Pseudopseudohypoparathyroidism
| Pseudopseudohypoparathyroidism | |
|---|---|
| Usual onset | Before birth |
| Duration | Lifetime |
| Differential diagnosis | Pseudohypoparathyroidism, hypoparathyroidism, Albright's hereditary osteodystrophy |
| Treatment | Treatments to reduce symptoms, genetic counseling |
Pseudopseudohypoparathyroidism (PPHP) is an inherited disorder,[1] named for its similarity to pseudohypoparathyroidism in presentation. It is more properly Albright hereditary osteodystrophy although without resistance of parathyroid hormone as frequently seen in that affliction. The term Pseudopseudohypoparathyroidism is used to describe a condition where the individual has the phenotypic appearance of Pseudohypoparathyroidism type 1a, but has (unexpected for the phenotype) normal labs including calcium and PTH.[2]
It can be considered a variant of Albright hereditary osteodystrophy,[3] or Pseudohypoparathyroidism type 1A, as they present with the same constellation of signs and symptoms, including short stature, brachydactyly, subcutaneous calcification, and obesity.
Signs and symptoms
Pseudopseudohypoparathyroidism can be best understood by comparing it to other conditions:
| Condition | Appearance | PTH levels | Calcitriol | Calcium | Phosphates | Imprinting | |
|---|---|---|---|---|---|---|---|
| Hypoparathyroidism | Normal | Low | Low | Low | High | Not applicable | |
| Pseudohypoparathyroidism | Type 1A | Skeletal defects | High | Low | Low | High | Gene defect from mother (GNAS1) |
| Type 1B | Normal | High | Low | Low | High | Gene defect from mother (GNAS1 and STX16) | |
| Type 2 | Normal | High | Low | Low | High | ? | |
| Pseudopseudohypoparathyroidism | Skeletal defects | Normal | Normal | Normal[4] | Normal | Gene defect from father | |
Hormone resistance is not present in Pseudopseudohypoparathyroidism.[5] Short stature may be present. Obesity is less common in Pseudopseudohypoparathyroidism than in Pseudohypoparathyroidism.[6] Osteoma cutis may be present.[7]
Genetics
A male with Pseudohypoparathyroidism has a 50% chance of passing on the defective GNAS gene to his children, although in an imprinted, inactive form. Any of his children receiving this gene will have Pseudopseudohypoparathyroidism. Any of his daughters that have Pseudopseudohypoparathyroidism may in turn pass along Pseudohypoparathyroidism 1A to her children as the imprinting pattern on the inherited paternal gene will be changed to the maternal pattern in the mother's ovum during meiosis. The gene will be reactivated in any children who inherit it.[citation needed]
Pseudopseudohypoparathyroidism and pseudohypoparathyroidism both involve the same GNAS gene,[8] but Pseudopseudohypoparathyroidism has normal calcium homeostasis because of the normal maternal allele in the kidney.[9]
Pathophysiology
The GNAS1 gene involved in both Pseudohypoparathyroidism type 1a and Pseudopseudohypoparathyroidism is greatly affected by imprinting. When a father who has Pseudohypoparathyroidism undergoes spermatogenesis, imprinting of the GNAS1 gene inactivates both copies of his genes: one will be Functional and the other will be defective. Tissues in the body will re-activate different copies of the GNAS1 gene selectively; the kidneys will selectively activate the (functional) maternal copy while keeping the (defective) paternally-derived gene imprinted and inactive, even in normal individuals. Since the maternally-derived GNAS1 gene is functional, renal handling of calcium and phosphate is normal, and homeostasis is maintained in Pseudopseudohypoparathyroidism. However, the rest of the tissues will instead selectively display the defective gene, resulting in haploinsufficiency of the GNAS1 product in most tissues, and giving the phenotype of Pseudohypoparathyroidism type 1a. As a result, there is also a normal response of urinary cAMP to PTH, and normal serum PTH.[citation needed]
Diagnosis
The diagnosis is based on the presence of the Albright hereditary osteodystrophy pseudotype but without the PTH resistance. Blood tests including calcium, phosphate, and PTH will exclude other forms of Pseudohypoparathyroidism. X-rays may reveal a short fourth metacarpal. Genetic testing can confirm the diagnosis by showing GNAS gene mutation.[1]
Treatment
Treatments focuses on symptoms, with genetic counseling recommended.[10]
History
It was characterized in 1952 by Fuller Albright as "pseudo-pseudohypoparathyroidism" (with hyphen).[11][12]
See also
- Antidisestablishmentarianism
- Floccinaucinihilipilification
- GNAS complex locus
- Honorificabilitudinitatibus
- Longest word in English
- Longest words
- Parathyroid hormone
- Pneumonoultramicroscopicsilicovolcanoconiosis
- Supercalifragilisticexpialidocious
References
- ↑ 1.0 1.1 "Pseudopseudohypoparathyroidism | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 2020-07-17. Retrieved 2017-01-31.
- ↑ Tafaj, O.; Jüppner, H. (April 2017). "Pseudohypoparathyroidism: one gene, several syndromes". Journal of Endocrinological Investigation. 40 (4): 347–356. doi:10.1007/s40618-016-0588-4. ISSN 1720-8386. PMID 27995443. S2CID 20811779.
- ↑ Solomon SS, Kerlan RM, King LE, Jones GM, Hashimoto K (January 1975). "Pseudopseudohypoparathyroidism with fibrous dysplasia". Arch Dermatol. 111 (1): 90–3. doi:10.1001/archderm.111.1.90. PMID 1119829.
- ↑ Shahid Hussain; Sharif Aaron Latif; Adrian Hall (1 July 2010). Rapid Review of Radiology. Manson Publishing. pp. 262–. ISBN 978-1-84076-120-7. Retrieved 30 October 2010.
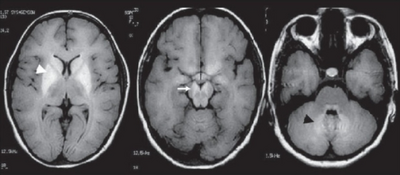
- ↑ Mouallem M, Shaharabany M, Weintrob N, et al. (February 2008). "Cognitive impairment is prevalent in pseudohypoparathyroidism type Ia, but not in pseudopseudohypoparathyroidism: possible cerebral imprinting of Gsalpha". Clin. Endocrinol. 68 (2): 233–9. doi:10.1111/j.1365-2265.2007.03025.x. PMID 17803690. S2CID 23654317.
- ↑ Long DN, McGuire S, Levine MA, Weinstein LS, Germain-Lee EL (March 2007). "Body mass index differences in pseudohypoparathyroidism type 1a versus pseudopseudohypoparathyroidism may implicate paternal imprinting of Galpha(s) in the development of human obesity". J. Clin. Endocrinol. Metab. 92 (3): 1073–9. doi:10.1210/jc.2006-1497. PMID 17164301. Archived from the original on 2020-08-29. Retrieved 2022-04-10.
- ↑ Jeong KH, Lew BL, Sim WY (May 2009). "Osteoma cutis as the presenting feature of albright hereditary osteodystrophy associated with pseudopseudohypoparathyroidism". Ann Dermatol. 21 (2): 154–8. doi:10.5021/ad.2009.21.2.154. PMC 2861203. PMID 20523775. Archived from the original on 2012-03-15. Retrieved 2010-10-30.
- ↑ Lebrun M, Richard N, Abeguilé G, et al. (June 2010). "Progressive osseous heteroplasia: a model for the imprinting effects of GNAS inactivating mutations in humans". J. Clin. Endocrinol. Metab. 95 (6): 3028–38. doi:10.1210/jc.2009-1451. PMID 20427508. Archived from the original on 2020-08-29. Retrieved 2022-04-10.
- ↑ David Terris; Christine G. Gourin (15 November 2008). Thyroid and Parathyroid Diseases: Medical and Surgical Management. Thieme. pp. 193–. ISBN 978-1-58890-518-5. Archived from the original on 18 December 2022. Retrieved 30 October 2010.
- ↑ Simpson, Catherine (21 March 2015). "Pseudopseudohypothyroidism" (PDF). The Lancet. 385 (9973): 1123. doi:10.1016/s0140-6736(14)61640-8. PMID 25484027. S2CID 208793989. Archived (PDF) from the original on 29 August 2020. Retrieved 10 April 2022.
- ↑ Philip R. Beales; I. Sadaf Farooqi; Stephen O'Rahilly (12 September 2008). The genetics of obesity syndromes. Oxford University Press US. pp. 91–. ISBN 978-0-19-530016-1. Archived from the original on 18 December 2022. Retrieved 30 October 2010.
- ↑ ALBRIGHT F, FORBES AP, HENNEMAN PH (1952). "Pseudo-pseudohypoparathyroidism". Trans. Assoc. Am. Physicians. 65: 337–50. PMID 13005676.
External links
| Classification |
|---|
| Look up pseudopseudohypoparathyroidism in Wiktionary, the free dictionary. |