Esophageal motility disorder
| Esophageal motility disorder | |
|---|---|
| Other names: Esophageal dysmotility (ED) | |
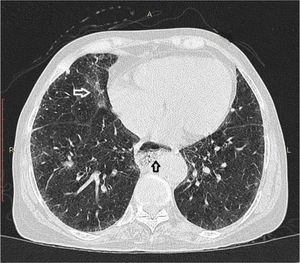 | |
| Esophageal dysmotility black arrow | |
| Specialty | Gastroenterology |
| Diagnostic method | Esophageal motility study Functional Lumen Imaging Probe |
| Treatment | Depends on cause |
An esophageal motility disorder (EMD) is any disorder causing difficulty in swallowing, regurgitation of food or a spasm-type pain. The most prominent one is dysphagia.
Esophageal motility disorder may be a result of CREST syndrome, referring to the five main features: calcinosis, Raynaud syndrome, esophageal dysmotility, sclerodactyly and telangiectasia.[1]
Types
Dysphagia could be for solids only, or for solids and liquids both.[citation needed]
- Solid dysphagia is due to obstructions such as esophageal cancer, esophageal webs, or stricture.
- Solid-and-liquid dysphagia is due to an esophageal motility disorder (or dysmotility) either in the upper esophagus (caused by, for example, myasthenia gravis, stroke, or dermatomyositis) or the lower esophagus (where causes include systemic sclerosis, CREST syndrome, or achalasia).
The most common form of dysphagia is achalasia, which is caused by degeneration of the nerves in the esophagus. This causes the muscles to stop working and prevents the valve at the bottom of the esophagus from being able to open properly.[2]
Signs and symptoms
Symptoms of EMD can include chest pain, and intermittent Dysphagia for solids, liquids, or both, and regurgitation.[3] There are contractions along the lower esophagus, and these contractions prevent the passage of food.[4]
Cause
The etiology of esophageal motility disorder is due to neuromuscular or structural disorders[5]
Diagnostics
Testing to diagnose an EMD include: Barium Esophagography, Upper Endoscopy, and Esophageal Manometry.[6]
Treatments
There is no cure for EMD, but symptoms can be managed. Some symptom management includes eating slower and taking smaller bites; in some cases medications can be useful to manage other issues that contribute to EMD such as a proton pump inhibitor to ease gastroesophageal reflux (acid reflux), or a smooth muscle relaxant for issues with the muscles.[6]
If there is a food allergy causing the dysmotility disorder, then physicians recommend an elimination diet. If this fails, then physicians will prescribe special types of medication to help resolve this problem.
See also
References
- ↑ Winterbauer RH (1964). "Multiple telangiectasia, Raynaud's phenomenon, sclerodactyly, and subcutaneous calcinosis: a syndrome mimicking hereditary hemorrhagic telangiectasia". Bulletin of the Johns Hopkins Hospital 114: 31–83. PMID 14171636.
- ↑ "Achalasia and Esophageal Motility Disorders". ctsurgerypatients.org. The Society of Thoracic Surgeons. Archived from the original on 16 November 2021. Retrieved 16 November 2021.
- ↑ Schlottmann, Francisco (2017). "Primary Esophageal Motility Disorders: Beyond Achalasia". International Journal of Molecular Sciences. 18 (7): 1399. doi:10.3390/ijms18071399. PMC 5535892. PMID 28665309.
- ↑ Medicine, UW. "Esophageal Motility Disorders - UW Medicine". www.uwmedicine.org. Archived from the original on 2018-09-27. Retrieved 2015-01-10.
- ↑ Goyal, Manjeet; Nagalli, Shivaraj (2022). "Esophageal Motility Disorders". StatPearls. StatPearls Publishing. Archived from the original on 24 July 2022. Retrieved 3 January 2023.
- ↑ 6.0 6.1 McQuaid, Kenneth (2022). Current Medical Diagnosis & Treatment 2022. McGraw Hill.
External links
| Classification | |
|---|---|
| External resources |