological effects and the mode of action of pyrethroid insecticides.
- ↑ Woolridge Emily; et al. (2005). "Cannabis use in HIV for pain and other medical symptoms". Journal of Pain and Symptom Management. 29 (4): 358–367. doi:10.1016/j.jpainsymman.2004.07.011. PMID 15857739.
- ↑ Cohen KR, Salbu RL, Frank J, Israel I (2013). "Presentation and management of herpes zoster (shingles) in the geriatric population". P T. 38 (4): 217–27. PMC 3684190. PMID 23785227.
- ↑ "Paresthesia Definition and Origin". dictionary.com. Archived from the original on 12 August 2015. Retrieved 1 August 2015.
External links
| Look up paresthesia in Wiktionary, the free dictionary. |
- paresthesia at NINDS
| Classification |
|---|
- Pages with script errors
- CS1 maint: url-status
- All articles with unsourced statements
- Articles with unsourced statements from January 2010
- Articles with invalid date parameter in template
- Articles with unsourced statements from June 2018
- Articles with unsourced statements from April 2015
- Articles with unsourced statements from July 2018
- Hallucinations
- Neurological disorders
- Symptoms and signs: Skin and subcutaneous tissue
- RTT