Macrocephaly
| Macrocephaly | |
|---|---|
 | |
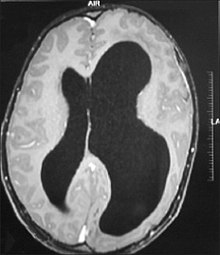
| An MRI of a patient with benign familial macrocephaly (male with head circumference > 60 cm) | |
Macrocephaly is a condition in which circumference of the human head is abnormally large.[1] It may be pathological or harmless, and can be a familial genetic characteristic. People diagnosed with macrocephaly will receive further medical tests to determine whether the syndrome is accompanied by particular disorders. Those with benign or familial macrocephaly are considered to have megalencephaly.
Signs and symptoms
Associated conditions
Below is a list of syndromes associated with macrocephaly that are noted in Signs and Symptoms of Genetic Conditions: A Handbook.[2]

Include multiple major and or minor anomalies
- Acrocallosal syndrome
- Apert syndrome
- Bannayan–Riley–Ruvalcaba syndrome
- Cardiofaciocutaneous syndrome
- Chromosome 14 - maternal disomy
- Chromosome 22qter deletion
- Cleidocranial dysostosis
- Costello syndrome
- Encephalocraniocutaneous lipomatosis
- FG syndrome
- Hallermann–Streiff syndrome
- Hydrolethalus syndrome
- Hypomelanosis syndrome
- Hypomelanosis of Ito
- Kelvin Peter anomaly plus syndrome
- Lujan–Fryns syndrome
- Macrocephaly-CM (MCAP)
- Marshall–Smith syndrome
- Neuhauser megalocornea/MR syndrome
- Neurofibromatosis type I
- Nevoid basal-cell carcinoma syndrome
- Noonan syndrome
- Ocular-ectodermal syndrome
- Osteopathia striata - cranial sclerosis
- Perlman syndrome
- Robinow syndrome
- Simpson–Golabi–Behmel syndrome
- Sotos syndrome
- Sturge–Weber syndrome
- Weaver syndrome
- Wiedemann–Rautenstrauch syndrome
- 3C syndrome

Secondary to a metabolic disorder
- Glutaric aciduria type II
- GM1 gangliosidosis
- Hunter syndrome
- Hurler syndrome
- MPS VII
- Sanfilippo syndrome
- Zellweger syndrome

Associated with a skeletal dysplasia
- Achondroplasia
- Campomelic dysplasia
- Craniodiaphyseal dysplasia
- Craniometaphyseal dysplasia
- Hypochondrogenesis
- Hypochondroplasia
- Kenny-Caffey syndrome
- Kniest dysplasia
- Lenz–Majewski syndrome
- Osteogenesis imperfecta III
- Osteopetrosis, autosomal recessive form
- Schneckenbecken dysplasia
- Sclerosteosis
- Short rib syndrome, beemer-langer type
- Short rib-polydactyly 2 (majewski type)
- Spondyloepiphyseal dysplasia congenita
- Thanatophoric dysplasia

With no obvious physical findings
- Alexander disease
- Canavan disease
- Cobalamin deficiency (combined methylmalonic aciduria and homocystinuria)
- Dandy–Walker malformation
- Glutaric aciduria type 1
- L-2-hydroxyglutaric aciduria
- Megalencephalic leukoencephalopathy with subcortical cysts
- Osteogenesis imperfecta IV
- Osteopathia striata-cranial sclerosis
- Periventricular heterotopia
- Sandhoff disease
- Tay–Sachs disease
Causes

Many people with abnormally large heads or large skulls are healthy, but macrocephaly may be pathological. Pathologic macrocephaly may be due to megalencephaly (enlarged brain), hydrocephalus (abnormally increased cerebrospinal fluid), cranial hyperostosis (bone overgrowth), and other conditions. Pathologic macrocephaly is called "syndromic", when it is associated with any other noteworthy condition, and "nonsyndromic" otherwise. Pathologic macrocephaly may be caused by congenital anatomic abnormalities, genetic conditions, or by environmental events.[3]
Many genetic conditions are associated with macrocephaly, including familial macrocephaly related to the holgate gene, autism, PTEN mutations such as Cowden disease, neurofibromatosis type 1, and tuberous sclerosis; overgrowth syndromes such as Sotos syndrome (cerebral gigantism), Weaver syndrome, Simpson–Golabi–Behmel syndrome (bulldog syndrome), and macrocephaly-capillary malformation (M-CMTC) syndrome; neurocardiofacial-cutaneous syndromes such as Noonan syndrome, Costello syndrome, Gorlin syndrome,[4] (also known as Basal Cell Nevus Syndrome) and cardiofaciocutaneous syndrome; Fragile X syndrome; leukodystrophies (brain white matter degeneration) such as Alexander disease, Canavan disease, and megalencephalic leukoencephalopathy with subcortical cysts; and glutaric aciduria type 1 and D-2-hydroxyglutaric aciduria.[3]
At one end of the genetic spectrum, duplications of chromosomes have been found to be related to autism and macrocephaly; at the other end, deletions of chromosomes have been found to be related to schizophrenia and microcephaly.[5][6][7]
Environmental events associated with macrocephaly include infection, neonatal intraventricular hemorrhage (bleeding within the infant brain), subdural hematoma (bleeding beneath the outer lining of the brain), subdural effusion (collection of fluid beneath the outer lining of the brain), and arachnoid cysts (cysts on the brain surface).[3]
In research, cranial height or brain imaging may be used to determine intracranial volume more accurately.[3]
Below is a list of causes of macrocephaly from Swaiman's Pediatric Neurology: Principles and Practice noted in The Little Black Book of Neurology:[8][9]
Hydrocephalus

Noncommunicating
- Arnold–Chiari malformation
- Aqueductal stenosis
- X-linked hydrocephalus with stenosis of the aqueduct of Sylvius (HSAS) syndrome (L1CAM)
- Dandy–Walker malformation
- Galenic vein aneurysm or malformation
- Neoplasms, supratentorial, and infratentorial
- Arachnoid cyst, infratentorial
- Holoprosencephaly with dorsal interhemispheric sac
Communicating
- External or extraventricular obstructive hydrocephalus (dilated subarachnoid space)
Arachnoid cyst, supratentorial
Meningeal fibrosis/obstruction
- Postinflammatory
- Posthemorrhagic
- Neoplastic infiltration

Vascular
Choroid plexus papilloma
Neurocutaneous syndromes
Destructive lesions

Familial, autosomal-dominant, autosomal-recessive, X-linked
Subdural fluid
Brain edema (toxic-metabolic)
- Intoxication
- Lead
- Vitamin A
- Tetracycline
- Endocrine (hypoparathyroidism, hypoadrenocorticism)
- Galactosemia
- Idiopathic (pseudotumorcerebri)
Thick skull or scalp (hyperostosis)

- Familial variation
- Anemia
- Osteoporosis, severe precocious autosomal-recessive osteoporosis (CLCN7, TCIRG1)
- Pycnodysostosis (CTSK)
- Craniometaphyseal dysplasia (ANKH)
- Craniodiaphyseal dysplasia
- Pyle dysplasia
- Sclerosteosis (SOST)
- Paget's disease[10]
- Idiopathic hyperphosphatasia
- Familial osteoectasia
- Osteogenesis imperfecta
- Rickets
- Cleidocranial dysostosis
- Hyperostosis corticalis generalisata (van Buchem disease)
- Proteus syndrome
Megalencephaly and hemimegalencephaly
Genetic
- Alpha-mannosidosis
- Atkin-Flaitz-Patil syndrome
- D-Bitfunctional protein deficiency
- Greig cephalopolysyndactyly syndrome
- Desmosterolosis
- Hyperostosis corticalis deformans juvenilis
- Legius syndrome
- Mucolipidosis II alpha/beta
- Mucopolysaccharidosis VII
- Muenke syndrome
- Opitz-Kaveggia syndrome
- Toriello-Carey syndrome
- Van der Knaap disease
- Waisman-Laxova syndrome
- Maple syrup urine disease
- Morquio syndrome
- Rubinstein-Taybi syndrome
- Tuberous sclerosis
- Cowden disease
- Congenital syphilis
Diagnosis
Macrocephaly is customarily diagnosed if head circumference is greater than two standard deviations (SDs) above the mean.[11] Relative macrocephaly occurs if the measure is less than two SDs above the mean, but is disproportionately above that when ethnicity and stature are considered. Diagnosis can be determined in utero or can be determined within 18–24 months after birth in some cases where head circumference tends to stabilize in infants.[12] Diagnosis in infants includes measuring the circumference of the child's head and comparing how significant it falls above the 97.5 percentile of children similar to their demographic. If falling above the 97.5th percentile then the patient will be checked to determine whether there is any intracranial pressure present and whether or not immediate surgery is needed.[2] If immediate surgery is not needed then further testing will be done to determine whether the patient has either macrocephaly or benign macrocephaly.
Diagnosis for macrocephaly involves the comparison of the infant's head circumference to that of other infants of the same age and ethnicity. If a patient is suspected of having macrocephaly molecular testing will be used to confirm diagnosis. Symptoms vary on the cause of macrocephaly on the child and if the child has any other accompanying syndromes which will be determined through molecular testing.
Benign or familial macrocephaly
Benign macrocephaly can occur without reason or be inherited by one or both parents (in which it is considered benign familial macrocephaly and is considered megalencephaly form of macrocephaly). Diagnoses for familial macrocephaly is determined by measuring the head circumference of both parents and comparing it to the child's. Benign and familial macrocephaly is not associated with neurological disorders.[2] While benign and familial macrocephaly does not result in neurological disorders, neurodevelopment will still be assessed.
Although neurological disorders do not occur, temporary symptoms of benign and familial macrocephaly include: developmental delay, epilepsy, and mild hypotonia.[2]
Neurodevelopment is assessed for all cases and suspected cases of macrocephaly to determine whether and what treatments may be needed, and whether any other syndrome/s may be present or likely to develop.
Treatment
Treatment varies depending on whether or not it occurs with other medical conditions in the child and where cerebrospinal fluid is present.[12] If benign and found between the brain and skull then no surgery is needed.[12][13] If excess fluid is found between the ventricle spaces in the brain then surgery will be needed.[13]
See also
References
- ↑ Toi A, Malinger G (2018). "36 - Cortical Development and Disorders". Obstetric imaging : fetal diagnosis and care (2nd ed.). Philadelphia, PA. ISBN 978-0-323-44548-1. Archived from the original on 24 March 2021.
- ↑ 2.0 2.1 2.2 2.3 Signs and symptoms of genetic conditions : a handbook. Hudgins, Louanne,, Toriello, Helga V.,, Enns, Gregory M.,, Hoyme, H. Eugene. Oxford. 30 May 2014. ISBN 978-0-19-938869-1. OCLC 879421703.
{{cite book}}: CS1 maint: others (link) - ↑ 3.0 3.1 3.2 3.3 Williams CA, Dagli A, Battaglia A (2008). "Genetic disorders associated with macrocephaly". Am J Med Genet A. 146A (16): 2023–37. doi:10.1002/ajmg.a.32434. PMID 18629877. S2CID 205309800.
- ↑ "Archived copy" (PDF). Archived from the original (PDF) on 2015-10-09. Retrieved 2015-05-04.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ Crespi; et al. (2010). "Comparative genomics of autism and schizophrenia". PNAS. 107 (Suppl 1): 1736–1741. doi:10.1073/pnas.0906080106. PMC 2868282. PMID 19955444.
- ↑ International Schizophrenia Consortium (September 2008). "Rare chromosomal deletions and duplications increase risk of schizophrenia; The International Schizophrenia Consortium;". Nature. 455 (7210): 237–241. doi:10.1038/nature07239. PMC 3912847. PMID 18668038.
- ↑ Dumas L.; Sikela J.M. (2009). "DUF1220 Domains, Cognitive Disease, and Human Brain Evolution". Cold Spring Harb. Symp. Quant. Biol. 74: 375–82. doi:10.1101/sqb.2009.74.025. PMC 2902282. PMID 19850849.
- ↑ Cooke, Rachel. "ProQuest Ebook Central". doi:10.5260/cca.199425.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Swaiman, Kenneth F.; Ashwal, Stephen; Ferriero, Donna M.; Schor, Nina F. (2012), "Preface to the Fifth Edition", Swaiman's Pediatric Neurology, Elsevier, pp. xiii–xiv, doi:10.1016/b978-1-4377-0435-8.00116-5, ISBN 978-1-4377-0435-8
- ↑ 10.0 10.1 Williams CA, Dagli A. (2008). "Genetic disorders associated with macrocephaly". Am J Med Genet A. 146A (16): 2023–37. doi:10.1002/ajmg.a.32434. Archived from the original on 2023-01-16. Retrieved 2023-02-17.
- ↑ Fenichel, Gerald M. (2009). Clinical Pediatric Neurology: A Signs and Symptoms Approach (6th ed.). Philadelphia, PA: Saunders/Elsevier. p. 369. ISBN 978-1416061854.
- ↑ 12.0 12.1 12.2 "Macrocephaly | Nicklaus Children's Hospital". www.nicklauschildrens.org. Archived from the original on 2020-09-19. Retrieved 2020-04-11.
- ↑ 13.0 13.1 "Macrocephaly or "Big Head"". Department of Neurosurgery. Archived from the original on 2020-08-05. Retrieved 2020-04-27.
External links
- GeneReviews/NCBI/NIH/UW entry on PTEN Hamartoma Tumor Syndrome (PHTS) Archived 2010-10-05 at the Wayback Machine
- GeneReviews/NCBI/NIH/UW entry on 9q22.3 Microdeletion Archived 2019-01-10 at the Wayback Machine
| Classification | |
|---|---|
| External resources |