Pseudohypoparathyroidism
| Pseudohypoparathyroidism | |
|---|---|
 | |
| Short 3rd to 5th metatarsals as may be seen in pseudohypoparathyroidism type 1a and 1c | |
| Specialty | Endocrinology |
| Symptoms | Numbness, muscle spasms[1] |
| Complications | Arrhythmias, growth hormone deficiency[1] |
| Usual onset | Childhood[1] |
| Duration | Long term[1] |
| Types | 1a, 1b, 1c, 2[1] |
| Causes | Genetic mutation[1] |
| Risk factors | Family history[1] |
| Diagnostic method | Low calcium, high phosphate, high PTH, genetic testing[1][2] |
| Differential diagnosis | Hypoparathyroidism, vitamin D deficiency, chronic kidney disease[1] |
| Treatment | Calcitriol, calcium supplementation[1] |
| Frequency | 0.3 to 1.1 per 100,000 people[1] |
Pseudohypoparathyroidism is a condition that occurs due to resistance to parathyroid hormone (PTH).[1] This results in low calcium and high phosphate, with symptoms including numbness and muscle spasms.[1] Certain types are also associated with obesity, sleep apnea, and intellectual disability.[1] Complications may include arrhythmias, cataracts, and growth hormone deficiency.[1][2]
It occurs due to a genetic mutation; either inherited from a person's parents or occurring in early development.[1][3] It may be inherited in an X-linked dominant or autosomal dominant manner.[4] It is divided into type 1a, 1b, 1c, and 2.[1] It differs from hypoparathyroidism by PTH levels being high.[1] Vitamin D levels are generally normal.[1] Confirmation of the diagnosis is by genetic testing.[2]
Treatment is typically with calcitriol to maintain calcium levels in the normal range.[1] If this is not sufficient calcium supplementation may be used.[1] Intravenous calcium gluconate may be used in people with calcium levels bellow 7.5 mg/dL.[1]
Pseudohypoparathyroidism affects 0.3 to 1.1 per 100,000 people.[1] The condition is usually discovered in early childhood.[1] Long term outcomes are variable.[1] The condition was first described in 1942 by Fuller Albright.[5]
Signs and symptom
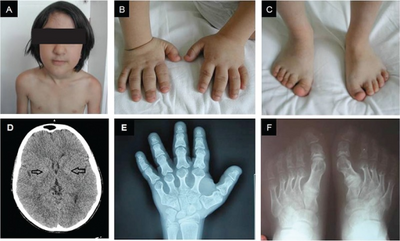
Patients may present with features of hypocalcaemia including carpo-pedal muscular spasms, cramping, tetany, and if the calcium deficit is severe, generalized seizures. IQ is typically mildly depressed or unaffected. Additional characteristics include short stature, obesity, developmental delay, and calcification of the basal ganglia in the deep white matter of the brain.[citation needed]
Type 1a Pseudohypoparathyroidism is clinically manifest by bone resorption with blunting of the fourth and fifth knuckles of the hand, most notable when the dorsum of the hand is viewed in closed fist position. This presentation is known as 'knuckle knuckle dimple dimple' sign (Archibald's sign). This is as opposed to Turner syndrome which is characterized by blunting of only the fourth knuckle, and Down syndrome, which is associated with a hypoplastic middle phalanx.
Related conditions
The term pseudopseudohypoparathyroidism is used to describe a condition where the individual has the phenotypic appearance of pseudohypoparathyroidism type 1a, but is biochemically normal.
| Condition | Appearance | PTH levels | Calcitriol | Calcium | Phosphates | Imprinting | |
|---|---|---|---|---|---|---|---|
| Hypoparathyroidism | Normal | Low | Low | Low | High | Not applicable | |
| Pseudohypoparathyroidism | Type 1A | Skeletal defects | High | Low | Low | High | Gene defect from mother (GNAS1) |
| Type 1B | Normal | High | Low | Low | High | Likely a gene defect from mother (GNAS1 and STX16) however it can also be the result of an imprinting issue of (GNAS1) due to mother and father in equal measure | |
| Type 2 | Normal | High | Low | Low | High | ? | |
| Pseudopseudohypoparathyroidism | Skeletal defects | Normal | Normal | Normal[7] | Normal | gene defect from father | |
Diagnosis
Biochemical findings
- hypocalcemia
- hyperphosphatemia
- elevated parathyroid hormone (hyperparathyroidism)
- Suppressed calcitriol levels[8]
Types
Types include:
- Type 1a (OMIM 103580)
- Has a characteristic phenotypic appearance (Albright's hereditary osteodystrophy), including short fourth and fifth metacarpals and a rounded facies. It is most likely an autosomal dominant disorder.[9] It is also associated with thyroid stimulating hormone resistance. Caused by GNAS1 mutation.[10]
- Type 1b (OMIM 603233)
- Lacks the physical appearance of type 1a, but is biochemically similar.[11] It is associated with a methylation defect in the A/B exon of GNAS1, caused by STX16 disruption.[12][13]
- Type 2 (OMIM 203330)
- Also lacks the physical appearance of type 1a.[14] Since the genetic defect in type 2 is further down the signalling pathway than in type 1, there is a normal cAMP response to PTH stimulation despite the inherent abnormality in calcium regulation. The specific gene is not identified.
While biochemically similar, type 1 and 2 disease may be distinguished by the differing urinary excretion of cyclic AMP in response to exogenous PTH.
Some sources also refer to a "type 1c" (OMIM 612462).[15] The phenotype is the same as in type 1a, but red blood cells show normal Gs activity. As it is also caused by a GNAS mutation, it is not clear whether it should be considered an entity separate from Ia.[16]
Treatment
Calcium and Calcitriol supplements, the latter with a larger dose than for treatment of hypoparathyroidism.[citation needed]
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 Ucciferro, Peter; Anastasolpoulou, Catherine (10 August 2020). Pseudohypoparathyroidism. Treasure Island (FL): StatPearls Publishing. Archived from the original on 29 August 2021. Retrieved 2 May 2021.
- ↑ 2.0 2.1 2.2 "Pseudohypoparathyroidism - About the Disease - Genetic and Rare Diseases Information Center". rarediseases.info.nih.gov. Archived from the original on 28 January 2022. Retrieved 21 July 2022.
- ↑ Mantovani, G; Bastepe, M; Monk, D; de Sanctis, L; Thiele, S; Usardi, A; Ahmed, SF; Bufo, R; Choplin, T; De Filippo, G; Devernois, G; Eggermann, T; Elli, FM; Freson, K; García Ramirez, A; Germain-Lee, EL; Groussin, L; Hamdy, N; Hanna, P; Hiort, O; Jüppner, H; Kamenický, P; Knight, N; Kottler, ML; Le Norcy, E; Lecumberri, B; Levine, MA; Mäkitie, O; Martin, R; Martos-Moreno, GÁ; Minagawa, M; Murray, P; Pereda, A; Pignolo, R; Rejnmark, L; Rodado, R; Rothenbuhler, A; Saraff, V; Shoemaker, AH; Shore, EM; Silve, C; Turan, S; Woods, P; Zillikens, MC; Perez de Nanclares, G; Linglart, A (August 2018). "Diagnosis and management of pseudohypoparathyroidism and related disorders: first international Consensus Statement". Nature reviews. Endocrinology. 14 (8): 476–500. doi:10.1038/s41574-018-0042-0. PMID 29959430.
- ↑ Sencen, Lisa. "Pseudohypoparathyroidism". NORD (National Organization for Rare Disorders). Archived from the original on 24 November 2021. Retrieved 21 July 2022.
- ↑ Camacho, Pauline M. (22 February 2019). Metabolic Bone Diseases: A Case-Based Approach. Springer. p. 58. ISBN 978-3-030-03694-2. Archived from the original on 29 July 2022. Retrieved 21 July 2022.
- ↑ Şahin, S; Hiort, O; Thiele, S; Evliyaoğlu, O; Tüysüz, B (1 March 2017). "Follow-up Findings in a Turkish Girl with Pseudohypoparathyroidism Type Ia Caused by a Novel Heterozygous Mutation in the GNAS Gene". Journal of clinical research in pediatric endocrinology. 9 (1): 74–79. doi:10.4274/jcrpe.3191. PMID 27425121.
- ↑ Shahid Hussain; Sharif Aaron Latif; Adrian Hall (1 July 2010). Rapid Review of Radiology. Manson Publishing. pp. 262–. ISBN 978-1-84076-120-7. Retrieved 30 October 2010.
- ↑ Levine, Michael. "Pseudohypoparathyroidism: A Variation on the Theme of Hypoparathyroidism" (PDF). Archived from the original (PDF) on 2016-03-04. Retrieved 2021-05-02.
- ↑ Online Mendelian Inheritance in Man (OMIM): 103580
- ↑ de Nanclares GP, Fernández-Rebollo E, Santin I, et al. (June 2007). "Epigenetic defects of GNAS in patients with pseudohypoparathyroidism and mild features of Albright's hereditary osteodystrophy". J. Clin. Endocrinol. Metab. 92 (6): 2370–3. doi:10.1210/jc.2006-2287. PMID 17405843. Archived from the original on 2021-08-29. Retrieved 2021-05-02.
- ↑ Online Mendelian Inheritance in Man (OMIM): 603233
- ↑ Laspa E, Bastepe M, Jüppner H, Tsatsoulis A (December 2004). "Phenotypic and molecular genetic aspects of pseudohypoparathyroidism type Ib in a Greek kindred: evidence for enhanced uric acid excretion due to parathyroid hormone resistance". J. Clin. Endocrinol. Metab. 89 (12): 5942–7. doi:10.1210/jc.2004-0249. PMID 15579741. Archived from the original on 2021-08-29. Retrieved 2021-05-02.
- ↑ Fröhlich LF, Bastepe M, Ozturk D, Abu-Zahra H, Jüppner H (June 2007). "Lack of Gnas epigenetic changes and pseudohypoparathyroidism type Ib in mice with targeted disruption of syntaxin-16". Endocrinology. 148 (6): 2925–35. doi:10.1210/en.2006-1298. PMID 17317779. Archived from the original on 2021-08-29. Retrieved 2021-05-02.
- ↑ Online Mendelian Inheritance in Man (OMIM): 203330
- ↑ Aldred MA (May 2006). "Genetics of pseudohypoparathyroidism types Ia and Ic". J. Pediatr. Endocrinol. Metab. 19 (Suppl 2): 635–40. doi:10.1515/jpem.2006.19.s2.635. PMID 16789628. S2CID 26538688.
- ↑ Bastepe, M (2008). "The GNAS locus and pseudohypoparathyroidism". Advances in Experimental Medicine and Biology. 626: 27–40. doi:10.1007/978-0-387-77576-0_3. ISBN 978-0-387-77575-3. PMID 18372789.
Further reading
- Mantovani, G; Bastepe, M; Monk, D; de Sanctis, L; Thiele, S; Usardi, A; Ahmed, SF; Bufo, R; Choplin, T; De Filippo, G; Devernois, G; Eggermann, T; Elli, FM; Freson, K; García Ramirez, A; Germain-Lee, EL; Groussin, L; Hamdy, N; Hanna, P; Hiort, O; Jüppner, H; Kamenický, P; Knight, N; Kottler, ML; Le Norcy, E; Lecumberri, B; Levine, MA; Mäkitie, O; Martin, R; Martos-Moreno, GÁ; Minagawa, M; Murray, P; Pereda, A; Pignolo, R; Rejnmark, L; Rodado, R; Rothenbuhler, A; Saraff, V; Shoemaker, AH; Shore, EM; Silve, C; Turan, S; Woods, P; Zillikens, MC; Perez de Nanclares, G; Linglart, A (August 2018). "Diagnosis and management of pseudohypoparathyroidism and related disorders: first international Consensus Statement" (PDF). Nature Reviews. Endocrinology. 14 (8): 476–500. doi:10.1038/s41574-018-0042-0. PMC 6541219. PMID 29959430. Archived (PDF) from the original on 2021-08-29. Retrieved 2021-05-02.
External links
| Classification | |
|---|---|
| External resources |