User:QuackGuru/Sand 25
https://pubmed.ncbi.nlm.nih.gov/31252671/ E-Cigarettes are More Addictive than Traditional Cigarettes-A Study in Highly Educated Young People
Fig. 4
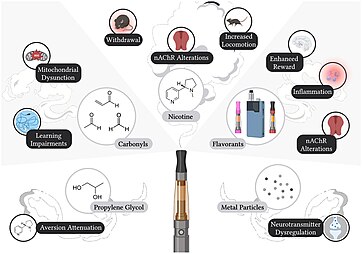
Health hazards of e-cigarette use
Developmental nicotine exposure engenders intergenerational downregulation and aberrant posttranslational modification of cardinal epigenetic factors in the frontal cortices, striata, and hippocampi of adolescent mice
https://pubmed.ncbi.nlm.nih.gov/?linkname=pubmed_pubmed_citedin&from_uid=32138755
https://pubmed.ncbi.nlm.nih.gov/37286509/ [3] (PMCID: available on 2024-06-07)
https://pubmed.ncbi.nlm.nih.gov/36804178/ [4]
https://pubmed.ncbi.nlm.nih.gov/36777290/ [5]
https://pubmed.ncbi.nlm.nih.gov/36728241/ [6] (PMCID: available on 2024-04-01)
https://pubmed.ncbi.nlm.nih.gov/36900893/ [7]
https://pubmed.ncbi.nlm.nih.gov/37185310/ [8]
https://pubmed.ncbi.nlm.nih.gov/36736923/ [9]
https://pubmed.ncbi.nlm.nih.gov/36370069/ [10]
https://pubmed.ncbi.nlm.nih.gov/37314028/ [11]
https://pubmed.ncbi.nlm.nih.gov/34615737/ [12]
https://pubmed.ncbi.nlm.nih.gov/37320902/ [13]
https://pubmed.ncbi.nlm.nih.gov/36915837/ [14]
https://pubmed.ncbi.nlm.nih.gov/36806607/ [15]
https://pubmed.ncbi.nlm.nih.gov/36773789/ [16]
https://pubmed.ncbi.nlm.nih.gov/37183777/ [17]
https://pubmed.ncbi.nlm.nih.gov/36399154/ [18]
https://pubmed.ncbi.nlm.nih.gov/36882378/ [19] (PMCID: available on 2024-07-01)
https://pubmed.ncbi.nlm.nih.gov/37202029/ [20]
https://pubmed.ncbi.nlm.nih.gov/36804352/ [21]
https://pubmed.ncbi.nlm.nih.gov/36120959/ [22]
https://pubmed.ncbi.nlm.nih.gov/36735735/ [23]
https://pubmed.ncbi.nlm.nih.gov/36833024/ [24]
https://pubmed.ncbi.nlm.nih.gov/36427562/ [25]
https://pubmed.ncbi.nlm.nih.gov/35998874/ [26]
https://pubmed.ncbi.nlm.nih.gov/36641959/ [27]
https://pubmed.ncbi.nlm.nih.gov/37295941/ [28]
https://pubmed.ncbi.nlm.nih.gov/36736944/ [29]
https://pubmed.ncbi.nlm.nih.gov/37290827/ [30]
https://pubmed.ncbi.nlm.nih.gov/37159065/ [31]
https://pubmed.ncbi.nlm.nih.gov/36767274/ [32]
https://pubmed.ncbi.nlm.nih.gov/36808672/ [33]
https://pubmed.ncbi.nlm.nih.gov/36208090/ [34]
Unable to open[35]
https://pubmed.ncbi.nlm.nih.gov/35787100/ (available on 2024-02-01)


The benefits and the health effects of electronic cigarettes are uncertain.[42] There is considerable variation among e-cigarettes and in their liquid ingredients and as a consequence there are differences in the aerosol delivered to the user.[43] Regulated US Food and Drug Administration (FDA) products such as nicotine inhalers may be safer than e-cigarettes,[44] but e-cigarettes are generally seen as safer than combusted tobacco products[note 1][50] such as cigarettes and cigars.[51] Since vapor does not contain tobacco and does not involve combustion, users may avoid several harmful constituents usually found in tobacco smoke,[52] such as ash, tar, and carbon monoxide.[53] However, vaping is more dangerous in the short-term than smoking.[48][54] Because of the risk of nicotine exposure to the fetus and adolescent causing long-term effects to the growing brain, the World Health Organization does not recommend it for children, adolescents, pregnant women, and women of childbearing age.[55] Vaping itself has no proven benefits[48] and with or without nicotine it cannot be considered harmless.[56] Their indiscriminate use is a threat to public health.[57]
The long-term effects of e-cigarette use are unknown[58][59][60] and unclear.[61] Short-term use may lead to death.[48] Less serious adverse effects include abdominal pain, headache, blurry vision,[62] throat and mouth irritation, vomiting, nausea, and coughing.[43] They may produce similar adverse effects compared to tobacco use.[63] E-cigarettes reduce lung function, reduce cardiac muscle function, and increase inflammation.[64] In 2019 and 2020, there was an outbreak of severe lung illness linked to vaping in the US[65] and Canada,[66] with 68 confirmed deaths in the US,[note 2][65] and one confirmed death in Europe.[71] There are also risks from misuse or accidents[52] such as nicotine poisoning (especially among small children[72]),[73] contact with liquid containing nicotine,[74] fires caused by vaporizer malfunction,[43] and explosions resulting from extended charging, unsuitable chargers, design flaws,[52] or user modifications.[75] Battery explosions are caused by an increase in internal battery temperature and some have resulted in severe skin burns.[76] There is a small risk of a battery explosion in devices modified to increase battery power.[77]
The cytotoxicity of e-liquids varies,[78] and contamination with various chemicals have been detected in the liquid.[79] Metal parts of e-cigarettes in contact with the e-liquid can contaminate it with metal particles.[52] Many chemicals including carbonyl compounds such as formaldehyde can inadvertently be produced when the nichrome wire (heating element) that touches the e-liquid is heated and chemically reacted with the liquid.[80] The later-generation and "tank-style" e-cigarettes with a higher voltage (5.0 V[78]) may generate equal or higher levels of formaldehyde compared to smoking.[81] Nicotine is associated with cardiovascular disease, increased serum cholesterol levels, and possible birth defects.[82] Children, youth,[47] and young adults are especially sensitive to the effects of nicotine.[83] Several studies demonstrate nicotine is carcinogenic.[84] Public health authorities do not recommend nicotine use for non-smokers.[85] Propylene glycol, glycerin, volatile organic compounds, and free radicals can impair lung health.[86] Many flavors are irritants[87] and certain flavoring agents can induce respiratory toxicity.[88]
E-cigarettes create vapor that consists of fine and ultrafine particles of particulate matter, with the majority of particles in the ultrafine range.[43] The vapor contains propylene glycol, glycerin, nicotine, flavors, small amounts of toxicants,[43] carcinogens,[note 3][89] and heavy metals, as well as metal nanoparticles, and other substances.[43] Exactly what the vapor consists of varies significantly in composition and concentration across and within brands, and depends on the e-liquid contents, the device design, and user behavior, among other factors.[note 4][90] E-cigarette vapor potentially contains harmful chemicals not found in tobacco smoke[91] such as propylene glycol.[92] E-cigarette vapor contains fewer toxic chemicals,[43] and lower concentrations of potentially toxic chemicals than in cigarette smoke.[93] Concern exists that the exhaled e-cigarette vapor may be inhaled by bystanders, particularly indoors.[94] There is limited information available on the environmental issues around production, use, and disposal of e-cigarettes that use cartridges.[95] E-cigarettes that are not reusable may contribute to the problem of electronic waste.[96]
Health effects
Overview of benefits and effects

Reviews on the safety of electronic cigarettes, evaluating roughly the same studies, have reached significantly different conclusions.[99] Broad-ranging statements regarding their safety cannot be reached because of the vast differences of devices and e-liquids available.[100] A consensus has not been established for the benefits as well as the effects related to their use.[88] A substantial amount of research has been conducted in the past decade prior to 2020 to examine the health effects of e-cigarette use, often providing conflicting evidence and claims.[42] What will cause the most or least undesirable effects of various blends of solvents, flavoring, and nicotine in e-liquids is unknown.[83]
There is considerable variation in e-cigarette product technologies as well as differing amounts of chemicals in their liquid solution, including an assortment of nicotine strengths and a vast array of additives and flavors, and as a consequence there are differences in the contents of the aerosol inhaled as well as exhaled by the user.[43] Due to the large variation in the quantities of each constituent across products and an ever-evolving product marketplace, it is challenging to fully understand the clinical relevance of e-cigarette use on the individual's health.[40] Although there is inconsistencies among the methodologies used (detection method, liquid or aerosol, animal models, conditions), the data generated by these investigations remains informative.[101] Moreover, due to various methodological issues, severe conflicts of interest, and inconsistent research, no firm views can be made regarding their effects.[102] However, e-cigarette use with or without nicotine cannot be considered harmless.[56] Nicotine-free e-cigarette aerosol contains chemicals that cause cancer as well as chemicals associated with severe lung damage.[61]
E-cigarettes cannot be considered absolutely safe because there is no safe level for carcinogens.[103] An uncountable amount of studies aimed at evaluating e-cigarette potential consequences on human health and the most updated panorama of scientific literature provides increasing evidence of vaping harmfulness.[104] Among e-cigarettes adverse health effects, respiratory impact is by far the most extensively studied.[104] Nicotine is the most studied biologically active chemical present in e-cigarettes, and several of the cardiovascular effects of e-cigarettes have been attributed to this alkaloid from the tobacco plant.[105] Nicotine has well-established effects on the metabolism and cardiovascular system.[105] In the same way as conventional cigarettes smokers, vapers' pulmonary epithelium is typically damaged and bronchial mucosa chronically inflamed.[104] Vaping has been promoted as being safer than cigarette smoking, though users can be inhaling toxicants such as diacetyl and carcinogens such as formaldehyde[106] and users can be inhaling contaminants such as traces of arsenic and other heavy metals.[63] Because of the belief that vaping is less dangerous than traditional cigarettes, vapers may vape products at a more frequent pace than traditional cigarettes and, as a consequence, produce higher levels of second-hand contaminants.[107] Vaping itself has no proven benefits,[48] and it is a deliberate exposure in contrast to numerous other toxicological exposures.[108] The potential benefits of nicotine vaping are significantly outweighed by its unwanted effects, such as threat of addiction, cancer, heart disease, hypertension, respiratory infections, and gastrointestinal discomfort.[109]

E-cigarettes were initially positioned as a "healthy alternative", though they may produce similar adverse effects compared to tobacco use.[63] There is emerging evidence demonstrating adverse effects attributable to e-cigarette use on every single human organ system.[111] Whether e-cigarettes are helping smokers or creating a new source of addiction is extensively being debated.[112] The overall public health effect related to their use is actively debated.[113] Available evidence on the benefits and risks of e-cigarette use are mixed and interpreted differently.[114] Some believe that e-cigarettes have the potential to reduce the burden of disease in smokers while others worry about the impact on public health and do not recommend, and even ban, their use.[114] Debates about the population health impact of alternative nicotine delivery products (i.e., e-cigarettes) are ongoing.[114]
Limited research
The long-term consequences from e-cigarette use on death and disease are unclear.[115] The risks from long-term use of nicotine as well as other toxicants that are unique to e-cigarettes are uncertain.[116] The potential long-term effects of e-cigarette consumption have been scarcely investigated.[117] Disease caused by tobacco has a latency period of no less than 25 years.[118] Therefore, as of 2019, it will conservatively take two decades until firm conclusions from long-term studies on using e-cigarettes are published.[118] Epidemiological data on cancer findings takes at least 20 to 40 years to become available.[119] As of 2023, evidence of the harms of e-cigarettes has been unfolding slowly and has been documented in many reviews and reports worldwide.[120]
The health effects related to e-cigarette use is mostly unknown.[121] Most of the available articles reported are limited in their design, methodology, and the used exposure time and had a lack of long-term follow-up.[122] There is insufficient data regarding the health benefits of vaping.[123] E-cigarettes have the potential for benefit and harm, the nature and scale of each being uncertain in the absence of ample evidence.[124] There is limited available research regarding their effects on vulnerable groups such as minors.[125] The effect on population health from e-cigarettes is unknown.[44] The chemical characteristics of the short-lived free radicals and long-lived free radicals produced from e-cigarettes is unclear.[126] The knowledge of possible acute and long-term health effects of aerosols inhaled from e-cigarettes is limited partially due to incomplete awareness of physical phenomena related to e-cigarette aerosol dynamics.[127]
In August 2014, the Forum of International Respiratory Societies stated that e-cigarettes have not been demonstrated to be safe.[128] Health Canada has stated that, "their safety, quality, and efficacy remain unknown."[129] The National Institute on Drug Abuse stated that "There are currently no accepted measures to confirm their purity or safety, and the long-term health consequence of e-cigarette use remain unknown."[130] A 2017 review found "There is a justifiable concern that any broad statement promoting e-cig safety may be unfounded considering the lack of inhalational toxicity data on the vast majority of the constituents in e-cigs. This is particularly true for individuals with existing lung disease such as asthma."[131]
Alternative to smoking

Tobacco companies have deliberately promoted the use of alternatives to traditional cigarettes with supposedly safer tobacco products, such as e-cigarettes, in an effort to reduce the harm caused by tobacco consumption.[note 5][135] There is a lack of evidence in favor of using e-cigarettes as a safe option to classical cigarettes and as a substitute to public health approaches that aim at curtailing tobacco use.[136]
A 2019 editorial in The Lancet stated that there is no solid proof showing that vaping is safer than cigarettes, but this conclusion was "criticized by Professor JN Newton, Director of Health Improvement at Public Health England, who stated that there is an international consensus that the use of e-cigarettes is likely to be much less harmful than smoking."[137] Clinical trials and other studies have demonstrated that e-cigarettes are not a safer option.[138] According to a 2020 review, e-cigarettes are repeatedly popularized and regarded as a safer option to classical cigarettes, but they are unsafe to use and therefore can hardly be construed as being less hazardous as proclaimed by the companies who are selling such devices.[139] Since e-liquids and vaping aerosols contain nicotine and many of the same toxic chemicals and carcinogens as classical cigarettes do, it may be assumed, especially when taking into account the growing evidence of toxic tobacco inhalation that has been observed in the users of these devices, that there is the possibility that vaping may result in similar unwanted effects..[140]


Vaping long-term is anticipated to raise the risk of developing some of the diseases linked to smoking.[87] Since vapor does not contain tobacco and does not involve combustion, users may avoid several harmful constituents usually found in tobacco smoke,[52] such as ash, tar, and carbon monoxide.[note 6][53] A 2014 review found that e-cigarette aerosol contains far fewer carcinogens than tobacco smoke, and concluded that e-cigarettes "impart a lower potential disease burden" than traditional cigarettes.[142] The public health community is divided, even polarized, over how the use of these devices will impact the tobacco epidemic.[143] Some tobacco control advocates predict that e-cigarettes will increase rates of cigarette uptake, especially among youth.[143] Others envision that these devices have potential for aiding cessation efforts, or reducing harm among people who continue to smoke.[143] Scientific studies advocate caution before designating e-cigarettes as beneficial but vapers continue to believe they are beneficial.[144]
E-cigarette vapor contains higher levels of carcinogens and toxicants than in an US Food and Drug Administration (FDA) regulated nicotine inhaler, which suggests that regulated US FDA devices may deliver nicotine more safely.[44] E-cigarettes are generally seen as safer than combusted tobacco products[51][145][50] such as cigarettes and cigars.[51] A 2019 review concluded: "no long term vaping toxicological/safety studies have been done in humans; without these data, saying with certainty that e-cigarettes are safer than combustible cigarettes is impossible."[37] Early research seemed to indicate that vaping might be safer than traditional cigarettes and provide a different method to give up smoking, though mounting evidence does not substantiate this.[45] Evidence has not been presented to demonstrate that e-cigarettes are less dangerous than tobacco.[46] The short-term health effects of e-cigarettes can be severe[47] and the short-term harms of e-cigarettes is greater than tobacco products.[48] E-cigarettes are frequently viewed as a safer alternative to conventional cigarettes; however, evidence to support this perspective has not materialized.[49] This appears to be due to the presence of toxicants in e-liquid composition, their adverse effects in animal models, association with acute lung injury and cardiovascular disease, and ability to modulate different cell populations in the lung and blood towards pro-inflammatory phenotypes.[49] Short-term e-cigarette use may lead to death.[48]
The surge in vaping among youth and the vaping-induced lung illness epidemic has increased the controversy surrounding vaping and casts doubt about their feasibility for public health gains as an alternative to traditional cigarettes.[137] The US National Association of County and City Health Officials has stated, "Public health experts have expressed concern that e-cigarettes may increase nicotine addiction and tobacco use in young people."[146] No long-term studies have evaluated future tobacco use as a result of e-cigarette use.[147] E-cigarette vapor potentially contains harmful substances not found in tobacco smoke[91] such as propylene glycol and/or glycerin and various flavoring agents along with other unknown chemicals.[92]
Opinions that e-cigarettes are a safe substitute to traditional cigarettes may compromise tobacco control efforts.[148] The American Cancer Society has stated, "E-cigarettes pose a threat to the health of users and the harms are becoming increasingly apparent. In the past few years, the use of these products has increased at an alarming rate among young people in significant part because the newest, re-engineered generation of e-cigarettes more effectively delivers large amounts of nicotine to the brain."[149] The Canadian Cancer Society has stated that, "A few studies have shown that there may be low levels of harmful substances in some e-cigarettes, even if they don't have nicotine."[150] In the UK a National Institute for Health and Care Excellence (NICE) guideline did not recommend e-cigarettes as there are questions regarding the safety, efficacy, and quality of these products.[151] While quitting smoking may be firmly recommended for smokers who have asthma, it is not clear whether replacing e-cigarettes for cigarettes is a universally safer alternative.[131] The American Diabetes Association states "There is no evidence that e-cigarettes are a healthier alternative to smoking."[152]
Studies evaluating whether e-cigarettes are less harmful than cigarettes are inconclusive.[122] As of 2020, there is still a lack of evidence that they are safe during repeated inhalation in long-term use.[122] Long-term data showing that vaping is a "healthier alternative" than cigarette smoking does not exist.[44]
Effects on increased availability of vaping products
A serious concern regarding e-cigarettes is that they could entice children to initiate smoking, either by subjecting them to nicotine that leads to smoking or by making smoking appear more acceptable again.[153] Concerns exist in respect to adolescence vaping due to studies indicating that nicotine use could induce potentially harmful effects on the growing brain.[154]
The medical community is concerned that increased availability of e-cigarettes could increase worldwide nicotine dependence, especially among the young as they are enticed by the various flavor options e-cigarettes have to offer.[155] Since vaping does not produce smoke from burning tobacco, the opponents of e-cigarettes fear that traditional smokers will substitute vaping for smoking in settings where smoking is not permitted without any real intention of quitting traditional cigarettes.[155] Furthermore, vaping in public places, coupled with recent e-cigarette commercials on national television, could possibly undermine or weaken current antismoking regulations.[155] Fear exists that wide-scale promotion and use of e-cigarettes, fueled by an increase in advertising of these products, may carry substantial public health risks.[156] Public health professionals have voiced concerns regarding vaping while using other tobacco products - particularly combustible products.[157]
A 2017 review states that the "Increased concentration of the ENDS market in the hands of the transnational tobacco companies is concerning to the public health community, given the industry's legacy of obfuscating many fundamental truths about their products and misleading the public with false claims, including that low-tar and so-called "light" cigarettes would reduce the harms associated with smoking. Although industry representatives are claiming interest in ENDS because of their harm-reduction potential, many observers believe that profit remains the dominant motivation."[157] E-cigarettes are expanding the tobacco epidemic by bringing lower-risk youth into the market, many of whom then transition to smoking cigarettes.[158] A 2016 review recommended the precautionary principle to be used for e-cigarettes because of the long history of the tobacco crisis, in order to assess their benefits and long-term effects and to avoid another nicotine crisis.[159]
Effects on dual vaping and smoking use
![The figure shows the known and unknown health effects of vaping in comparison to cigarette smoke. The major toxic effects of compounds found in cigarette smoke (right lung) and in vaping aerosols (left lung) are lung inflammation, oxidative stress, cell death, impaired immune response, DNA damage, and epigenetic modifications. The respiratory diseases caused by cigarette smoke (lung cancer, COPD [emphysema and/orobstruction of airways]) are not yet established to be caused by vaping (represented by question marks in the left lung). There is an association with the presence of lipid-laden macrophages and the use of vaping products. E-cigarettes containing THC and vitamin E acetate or nicotine can cause a vaping-induced lung injury disease.](https://upload.wikimedia.org/wikipedia/commons/thumb/6/6f/Health_effects_of_vaping_in_comparison_to_cigarette_smoke.png/362px-Health_effects_of_vaping_in_comparison_to_cigarette_smoke.png)
The entrance of large US tobacco manufacturers, such as Altria Group, Reynolds American, and Lorillard, into the e-cigarette sector raises many potential public health issues.[162] Instead of pushing for quitting smoking, the tobacco industry may promote e-cigarettes as a way to get around clean indoor air laws, which promotes dual use and the increased sale of traditional cigarettes.[162] A 2015 review recommended the precautionary principle to be used because dual use could end up being an additional risk.[99] The industry could also lead vapers to tobacco products, which would increase instead of decrease overall addiction.[162] Concerns exist that the emergence of e-cigarettes may benefit Big Tobacco to sustain an industry for tobacco.[163]
Many continue to use both, exposing themselves to the harms of tobacco smoking and e-cigarette use.[164] The long-term research on the effects of dual use of tobacco smoking and vaping are not available.[165] A 2018 study found that both e-cigarette and cigarette users had similar levels of metals toluene, benzene, and carbon disulfide, while dual users had the greatest amount of exposure to nicotine, tobacco biomarkers, metals toluene, benzene, and carbon disulfide.[140] Vaping can hinder smokers from trying to quit, resulting in increased tobacco use and associated health problems.[166] Compared to just smoking, dual use of smoking and vaping may increase the chance of developing heart disease, lung disease, and cancer.[167] There is a greater risk for a heart attack with the use of both e-cigarettes and traditional cigarettes.[168] Quitting smoking entirely would probably have much greater beneficial effects to overall health than vaping to decrease the number of cigarettes smoked.[43]
Ten large, good-quality surveys, including between 3,400 and almost 450,00 persons from the general population, investigated the cardiovascular and metabolic health effects of dual use.[114] The best available of these studies had adjusted for tobacco consumption and found higher HbA1c levels in dual users than in exclusive smoking of conventional cigarettes, but significance levels were not tested.[114] Four of the good-quality surveys investigated cardiovascular risk factors and found that dual users had a significantly higher unadjusted and adjusted odds ratios of cardiovascular disease, significantly higher prevalence unadjusted and adjusted odds ratios of cardiovascular risk factors and diagnosis of metabolic syndrome, significantly higher unadjusted and adjusted odds ratios of elevated human c-reactive protein, significantly higher risk of stroke, significantly higher prevalence of arrythmia, significantly higher unadjusted and adjusted odds ratios of elevated c-reactive protein, and significantly higher unadjusted and adjusted odds ratios of abdominal obesity than exclusive smoking of conventional cigarettes.[114] The two remaining surveys found higher unadjusted and adjusted odds ratios of myocardial infarction and stroke, but significance level was not tested, and higher but not significant unadjusted and adjusted odds ratios of hypertension in dual users than in exclusive smoking of conventional cigarettes.[114] Furthermore, one survey found that dual users had similar fasting glucose as exclusive smoking of conventional cigarettes, and another study found the same levels of insulin resistance.[114]
A 2020 clinical study performed vascular function testing in almost 500 young persons and reported that dual users had similar arterial stiffness as exclusive smoking of conventional cigarettes.[114] Large good-quality surveys (only one did not weight data) including adults found that dual users had significantly worse fitness and significantly higher levels of uric acid and prevalence of hyperuricemia compared with exclusive smoking of conventional cigarettes.[114] Large surveys including adolescent dual users reported insufficient sleep significantly more often than exclusive smoking of conventional cigarettes, and higher odds of dental problems.[114] In a large survey, homeless persons with dual use reported significantly higher rates of asthma and cancer compared to exclusive smoking of conventional cigarettes.[114] Finally, in a small human clinical study in 2020, dual users had higher levels of most biomarkers of systemic inflammation than exclusive smoking of conventional cigarettes, but the difference was not significant.[114]
Evidence on the effects of dual e-cigarette and traditional cigarette use compared to using one product alone is limited.[42] Dual users reported a lower general health score, and more difficulty in breathing in the past month, compared to cigarette-only users.[169] Additionally, a significant difference was observed in the history of arrhythmia between cigarette-only users (14.2%) and dual users (17.8%).[169] More respiratory symptoms were found in dual smokers than in smokers who did not use e-cigarettes, and the possibility of reversible cerebral vasoconstriction syndrome was more likely to be observed in dual users.[169] A positive association between dual use and the prevalence of asthma was reported in one systematic review in 2021, while a 2021 meta-analysis found that the association with asthma prevalence was even stronger for dual use than for traditional cigarette use alone.[42] Temporality and a dose–response relationship were not determined due to the cross-sectional nature of the associations and lack of information on the intensity and duration of use.[42] A 2020 systematic review concluded that e-cigarette use, as compared to traditional cigarette use, contributes independently to respiratory risk.[42]
Effects on smoking cessation

The safety of e-cigarette consumption and its potential as a smoking cessation method remain controversial due to limited evidence.[117] Moreover, it has been reported that the heating process itself can lead to the formation of new decomposition compounds of questionable toxicity.[117] There is concern that e-cigarettes may result in many smokers rejecting historically effective smoking quitting smoking methods.[142] Concern exists that the majority of smokers attempting to quit with the help of vaping may stop smoking but will keep on using nicotine, because their long-term effects are not clear.[171] Since e-cigarettes are intended to be used repeatedly, they can conveniently be used for an extended period of time, which may contribute to increased adverse effects.[172]
The most frequently reported less harmful effects of vaping compared to smoking were reduced shortness of breath, reduced cough, reduced spitting, and reduced sore throat.[144] More serious adverse effects frequently related with smoking cessation including depression, insomnia, and anxiety are uncommon with e-cigarette use.[62] Many health benefits are associated with switching from tobacco products to e-cigarettes including decreased weight gain after smoking cessation and improved exercise tolerance.[173] Reported in 2013, quitting smoking with the use of a vape alleviated chronic idiopathic neutrophilia in a smoker.[174] Vaping is possibly harmful by virtue of putting off quitting smoking, serving as a gateway to tobacco use in never-smokers or causing a return to smoking in former smokers.[175] Many individuals use e-cigarettes as a way to quit smoking, but there is not clear evidence that e-cigarettes help people quit smoking entirely.[164] E-cigarettes may help smokers reduce the number of cigarettes they smoke, though decreasing daily cigarette use is still not safe.[164]
They are similar in toxicity to other nicotine replacement products,[176] but e-cigarettes manufacturing standards are variable standards, and many as a result are probably more toxic than nicotine replacement products.[177] E-cigarettes produce more toxicants than other forms of nicotine replacement products and are likely to be more harmful.[178] The most frequently cited adverse effects related to nicotine vaping in studies were throat and mouth irritation, cough, nausea, and headache.[179]
Effects on vaping cessation
The short-term effects of vaping causing greater airway resistance and inflammation may not be permanent following quitting vaping.[60] A 2022 review states that a better choice for quitting smoking or quitting nicotine might be to immediately stop using e-cigarettes and smoking combustible cigarettes, which might be a better way to reduce organ injuries.[180] Cardiotoxicity can be irreversible, when necrosis or apoptosis of the myocardial cells occurs, or reversible, as in the case of short-term nicotine product consumption.[24]
Primary-care interventions
Research indicates that screening patients for e-cigarette usage in primary practice is not frequently undertaken by medical practitioners.[181] A 2015 study found a low prevalence of screening for e-cigarettes in primary-care practice relative to smoking screening (14% versus 86%) in a sample of 776 practitioners across the United States.[181] This low uptake is concerning, given the serious health risks of e-cigarettes.[181] A 2016 qualitative study in the US further confirmed that there is insufficient knowledge of e-cigarettes among physicians, including both the potential benefits and health risks.[181] A 2017 study in US college students found that most students did not receive any form of counseling about risks from medical practitioners, including dental hygienists.[181] Studies have also shown that there is a need for stronger education on e-cigarettes in medical curricula, which will allow physicians to begin addressing e-cigarette use in teenagers.[181]
As of 2022, there is little information on primary-care interventions for e-cigarette use in teenagers and young adults.[181] A 2020 case study of a 23-year-old e-cigarette user shows promising results for tapering e-cigarette use with the assistance of a pharmacist, which suggests that different healthcare practitioners may play a role helping patients with gradually tapering off e-cigarettes.[181] A 2021 randomized controlled trial of asthmatic teenagers who attended one of four clinics found that physicians discussed smoking during 38.2% of thee visits, but vaping was never brought up as a topic.[181] According to a 2022 review, this emphasizes that physicians should discuss both smoking and vaping during appointments, in particular in youth presenting with asthma.[181]
Overall risk relative to smoking
—Yogi H Hendlin and colleagues, American Journal of Public Health[135]
A 2018 Public Health England (PHE) report stated, "The previous estimate that, based on current knowledge, vaping is at least 95% less harmful than smoking remains a good way to communicate the large difference in relative risk unambiguously so that more smokers are encouraged to make the switch from smoking to vaping," but noted that this in no way means that vaping is safe.[182] They also noted it is associated with some risks as well as uncertainties.[48] A 2015 PHE report stated that e-cigarettes are estimated to be 95% less harmful than smoking,[183] but the studies used to support this estimate were viewed as having a weak methodology.[184] The estimate has been extensively disputed in medical journals.[185] Many vigorously criticized the validity of the estimate that vaping is 95% less harmful than smoking.[157] The PHE's encouragement of using vaping products has been characterized as "a reckless and irresponsible decision".[48]
Influential health organizations in England, including PHE, the Royal College of Physicians, the Royal Society for Public Health, and the National Health Service, have unequivocally stated that e-cigarettes are 95% safer than traditional cigarettes.[158] This claim originated from a single consensus meeting of 12 people convened by D.J. Nutt in 2014.[158] They reached this conclusion without citing any specific evidence.[158] The Nutt et al. paper did include this caveat: "A limitation of this study is the lack of hard evidence for the harms of most products on most of the criteria", which has generally been ignored by those quoting this report.[158] A 2015 editorial in The Lancet identified financial conflicts of interest associated with Nutt et al., noting that "there was no formal criterion for the recruitment of the experts."[158]

(b) Figure also shows health risks associated to chemical compounds from conventional cigarettes.[186]
The Nutt et al. meeting was funded by Euroswiss Health and Lega Italiana Anti Fumo (LIAF).[158] EuroSwiss Health is one of several companies registered at the same address in a village outside Geneva with the same chief executive, who was reported to have received funding from British American Tobacco for writing a book on nicotine as a means of harm reduction and who also endorsed BAT's public health credentials.[158] Another of Nutt's coauthors, Riccardo Polosa, was Chief Scientific Advisor to LIAF, received funding from LIAF, and reported serving as a consultant to Arbi Group Srl, an e-cigarette distributor.[158] He also received funding from Philip Morris International.[158] Polosa, founder of the Center of Excellence for the Acceleration of Harm Reduction, has repeatedly and varioulsy neglected to declare the money he was given for research came from Philip Morris International, his advisory costs from British American Tobacco, the Center of Excellence for the Acceleration of Harm Reduction’s ties to the Foundation for a Smoke-Free World, and the Foundation for a Smoke-Free World’s ties to Philip Morris International.[187] In regard to the Foundation for a Smoke-Free World, John Britton stated that it is "the latest in a long history of third-party organisations set up by the tobacco industry to promote its interests, and in this case act as a conduit for funds to researchers and organisations sympathetic to promoting the use of tobacco, promoting their careers, or both."[188]
Later in 2015, The BMJ published an investigative report that raised broader issues surrounding potential conflicts of interest between individuals involved in the Nutt et al. paper.[158] The BMJ provided an infographic illuminating undisclosed connections between key people involved in the paper and the tobacco and e-cigarette industries as well as links between the paper and Public Health England via one of the coauthors.[158] Even so, as of June 2017, the "95% safer" figure remains widely quoted, despite the fact that evidence of the dangers of e-cigarette use has rapidly accumulated since 2014.[158] As of 2018, the evidence indicates that the risk of e-cigarette use is substantially higher than the "95% safer" figure would indicate.[158] It was also criticized by the journal The Lancet for constructing its conclusions on 'flimsy' evidence, which included citing literature with apparent conflicts of interest.[189] It was later discovered that many of the authors who came up with the "95% safer" assertion have ties to the tobacco industry.[184] Some researchers consider that the 95% figure is flawed and confusing, by making opinions at odds with existing knowledge.[190] Despite this, most other health organizations have been more cautious in their public statements on the safety of e-cigarettes.[191]
Mortality
E-cigarette use induces an acute rise in cardiac sympathetic nerve activity.[192] This can trigger electrocardiogram abnormalities, and as a result, lead to a higher chance of sudden death in people with co-morbidities.[192] The risk of early death is anticipated to be similar to that of smokeless tobacco.[58] There is a significant risk of long-lasting lung injury from vaping that may contribute to or lead to death, in old people.[193]
Multigenerational effects
The multigenerational epigenetic effect of nicotine on lung function has been demonstrated.[195] Vaping or the use of any nicotine-based product during pregnancy or during pregnancy and during the breastfeeding, postpartum period causes the "concurrent exposure of three generations to nicotine".[196]
In 2020, mice that were exposed to nicotine during early development and their offspring showed changes in the levels of epigenetic factors that regulate gene expression in certain brain regions.[194] The observed changes were consistent with altered patterns of epigenetic modifications seen in mice and humans with neurological and behavioral disorders.[194] Epigenetic changes can persist for generations after nicotine exposure.[194] It remains unclear how nicotine exposure elicits changes in epigenetic factor levels and how these changes are passed on across generations.[194]
Maternal smoking of traditional cigarettes and maternal vaping of e-cigarettes during pregnancy exposes the fetus to nicotine; developmental nicotine exposure (DNE) can harm the baby's brain development and has been linked to disorders such as attention deficit/hyperactivity disorder, autism, and schizophrenia in children.[194] Of particular concern, animal model studies of maternal and grandmaternal cigarette smoking or vaping nicotine show that DNE is associated with behavioral and neurological changes that can persist across multiple generations.[194] A 2020 National Institute on Drug Abuse-funded study by Jordan M. Buck and colleagues at the University of Colorado has identified a mechanism that may be responsible for this intergenerational transmission.[194] The researchers focused on epigenetic changes—chemical modifications of the DNA and associated proteins that influence gene expression.[194] "Our findings imply that epigenetic perturbations may constitute a nexus for intergenerational transmission of DNE-induced neurodevelopmental deficits," says Buck.[194]
Regulation
Guidelines for the design, manufacture, and assessment of the safety of e-cigarette devices has not been established.[197] Following years of regulatory discussions, suggested policies and directives, e-cigarettes mainly targeting the youth continue to be underregulated, as of 2020.[198] A 2020 meta-analysis states that e-cigarettes should not be available as consumer products, though they may be considered for sale as a prescription drug.[167] A 2015 review suggested that e-cigarettes could be regulated in a similar way as inhalation therapeutic medicine, meaning, they would be regulated based on toxicology and safety clinical trials.[77] A 2014 review recommended that e-cigarettes could be adequately regulated for consumer safety with existing regulations on the design of electronic products.[199] A 2015 review recommended that regulations provide detailed quality standards for products, policies to not allow chemicals of justifiable concern, and allocate testing for plausible contaminants.[99] According to a 2020 review, regulation is needed to inform e-cigarette users of possible metal/metalloid exposure through vaping as well as to prevent metal/metalloid exposure during e-cigarette use..[200]
Regulation of the production and promotion of e-cigarettes may help lower some of the adverse effects associated with tobacco use.[201] Scientists are doing research to obtain more data regarding e-cigarettes and their usage.[202] This knowledge could result in additional regulations in the US.[202] E-cigarettes are permitted for sales in the US, though some organizations in the US have recommended they be completed banned.[112] The American Heart Association had urged a total ban on e-cigarette sales, stating that there is sufficient evidence linking e-cigarettes with adolescent's addiction to nicotine and with lure of never-smokers to smoking.[112]
In order to protect the public from both second-hand smoke and second-hand e-cigarette aerosol, the Surgeon General of the United States emphasized that smoke-free policies should be modernized to incorporate e-cigarettes, an approach that "will maintain current standards for clean indoor air, reduce the potential for renormalization of tobacco product use, and prevent involuntary exposure to nicotine and other aerosolized emissions from e-cigarettes".[203] A 2019 review states, "It is urgent to regulate e-cigarette design, e-liquid and aerosol composition, health warnings, marketing, promotion, sales, taxation, and secondhand vapor exposure at least at a level equivalent to that of regular tobacco products."[204]
Public health consequences
The public health consequence of vaping is actively being debated.[205] The health community, pharmaceutical industry, and other groups have raised concerns about the emerging phenomenon of e-cigarettes, including the unknown health risks from their long-term use.[199] The rise in e-cigarette use among the general population raises concern.[164] E-cigarettes pose potential risks to the population as a whole.[206] Concerns have been raised that higher rates of never smokers initiating e-cigarettes would result in net public health harms via increased nicotine addiction.[207] One of the serious concerns in public health is the increase in trying an e-cigarette among people who have not smoked, particularly children and adolescents, which can result in nicotine addiction and possible progression to smoking.[204] The prevalence of newer types of e-cigarettes, including Juul, with greater levels of nicotine is a public health catastrophe.[140] In December 2018, the US Surgeon General said vaping among youth is an epidemic.[140] Misinformation may downplay the risks of vape use and may be in part responsible for the recent youth vaping epidemic.[208] The rise in the rate of vaping among youth in Australia and New Zealand are a major public health concern.[61] Their indiscriminate use is a threat to public health.[57]
E-cigarettes could cause public health harm if they: increase the number of youth and young adults who are exposed to nicotine, or lead non-smokers to start smoking conventional cigarettes and other burned tobacco products such as cigars and hookah, or sustain nicotine addiction so smokers continue using the most dangerous tobacco products – those that are burned – as well as e-cigarettes, instead of quitting completely, or increase the likelihood that former smokers will again become addicted to nicotine by using e-cigarettes, and will start using burned tobacco products again.[206] A 2014 review has stated, there are "Many unanswered questions about their safety, efficacy for harm reduction and cessation, and total impact on public health."[43]
A policy statement by the American Association for Cancer Research and the American Society of Clinical Oncology has reported that "The benefits and harms must be evaluated with respect to the population as a whole, taking into account the effect on youth, adults, nonsmokers, and smokers."[73] The range of e-liquid flavors available to consumers is extensive and is used to attract both current smokers and new e-cigarette users, which is a growing public health concern.[117] The widespread availability and popularity of flavored e-cigarettes is a key concern regarding the potential public health implications of the products.[209] A critical public health concern is the increased use among pregnant women.[210] E-cigarettes are not safe for youth, young adults, pregnant women, or adults who do not currently use tobacco products.[211] Because of the risk of nicotine exposure to the fetus and adolescent causing long-term effects to the growing brain, the World Health Organization does not recommend it for children, adolescents, pregnant women, and women of childbearing age.[55] E-cigarettes are an increasing public health concern due to the rapid rise among adolescents and the uncertainty of potential health consequences.[212]
Another area of concern is the public health consequences of second-hand e-cigarette vapor on bystanders.[213] Second-hand e-cigarette vapor is a significant public health issue because of the tremendous growth in the number of e-cigarette users.[94] The use of e-cigarettes in public areas poses a serious health risk considering the various toxic constituents that have been shown to affect both the primary user and bystanders of passive vaping.[213] It is pertinent to note that smoke-free laws in the US were passed before e-cigarettes entered the market and do not specifically mention the prohibition of e-cigarette vaping in many places.[213] As such, this non-clarity may lead to non-compliance or exploitation of smoke-free rules.[213] Greater e-cigarette vapor exposure to bystanders may undermine public policies to restrict second-hand smoke and may renormalize smoking habits.[214]
Adverse effects

The short-term and long-term effects from e-cigarette use remain unclear.[61] Makers of vaping products state that these products are non-toxic, but they are correlated with a myriad of adverse effects.[125] They may cause long-term and short-term adverse effects, including airway resistance, irritation of the airways, eyes redness, and dry throat.[216] Since vaping is relatively in its infancy, it will probably take decades for long-term harm research to be available.[217] The growing evidence reinforces the idea that persistent and long-term exposure to e-cigarette aerosols possibly affects health adversely.[218] The long-term health consequences from vaping is probably somewhat greater than nicotine replacement products,[116] though repeated exposure over a long time to e-cigarette vapor poses substantial potential risk.[219] A 2016 review found "it is impossible to reach a consensus on the safety of e-cigarettes except perhaps to say that they may be safer than conventional cigarettes but are also likely to pose risks to health that are not present when neither product is used."[220] The wide range of e-cigarette products available to users and the lack of standardization of toxicological approaches towards e-cigarette evaluation complicates the assessment of adverse effects of their use.[221] Adverse effects are mostly associated with short-term use and the reported adverse effects decreased over time.[222] Long-term studies regarding the effects of constant use of e-cigarettes are unavailable.[222] Studies over one year on the effects of exposure to e-cigarettes have not been conducted, as of 2019.[223] The adverse effects of e-cigarettes on people with cancer is unknown.[73] Several serious adverse events were decribed in case studies and by news agencies.[72]
A 2015 study found serious adverse events related to e-cigarettes were hypotension, seizure, chest pain, rapid heartbeat, disorientation, and congestive heart failure but it was unclear the degree to which they were the result of e-cigarettes.[62] Less serious adverse effects include abdominal pain, dizziness, headache, blurry vision,[62] throat and mouth irritation, vomiting, nausea, and coughing.[43] Vaping induces irritation of the pharynx.[166] Short-term adverse effects reported most often were mouth and throat irritation, dry cough, and nausea.[222] The majority of adverse effects reported were nausea, vomiting, dizziness and oral irritation.[52] Some case reports found harms to health brought about by e-cigarettes in many countries, such as the US and in Europe; the most common effect were dryness of the mouth and throat.[80] Dryness of the mouth and throat is believed to stem from the ability of both propylene glycol and glycerin to absorb water.[224] Some e-cigarettes users experience adverse effects like throat irritation which could be the result of exposure to nicotine, nicotine solvents, or toxicants in the aerosol.[73] Vaping may harm neurons and trigger tremors and spasms.[225] The use of e-cigarettes has been found to be associated with nose bleeding, change in bronchial gene expression, release of cytokines and proinflammatory mediators, and increase in allergic airway inflammation which can exacerbate asthmatic symptoms, thus elevating infiltration of inflammatory cells including eosinophils into airways.[156]
Reports to the US FDA in 2013 for minor adverse effects identified with using e-cigarettes included headache, chest pain, nausea, and cough.[76] Major adverse events reported to the US FDA in 2013 included hospitalizations for pneumonia, congestive heart failure, seizure, rapid heart rate, and burns.[76] However, no direct relationship has been proven between these effects and events and e-cigarette use, and some may be due to existing health problems.[76] Many of the observed negative effects from e-cigarette use concerning the nervous system and the sensory system are probably related to nicotine overdose or withdrawal.[226] No information is available on the effects of long-term e-cigarette use on taste receptors.[77]
Youth and young adults

There is no benefit for vaping among youth[229] and, according to a 2016 review, their use in this population should be discouraged.[207] There is broad consensus on the need to protect young people from this disruptive technology.[230] Vaping is especially harmful to children and youth.[231] Multiple researchers have concluded that e-cigarettes are unsafe for youth and that allowing them to be marketed as consumer products is likely to lead to increasing youth nicotine addiction and long-term consequences seen in current research evidence.[120] Children's health has long been a concern in tobacco control.[120]
Beyond their unknown long-term effects on human health, the extended list of appealing flavors available seems to attract new "never-smokers", which is especially worrying among young users.[117] Given the unknown health effects of long-term nicotine use and inhaled propylene glycol, the safety profile of even the most reliable e-cigarette is yet unknown, and the consumption of nicotine among youth remains undesirable, there is widespread consensus concerning attempts to restrict e-cigarette sales to youth in the US.[207] A 2017 review found "Because the brain does not reach full maturity until the mid-20s, restricting sales of electronic cigarettes and all tobacco products to individuals aged at least 21 years and older could have positive health benefits for adolescents and young adults."[232] Their harmful effects on children is not well understood.[233] E-cigarettes are a source of potential developmental toxicants.[234] Children subjected to e-cigarettes had a higher likelihood of having more than one adverse effect and those were more significant than with children subjected to traditional cigarettes.[233] Significant harmful effects to children were cyanosis, nausea, and coma, among others.[233] Little is known regarding their mental health consequences on children.[235]
Frequent vaping among middle and high school students has been said to be linked to oral symptoms, such as cracked/broken teeth and tongue/cheek pain.[236] Information on the long-term health effects of vaping for adolescent and young adults are scant because of the limited amount of time they have been available.[236] There is fair evidence that coughing and wheezing is higher in adolescents who vape.[237]
According to various studies involving high school students, vapers have a twofold higher risk of chronic cough, phlegm or dyspnea, together with a greater incidence of asthma.[104] A higher prevalence of e-cigarette use is reported among adults living with a child affected by asthma, whose risk of acute exacerbation can increase by 30%.[104] Schoolwork is indirectly affected too, as a result of absenteeism secondary to the aforementioned symptoms.[104]
Reported deaths
The US Food and Drug Administration Center for Tobacco Products reported between 2008 and the beginning of 2012, 47 cases of adverse effects associated with e-cigarettes, of which eight were considered serious.[72] Two peer-reviewed reports of lipoid pneumonia were related to e-cigarette use, as well as two reports in the media in Spain and the UK.[121] In the UK, the man reportedly died from severe lipoid pneumonia[121] in 2010.[238] In August 2019, the Illinois Department of Public Health (IDPH) reported the first death in the US linked to vaping.[239] The deceased had been recently using an e-cigarette and was hospitalized with serious respiratory problems.[239] Several people have died as a result of e-cigarette blasts with parts of the device hitting the head and neck area.[47] In March 2020, Europe announced its first confirmed death of a vaping-induced lung injury.[71] Since the start of the COVID-19 pandemic in March 2020, one confirmed death in California has been reported to the California Department of Public Health.[240]
Poisoning

Nicotine poisoning associated with e-cigarettes may arise from inhalation, absorption, or ingestion via the skin or eyes.[73] Accidental poisoning can result from using undiluted concentrated nicotine when mistakenly used as prepared e-liquids.[242] E-cigarettes involve accidental nicotine exposure in children.[74] Accidental exposures in pediatric patients include ingesting of e-liquids and inhaling of e-cigarette vapors.[74] Choking on e-cigarette components is a potential risk.[74] In 2014, an infant died from choking on an e-cigarette component.[243] It is recommended that youth access to e-cigarettes be prohibited.[note 7][244] Concerns exist regarding poisoning, considering they may appeal to children.[243] E-liquid presents a poisoning risk, particularly for small children, who may see the colorful bottles as toys or candy.[203]
The e-liquid can be toxic if swallowed, especially among small children.[72] Four adults died in the US and Europe, after intentionally ingesting liquid.[121] Two children, one in the US in 2014 and another in Israel in 2013, died after ingesting liquid nicotine.[245] A two year old girl in the UK in 2014 was hospitalized after licking an e-cigarette liquid refill.[246] Death from accidental nicotine poisoning is very uncommon.[247]
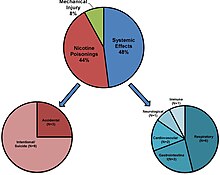
Calls to US poison control centers related to e-cigarette exposures involved inhalations, eye exposures, skin exposures, and ingestion, in both adults and young children.[248] Minor, moderate, and serious adverse effects involved adults and young children.[249] Minor effects correlated with e-cigarette liquid poisoning were tachycardia, tremor, chest pain and hypertension.[250] More serious effects were bradycardia, hypotension, nausea, respiratory paralysis, atrial fibrillation and dyspnea.[250] The exact correlation is not fully known between these effects and e-cigarettes.[250] The initial symptoms of nicotine poisoning may include rapid heart rate, sweating, feeling sick, and throwing up, and delayed symptoms include low blood pressure, seizures, and hypoventilation.[251] Rare serious effects included coma, seizure, cessation of breathing, and heart attack.[252] Since June 2018, the US FDA observed a slight but noticeable increase in reports of seizures.[253] After examining poison control centers' reports between 2010 and early 2019, the US FDA determined that, between the poison control centers and the US FDA, there were a total of 35 reported cases of seizures mentioning use of e-cigarettes within that timeframe.[253] Due to the voluntary nature of these case reports, there may be more instances of seizure in e-cigarette users than have been reported.[253]
Since 2011, accidental poisoning from e-liquids that contain nicotine have grown rapidly in the US.[254] From September 1, 2010, to December 31, 2014, 58% of e-cigarette calls to US poison control centers were related to children 5 years old or less.[249] Exposures for children below the age of 6 is a concern because a small dose of nicotine e-liquid may be fatal.[252] A 2014 Centers for Disease Control and Prevention report found 51.1% of the calls to US poison centers due to e-cigarettes were related to children under age 5, and about 42% of the US poison center calls were related to people age 20 and older.[255] E-cigarette calls had a greater chance to report an adverse effect and a greater chance to report a moderate or major adverse effect than traditional cigarette calls.[249] Most of the e-cigarette and traditional cigarette calls were a minor effect.[249] Severe outcomes were more than 2.5 times more frequent in children exposed to e-cigarettes and nicotine e-liquid than with traditional cigarettes.[256] E-cigarette sales were roughly equivalent to just 3.5% of traditional cigarette sales, but e-cigarettes represented 44% of the total number of e-cigarette and traditional cigarette calls to US poison control centers in December 2014.[249]

The US poison control centers reported 92.5% of children coming in contact with liquid nicotine was from swallowing during the period from January 2012 to April 2017.[252] From September 1, 2010, to December 31, 2014, the most frequent adverse effects to e-cigarettes and e-liquid reported to US poison control centers were: Ingestion exposure resulted in vomiting, nausea, drowsy, tachycardia, or agitation;[249] inhalation/nasal exposure resulted in nausea, vomiting, dizziness, agitated, or headache;[249] ocular exposure resulted in eye irritation or pain, red eye or conjunctivitis, blurred vision, headache, or corneal abrasion;[249] multiple routes of exposure resulted in eye irritation or pain, vomiting, red eye or conjunctivitis, nausea, or cough;[249] and dermal exposure that resulted in nausea, dizziness, vomiting, headache, or tachycardia.[249] The ten most frequent adverse effects to e-cigarettes and e-liquid reported to US poison control centers were vomiting (40.4%), eye irritation or pain (20.3%), nausea (16.8%), red eye or conjunctivitis (10.5%), dizziness (7.5%), tachycardia (7.1%), drowsiness (7.1%), agitation (6.3%), headache (4.8%), and cough (4.5%).[249] In nine reported calls, exposed individuals stated the device leaked.[249] In five reported calls, individuals used e-liquid for their eyes rather than use eye drops.[249] In one reported call, an infant was given the e-liquid by an adult who thought it was the infant's medication.[249] There were also reports of choking on e-cigarette components.[74]
From January 1, 2016, and April 30, 2016, the American Association of Poison Control Centers (AAPCC) reported 623 exposures related to e-cigarettes.[164] In 2016 AAPCC reported there were a total of 2,907 exposures regarding e-cigarettes and liquid nicotine.[257] The yearly nicotine exposure rate in the US involving children went up by 1398.2% from 2012 to 2015, and later dropped by 19.8% from 2015 to 2016.[252] The AAPCC reported 3,067 exposures relating to e-cigarettes and liquid nicotine in 2015, and 3,783 in 2014.[258] As of October 31, 2018, there were a total of 2,555 exposures regarding e-cigarettes and liquid nicotine in 2018.[257] The US National Poison Control database showed that in 2015 more than 1000 needed medical attention from being exposed to nicotine e-liquid.[259] Most exposures in 2015 were related to children under the age of 5.[259] The reported e-cigarette poisonings to medical centres in the UK most often happen in children under the age of five.[260] Toxic effects for children under the age of five in the UK are typically short in length and not severe.[260] From September 1, 2010, to December 31, 2014, there were at least 5,970 e-cigarette calls to US poison control centers.[249] Calls to US poison control centers related to e-cigarettes increased between September 2010 to February 2014, and of the total number of cigarettes and e-cigarettes calls, e-cigarette calls increased from 0.3% to 41.7%.[261] Calls to US poison controls centers related to e-cigarette liquid poisoning increased from 1 in September 2010 to 215 for the month of February 2014.[250] E-cigarette calls was 401 for the month of April 2014.[249] The National Poison Data System stated that exposures to e-cigarettes and liquid nicotine among young children is rising significantly.[262] The California Poison Control System reported 35 cases of e-cigarette contact from 2010 to 2012, 14 were in children and 25 were from accidental contact.[52] Calls associated with e-cigarette poisoning in Texas found that 57% was associated with children under the age of 5.[216] They were accidental, and in 96% of instances happened where they lived.[216] Of these, 85% were from swallowing, and 11% from skin contact.[216]
In 2017, the US FDA states that the e-cigarette aerosol can cause problems for the user and their pets.[263] Some studies have shown that the aerosol made by these devices may expose the user and, therefore, their pets to higher-than-normal amounts of nicotine and other toxic chemicals, like formaldehyde.[263] E-cigarettes use capsules that can contain nicotine.[263] Some of these capsules can be re-filled using a special liquid.[263] Sometimes, pets—mainly dogs—find the capsules and bite them or get into the liquid refilling solution.[263] In a March 15, 2016, letter to the editor of the Journal of the American Veterinary Medical Association, the Texas Poison Center Network reported 11 cases of dogs being exposed to e-cigarettes or refills.[263] Moreover, there is no antidote for nicotine poisoning.[263] If someone's pet gets into an e-cigarette, nicotine capsule, or the liquid refilling solution, it is an emergency, according to the US FDA.[263] Get him or her to the veterinarian or to a veterinary emergency clinic as quickly as possible, according to the US FDA.[263] The Animal Poison Control Center states that all the nicotine toxicity cases in 2012 included 4.6% of e-cigarettes causes and it increased to 13.6% in 2013.[264]
In 2021, poison control centers documented more than 4,500 exposures associated with e-cigarette devices or nicotine-containing e-liquids.[2]
Direct exposure to e-cigarette liquid

There is a possibility that inhalation, ingestion, or skin contact can expose people to high levels of nicotine.[201] Concerns with exposure to the e-liquids include leaks or spills and contact with contaminants in the e-liquid.[265] This may be especially risky to children, pregnant women, and nursing mothers.[201] The US FDA intends to develop product standards around concerns about children's exposure to liquid nicotine.[266] E-liquid exposure whether intentional or unintentional from ingestion, eye contact, or skin contact can cause adverse effects such as seizures, anoxic brain trauma, throwing up, and lactic acidosis.[267] The liquid does quickly absorb into the skin.[268] Local irritation can be induced by skin or mucosal nicotine exposure.[269] The nicotine in e-liquid can be hazardous to infants.[270] Even a portion of e-liquid may be lethal to a little child.[271] An excessive amount of nicotine for a child that is capable of being fatal is 0.1–0.2 mg/kg of body weight.[201] Less than a 1 tablespoon of contact or ingestion of e-liquid can cause nausea, vomiting, cardiac arrest, seizures, or coma.[272] An accidental ingestion of only 6 mg may be lethal to children.[171][57]
Children are susceptible to ingestion due to their curiosity and desire for oral exploration.[256] Children could confuse the fruity or sweet flavored e-liquid bottles for fruit juices.[216] E-liquids are packed in colorful containers[249] and children may be attracted to the flavored liquids.[147] More youth-oriented flavors include "My Birthday Cake" or "Tutti Frutti Gumballs".[245] Many nicotine cartridges and bottles of liquid are not child-resistant to stop contact or accidental ingestion of nicotine by children.[273] "Open" e-cigarette devices, with a refillable tank for e-liquids, are believed to be the biggest risk to young children.[272] If flavored e-cigarettes are left alone, pets and children could be attracted to them.[274] The US FDA states that children are curious and put all sorts of things in their mouths.[275] Even if you turn away for a few seconds, they can quickly get into things that could harm them.[275] The US FDA recommends that adults can help prevent accidental exposure to e-liquids by always putting their e-cigarettes and e-liquids up and away—and out of kids' and pets' reach and sight—every time you use them.[275] The US FDA recommends to also ask family members, house guests, and other visitors who vape to keep bags or coats that hold e-cigarettes or e-liquids up and away and out of reach and sight of children and pets.[275] They recommend for children old enough to understand, explain to them that these products can be dangerous and should not be touched.[275] The US FDA states to tell kids that adults are the only people who should handle these products.[275]
As part of ongoing efforts to protect youth from the dangers of nicotine and tobacco products, the US FDA and the Federal Trade Commission announced on May 1, 2018, they issued 13 warning letters to manufacturers, distributors, and retailers for selling e-liquids used in e-cigarettes with labeling and/or advertising that cause them to resemble kid-friendly food products, such as juice boxes, candy or cookies, some of them with cartoon-like imagery.[276] Several of the companies receiving warning letters were also cited for illegally selling the products to minors.[276] "No child should be using any tobacco product, and no tobacco products should be marketed in a way that endangers kids – especially by using imagery that misleads them into thinking the products are things they would eat or drink. Looking at these side-to-side comparisons is alarming. It is easy to see how a child could confuse these e-liquid products for something they believe they have consumed before – like a juice box. These are preventable accidents that have the potential to result in serious harm or even death. Companies selling these products have a responsibility to ensure they are not putting children in harm's way or enticing youth use, and we'll continue to take action against those who sell tobacco products to youth and market products in this egregious fashion," the US FDA Commissioner Scott Gottlieb, said in 2018.[276] E-liquids have been sold in packaging that looks similar to Tree Top-brand juice boxes, Reddi-wip whipped cream, and Sour Patch Kids gummy candy.[277]
The US FDA announced on August 23, 2018, that all 17 manufacturers, distributors and retailers that were warned by the agency in May, have stopped selling the nicotine-containing e-liquids used in e-cigarettes with labeling or advertising resembling kid-friendly food products, such as juice boxes, candy or cookies that were identified through warning letters as being false or misleading.[278] Following the warning letters in May, the US FDA worked to ensure the companies took appropriate corrective action – such as no longer selling the products with the misleading labeling or advertising – and issued close-out letters to the firms. The agency expects some of the companies may sell the products with revised labeling that addresses the concerns expressed in the warning letters.[278] "Removing these products from the market was a critical step toward protecting our kids. We can all agree no kid should ever start using any tobacco or nicotine-containing product, and companies that sell them have a responsibility to ensure they aren't enticing youth use. When companies market these products using imagery that misleads a child into thinking they're things they've consumed before, like a juice box or candy, that can create an imminent risk of harm to a child who may confuse the product for something safe and familiar," said US FDA Commissioner Scott Gottlieb.[278]
Nicotine toxicity is of concern when e-cigarette solutions are swallowed intentionally by adults as a suicidal overdose.[162] Seizures or convulsions are known potential side effects of nicotine toxicity and have been reported in the scientific literature in relation to intentional or accidental swallowing of e-liquid.[253] Six people attempted suicide by injecting e-liquid.[121] One adolescent attempted suicide by swallowing the e-liquid.[74] Three deaths were reported to have resulted from swallowing or injecting e-liquid containing nicotine.[121] An excessive amount of nicotine for an adult that is capable of being fatal is 0.5–1 mg/kg of body weight.[201] An oral lethal dose for adults is about 30–60 mg.[144] However the widely used human LD50 estimate of around 0.8 mg/kg was questioned in a 2013 review, in light of several documented cases of humans surviving much higher doses; the 2013 review suggests that the lower limit resulting in fatal events is 500–1000 mg of ingested nicotine, which is equivalent to 6.5–13 mg/kg orally.[279] Reports of serious adverse effects associated with acute nicotine toxicity that resulting in hospitalization were very uncommon.[174] Death from intentional nicotine poisoning is very uncommon.[247] Clear labeling of devices and e-liquid could reduce unintentional exposures.[249] Child-proof packaging and directions for safe handling of e-liquids could minimize some of the risks.[270] Some vaping companies willingly used child-proof packaging in response to the public danger.[243] In January 2016, the Child Nicotine Poisoning Prevention Act of 2015 was passed into law in the US,[280] which requires child-proof packaging.[281] The nicotine exposure rate in the US has since dropped by 18.9% from August 2016 to April 2017, following the Child Nicotine Poisoning Prevention Act of 2015, a federal law mandating child-resistant packaging for e-liquid, came into effect, on July 26, 2016.[252] The states in the US that did not already have a law, experienced a notable decline in the average number of exposures during the 9 months after the Child Nicotine Poisoning Prevention Act of 2015 came into effect compared to before it became law.[252] E-liquids have been observed in 2016 to include a press-and-turn feature similar to what is used for aspirin.[243] E-liquids that were normally available in bottles that were not regarded as child-resistant, have been reported in 2016.[243]
There was inconsistent labeling of the actual nicotine content on e-liquid cartridges from some brands,[43] and some nicotine has been found in ‘no nicotine' liquids.[79] A 2015 PHE report noted overall the labelling accuracy has improved.[282] Most inaccurately-labelled examples contained less nicotine than stated.[282] Due to nicotine content inconstancy, it is recommended that e-cigarette companies develop quality standards with respect to nicotine content.[90]
Because of the lack of production standards and controls, the pureness of e-liquid are generally not dependable, and testing of some products has shown the existence of harmful substances.[270] The German Cancer Research Center in Germany released a report stating that e-cigarettes cannot be considered safe, in part due to technical flaws that have been found.[171] This includes leaking cartridges, accidental contact with nicotine when changing cartridges, and potential of unintended overdose.[171] The Therapeutic Goods Administration (TGA) of Australia has stated that, "Some overseas studies suggest that electronic cigarettes containing nicotine may be dangerous, delivering unreliable doses of nicotine (above or below the stated quantity), or containing toxic chemicals or carcinogens, or leaking nicotine. Leaked nicotine is a poisoning hazard for the user of electronic cigarettes, as well as others around them, particularly children."[283]
Cannabinoid-enriched e-liquids require lengthy, complex processing, some being readily available online despite lack of quality control, expiry date, conditions of preservation, or any toxicological and clinical assessment.[284] The health effects specific to vaping these cannabis preparations is largely unknown.[284] There is a connection between cannabis vaping and a variety of unwelcomed health effects.[285]
Concern exists from the risk of injury associated with e-cigarette explosions for adults and children.[74] The exact causes of such incidents are not yet clear.[286] Most e-cigarettes use lithium batteries, the improper use of which may result in accidents.[52] Most fires caused by vaporing devices are a result of the lithium batteries becoming too hot and igniting.[287] Defective e-cigarette batteries have been known to cause fires and explosions.[288] The chance of an e-cigarette blast resulting in burns and projectile harms greatly rises when using low-quality batteries, if stored incorrectly or was altered by the user.[289] E-cigarettes are frequently not made by tobacco or pharmaceutical firms, but by independent manufacturers with little quality control in the making of the e-cigarette device and battery.[290] Inexpensive manufacturing with poor quality control could account for some of the explosions.[197] It has been recommended that manufacturing quality standards be imposed in order to prevent such accidents.[52] Better product design and standards could probably reduce some of the risks.[265] There can be manufacturing defects and damage to the e-cigarette device.[291]
It is recommended that users be informed of appropriate charging and storage methods.[292] In the event the lithium ion substances leak from the battery as a result of an e-cigarette blast, first aid is recommended to prevent additional chemical reaction.[292] An e-cigarette blast can induce serious burns and harms that need thorough and lengthy medical treatment particularly when a device goes off in hands, mouths, or pockets.[293] A 2017 review found "The electrolyte liquid within the lithium ion battery cells is at risk for overheating, thus building pressure that may exceed the capacity of the battery casing. This "thermal runway" [sic] can ultimately result in cell rupture or combustion."[294] Some lithium-ion batteries used in e-cigarettes do not have any protection to prevent the coil from overheating.[290] Metal objects, including coins or keys, can cause a short circuit when kept with batteries, which can result in overheating of the battery.[294] It is recommended to use insulated protective cases for batteries not in use to lessen the potential risk related to thermal runaway.[295] There are vaping devices available that are made with safety features such as firing buttons locks, vent holes, and protection against overcharging..[296] Swallowing e-cigarette batteries can be toxic.[297]

The numbers of medical reports from harms resulting from vaping have continued to increase since 2016.[197] Some batteries are not well designed, are made with poor quality components, or have defects.[76] Major injuries have occurred from battery explosions and fires.[43] Fires caused by e-cigarettes appear to be increasingly frequent.[287] Direct harms from an e-cigarette blast include hand harms, face harms, waist/groin harms, and inhalation harms.[287] Indirect harms happened when the vaporing device set on fire another object and resulted in a house fire, followed by harm from fire burns or inhalation.[287] E-cigarette explosions have resulted in burns, lost teeth, neck fractures,[298] bone fractures,[15] and battery acid contact to the face, mouth, and eyes.[298] The extent of the burns varied from 1% to 8% total body surface area, were reported and most commonly occurred in the lower extremity, hands, head and neck, and genitalia.[294] The extent of the burn was mainly deep partial and full thickness.[294] E-cigarette explosion harms correlated with malfunctioning of the device can result in minor total body surface area 2nd and 3rd degree burns.[299] Around 50% needed surgical management for the burn.[294] This was due to the extent of the injury.[294] The most common harms are burns as a result of explosion in the pocket and harms to the face.[287] A 2017 review found "Several of the reported cases show that 'the battery in pocket' precedes the incident. The damp environment in the pocket may have sufficient moisture to start a chemical reaction within the lithium-ion battery and the presence of metal objects can produce short-circuit which can over heat the battery leading to an explosion."[292] Flame burns, chemical burns, and blast injuries have occurred as a result of the e-cigarette battery overheating.[300]
A man endured a unilateral corneoscleral laceration with prolapsed iris tissue and hyphemato to the eye area when an e-cigarette exploded in his mouth.[298] A young man endured bilateral corneal burns to the eye area when an e-cigarette exploded near his chest.[298] A man perished when his charging e-cigarette blew up and caught on fire next to oxygen equipment.[298] House and car fires and skin burns have resulted from some of the explosions.[76] The explosions were the result of extended charging, use of unsuitable chargers, or design flaws.[52] There is a possible risk to bystanders from e-cigarette explosions.[298] There is also a risk of property damage as a result of flammable materials catching on fire from an e-cigarette explosion.[298] A March 2016 research article assembled reports by US government agencies and in the media of 92 e-cigarette blasts, fire, or overheating events, with related injuries in 47 individuals.[301] Prominent harms included 2 cervical vertebral fractures, 1 palate fracture, 3 instances of damaged teeth, 33 thermal burns, 4 chemical burns, and 5 lacerations.[301]

Between January 2015 and May 2016, 35 burns and correlated injuries were caused by e-cigarette explosions.[294] Between January 2009 and December 31, 2016, 195 separate incidents of explosion and fire involving an e-cigarette were reported by the US media.[291] These incidents resulted in 133 acute injuries.[291] Of these injuries, 38 (29 percent) were severe.[291] Sixty-one incidents occurred when either the device or spare batteries for the device were in a pocket.[291] Sixty incidents occurred while the device was being used.[291] Forty-eight incidents occurred while the battery in the device was being charged.[291] Eighteen incidents occurred while the device or battery was stored.[291] In seven incidents, it is not reported whether the e-cigarette was in use, stored, or being charged.[291] One incident occurred during transportation on a cargo aircraft.[291] Media reports generally characterize these incidents as explosions.[291] While there is generally a brief period of overheating and off-gassing at the onset of the event, the events tend to occur suddenly, and are accompanied by loud noise, a flash of light, smoke, flames, and often vigorous ejection of the battery and other parts.[291] A number of the media reports state that the battery or other components of the device were ejected under pressure and "flew across the room," often igniting combustible items where they landed.[291]
The United States Fire Administration stated in 2014 that 25 fires and explosions in the US were caused by e-cigarettes between 2009 and August 2014.[291] This list is not considered to be complete because it is very possible that there were events that were not disclosed to the fire department or mentioned in the media.[291] Up to 2014, twenty events happened when charging the battery in the e-cigarette.[291] Two events happened during use.[291] In two events, it is unclear whether the device was in use, not in use or was charging.[291] One event happened while being transported on a cargo aircraft.[291] Several burns were reported.[291] Two serious harms were the result of devices exploding in users' mouths.[291] A 2017 review found that "The U.S. Fire Administration reports that 80% of e-cigarette explosions occurred while the battery was being charged. The report revealed that many of the e-cigarettes were being charged by power adaptors that were not provided by the manufacturer, subjecting the battery to an inappropriately high current, which led to thermal runaway and subsequent explosion and/or fire. This problem is potentially further exacerbated by third-party vendors who assemble e-cigarettes from noncompatible parts that may not meet the manufacturers' specifications."[301] The shape of these devices is another concern.[301] They are likely to be cylindrical, with the least strongest structural points at both ends.[301] In the event there is a breach in the battery seal, the pressure inside the e-cigarette can quickly build, launching the ends of the device with a great abundance of force.[301]
The United States Fire Administration stated in 2017 that of the reported fire and explosion incidents involving e-cigarettes, 128 (66 percent) resulted in ignition of nearby contents such as clothing, carpets, drapes, bedding, couches, or vehicle seats.[291] Users were generally nearby when the incident occurred, were alerted by the sound of the explosion, and were able to take action to extinguish the fires while they were still small.[291] In 91 incidents, the fire spread was minor, meaning that the scorching or flames either self-extinguished or were extinguished very quickly by persons nearby.[291] Typically, in these incidents, the burned areas were 6 inches or less in diameter.[291] In 27 incidents, the fire spread was moderate, where the burned area was larger than 6 inches in diameter, but the fire was extinguished by occupants before the fire department arrived.[291] In 10 incidents, the fire spread was major and involved significant portions of a building, and required suppression by the fire department.[291] Typically, these incidents are what the fire service refers to as "room and contents" type fires, or larger.[291] In 67 of the incidents (34 percent), there was no fire spread, or fire spread was not evident in the reports reviewed.[291]
The majority of reported e-cigarette-related oral injuries have been serious and have frequently required the intervention of a plastic surgeon.[302] The injuries included tooth fracture and tooth avulsion, jaw fracture, dento-alveolar fracture, hematoma formation, traumatic ulceration and tattooing, intra-oral burns and subsequent necrosis, palate perforation with extension into the nasal cavity and extensive soft tissue deficits.[302] A 2020 case report of a 19-year-old male was presented with a maxillofacial injury after an e-cigarette battery-related explosion occurred in his mouth.[302] Significant hard and soft tissue injuries of the oral cavity, in particular the anterior left maxilla was observed.[302] Additionally, there were epidermal burns to the facial area, including the lips and upper chest; the upper lip sustained minimal soft tissue damage.[302]

Even though there are knowns risks with unregulated lithium batteries causing serious harm, importing e-cigarettes to the UK is still not restricted and they do not conform to the British Standards, which may increase their chance of resulting in fire and blowing up.[292] There has been a rise in the number of burns due to blasts of the e-cigarettes battery in South Wales and South West England.[292] In the UK fire service call-outs had risen, from 43 in 2013 to 62 in 2014.[304] A 2015 PHE report concluded that the risks of fire from e-cigarettes "appear to be comparable to similar electrical goods".[305] A 2018 PHE report found six case studies involving e-cigarettes with burns in the UK.[306] Every person were male and 33 years was the average age.[306] In five cases, they received burn harms resulting from an e-cigarette blast in their pants pocket.[306] One case happened while coins and the e-cigarette were in the same pocket.[306] Another case happened when the e-cigarette was being charged.[306] Harms included burns accounting for 1–7% of the complete body surface region.[306] Harms happened to the thigh, genitals, foot, and hands.[306] Chemical burns from the battery was included in one case.[306] Since e-cigarettes are not subjected to product safety testing, they may not have safety designs to avoid overheating, thermal runaway, and battery failure including fire and explosions.[298] There is inadequate product labeling to inform users of the possible serious harms.[298] The risk from serious adverse events is low, but the aftermath may be disastrous in respect to an e-cigarette blast.[298] Numerous stories about the e-cigarette blasts were reported in the news media and victims have filed lawsuits to make restitution from the blasts.[121] Adverse events may be under-reported because reports to the US FDA is voluntary.[298]

In January 2015 the US Federal Aviation Administration issued a safety alert to air carriers that e-cigarettes should not be allowed in checked baggage after a review of fire safety issues, including two fires caused by e-cigarettes in checked baggage.[308][309] The International Civil Aviation Organization, a United Nations agency, also recommends prohibiting e-cigarettes in checked luggage.[308] A spokesman for the Tobacco Vapor Electronic Cigarette Association said that e-cigarettes do not pose a problem if they are packed correctly in static-free packaging, but that irresponsible people may sometimes pack them carelessly or tamper with them.[308] In 2015 the US Department of Transportation prohibited storage of e-cigarettes in checked baggage on airplanes to avoid damage and injury due to an explosion.[121] In-flight use of e-cigarettes is prohibited in the US.[309] A 2017 review stated "Passengers are allowed to carry e-cigarettes with them onto planes, but are not allowed to charge their batteries during flight."[166]
Individuals sent to Saint Louis Hospital Burn Center in Paris, France from June 2016 to July 2017 for harms resulting from e-cigarettes were ten.[197] Four individuals were admitted to the hospital and six of them received care at an Outpatient Burn Clinic.[197] All of them had burns of at least one arm or leg.[197] In 2014 a 72-year-old male with pulmonary fibrosis was hospitalized for 5 days at the Maisonneuve-Rosemont Hospital in Montreal with facial burns that happened after his nasal prongs caught on fire from using an e-cigarette while on oxygen therapy.[310] Several burn events during vaping while on home oxygen therapy have happened, leading Health Canada in 2014 to release a warning of fire risk to oxygen therapy users from vaping.[310] The heating element in vaping devices reaches a high temperature which can possibly ignite in the presence of oxygen.[310] Vaping while on oxygen therapy is not recommended.[310]
E-cigarette-related fires and explosions are a new risk to people and pets.[263] In 2016, the US FDA Center for Tobacco Products reviewed and summarized reports from other US government agencies, the news media, and scientific articles about e-cigarette-related fires and explosions, finding that some events have resulted in life-threatening injury, and permanent disfigurement or disability.[263] Although there were no reports of pets being injured, the risk still exists.[263] Pets that chew on the devices may potentially puncture the cartridges or batteries, or they may inadvertently turn on the devices.[263] The US Food and Drug Administration recommends to keep e-cigarettes and all other tobacco products out of reach of children and pets at all times.[263]
Users may alter many of the devices, such as using them to administer other drugs like cannabis.[43] E-liquid mixing is another way users tamper with e-cigarettes.[75] Mixing liquid in an unclean area runs the risk of contamination.[62] User modified THC and nicotine products can contain unidentified contaminants.[311] Users may add various flavorings and diluents.[75] Vodka or other forms of alcohol may also be added.[75] The addition of alcohol or nicotine could expose the user to more toxicants, especially when added in combinations.[75] Some ingredients in e-liquids could be flammable; this risk is more of concern for users who are inexperienced or do not use protective gear.[75] Users can adjust the voltage of some e-cigarettes.[75] The amount of vapor produced is controlled by the power of the battery, which has led some users to adjust their e-cigarettes to increase battery power to obtain a stronger nicotine "hit", but there is a small risk of battery explosion.[77] Some users add additional batteries or a bigger battery to a nonadjustable e-cigarette to boost voltage output, which may end up causing a leaking battery or explosion.[75] The US FDA stated to only use batteries recommended for use with the device.[286] The US FDA recommended to replace the batteries if they get damaged or wet.[286] The extent to which teens are altering e-cigarettes, such as dripping the liquids onto the atomizer to get more nicotine intake, is not known.[74]
| Patient demographics (age, sex, country) | Pre-existing medical history | Smoking history | Presentation/signs | Treatment | EC device/refill fluid info | Diagnosis | Health outcome | Other notes & comments | Source |
| Systemic effects respiratory | |||||||||
| 42, F, USA | 7 mo. history dyspnea, productive cough, subjective fevers, asthma, rheumatoid arthritis, fibromyalgia, schizoaffective disorder, hypertension. Respiratory symptoms coincided with EC use 7 mo. prior. | N/A | 7 mo. history of dyspnea, productive cough, subjective fever. Mild tachycardia | Abstained EC use; prescribed medication | No EC brand, EC refill fluid specified. 7 mo. history of EC use | (2) Exogenous lipoid pneumonia due to EC use. | Symptoms improved after abstained EC use; chest radiograph showed mild diffusion impairment but no permanent damage. | First respiratory case report attributed to EC use. Three other known cases of lipoid pneumonia linked to EC have been reported. | McCauley et al. (2012) |
| 43, M, FR | Pulmonary lung adenocarcinoma and isolated brain metastasis. | 45 pk-yr, history; cessation attempt w/ nic. patch (21 mg) and cont. Smoking 20 cig/day. | Bronchial syndrome associated w/ deterioration of pulmonary function tests after starting EC use. | Abstained EC use | La dynamique (CIGARTEX); EC refill fluids: Kentucky and Eastern (19 mg/ml). Vaped 25 ×/day, 56 puffs/session (125150/day). | Subacute bronchial toxicity | After 48 h. improvement in cough, sputum, breathlessness; by day 7 all symptoms resolved. | Hureaux et al. (2014) | |
| 20, M, USA | Previously healthy; family history of pulmonary embolism | N/A | Shortness of breath, tachycardia. | Prescribed medications | No EC brand, EC refill fluid specified. | Acute eosinophilic pneumonia | Resolved health effects with medical care and treatment | Trigger undesired resp. effects in previously healthy individual. | Thota and Latham (2014) |
| 43, M, US | History of hypertension. | Unspecified 7 yr. smoking history. | Shortness of breath, pleuritic chest pain. | Breathing treatments and antibiotic treatments. | No EC brand, EC refill fluid specified. | Pneumonia and bilateral pleural effusions. | Dismissed after two days hospitalization and resolved. | Fourth case of pneumonia and first case of pleurisy | Moore et al. (2015) |
| 60, M, USA | N/A | Unspecified smoking history | Shortness of breath, pleuritic | Medical care received | No EC brand specified Unspecified flavors with diacetyl | Acute lipoid pneumonia. | Dismissed after two days hospitalization and resolved. | Second case of lipoid pneumonia in USA | Atkins and Drescher (2015) |
| 31, F, USA | N/A | Unspecified smoking history | Shortness of breath | Medical care received | No EC brand, EC refill fluid specified. | Inhalation injury and suspected hypersensitivity | Dismissed and in two days health effects resolved. | Inhalation of diacetyl in EC refill fluids is a health concern. | Modi et al. (2015) |
| Gastrointestinal | |||||||||
| 35, M, USA | 1.5 year history of pan-ulcerative colitis (UC); began 4 wks. after smoking cessation. | Past smoker; details not provided. | Before EC use: daily bloody bowel movements w/ severe incontinence | EC use initiated | No EC brand, EC refill fluid specified mean 105 puffs/day (range: 45191). Effects for 12 weeks | Relapsed medically refractive UC after EC use. | EC use was associated w/ steroid-free clinical remission in patient UC. | EC use w/ smoking cessation helped symptoms. | Lee et al. (2013) |
| 49, F, FR | UC affecting rectum and rectum and sigmoid colon (diag. 2004); Hysterectomy for endometriosis (diag. 2008) | 20 cigarettes/day for 20 yrs. | UC symptoms began 3 mo. after patient quit smoking; bloody diarrhea. | Patient resumed smoking 9 mo. after UC diagnosis | No EC brand info; 30 mg liquid nicotine/day w/ use of disposable cartridges of 10 ml every 5 days at 16 mg/ml | Smoking dependent UC | Clinical remission within a few days of resumed smoking | Indicates nicotine may not be the only factor with protective effects for UC. | Camus et al. (2014) |
| 1 day old infant, M, USA | Gastrointestinal bleeding | N/A | Abdominal distention, respiratory distress. | Double barrel ileostomy w/ subsequent surgery procedures | N/A; suspected cause due to in utero exposure, mother using EC ~ 3050 ×/day; ~ 5070 ×/day. No EC brand, EC refill fluid specified. | Isolated chronic necrotizing enterocolitis. | At 6 month infant recovered; 9 month development milestone met. | First pregnancy health effect linked to EC | Gillen and Saltzman (2014) |
| Cardiovascular | |||||||||
| 70, F, USA | Hypertension, hyperlipidemia osteoarthritis, allergic rhinitis, remote history of breast adenocarcinoma; right hip fracture, hip during arthroplasty. | 40 pack-year history; attempted cessation in preceding 56 months | Subsequent hematoma drainage, patient developed 3 ep. of asymptomatic acute atrial fibrillation (AF) | Patient asked to discontinue EC use. | No EC brand, EC refill fluid specified | Paroxysmal AF | Eliminated episodes of AF for remainder of hospitalization. | Although the patient has significant medical history, all AF ep. occurred only EC use. | Monroy et al. (2012) |
| 24, M, TR | Previously healthy | 1 pack/day for 4 yrs.; 1 mo. cessation attempt. | Chest pain 4 h prior to liquid nicotine use. | Prescribed med. | No EC brand specified; tobacco flavored nicotine concentration 16 mg/day use. | Acute myocardial infarction | Evaluated one month later and free of symptoms. | Myocardial infarction in individuals < 30 yr. of age is rare. | Kivrak et al. (2014) |
| Neurological | |||||||||
| 39, M, FR | Previously healthy | 60 cig/day for 20 yrs. | 7 day history of headaches and 2 seizures. | Prescribed med and abstained EC use; cont smoking 1015 cig/day w/ nicotine patch. | No EC brand specified; Nicotine concentration was 12 mg/ml. | Reversible cerebral vaso-constriction syndrome. | Headache resolved by day 3, no recurrence of seizures. | First neurological negative case report associated with EC use. | Vannier et al. (2015) |
| Immune | |||||||||
| 28, M, GR | Chronic idiopathic neutrophilia CIN) since 2005; hyperlipidemia treated w/ med.; no other history of infection, trauma, or fever. | Smoker since 1996; 9 pack-yr | After EC use, patient quit smoking in 10 days and leukocyte and C reactive protein normalized in 6 mo. | Prescribed med. for elevated LDL levels, cont. EC use | No EC brand specified; nicotine concentration 9 mg/ml | Smoking cessation w/ EC use reversed CIN. | First positive health affected attributed to EC use. | Farsalinos and Romagna (2013) | |
| Accidental nicotine poisonings | |||||||||
| 10 mo. old infant, M, USA N/A | N/A | Vomiting, tachycardia grunting respirations, truncal ataxia developed after ingestion of EC refill fluid. | Unspecified medical treatment. | N/A; affected accidental ingestion of Wintergreen EC refill fluid w/ nicotine (18 mg/ml) but unknown PG, glycerin, and flavoring concentrations. | Nicotine poisonings | Recovered baseline health after 6 h of ingesting EC refill fluid. | First reported case of nicotine poisoning in a young child in literature. | Bassett et al. (2014) | |
Toxicology
Limited understanding

The long-term health impacts of e-cigarette use are unknown.[72] The long-term health impacts of the main chemicals nicotine and propylene glycol in the aerosol are not fully understood.[313] There is limited peer-reviewed data about the toxicity of e-cigarettes for a complete toxicological evaluation,[314] and their cytotoxicity is unknown.[315] A limited number of e-cigarettes in the marketplace have undergone a comprehensive toxicological examination.[123] The chemicals and toxicants used in e-cigarettes have not been completely disclosed and their safety is not guaranteed.[201] While there is variability in the ingredients and concentrations of ingredients in e-cigarette liquids, tobacco smoke contains thousands of chemicals, most of which are not understood and many of which are known to be harmful.[199] Because there are numerous variations of vaping devices, diverseness in e‑liquids, and differences in usage behaviors, the potential toxicity of the inhaled emissions to the user is hard to quantify.[126] Many variables affect the levels of toxicants in the e-cigarette vapor, including the design, the type of liquid, and user behavior.[174]
Carcinogenicity
Concerns about the carcinogenicity of e-cigarettes arise from both nicotine[82] and from other chemicals that may be in the vapor.[90] There is no long-term research regarding the cancer risk related to the potentially small level of exposure to the identified carcinogens in the e-cigarette vapor.[44] Their long-term effect on risk of developing cancer is not known.[81] Heating the products in e-cigarettes produces condensed carcinogenic hydrocarbons and products toxic to the human body.[316] One example is the presence of nickel and ethylene oxide, substances linked to lung and sinus cancers, lymphomas, multiple myeloma, and leukemia.[316] In animal studies, nicotine alone causes sarcomas and leiomyomas.[317]
The International Agency for Research on Cancer does not consider nicotine to be a carcinogen, though several studies demonstrate it is carcinogenic.[84] Because it can form nitrosamine compounds (particularly N-Nitrosonornicotine (NNN) and nicotine-derived nitrosamine ketone (NNK)) through a conversion process, nicotine itself exhibits a strong potential for causing cancer.[39] About 10% of breathed in nicotine is estimated to convert to these nitrosamine compounds.[39] Nitrosamine carcinogenicity is thought to be a result of enhanced DNA methylation and may lead to an agonist response on the nicotinic acetylcholine receptors, which acts to encourage tumors to grow, stay alive, and penetrate into neighboring tissues.[39] Although nicotine in the form of nicotine replacement products is less of a cancer risk than with smoking,[318] there is evidence that nicotine may cause oral, esophageal, or pancreatic cancer.[319] Nicotine has a strong tumor-inducing effect on several kinds of cancers.[50] This is because "nicotinic receptors are expressed on the surface of tumor and immune cells, enabling nicotine to directly affect the tumor microenvironment."[50]
The World Health Organization has identified heated propylene glycol as a carcinogen, and the saliva of e-cigarette users has been found to contain carcinogens commonly associated with traditional smoking, including N-nitrosonornicotine and thiocyanates.[320] Therefore, e-cigarette vapors could still have cytotoxic, genotoxic, and inflammatory effects.[320] Many adverse effects could occur at the cellular level after long-term exposure to these harmful aerosols, including reduced cell proliferation and activity, changes in cell morphology and activity, cell apoptosis and necrosis, DNA damage, and increased transcription of pro-inflammatory cytokines, with an increased risk of carcinogenesis.[320]
Cancer cell proliferation and survival

Evidence from experimental in vitro studies on cell cultures, in vivo studies on rodents as well as studies on humans inclusive of epidemiological studies indicate that nicotine itself, independent of other tobacco constituents, may stimulate a number of effects of importance in cancer development.[322] Nicotine acts primarily by activation of nicotine acetylcholine receptors and nicotine binds to these receptors with a higher affinity than acetylcholine.[322] Nicotine can enhance cancer cell survival via attaching to nicotinic receptors.[50] It may also diminish cancer cell death resulting from chemotherapy, radiotherapy, or tyrosine kinase inhibitors.[50] Nicotine promotes metastasis by causing cell cycle progression, epithelial-to-mesenchymal transition, migration, invasion, angiogenesis, and avoidance of apoptosis in a number of systems.[323] Nicotine does promote the growth of blood vessels that supply tumors and it speeds tumor growth.[158] Whether long-term vaping can raise the chance for malignancy in individuals with a susceptibility for tumor growth is unknown.[324] The effects of nicotine on the sympathoadrenal system could stimulate the advancement of cancer in people who have cancer.[50] The stimulation effects of nicotine on cancer development and growth may also be associated with other forms of nicotine use such as patch, nasal or mouth spray, inhalator, mouth strip, gum, and lozenge.[50]
The interaction of nicotine with nicotinic acetylcholine receptors activates signaling pathways that result in a number of reactions, such as increased cell proliferation and cell survival.[322] Although nicotinic acetylcholine receptors are the primary receptors, binding of nicotine to β-ARs and EGFRs may also be important.[322] Nicotine induces epithelial–mesenchymal transition, which is one of the vital steps for the acquisition of malignant phenotype.[322] This transition allows the cell to acquire migratory properties, which may facilitate cancer metastases.[322] Moreover, nicotine induces changes that mimic the effects of angiogenic growth factors.[322]
In mice studies with NNK as an initiator, nicotine acts as a promoter after injection or dermal absorption, but not after oral administration.[322] In drinking water experiments, there is considerable first-pass metabolism of nicotine before nicotine enters the systemic circulation.[322] As a result, serum concentration is much lower after ingestion than after intraperitoneal injection administration.[322] Nicotine enhanced tumor growth and progression after injection of malignant cells in mice.[322] Enhancements were found both after exposure of nicotine by intraperitoneal injection, oral, and skin administration.[322] Moreover, cotinine did also enhance tumor growth.[322] Nicotine may inhibit antitumor immune response.[322] It has also been reported that exposure to nicotine adversely affects dendritic cells, a cell type that has an important role in anticancer immunosurveillance.[322] Moreover, in studies on xenograft in mice, nicotine has been found to reduce the effect of radiotherapy and chemoradiotherapy.[322]
Upregulation of FOXM1 expression is an early event during cancer development.[325] The evidence suggests that FOXM1 plays a key role in cancer initiation.[325] FOXM1 also promotes cancer progression by facilitating cancer angiogenesis, invasion, and metastasis.[325] Upregulation of FOXM1 by itself can exacerbate genomic instability.[326] This is calculated by loss of heterozygosity and copy number variations in human oral keratinocytes.[326] Moreover, nicotine intensifies FOXM1-induced genomic instability.[326]
DNA damage and oxidative stress

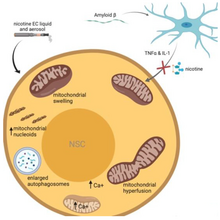
Nicotine has been shown to induce DNA damage in the Escherichia colipol A+/pol− test.[322] Low concentrations of nicotine stimulate cell proliferation, while high concentrations are cytotoxic.[322] Nicotine decreases the tumor suppressor Chk2, which is activated by DNA damage.[322] The decrease in Chk2 in cells exposed to nicotine suggests that nicotine may be capable of overriding DNA damage checkpoint activation, disrupting genetic surveillance, and increasing the risk of oncogenesis.[322] There is strong evidence that some substances found in e-cigarette vapors such as formaldehyde and acrolein can induce DNA damage and mutagenesis.[329]
Nicotine has been shown to induce chromosomal aberration, chromatid exchange, single-strand DNA strand breaks, and micronuclei in vitro.[322] Oxidative stress is probably involved since the effects are reduced in the presence of antioxidants.[322] The finding that the effects decrease after co-incubation with a nicotinic acetylcholine receptor antagonist indicates a receptor-dependent pathway for induction of oxidative stress.[322] All types of e-cigarettes, including non-nicotine ones, have been reported to induce oxidative stress, thereby increasing the risk of cognitive-related impairment in teenagers.[181]
The e-cigarette vapors triggered DNA strand breaks and lowered cell survival in vitro,[121] regardless of nicotine content.[246] A 2013 study found some samples of e-cigarette vapors had cytotoxic effects on cardiac muscle cells, though the effects were less than with cigarette smoke.[51] Studies demonstrate that e-cigarette vapor have adverse effects on primary airway epithelial cells and tumor cell lines, and other epithelial cell lines, that ranged from reducing viability, an increase in production of inflammatory mediators and oxidative stress, to reducing antimicrobial defences and pro-carcinogenic events.[221]
The potential effects of next-generation products on oxidative stress are being debated.[312] A deviation from the metabolic steady state leads to the concept of oxidative stress.[312] Oxidative stress describes an imbalance between oxidants, such as reactive oxygen species or reactive nitrogen species, and antioxidant species, in favor of oxidants.[312] The aerosols produced from next-generation products (such as e-cigarettes) can result in oxidative stress.[312] A 2017 study showed that e-cigarettes have a potent booster effect on phase I carcinogen bioactivation enzymes, including polycyclic aromatic hydrocarbon activators, and increase oxygen free radical production and DNA oxidation to 8-hydroxy-2'-deoxyguanosine.[312]
There is limited research examining the impact of nicotine exposure on neural stem cells and their mitochondria.[328] A 2019 study demonstrated a mitochondrial stress response in neural stem cells following exposure to e-liquids and their aerosols.[328] The study also reported that the effects of e-cigarettes on the mitochondria are mediated by nicotine and not by the transfer of volatile organic chemicals or solvents found in e-liquids (propylene glycol and glycerin).[328] This study also provided evidence that e-liquids and aerosols can cause significant, not-easily-reversible damage to the mitochondria of neural stem cells.[328] E-cigarette treatments led to changes in the mitochondrial membrane potential, incited aggregation of mitochondrial nucleoids and mitochondrial DNA, and incited calcium influx, which resulted in plasma membrane retraction and intracellular calcium overload.[328] Nicotine appears to have differential effects on these immature cells of neural lineage, which depends on both location and maturation.[328] The mitochondria of neural stem cells appear to play an important role in these interactions between neural stem cells, glia, and nicotine.[328] Nicotine may have varying effects on neural stem cells which depends on the route of administration.[328]
Tobacco-specific nitrosamines and toxicants

A range of chemicals and ultrafine particles are toxic and/or carcinogenic have been found in the e-liquids and inhaled and exhaled e-cigarette aerosols.[90] The majority of e-cigarettes evaluated included carcinogenic tobacco-specific nitrosamines (TSNAs); heavy metals such as cadmium, nickel, and lead; and the carcinogen toluene.[201] However, in comparison to traditional cigarette smoke, the toxic substance levels identified in e-cigarette vapor were 9- to 450-fold less.[201] E-liquid with tin was cytotoxic.[102] A 2018 study found significantly higher amounts of metals in e-cigarette vapor samples in comparison with the e-liquids before they came in contact with the customized e-cigarettes.[330] For example, nickel and tin were 600% higher in the e-cigarette vapor than in the e-liquid.[330]
Since nicotine-containing e-liquids are made from tobacco they may contain impurities like cotinine, anabasine, anatabine, myosmine and beta-nicotyrine.[72] The health implications of nicotine-related impurities are not known.[209] A 2016 review found "Some studies have demonstrated that impurities and nicotine degradation products such as nicotine-cis-N-oxide, nicotine-trans-N-oxide, myosmine, anabasine, and anatabine, which are very carcinogenic, can be found in e-cigarette refill liquids. The molecules can lead to mutations in genes such as Ras (vital function in signal transduction of cell proliferation), p53 and Retinoblastoma (with roles as tumour suppressors) as these molecules can form adducts with cellular DNA."[216]
The TSNAs NNN (N-nitrosonornicotine) and NNK (4-(metylnitrosamino)-1-(3-pyridyl)-1-butanone) may be formed from nicotine after oral administration.[322] After uptake of nitrosamines, including but not limited to NNK and NNN, they are metabolized by cytochrome P450s, and the resulting metabolites can subsequently breakdown into formaldehyde, methyldiazohydroxides, and pyridylic-butylic by-products.[317] All of these by-products are possible DNA harming substances, whereas the cancer-causing characteristics of nitrosamines are mainly associated with methyldiazohydroxides.[317] Methyldiazohydroxides can provoke the formation of mutagenic and carcinogenic O6-methyl-deoxyguanosines adducts, and can also form minuscule adducts of methylated thymine and methylated cytosine.[317] NNN and NNK are classified by International Agency for Research on Cancer as human carcinogens.[322]
Brain cancer
In a 2020 study, chronic administration of nicotine to mice (1 mg/kg every 3 days for a 60-day period) enhanced brain metastasis by skewing the polarity of M2 microglia, which increases metastatic tumor growth.[117] Nicotine can contribute to causing brain metastasis.[331] A 2021 review states that a 2020 study produced conclusive evidence that e-cigarette use may aid in sustaining malignancy.[49] Immunocompetent mice undergoing orthotopic breast tumor cell injection exposed to nicotine containing e-cigarette aerosol successfully developed tumors in all cases, whereas only one third of the control group did.[49]
Breast cancer
Nicotine may promote breast cancer initiation, development, angiogenesis, invasion, and metastasis, as well as possibly reducing the response to breast cancer treatment.[332] E-cigarette aerosol encourages breast carcinoma development in vitro by means of macrophage-tumor cells cross-talk, aided by both CCL5 and VCAM-1.[119]
Colorectal cancer
The use of alcohol with nicotine increases the likelihood of getting colorectal cancer.[333]
Gastrointestinal cancer
4-(metylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK), a nitrosated derivative of nicotine, has been implicated in its carcinogenic effects in promoting gastrointestinal cancers.[334]
Head and neck cancers

Nicotine encourages the development of head and neck cancer by inducing endogenous activity of FOXM1 through loss of heterozygosity via participation in the entirety of chromosome 13 and by inducing copy number abnormality via participation in oral keratinocytes.[336][337] FOXM1 has been shown to possess the ability to cross-talk with other molecules that play a role in cancer development (like: NF-κB, prostaglandin-endoperoxide synthase 2, extracellular signal-regulated kinases, and matrix metalloproteinase).[338] In most human cancers, FOXM1 is overexpressed.[339] FOXM1 is a crucial regulator of many biological processes and tissues, and dysregulation of FOXM1 can significantly contribute to tumorigenesis and cancer progression.[339]
Because of the conflicting evidence, the role that vaping plays in the development of head and neck cancers is obscure and inconclusive.[340] There is just a minimal amount of literature that is applicable to vaping and head and neck cancers.[340] There is some evidence suggesting a potentially carcinogenic role of e-cigarettes in the pathogenesis of head and neck cancers.[341]
According to the International Agency for Research on Cancer, acrolein, which has been found in e-cigarette aerosol, is classified as a group 2A compound—probably carcinogenic to humans.[316] There is plenty of evidence from in vitro, in vivo, and human cohort studies that indicate this aldehyde’s cancer potential.[316] Moreover, the research shows that acrolein, by affecting specific signaling pathways, is not only directly involved in mutagenesis but also contributes to increasing the resistance of cancer cells to traditional cisplatin chemotherapy.[316] Clear evidence for the carcinogenic and cytotoxic properties of acrolein is provided by the studies of Matsumoto et al., where a 2-year inhalation of acrolein in both mice and rats induced, among others, squamous cell carcinomas in the nasal cavity.[316]
Lung and bladder cancers
There is growing concern that vaping may increase the likelihood of developing lung cancer.[39] The long-term effects of e-cigarette use on developing lung cancer is unknown,[39] though their long-term use is anticipated to raise the risk of developing lung cancer.[87] A 2021 review suggested that e-cigarette use may greatly increase the risk of developing lung cancer.[39] There is emerging evidence that indicates vaping could play a part in the development of other malignant tumors like lung and bladder cancers.[340]
A 2019 study showed that mice exposed to nicotine delivered by means of e-cigarette aerosol develop lung adenocarcinoma.[342] This suggests the need for caution when using nicotine replacement therapies and e-cigarettes.[342] A 2019 study showed that FVB/N mice exposed for 54 weeks to e-cigarette aerosol resulted in extensive DNA damage in the lungs, heart, and bladder mucosa and reduced DNA repair in the lungs.[312] Products derived from e-cigarette aerosol, such as nicotine and its derivatives, cause the same deleterious effects in human lung epithelial cells and bladder urothelial cells.[312]

Nicotine promotes endothelial cell migration, proliferation, survival, tube formation, and nitric oxide production in vitro, mimicking the effect of other angiogenic growth factors.[322] In 2001, it was found that nicotine was a potent angiogenic agent at tissue and plasma concentrations similar to those induced by light to moderate smoking.[322] Effects of nicotine on angiogenesis have been demonstrated for a number of tumor cells, such as breast, colon, and lung.[322] Similar results have also been demonstrated in in vivo mouse models of lung cancer, where nicotine significantly increased the size and number of tumors in the lung, and enhanced metastasis.[322]
In several in vitro experiments, it has been found that nicotine in concentrations as low as 1 μM decreased the anti-proliferative and pro-apoptotic effects exerted by chemotherapeutics on several different malignant cell lines.[322] These effects were partially reverted by exposure to α-bungarotoxin (α-BTX), an inhibitor of α7-nAChR.[322] In the case of radiotherapy (RT), nicotine administration increased survival of H460 and A549 lung cancer cells.[322] This effect was likewise reduced by addition of α-BTX prior to nicotine addition and radiation.[322] On this basis, it is expected that use of nicotine products during cancer treatment may reduce the effects due to reactions following interaction of nicotine with α7-nAChR.[322]
E-cigarettes deliver the potent lung carcinogen NNK.[158] Some evidence indicates that the NNK dose-response curve for cancer is highly nonlinear, with substantial increases in risk at low doses.[158] Known bladder carcinogens have been detected in the urine of e-cigarette users but not in non-users.[158] This included pyrene, naphthalene, fluorene, phenanthrene, and o-toluidine.[119] A 2015 study reported that the urine from users of e-cigarettes had very low levels of NNAL (4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol), which may suggest that endogenous formation of TSNA after nicotine inhalation is negligible.[322] The data does indicate that TSNA may be formed internally after absorption of nicotine through the mucous membranes in the oral cavity and through the skin, while formation after lung absorption may be negligible.[322] Thus, the toxicokinetics of nicotine may depend on the route of administration.[322] The role of nicotine in carcinogenesis is of great importance in the evaluation of potentially harmful effects from non-tobacco related sources of nicotine, such as e-cigarettes.[322]
Mouth and throat cancers
—Meenu Maan and colleagues, Critical Reviews in Toxicology[343]
A 2015 study found carcinogenicity activity mainly occurred in the lungs, mouth, and throat, which may be associated with nitrosamines, propylene glycol and some flavoring additives.[225] No compelling evidence from vaping indicates it directly causes oral cancer,[344] though several case studies have reported oral cancer development in people with a history of vaping.[49]
Stomach cancer
There is an association between long-term nicotine use and initiating the onset of gastric tumors.[334]
Urologic cancer
The long-term effects of vaping on urologic malignancy are not well understood but because of their likenesses to tobacco smoke, their possible consequences are worrying.[119]
Sarcoma
Nicotine can cause muscle sarcomas in A/J mice.[336] Long-term uptake of nicotine in A/J mice causes leiomyosarcomas and rhabdomyosarcomas.[336] This suggests nicotine directly participates in initiating cancer.[336]
Propylene glycol and other content

The primary base ingredients of the liquid solution is propylene glycol and glycerin.[43] About 20% to 27% of propylene glycol and glycerin-based liquid particles are inhaled.[345] A 2016 study found that 6% of nicotine, 8% of propylene glycol, and 16% of glycerin was breathed out by e-cigarette users.[346] The long-term effects of inhaled propylene glycol has not been studied,[147] and is unknown.[207] The effects of inhaled glycerin are unknown.[57] Being exposed to propylene glycol may cause irritation to the eyes and respiratory tract.[43] When propylene glycol is heated and aerosolized, it could turn into propylene oxide, which the International Agency for Research on Cancer states is possibly carcinogenic to humans.[43][246] Propylene glycol and glycerin have not been shown to be safe.[57] Some research states that propylene glycol emissions may cause respiratory irritation and raise the likelihood to develop asthma.[142] Long-term inhalation of propylene glycol indoors could increase risk to children to develop asthma.[171] To lessen the risks, most e-cigarettes companies began to use water and glycerin as replacement for propylene glycol.[142] The inhaled glycerin could cause lipoid pneumonia.[347] Propylene glycol and glycerin had increased the amount of hydrogen peroxide.[348] E-cigarettes vapors have been found to contain propylene glycol, glycerin, volatile organic compounds, and free radicals, which can impair lung health.[86]
Some e-cigarette products had acrolein identified in the aerosol.[72] It may be generated when glycerin is heated to higher temperatures.[72] Acrolein may induce irritation to the upper respiratory tract,[43] and harm the lining of the lungs.[80] Acrolein induces oxidative stress and inflammation, leading to a disruption in the function of the endothelial cell barrier in the lung.[348] Acrolein may lead to chronic obstructive pulmonary disease.[348] Acrolein levels were reduced by 60% in dual users and 80% for those that completely switched to e-cigarettes when compared to traditional cigarettes.[72] A 2017 review stated that "based on the average of 120 puffs/day reported in the literature, our calculated levels of acrolein emitted by e‐cigarette users per day were found to vary between 0.00792 and 8.94 ppm/day."[225] E-cigarettes vapor have been found to create oxidants and reactive oxygen species (OX/ROS).[77] OX/ROS could react with other substances in the e-cigarette vapor because they are highly reactive.[77] Although e-cigarettes have been found to contain OX/ROS at about 100 times less than in cigarette smoke, they probably induce meaningful biological effects.[77] A 2014 study showed that e-liquids from a specific manufacturer contained greater amounts of ethylene glycol than glycerin or propylene glycol, but ethylene glycol has not been permitted for use in products meant for human consumption.[220]
The toxicity of e-cigarettes and e-liquid can vary greatly, as there are differences in construction and materials in the delivery device, kind and origin of ingredients in the e-liquid, and the use or non-use of good manufacturing practices and quality control approaches.[314] If exposure of aerosols to propylene glycol and glycerin rises to levels that one would consider the exposure in association with a workplace setting, it would be sensible to investigate the health of exposed persons.[145] The short-term toxicity of e-cigarette use appears to be low, with the exception for some people with reactive airways.[79]
Ethanol
Different amounts of ethanol have been identified in e-liquids, even in instances when it is not disclosed as an ingredient.[349] There are flavoring chemicals that are sold in solvents.[350] For instance, vanilla extract is typically available in a liquid containing ethanol.[350] A 2017 study discovered the highest amounts of ethanol in testing various e-liquids were 7.7-fold greater than the restricted amount of 0.05% for pharmaceutical drugs.[349] Ethanol is commonly included as a solvent.[88] For example, a 2016 study found that 30 of 42 of e-liquid brands were made up of ethanol, which is linked to an unfavorable impact on psychomotor performance.[88] A 2016 study found vaping using an e-liquid containing 23% alcohol was linked to reduced performance on the Purdue Pegboard Test.[351] E-liquids containing alcohol produce detectable levels of alcohol metabolites in the urine.[352] The amount of ethanol inhaled by the e-cigarette user is unknown.[349] The short-term pharmacodynamics of breathing in alcohol e-cigarette vapor is not known.[351]
Flavoring

The essential propylene glycol and/or glycerin mixture may consist of natural or artificial substances to provide it flavor.[79] Health effects of e-cigarette flavorings are not entirely known.[353] There is very limited toxicological data on inhaling flavoring additives.[131] Flavorings can be a significant part of toxicants in the e-cigarette vapor.[218] Each flavor has a different chemical composition, and therefore, probably, a distinct composition of toxicant emissions.[218] The cytotoxicity of e-liquids varies,[78] and contamination with various chemicals have been detected in the liquid.[79] Some liquids were very toxic and others had little or no cytotoxicity.[78] The cytotoxicity is mostly due to the amount and number of flavors added.[78]
Since nicotine has a bitter taste, nicotine e-liquids contain chemicals to cover up the nicotine taste.[77] The liquids contain aromatic substances like tobacco, fruit, vanilla, caramel, and coffee.[79] Generally, these additives are imprecisely described, using terms such as "vegetable flavoring".[79] Although they are approved for human consumption there are no studies on the short-term or long-term effects of inhaling them.[79] The safety of inhaling flavors is mostly unknown,[354] and their safety has not been determined by the Flavor and Extract Manufacturers Association.[121] The majority of flavorings in e-liquids have not been investigated for toxicity by means of inhalation.[355] A 2017 review found "The Flavor and Extract Manufacturers Association (FEMA) of the USA, a trade association of flavor ingredient manufacturers which evaluates the safety of food flavorings, has identified 1037 flavoring agents as potential respiratory hazards due to possible volatility and respiratory irritant properties. Common e-cig flavoring agents on this list include, but are not limited to: diacetyl, acetoin, 2,3-pentanedione (buttery flavors), camphor and cyclohexanone (minty flavors), benzaldehyde (cherry or almond flavors), cinnamaldehyde (cinnamon flavor), cresol (leathery or medicinal flavor), butyraldehyde (chocolate flavor), and isoamyl acetate (banana flavor)."[131] A 2017 review stated, "the implication by manufacturers that flavor ingredients used in e-cigarettes and related devices (e.g. hookahs) are safe for inhalation because they have FEMA GRAS™ status for use in food has been stated to be 'false and misleading' by FEMA."[234]
The extensive and unregulated use of flavoring additives may pose health concerns.[131] Many flavors are irritants.[87] The limited data available on their flavoring agents suggest that the majority of flavorings could lead to significant health risks from long-term use, particularly the ones that are sweet.[356] In some cases e-liquids contain very large amounts of flavorings, which may cause irritation and inflammation on respiratory and cardiovascular systems.[242] A 2016 study of 30 e-cigarette products in the US market found that 13 were more than 1% flavor chemicals by weight, some of which were of potential toxicological concern (e.g., cause respiratory irritation).[357] Some flavors are regarded as toxic and a number of them resemble known carcinogens.[79] The cytotoxicity of some flavors such as strawberry seems to be greater than others.[358] A 2016 study of five flavors across six types of e-cigarettes found that flavors significantly affected the in vitro toxicity profile and the strawberry-flavored product was the most toxic.[357] Some artificial flavors are known to be cytotoxic.[79] Unflavored vapor is less cytotoxic than flavored vapor.[359] A 2012 study demonstrated that in embryonic and adult cellular models, some substances of the e-cigarette vapor such as flavoring not found in tobacco smoke were cytotoxic.[360] The caffeine exposures from vaping are approximately at amounts considerably less than in comparison with consuming caffeinated beverages.[361] There is very limited information available regarding the effects of breathing in caffeine.[361] The evidence is unclear that particular flavorings carry health risks, though there are indications that breathing in some may be a source of avoidable risks.[362]
Cinnamaldehyde has been described as a highly cytotoxic material in vitro in cinnamon-flavored refill liquids.[76] Cinnamaldehyde has also been detected in tobacco flavors, sweet flavors (e.g. caramel), and fruit flavors.[363] Cinnamaldehyde have been identified as cytotoxic at the amount of about 400 times less than those allowed for use by the US Environmental Protection Agency.[52] Compared to other flavors, coffee and cinnamon flavor are the most toxic.[364] An 18-year-old patient reported using a Juul device with mint flavored pods in the days leading to episodes of pneumothorax in January 2019.[365] In sampling multiple e-cigarette delivery systems, a 2019 study found Juul pods were the only product to demonstrate in vitro cytotoxicity from both nicotine and flavor chemical content, in particular ethyl maltol.[365] Pulegone, a chemical for menthol and mint flavors, is a carcinogen that induces pulmonary metaplasia.[366] There is limited information on the effects of inhaling menthol.[131] Preliminary toxicological data suggests that synthetic coolants (e.g., WS-23 and WS-3) inhaled from the e-cigarette vapors are high enough to inflict adverse effects and possibly high enough to inflict toxicological effects.[367]

At least 65 unique flavor chemicals in e-cigarette aerosols trigger toxicity in the circulatory system, skeletal system, respiratory tract, and skin, as of 2021.[368] Many flavoring additives likely cause respiratory effects not typically seen in cigarette smokers.[131] The evidence is sparse to directly associate inhalations of cinnamon with developing or aggravating asthma.[131] Some flavorings could cause lung inflammation.[369] Fruity, sweet, and traditional tobacco flavorings may result in lung toxicity.[234] Flavorings can harm lung cells by producing free radicals and inflammation.[246] Some e-liquids containing cinnamaldehyde stimulate TRPA1, which might induce effects on the lung.[77] In human lung fibroblasts, cinnamon roll flavoring resulted in a noticeable rise in the amount of inflammatory cytokine IL-8.[348] Chemical reactions may happen in e-liquids such as a reaction between aldehyde-containing flavors like vanillin and propylene glycol or glycerin.[350] This reaction happens at room temperature and creates new acetal substances which have a higher likelihood of causing irritation than the original substances they were created from.[350]
E-liquids contain possibly toxic aldehydes and reactive oxygen species (ROS).[77] Many flavors are known aldehydes, such as anisaldehyde, cinnamaldehyde, and isovaleraldehyde.[77] Saccharides in sweet e-liquid flavors break down and generate furans and aldehydes when vaporized.[370] The consequences of aldehyde-containing flavors on pulmonary surfaces are unknown.[77] A 2012 study found butterscotch flavor was highly toxic with one liquid and two others had a low toxicity.[162] A 2014 in vitro study showed that menthol flavors have a damaging effect on human periodontal ligament fibroblast growth.[345] Methanol had increased the amount of hydrogen peroxide.[348] A 2017 study found a variety of flavoring initiated inflammatory cytokines in lung cell cultures, of which acetoin and maltol were among the most strongest.[369] A 2014 in vitro study demonstrated that e-cigarette use of a "balsamic" flavor with no nicotine can activate the release of proinflammatory cytokine in lung epithelial cells and keratinocytes.[201] Some additives may be added to reduce the irritation on the pharynx.[57] The long-term toxicity is subject to the additives and contaminants in the e-liquid.[79] It is possible that flavors may worsen some of harmful effects in various cell types such as diminished cell viability, escalated rates of apoptosis, escalated DNA strand breaks, alterations in cell morphology and intensified inflammatory mediator production.[218] There is limited information available on the impact of flavors in the e-cigarette vapor on the DNA damage at the molecular scale.[317]
Certain flavorings contain diacetyl and acetyl propionyl which give a buttery taste.[91] Some sweet flavors containing diacetyl and acetyl propionyl include butter, chocolate, milk, or toffee.[364] Diacetyl occurs in a variety of e-cigarette flavorings such as caramel, butterscotch, watermelon, pina colada, and strawberry.[369] A 2016 Harvard study detected 39 of the 51 flavored e-cigarettes tested contained diacetyl.[371] The American Lung Association recommended in 2016 that the US FDA require that diacetyl and other unsafe chemicals be omitted from e-cigarettes.[371] Menthol flavorings could also contain diacetyl.[369] Diacetyl and acetyl propionyl are associated with bronchiolitis obliterans.[91] A 2018 PHE report stated that the e-cigarette flavorings containing diacetyl is not likely to present a considerable risk.[372] A 2015 review recommended for specific regulation of diacetyl and acetyl propionyl in e-liquid, which are safe when ingested but have been associated with respiratory harm when inhaled.[99] Being exposed to diacetyl produces morphological alterations in the liver according to animal studies.[216] Both diacetyl and acetyl-propionyl have been found in concentrations above those recommended by the US National Institute for Occupational Safety and Health.[91] Diacetyl is normally found at lower levels in e-cigarettes than in traditional cigarettes.[91]
2, 3-pentanedione, is a α-diketone that is chemically and structurally similar to diacetyl.[209] Although it has become a popular replacement for diacetyl, acute inhalation exposure to 2, 3-pentanedione has been shown to cause airway epithelial damage similar to diacetyl.[209] Some liquids use butyric acid instead of diacetyl and acetyl propionyl, but it could have negative health effects.[373] Respiratory toxicity resulting from flavoring agents primarily involving diacetyl and its alternatives raises concerns.[88] Concerns exist that the flavors and additives in e-cigarettes might lead to diseases, including popcorn lung.[190] The cardiovascular effects, including a vast range of flavorings and fragrances, is unknown.[374] Compared to other flavors, cherry contains a greater amount of benzaldehyde,[364] a main ingredient for a variety of fruit flavors.[369] Because benzaldehyde can irritate the eyes and mucous membranes of the respiratory tracts with workplace exposure, concerns have been expressed regarding the toxicity of flavored e-cigarette vapor.[375] The irritants butyl acetate, diethyl carbonate, benzoic acid, quinoline, bis(2-ethylhexyl) phthalate, and 2,6-dimethyl phenol were present as undeclared ingredients in the e-liquid.[173] The precise ingredients of e-cigarettes are not known.[376] A 2010 study found rimonabant when examining e-liquids.[377] This weight loss drug has been linked to seizures and suicide.[377] The same study also determined e-liquid can contain amino-tadalafil which is a component of Cialis, used for erectile dysfunction.[377] Users are at risk of encountering negative health outcomes from the small possibility of being exposed to pharmacologic compounds in some e-liquids.[377]
The Centers for Disease Control tested in 2015 36 e-cigarette products for 10 flavor compounds commonly used as additives in tobacco products.[209] Measurable levels of eucalyptol and pulegone were found in the menthol-flavored varieties for all manufacturers.[209] Menthol concentrations ranged from 3,700 to 12,000 μg/g in flavored e-liquids, levels similar to those found in the filler of traditional cigarettes.[209] Interestingly, menthol was found at low concentrations in 40% of the tobacco-flavored nonmenthol products tested.[209] Other flavor compounds found were camphor, methyl, salicylate, pulegone, cinnamaldehyde (CAD), and eugenol.[209] Tierney and colleagues in 2016 analyzed 30 e-cigarette products on the U.S. market and found 13 products contained more than 1% flavor chemicals by weight.[209] Among the chemicals identified were aldehydes (e.g., benzaldehyde and vanillin), which are categorized as primary irritants of the respiratory tract.[209] Tierney and colleagues also found that tobacco-flavored e-liquids were derived from confection-flavored chemicals (e.g., bubble gum and cotton candy flavoring) rather than tobacco extract.[209] In comparison to tobacco flavor, menthol created 330% higher levels of benzene and 120% higher levels of toluene.[118] Fruit flavor created 240% higher levels of benzene and 30% lower levels of toluene than tobacco flavor.[118] Various candy and fruit flavor e-liquids that are enticing to youth exhibit in cell culture cytotoxic or mutagenic effects.[236]
The available evidence suggests that many aldehydes flavoring compounds, including vanillin, ethyl vanillin (vanilla), and benzaldehyde (berry/fruit), react in liquids with propylene glycol and glycerin solvents to form chemical adducts called flavor aldehyde propylene glycol/glycerin acetals.[312] Assessing the effect of these chemical flavors and their corresponding acetals on bronchial and alveolar epithelial cells, a 2020 preliminary study observed that propylene glycol acetals diminished key parameters of cellular energy metabolic functions, including basal respiration, adenosine triphosphate production, and spare respiratory capacity.[312]
Flavoring enhancers
Flavoring enhancers are frequently used in e-liquids to improve flavor.[378] Flavoring enhancers used in e-liquid include monosodium glutamate, amino acids and hydrolyzed proteins such as inositol, leucine, and glutamic acid, ethyl pyrazine, caffeine, capsicum, ethylguaiacol, ethyl maltol, γ-Octalactone, isobutavan, malic acid, citric acid, sucralose, syringol, triacetin, vanillin, maltol, sucralose, and tartarazine.[378] Some of these substances such as monosodium glutamate can lead to allergic reactions.[378] The toxicological profiles of them are unknown, though It is believed that some of these flavoring additives can function as oxidative and inflammatory mediators and result in pro-fibrotic, pro-atherogenic, pro-audiogenic, and pro-diabetic reactions such as insulin resistance as well as neurological, developmental and reproductive conditions.[378] It is unknown whether these additives may be carcinogenic - particularly when heating at high voltages with flavors.[378]
Formaldehyde
The International Agency for Research on Cancer has categorized formaldehyde as a human carcinogen, and acetaldehyde is categorized as a possible carcinogen to humans.[80] Formaldehyde induces DNA damage and inhibits DNA repair.[379] Acetaldehyde generated crosslinking of DNA-protein which impede with DNA metabolic functions, including replication, repair, recombination, transcription and chromatin remodeling.[379] Aldehydes may cause harmful health effects; though, in the majority of cases, the amounts inhaled are less than with traditional cigarettes.[80] A 2016 study found that e-liquids without flavoring generated no aldehydes, which indicated that the flavors were causing the creation of aldehydes, according to a 2018 PHE report.[380] Many chemical compounds can inadvertently be produced from e-cigarettes, especially carbonyl compounds like formaldehyde, acetaldehyde, acrolein, and glyoxal by the chemical reaction of the e-liquid when the nichrome wire (heating element) is heated,[80] to high temperatures.[201] These compounds are frequently identified in e-cigarette aerosols.[80]
Potentially hazardous carbonyls have been identified in e-cigarette aerosols produced at temperatures above 200 °C.[131] The propylene glycol-containing liquids produced the most amounts of carbonyls in e-cigarette aerosols.[80] The levels of toxic chemicals in the e-cigarette vapor were found to be 1 to 2 orders of magnitude smaller than with cigarette smoke but greater than from a nicotine inhaler.[43] Nearly all e-cigarettes evaluated, toxic and irritation-causing carbonyls were identified.[201] Reports regarding the levels of toxic chemicals were inconsistent.[201] This includes a study showing that the levels of toxicants in e-cigarettes may be higher than with cigarette smoke.[201]
Battery output voltage influences the level of the carbonyl substances in the e-cigarette vapor.[80] Some newer e-cigarette models let users boost the amount of vapor and nicotine provided by modifying the battery output voltage.[80] E-cigarettes that were modified to boost the vapor production are more dangerous to use.[197] High-voltage e-cigarettes could subject users to large amounts of carbonyls.[80] E-cigarettes with higher voltages (5.0 V[78]) can emit carcinogens including formaldehyde at levels comparable to cigarette smoke,[324] while reduced voltages (3.0 V[90]) generate aerosol with levels of formaldehyde and acetaldehyde roughly 13 and 807-fold less than in cigarette smoke.[80] The average amount of formaldehyde in vapor from high-voltage devices is higher than the average amount of formaldehyde released from cigarettes.[166] "Dripping", where the liquid is dripped directly onto the atomizer, can create carbonyls including formaldehyde.[381] Formaldehyde, acetaldehyde, and acrolein have been detected at concentrations above those recommended for a brief period of exposure by the US National Institute for Occupational Safety and Health.[204]
Controversy exists regarding the specific amount of formaldehyde expected to be breathed in by the user.[218] Studies have established that free aldehydes are produced during regular use conditions, although formaldehyde hemiacetal production increases dramatically with battery output.[49] Initial studies reported that formaldehyde was formed during the vaping process under high heat conditions.[37] Although some of the more recent e-cigarette devices limit temperature in an attempt to minimize this, multiple reports have documented the formation of acetaldehyde, acrolein, diacetyl, and formaldehyde under a wide range of conditions.[37] A 2018 study "shows that carbonyl formation can be catalyzed by e-cigarette metal heating coil materials, enabling carbonyl formation at coil temperatures far below those associated with the dry puff phenomenon."[118] A 2018 study regarding "coil temperature and wicking variables also resulted in the conclusion that concerning levels of formaldehyde in frequent e-cigarette users can be produced at relatively low power levels, and within the range of operating temperatures observed by human subjects to afford sensorially pleasant conditions, i.e., not under dry-puff conditions."[118]
Later-generation and "hotter" e-cigarettes may generate equal or higher levels of formaldehyde compared to smoking.[81] A 2015 study analyzing 10 puffs found that vaping at a high voltage (5.0 V) generates formaldehyde in e-cigarette vapor; they inferred from the finding that the user vaping at high voltage with 3 ml of e-liquid daily would inhale 14.4±3.3 mg of formaldehyde daily in formaldehyde-emitting chemicals.[78] This was estimated to be a lifetime cancer risk of 5 to 15 times greater than compared with long-term smoking.[78] A 2015 study using a third-generation device, very low levels of formaldehyde were produced on lower power, although, when adjusted to a maximum power setting, levels were greater than with cigarette smoke.[359] Running at a higher power (temperature) not only increases nicotine delivery, but also increases the amount of formaldehyde and other aldehydes that are naturally produced by heating up propylene glycol or glycerin and other toxicants produced in the e-cigarette aerosol.[158] It has been suggested that e-cigarette users tend to stay clear of the harsh taste that is related to the creation of aldehydes during excessive heating or dry puffing (also known as a "dry hit"[382]).[77] However, e-cigarette users may learn to overcome the unpleasant taste due to elevated aldehyde formation, when the nicotine craving is high enough.[77]
Nicotine


Pregnant women, breastfeeding mothers, and the elderly are more sensitive to nicotine than other individuals.[354] There are safety issues with the nicotine exposure from e-cigarette use, which may cause addiction and other adverse effects.[90] Nicotine is regarded as a potentially lethal poison.[73] Concerns exist that vaping can be harmful by exposing users to toxic levels of nicotine.[73] At low amounts, it has a mild analgesic effect.[354] At sufficiently high doses, nicotine may result in nausea, vomiting, diarrhea, salivation, bradyarrhythmia, and possibly seizures and hypoventilation.[385] High doses can induce deleterious effects on the growth of osteoblasts.[386] Higher-doses leads to loss of nicotinic receptor specificity and induces cholinergic toxicity.[269] The highest-doses can lead to coma.[269] However, at the low amount of nicotine provided by e-cigarettes fatal overdose from use is unlikely; in contrast, the potent amount of nicotine in e-cigarettes liquids may be toxic if it is accidentally ingested or absorbed via the skin.[73] The health effects of nicotine in infants and children are unclear.[385]
E-cigarettes provide nicotine to the blood quicker than nicotine inhalers.[144] The levels were above that of nicotine replacement product users.[73] E-cigarettes seem to have a pharmacokinetic nicotine profile closer to nicotine replacement products than with traditional cigarettes.[387] How efficiently different e-cigarettes give nicotine is unclear.[73] Serum cotinine levels are comparable to that of traditional cigarettes,[388] but are inharmonious and rely upon the user and the device.[44] Blood nicotine levels raised more gradually and took more time to get to peak concentration with e-cigarettes than with traditional cigarettes.[389] Vaping was found to have comparable levels of nicotine urinary metabolites to those who were tobacco and smokeless tobacco product users.[234] Though, the oxidative nicotine metabolites were less in those who were vaping.[234] Evidence indicates that some vaping products may deliver the same amount of nicotine as traditional cigarettes.[232] There is fair evidence that chance and degree of dependence are less for e-cigarettes than traditional cigarettes, according to a 2018 National Academies of Sciences, Engineering, and Medicine report.[390] It not clear the level of addictiveness of e-cigarettes, compared with traditional cigarettes, according to a 2018 PHE report.[391] The report also stated "nicotine addictiveness depends on a number of factors including presence of other chemicals, speed of delivery, pH, rate of absorption, the dose, and other aspects of the nicotine delivery system, environment and behaviour."[392] A 2019 study on highly educated young people found that a higher level of nicotine dependence was observed when using e-cigarettes compared with tobacco smoking.[393] In regards to the diversity of devices available, there is limited information available on the vulnerability of nicotine dependency.[394] Users vaping without using nicotine exhibited symptoms of dependence, according to a 2015 study.[395] E-cigarette packages and advertisements require health warnings under US law, stating "WARNING: This product contains nicotine. Nicotine is an addictive chemical."[232]
A 2020 study of "chronic electronic cigarette users, nicotine-containing electronic cigarettes induced acute elevations in heart rate, systolic blood pressure, diastolic blood pressure, and mean blood pressure; these effects were not replicated by a nicotine inhaler or a nicotine-free electronic cigarette, suggesting an interaction between nicotine and other tobacco product-associated environmental inhalants."[396]
First-generation nicotine-containing devices
E-cigarettes resembling cigarettes typically produce much less blood nicotine levels.[353] When compared to traditional cigarettes older devices usually delivered low amounts of nicotine.[73] E-cigarette use can be associated with a substantial dispersion of nicotine, thus generating a plasma nicotine concentration which can be comparable to that of traditional cigarettes.[397] This is due to the minute nicotine particles in the e-cigarette vapor, which permit quick delivery into the bloodstream.[397] The nicotine delivered from e-cigarettes enters the body slower than traditional cigarettes.[96] Studies suggest that inexperienced users obtain moderate amounts of nicotine from e-cigarettes.[398] Concerns were raised over inconsistent amounts of nicotine delivered when drawing on the device.[399]
Later-generation nicotine-containing devices
Tank or adjustable e-cigarettes can raise nicotine levels as high as traditional cigarettes.[353] Later-generation e-cigarettes give nicotine more effectively than first-generation e-cigarettes.[76] Later-generation models with concentrated nicotine liquids may deliver nicotine at levels similar to traditional cigarettes.[73] Some e-cigarette tank devices with stronger batteries heat solutions to greater temperatures, which may raise levels of nicotine in the blood similar to those of traditional cigarettes.[162] Research suggests that experienced e-cigarettes users are able to get as much nicotine from e-cigarettes as traditional cigarettes.[73] Later-generation e-cigarettes containing sufficient nicotine elevate heart rate comparable to traditional cigarettes.[374] Later-generation devices delivery 35% to 72% more nicotine than compared with first‐generation devices.[225] Second-generation e-cigarettes raised the heart rate and blood pressure similar to traditional cigarettes.[400] As there are design changes, later-generation devices may provide nicotine similar to traditional cigarettes with a highly concentrated amount potential straight to the brain.[356] Such devices may largely reshape the effects on cardiac safety, misuse, and addiction.[356] There is not much research on fourth-generation devices.[157] Pod mods may provide nicotine at the same or higher concentration than traditional cigarettes which increases the possibility of addiction.[137] Minors using pod mods are more likely than traditional e-cigarette users to exhibit higher nicotine dependence symptoms.[401]
Intensity of use
Vaping requires more forceful sucking than smoking, and this action is unclear on increased uptake of harmful substances and the user's health.[397] E-cigarette use has an almost immediate effect on airway resistance, which decreases the ability to draw air in.[24] Sucking more forcefully may be harmful to the e-cigarette user.[356] A "cloud-chasing" competition or a presentation of a device might trigger an extra "performing" effort involving higher puff volume.[402] The health impacts of intensive vaping is unknown.[81] A range of possibly hazardous chemicals may be exhaled, including nicotine, while repeatedly puffing on a device.[397]
Some evidence indicates that vaping products that supply a lower level of nicotine may be more risky to use.[179] This is due to the devices that offer a low amount of nicotine require to be puffed with greater intensity to give users the amount of nicotine they desire, and greater intensive puffing results in, more breathing in of possible toxicants.[179] When compensating for reduced nicotine by puffing more intensely, e-cigarette users are exposed to higher concentrations of carbonyls.[403] Growing evidence indicates that e-cigarette devices that deliver greater nicotine concentrations may reduce the number of puffs needed to reach adequate nicotine uptake in contrast to lower nicotine concentration ones.[404] By vaping longer, lower nicotine concentration devices can expose users to higher levels of hazardous emissions, notably carbonyls.[404] Furthermore, greater nicotine concentration devices may also possibly exacerbate nicotine dependency and other health issues.[404] Commercial e-cigarette products are continuing to evolve across time which may lead to increased intensity of use, for instance based on increasing nicotine levels, pH modifications, and potentially other design features.[40]
Nicotine concerns

How do e-cigarettes affect the brain?[406] The nicotine in e-liquids readily absorbs into the bloodstream when a person uses an e-cigarette.[406] Upon entering the blood, nicotine stimulates the adrenal glands to release the hormone epinephrine (adrenaline).[406] Epinephrine stimulates the central nervous system and increases blood pressure, breathing, and heart rate.[406] As with most addictive substances, nicotine increases levels of a chemical messenger in the brain called dopamine, which affects parts of the brain that control reward (pleasure from natural behaviors such as eating).[406] These feelings motivate some people to use nicotine again and again, despite possible risks to their health and well-being.[406]
The health effects of long-term nicotine use is unknown.[207] It may be decades before the long-term health effects of nicotine vapor inhalation is known.[407] It is not recommended for non-smokers.[52] Public health authorities do not recommend nicotine use for non-smokers.[85] The pureness of the nicotine differs by grade and producer.[408] The impurities associated with nicotine are not as toxic as nicotine.[408] The health effects of vaping tobacco alkaloids that stem from nicotine impurities in e-liquids is not known.[408] Nicotine affects practically every cell in the body.[354] The complex effects of nicotine are not entirely understood.[82] It poses several health risks.[84] Short-term nicotine use excites the autonomic ganglia nerves and autonomic nerves, but chronic use seems to induce negative effects on endothelial cells.[409] Nicotine may have a profound impact on sleep.[410] The effects on sleep vary after being intoxicated, during withdrawal, and from long-term use.[410] Nicotine may result in arousal and wakefulness, mainly via incitement in the basal forebrain.[411] Nicotine withdrawal, after abstaining from nicotine use in non-smokers, was linked with longer overall length of sleep and REM rebound.[410] A 2016 review states that "Although smokers say they smoke to control stress, studies show a significant increase in cortisol concentrations in daily smokers compared with occasional smokers or nonsmokers. These findings suggest that, despite the subjective effects, smoking may actually worsen the negative emotional states. The effects of nicotine on the sleep-wake cycle through nicotine receptors may have a functional significance. Nicotine receptor stimulation promotes wake time and reduces both total sleep time and rapid eye movement sleep."[412]
Nicotine can weaken antibacterial defenses and modify macrophage activation.[174] Nicotine can cause tremors,[246] high blood pressure, abnormal heart rhythms,[413] increased serum cholesterol levels,[82] and lower coronary blood flow.[374] Nicotine constricts blood vessels.[126] This includes coronary blood vessels and those in the skin.[414] However, blood vessels in the skeletal muscle dilate as a result of nicotine.[414] It can also cause nausea, sweating, and diarrhea.[356] In reaction to nitric oxide, it hinders endothelial-dependent widening of blood vessels.[82] It is associated with stroke, peripheral vascular disease, delayed wound healing, peptic ulcer disease, and esophageal reflux.[166] Vapers that get a higher amount of blood nicotine are probably correlated with increased heart rates.[174] Acute administration of nicotine causes a variety of well-characterized, dose- and route-dependent effects in adults, including cardiovascular effects, such as greater cardiac output, leading to an increase in myocardial oxygen demand.[209] Nicotine is correlated with lung inflammation in adults, which may be as a result of it chemotactic effects.[157] Nicotine may have adverse effects on lipids,[415] cause insulin resistance,[162] and may cause pro-inflammatory effects that could impact beta cell function.[416] Nicotine lowers activity of free radical scavenging enzymes, resulting in more production of hydroxyl free radicals.[416] Nicotine impairs glucose homeostasis, indicating a major role in the development of type 2 diabetes.[416] Osseointegration is a pertinent part of the survival of implants.[417] Nicotine considerably impedes the regenerative capability of mesenchymal stem cells.[418] This includes impeding their proliferation, migration, and differentiation.[418] Nicotine has been correlated with vasoconstriction and a weakened ability to heal at the cellular level.[417] Thus, it apparently compromises implant osseointegration.[417] Nicotine lowers estrogen levels and has been associated with early menopause in women.[413] Nicotine is negatively associated with total sperm motility.[358]
A 2016 review found "Evidence from experimental animal models clearly demonstrate nicotine's ability to enhance existing tissue injury and diseases such as cancer, cardiovascular disease, stroke, pancreatitis, peptic ulcer, renal injury and developmental (e.g. pulmonary, reproductive and central nervous system) abnormalities."[419] The consequence of nicotine use in autoimmunity has been conflicting.[420] Nicotine could have cancer-promoting properties, therefore long-term use may not be harmless.[75] Nicotine may result in neuroplasticity variations in the brain.[268] Nicotine has been demonstrated to alter the amounts of brain-derived neurotrophic factor in humans.[421] Nicotine could make cancer therapies less effective.[62] Based on in vitro and in vivo effects of nicotine, patients should be advised not to use nicotine products during cancer treatment unless it is temporarily needed to stop tobacco smoking.[322] Nicotine can suppress appetite.[56] Nicotine users will probably gain weight after using less nicotine.[422] A long-term risk from vaping a base containing nicotine is nicotine dependence.[236]
Youth nicotine concerns
Children are more sensitive to nicotine than adults.[354] The use of products containing nicotine in any form among youth, including in e-cigarettes, is unsafe.[209] Nicotine has more significant and durable damaging effects on adolescent brains compared to adult brains, the former causing more harmful effects.[209] Animal research offers strong evidence that the limbic system is particularly vulnerable to the long lasting effects of nicotine.[424] In youth, nicotine may result in cognitive impairment[424] as well as the chance of nicotine addiction for life.[413] The adolescent's developing brain is especially sensitive to the harmful effects of nicotine.[425] A short period of regular or occasional nicotine exposure in adolescence exerts long-term neurobehavioral damage.[425] Risks of exposing the developing brain to nicotine include mood disorders and permanent lowering of impulse control.[288] The rise in vaping is of great concern because the parts encompassing in greater cognitive activities including the prefrontal cortex of the brain continues to develop into the 20s[385] Nicotine exposure during brain development may hamper growth of neurons and brain circuits, effecting brain architecture, chemistry, and neurobehavioral activity.[385]
Nicotine changes the way synapses are formed, which can harm the parts of the brain that control attention and learning.[288] Preclinical studies indicate that teens being exposed to nicotine interferes with the structural development of the brain, inducing lasting alterations in the brain's neural circuits.[274] Each e-cigarette brand differs in the exact amount of ingredients and nicotine in each product.[274] Therefore, little is known regarding the health consequences of each brand to the growing brains of youth.[274] In August 2014, the American Heart Association noted that "e-cigarettes could fuel and promote nicotine addiction, especially in children."[162] Whether there are subgroups of adolescents who are at greater risk of developing a nicotine dependence from vaping is not known.[236] A 2014 policy statement by the UK's Faculty of Public Health has stated, "A key concern for everyone in public health is that children and young people are being targeted by mass advertising of e-cigarettes. There is a danger that e-cigarettes will lead to young people and non-smokers becoming addicted to nicotine and smoking. Evidence from the US backs up this concern."[426] Long-term studies on the safety of nicotine-only exposure (e.g., as with using e-cigarettes rather than smoking traditional cigarettes) among youth have not been conducted.[209]
In 2015 the psychological and behavioral effects of e-cigarettes were studied using whole-body exposure to e-cigarette vapor, followed by a series of biochemical and behavioral studies.[221] The results showed that nicotine-containing e-cigarette vapor induces addiction-related neurochemical, physiological and behavioral changes.[221] A 2015 study on the offspring of the pregnant mice, which were exposed to nicotine-containing e-cigarette liquid, showed significant behavioral alterations.[221] This indicated that exposure to e-cigarette components in a susceptible time period of brain development could induce persistent behavioral changes.[221] As indicated in the limited research from animal studies, there is the potential for induced changes in neurocognitive growth among children who have been subjected to e-cigarette vapors consisting of nicotine.[427] The US FDA stated in 2019 that some people who use e-cigarettes have experienced seizures, with most reports involving youth or young adult users.[253]

Metals
There is limited evidence on the long-term exposure of metals.[52] Exposure to the levels and kinds of metals found in the aerosol relies upon the material and other manufacturing designs of the heating element.[162] E-cigarettes contain some contamination with small amounts of metals in the emissions.[52] The device itself could contribute to the toxicity from the small amounts of silicate and heavy metals found in the liquid and vapor,[381] because they have metal parts that come in contact with the e-liquid.[52]
Numerous studies have shown that e-liquids in contact with heating coils like Kanthal or nichrome facilitate leaching of metals/metalloids into the liquid present in the tank or cartomizer.[200] A 2019 study showed that metals were used in various device components, such as thick wires, wicks, sheaths, and joints.[200] These device components may also transfer metals/metalloids into the e-liquid because the presence of brass clamps and copper wires with silver coatings have been associated with higher zinc, copper, silver, and aluminum in the aerosol.[200] Furthermore, the presence of soldered joints of poor quality or with signs of fraying were associated with higher tin levels, emphasizing that poor manufacturing techniques make a notable contribution to potential metal impurities that may reach the user.[200] The e-cigarette user’s vaping regimen, which includes modifications in voltage, resistance, temperature, and puff duration, may also play a role in the degradation of the heating coils and other metal elements, and in turn modify the aerosol composition and degree of metal/metalloid exposure.[200] According to a 2018 PHE report, metals emissions no matter how small, are not needed.[362] They further stated, "EC [e-cigarettes] that generate minimal metal emissions should become an industry standard."[346]
Low levels of possibly harmful chromium, lead, and nickel metals have been found in the emissions.[162] Chromium and nickel nanoparticles have also been found.[43] Copper nanoparticles can induce mitochondrial and DNA injury in lung fibroblasts.[429] DNA repair can be impeded by titanium dioxide nanoparticles from the e-cigarette vapor.[125] This was demonstrated that the titanium dioxide nanoparticles induced single-strand breaks and produced oxidative stress in the DNA of A549 cells.[125] The risk of inhaling nanoparticles is an area of concern.[270] The toxicity of nanoparticles is unknown.[430] Nanoparticles can enter the brain and are associated with developmental neurotoxicity.[210] Metals including nickel, cadmium, lead, and silicate can found in the e-cigarette aerosols, and are thought to be carcinogenic, nephrotoxic, neurotoxic, and hemotoxic.[216] Heavy metals are correlated with serious health issues.[53] Inhaling lead can induce serious neurologic injury, notably to the growing brains of children.[53] No specific research is available on the consequences of vaping-associated metals on the brain.[210]
The presence of metals and metalloids (e.g., arsenic, chromium, lead, nickel) in e-cigarette aerosols is a major concern, given their serious health effects, including cancer, cardiovascular disease, renal damage, and neurotoxicity.[200] Metals may adversely affect the nervous system.[244] Metals found in the e-cigarette vapor may induce cell damage and initiate inflammatory cytokine such as in human lung fibroblasts.[369] A 2017 review found "E-cigarette aerosols and copper nanoparticles induced mitochondrial ROS production, mitochondrial stress (reduced stability of OxPhos electron transport chain (ETC) complex IV subunit) and DNA fragmentation in lung fibroblasts."[348] A 2013 review found metallic and nanoparticles are associated with respiratory distress and disease.[431] A 2014 review found considerable amounts of tin, metals, and silicate particles that came from various components of the e-cigarette were released into the aerosol, which result in exposure that could be higher than with cigarette smoke.[201] A 2013 study found metal particles in the aerosol were at levels 10-50 times less than permitted in inhalation medicines.[72] A 2014 review suggested that there is no evidence of contamination of the aerosol with metals that justifies a health concern.[145] Cadmium that have been found in the e-cigarette vapor is linked to low sperm density.[358]
Neurotoxicity of e-cigarette aerosols diagram
Potential neurotoxicity of e-cigarette aerosols
|
Comparison of levels of toxicants in e-cigarette aerosol
| Toxicant | Range of content in nicotine inhaler mist (15 puffs∗) | Content in aerosol from 12 e-cigarettes (15 puffs∗) | Content in traditional cigarette micrograms (μg) in smoke from one cigarette |
|---|---|---|---|
| Formaldehyde (μg) | 0.2 | 0.2-5.61 | 1.6-52 |
| Acetaldehyde (μg) | 0.11 | 0.11-1.36 | 52-140 |
| Acrolein (μg) | ND | 0.07-4.19 | 2.4-62 |
| o-Methylbenzaldehyde (μg) | 0.07 | 0.13-0.71 | — |
| Toluene (μg) | ND | ND-0.63 | 8.3-70 |
| p- and m-Xylene (μg) | ND | ND-0.2 | — |
| NNN (ng) | ND | ND-0.00043 | 0.0005-0.19 |
| Cadmium (ng) | 0.003 | ND-0.022 | — |
| Nickel (ng) | 0.019 | 0.011-0.029 | — |
| Lead (ng) | 0.004 | 0.003-0.057 | — |
Abbreviations: μg, microgram; ng, nanogram; ND, not detected.[78]
∗Fifteen puffs were chosen to estimate the nicotine delivery of one traditional cigarette.[78]
Summary of ethical concerns
| Ethical considerations[207] | Supporting arguments[207] | Opposing arguments[207] |
|---|---|---|
| Tobacco harm reduction[207] | ||
| Potential for smoking cessation[207] | E-cigarettes may be as effective as the nicotine patch.[207] | Inconclusive evidence of efficacy for smoking cessation.[207] |
| Potential for smoking reduction[207] | Demonstrated in multiple studies.[207] | Unlikely that cigarette reduction results in significant health benefits.[207] |
| Product safety[207] | ||
| Potential for long-term adverse effects[207] | Unknown impact of long-term propylene glycol inhalation.[207] | There were no publicized serious adverse events in 2016.[207] |
| Propylene glycol inhalation causes short-term respiratory irritation.[207] | ||
| Autonomy to use a product of unknown risk[207] | Ethical imperative given informed consent.[207] | Public health concerns trump individual rights.[207] |
| Use among non-smokers[207] | ||
| Potential to lead to nicotine addiction[207] | Perceived harmlessness may lead never smokers to initiate e-cigarettes.[207] | No evidence for increased nicotine addiction to cause net public health harms.[207] |
| Potential gateway effect[207] | Nicotine acts as a priming agent for the brain.[207] | Unclear implications for transitioning to tobacco cigarettes.[207] |
| Use among youth[207] | ||
| Potential to lead to nicotine addiction[207] | Minors require protection.[207] | No evidence of increased nicotine addiction causing net public health harms.[207] |
| E-liquid flavorings are attractive to youth.[207] | ||
| Potential gateway effect[207] | Nicotine is a priming agent for the brain.[207] | Unclear implications for transitioning to tobacco cigarettes.[207] |
| Nicotine poisoning among children[207] | Increased calls to poison control centers.[207] | None.[207] |
| E-liquid flavors are appealing to youth.[207] | ||
| Use in public places[207] | ||
| Potential for passive vaping[207] | Stem cell cytotoxicity.[207] | Limited evidence that passive vaping poses significant health concerns.[207] |
| Aerosolized nicotine emissions.[207] | ||
| Renormalized smoking culture[207] | ||
| Potential to subvert decades of anti-smoking efforts[207] | Increased acceptability of smoke-like vapor and smoking behavior.[207] | No evidence that e-cigarettes would be conflated with tobacco cigarettes.[207] |
| Market ownership[207] | ||
| Unethical collaboration with the tobacco industry[207] | Public health endorsement of e-cigarettes increases tobacco company market share.[207] | Possible necessity to collaborate with the tobacco industry to achieve public health gains.[207] |
Pathogens
Microbial toxins
The existing research pertaining to the microbiomes of e-liquids and cartridges are sparse.[432] A 2019 study found popular US vape liquids were contaminated with B-D-glucan and endotoxin.[433] Asthma and hypersensitivity pneumonitis are connected with these two microbial toxins.[433] B-D-glucans and endotoxin may induce respiratory discomfort, but studies have not been conducted on the long-term effects at the levels detected in vape liquids.[106]
Virulence
E-cigarette exposure can enhance the virulence of certain pathogens.[434] This strengthens their potential to stay alive in the host.[434] Differing bacterial strains became more destructive in a larval infection model after exposure to e-cigarette vapor.[434] Methicillin-resistant Staphylococcus aureus colonized in e-cigarette vapor extract were more damaging in mice, and had an increased ability to create biofilms, permeate and occupy within epithelial cells, and withstand the antimicrobial LL-37.[434]
E-cigarette vapor rapidly augment biofilm formation on the polystyrene surface by various Gram-positive and Gram-negative pathogens in a dose- and bacterial-strain-dependent manner.[435] Reactive oxygen species and nicotine are the main chemical drivers of e-cigarette vapor-dependent biofilm augmentation.[435] Exposure to e-cigarette vapor induces adherence of Staphylococcus aureus and Porphyromonas gingivalis to host cells and proteins while the adherence of Streptococcus pneumoniae or Pseudomonas aeruginosa is unaffected by e-cigarette vapor exposure.[435]
The bioactive chemicals in e-cigarette vapor may affect pathogenic bacteria in the nasopharyngeal microflora, which may have implications on the pathophysiology of respiratory infections in e-cigarette users.[435] Research shows that the e-cigarette vapor-mediated alterations in bacterial virulence were dependent on the length of exposure and the strain of pathogen under examination and that reactive oxygen species and nicotine were the primary chemical drivers of e-cigarette vapor-mediated alterations in the pathogen virulence.[435] Exposure to e-cigarette vapor induces pleiotropic changes affecting the physiology of the host and the pathogens known to asymptomatically colonize the respiratory tract and the mouth.[435]
Effects on breathing and lung function
Respiratory effects

When vaping, hundreds to thousands of chemicals are inhaled into the lungs.[433] The risks to the lungs are not fully understood,[77] and concern exists regarding the negative effects on lung function.[437] The long-term effects on lung function is unknown.[44] There is limited evidence on the long-term health effects to the lungs.[81] The long-term effect from vaping a base containing nicotine on lung tissue is unknown.[438] Limited evidence suggests that e-cigarettes produce less short-term effects on lung function than with traditional cigarettes.[44] Many ingredients used in e-liquids have not been examined in the lung.[77] E-cigarettes increase the risk of developing asthma and chronic obstructive pulmonary disease.[439] Vaping may induce acute lung disease[81] and increase the risk of developing lung disease.[440] Vaping might cause sub-acute bronchial toxicity.[174] Little is known about the short- and long-term effects of e-cigarettes on the respiratory microbiota and their impact on the innate immune response.[436]
E-cigarette use can have deleterious effects on lung lipid metabolism regardless of nicotine content.[441] Lipid-laden macrophages, discovered in bronchoalveolar lavage fluid from e-cigarette users, suggest users are at risk for lipid-mediated lung injury and interfered pathogen clearance via macrophages.[352] The lipid concentrations may be related to aerosolization of propylene glycol and glycerin solvents in e-liquid.[352] Exposure to inhaled nicotine-containing e-cigarette fluids triggered effects normally associated with the development of a chronic obstructive lung disease-like tissue damage in a nicotine-dependent manner.[221] Preclinical research indicate that vaping escalates the virulence of drug resistant microorganisms and diminishes the capacity of lung cells to eliminate bacteria.[442] E-cigarettes have been correlated with pleural effusions.[429] A 2015 study found that e-cigarette vapors can induce oxidative stress in lung endothelial cells.[242] Constant lung inflammation as a result of the e-cigarette vapor could result in lung pathogenesis and induce serious diseases, including chronic obstructive pulmonary disease and fibrosis.[121] There is strong evidence that e-cigarette vapors can result in acute endothelial cell injury, but the long-term effects regarding this matter on being exposed over a prolonged period of time to e-cigarette vapor is uncertain.[443] A 2017 review found "Exposure to nicotine that was specifically generated by the use of e-cigarettes, was shown to promote oxidative stress and impairment of autophagy, which in turn serves as a potential mechanism leading to development of chronic obstructive pulmonary disease."[348] A 2014 case report observed the correlation between sub-acute bronchiolitis and vaping.[81] After quitting vaping the symptoms improved.[81] Vaping causes bronchospasm.[225] Adolescents who vaped had a higher frequency of chronic bronchitis symptoms.[369]
The long-term effects regarding respiratory flow resistance are unknown.[222] The available evidence indicates that e-cigarettes may result in respiratory effects that are like as well as unlike that of traditional cigarettes.[131] E-cigarettes, particularly the ones containing nicotine, decrease lung function, but to a considerable lower extent than with traditional cigarettes.[64] E-cigarette use lowers oxygen saturation.[444] E-cigarettes could harm the respiratory system.[79] Vaping induces irritation of the upper and lower respiratory system.[166] The immediate effects of e-cigarettes after 5 minutes of use on pulmonary function resulted in considerable increases in resistance to lung airflow.[76] Vaping induces fundamental changes to the airway epithelial proteome and these changes, such as an altered look of the airways, are unique from what has been observed in smokers.[445] A 2013 review found an instant increase in airway resistance after using a single e-cigarette.[79] Higher levels of exhaled nitric oxide were found among test subjects in a 2014 study who vaped with a base of nicotine which was associated with lung inflammation.[446] Any reported harmful effects to cardiovascular and respiratory functions after short-term use of e-cigarettes were appreciably milder in comparison to cigarette smoke.[52] When used in the short-term, an e-cigarette resulted in a rise of respiratory resistance comparatively to traditional cigarettes.[222] E-cigarette use could result in respiratory diseases among youth.[447] Evidence from animal studies indicate that children or adolescents exposed to second-hand vapor containing nicotine may impede their lung development.[259]
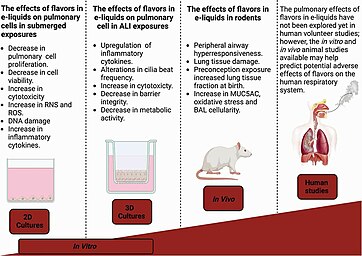
Data suggest that e-cigarette users produce significantly more sputum than smokers and show increased markers of inflammation in their airways.[449] As airway inflammation and mucus hypersecretion are central features underlying asthma pathology, asthmatics might be at increased risk for e-cigarette-induced health effects.[449] Adolescents with asthma who vape could have greater odds of having a higher number of respiratory symptoms and aggravations in contrast to their peers who do not vape.[450] Adolescents and children with other respiratory ailments who vape may be at greater chance for aggravating of respiratory symptoms.[450] A 2018 PHE report found "There have been some studies with adolescents suggesting respiratory symptoms among EC experimenters. However, small scale or uncontrolled switching studies from smoking to vaping have demonstrated some respiratory improvements."[451]
Comparable to a traditional cigarette, e-cigarette particles are tiny enough to enter the alveoli, enabling nicotine absorption.[76] These particles are also tiny enough to go deep in the lungs and enter into the systemic circulation.[43] Research indicates that e‐cigarette vapor containing particulate matter with a diameter of 2.5 μm, just from one puff, enters the systemic circulation via the cardiopulmonary system, leading to a large amount being deposited in the respiratory tract.[225] Local pulmonary toxicity may occur because metal nanoparticles can deposit in the lung's alveolar sacs.[43] E-cigarettes companies state that the particulates produced by an e-cigarette are too tiny to be deposited in the alveoli.[144] Tinier particles deposit more nicotine in the alveoli.[174]
Different devices generate different particle sizes and cause different depositions in the respiratory tract, even from the same nicotine liquid.[324] The aerosol production of e-cigarettes during vaping decreases, which requires a more forceful suction to create a similar volume of aerosol.[172] A more forceful suction could affect the deposition of substances into the lungs.[172] Compared to cigarette smoke, e-cigarettes produce on average smaller size particles, and the health effects of these smaller size particles is unclear.[454] Reports in the literature have shown respiratory and cardiovascular effects by these smaller size particles, suggesting a possible health concern.[455] Vaping is potentially harmful, especially to the critically ill, such as people with oncologic, lung, or cardiac diseases.[166] A 2019 case study of hard-metal pneumoconiosis was published in the European Respiratory Journal.[456] Researchers tested the patient's e-cigarette, which was used with cannabis.[456] Cobalt was found in the vapor, including other toxic metals-nickel, aluminum, manganese, lead, and chromium.[456] Metal-induced toxicity in the lung can result in long-term, if not, permanent scarring of the lungs.[456]
As with cardiovascular disease, evidence consistently indicates that exposure to e-cigarette aerosol has adverse effects on lungs and pulmonary function.[158] Repeated exposure to acrolein, which is produced by heating the propylene glycol and glycerin in e-liquids, causes chronic pulmonary inflammation, reduction of host defense, neutrophil inflammation, mucus hypersecretion, and protease-mediated lung tissue damage, which are linked to the development of chronic obstructive pulmonary disease.[158] E-cigarette aerosol also exposes users to highly oxidizing free radicals.[158] Animal studies have also shown that e-cigarettes increase pulmonary inflammation and oxidative stress while inhibiting the immune system.[158]
Consistent with these experimental results, people who used e-cigarettes experienced decreased expression of immune-related genes in their nasal cavities, with more genes suppressed than among cigarette smokers, indicating immune suppression in the nasal mucosa.[158] E-cigarette use upregulates expression of platelet-activating factor receptor (PAFR) in users' nasal epithelial cells; PAFR is an important molecule involved in the ability of S.pneumoniae, the leading cause of bacterial pneumonia, to attach to cells it infects (adherence).[158] In light of the immunosuppressive effects observed in nasal mucosa, there is concern that e-cigarette use will predispose users toward more severe respiratory infections, as has been demonstrated in mouse studies.[158]
Vaping is reportedly tied to a range of lung injuries which include hypersensitivity pneumonitis, diffuse alveolar hemorrhage, acute eosinophilic pneumonia, diffuse alveolar damage, organizing pneumonia, lipoid pneumonia, and giant cell interstitial pneumonia.[457]
Vaping cannabinoid plants may lead to lung injury similar to that of smoking tobacco.[458] Vaping poses unique risks, as contaminants and additives to the vape medium may cause significant lung damage apart from cannabinoids.[458]
Respiratory effects in youth and young adults
As of 2021, little information is available regarding the effect of e-cigarette exposure on children's respiratory health.[459] Available data on the respiratory effects among young people are mainly self-reported and may be subjected to recall bias, as of 2021.[459]
A 2016 survey conducted on 44,662 Chinese students (mean age 14.6 years), reported that e-cigarette use was significantly associated with respiratory symptoms, e.g., cough or phlegm for 3 consecutive months in the past 12 months.[459] Likewise, in a 2017 study on 2,086 adolescents aged 16–18 years who took part in the Southern California Children's Health Study, self-reported wheeze in the last 12 months was associated with current but not past use of e-cigarette.[459] In the same study, chronic bronchitis symptoms during the previous year were associated with both past and present use of e-cigarette.[459] The risk of bronchitis symptoms was directly proportional to the number of days of e-cigarette use in the past month, compared with non-e-cigarette users.[459] Vaping among 11th-grade and 12th-grade students in California was linked with twice the chance of respiratory complaints, and the chance went up with vaping more regularly.[212] In a 2020 cohort study of 7,049 adolescents, the association of e-cigarette use alone with wheezing in the past 12 months proved not to be significant.[459]
A 2017 cross-sectional study investigating the effects of active, passive, and e-cigarette vaping in Korean adolescents, including 4,890 with asthma in the last 12 months, reported significant associations between active and passive smoking and asthma.[459] In addition, the authors found that asthma was significantly more frequent in the e-cigarette group.[459] In a 2016 cross-sectional study on a large sample of 35,904 high school students (mean age 16.4 years) in South Korea, the authors found that e-cigarette users had an increased association with asthma diagnosis in comparison with non-e-cigarette users, suggesting that e-cigarette use may be a risk factor for asthma.[459] Of note, current e-cigarette users had the highest risk for severe asthma, defined as the number of days (greater than or equal to 4) absent from school in the past year due to asthma symptoms, compared to non-e-cigarette users.[459] Similarly, in a 2017 survey on 6089 adolescents (mean age 15.8 years) in Hawaii, the authors reported that current use of e-cigarettes showed a significant association with current asthma and a marginal one with asthma at any time.[459] A 2020 study on 21,532 U.S. adolescents (age range: 14–18 years), in which use of an e-vapor product was associated with asthma, showed an additional harmful effect on asthma of the combined use of vapor products with marijuana and cigarette smoking: use of an e-vapor product was associated with asthma, and this association was even more evident when its use was coupled with marijuana, particularly when cigarette smoking was also involved.[459] When adjusting for frequent cigarette smoking and marijuana use, frequent use of an e-vapor product (greater than or equal to 10 days per month) was significantly associated with asthma.[459]
Asthma exacerbations were found to be associated with e-cigarette vaping.[459] Data from the 2012 Florida Youth Tobacco Survey, involving 36,085 high school students, reported that prevalence of ever having used e-cigarette and having used them in the past 30 days among those who reported asthma was 10.4 and 5.3%, and this was significantly higher than in those without asthma.[459] Among students with asthma, use of e-cigarette in the past 30 days was positively associated with an asthma attack in the past 12 months.[459]
E-cigarette use is associated with a doubling of the risk of symptoms of chronic bronchitis among US high school juniors and seniors with higher risk associated with higher use; these risks persisted among former users.[158] Similarly, current e-cigarette use was associated with an increased diagnosis of asthma among Korean high school students among current (e-cigarette users who were never cigarette smokers).[158] E-cigarette users were also more likely to have had days absent from school due to severe asthma symptoms.[158]
2019–2020 vaping lung illness outbreak

In 2019 and 2020, an outbreak of severe vaping-induced lung illness (called e-cigarette, or vaping, product use-associated lung injury[368]) had affected certain users of vaping products in the US[65] and Canada.[66] Cases involved in a cluster of lung illnesses were first identified in Illinois and Wisconsin in April 2019.[461] Published case reports of vaping-related lung illnesses can be traced back to 2012.[462] Similar cases of vaping-induced lung injuries were reported in the UK and Japan before the outbreak occurred.[37][350] The prevalence of vaping-induced lung injuries ocurring worldwide remains unclear.[37] As of February 18, 2020, a total of 2,807 hospitalized cases have been reported to the Centers for Disease Control and Prevention (CDC) from all 50 states, the District of Columbia, and two US territories (Puerto Rico and US Virgin Islands).[65] 68 deaths in the US have been confirmed in 29 states and the District of Columbia, as of February 18, 2020.[65] Cases peaked in September 2019, and a slow decline followed.[note 8][65] Chief Public Health Officer of Canada announced on October 11, 2019 that they are aware of the initial cases of vaping-induced lung injury.[463] As of August 14, 2020, 20 cases of lung injuries have been reported to the Public Health Agency of Canada.[66] The majority of cases in Canada involving lung injuries do not seem to have been connected with the use of THC-infused products.[66]
Of the 2,807 reported cases, 2,022 hospitalized persons had data on substance use, as of January 14, 2020.[65] 82% reported THC use, 33% reported exclusive THC use, 57% reported using nicotine-containing products, and 14% reported exclusive use of nicotine-containing products.[65] Many of the samples tested by the states or by the US Food and Drug Administration (FDA) as part of the 2019 investigation have been identified as vaping products containing tetrahydrocannabinol (or THC, a psychoactive component of the cannabis plant).[464] Most of those samples with THC tested also contained significant amounts of vitamin E acetate.[464] The CDC reported that their findings suggest vaping products containing THC are linked to most of the cases and play a major role in the outbreak.[65] The CDC stated that the chemical vitamin E acetate is a very strong culprit of concern in the lung illnesses related to THC-based vaping products, but did not rule out other chemicals as possible causes.[note 9][465] The majority of those affected were young adults aged 18 to 34, which is the group with the greatest prevalence of cannabis use in the US.[67] Nicotine e-cigarette use has been linked to the vaping-induced lung injury cases in a small subset of users.[69]
Thickening agents were used to dilute vape oils.[466] There has been an increase in attention to companies that sell diluent products that are made with vitamin E acetate.[466] Previously, vitamin E acetate was used in low concentrations, or lower than 20% of the formula in vape cartridges.[466] As a result of a limited availability of cannabis in California as well as high demand, illicit sellers had used about 50% or higher of diluent thickeners in their formulas to bulk up tiny potency vape cartridges.[466] In September 2019, New York Governor Andrew Cuomo instructed the state health department to issue subpoenas against three sellers of thickening agents used in illicit vaping products.[467] The use of vitamin E acetate in vaping products is not banned in the US,[456] though Colorado,[468] Ohio,[468] and Washington have banned it in vaping products,[469] and Oregon has banned it in cannabis vaping products.[470] Health Canada does not permit vitamin E acetate in cannabis vaping products in Canada.[471] On November 18, 2022, six people involved in an elaborate criminal THC vape cartridge ring were convicted, and each one received fines or probation.[472] Jacob and Tyler Huffhines, and their mom Courtney, were convicted of criminal charges related to THC vape cartridges without receiving a prison sentence.[473] Wesley Webb, Hannah Curt, and Daniel Graumenz, were all fined.[472] Both Jordan Lynam and Tarail King were anticipated to be sentenced in November 2022.[474]
The e-cigarette industry is placing the blame on illicit vaping liquids for the lung injuries.[475] Juul Labs stated that some news agencies report that several cases of lung illness are associated with vaping THC, found in cannabis, "a Schedule 1, controlled substance that we do not sell."[476] The CDC and US FDA recommend that people not use THC-containing e-cigarette, or vaping, products, particularly from informal sources like friends, family, or in-person or online dealers, as of February 18, 2020.[65] The US FDA considers it prudent to avoid inhaling vitamin E acetate.[464] On September 6, 2019, the US FDA stated that because consumers cannot be sure whether any THC vaping products may contain vitamin E acetate, consumers are urged to avoid buying vaping products on the street, and to refrain from using THC oil or modifying/adding any substances to products purchased in stores.[464] The Public Health Agency of Canada recommends for adults and parents or guardians who are smoking or vaping to contact a health care provider for guidance on ways to stop.[66] The vaping-induced lung injuries has led to concern around the world.[179] In 2020, the first uptick in vaping-induced lung injury cases had occurred in Utah since the decline of 2019.[70]
Cardiovascular effects

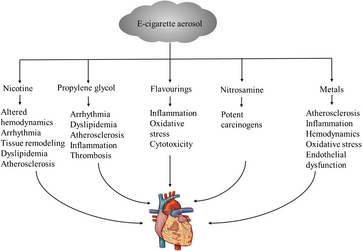


There is limited available evidence on their long-term cardiovascular effects.[479] No data is available on their effects in individuals with cardiovascular disease, as of 2016.[374] Their cardiovascular effects in individuals who do not have cardiovascular disease is uncertain.[480] Although limited, there is supportive evidence that vaping adversely impacts endothelial function and arterial hardening.[479] Most of the cardiovascular effects of vaping are consistent with those of nicotine.[126] E-cigarettes may lead to adverse effects on the cardiovascular system through various mechanisms, such as oxidative stress, inflammation, endothelial dysfunction, atherosclerosis, hemodynamic effects, and platelet activity.[477]
A 2023 systematic review and meta-analysis finds that nicotine-containing e-cigarettes cause a substantial, potentially harmful effect on several short-term cardiovascular parameters.[481] Their short-term use may result in adverse effects in vascular endothelial function.[136] Vaping might bring about some adverse cardiovascular effects to users, especially those who already have cardiovascular disease.[126] However, the risk is believed to be lower than that of cigarette smoking based on research comparing e-cigarette aerosol in contrast to cigarette smoke chemicals.[126] Compared to non-users, e-cigarette use increases the chance of experiencing a heart attack by 33%.[482]
There is a substantial amount of evidence that e-cigarettes can be equally (if not even more) harmful to the cardiovascular system than traditional tobacco.[483] Like classic tobacco smoking, e-cigarettes can also increase sympathetic nervous system activity, oxidative stress and inflammation, endothelial dysfunction, and platelet activation, leading to cardiac arrhythmias, atherosclerosis and plaque instability, thrombosis and acute ischemia, etc.[483] The effects of e‐cigarettes on RAAS activity and specifically on aldosterone levels are presently not known.[483] Given the similarity between their cardiovascular effects and those of traditional tobacco smoking, it is quite plausible that e-cigarette–derived nicotine also activates the RAAS axis and elevates circulating aldosterone levels, exactly as the nicotine delivered by traditional tobacco products does.[483] Nicotine has systemic hemodynamic effects that are mediated by the activation of the sympathetic nervous system.[105] Thus, acute nicotine treatment can stimulate cardiac output by producing systemic vasoconstriction and increasing heart rate.[105]
The effects of aldehydes, particulates, and flavorings used in vaping devices on cardiovascular health is not clear.[126] Low amounts of aldehydes can still be a health concern, particularly among individuals with cardiovascular disease.[225] E-cigarettes reduce cardiac muscle function and increase inflammation, but these changes were only substantial with traditional cigarettes.[64] No published research is available on vaping and thrombosis, platelet reactivity, atherosclerosis, or blood vessel function.[81] The small particles generated from e-cigarette use have the ability to get through airways and enter circulation, which pose a potential risk to cardiovascular systems.[225] The minute nicotine particles in the e-cigarette vapor could increase the risk of cardiac arrhythmias and hypertension which may put some users, particularly those with atherosclerosis or other cardiovascular risk factors, at significant risk of acute coronary syndrome.[397] There are many compounds in the e-cigarette vapor that have an impact on the onset and advancement of atherosclerosis.[484] Some case reports documented the possible cardiovascular adverse effects from using e-cigarettes, the majority associated was with improper use.[397] Even though e-cigarettes are anticipated to produce fewer harmful substances than traditional cigarettes, limited evidence recognizes they comparatively have a lowered raised cardiovascular risk.[397]
Preliminary studies have shown that using a nicotine containing e-cigarette for just five minutes causes similar lung irritation, inflammation, and effect on blood vessels as smoking a traditional cigarette, which may increase the risk of a heart attack.[485] E-cigarette use leads to sympathomimetic effects because of nicotine intake.[486] The evidence suggests that vaping may induce tachycardia-induced cardiomyopathy.[486] E-cigarettes containing nicotine may have a lower cardiovascular effect than traditional cigarettes containing nicotine.[374] Research on the consequences of vaping on blood pressure is limited.[487] Short-term physiological effects include increases in blood pressure and heart rate.[81] The increased blood pressure and heart rate among smokers who vaped was lower than with cigarette smoking.[225] A 2016 study found vaping increases aortic stiffness in people who did not have cardiovascular risk factors, an effect that was lower than with cigarette smoking.[126] A 30-minute vaping session seems to induce an unfavorable effect on aortic stiffness similar to traditional smoking.[104] Habitual vaping was associated with oxidative stress and a shift towards cardiac sympathetic activity, which are both associated with a risk of developing cardiovascular disease.[348] A 2012 case report found a correlation between paroxysmal atrial fibrillation and vaping.[81] Research indicates a relationship between exposure to particulate matter with a diameter of 2.5 μm and the chance of developing cardiovascular disease.[225]
E-cigarettes adversely impact the cardiovascular system.[158] Although the specific role of nicotine in cardiovascular disease remains debated, nicotine is not the only biologically active component in e-cigarette aerosol.[158] E-cigarettes work by creating an aerosol of ultrafine particles to carry nicotine deep into the lungs.[158] These particles are as small as—and sometimes smaller than—those in traditional cigarettes.[158] These ultrafine particles are themselves biologically active, trigger inflammatory processes, and are directly implicated in causing cardiovascular disease and acute cardiovascular events.[158] The dose-response effect for exposure to particles is nonlinear, with substantial increases in cardiovascular risk with even low levels of exposure to ultrafine particles.[158] For example, exposure to second-hand cigarette smoke has nearly as large an effect on many risk factors for cardiovascular disease and the risk of acute myocardial infarction as does being an active smoker.[158] Like traditional cigarette smokers, e-cigarette users experience increased oxidative stress and increases in the release of inflammatory mediators.[158] E-cigarette aerosol also induces platelet activation, aggregation, and adhesion.[158] All these changes are associated with an increased risk of cardiovascular disease.[158] These physiological changes are manifest in rapid deterioration of vascular function following use of e-cigarettes.[158]
E-cigarette and traditional cigarette smoking in healthy individuals with no known cardiovascular disease exhibit similar inhibition of the ability of arteries to dilate in response to the need for more blood flow.[158] This change reflects damage to the lining of the arteries (the vascular endothelium), which increases both the risk of long-term heart disease and an acute event such as a myocardial infarction (heart attack).[158] Using e-cigarettes is also accompanied by a shift in balance of the autonomic (reflex) nervous system toward sympathetic predominance, which is also associated with increased cardiac risk.[158] The biological stresses that e-cigarette use impose on the cardiovascular system are manifest as an increase in risk of acute myocardial infarction.[158] A cross-sectional analysis of data in the US 2014 and 2016 National Health Interview Surveys showed that daily e-cigarette use was associated with increased odds of having suffered a myocardial infarction, controlling for traditional cigarette smoking, demographic characteristics (age, gender, body mass index, family income) and health characteristics (hypertension, diabetes, and hypercholesterolemia).[158] Significantly, the effect of using e-cigarettes on the odds of myocardial infarction approached what was found with traditional cigarette smoking.[158] Daily vaping represents an independent risk factor for myocardial infarction, synergically amplified by exposure to nicotine, a parasympathomimetic alkaloid increasing heart rate and blood pressure.[104]
Hypertension effects
The research conducted by Farsalinos et al. in 2014 demonstrated that short-term e-cigarette using caused a fractional increase in diastolic blood pressure.[122] In the study conducted by Yan et al. in 2015, a lower nicotine content was reported in the blood of persons vaping e-cigarettes than in the case of people smoking traditional cigarettes, which contributed to a smaller increase in arterial pressure and heart rate in this group.[122] Research by Vlachopoulos et al. in 2016 was conducted among people of 30 ± 8 years of age without cardiovascular risk.[122] The subject of analysis was arterial pressure measured in 4 sessions: smoking traditional cigarettes and e-cigarettes for 5 minutes, 30 minutes of vaping e-cigarettes, and sham procedure that lasted 60 minutes .[122] The analysis of the obtained results did not show any differences in all the readings between the sessions, while the systolic and diastolic arterial pressure values as well as the heart rate increased both during smoking traditional cigarettes and e-cigarettes.[122]
Very significant results were obtained in the research conducted by Polosa et al. in 2017.[122] During a 3.5 years' observation of a group of young people (29.7 ± 6 years of age), daily e-cigarette users, who had never smoked before, no significant changes in the heart rate and arterial pressure values were demonstrated in comparison with the control group, who had never smoked any kind of cigarettes.[122] In turn, in a study conducted by Franzen et al. in 2018, persons vaping e-cigarettes and traditional cigarettes were subjected to a 2 hour observation immediately after having smoked a cigarette.[122] The analysis of the obtained results demonstrated that systolic blood pressure increased for up to 45 minutes after the person had stopped using an e-cigarette containing nicotine and for about 15 minutes in the case of normal cigarettes.[122] No significant changes in arterial pressure values in the first hour of observation were reported for e-cigarettes.[122] A similar correlation was demonstrated for heart rate readings.[122] Research in that field was also conducted by Antoniewicz et al. in 2019 to assess acute influence of inhaling e-cigarettes with nicotine and without it within the period of 0, 2, and 4 hours after exposure.[122] A significant increase in heart rate was reported in the case of vaping e-cigarettes containing nicotine and an increase in arterial blood pressure in both analyzed cases.[122]
In the study of Arastoo et al. in 2020 among 100 electronic and traditional smokers, including chronic smokers, the baseline heart rate variability as well as hemodynamics (blood pressure and heart rate) were analyzed.[122] In this research, the authors hypothesized that the changes in these parameters are caused by nicotine, and not by the non-nicotine components of the e-cigarette aerosol.[122] Based on the conducted research, it was shown that people who were chronic smokers of both types of cigarettes had a similar level of heart rate variability.[122] When assessing the effect of vaping e-cigarettes, a sharp increase in blood pressure and heart rate was noticed only after the use of e-cigarettes with nicotine, which confirmed the hypothesis.[122]
An interesting study was also conducted by George et al. in 2019 on a group of people of 18 of age or older, who had been smoking ≥15 cigarettes for ≥2 years.[122] During the study, the examined persons changed to using e-cigarettes with or without nicotine.[122] The analysis of the obtained results demonstrated that once both groups of e-cigarette vapers had been combined, a greater decrease in systolic blood pressure was reported than in the group of traditional smokers.[122] Abnormalities in heart rate during vaping e-cigarettes in comparison with nonsmokers were also demonstrated by Moheimani et al. in 2017.[122] Moreover, the authors indicate that it was not caused by the nicotine content in the e-cigarette liquid, because it was untraceable in the plasma of the examined persons.[122] At the same time, they emphasize that it is nicotine metabolites that can produce adverse effects leading to a greater risk of cardiovascular diseases among people using this type of cigarettes.[122]
E-cigarettes are very often chosen when a person wants to quit smoking traditional cigarettes.[122] In a 12-month prospective randomized research conducted by Caponetto et al. in 2013, the researchers subjected 300 participants divided into 3 groups to an analysis.[122] Study groups were given nicotine refill cartridges: 7.2 mg for 12 weeks; 7.2 mg for 6 weeks and 5.4 mg for another 6 weeks.[122] The control one was given cartridges without nicotine for 12 weeks.[122] The analysis of the obtained results demonstrated a decrease in the frequency of smoking in each group.[122] However, what is important is the fact that within the duration of the study, no significant changes in systolic and diastolic pressure or heart rate were demonstrated.[122] Moreover, no differences between the analyzed groups were revealed.[122] In turn, in a continuation of that study, conducted by Farsalinos et al. in 2017, an additional classification of constant smoking phenotype was made, in which people were divided into those who quitted smoking in full, those who limited the number of smoked cigarettes and those in whose case quitting ended in failure.[122] It was demonstrated that persons who limited or quitted smoking and changed to e-cigarettes were characterized by lower systolic arterial blood pressure.[122] This effect was especially visible in persons with elevated values at the beginning of the examination.[122]
In the context of e-cigarettes, by contributing to an increased sympathetic heart activity, can be also responsible for increased oxidative stress, which will cause an increased cardiovascular risk.[122] Moreover, the increased oxidative stress and inflammatory conditions can induce the development of atherosclerosis.[122]
Alzheimer's disease effects
Nicotine independently promotes the development of neurodegenerative disorders,[348] induces oxidative stress, and inhibits the process of autophagy.[348] Out of 28 e-liquids tested from seven companies in 2014, the four most commonly found flavor additives were vanillin, ethyl maltol, ethyl vanillin, and menthol.[348] They are carcinogenic or toxic, which may contribute to causing cardiopulmonary diseases such as chronic obstructive pulmonary disease and neurodegenerative disorders such as Alzheimer's disease.[348] E-cigarette use results in oxidize stress, which play a role in contributing to cardiopulmonary diseases and neurodegenerative disorders.[348]
Brain effects
The long-term effects of e-cigarette use on the brain is unknown.[40] With long-term nicotine use, cellular adaptations (as the brain reacts to recurring periods of uptake and withdrawal) within the brain may result in almost permanent alterations in neurons and neural circuits.[46] While a clear positive correlation between e-cigarette use and depression has been established, the causality and mitigating factors affecting this relationship are largely undetermined.[40] There is growing evidence that vaping is hazardous to one's health including risk of depression which increases the risk of suicidal thoughts and suicide.[456]
Chronic farnesol administration increases the firing rate of nicotinic acetylcholine receptor-expressing neurons in the ventral tegmental area.[40] Thus, the addition of the green apple flavorant, which is acquired by adding the chemical farnesol, induces neurobiological changes in the brain’s reward-related circuitry, which enhances nicotine’s rewarding properties to reinforce continued product use.[40]
E-cigarette-emitted metal particulates have been shown to readily cross the blood–brain barrier, as evidenced by metal accumulation in the mouse brain.[40] Moreover, following e-cigarette exposure, arsenic, chromium, copper, iron, manganese, nickel, lead, selenium, strontium, and zinc were found to accumulate across different regions of the mouse brain, with the greatest accumulation observed in the anterior frontal cortex and striatum.[40] Specifically, in the anterior frontal cortex, copper and strontium were enriched, whereas arsenic, chromium, copper, iron, lead, and selenium were enriched in the striatum.[40] Like other types of e-cigarette emissions, the type and relative proportion of metals that might accumulate in the brain are expected to vary among commercially available brands due to differences in the vape liquid constituents and electronic cigarette device characteristics.[40]
Cerebrovascular disease effects
Adequate research is not available to ascertain the risk of long-term harm resulting in cerebrovascular disease.[488]
Effects on COVID-19

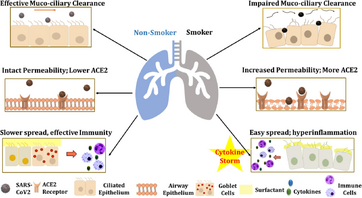
Because of their possible acute lung and cardiovascular toxicity, vaping may pose a greater risk of severe sickness for individuals with COVID-19.[112] The impact of vaping on being more susceptible to being diagnosed with COVID-19 is unknown.[491] A 2020 study found a clear link between vaping and various COVID-19 cases and fatalities.[492]
Vaping habits, such as the hand-to-mouth actions as well as touching the face, could increase the chance of COVID-19 infection and spread of the virus.[205] Through the transmission of asymptomatic carriers, sharing vaping devices could contribute to the spread of the virus.[205] It is possible the surface of a vaping device can be a vehicle for the transmission of the virus.[493] This is because the virus can survive on surfaces for a few hours to days.[493] Due to their design, e-cigarettes devices are brought to the mouth and face to inhale repeatedly, and many users have an increased urge to cough or expectorate which can increase the transmission of COVID-19.[138] In addition, the aerosols generated by these devices could contribute to SARS-CoV-2 transmission.[138]
E-cigarettes which contain high amount of nicotine might contribute to overexpression of ACE2 and contribute in the serious COVID 19 associated complications.[489] Moreover, ACE2 is linked to nicotinic acetylcholine receptors (nAChRs), particularly alpha7nAChR receptors, further supporting the notion that vaping (nicotine) might be playing a significant role in the pathophysiology of COVID-19.[489] Furthermore, TMPRSS2 protease important in the virus entry into the host cells are is suggested to be altered by ACE2 in vapers.[489]
E-cigarette use impair mucociliary clearance, increased mucosal permeability, promote peribronchial inflammation, and fibrosis.[489] It is well-established that the mucociliary epithelium and the mucous layers act as the primary line of defense against pathogens.[489] Further, vaping induces oxidative stress and inflammatory responses which may further contribute to COVID-19 related complication in vapers.[489]
A 2020 analysis showed that the occurrence of COVID-19 was associated with the use of e-cigarettes or the use of e-cigarettes and cigarettes together.[489] COVID-19 diagnosis was five times more likely among e-cigarettes users and seven times more likely among ever-dual-users.[489] Further, the testing was nine times more likely among past 30-day dual-users and 2.6 times more likely among past 30-day e-cigarette only users.[489] A 2021 review speculates that dual users of e-cigarettes and alcohol may be at higher risk to complications of COVID-19.[352] Higher odds of COVID-19 symptoms and higher odds of confirmed/suspected COVID-19 diagnosis were found in dual users than in exclusive smoking of conventional cigarettes.[114]
A 2020 study showed that while the use of nicotine or flavor-containing e-cigarettes led to significant cytokine dysregulation and potential inflammasome activation, none of these effects were detected in non-flavored and non-nicotine-containing e-cigarettes.[117] Therefore, taking together these observations, e-cigarette use may still be a potent risk factor for severe COVID-19 development depending on the flavor and nicotine content.[117] While smoking is linked with progression to more dire cases of COVID-19, a 2020 review recommends to give up vaping to minimize the chance of developing a severe case of COVID-19.[494]
Vaping websites inquired abouts the risks related to e-cigarette use and COVID-19, and unverified statements that vaping and nicotine can be used to guard against COVID-19 spread across social media.[495] The use of-cigarettes and the possible greater chance of transmission and susceptibility to COVID-19, as well as the possible greater chance of severity to this illness is a public health concern.[496] Medical organizations and public health professional across the globe have voiced their concern that e-cigarette use may increase the likelihood for COVID-19 susceptibility, severity, and negative consequences.[496]
Erectile dysfunction effects
Vaping may cause oxidative stress, such as the creation of reactive oxygen species and hydroxyl radicals.[497] This can lead to endothelial dysfunction, which in turn may lead to erectile dysfunction.[497] Nicotine causes dysfunction of nitric oxide synthesis.[84] This may result in an inability to get penile erections, resulting in erectile dysfunction.[84] Mutiple studies have shown endothelial dysfunction from vaping, from nicotine itself as well as additives and flavors in e-cigarette emissions.[497] No study has conclusively demonstrated vaping causes erectile dysfunction, although nicotine use has been demonstrated to cause erectile dysfunction.[497]
Esophagitis effects
E-cigarettes are potential triggers of esophagitis exacerbations.[104]
Effects on eye health
Limited research is available on the consequences of vaping on eye health, though chemicals such as nicotine and aldehydes are possibly harmful to the eyes.[498] Exposure to toxic chemicals from e-liquid or its vapor may result in dry eye and tear film break-up.[498]
Reproductive effects
Male
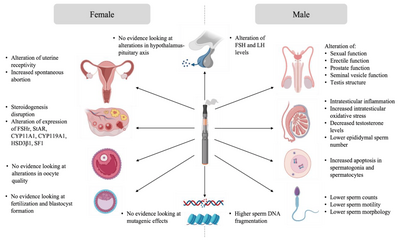
While studies on the effect of e-cigarettes on human male reproduction are limited, numerous studies have investigated their effect in animal models.[101]
Exposure to e-cigarettes was reported to disturb the hypothalamo-pituitary axis, resulting in altered gonadal function and semen quality.[101] Wawryk-Gawda and collaborators in 2019 showed that in male rats exposed to e-cigarette vapor had increased apoptosis in spermatogonia and spermatocyte, an alteration of the morphology and function of the seminiferous epithelium, as well as unica albuginea malformations.[101] Other studies linked e-cigarette utilization with steroidogenesis disruption and global disorganisation of the testes, accompanied by significant desquamation of germ cells.[101] Moreover, low testicular weight and a higher apoptotic cell number in the testis was observed in the context of e-cigarette exposure.[101] Intraperitoneal injection of e-cigarette liquid in male rats induced toxicity and testicular inflammation, which, in turn, affected sperm production and sperm quality with lower sperm density, reduction of epididymal sperm number, and lower sperm viability.[101] When inhaled for 4 weeks by male rats, the same flavoring induced apoptosis in testes.[101] The sperm of rats exposed to e-cigarette vapor showed increased teratozoospermia (looped tail, flagellar angulation, and complete absence of flagellum).[101] Studies showed that sperm chromatin integrity could also be affected by e-cigarette exposure.[101] In fact, higher DNA damage was observed in both testis and sperm of exposed rats.[101] These findings suggest potential mutagenic effects of e-cigarettes on sperm.[101]
Little to no studies have corroborated these findings in humans.[101] A preliminary study, presented at the British Fertility Society Conference in 2017, investigating the effect of e-cigarette flavoring on human sperm, showed a significant decrease in motility in specimen cultured with e-liquid flavoring.[101] This study and the results obtained in animal models all suggest that vaping could have pathogenic effects on male reproduction and caution should be used when vaping and trying to conceive.[101]
Female
Evidence of the impact of e-cigarettes on female reproduction suggests that the female reproductive system is not left unaffected by exposure to e-cigarettes.[101] Unlike sperm, there is no evidence linking the impact of e-cigarette utilization on intrinsic oocyte quality and oocyte genome integrity.[101] However, some data suggests that ovarian function is impaired in animal models exposed to e-cigarettes.[101] A decreased percentage of normal follicles was described in the ovaries of female rats exposed to e-cigarette fluid.[101] Hormone levels were also affected in these animals, where a reduction in estrogen secretion was observed.[101] Implantation and pregnancy outcomes were also affected in mice exposed to e-cigarette vapor.[101] Microarray analysis showed an alteration in uterine receptivity transcripts in e-cigarette exposed mice.[101] These females experienced a delay in embryo implantation, although the animals showed high progesterone levels, resulting in a decreased offspring number.[101]
Although reproductive trials have demonstrated that e-cigarettes can be responsible for embryo implantation and development impairments in mice, studies have not yet been performed specifically regarding e-cigarette-associated exposure in mammal granulosa cells.[499] In a 2017 study carried out in pregnant smokers, it was observed that the use of e-cigarettes as a way to quit tobacco smoking was consideerably more common than any other US FDA-approved smoking cessation tool.[499] For this reason, both fertility and embryo implantation trials in 2019 have been performed in mice following exposure of the animals to e-cigarette-produced aerosol for 4 months.[499] Exposed dams showed a significant delay in the onset of the first litter and a noticeable impaired embryo implantation despite the detection of high progesterone levels, a known pregnancy indicator.[499] As a consequence, existing studies could indicate that e-cigarettes are capable of impairing pregnancy initiation and fetal health, further suggesting that their use on behalf of reproductive-aged women or during pregnancy should be considered with extreme caution, a 2020 review states.[499]
Effects on gastrointestinal system
The most common gastrointestinal symptoms associated with vaping were epigastric pain, nausea and vomiting, followed by diarrhea and hemorrhage, which Gaur et al. attributed to the trace metals copper and chromium in the aerosol if exposed to high levels.[111] Further reports have documented relapsed ulcerative colitis in two unrelated cases of heavy cigarette smokers after having stopped cigarette smoking and starting e‑cigarette use.[111] In these cases, either the continued use of e‑cigarettes or switching back to cigarette smoking helped alleviate the symptoms.[111] In another case report of a pregnancy health effect linked to e‑cigarette use, a 1-day-old infant suffered gastrointestinal bleeding with abdominal distension and respiratory distress.[111] The infant recovered at 6 months, after having undergone double barrel ileostomy and subsequent surgical procedures.[111] Vaping might induce recurring ulcerative colitis.[174]
Effects on immunology
Concern exists regarding the immunological effects of e-liquid, and analysis on animals demonstrate that nicotine as well as e-liquid vapor, appear to have adverse effects on the immune system.[174] The health consequences of smoking are widely documented, but the immunological effects of e-cigarette use is not well understood.[125] The finding of the limited available research on the immunological effects appear to be contradictory.[125] There is a small amount of research available that is related to gastrointestinal and neurological health risks.[125] There were reports of e-cigarettes causing an immune system reaction involving inflammation of the gastrointestinal system.[121]
Insulin resistance effects
Studies have shown that nicotine causes decreased sensitivity of tissues to insulin, thus increasing the risk of developing type 2 diabetes.[122] Nicotine contributes to an increase in the level of hormones antagonistic to insulin, i.e, catecholamines and cortisol.[122] In turn, research studies conducted on animals have shown a direct influence of nicotine on activation of protein kinase dependent on AMP in adipose tissue.[122] It increased the speed of lipolysis and promoted insulin resistance.[122] Insulin resistance, which causes the development of diabetes, is connected with prothrombotic inflammatory conditions and provokes atherogenic changes in blood lipids.[122] It increases the risk of ischemic heart disease, diseases of peripheral arteries, and brain stroke.[122]
Research on the influence of nicotine on the organism has demonstrated its ability to induce hyperglycemia by activating glycogenesis and gluconeogenesis.[122] El Golli et al. in 2016 conducted experiment on rats administered intraperitoneally exposed to pure nicotine (0.5 mg/kg of body weight), e-liquid with or without nicotine for 28 days, and a significant increase in the level of blood glucose was reported.[122] Additionally, a reduced level of liver proteins and increased transaminase activity were detected in all the examined groups, yet it was the rats exposed to e-cigarettes which achieved worse results than the rats exposed to pure nicotine.[122] This can suggest that the mechanism of disorders of glucose metabolism induced by e-cigarettes is different than in the case of nicotine alone.[122] A 2019 study demonstrated that e-cigarettes users were at a greater risk of being diagnosed with prediabetes than those who had never used this kind of cigarettes.[122]
Kidney effects
A 2016 study regarding e-liquid exposure in adults rats showed e-cigarettes have an adverse impact on the kidneys.[379]
Liver effects
Animal studies have shown that vaping can induce hepatic steatosis through heterogeneous mechanisms, involving oxidative stress, hepatocytes apoptosis and impairment of cholesterol and lipid metabolism.[104] A 2020 case report documented e-cigarettes-induced hepatic injury even in humans, describing an increase of liver enzymes in a young vaper presenting to the emergency department for fever, abdominal pain, vomiting, and diarrhea.[104]
Effects on medication
Two cases highlighted that the use of the e-cigarette increased their clozapine levels and one publication presenting a patient with epilepsy for whom it increased their seizure frequency.[198] Two of the patients were 16 years old and 23 years old females and there was one 52-year-old male.[198] The increased clozapine levels reported cases, demonstrate the effect of nicotine on medication plasma levels and raise wider concerns regarding potential interactions with other medications as well.[198] Switching between different e-cigarette products and vice versa, or planning on quitting smoking, might alter the serum levels of a person's medication.[198]
Metabolism
Metabolic effects
There is a limited amount of research available on the metabolic effects of vaping.[500] It has not been fully studied in humans as to whether vaping has the same negative effects on metabolic processes as cigarette smoking.[500] Though, animal studies show similar effects of vaping, even without being exposed to nicotine, on weight and metabolic processes, comparing cigarette smoking.[500] This shows other things are responsible for the metabolic effects than just nicotine.[500] Animal studies indicate that vaping has similar negative effects on weight, body fat, glucose and lipid profiles and other cardiovascular potential dangers as traditional cigarettes, but they may be less prominent.[500] A lot of these cardiometabolic effects happen even without nicotine being present.[500]
Metabolic syndrome effects
As of 2020, there have been very few publications demonstrating the influence of e-cigarettes on the risk of occurrence of metabolic syndrome in people.[122] Research on a group of 18,300 volunteers was conducted by Lequy et al. 2018.[122] The obtained results allowed the researchers to claim that the occurrence of metabolic syndrome was connected with using e-cigarettes, whenever patients were not on a diet.[122] Another study in 2020 has been conducted on a group of 7505 Korean males over 19 years of age to compare the frequency of occurrence of cardiovascular risk factors among: males smoking conventional cigarettes, dual users (e-cigarettes and traditional cigarettes users) and never-smokers.[122] The multivariate logistic regression analysis showed that, in the adjusted model, the odds ratio (OR) for the prevalence of metabolic syndrome equaled 2.79 (p < 0.001) in comparison with never-smokers and 1.57 (p = 0.038) in relation to cigarette-only smokers.[122] In this model, dual users were characterized by an increased waist circumference and triglycerides level, as well as reduced high-density lipoproteins (HDL) in comparison with both the people who had never smoked and those who smoked only traditional cigarettes; therefore, it may be concluded that dual users are more vulnerable to cardiovascular risk factors.[122]
Blood lipids
High levels of triglycerides and low levels of HDL are risk factors for cardiovascular disease.[105] Nicotine promotes loss of body weight and the disturbance of lipoprotein metabolism through the secretion of catecholamines, such as norepinephrine.[105] Catecholamine secretion favors the elevation of low-density lipoprotein (LDL) and very low-density lipoprotein (VLDL) and is also associated with decreased HDL levels.[105] Higher levels of LDL and VLDL are also known risk factors for cardiovascular diseases.[105] A health survey in Korean men showed significantly elevated triglyceride levels in dual users of conventional cigarettes and e-cigarettes compared to non-smokers.[105] In addition, there was no significant difference in triglyceride levels between dual users and conventional cigarette-only smokers.[105] However, another work has shown that e-cigarette users have higher triglycerides and lower HDL than never users.[105] HDL cholesterol was significantly lower in both dual users and conventional cigarette only smokers compared to those who never have smoked.[105] E-cigarette vapers had increased levels of LDL and VLDL compared to nonsmokers.[105] Habitual e-cigarette users had increased oxidized LDL levels compared with non-user control individuals.[105] Oxidized LDL can lead to atherosclerosis as it can contribute to the buildup of atherosclerotic plaques.[105]
A 2019 study shows that e-cigarettes influence the lipid profile.[122] A comparison between nonsmokers, people smoking traditional cigarettes, and those using e-cigarettes demonstrated that the LDL fraction concentration was significantly higher in the group vaping e-cigarettes than in the control group, as opposed to those smoking traditional cigarettes, in whose case a negligible increase was reported.[122] In both groups also a slight decrease in the HDL fraction cholesterol was reported in comparison with the nonsmoking group, yet this decrease was greater in the group of people vaping e-cigarettes.[122] In turn, in the case of VLDL, the group of e-cigarettes users demonstrated a smaller increase in its concentration in blood serum.[122]
Effects on microbial pathogens
Vaping may weaken the body's ability to get rid of microbial pathogens, resulting in greater vulnerability to viral, fungal, or bacterial infections.[501] However, the effects of such findings continue to be unclear.[501]
Effects on multisystem inflammatory syndrome
Studies have shown an association between multisystem inflammatory syndrome and vaping, and a 2021 review speculates that adolescents who vape might be especially vulnerable to serious respiratory symptoms if they develop a hyper-inflammatory state multisystem inflammatory syndrome.[489]
Effects on nasal tissues
Research has been conducted on nasal tissues, partly due to a great number of e-cigarette users exhale via the nose.[492] There is a noticeable decline in gene expression associated with the immune system in the nasal epithelium, which suggests the immune genes had been impaired, and as consequence e-cigarette users may be more prone to infections.[492]
Effects on neuropsychiatric disorders
There is scant evidence on the neuropathological effects induced by nicotine exposure on the developing brain.[502] Due to this lack of knowledge, there is a rising public health concern when taking into account the surge in teen nicotine use and the emergence of innovative nicotine delivery devices like e-cigarettes.[502] There is persuasive evidence implying that teen nicotine exposure raises the likelihood of anxiety-associated behavior in the near term.[503] There is an association between teen nicotine exposure and a higher susceptibility of developing mood and anxiety-associated disorders in adulthood.[502] No effect has been observed on symptoms of schizophrenia from e-cigarette use.[174] Given the lack of data, there is currently no recommendation regarding dose adjustment of antipsychotics in the context of e-cigarette use.[504]
Data from rodents support findings from human studies associating e-cigarette exposure with anxiety- and depression-associated behaviors.[40] Specifically, withdrawal from nicotine was shown to induce persistent changes in anxiety-, depression- and compulsive-like behaviors following seven weeks of e-cigarette exposure, and surprisingly, these behavioral changes persisted 90 days following the last e-cigarette exposure in male mice.[40] Behavioral changes have also been observed even in the absence of nicotine, as nicotine-free e-cigarette vapor exposure was shown to result in anxiogenic phenotypes in both male and female mice.[40]
Abdominal obesity effects
Research conducted on rats demonstrated that exposure to nicotine contributes to significant adipocytes hypertrophy with increased expression of transcription factors of proadipogenic genes.[122] Such factors include the peroxisome proliferator activated receptor γ (PPAR-γ).[122] The result of the aforementioned situation is an increase in body weight and accumulation of adipose tissue.[122] The creation of mature adipocytes is also influenced by oxidative stress.[122]
So far not much has been learnt about the influence of e-cigarettes on adipose tissue and adipocyte functions.[122] The first such research was conducted by Zagoriti et al. in 2020.[122] It compared the influence of traditional cigarettes, e-cigarettes, and heated tobacco products on the differentiation of preadipocytes into beige adipocytes.[122] The increased activity of this kind of adipocytes (so-called thermogenic ones) was suggested as a means of reducing obesity and metabolic disorders.[122] It was demonstrated that the extract of traditional cigarettes, as opposed to the other two extracts, significantly disrupted the differentiation of preadipocytes into beige adipocytes, which can influence the metabolic function of adipose tissue.[122] In turn, the results of research on e-cigarettes conducted on mice demonstrated that pure nicotine did not fully answer for lower body weight.[122] Further studies involving exposure of mice to equivalent nicotine doses, through inhaling e-cigarette or traditional cigarette fumes, did not show any influence on the body weight reduction in those exposed to e-cigarettes.[122] It can suggest that it is other compounds in cigarettes that can participate in reducing body weight while smoking traditional cigarettes.[122] On the other hand, opposite results were obtained by El Goli et al. in 2001 and Werley et al. in 2016 in their research on rats.[122]
Effects on oral health
The tissues of the oral cavity are those first exposed to the inhaled e-aerosol and they interact directly with its toxicants and chemical components.[302] Nicotine can cause vasoconstriction and decreased blood flow, which results in a reduced oxygen and blood supply to the gums and a reduction in the ability of the gums to remain healthy.[320] Research on potential oral health changes following e-cigarette exposure is limited and daily vaping is associated with poor oral health.[302] A 2020 pilot cross-sectional study was performed with volunteers to assess the effect of e-cigarette use on biomarkers of inflammation, oxidative stress, anti-inflammatory lipid mediators, tissue injury and repair and growth factors in saliva and gingival crevicular fluid. The obtained results were compared between four groups of participants as e-cigarette users, non-smokers, cigarette smokers and both e-cigarette and cigarette (dual) smokers.[302] There was significant increase between levels of myeloperoxidase and matrix metaloproteinase-9 in e-cigarette users vs. non-smokers, and between dual smokers and e-cigarette users in inflammatory mediators as receptor for advanced glycation end products, myeloperoxidase and recombinant human uteroglobin/CC10.[302]
The changes in antioxidant capacity of saliva in e-cigarette users and cigarette smokers comparing to non-smokers were observed in a study by in 2021.[302] The uric acid, hypoxanthine, xanthine, TAOS (total antioxidant status) and TEAC (Trolox equivalent antioxidant capacity) were determined in the samples of saliva patients.[302] The antioxidant capacity of saliva was affected in the e-cigarette users in a similar degree as in cigarette smokers when compared to the saliva of non-smokers.[302] The impaired antioxidant function of saliva can stimulate the formation of free radicals and reactive oxygen species (ROS), which play a role in the progression of periodontitis and destruction of tissue.[302]
The microorganisms, harboring over 700 species, that reside in the human oral cavity are described as the oral microbiome, oral microflora or oral microbiota.[302] The microorganisms play an important role in the maintenance of the proper environment in the oral cavity and encompasses oral niches, such as teeth surface, tongue, cheeks, subgingival and supragingival plaque, palates, tonsils and salivary.[302] A dysbiosis, an imbalance in the microbial ecosystem, can produce changes in their functional composition and can result in pathological conditions.[302] The flavoring compounds of e-liquids have various aromas and tastes, and some chemical components, such as saccharides and sucralose are added to provide a sweet taste, they may selectively disrupt the homeostasis of the oral microbiome and can be associated with a variety of oral diseases, such as periodontitis and caries.[302] There is evidence that e-cigarette use is associated with a compositional and functional shift in the oral microbiome, with an increase in opportunistic pathogens and virulence traits.[302] Preliminary research indicates that the health risks of e-cigarettes to the oral microbiome may be comparable to or more than smoking.[45] The combination of glycerin and flavoring agent in e-liquid pods may be associated with a four-fold increase in microbial adhesion and a two-fold increase in biofilm formation.[320] Sticky aerosols produced by heated e-liquid encourage the caries-causing bacterium Streptococcus mutans to adhere to tooth enamel, leading to demineralization and caries.[320]
There is little evidence indicating that using e-cigarettes rather than continue to smoke will help with periodontal disease.[505] Vaping may be equally as dangerous or possibly more dangerous to oral health than tobacco smoking.[506] Vaping with or without nicotine or flavoring may help cause periodontal disease.[507] Nicotine as well as their flavoring may be damaging to periodontal ligament, stem cells, and gingival fibroblasts in cultures as a result of creation of aldehydes and/or carbonyls from e-cigarette vapor.[507] It is possible that e-cigarettes could harm the periodontium because of the effects of nicotine on gum tissues and the immune system.[189] A 2023 review found every study demonstrated an increased marginal bone loss, probing depth, and plaque index, as well as decreased bleeding on probing in e-cigarette users as opposed to non-smokers who had an implant-supported prosthesis with over a year in use.[508] Early research suggests that e-cigarettes have an adverse effect on the results of dental implants in males.[509] A 2016 study found 6.9-8.1% of e-cigarette users had a toothache compared with 3.9-16.7% in traditional cigarette users.[510]
The potential connection of e-cigarette use with dry mouth has not been fully investigated.[511] Dry mouth is one of the oral complaints related to e-cigarettes and the oral diagnoses related to their use include nicotine stomatitis, black hairy tongue, and angular cheilitis.[344] Dry mouth from using e-cigarette affects adults and youth.[511] Vaping can increase the risk of developing oral mucosal lesions, nicotine stomatitis, hyperplastic candidiasis, and black hairy tongue.[512] The oral mucosal lesions nicotine stomatitis, hyperplastic candidiasis, and black hairy tongue are more frequent in vapers than in previous smokers.[512] In 2015, after an individual was diagnosed with black hairy tongue they quit vaping and started smoking again, which cured her discolored tongue.[512] When she started vaping again, the discoloration came back.[512]
Otology effects
Although little is known about the effects of e-cigarettes in otology, preliminary in vitro studies have shown middle-ear epithelial cell cytotoxicity is associated with nicotine and propylene glycol.[513] A 2014 study on guinea pigs showed that nicotine causes injury at the cochlear outer hair cells, which were deformed in shape with vacuolated cytoplasm and heterochromatic nuclei.[513]
Effects on reversible cerebral vasoconstriction syndrome
A 2015 case report found that vaping might trigger the onset of reversible cerebral vasoconstriction syndrome.[174]
Effects on skin
Dermal exposure
The first case of contact dermatitis linked to vaping was reported in 2015.[512] Over the last three years leading up to 2019, there has been a rise in cases of contact dermatitis from e-cigarette nickel exposure.[512]
Contact dermatitis from nickel exposure has been reported, following e-cigarette use.[259] The nickel from the heating coil leaches out of the device, resulting in irritation to the hand from holding the device.[512] Cases of contact dermatitis have been treated with the avoidance of the e-cigarette.[198]
E-cigarette aerosol exposure
Little is known regarding the impacts of e-cigarette aerosol on the skin.[368] A 2014 study found HaCaT skin cells were injuried after directly being exposed to aerosolized Balsamic flavored e-liquid.[368] The aerosolized flavor free e-liquid did not exhibit any effects.[368]
Effects on spine health
Due to the growing worldwide popularity of e-cigarette products advertised as a healthier alternative to tobacco, there is an increasing concern over health risks that are linked to vape use and how it affects bone health.[514] There is evidence that many of the major constituents of e-cigarettes, such as nicotine and carbonyl compounds can significantly impair osteoblast function, suggesting e-cigarette use may be detrimental to bone health.[515]
A 1995 study demonstrated systemic nicotine significantly increased pseudoarthrosis rate to 100% compared to 44% in control animals in a rabbit model of posterolateral spine fusion.[514] A 2000 study showed nicotine alone inhibits the expression of multiple cytokines with a variety of functions during spine fusion.[514] An e-cigarette solution containing nicotine can impact intervertebral disc health through the degeneration of both vasculature and nucleus pulposus and annulus fibrosus cells.[514]
Stroke effects
A 2021 observational study found an association between e-cigarette use and stroke.[516] The role of e-cigarette use in the development of stroke is inconclusive, due to the strong effect of prior tobacco use as a risk factor for stroke.[180]
Effects on surgical outcomes
There is limited information on the physiologic effect of nicotine vaping on surgical outcomes.[517] Nicotine can induce vasoconstriction while in otologic surgery.[407] It is not known whether there is a benefit for vaping to aid with quitting smoking before surgery.[517] Vaping may have a considerable negative effect on wound healing[517] and may hamper tissue regeneration.[518]
Effects on tuberculosis
Long-term e-cigarette use could increase the chance of developing tuberculosis.[102]
Effects on urologic health
Data on the impact of vaping on urologic health is not available.[358]
Vascular disease effects
The detrimental effects of aerosols associated with e-cigarettes start at the endothelial level.[24] The oxidative stress reduces the bioavailability of nitric oxide which in turn plays a key role in endothelium dysfunction alongside peroxynitrite (produced by superoxide) which causes low-density lipoprotein oxidation and inflammatory cytokines.[24] A healthy endothelium is responsible for the production of vasodilators; however this function becomes impaired when the endothelium is injured (e.g., by cigarette smoke or toxic compounds found in e-cigarettes) leading to an imbalance between vasoconstrictors and vasodilators.[24] The damaged cells from the endothelium must be replaced in order to maintain vascular tone, an ability that is reduced in users of e-cigarettes.[24] Platelet activation, coagulation cascade stimulation, and impairment of anticoagulative fibrinolysis leads to vascular disease.[24]
Tooth discoloration
Little evidence is present for the exact mechanisms of how tobacco and nicotine products may discolor teeth.[519] Cigarette smoke considerably impacts the color stability of dental composites, the existing evidence indicates.[520] Although data is limited, e-cigarettes induce a decrease in color variation of dental composites compared to cigarette smoke.[520] There is some evidence to suggest that the e‐liquid composition has some influence on staining.[519] Repolishing or whitening procedures can help with the changes in color to dental composites caused by vaping.[520]
Researchers used spectrophotometry to compare enamel specimens after exposure to e-liquid aerosol according to flavor and nicotine content and found discoloration of enamel in vitro.[320] The chemical substances used to flavor e-liquids, such as menthol, may be the reason behind the color alteration of enamel.[320] A 2020 study reported that exposure to e-cigarettes produced discoloration levels on prosthodontic materials that was similar to that associated with the smoking of tobacco products.[320] In their study, which included ceramics and resin materials with different surface properties, discoloration caused by both e-cigarettes and conventional tobacco cigarettes was below clinically perceptible levels for ceramic materials but was visually perceptible for composite resins.[320]
Although the effect of e-cigarettes on tooth color may be less pronounced than that of traditional cigarettes, long-term, high-dose exposure to e-cigarettes does cause tooth discoloration.[320] The rate of color change varies between natural tooth enamel and restoration materials composed of resin or ceramics.[320] The rate of color change may also be affected by the brand and flavor of the e-liquid.[320]
Aerosol
Composition
The chemical composition of the electronic cigarette aerosol varies significantly across and within brands.[note 10][90] Limited data exists regarding their chemistry.[90] The aerosol of e-cigarettes is generated when the e-liquid comes in contact with a coil heated to a temperature of roughly 100–250 °C (212–482 °F) within a chamber, which is thought to cause pyrolysis of the e-liquid and could also lead to decomposition of other liquid ingredients.[note 11][77] The aerosol (mist[79]) produced by an e-cigarette is commonly but inaccurately called vapor.[note 12][90] The e‑cigarette aerosol is absorbed through the lungs, and at this point it rapidly travels through the heart and subsequently delivers nicotine to the brain within a matter of a few seconds.[111] Nicotine in the brain of e-cigarette users is typically between 0.05 and 0.5 μM.[328] The use of an e-cigarette simulates the action of smoking,[76] but without tobacco combustion.[521] The e-cigarette aerosol somewhat resembles cigarette smoke.[262] E-cigarettes do not produce aerosol between puffs.[522] Both smoke and carbon monoxide are not generated,[204] although insignificant quantities of incomplete combustion products are produced.[317]
The e-cigarette aerosol usually contains propylene glycol, glycerin, nicotine, flavors, aroma transporters, and other substances.[note 13][72] The levels of nicotine, tobacco-specific nitrosamines (TSNAs), aldehydes, metals, volatile organic compounds (VOCs), flavors, and tobacco alkaloids in e-cigarette aerosols vary greatly.[90] The yield of chemicals found in the e-cigarette aerosol varies depending on, several factors, including the e-liquid contents, puffing rate, and the battery voltage.[note 14][246] About 250 chemicals have been found in e-cigarette vapors.[523] There is emerging evidence indicating that over a thousand chemicals can be present in the e-liquid and aerosol.[524] There is also a variety of unknown chemicals in the e-cigarette aerosol.[92]
Metal parts of e-cigarettes in contact with the e-liquid can contaminate it with metal particles.[52] Heavy metals and metal nanoparticles have been found in tiny amounts in the e-cigarette aerosol.[note 15][52] Once aerosolized, the ingredients in the e-liquid go through chemical reactions that form new compounds not previously found in the liquid.[78] Many chemicals including carbonyl compounds such as formaldehyde can inadvertently be produced when the nichrome wire (heating element) that touches the e-liquid is heated and chemically reacted with the liquid.[80] Propylene glycol-containing liquids produced the most amounts of carbonyls in e-cigarette vapors.[80] In 2015, e-cigarettes companies attempted to reduce the formation of formaldehyde and metal substances of the e-cigarette vapor by producing an e-liquid in which propylene glycol is replaced by glycerin.[525]
Propylene glycol and glycerin are oxidized to create aldehydes that are also found in cigarette smoke when e-liquids are heated and aerosolized at a voltage higher than 3 V.[90] Depending on the heating temperature, the carcinogens in the e-cigarette aerosol may surpass the levels of cigarette smoke.[78] Reduced voltage e-cigarettes generate very low levels of formaldehyde.[80] Initial studies reported that formaldehyde was formed during the vaping process under high heat conditions.[37] Although some of the more recent e-cigarette devices limit temperature in an attempt to minimize this, multiple reports have documented the formation of acetaldehyde, acrolein, diacetyl, and formaldehyde under a wide range of conditions.[37] As e-cigarette engineering evolves, the later-generation and "hotter" devices could expose users to greater amounts of carcinogens.[81]
Second-hand exposure
After the aerosol is inhaled, it is exhaled.[90] Emissions from e-cigarettes are not comparable to environmental pollution or cigarette smoke as their nature and chemical composition are completely different.[52] The particles are larger, with the mean size being 600 nm in inhaled aerosol and 300 nm in exhaled aerosol.[79] The exhaled aerosol particle concentration is 5 times lower from an e-cigarette than from a traditional cigarette.[44] The density of particles in the e-cigarette vapor is lower than in cigarette smoke by a factor of between 6 and 880 times lower.[52]
For particulate matter emissions, e-cigarettes slightly exceeded the World Health Organization guidelines, but emissions were 15 times less than traditional cigarette use.[245] In January 2014, the International Union Against Tuberculosis and Lung Disease stated "Adverse health effects for exposed third parties (second-hand exposure) cannot be excluded because the use of electronic cigarettes leads to emission of fine and ultrafine inhalable liquid particles, nicotine and cancer-causing substances into indoor air."[526] The dense vapor consists of liquid sub-micron droplets.[527] Each e-cigarette company generates different amounts of heating power.[360] Substantial levels of particulate matter with a diameter of 2.5 μm are exhaled by vapers.[225] Estimates indicate that more than 70% of inhaled e-cigarette aerosols are eventually exhaled, which may cause second-hand exposures.[94]

Since e-cigarettes have not been widely used long enough for evaluation, the long-term health effects from the second-hand vapor are not known.[43] The short-term health effects from the second-hand vapor is also not known.[93] There is insufficient data to determine the impact on public health from e-cigarettes.[388] The potential harm to bystanders from e-cigarettes is unknown.[529] This is because no long-term data is available.[72] There are limited information on the health effects for children inhaling second-hand vapor.[236] Long-term effects for children inhaling second-hand vapor is not known.[236] Vaping has quickly gained public awareness with greater use among adolescents and adults, resulting in greater inhaled second-hand vapor for adolescents, children, and infants.[236] Second-hand vapor does vary depending on the e-liquid, the device and in the way it is used.[530] There is an array in e-cigarette designs, which has an impact on the amounts of ingredients being exposed to non-users.[225] Heavy advertising and promotion included the assertion that vaping would present little risk to bystanders.[531] E-cigarettes are marketed as "free of primary and second-hand smoke risk" due to no carbon monoxide or tar is expected to be generated during use.[431] However, there is a concern for the health impact of nicotine and other ingredients.[431] Exposure to second-hand vapor may be common.[236] Concerns exist that the increased rates of e-cigarette users who have never smoked could cause harms to public health from the increased nicotine addiction.[207] The growing experimentation with vaping among people under that age of 18 is especially concerning in respect to public health.[220] Ethical concerns arise from possibly vulnerable bystanders being exposed to the not yet known health effects of second-hand vapor.[207] Especially compared to the adverse effects of traditional cigarettes, the overall safety of e-cigarettes is not likely to justify significant public health concerns.[207] Overall, there is a possibility they may greatly harm the public's health.[212] Vaping in areas where smoking is banned indoors could be a move in the wrong direction for public health when considering air quality in addition to being unfavorable for an individual who may have quit nicotine use if they did not vape.[356] Some of the few studies examining the effects on health shown that being exposed to e-cigarette vapor may produce biological effects.[43]

Some non-users have reported adverse effects from the second-hand vapor.[174] Second-hand vapor exhaled into the air by e-cigarette users can expose others to potentially harmful chemicals.[528] Vaping exposes non-users to particulate matter with a diameter of 2.5 μm, which poses health risks to non-users.[225] E-cigarettes produce propylene glycol aerosols at levels known to cause eye and respiratory irritation to non-users.[209] A 2014 study demonstrated that non-smokers living with vaping device users were exposed to nicotine.[446] A 2015 study concluded that, for indirect exposure, two chemicals—nicotine and propylene glycol—exceeded California Environmental Protection Agency exposure level standards for noncarcinogenic health effects.[209] Second-hand exposure to vaping can increase the possibility of experiencing an asthma attack.[532] Among youth with asthma, exposure to second-hand vapors resulted in an increased risk of exacerbating their condition.[533] A 2016 Florida Youth Tobacco survey showed that among students with a self-reported diagnosis of asthma, second-hand e-cigarette aerosol exposure was associated with higher risk of asthma attacks in the past 12 months.[459]
Between January 2012 and December 2014, the US FDA noted 35 adverse effect reports regarding second-hand vaping exposure.[534] A 2016 survey found a sizable percentage of middle and high school students were exposed to second-hand e-cigarette vapors.[225] It is recommended that adolescents stay away from being exposed to second-hand e-cigarette vapor.[232] A 2016 study showed that most participated coughed right away and briefly following a single exposure to e-cigarette vapor, while after 15 minutes it induced a diminished cough reflex sensitivity in healthy never-smokers.[535] Nicotine-free e-cigarette vapor did not have this effect.[535] The health effects of passive exposure to e-cigarettes with no nicotine, as well as the extent of exposure to these products, have just begun to be studied in 2016.[209] E-cigarettes that do not contain nicotine generate hazardous vapors[536] and could still present a risk to non-users.[537] A 2014 study found greater amounts of particulates with e-cigarette emissions from e-liquids that were free from nicotine compared with those made with nicotine.[324] This study indicates that flavored, nicotine-free e-cigarette vapor may still be harmful to non-users.[324] Research has not evaluated whether non-users can have allergic reactions from nut potential allergens in e-cigarette aerosol.[209]
Since e-cigarettes do not burn tobacco, no side-stream smoke or any cigarette smoke is produced.[43] Only what is exhaled by e-cigarettes users enters the surrounding air.[72] It is not clear how much of inhaled e-cigarette aerosol is exhaled into the environment where non-users can be exposed.[209] Exhaled vapor consists of nicotine and some other particles, primarily consisting of propylene glycol, glycerin, flavors, and aroma transporters.[72] Bystanders are exposed to these particles from exhaled e-cigarette vapor.[43] Clean air is safer than e-cigarette vapor.[538] A mixture of harmful substances, particularly nicotine, ultrafine particles, and volatile organic compounds can be exhaled into the air.[397] The liquid particles condenses into a viewable fog.[79] The e-cigarette vapor is in the air for a short time, with a half-life of about 10 seconds; traditional cigarette smoke is in the air 100 times longer.[79] This is because of fast revaporization at room temperature.[79]
A 2017 review found that the "rapid production of new products has made it hard for the concerned stakeholders such as researchers in the public health field and policy makers to ensure that the products introduced to the public are safe for the users and non-users who are involuntarily exposed to e-cigarette vapors."[446] Little research exists on the exhaled particles, nicotine, and cancer-promoting chemicals into indoor air.[413] Concern exists that the exhaled e-cigarette vapor may be inhaled by bystanders, particularly indoors.[94] People living with e‐cigarette users had increased salivary concentrations of cotinine.[225] A small number of e-cigarette studies exist on the effect of indoor air quality done on human test subjects in natural settings.[446] Though, the available studies presented conflicting scientific evidence on the exact exposure from the e-cigarette vapor contents which may be a result of the contrasting methodology used during the research process.[446] Vaping can expose non-users to aldehydes and it reduced indoor air quality due to their released aldehydes.[225] Since e-cigarettes involve an aerosolization process, it is suggested that no meaningful amounts of carbon monoxide are emitted.[96] Thus, cardiocirculatory effects caused by carbon monoxide are not likely.[96] However, in an experimental study, e-cigarettes increased levels of carcinogenic polycyclic aromatic hydrocarbons in the surrounding air.[96] Passive inhalation of vapor might have significant adverse effects.[201] Though, e-cigarettes exposes non-users to nicotine but not to tobacco-related combustion toxicants.[201] Exposure to e-cigarette vapor can reduce lung function.[539]
E-cigarettes do pollute the air in the form of exhaled mainstream aerosol from people using e-cigarettes.[158] Nicotine, ultrafine particles, and products of heating propylene glycol and glycerin are increased in the air where e-cigarettes are being used, although, as expected, at lower levels than produced by smoking the same number of traditional cigarettes.[158] As with traditional cigarettes, however, when several people are using e-cigarettes indoors at the same time, the air can become polluted.[158] For example, levels of fine particulate matter (PM2.5) in a large hotel event room (4,023m3) increased from 2–3 μg/m3 to as high as 819 μg/m3 (interquartile range: 761–975 μg/m3) when 59–86 people were using e-cigarettes.[158] This level is comparable to a very (conventional tobacco) smoky bar or casino and dramatically exceeds the US Environmental Protection Agency annual time-weighted standard for PM2.5 of 12 μg/m3.[158]
Evidence has also shown that bystanders absorb nicotine when people around them use e-cigarettes at levels comparable with exposure to traditional cigarette second-hand smoke.[158] In a study of non-smokers living with nicotine e-cigarette users, those living with traditional cigarette smokers, or those living in homes where no one used either product, cotinine (a metabolite of nicotine) levels in bystanders' urine were significantly elevated in both the people exposed to second-hand e-cigarette aerosol and those exposed to second-hand tobacco smoke compared with people living in aerosol- and smoker-free homes.[158] Interestingly, the levels of elevated urinary cotinine in the two exposed groups were not significantly different (although the passive smokers had higher point estimates), despite the fact that the increase in air pollution in the smokers' homes was much higher than in the e-cigarette users' homes (geometric mean air nicotine concentrations of 0.13 μg/m3 in e-cigarette users' homes, 0.74 μg/m3 in smokers' homes, and 0.02 μg/m3 in the control homes).[158]
On the basis of emerging evidence, in 2014 the American Industrial Hygiene Association concluded that "e-cigarettes are not emission-free and that their pollutants could be of health concern for users and those who are exposed secondhand....[T]heir use in the indoor environment should be restricted, consistent with current smoking bans, until and unless research documents that they will not significantly increase the risk of adverse health effects to room occupants."[158] Similarly, in 2016 the American Society of Heating, Refrigeration and Air-Conditioning Engineers (ASHRAE) updated its standard for "Ventilation for Acceptable Indoor Air Quality" to incorporate emissions from e-cigarettes into the definition of "environmental tobacco smoke," which is incompatible with acceptable indoor air quality.[158] As of April 2017[update], 12 US states and 615 localities had prohibited the use of e-cigarettes in venues in which traditional cigarette smoking was prohibited.[158]
There are benefits to banning vaping indoors in public and working areas, since there is a potential harm of renormalizing tobacco use in smoke-free areas, in addition to, vaping may result in spread of nicotine and other chemicals indoors.[540] E-cigarettes used in indoor environments can put at risk non-smokers to elevated levels of nicotine and aerosol emissions.[44] Non-smokers exposed to e-cigarette aerosol produced by a machine and pumped into a room were found to have detectable levels of the nicotine metabolite cotinine in their blood.[43] The same study stated that 80% of nicotine is normally absorbed by the user, so these results may be higher than in actual second-hand exposure.[43] Of particularly noteworthy is the problem of vaping in small rooms, in close proximity to other people, and around children.[541]

The available evidence demonstrates that the e-cigarette vapor emitted from e-cigarettes is not just "harmless water vapor" as is repeatedly stated in the advertising of e-cigarettes, and they can cause indoor air pollution.[43] A 2014 practice guideline by NPS MedicineWise states, "Although data on health effects of passive vapour are currently lacking, the risks are argued to be small, but claims that e-cigarettes emit only water vapour are nevertheless incorrect. Serum cotinine levels (a metabolite of nicotine) have been found to be similar in bystanders exposed to either e-cigarette vapour or cigarette smoke."[542] A 2015 California Department of Public Health report states that "Mainstream and secondhand e-cigarette aerosol has been found to contain at least ten chemicals that are on California's Proposition 65 list of chemicals known to cause cancer, birth defects, or other reproductive harm."[543] These are acetaldehyde, benzene, cadmium, formaldehyde, isoprene, lead, nickel, nicotine, N-nitrosonornicotine, and toluene.[425]
A white paper published in 2014 by the American Industrial Hygiene Association concluded e-cigarettes emit airborne contaminants that may be inhaled by the user and those nearby.[455] Due to this possible risk, they urged restriction of their use indoors, similar to smoking bans, until research has shown the aerosol does not significantly harm others in the area.[455] A 2014 review suggested that the levels of inhaled contaminants from the e-cigarette vapor are not of significant health concern for human exposures by the standards used in workplaces to ensure safety.[145] The compounds that are present, are mostly below 1% of the corresponding levels permissible by workplace safety standards.[145] But workplace safety standards do not recognize exposure to certain vulnerable groups such as people with medical ailments, children, and infants who may be exposed to second-hand vapor.[43] Some chemicals from e-cigarette exposures could surpass workplace safety standards.[131] E-cigarette convention studies indicate that second-hand e-cigarette vapor may be significant for workers in conventions where there are people using e-cigarettes, particularly those who encounter the vapor in more than one of these events.[544] Exposure studies suggest that e-cigarette use in indoor areas is higher than the smoke-free level put forth by the US Surgeon General and the WHO Framework Convention on Tobacco Control.[544] The use of e-cigarettes in a smoke-free area could expose non-users to toxicants.[545]
Second-hand vapor exposes bystanders to numerous pollutants at amounts higher than background air.[537] A 2016 World Health Organization report stated that "While some argue that exposure to SHA [second-hand aerosol] is unlikely to cause significant health risks, they concede that SHA can be deleterious to bystanders with some respiratory pre-conditions. It is nevertheless reasonable to assume that the increased concentration of toxicants from SHA over background [air] levels poses an increased risk for the health of all bystanders."[546] The exhaled vapor may involuntarily expose bystanders to toxicants that are in the range as some cigarettes.[55] This is due to the fact that some vaping devices generate toxicants in the range as some cigarettes do.[55] The report stated that "it is unknown if the increased exposure to toxicants and particles in exhaled aerosol will lead to an increased risk of disease and death among bystanders."[55] The British Medical Association (BMA) reported in 2013 that there are "concerns that the use of e-cigarettes could threaten the norm of not smoking in public places and workplaces."[547] Several medical organizations advocate that vaping be banned in public places and workplaces.[356] A 2014 review found it is safe to infer that their effects on bystanders are minimal in comparison to traditional cigarettes.[52] E-cigarette vapor has notably fewer toxicants than cigarette smoke.[43]
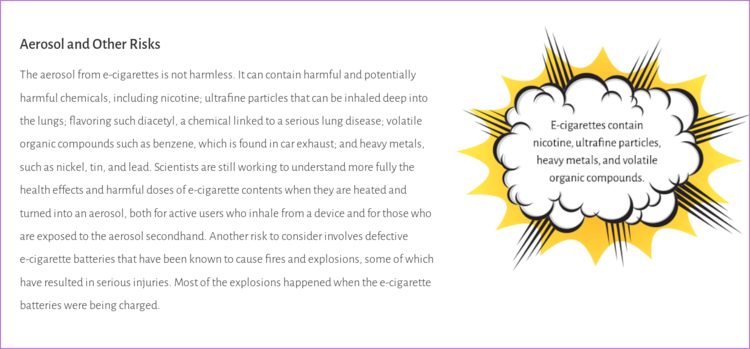
Third-hand exposure
E‐cigarettes can be unsafe to non-users via third-hand exposure, including children, pregnant women, casino employees, housekeeping employees, and vulnerable groups.[225] E-cigarette use by a parent might lead to inadvertent health risks to offspring.[385] E-cigarettes pose many safety concerns to children.[385] For example, indoor surfaces can accumulate nicotine where e-cigarettes were used, which may be inhaled by children, particularly youngsters, long after they were used.[385] A policy statement by the American Association for Cancer Research and the American Society of Clinical Oncology has reported that "Third-hand exposure occurs when nicotine and other chemicals from second-hand aerosol deposit on surfaces, exposing people through touch, ingestion, and inhalation".[73] A 2015 PHE report stated the amount of nicotine deposited was low and that an infant would have to lick 30 square meters to be exposed to 1 mg of nicotine.[549] There are no published studies of third-hand exposure from e-cigarettes, however initial data suggests that nicotine from e-cigarettes may stick to surfaces and would be hard to remove.[73] The extent of third-hand contamination indoors from e-cigarettes in real-world settings has not been established but would be of particular concern for children living in homes of e-cigarette users, as they spend more time indoors, are in proximity to and engage in greater activity in areas where dust collects and may be resuspended (e.g., carpets on the floor), and insert nonfood items in their mouths more frequently.[209]
Effects on pregnancy and infants
Concerns exist regarding pregnant women exposure to e-cigarette vapor through direct use or via exhaled vapor.[43] Vaping during pregnancy is not recommended.[551] It is recommended that pregnant women stay away from being exposed to second-hand e-cigarette vapor.[232] No evidence have shown that e-cigarettes are safe to use for pregnant women.[551] No amount of nicotine is safe for pregnant women.[551] There is an increasing amount of research on the negative effects of nicotine on prenatal brain development.[44] Some earlier research suggested that e-cigarette use is less risky to pregnancy outcomes, but more newer research refute these findings.[552]
The use of both cigarettes and e-cigarettes during pregnancy may lead to higher nicotine exposure.[553] E-cigarette use during pregnancy can be harmful to the fetus.[554] Nicotine-free e-cigarette aerosols may cause harm to the fetus.[459] There is growing evidence that exposure of pregnant women to e-cigarettes may impair placental function and may result in fetal structural abnormalities.[459] Specifically, this may cause physio-pathologic changes in the developing lung, which in turn may impair respiratory health later in life.[459] Nicotine accumulates in the fetus because it goes through the placenta.[171] Nicotine has been found in placental tissue as early as seven weeks of embryonic gestation, and nicotine concentrations are higher in fetal fluids than in maternal fluids.[209] It also attaches to nicotinic acetylcholine receptors in the fetus brain.[232] When the brain is being developed, activating nicotinic acetylcholine receptors by nicotine can result in long-term developmental turmoil.[232] Nicotine can induce a genotoxic effect in fetal cells.[376] Nicotine is harmful to the growing fetus.[555] It seems to be more harmful to the growing fetus during the latter stage of pregnancy.[551] Exposure of pregnant females to nicotine can lead to an altered inflammatory environment during gestation, which may have consequences on fetal hematopoiesis.[556] Moreover, it is yet unknown whether this is caused directly by nicotine in the fetal environment or by passage of maternal nicotine-induced inflammatory cytokines to the fetus during development.[556] It is unknown whether nicotine leads to transient or persisting alterations in developmental hematopoiesis.[556]
As of 2021[update], the risks of vaping e-cigarettes during pregnancy are largely unknown.[459] As of 2015[update], the long-term issues of e-cigarettes on both mother and unborn baby are unknown.[557] Being exposed over a long period of time to e-cigarette vapors may raise the possibility of unfavorable reproductive outcomes.[558] Although there is a scarcity of studies examining the birth results in mothers who vape nicotine while pregnant, a 2015 study in the UK found a noticeable increase in respiratory anomalies in mothers who used nicotine replacement products in contrast to mother who did not use these products.[559] The rate of e-cigarette use among pregnant adolescents is unknown, but the effects of nicotine and the potential for harm by other e-cigarette toxicants indicate that the use of e-cigarettes is a fetal risk factor among pregnant adolescent girls.[209] Prenatal nicotine exposure is associated with adverse effects on the growing fetus, including effects to normal growth of the endocrine, reproductive, respiratory, cardiovascular, and neurologic systems.[551] Prenatal nicotine exposure has been associated with dysregulation of catecholaminergic, serotonergic, and other neurotransmitter systems.[209] Prenatal nicotine exposure is associated with lower birth weights compared to other infants,[551] preterm birth,[485] stillbirth,[485] sudden infant death syndrome, and alterations to normal brain development.[551] When birth weight is normal there still can be damage.[232] Nicotine may result in premature birth, miscarriage, fetal neurotoxicity, and fetal lung development issues.[157] Nicotine delivered by e-cigarettes during pregnancy can result in multiple adverse consequences, including sudden infant death syndrome, and could result in altered corpus callosum and deficits in auditory processing.[209] Prenatal nicotine exposure is associated with asthma and wheezing which may continue into adulthood.[551] Gestational age nicotine exposure is associated with many neurological deficits.[551] Prenatal exposure has been associated with obesity, diabetes, high cholesterol, and high blood pressure in minors.[413] Prenatal nicotine exposure in females may lead toward early menarche.[551] An infant was born with necrotizing enterocolitis due to e-cigarette use during pregnancy.[121] Evidence from animal studies indicate that being exposed to second-hand vapor containing nicotine during pregnancy may impede fetal lung development.[259] Vaping during pregnancy resulted in a reduction in lung volume.[379] Vaping during pregnancy could impact lung pathophysiology as well as function in infants.[139] Low amounts of aldehydes can still be a health concern among pregnant women.[225]
Some studies suggest that e-cigarette exposure not only has a negative impact on one's reproductive health but also on the offspring when exposed to e-cigarette components in utero.[101] There was a trend towards lower fertility in male offspring and lower body weight and length in all offspring.[101] These findings suggest a hypothetical toxicity of e-cigarette exposure on an in utero developing fetus.[101] Neonatal exposure to e-cigarette induced altered lung growth, weight gain with significant and persistent behavioral alterations.[101] This raises the question of the potential impact of e-cigarettes on non-users that are passively exposed to the vapor during pregnancy.[101]
Dual users (smoking and vaping) in pregnancy have higher odds of giving birth to a small-for-gestational-age child than with exclusive smoking of conventional cigarettes according to two 2019 studies and a 2020 study found higher incidence of birthweight (below 10th percentile) and a higher rate of admission to a neonatal intensive care unit in offspring of dual users than in offspring of exclusive smoking of conventional cigarettes.[114] However, the latter study also found the same birthweight, Apgar score, and gestation at delivery in offspring of dual users as in offspring of exclusive smoking of conventional cigarettes, and another study in 2016 found that dual users had the same (elevated) risk of small-for-gestational-age and preterm birth as exclusive smoking of conventional cigarettes.[114] Furthermore, a very large cohort study in 2021 of young women found a lower but not significantly different fecundability ratio in dual users than in exclusive smoking of conventional cigarettes.[114]
In what way the e-liquid ingredients could affect a fetus is unknown.[560] Several ingredients used in e-liquid has not been studied for safety during pregnancy.[551] Studies examining the cytotoxicity of e-liquid flavorings found toxicity to be greater in undifferentiated embryonic stem cells relative to human pulmonary fibroblasts, raising potential concerns about exposure risks for pregnant women.[207] There are concerns about the health impacts of pediatric exposure to second-hand and third-hand e-cigarette vapor.[74] A 2014 Surgeon General report found "that nicotine adversely affects maternal and fetal health during pregnancy, and that exposure to nicotine during fetal development has lasting adverse consequences for brain development."[73] The belief that e-cigarettes are safer than traditional cigarettes could increase their use in pregnant women.[76] The toxic effects identified with e-cigarette refill liquids on stem cells may be interpreted as embryonic death or birth defects.[76] In a 2020 study, the effects of cinnamon-flavor exposure in Balb/c pregnant mice and their offspring showed that preconception flavor exposure increases lung tissue fraction at birth compared to non-exposed groups, suggesting that cinnamaldehyde may be teratogenic.[448] Since e-cigarettes are not substantiated as cessation tools, may contain nicotine at inconsistent levels and added ingredients that are possibly harmful, to bear with e-cigarettes to be used among pregnant women to decrease smoking puts this group at considerable risk.[385]
Nicotine has been found in breast milk.[561] Infant heart rate and blood pressure fluctuations are linked to higher nicotine levels in breast milk.[561] It is discouraged for pregnant and breastfeeding females to substitute cigarettes with e-cigarettes.[53] It is recommended that females who smoke during pregnancy to quit using cigarettes.[53] There is concern for breastfeeding females using e-cigarettes, due to the lack of data on propylene glycol transferring to breast milk.[79] It is discouraged to use e-cigarettes while breastfeeding infants or young children.[53] The consequences of vaping on infants feeding on breast milk is uncertain.[53]
Environmental impact


There are a range of consequences for the environment surrounding the use of e-cigarettes, such as air quality effects, energy and materials used, issues related to environmentally responsible disposal, and land-use decisions.[541]
There is limited information available on any environmental issues connected to the production, usage, and disposal of e-cigarette models that use cartridges.[95] Studies directly describing environmental exposure to chemicals from e-cigarette waste on minorities and low-income populations are limited.[562] As of 2014[update], no formal studies have been done to evaluate the environmental effects of making or disposing of any part of e-cigarettes including the batteries or nicotine production.[95] As of 2014[update], it is uncertain if the nicotine in e-liquid is United States Pharmacopeia-grade nicotine, a tobacco extract, or synthetic nicotine when questioning the environmental impact of how it is made.[95] It is not clear which manufacturing methods are used to make the nicotine used in e-cigarettes.[95] The emissions from making nicotine could be considerable from manufacturing if not appropriately controlled.[95] Some e-cigarette brands that use cartridges state their products are 'eco-friendly' or 'green', despite the absence of any supporting studies.[95] Some writers contend that such marketing may raise sales and increase e-cigarette interest, particularly among minors.[95]
E-cigarettes that are thrown away that end up in landfills is a rising public health concern.[53] A July 2018–April 2019 garbology study found e-cigarette products composed 19% of the waste from all traditional and electronic tobacco and cannabis products collected at 12 public high schools in the San Francisco Bay Area.[563] It is unclear how many traditional cigarettes are comparable to using one e-cigarette that uses a cartridge for the average user.[95] Information is limited on energy and materials used for production of e-cigarettes versus traditional cigarettes, for comparable use.[95] E-cigarettes can be made manually put together in small factories, or they can be made in automated lines on a much bigger scale.[95] Larger plants will produce greater emissions to the surrounding environment, and thus will have a greater environmental impact.[95] Tobacco factories create toxic nicotine waste from the manufacturing of tobacco products.[564] While cigarettes still comprise almost 90% of all tobacco sales globally as of 2020 (except for South Asia), other tobacco products, especially e-cigarettes, also weigh heavily on the environment.[565] The rise of e-cigarettes in industrialized countries is changing the composition of the environmental harms of tobacco.[565] Because these products are composed of low-value but sophisticated electronics, the environmental costs from manufacturing e-cigarettes may be substantially more severe than cigarettes per unit.[565]
Although some brands have begun recycling services for their e-cigarette cartridges and batteries, the prevalence of recycling is unknown, as is the prevalence of information provided by manufacturers on how to recycle disposable parts.[95] E-cigarettes that are not reusable may contribute to the problem of electronic waste.[96] A 2016 review found "Heavy metals may be released, if disposable ECs are disposed into the environment."[246] E-cigarettes batteries contaminate the land and water and may release lead into the environment.[53] E-liquids that are not entirely used up could contain nicotine and heavy metals.[53] This is another risk for the environment.[53] Littered or improperly discarded e-cigarettes can leach heavy metals, battery acids, and organic chemicals, potentially affecting humans and other organisms.[562] Small components (e.g., pods, cartridges) may be eaten by birds and other animals.[562] Since the majority of e-cigarettes are reusable they are possibly more environmentally friendly than using single-use devices.[566] Compared to traditional cigarettes, e-cigarettes do not create litter in the form of discarded cigarette butts.[566] Tobacco cigarette waste can be seen on city sidewalks and public beaches.[567] Traditional cigarettes tend to end up in the ocean where they cause pollution.[566]
According to the US FDA, e-cigarettes, including rechargeable batteries and the cartridges and bottles that contain e-liquids (liquid nicotine mixtures), can pose a threat to the environment if they are not disposed of properly.[568] E-cigarette and e-liquid waste should not be thrown in the regular trash or flushed down a sink.[568] Instead, these items should be taken safely to a hazardous waste facility, the US FDA states.[568] Improper disposal of e-cigarettes and e-liquid products can hurt the environment.[568] If thrown in the trash or flushed into the sewer system, the nicotine solution in an e-liquid product can seep into the ground or water and become a danger for wildlife and humans.[568] As e-cigarette batteries degrade, the compounds in them can also seep into nearby water.[568] Additionally, lithium ion batteries have been linked to explosions in recycling trucks when batteries are not properly disposed of.[568] As sales of e-cigarettes have increased significantly in the past few years leading up to 2020, institutions face a burden to dispose of e-cigarette waste in a way that protects the environment.[568] Schools face challenges with waste littered by students on school property.[568] According to the Minnesota Pollution Control Agency, products that contain nicotine including e-liquids and e-cigarettes, pose a threat to the environment if they are not disarded of properly.[569]
E-cigarettes made in different countries are manufactured according to the standards of the manufacturer’s country, and do not always conform to laws for exposures to metals and other toxicants in the countries they are used.[565] In the US, e-cigarettes originally were to be included as drug-delivery devices under the US FDA, which would have required much stricter product regulation.[565] However, a 2010 suit overturned this designation.[565] The 2016 FDA Deeming Rule aimed to place e-cigarettes under a 2007 regulatory cut-off which would require extensive testing of e-cigarettes if they wished to remain on the market.[565] As the deadline for this requirement has been postponed from 2018 to 2022, e-cigarette manufactures are free to produce and sell devices with minimal oversight by health or environmental regulatory institutions.[565] In the UK, while e-cigarettes disposal and reclamation must adhere to the Waste Electrical and Electronic Equipment Regulations, requiring companies to receive and process electronic waste, the arduous process of sending these products back to manufactures and having to pack and pay for postage to responsibly return these products likely limits the effectiveness of such consumer-side responsibility to unknown efficacy.[565]
The chemical content of e-liquids and the construction of e-cigarettes vary widely—from disposable single-use "cig-a-like" products resembling cigarettes, to refillable "vape pens," to "mods" and "tanks."[565] In 2018, the best-selling device in the US was the Juul cartridge-based or "pod" e-cigarette.[565] While the USB stick-shaped device is not single-use, its hard plastic e-juice cartridges are.[565] Because of the overwhelming diversity of products, no blanket assertion on the environmental impact of these products is possible.[565] Introducing new classes of plastics, metals, cartridges, lithium-ion batteries, and concentrated nicotine solutions, however, involves significantly more environmentally intensive manufacturing processes than products that are primarily made of plant material and plastic filters, as combustible cigarettes are.[565]
Ibis World, an industry market research company, predicts that "the [traditional] Cigarette and Tobacco Product Manufacturing industry is in the declining stage of its life cycle".[565] They note, however, that the industry will resist this decline through expansion into e-cigarettes and other electronic nicotine delivery devices.[565]
The tobacco industry is aware of the new scope of environmental harms e-cigarettes pose.[565] Philip Morris International discussed the "need to manage new areas of impact due to the increasing use of electronics and batteries in our products".[565] As tobacco companies increasingly are selling electronic smoking devices, they acknowledge that "while we embed new processes, the efficiency of our energy and water use may worsen until both knowledge and economies of scale improve".[565] Philip Morris International's Lifecycle Analysis performed for e-cigarettes and other so-called reduced-risk products (RRPs) "highlighted the impact that RRPs will have in [their ecological] footprint and plans in product development, manufacturing, distribution and rest of value chain have been implemented to mitigate their impact in our footprint”.[565]
Fundamentally, the tobacco industry has been aware of "cradle to grave" extended-producer responsibility manufacturing since at least as early as 1991, and has nonetheless refrained from implementing practices that could reduce the waste from their products, both in terms of production and disposal.[565] Conventional cigarette filters, for instance, have been proven to do more harm than good in terms of health, and these unnecessary appendages to cigarettes, originally developed in the 1950's to assuage growing fears over the health harms of cigarettes, directly harm the environment in their material production and disposal.[565] Based on reviewing industry documents, it does not appear as if any cradle-to-grave industrial ecology has been undertaken to minimize the amount of ecological impact of e-cigarette manufacture and disposal.[565]
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3995274/#s1title Create Figure 1
History of e-cigarette research and commentary
For over 50 years, there has been a compelling assemblance of irrefutable evidence demonstrating that smoking cigarettes leads to disease in nearly every human organ.[204] At least as early as the 1950s the tobacco industry has intentionally mislead the public regarding the health risks of smoking.[36] When more evidence demonstrating a link between smoking and cancer was starting to become more apparent, the tobacco industry created the Tobacco Industry Research Committee in 1953, which was a group devoted to attacking scholarly research.[36] While millions of people were dying, it was hard to show in the early 1960s the true cost of tobacco on health worldwide, as the proof needed decades to arise fully.[204] Confronted with the undeniable evidence of the deaths caused by tobacco products, the tobacco industry devised an extensive and thorough approach to maintain and grow their market.[204] Fabricating uncertainty and controversy surrounding the health impacts of tobacco and pushing disingenuously less risky smoking products were bedrocks of this approach.[204] Big Tobacco has partnered with firms, including the Electronic Cigarette Association, Consumer Advocates for Smoke-Free Alternatives Association, and Vapers International, Inc., that were set up to promote the use of e-cigarettes.[44] These factions, coupled with other vested interested parties, have had taken steps to stall or abolish legislation targeted at curbing the sales and the use of e-cigarettes.[44] Methodical e-cigarette industry groups were partly responsible for the initial surge in the sales of these products.[570]
While cigarettes have been the leading source of tobacco consumption, a diverse range and usage of more recently created products had been accelerating by 2021.[571] These newly created tobacco, nicotine, and other aerosolized products were perpetually being introduced into the marketplace and were vigorously being pushed both in affluent countries where cigarette consumption is descending and where people are able to pay for the latest products, in addition to less affluent countries, thus sidestepping laws prohibiting tobacco advertising or the importation of nicotine vaping devices.[571] Modern advancements in nicotine delivery systems sparked the creation of e-cigarettes.[352] With the onset and rapid growth of e-cigarettes, this has challenged people in the scientific, and public health circles, because they have to make regulatory decisions in accordance with public health, in spite of the lack of evidence.[204] There has been an escalation in their use in the decade prior to 2020, which has spurred the medical community to examine their potential health effects.[572] As a consequence of past lessons learned from Big Tobacco companies, the medical community is suspicious of e-cigarettes and has routinely advised against their use.[155] Many physicians fear that patients who vape are merely substituting one form of nicotine addiction for another.[155]
Cigarette smoking accelerated in the late 19th and early 20th centuries in tandem with the growth of mass production technologies and advertising.[37] However, it was not until the 1930s that statisticians noted increased cancer mortality rates and thoracic surgeons reported an increase in pneumonectomy to remove lung cancers.[37] Three decades later the landmark 1964 US Surgeon General's Report causally attributed lung cancer to cigarette smoking, and four decades after this the tobacco companies were defeated in the US court system on racketeering charges that they systematically deceived the public in the pursuit of profits.[37] The lesson from smoking in the 20th "cigarette" century is that it took decades to show that addictive, heavily marketed inhaled tobacco products caused lung disease.[37] On April 15, 1994, senior executives of the seven major tobacco companies in the US spoke before the US Congress.[573] Each one testified that they believe nicotine is not addictive.[573] This was one of the more peculiar moments in the history of tobacco politics that occurred in Washington, D.C., Philip J. Hilts stated.[574] Research that divulged monetary support from the tobacco industry had increased rates of endorsing e-cigarette use as a quitting smoking-aid.[575] Moreover, industry funding is strongly associated with finding no harm of e-cigarettes, compared with studies without a potential conflict of interest.[37] Researchers who had ties to the tobacco industry or were funded by tobacco companies were less likely to report the harmful effects of using e-cigarettes.[393]
In the years before the advent of electronic nicotine delivery systems technology, various public health measures made significant progress in tobacco control yielding a 6.9% reduction in smoking across the US population from 2005 to 2017.[213] Smoking among high-school students in the US had started to decline significantly, from 28% in 1996–1997 to 15.8% in 2011 to 7.6% in 2017.[203] This decline—a true public health triumph—may be attributed to multiple tobacco control measures, including restrictions on tobacco company advertising, promotions and sponsorship, taxation of tobacco products, clean indoor air laws, banning of flavorings in cigarettes (except menthol), and decreased access of cigarettes to teenagers through the adoption of local and statewide Tobacco 21 legislation (raising the legal age of sale from 18 to 21).[203] Keeping in mind the economic and social burden exacted by smoking-related diseases, the US federal government had enacted various laws to make the sale of conventional tobacco products more difficult especially for the younger generation.[213] However, rapid and unchecked increase in e-cigarette use has once again threatened to endanger the health of youth through nicotine addiction and vaping-related disease.[213] The National Youth Tobacco Survey held jointly by the US FDA and the Centers for Disease Control and Prevention shows that around 3.6 million students (both middle and high school) were using e-cigarettes in 2018, up from 2.1 million in 2017.[213] In the past decades, attitudes have changed: teenagers recognize the dangers of smoking and no longer find it attractive or "cool."[203] By contrast, e-cigarettes, now used by over 20% of high-school students as of 2018, are not viewed by adolescents as dangerous or even comparable to cigarettes.[203]
It is well known the tobacco industry has funded research to call into question the evidence of the dangers of tobacco consumption.[135] Research paid for by the tobacco industry supports ideas sympathetic to the tobacco industry.[135] This includes tobacco industry affiliated studies in favor of nicotine's assistance with Alzheimer's disease, neuroenhancement, and ulcerative colitis.[135] In the late 1980s, researchers without ties to the tobacco industry gradually became increasingly critical of tobacco-affiliated investigators and their researchers.[504] This culminated in the critical analysis of the role of the tobacco industry as one of the forefront funders of medical research and the negatives of this in the 1990s.[504] At this time, tobacco-funded researchers were heavily scrutinized, as were their research proposals and conclusions.[504] In the early 2000s, the tobacco industry cultivated a new image and proposed transparency in its involvement in scientific research in the context of an increasingly critical public.[504] Still, a major study of the time concluded that tobacco industry research revolved around projecting a positive corporate image above public health policies and that the escalation in transparency may be a part of this agenda.[504] Initial hopes that e-cigarettes would be both a less toxic competitor to conventional cigarettes and a help to people who attempt to quit smoking cigarettes have not translated into real-world positive effects.[158] Instead, e-cigarettes have simply become another class of tobacco products that are maintaining and expanding the tobacco epidemic.[158]
—Stanton A. Glantz and David W. Bareham, Annual Review of Public Health[158]
Although their initial inception dates back to 1963, the design of e-cigarettes in 2003 by Hon Lik, has spurred increasing global sales, which now show profits worth billions of dollars.[541] Traditionally dominated by small start-up companies, the e-cigarette market has experienced rapid growth and transition, and more recently as of 2019, large manufacturers and transnational tobacco companies have come to dominate the market.[576] Major tobacco companies have entered the vaping industry by either acquiring e-cigarette companies and brands or developing their own products.[576] As the major tobacco companies have moved into, and increasingly dominated, the e-cigarette market, they are dominating the political and policy-making environments just as they have in conventional cigarette policy making.[158] Major tobacco companies now involved in the vaping industry include British American Tobacco, Imperial Brands, the Altria Group, Reynolds American, Philip Morris International, and Japan Tobacco International.[576] These companies have benefited from large advertising and marketing budgets, which enable promotion across the World Wide Web.[576] Heavily promoted by the industry, with fierce marketing campaigns targeted mainly at the most socially vulnerable and easily influenced populations, such as adolescents and young adults, they are growing fast in popularity, as of 2019.[483] One of the selling arguments for using e-cigarettes that they provide assistance for people to stop smoking and abolish nicotine addiction may be a lie.[577] This is because the starting age for e-cigarette use is typically lower than that of traditional cigarettes and may result in more regular use.[577] As cigarette companies have acquired the largest e-cigarette brands, they currently benefit from a dual market of smokers and e-cigarette users while simultaneously presenting themselves as agents of harm reduction.[207] This raises concerns about the appropriateness of endorsing a product that directly profits the tobacco industry.[207] Regardless of their industry ownership, e-cigarette companies have a vested interest in maximizing the number of long-term product users.[207] Thus, the ethical onus falls on governments to restrict the influence of industry through appropriate regulations targeting product manufacturing, availability, and use, devised in light of public health interests.[207]
In recent years leading up to 2022, the tobacco industry has been pushing a narrative that their newer lines of products-including electronic nicotine delivery devices-are offered in part to meet a social responsibility of providing potentially reduced-harm choices to their consumers.[578] While some of the newer tobacco products might potentially be less harmful than combustible tobacco products, there is also significant deviation from the very concept of harm reduction when it is used for such a conspicuously commercialized purpose.[578] The framing of commercialized tobacco harm reduction as a mere consumer preference by the industry is not clearly consistent with the core principles of harm reduction, let alone the human right to health and the highest attainable level of health.[578] The industry's continued marketing of combustible products alongside their "potentially less harmful" products, and preference that their non-combustible products be regulated less strictly than cigarettes and cigars, adulterates the public health principles of harm reduction and undermines the right to health.[578] The tobacco industry itself has made clear that whatever benefit its "next-generation" products may provide, it coexists with the continued profit-making from manufacture, distribution, and sale of combustible tobacco products to consumers, with minimal if any marketing restrictions including on who may purchase these allegedly less harmful goods (e.g., non-smokers and first-time users).[578] The tobacco industry wants to continue to sell harmful products directly to consumers while enjoying the social and political capital that may accrue from also selling potentially less—but still—harmful products directly to those same, and new, consumers.[578]
The US FDA in 2009 analyzed e-liquid cartridge samples[82] from two brands of e-cigarettes,[579] which were NJOY and Smoking Everywhere.[103] Their analysis of the e-cigarette samples showed that the products contained detectable levels of known carcinogens and toxic chemicals to which users could potentially be exposed.[580] Diethylene glycol was detected in one cartridge at approximately 1%.[580] Diethylene glycol, an ingredient used in antifreeze, is toxic to humans.[580] The source of the diethylene glycol contamination is not clear but could reflect the use of non-pharmaceutical grade propylene glycol.[155] On July 22, 2009,[579] the FDA warned that e-cigarettes may present a health risk.[44] On October 6, 2022 in a press release, the US FDA Commissioner Robert M. Califf stated, "The FDA remains deeply concerned about e-cigarette use among our nation’s youth. It’s clear that we still have a serious public health problem that threatens the years of progress we have made combatting youth tobacco product use. We cannot and will not let our guard down on this issue. The FDA remains steadfast in its commitment to using the full range of our authorities to address youth e-cigarette use head-on."[581]
Their short as well as their long-term consequences, including their potential carcinogenicity, are actively being scientifically investigated.[582] In May 2014, Cancer Research UK stated that there are "very preliminary unpublished results that suggest that e-cigarettes promote tumour growth in human cells."[313] In October 2012, the World Medical Association stated, "Manufacturers and marketers of e-cigarettes often claim that use of their products is a safe alternative to smoking, particularly since they do not produce carcinogenic smoke. However, no studies have been conducted to determine that the vapor is not carcinogenic, and there are other potential risks associated with these devices."[583] In 2014, the World Lung Foundation (now known as Vital Strategies) stated that "Researchers find that many e-cigarettes contain toxins [toxicants], contaminants and carcinogens that conflict with the industry's portrayal of its products as purer, healthier alternatives. They also find considerable variations in the amount of nicotine delivered by different brands. None of this information is made available to consumers so they really don't know what they are ingesting, or how much."[413]
Biased research paid for by the tobacco industry continues to be rampant in the e-cigarette topic area, as of 2019.[584] The tobacco companies have had an impact on research-based conclusions by providing funding for scientists.[585] The extent to which research related to e-cigarettes has ties to businesses and other special interests in this industry, is an area of concern.[586] In 2021, Juul provided $51,000 to allocate the full May/June issue of the American Journal of Health Behavior to publish 11 studies paid for by the company to present evidence that its products assist smokers to cease smoking.[587] All the studies were co-authored by people who were current or former Juul employees or somehow affiliated to or under contract with Juul.[588] Elbert Glover, the owner of the American Journal of Health Behavior journal at that time, did not tell the peer reviewers allocated to the studies that Juul bought the whole issue.[589] Several stopped reviewing the studies when they found out.[589] Glover recruited other people to review the studies for a cost of $75, which is not normally done..[589] Nearly all the articles did not acknowledge that Juul and other e-cigarette companies profit off of luring an untold number of new users to nicotine addiction.[588]
Public perception

Marketing and advertisement play a significant role in the public's perception of e-cigarettes.[207] E-cigarettes have been marketed as a safe substitute for tobacco products.[572] This has led to the creation of a misleading impression of safety with their users.[572] The public generally thinks that vaping is correlated with few health risks.[214] Some tobacco users think vaping is safer than tobacco or other smoking cessation aids.[590] It is generally considered by users that e-cigarettes are safer than tobacco.[376] Emerging research indicates that vaping is not as safe as previously thought.[591] Many users think that e-cigarettes are healthier than traditional cigarettes for personal use or for other people.[147] Many youth believe vaping is a safe substitute to traditional cigarettes.[274] The evidence suggests that the parental perception of a child's health risks connected to e-cigarette exposure during both prenatal and post-natal life is low.[459]
A 2016 review suggests "that the perceived health risks, specific product characteristics (such as taste, price and inconspicuous use), and higher levels of acceptance among peers and others potentially make e-cigarettes initially more attractive to adolescents than tobacco cigarettes."[592] Youths who have lower harm perceptions may be particularly susceptible to e-cigarette and polytobacco use, conversely those who perceive e-cigarettes as more harmful would be less likely to use them.[593] Usually, only a small proportion of users are concerned about the potential adverse health effects or toxicity of e-cigarettes.[147] A nation-wide US survey among adults found 11.1% thought vaping during pregnancy was not as harmful as smoking, 51.0% thought it was as harmful, 11.6% thought it would be an increased harm, and 26.2% were unsure.[594] A 2015 study showed that 60% of all adolescence stated vaping were safe or a minor health risk and that 53.4% considered vaping safer than cigarette smoking.[154] A 2017 review found, based on literature from January 2006 to October 2016, examining perceptions regarding vaping during pregnancy, that the majority of respondents perceived vaping can carry health risks to mother and child, but also thought they may be less harmful than traditional cigarettes.[595] Many adolescent asthmatics have a favorable view of vaping.[131] A 2016 survey of people 14 years of age and up in Germany reported that 20.7% of participants consider e-cigarettes to be not as harmful as cigarettes, 46.3% just as harmful, and 16.1% thought they were more harmful, and 17.0% gave no answer.[596] In terms of harm perception, a 2016 study found that flavored e-cigarette use reduced the prevalence of perception of the dangers of tobacco use among youth.[357] Another 2016 study found more nuanced results, demonstrating that tobacco flavor increased harm perception while fruit and sweet flavors decreased harm perception among UK adolescents.[357] Similarly, a 2016 study in the US found that, for US adolescents, fruit-flavored e-cigarettes were perceived to be less harmful than tobacco flavored ones.[357] There is indication that an individual's perception of a substance's potential harms and benefits and their behavior of use is influenced by the availability of information discussing the health effects of that substance.[576] A 2015 analysis reports that 34.20% (8,433/24,658) of American youth sampled believe that e-cigarettes are less harmful than cigarettes, and 45% (11,096/24,658) are not sure.[576]
As of 2018[update], under 50% of adults in the UK believe vaping is less harmful than smoking.[597] Action on Smoking and Health (ASH) in the UK found that in 2015, compared to the year before, "there has been a growing false belief that electronic cigarettes could be as harmful as smoking".[598] Among smokers who had heard of e-cigarettes but never tried them, this "perception of harm has nearly doubled from 12% in 2014 to 22% in 2015."[598] ASH expressed concern that "The growth of this false perception risks discouraging many smokers from using electronic cigarettes to quit and keep them smoking instead which would be bad for their health and the health of those around them."[598] A 2015 PHE report noted that in the US belief among respondents to a survey that vaping was safer than smoking cigarettes fell from 82% in 2010 to 51% in 2014.[599] The report blamed "misinterpreted research findings", attracting negative media coverage, for the growth in the "inaccurate" belief that e-cigarettes were as harmful as smoking.[600] A 2017 review noted that there is a public misconception that vaping is safer than cigarette smoking.[517] A 2016 review noted that the increasing use of e-cigarettes may be due in part to "the misperception that e-cigarettes are a safer alternative to traditional cigarettes."[601] A 2014 review noted that "users do not appear to fully understand their health risks."[387] Beliefs on vaping may be surpassing our scientific knowledge of these products.[602] Proponents of vaping have stated that nicotine is 'as safe as caffeine'.[603] E-cigarettes are believed to be considerably safer compared with smoking while nicotine is thought to be comparatively benign, except for its addiction potential.[604] Consequently, it is believed to be without risk to use them indoors or near babies.[604]
A 2014 worldwide survey found that 88% of respondents stated that vaping were less harmful than cigarette smoke and 11% believed that vaping were absolutely harmless.[605] A 2013 four-country survey found higher than 75% of current and former smokers think e-cigarettes are safer than traditional cigarettes.[76] A 2017 report found that among high income countries, Republic of Korea in 2016 was 66%, the US in 2016 was 37%, Netherlands in 2015 was 32%, Canada in 2016 was 30%, the UK in 2016 was 24%, Australia in 2016 was 22%, Uruguay in 2014 was 19%, and among low income countries, Malaysia in 2013 was 70%, Zambia in 2014 was 57%, Thailand in 2012 was 54%, Mexico from 2014 to 2015 was 38%, Bangladesh from 2014 to 2015 was 37%, Brazil from 2012 to 2013 was 22%, and China from 2013 to 2015 was 15%, for the percentage of respondents of adult smokers believing e-cigarette use is just as risky or more risky to health than cigarettes.[606]
A 2016 review found that "The vaping communities' apparent lack of acknowledgment of the potential negative impacts of e-cigarettes appears to have discredited them in the eyes of many public health officials. Continuing down this path may generate beliefs that the vaping community cares little for public health, are primarily interested in selling their fast-growing companies to the highest tobacco company bidder, and will oppose any meaningful regulations of their product, however reasonable and necessary they may be—essentially aligning the vaping community's practices to tobacco companies' well-established playbook."[607] A 2017 review found that "Although it was originally argued that e‐cigarettes are 'harm free,' the present prevailing belief is that they are 'reduced harm' alternatives to conventional cigarettes. This latter notion is still debatable and not supported by conclusive evidence, especially considering the wide variation between e‐cigarette products."[225] E-cigarette advertisements with warnings could strengthen e-cigarette harm perceptions, and lower the likelihood of buying e-cigarettes.[608]
Related media
- E-cigarette related media
-
NIDA Live - The Science of Vaping
-
Why Teens are Attracted to Vaping
-
Nora Volkow on Addiction - A Disease of Free Will
-
Julius Dein Performs A Magic Trick on a Vape
-
E-cigarette battery explosion injuries
See also
Notes
- ↑ A 2019 review concluded: "no long term vaping toxicological/safety studies have been done in humans; without these data, saying with certainty that e-cigarettes are safer than combustible cigarettes is impossible."[37] Early research seemed to indicate that vaping might be safer than traditional cigarettes and provide a different method to give up smoking, though mounting evidence does not substantiate this.[45] Evidence has not been presented to demonstrate that e-cigarettes are less dangerous than tobacco.[46] The short-term health effects of e-cigarettes can be severe[47] and the short-term harms of e-cigarettes is greater than tobacco products.[48] E-cigarettes are frequently viewed as a safer alternative to conventional cigarettes; however, evidence to support this perspective has not materialized.[49] This appears to be due to the presence of toxicants in e-liquid composition, their adverse effects in animal models, association with acute lung injury and cardiovascular disease, and ability to modulate different cell populations in the lung and blood towards pro-inflammatory phenotypes.[49] A 2020 review noted, "although there is overlap with the toxicity of tobacco, vaping introduces exposures and has effects which are not seen with tobacco. Thus the idea that vaping is a safer, watered-down version of smoking, is scientific nonsense."[48]
- ↑ While vitamin E acetate is strongly linked to this outbreak, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC or non-THC products, in some of the reported vaping-related lung injury cases.[65] There is likely more than one cause of the outbreak.[67] The majority of cases in Canada involving lung injuries do not seem to have been connected with the use of THC-infused products.[66] In 2019, some people diagnosed with a vaping-induced lung injury reported using only nicotine-containing products.[68] Nicotine e-cigarette use has been linked to the vaping-induced lung injury cases in a small subset of users.[69] In 2020, the first uptick in vaping-induced lung injury cases had occurred in Utah since the decline of 2019.[70] This research indicates the recurrent nature of the vaping-induced lung illness epidemic with new occurrences continuing to be reported.[70]
- ↑ A 2021 review found "Formaldehyde, acetaldehyde, acrolein, carcinogenic nitrosamines N'-nitrosonornicotine (NNN) and nicotine-derived nitrosamine ketones (NNK) were found in vapors of a variety of e-cigarette products and are all carcinogenic to humans."[89]
- ↑ The engineering designs, including the kind of the battery, heating temperature of the solution, and the style of heating element and storage for the solution, typically affects the nature, number, and size of particles generated.[43]
- ↑ E-cigarettes were initially marketed as a safe replacement for smoking, but clinical and experimental studies have observed the potentially, lethal consequences of these products.[133] The industry's marketing approach for these instruments of addiction has been to promote them as a safer alternative to tobacco, a behavioral choice supporting smoking cessation, and as the 'cool' appearance of vaping with flavored products (e.g. tutti frutti, bubble gum, and buttered popcorn etc.).[134]
- ↑ E-cigarette aerosol generally contains fewer toxic chemicals than the deadly mix of 7,000 chemicals in smoke from regular cigarettes.[141]
- ↑ A 2019 review states, "Experts who favor abstinence contend that if ENDS regulations are too lax, the e-cigarette industry will repeat tobacco manufacturer offences including using media to target youth and misleading the public through false safety claims. They point out that ENDS contain harmful chemicals, lack safety oversight, may renormalize smoking behaviors, and if unchecked, could provide a gateway to tobacco. From this perspective, ENDS may compromise existing tobacco control efforts and have a negative public health impact."[58]
- ↑ Due to the subsequent identification of the primary cause of cases in the US, and the considerable decline in cases and deaths since a peak in September 2019, the CDC stopped collecting these data from states as of February 2020.[65]
- ↑ Vitamin E acetate is used as an additive, most notably in THCl-containing e-cigarette, or vaping, products.[65] Vitamin E acetate dilutes THC oil without altering the look or thickness.[106] Research suggests that when vitamin E acetate is inhaled, it may interfere with normal lung functioning.[65]
- ↑ A 2014 review found "Wide ranges in the levels of chemical substances such as tobacco-specific nitrosamines, aldehydes, metals, volatile organic compounds, phenolic compounds, polycyclic aromatic hydrocarbons, flavours, solvent carriers, tobacco alkaloids and drugs have been reported in e-cigarette refill solutions, cartridges, aerosols and environmental emissions."[90]
- ↑ A 2014 review found "there is enough heat generated during puffing to cause the fluid to decompose and/or components of the device to pyrolyze, whereby toxic/carcinogenic substances may be formed."[102]
- ↑ The term vapor is a misnomer due to the fact that the aerosol generated by e-cigarettes has both a particulate and gas phase.[81]
- ↑ E-cigarette aerosol is composed of droplets of e-liquids, which contain mainly propylene glycol, glycerin, nicotine, water, flavorings (if added to e-liquid), preservatives and also small amounts of by-products of thermal decomposition of some of these constituents.[127]
- ↑ A 2017 review found "The physical composition of the aerosol can be altered by many factors: the temperature of the metal coil, rate of e-liquid flow through the heated coil, chemical composition of the coil, the coil connection to the power source, the wicking material transporting e-liquid and the hot aerosol contacts."[353]
- ↑ A 2017 review found "As e-cig metal components undergo repeated cycles of heating and cooling, traces of these metal components can leech into the e-liquid, causing the device to emit metallic nanoparticles."[259]
Bibliography
- McNeill, A; Brose, LS; Calder, R; Bauld, L; Robson, D (February 2018). "Evidence review of e-cigarettes and heated tobacco products 2018" (PDF). UK: Public Health England. pp. 1–243.
- National Academies of Sciences, Engineering, and Medicine; et al. (Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems) (23 January 2018). Stratton, Kathleen; Kwan, Leslie Y.; Eaton, David L. (eds.). Public Health Consequences of E-Cigarettes. Washington, DC: National Academies Press. pp. 1–774. doi:10.17226/24952. ISBN 978-0-309-46834-3. PMID 29894118.
{{cite book}}: CS1 maint: multiple names: authors list (link) CS1 maint: ref duplicates default (link) Summary - "Electronic Nicotine Delivery Systems and Electronic Non-Nicotine Delivery Systems (ENDS/ENNDS)". World Health Organization. 1 August 2016. pp. 1–11.
- Wilder, Natalie; Daley, Claire; Sugarman, Jane; Partridge, James (April 2016). "Nicotine without smoke: Tobacco harm reduction". UK: Royal College of Physicians. pp. 1–191.
- McNeill, A; Brose, LS; Calder, R; Hitchman, SC; Hajek, P; McRobbie, H (August 2015). "E-cigarettes: an evidence update" (PDF). UK: Public Health England. pp. 1–113.
- "E-Cigarette Fire Risks and Reported Incidents" (PDF). Government of New South Wales. 30 January 2015. pp. 1–13.
- "State Health Officer's Report on E-Cigarettes: A Community Health Threat" (PDF). California Tobacco Control Program. California Department of Public Health. January 2015. pp. 1–21.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - National Center for Chronic Disease Prevention Health Promotion (US) Office on Smoking Health (2014). The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Surgeon General of the United States. pp. 1–943. PMID 24455788.
References
- ↑ Sapru, Sakshi; Vardhan, Mridula; Li, Qianhao; Guo, Yuqi; Li, Xin; Saxena, Deepak (December 2020). "E-cigarettes use in the United States: reasons for use, perceptions, and effects on health". BMC Public Health. 20 (1). doi:10.1186/s12889-020-09572-x. PMC 7545933. PMID 33032554.
 This article incorporates text by Sakshi Sapru, Mridula Vardhan, Qianhao Li, Yuqi Guo, Xin Li, and Deepak Saxena available under the CC BY 4.0 license.
This article incorporates text by Sakshi Sapru, Mridula Vardhan, Qianhao Li, Yuqi Guo, Xin Li, and Deepak Saxena available under the CC BY 4.0 license.
- ↑ 2.0 2.1 Kathuria, Hasmeena (November 2022). "Electronic Cigarette Use, Misuse, and Harm". Medical Clinics of North America. 106 (6): 1081–1092. doi:10.1016/j.mcna.2022.07.009. PMID 36280334.
- ↑ Asfar, Taghrid; Livingstone-Banks, Jonathan; Ward, Kenneth D; Eissenberg, Thomas; Oluwole, Olusanya; Bursac, Zoran; Ghaddar, Tarek; Maziak, Wasim (7 June 2023). "Interventions for waterpipe smoking cessation". Cochrane Database of Systematic Reviews. 2023 (6). doi:10.1002/14651858.CD005549.pub4. PMC 10245833. PMID 37286509.
{{cite journal}}: Check|pmc=value (help) - ↑ Raghubeer, Shanel (February 2023). "The influence of epigenetics and inflammation on cardiometabolic risks". Seminars in Cell & Developmental Biology. doi:10.1016/j.semcdb.2023.02.006. PMID 36804178.
- ↑ Guo, Xingtong; Hou, Lili; Peng, Xuepei; Tang, Fuyou (9 February 2023). "The prevalence of xerostomia among e-cigarette or combustible tobacco users: A systematic review and meta-analysis". Tobacco Induced Diseases. 21 (February): 1–11. doi:10.18332/tid/156676. PMID 36777290.
- ↑ Lee, Julia X.; Phipatanakul, Wanda; Gaffin, Jonathan M. (April 2023). "Environment and the development of severe asthma in inner city population". Current Opinion in Allergy & Clinical Immunology. 23 (2): 179–184. doi:10.1097/ACI.0000000000000890. PMC 9974609. PMID 36728241.
{{cite journal}}: Check|pmc=value (help) - ↑ Jane Ling, Miaw Yn; Abdul Halim, Ahmad Farid Nazmi; Ahmad, Dzulfitree; Ahmad, Norfazilah; Safian, Nazarudin; Mohammed Nawi, Azmawati (22 February 2023). "Prevalence and Associated Factors of E-Cigarette Use among Adolescents in Southeast Asia: A Systematic Review". International Journal of Environmental Research and Public Health. 20 (5): 3883. doi:10.3390/ijerph20053883. PMC 10001692. PMID 36900893.
{{cite journal}}: Check|pmc=value (help) - ↑ Assanangkornchai, Sawitri; Kalayasiri, Rasmon; Ratta-apha, Woraphat; Tanaree, Athip (July 2023). "Effects of cannabis legalization on the use of cannabis and other substances". Current Opinion in Psychiatry. 36 (4): 283–289. doi:10.1097/YCO.0000000000000868. PMID 37185310.
- ↑ Cashion, Jake M.; Young, Kaylene M.; Sutherland, Brad A. (March 2023). "How does neurovascular unit dysfunction contribute to multiple sclerosis?". Neurobiology of Disease. 178: 106028. doi:10.1016/j.nbd.2023.106028. PMID 36736923.
- ↑ Notley, Caitlin; West, Robert; Soar, Kirstie; Hastings, Janna; Cox, Sharon (March 2023). "Toward an ontology of identity‐related constructs in addiction, with examples from nicotine and tobacco research". Addiction. 118 (3): 548–557. doi:10.1111/add.16079. PMID 36370069.
- ↑ Fadeyi, Olaniyi; Randhawa, Anantbir; Shankar, Abhirami; Garabetian, Christine; Singh, Harpreet; Topacio, Antonio (January 2023). "Thromboembolism Triggered by a Combination of Electronic Cigarettes and Oral Contraceptives: A Case Report and Review of Literature". Journal of Investigative Medicine High Impact Case Reports. 11. doi:10.1177/23247096231181072. PMID 37314028.
- ↑ Bernat, Jennifer K; Jackson, Kia J; Krüsemann, Erna J Z; Boesveldt, Sanne; Rudy, Susan F; Talhout, Reinskje (April 2023). "Sensory methods to evaluate perception of flavours in tobacco and other nicotine-containing products: a review". Tobacco Control. 32 (e1): e95–e102. doi:10.1136/tobaccocontrol-2021-056681. PMID 34615737.
- ↑ Ali, Nurshad; Xavier, Joseph; Engur, Melih; Pv, Mohanan; Bernardino de la Serna, Jorge (September 2023). "The impact of e-cigarette exposure on different organ systems: A review of recent evidence and future perspectives". Journal of Hazardous Materials. 457: 131828. doi:10.1016/j.jhazmat.2023.131828. PMID 37320902.
- ↑ Mahfooz, Kamran; Vasavada, Advait M; Joshi, Arpit; Pichuthirumalai, Srikrishnan; Andani, Rupesh; Rajotia, Arush; Hans, Aakash; Mandalia, Bilvesh; Dayama, Neeraj; Younas, Zara; Hafeez, Nosheen; Bheemisetty, Niharika; Patel, Yash; Tumkur Ranganathan, Hemalatha; Sodala, Ashok (9 February 2023). "Waterpipe Use and Its Cardiovascular Effects: A Systematic Review and Meta-Analysis of Case-Control, Cross-Sectional, and Non-Randomized Studies". Cureus. doi:10.7759/cureus.34802. PMC 10008028. PMID 36915837.
{{cite journal}}: Check|pmc=value (help) - ↑ 15.0 15.1 Tran, Vincent; Mian, Mustafa; Sreedharan, Subhashaan; Robertson, Ross; Saha, Anik; Tadakamadla, Santosh Kumar; Lee, Kai (May 2023). "Oral and Maxillofacial Injuries Associated With E-Cigarette Explosions: A Systematic Review and Management Guidelines Proposal". Journal of Oral and Maxillofacial Surgery. 81 (5): 583–592. doi:10.1016/j.joms.2023.01.009. PMID 36806607. Cite error: Invalid
<ref>tag; name "Tran2023" defined multiple times with different content - ↑ Cao, Xia; Wang, Yi; Chen, Ying; Zhao, Mantong; Liang, Lanyuan; Yang, Mengru; Li, Jianhua; Peng, Mingming; Li, Wei; Yue, Yiming; Zhang, Han; Li, Chuanqiu; Shu, Zunpeng (May 2023). "Advances in traditional Chinese medicine for the treatment of chronic obstructive pulmonary disease". Journal of Ethnopharmacology. 307: 116229. doi:10.1016/j.jep.2023.116229. PMID 36773789.
- ↑ Noar, Seth M.; Ma, Haijing; Kieu, Talia; Ribisl, Kurt M. (3 July 2023). "Can Extant Vaping Prevention Message Experiments Tell Us Something About What Works? A Response to O'Keefe". Health Communication. 38 (8): 1727–1730. doi:10.1080/10410236.2023.2212195. PMID 37183777.
- ↑ Lindson, Nicola; Butler, Ailsa R.; Liber, Alex; Levy, David T.; Barnett, Phoebe; Theodoulou, Annika; Notley, Caitlin; Rigotti, Nancy A.; Hartmann‐Boyce, Jamie (April 2023). "An exploration of flavours in studies of e‐cigarettes for smoking cessation: secondary analyses of a systematic review with meta‐analyses". Addiction. 118 (4): 634–645. doi:10.1111/add.16091. PMID 36399154.
- ↑ Ma, Haijing; Kieu, Talia Kim-Thanh; Ribisl, Kurt M.; Noar, Seth M. (3 July 2023). "Do Vaping Prevention Messages Impact Adolescents and Young Adults? A Meta-Analysis of Experimental Studies". Health Communication. 38 (8): 1709–1722. doi:10.1080/10410236.2023.2185578. PMC 10258164. PMID 36882378.
{{cite journal}}: Check|pmc=value (help) - ↑ Chugh, Aastha; Arora, Monika; Jain, Neha; Vidyasagaran, Aishwarya; Readshaw, Anne; Sheikh, Aziz; Eckhardt, Jappe; Siddiqi, Kamran; Chopra, Mansi; Mishu, Masuma Pervin; Kanaan, Mona; Rahman, Muhammad Aziz; Mehrotra, Ravi; Huque, Rumana; Forberger, Sarah; Dahanayake, Suranji; Khan, Zohaib; Boeckmann, Melanie; Dogar, Omara (June 2023). "The global impact of tobacco control policies on smokeless tobacco use: a systematic review". The Lancet Global Health. 11 (6): e953–e968. doi:10.1016/S2214-109X(23)00205-X. PMID 37202029.
- ↑ Coughlin, Lara N.; Salino, Sarah; Jennings, Claudia; Lacek, Madelyn; Townsend, Whitney; Koffarnus, Mikhail N.; Bonar, Erin E. (April 2023). "A systematic review of remotely delivered contingency management treatment for substance use". Journal of Substance Use and Addiction Treatment. 147: 208977. doi:10.1016/j.josat.2023.208977. PMID 36804352.
- ↑ McKeon, Gemma; Scott, James G (February 2023). "Smoke and mirrors: Support from psychiatrists for nicotine e-cigarette availability in Australia". Australian & New Zealand Journal of Psychiatry. 57 (2): 169–180. doi:10.1177/00048674221126458. PMID 36120959.
- ↑ Phillips, Lucy; Thomson, Ross; Coleman-Haynes, Tom; Cooper, Sue; Naughton, Felix; Mcdaid, Lisa; Emery, Joanne; Coleman, Tim (3 February 2023). "Developing a taxonomy to describe offspring outcomes in studies involving pregnant mammals' exposure to non-tobacco nicotine: A systematic scoping review". PLOS ONE. 18 (2): e0280805. doi:10.1371/journal.pone.0280805. PMC 9897539. PMID 36735735.
{{cite journal}}: Check|pmc=value (help) - ↑ 24.0 24.1 24.2 24.3 24.4 24.5 24.6 24.7 Luca, Alina-Costina; Curpăn, Alexandrina-Ștefania; Iordache, Alin-Constantin; Mîndru, Dana Elena; Țarcă, Elena; Luca, Florin-Alexandru; Pădureț, Ioana-Alexandra (8 February 2023). "Cardiotoxicity of Electronic Cigarettes and Heat-Not-Burn Tobacco Products—A Problem for the Modern Pediatric Cardiologist". Healthcare. 11 (4): 491. doi:10.3390/healthcare11040491. PMC 9957306. PMID 36833024.
{{cite journal}}: Check|pmc=value (help) Cite error: Invalid<ref>tag; name "Luca2023" defined multiple times with different content - ↑ Ismail, Amr; Berdine, Gilbert; Nugent, Kenneth (March 2023). "Subpleural sparing: Clinical, physiological, and radiological implications". The American Journal of the Medical Sciences. 365 (3): 219–225. doi:10.1016/j.amjms.2022.11.002. PMID 36427562.
- ↑ Ding, Ruiyang; Ren, Xiaoke; Sun, Qinglin; Sun, Zhiwei; Duan, Junchao (August 2022). "An integral perspective of canonical cigarette and e-cigarette-related cardiovascular toxicity based on the adverse outcome pathway framework". Journal of Advanced Research. doi:10.1016/j.jare.2022.08.012. PMC 10248804. PMID 35998874.
{{cite journal}}: Check|pmc=value (help) - ↑ Riwu Bara, Roy Pefi; McCausland, Kahlia; Swanson, Maurice; Scott, Lucy; Jancey, Jonine (February 2023). ""They're sleek, stylish and sexy:" selling e-cigarettes online". Australian and New Zealand Journal of Public Health. 47 (1): 100013. doi:10.1016/j.anzjph.2022.100013. PMID 36641959.
- ↑ Vu, Giang T; Stjepanović, Daniel; Sun, Tianze; Leung, Janni; Chung, Jack; Connor, Jason; Thai, Phong K; Gartner, Coral E; Tran, Bach Xuan; Hall, Wayne D; Chan, Gary (9 June 2023). "Predicting the long-term effects of electronic cigarette use on population health: a systematic review of modelling studies". Tobacco Control: tc–2022–057748. doi:10.1136/tc-2022-057748. PMID 37295941.
- ↑ Wang, Qian; Du, Weihong; Wang, Hao; Geng, Panpan; Sun, Yanyun; Zhang, Junfang; Wang, Wei; Jin, Xinchun (June 2023). "Nicotine's effect on cognition, a friend or foe?". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 124: 110723. doi:10.1016/j.pnpbp.2023.110723. PMID 36736944.
- ↑ Khanna, Niharika; Klyushnenkova, Elena; Gaynor, Adam; Dark, Michael; Melamed, Julia; Bennett, Melanie; Deepak, Janaki (8 May 2023). "Integrating a Systematic, Comprehensive E-Cigarette and Vaping Assessment Tool into the Electronic Health Record". The Journal of the American Board of Family Medicine. 36 (3): 405–413. doi:10.3122/jabfm.2022.220410R1. PMID 37290827.
- ↑ Tweet, Marit S.; Wilson, Meaghan; Rosario, Jennifer M.; Duong, Myto (May 2023). "Acute Pediatric Liquid Nicotine Ingestions". Pediatric Annals. 52 (5). doi:10.3928/19382359-20230307-09. PMID 37159065.
- ↑ Travis, Nargiz; Knoll, Marie; Cook, Steven; Oh, Hayoung; Cadham, Christopher J.; Sánchez-Romero, Luz María; Levy, David T. (20 January 2023). "Chemical Profiles and Toxicity of Electronic Cigarettes: An Umbrella Review and Methodological Considerations". International Journal of Environmental Research and Public Health. 20 (3): 1908. doi:10.3390/ijerph20031908. PMC 9914618. PMID 36767274.
{{cite journal}}: Check|pmc=value (help) - ↑ Mendelsohn, Colin P.; Hall, Wayne; Borland, Ron; Wodak, Alex; Beaglehole, Robert; Benowitz, Neal L.; Britton, John; Bullen, Chris; Etter, Jean‐François; McNeill, Ann; Rigotti, Nancy A. (June 2023). "A critique of the Australian National Health and Medical Research Council CEO statement on electronic cigarettes". Addiction. 118 (6): 1184–1192. doi:10.1111/add.16143. PMID 36808672.
- ↑ Hartmann‐Boyce, Jamie; Butler, Ailsa R.; Theodoulou, Annika; Onakpoya, Igho J.; Hajek, Peter; Bullen, Chris; Rigotti, Nancy A.; Lindson, Nicola (March 2023). "Biomarkers of potential harm in people switching from smoking tobacco to exclusive e‐cigarette use, dual use or abstinence: secondary analysis of Cochrane systematic review of trials of e‐cigarettes for smoking cessation". Addiction. 118 (3): 539–545. doi:10.1111/add.16063. PMC 10092879. PMID 36208090.
{{cite journal}}: Check|pmc=value (help) - ↑ Amanian, Ameen; Phulka, Jobanjit; Hu, Amanda C. (January 2023). "Unintended Side Effects of Electronic Cigarettes in Otolaryngology: A Scoping Review". Otolaryngology–Head and Neck Surgery. 168 (1): 7–13. doi:10.1177/01945998211069502. PMID 34982602.
- ↑ 36.0 36.1 36.2 Scott-Wellington, Felicia; Resnick, Elissa A.; Klein, Jonathan D. (February 2023). "Advocacy for Global Tobacco Control and Child Health". Pediatric Clinics of North America. 70 (1): 117–135. doi:10.1016/j.pcl.2022.09.011. PMID 36402463.
- ↑ 37.00 37.01 37.02 37.03 37.04 37.05 37.06 37.07 37.08 37.09 37.10 37.11 37.12 37.13 Gotts, Jeffrey E; Jordt, Sven-Eric; McConnell, Rob; Tarran, Robert (30 September 2019). "What are the respiratory effects of e-cigarettes?". BMJ (Clinical research ed.). BMJ. 366: l5275. doi:10.1136/bmj.l5275. ISSN 1756-1833. PMC 7850161. PMID 31570493.
 This article incorporates text by Jeffrey E Gotts, Sven-Eric Jordt, Rob McConnel, and Robert Tarran available under the CC BY 4.0 license.
This article incorporates text by Jeffrey E Gotts, Sven-Eric Jordt, Rob McConnel, and Robert Tarran available under the CC BY 4.0 license.
- ↑ 38.0 38.1 Pajai, Devanjali D; Paul, Priyanka; Reche, Amit (16 February 2023). "Pharmacotherapy in Tobacco Cessation: A Narrative Review". Cureus. doi:10.7759/cureus.35086. PMC 10023046. PMID 36938244.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Devanjali D Pajai, Priyanka Paul, and Amit Reche available under the CC BY 4.0 license.
This article incorporates text by Devanjali D Pajai, Priyanka Paul, and Amit Reche available under the CC BY 4.0 license.
- ↑ 39.0 39.1 39.2 39.3 39.4 39.5 39.6 Bracken-Clarke, Dara; Kapoor, Dhruv; Baird, Anne Marie; Buchanan, Paul James; Gately, Kathy; Cuffe, Sinead; Finn, Stephen P. (2021). "Vaping and lung cancer – A review of current data and recommendations". Lung Cancer. 153: 11–20. doi:10.1016/j.lungcan.2020.12.030. ISSN 0169-5002. PMID 33429159.
- ↑ 40.00 40.01 40.02 40.03 40.04 40.05 40.06 40.07 40.08 40.09 40.10 40.11 40.12 40.13 40.14 Bautista, Malia; Mogul, Allison S.; Fowler, Christie D. (14 August 2023). "Beyond the label: current evidence and future directions for the interrelationship between electronic cigarettes and mental health". Frontiers in Psychiatry. 14. doi:10.3389/fpsyt.2023.1134079. PMC 10460914. PMID 37645635.
{{cite journal}}: Check|pmc=value (help) This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ↑ "What Is in E-cigarette Aerosol?". Centers for Disease Control and Prevention. 2 November 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 42.0 42.1 42.2 42.3 42.4 42.5 Travis, Nargiz; Knoll, Marie; Cadham, Christopher J.; Cook, Steven; Warner, Kenneth E.; Fleischer, Nancy L.; Douglas, Clifford E.; Sánchez-Romero, Luz María; Mistry, Ritesh; Meza, Rafael; Hirschtick, Jana L.; Levy, David T. (25 July 2022). "Health Effects of Electronic Cigarettes: An Umbrella Review and Methodological Considerations". International Journal of Environmental Research and Public Health. 19 (15): 9054. doi:10.3390/ijerph19159054. PMC 9330875. PMID 35897421.
 This article incorporates text by Nargiz Travis, Marie Knoll, Christopher J. Cadham, Steven Cook, Kenneth E. Warner, Nancy L. Fleischer, Clifford E. Douglas, Luz María Sánchez-Romero, Ritesh Mistry, Rafael Meza, Jana L. Hirschtick, and David T. Levy available under the CC BY 4.0 license.
This article incorporates text by Nargiz Travis, Marie Knoll, Christopher J. Cadham, Steven Cook, Kenneth E. Warner, Nancy L. Fleischer, Clifford E. Douglas, Luz María Sánchez-Romero, Ritesh Mistry, Rafael Meza, Jana L. Hirschtick, and David T. Levy available under the CC BY 4.0 license.
- ↑ 43.00 43.01 43.02 43.03 43.04 43.05 43.06 43.07 43.08 43.09 43.10 43.11 43.12 43.13 43.14 43.15 43.16 43.17 43.18 43.19 43.20 43.21 43.22 43.23 43.24 43.25 43.26 43.27 43.28 43.29 43.30 43.31 43.32 Grana, Rachel; Benowitz, Neal; Glantz, Stanton A. (13 May 2014). "E-Cigarettes: A Scientific Review". Circulation. 129 (19): 1972–1986. doi:10.1161/circulationaha.114.007667. PMC 4018182. PMID 24821826.
- ↑ 44.00 44.01 44.02 44.03 44.04 44.05 44.06 44.07 44.08 44.09 44.10 44.11 44.12 44.13 Drummond, MB; Upson, D (February 2014). "Electronic cigarettes. Potential harms and benefits". Annals of the American Thoracic Society. 11 (2): 236–42. doi:10.1513/annalsats.201311-391fr. PMC 5469426. PMID 24575993.
- ↑ 45.0 45.1 45.2 Kumar, P.S.; Clark, P.; Brinkman, M.C.; Saxena, D. (2019). "Novel Nicotine Delivery Systems". Advances in Dental Research. 30 (1): 11–15. doi:10.1177/0022034519872475. ISSN 0895-9374. PMID 31538804.
- ↑ 46.0 46.1 46.2 Herman, Melissa; Tarran, Robert (2020). "E‐cigarettes, nicotine, the lung and the brain: multi‐level cascading pathophysiology". The Journal of Physiology. 598 (22): 5063–5071. doi:10.1113/JP278388. ISSN 0022-3751. PMC 7721976. PMID 32515030.
- ↑ 47.0 47.1 47.2 47.3 Gilley, Meghan; Beno, Suzanne (June 2020). "Vaping implications for children and youth". Current Opinion in Pediatrics. 32 (3): 343–348. doi:10.1097/MOP.0000000000000889. ISSN 1040-8703. PMID 32332326.
- ↑ 48.0 48.1 48.2 48.3 48.4 48.5 48.6 48.7 48.8 48.9 Bhatt, Jayesh Mahendra; Ramphul, Manisha; Bush, Andrew (2020). "An update on controversies in e-cigarettes". Paediatric Respiratory Reviews. 36: 75–86. doi:10.1016/j.prrv.2020.09.003. ISSN 1526-0542. PMC 7518964. PMID 33071065.
- ↑ 49.00 49.01 49.02 49.03 49.04 49.05 49.06 49.07 49.08 49.09 49.10 49.11 49.12 49.13 49.14 49.15 49.16 Snoderly, Hunter T.; Nurkiewicz, Timothy R.; Bowdridge, Elizabeth C.; Bennewitz, Margaret F. (18 November 2021). "E-Cigarette Use: Device Market, Study Design, and Emerging Evidence of Biological Consequences". International Journal of Molecular Sciences. MDPI AG. 22 (22): 12452. doi:10.3390/ijms222212452. ISSN 1422-0067. PMC 8619996. PMID 34830344.
 This article incorporates text by Hunter T. Snoderly,Timothy R. Nurkiewicz, Elizabeth C. Bowdridge, and Margaret F. Bennewitz available under the CC BY 4.0 license.
This article incorporates text by Hunter T. Snoderly,Timothy R. Nurkiewicz, Elizabeth C. Bowdridge, and Margaret F. Bennewitz available under the CC BY 4.0 license.
- ↑ 50.0 50.1 50.2 50.3 50.4 50.5 50.6 50.7 Mravec, Boris; Tibensky, Miroslav; Horvathova, Lubica; Babal, Pavel (2020). "E-Cigarettes and Cancer Risk". Cancer Prevention Research. 13 (2): 137–144. doi:10.1158/1940-6207.CAPR-19-0346. ISSN 1940-6207. PMID 31619443.
- ↑ 51.0 51.1 51.2 51.3 Knorst, Marli Maria; Benedetto, Igor Gorski; Hoffmeister, Mariana Costa; Gazzana, Marcelo Basso (2014). "The electronic cigarette: the new cigarette of the 21st century?". Jornal Brasileiro de Pneumologia. 40 (5): 564–572. doi:10.1590/S1806-37132014000500013. ISSN 1806-3713. PMC 4263338. PMID 25410845.
- ↑ 52.00 52.01 52.02 52.03 52.04 52.05 52.06 52.07 52.08 52.09 52.10 52.11 52.12 52.13 52.14 52.15 52.16 52.17 52.18 52.19 52.20 Farsalinos, K. E.; Polosa, R. (2014). "Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review". Therapeutic Advances in Drug Safety. 5 (2): 67–86. doi:10.1177/2042098614524430. ISSN 2042-0986. PMC 4110871. PMID 25083263.
- ↑ 53.00 53.01 53.02 53.03 53.04 53.05 53.06 53.07 53.08 53.09 53.10 53.11 Smith, L; Brar, K; Srinivasan, K; Enja, M; Lippmann, S (June 2016). "E-cigarettes: How "safe" are they?". J Fam Pract. 65 (6): 380–5. PMID 27474819.
- ↑ Bush, Andrew; Ferkol, Thomas; Valiulis, Algirdas; Mazur, Artur; Chkhaidze, Ivane; Maglakelidze, Tamaz; Sargsyan, Sergey; Boyajyan, Gevorg; Cirstea, Olga; Doan, Svitlana; Katilov, Oleksandr; Pokhylko, Valeriy; Dubey, Leonid; Poluziorovienė, Edita; Prokopčiuk, Nina; Taminskienė, Vaida; Valiulis, Arūnas (8 February 2021). "Unfriendly Fire: How the Tobacco Industry is Destroying the Future of Our Children". Acta medica Lituanica. 28 (1): 6–18. doi:10.15388/Amed.2020.28.1.6. PMC 8311841. PMID 34393624.
- ↑ 55.0 55.1 55.2 55.3 55.4 "Electronic nicotine delivery systems" (PDF). World Health Organization. 21 July 2014. pp. 1–13.
- ↑ 56.0 56.1 56.2 Glover, Marewa; Breier, Bernhard H.; Bauld, Linda (2016). "Could Vaping be a New Weapon in the Battle of the Bulge?". Nicotine & Tobacco Research. 19 (12): 1536–1540. doi:10.1093/ntr/ntw278. hdl:1893/26149. ISSN 1462-2203. PMID 27798086.
- ↑ 57.0 57.1 57.2 57.3 57.4 57.5 Jimenez Ruiz, CA; Solano Reina, S; de Granda Orive, JI; Signes-Costa Minaya, J; de Higes Martinez, E; Riesco Miranda, JA; Altet Gómez, N; Lorza Blasco, JJ; Barrueco Ferrero, M; de Lucas Ramos, P (August 2014). "The electronic cigarette. Official statement of the Spanish Society of Pneumology and Thoracic Surgery (SEPAR) on the efficacy, safety and regulation of electronic cigarettes". Archivos de Bronconeumologia. 50 (8): 362–7. doi:10.1016/j.arbres.2014.02.006. PMID 24684764.
- ↑ 58.0 58.1 58.2 Brady, Benjamin R.; De La Rosa, Jennifer S.; Nair, Uma S.; Leischow, Scott J. (2019). "Electronic Cigarette Policy Recommendations: A Scoping Review". American Journal of Health Behavior. 43 (1): 88–104. doi:10.5993/AJHB.43.1.8. ISSN 1087-3244. PMID 30522569.
- ↑ Bals, Robert; Boyd, Jeanette; Esposito, Susanna; Foronjy, Robert; Hiemstra, Pieter S.; Jiménez-Ruiz, Carlos A.; Katsaounou, Paraskevi; Lindberg, Anne; Metz, Carlos; Schober, Wolfgang; Spira, Avrum; Blasi, Francesco (2019). "Electronic cigarettes: a task force report from the European Respiratory Society". European Respiratory Journal. 53 (2): 1801151. doi:10.1183/13993003.01151-2018. ISSN 0903-1936. PMID 30464018.
- ↑ 60.0 60.1 Tsai, MuChun; Byun, Min Kwang; Shin, John; Crotty Alexander, Laura E. (2020). "Effects of e‐cigarettes and vaping devices on cardiac and pulmonary physiology". The Journal of Physiology. 598 (22): 5039–5062. doi:10.1113/JP279754. ISSN 0022-3751. PMID 32975834.
- ↑ 61.0 61.1 61.2 61.3 Riwu Bara, Roy Pefi; McCausland, Kahlia; Swanson, Maurice; Scott, Lucy; Jancey, Jonine (February 2023). ""They're sleek, stylish and sexy:" selling e-cigarettes online". Australian and New Zealand Journal of Public Health. 47 (1): 100013. doi:10.1016/j.anzjph.2022.100013. PMID 36641959.
- ↑ 62.0 62.1 62.2 62.3 62.4 62.5 Breland, Alison B.; Spindle, Tory; Weaver, Michael; Eissenberg, Thomas (2014). "Science and Electronic Cigarettes". Journal of Addiction Medicine. 8 (4): 223–233. doi:10.1097/ADM.0000000000000049. ISSN 1932-0620. PMC 4122311. PMID 25089952.
- ↑ 63.0 63.1 63.2 Gaur, Sumit; Agnihotri, Rupali (2018). "Health Effects of Trace Metals in Electronic Cigarette Aerosols—a Systematic Review". Biological Trace Element Research. 188 (2): 295–315. doi:10.1007/s12011-018-1423-x. ISSN 0163-4984. PMID 29974385.
- ↑ 64.0 64.1 64.2 Harrell, PT; Simmons, VN; Correa, JB; Padhya, TA; Brandon, TH (4 June 2014). "Electronic Nicotine Delivery Systems ("E-cigarettes"): Review of Safety and Smoking Cessation Efficacy". Otolaryngology–Head and Neck Surgery. 151 (3): 381–393. doi:10.1177/0194599814536847. PMC 4376316. PMID 24898072.
- ↑ 65.00 65.01 65.02 65.03 65.04 65.05 65.06 65.07 65.08 65.09 65.10 65.11 65.12 65.13 "Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products". Centers for Disease Control and Prevention. 3 August 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 66.0 66.1 66.2 66.3 66.4 66.5 "Vaping-associated lung illness". Public Health Agency of Canada. 20 August 2020.
- ↑ 67.0 67.1 King, Brian A.; Jones, Christopher M.; Baldwin, Grant T.; Briss, Peter A. (2020). "The EVALI and Youth Vaping Epidemics — Implications for Public Health". New England Journal of Medicine. 382 (8): 689–691. doi:10.1056/NEJMp1916171. ISSN 0028-4793. PMID 31951683.
- ↑ Ghinai, Isaac; Navon, Livia; Gunn, Jayleen K.L.; Duca, Lindsey M.; Brister, Sarah; Love, Sarah; Brink, Rachel; Fajardo, Geroncio; Johnson, Jona; Saathoff-Huber, Lori; King, Brian A.; Jones, Christopher M.; Krishnasamy, Vikram P.; Layden, Jennifer E. (24 January 2020). "Characteristics of Persons Who Report Using Only Nicotine-Containing Products Among Interviewed Patients with E-cigarette, or Vaping, Product Use–Associated Lung Injury — Illinois, August–December 2019". MMWR. Morbidity and Mortality Weekly Report. 69 (3): 84–89. doi:10.15585/mmwr.mm6903e1. PMC 7367041. PMID 31971930.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 69.0 69.1 Marrocco, Antonella; Singh, Dilpreet; Christiani, David C.; Demokritou, Philip (16 March 2022). "E-cigarette vaping associated acute lung injury (EVALI): state of science and future research needs". Critical Reviews in Toxicology. 52 (3): 188–220. doi:10.1080/10408444.2022.2082918. PMC 9716650. PMID 35822508.
{{cite journal}}: Check|pmc=value (help) - ↑ 70.0 70.1 70.2 Smith, Maxwell L.; Gotway, Michael B.; Crotty Alexander, Laura E.; Hariri, Lida P. (2020). "Vaping-related lung injury". Virchows Archiv. 478 (1): 81–88. doi:10.1007/s00428-020-02943-0. ISSN 0945-6317. PMC 7590536. PMID 33106908.
- ↑ 71.0 71.1 Zulfiqar, Hassam; Rahman, Omar (14 March 2021). Vaping Associated Pulmonary Injury. StatPearls Publishing. PMID 32809491.
- ↑ 72.00 72.01 72.02 72.03 72.04 72.05 72.06 72.07 72.08 72.09 72.10 72.11 72.12 72.13 Hajek, P; Etter, JF; Benowitz, N; Eissenberg, T; McRobbie, H (31 July 2014). "Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit". Addiction. 109 (11): 1801–10. doi:10.1111/add.12659. PMC 4487785. PMID 25078252.
- ↑ 73.00 73.01 73.02 73.03 73.04 73.05 73.06 73.07 73.08 73.09 73.10 73.11 73.12 73.13 73.14 73.15 Brandon, T. H.; Goniewicz, M. L.; Hanna, N. H.; Hatsukami, D. K.; Herbst, R. S.; Hobin, J. A.; Ostroff, J. S.; Shields, P. G.; Toll, B. A.; Tyne, C. A.; Viswanath, K.; Warren, G. W. (2015). "Electronic Nicotine Delivery Systems: A Policy Statement from the American Association for Cancer Research and the American Society of Clinical Oncology". Clinical Cancer Research. 21 (3): 514–525. doi:10.1158/1078-0432.CCR-14-2544. ISSN 1078-0432. PMID 25573384.
- ↑ 74.0 74.1 74.2 74.3 74.4 74.5 74.6 74.7 74.8 Durmowicz, E. L. (2014). "The impact of electronic cigarettes on the paediatric population". Tobacco Control. 23 (Supplement 2): ii41–ii46. doi:10.1136/tobaccocontrol-2013-051468. ISSN 0964-4563. PMC 3995262. PMID 24732163.
- ↑ 75.0 75.1 75.2 75.3 75.4 75.5 75.6 75.7 75.8 Weaver, Michael; Breland, Alison; Spindle, Tory; Eissenberg, Thomas (2014). "Electronic Cigarettes". Journal of Addiction Medicine. 8 (4): 234–240. doi:10.1097/ADM.0000000000000043. ISSN 1932-0620. PMC 4123220. PMID 25089953.
- ↑ 76.00 76.01 76.02 76.03 76.04 76.05 76.06 76.07 76.08 76.09 76.10 76.11 76.12 76.13 Ebbert, Jon O.; Agunwamba, Amenah A.; Rutten, Lila J. (2015). "Counseling Patients on the Use of Electronic Cigarettes". Mayo Clinic Proceedings. 90 (1): 128–134. doi:10.1016/j.mayocp.2014.11.004. ISSN 0025-6196. PMID 25572196.
- ↑ 77.00 77.01 77.02 77.03 77.04 77.05 77.06 77.07 77.08 77.09 77.10 77.11 77.12 77.13 77.14 77.15 77.16 Rowell, Temperance R.; Tarran, Robert (15 December 2015). "Will chronic e-cigarette use cause lung disease?". American Journal of Physiology. Lung Cellular and Molecular Physiology. 309 (12): L1398–L1409. doi:10.1152/ajplung.00272.2015. ISSN 1040-0605. PMC 4683316. PMID 26408554.
- ↑ 78.00 78.01 78.02 78.03 78.04 78.05 78.06 78.07 78.08 78.09 78.10 78.11 78.12 Cooke, Andrew; Fergeson, Jennifer; Bulkhi, Adeeb; Casale, Thomas B. (July 2015). "The Electronic Cigarette: The Good, the Bad, and the Ugly". The Journal of Allergy and Clinical Immunology: In Practice. 3 (4): 498–505. doi:10.1016/j.jaip.2015.05.022. ISSN 2213-2198. PMID 26164573.
- ↑ 79.00 79.01 79.02 79.03 79.04 79.05 79.06 79.07 79.08 79.09 79.10 79.11 79.12 79.13 79.14 79.15 79.16 79.17 79.18 Bertholon, J.F.; Becquemin, M.H.; Annesi-Maesano, I.; Dautzenberg, B. (2013). "Electronic Cigarettes: A Short Review". Respiration. 86 (5): 433–8. doi:10.1159/000353253. ISSN 1423-0356. PMID 24080743.
- ↑ 80.00 80.01 80.02 80.03 80.04 80.05 80.06 80.07 80.08 80.09 80.10 80.11 80.12 80.13 80.14 Bekki, Kanae; Uchiyama, Shigehisa; Ohta, Kazushi; Inaba, Yohei; Nakagome, Hideki; Kunugita, Naoki (2014). "Carbonyl Compounds Generated from Electronic Cigarettes". International Journal of Environmental Research and Public Health. 11 (11): 11192–11200. doi:10.3390/ijerph111111192. ISSN 1660-4601. PMC 4245608. PMID 25353061.
- ↑ 81.00 81.01 81.02 81.03 81.04 81.05 81.06 81.07 81.08 81.09 81.10 81.11 81.12 Orellana-Barrios, Menfil A.; Payne, Drew; Mulkey, Zachary; Nugent, Kenneth (2015). "Electronic cigarettes-a narrative review for clinicians". The American Journal of Medicine. 128 (7): 674–81. doi:10.1016/j.amjmed.2015.01.033. ISSN 0002-9343. PMID 25731134.
- ↑ 82.0 82.1 82.2 82.3 82.4 82.5 Jerry JM, Collins GB, Streem D (2015). "E-cigarettes: Safe to recommend to patients?". Cleve Clin J Med. 82 (8): 521–6. doi:10.3949/ccjm.82a.14054. PMID 26270431.
- ↑ 83.0 83.1 Dinardo, Perry; Rome, Ellen S. (2019). "Vaping: The new wave of nicotine addiction". Cleveland Clinic Journal of Medicine. 86 (12): 789–798. doi:10.3949/ccjm.86a.19118. ISSN 0891-1150. PMID 31821136.
- ↑ 84.0 84.1 84.2 84.3 84.4 Chaturvedi, Pankaj; Mishra, Aseem; Datta, Sourav; Sinukumar, Snita; Joshi, Poonam; Garg, Apurva (2015). "Harmful effects of nicotine". Indian Journal of Medical and Paediatric Oncology. 36 (1): 24. doi:10.4103/0971-5851.151771. ISSN 0971-5851. PMC 4363846. PMID 25810571.
- ↑ 85.0 85.1 McNeill 2018, p. 58.
- ↑ 86.0 86.1 Shinbashi, Meagan; Rubin, Bruce K. (2020). "Electronic cigarettes and e-cigarette/vaping product use associated lung injury (EVALI)". Paediatric Respiratory Reviews. 36: 87–91. doi:10.1016/j.prrv.2020.06.003. ISSN 1526-0542. PMID 32653465.
- ↑ 87.0 87.1 87.2 87.3 WHO 2016, p. 3.
- ↑ 88.0 88.1 88.2 88.3 88.4 Eltorai, Adam EM; Choi, Ariel R; Eltorai, Ashley Szabo (2018). "Impact of Electronic Cigarettes on Various Organ Systems". Respiratory Care. 64 (3): 328–336. doi:10.4187/respcare.06300. ISSN 0020-1324. PMID 30401756.
- ↑ 89.0 89.1 Famiglietti, Amber; Memoli, Jessica Wang; Khaitan, Puja Gaur (2021). "Are electronic cigarettes and vaping effective tools for smoking cessation? Limited evidence on surgical outcomes: a narrative review". Journal of Thoracic Disease. 13 (1): 384–395. doi:10.21037/jtd-20-2529. ISSN 2072-1439. PMC 7867832. PMID 33569219.
- ↑ 90.00 90.01 90.02 90.03 90.04 90.05 90.06 90.07 90.08 90.09 90.10 90.11 90.12 Cheng, T. (2014). "Chemical evaluation of electronic cigarettes". Tobacco Control. 23 (Supplement 2): ii11–ii17. doi:10.1136/tobaccocontrol-2013-051482. ISSN 0964-4563. PMC 3995255. PMID 24732157.
- ↑ 91.0 91.1 91.2 91.3 91.4 91.5 Hildick-Smith, Gordon J.; Pesko, Michael F.; Shearer, Lee; Hughes, Jenna M.; Chang, Jane; Loughlin, Gerald M.; Ipp, Lisa S. (2015). "A Practitioner's Guide to Electronic Cigarettes in the Adolescent Population". Journal of Adolescent Health. 57 (6): 574–9. doi:10.1016/j.jadohealth.2015.07.020. ISSN 1054-139X. PMID 26422289.
- ↑ 92.0 92.1 92.2 Lai, Lo; Qiu, Hongyu (April 2021). "Biological Toxicity of the Compositions in Electronic-Cigarette on Cardiovascular System". Journal of Cardiovascular Translational Research. 14 (2): 371–376. doi:10.1007/s12265-020-10060-1. ISSN 1937-5387. PMC 7855637. PMID 32748205.
- ↑ 93.0 93.1 Fernández, Esteve; Ballbè, Montse; Sureda, Xisca; Fu, Marcela; Saltó, Esteve; Martínez-Sánchez, Jose M. (2015). "Particulate Matter from Electronic Cigarettes and Conventional Cigarettes: a Systematic Review and Observational Study". Current Environmental Health Reports. 2 (4): 423–429. doi:10.1007/s40572-015-0072-x. ISSN 2196-5412. PMID 26452675.
- ↑ 94.0 94.1 94.2 94.3 94.4 Li, Liqiao; Lin, Yan; Xia, Tian; Zhu, Yifang (2020). "Effects of Electronic Cigarettes on Indoor Air Quality and Health". Annual Review of Public Health. 41 (1): 363–380. doi:10.1146/annurev-publhealth-040119-094043. ISSN 0163-7525. PMC 7346849. PMID 31910714.
 This article incorporates text by Liqiao Li, Yan Lin, Tian Xia, and Yifang Zhu1 available under the CC BY 4.0 license.
This article incorporates text by Liqiao Li, Yan Lin, Tian Xia, and Yifang Zhu1 available under the CC BY 4.0 license.
- ↑ 95.00 95.01 95.02 95.03 95.04 95.05 95.06 95.07 95.08 95.09 95.10 95.11 95.12 Chang, H. (2014). "Research gaps related to the environmental impacts of electronic cigarettes". Tobacco Control. 23 (Supplement 2): ii54–ii58. doi:10.1136/tobaccocontrol-2013-051480. ISSN 0964-4563. PMC 3995274. PMID 24732165.
- ↑ 96.0 96.1 96.2 96.3 96.4 96.5 Nowak, Dennis; Jörres, Rudolf A.; Rüther, Tobias (16 May 2014). "E-cigarettes--prevention, pulmonary health, and addiction". Deutsches Ärzteblatt International. 111 (20): 349–55. doi:10.3238/arztebl.2014.0349. PMC 4047602. PMID 24882626.
- ↑ Chapman 2015, p. 15.
- ↑ "E-cigarettes: An Emerging Public Health Challenge". Centers for Disease Control and Prevention. 20 October 2015.
- ↑ 99.0 99.1 99.2 99.3 Farsalinos, Konstantinos; LeHouezec, Jacques (2015). "Regulation in the face of uncertainty: the evidence on electronic nicotine delivery systems (e-cigarettes)". Risk Management and Healthcare Policy. 8: 157–167. doi:10.2147/RMHP.S62116. ISSN 1179-1594. PMC 4598199. PMID 26457058.
- ↑ Baraona, L. Kim; Lovelace, Dawn; Daniels, Julie L.; McDaniel, Linda (2017). "Tobacco Harms, Nicotine Pharmacology, and Pharmacologic Tobacco Cessation Interventions for Women". Journal of Midwifery & Women's Health. 62 (3): 253–269. doi:10.1111/jmwh.12616. ISSN 1526-9523. PMID 28556464.
- ↑ 101.00 101.01 101.02 101.03 101.04 101.05 101.06 101.07 101.08 101.09 101.10 101.11 101.12 101.13 101.14 101.15 101.16 101.17 101.18 101.19 101.20 101.21 101.22 101.23 101.24 101.25 101.26 101.27 101.28 Montjean, Debbie; Godin Pagé, Marie-Hélène; Bélanger, Marie-Claire; Benkhalifa, Moncef; Miron, Pierre (18 March 2023). "An Overview of E-Cigarette Impact on Reproductive Health". Life. 13 (3): 827. doi:10.3390/life13030827. PMID 36983982.
 This article incorporates text by Debbie Montjean, Marie-Hélène Godin Pagé, Marie-Claire Bélanger, Moncef Benkhalifa, and Pierre Miron available under the CC BY 4.0 license.
This article incorporates text by Debbie Montjean, Marie-Hélène Godin Pagé, Marie-Claire Bélanger, Moncef Benkhalifa, and Pierre Miron available under the CC BY 4.0 license.
- ↑ 102.0 102.1 102.2 102.3 Pisinger, Charlotta; Døssing, Martin (December 2014). "A systematic review of health effects of electronic cigarettes". Preventive Medicine. 69: 248–260. doi:10.1016/j.ypmed.2014.10.009. PMID 25456810.
- ↑ 103.0 103.1 Cahn, Z.; Siegel, M. (February 2011). "Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes?". Journal of Public Health Policy. 32 (1): 16–31. doi:10.1057/jphp.2010.41. PMID 21150942.
- ↑ 104.00 104.01 104.02 104.03 104.04 104.05 104.06 104.07 104.08 104.09 104.10 Virgili, Fabrizio; Nenna, Raffaella; Ben David, Shira; Mancino, Enrica; Di Mattia, Greta; Matera, Luigi; Petrarca, Laura; Midulla, Fabio (December 2022). "E-cigarettes and youth: an unresolved Public Health concern". Italian Journal of Pediatrics. 48 (1): 97. doi:10.1186/s13052-022-01286-7. PMC 9194784. PMID 35701844.
 This article incorporates text by Fabrizio Virgili, Raffaella Nenna, Shira Ben David, Enrica Mancino, Greta Di Mattia, Luigi Matera, Laura Petrarca, and Fabio Midulla available under the CC BY 4.0 license.
This article incorporates text by Fabrizio Virgili, Raffaella Nenna, Shira Ben David, Enrica Mancino, Greta Di Mattia, Luigi Matera, Laura Petrarca, and Fabio Midulla available under the CC BY 4.0 license.
- ↑ 105.00 105.01 105.02 105.03 105.04 105.05 105.06 105.07 105.08 105.09 105.10 105.11 105.12 105.13 105.14 Espinoza-Derout, Jorge; Shao, Xuesi M.; Lao, Candice J.; Hasan, Kamrul M.; Rivera, Juan Carlos; Jordan, Maria C.; Echeverria, Valentina; Roos, Kenneth P.; Sinha-Hikim, Amiya P.; Friedman, Theodore C. (7 April 2022). "Electronic Cigarette Use and the Risk of Cardiovascular Diseases". Frontiers in Cardiovascular Medicine. 9: 879726. doi:10.3389/fcvm.2022.879726. PMC 9021536. PMID 35463745.
 This article incorporates text by Jorge Espinoza-Derout, Xuesi M. Shao, Candice J. Lao, Kamrul M. Hasan, Juan Carlos Rivera, Maria C. Jordan, Valentina Echeverria, Kenneth P. Roos, Amiya P. Sinha-Hikim, and Theodore C. Friedman available under the CC BY 4.0 license.
This article incorporates text by Jorge Espinoza-Derout, Xuesi M. Shao, Candice J. Lao, Kamrul M. Hasan, Juan Carlos Rivera, Maria C. Jordan, Valentina Echeverria, Kenneth P. Roos, Amiya P. Sinha-Hikim, and Theodore C. Friedman available under the CC BY 4.0 license.
- ↑ 106.0 106.1 106.2 Cao, Dazhe James; Aldy, Kim; Hsu, Stephanie; McGetrick, Molly; Verbeck, Guido; De Silva, Imesha; Feng, Sing-yi (2020). "Review of Health Consequences of Electronic Cigarettes and the Outbreak of Electronic Cigarette, or Vaping, Product Use-Associated Lung Injury". Journal of Medical Toxicology. 16 (3): 295–310. doi:10.1007/s13181-020-00772-w. ISSN 1556-9039. PMC 7320089. PMID 32301069.
- ↑ Marcham, Cheryl L.; Springston, John P. (2019). "Electronic cigarettes in the indoor environment". Reviews on Environmental Health. 34 (2): 105–124. doi:10.1515/reveh-2019-0012. ISSN 2191-0308. PMID 31112510. S2CID 135122336.
- ↑ Bonner, Emily; Chang, Yvonne; Christie, Emerson; Colvin, Victoria; Cunningham, Brittany; Elson, Daniel; Ghetu, Christine; Huizenga, Juliana; Hutton, Sara J.; Kolluri, Siva K.; Maggio, Stephanie; Moran, Ian; Parker, Bethany; Rericha, Yvonne; Rivera, Brianna N.; Samon, Samantha; Schwichtenberg, Trever; Shankar, Prarthana; Simonich, Michael T.; Wilson, Lindsay B.; Tanguay, Robyn L. (September 2021). "The chemistry and toxicology of vaping". Pharmacology & Therapeutics. 225: 107837. doi:10.1016/j.pharmthera.2021.107837. ISSN 0163-7258. PMC 8263470. PMID 33753133.
- ↑ Ren, Michelle; Lotfipour, Shahrdad; Leslie, Frances (March 2022). "Unique effects of nicotine across the lifespan". Pharmacology Biochemistry and Behavior. 214: 173343. doi:10.1016/j.pbb.2022.173343. PMC 8904294. PMID 35122768.
- ↑ "Electronic Cigarettes – What are the health effects of using e-cigarettes?" (PDF). Centers for Disease Control and Prevention. 22 February 2018.
- ↑ 111.0 111.1 111.2 111.3 111.4 111.5 111.6 Seiler-Ramadas, Radhika; Sandner, Isabell; Haider, Sandra; Grabovac, Igor; Dorner, Thomas Ernst (2020). "Health effects of electronic cigarette (e‑cigarette) use on organ systems and its implications for public health". Wiener klinische Wochenschrift. doi:10.1007/s00508-020-01711-z. ISSN 0043-5325. PMID 32691214.
 This article incorporates text by Radhika Seiler-Ramadas, Isabell Sandner, Sandra Haider, Igor Grabovac, and Thomas Ernst Dorner available under the CC BY 4.0 license.
This article incorporates text by Radhika Seiler-Ramadas, Isabell Sandner, Sandra Haider, Igor Grabovac, and Thomas Ernst Dorner available under the CC BY 4.0 license.
- ↑ 112.0 112.1 112.2 112.3 Münzel, Thomas; Hahad, Omar; Kuntic, Marin; Keaney, John F; Deanfield, John E; Daiber, Andreas (2020). "Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes". European Heart Journal. 41 (41): 4057–4070. doi:10.1093/eurheartj/ehaa460. ISSN 0195-668X. PMC 7454514. PMID 32585699.
- ↑ Bhatnagar, Aruni; Whitsel, Laurie P.; Blaha, Michael J.; Huffman, Mark D.; Krishan-Sarin, Suchitra; Maa, John; Rigotti, Nancy; Robertson, Rose Marie; Warner, John J. (2019). "New and Emerging Tobacco Products and the Nicotine Endgame: The Role of Robust Regulation and Comprehensive Tobacco Control and Prevention: A Presidential Advisory From the American Heart Association". Circulation. 139 (19). doi:10.1161/CIR.0000000000000669. ISSN 0009-7322. PMID 30862181.
- ↑ 114.00 114.01 114.02 114.03 114.04 114.05 114.06 114.07 114.08 114.09 114.10 114.11 114.12 114.13 114.14 114.15 114.16 Pisinger, Charlotta; Rasmussen, Sofie K. Bergman (21 October 2022). "The Health Effects of Real-World Dual Use of Electronic and Conventional Cigarettes versus the Health Effects of Exclusive Smoking of Conventional Cigarettes: A Systematic Review". International Journal of Environmental Research and Public Health. 19 (20): 13687. doi:10.3390/ijerph192013687. PMC 9603628. PMID 36294263.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Charlotta Pisinger and Sofie K. Bergman Rasmussen available under the CC BY 4.0 license.
This article incorporates text by Charlotta Pisinger and Sofie K. Bergman Rasmussen available under the CC BY 4.0 license.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 9, Summary.
- ↑ 116.0 116.1 Wilder 2016, p. 127.
- ↑ 117.00 117.01 117.02 117.03 117.04 117.05 117.06 117.07 117.08 117.09 117.10 117.11 117.12 117.13 117.14 117.15 Marques, P; Piqueras, L; Sanz, MJ (18 May 2021). "An updated overview of e-cigarette impact on human health". Respiratory research. 22 (1): 151. doi:10.1186/s12931-021-01737-5. ISSN 1465-9921. PMC 8129966. PMID 34006276.
 This article incorporates text by Patrice Marques, Laura Piqueras, and Maria-Jesus Sanz available under the CC BY 4.0 license.
This article incorporates text by Patrice Marques, Laura Piqueras, and Maria-Jesus Sanz available under the CC BY 4.0 license.
- ↑ 118.0 118.1 118.2 118.3 118.4 118.5 Strongin, Robert M. (12 June 2019). "E-Cigarette Chemistry and Analytical Detection". Annual review of analytical chemistry (Palo Alto, Calif.). Annual Reviews. 12 (1): 23–39. doi:10.1146/annurev-anchem-061318-115329. ISSN 1936-1327. PMC 6565477. PMID 30848928.
- ↑ 119.0 119.1 119.2 119.3 "Alternative tobacco products use and its impact on urologic health – Will the lesser evil still be evil? A commentary and review of literature". Central European Journal of Urology. 74 (2). May 2021. doi:10.5173/ceju.2021.0110.
- ↑ 120.0 120.1 120.2 Hamann, Stephen L.; Kungskulniti, Nipapun; Charoenca, Naowarut; Kasemsup, Vijj; Ruangkanchanasetr, Suwanna; Jongkhajornpong, Passara (22 September 2023). "Electronic Cigarette Harms: Aggregate Evidence Shows Damage to Biological Systems". International Journal of Environmental Research and Public Health. 20 (19): 6808. doi:10.3390/ijerph20196808. PMC 10572885. PMID 37835078.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Stephen L Hamann, Nipapun Kungskulniti, Naowarut Charoenca, Vijj Kasemsup, Suwanna Ruangkanchanasetr, and Passara Jongkhajornpongs available under the CC BY 4.0 license.
This article incorporates text by Stephen L Hamann, Nipapun Kungskulniti, Naowarut Charoenca, Vijj Kasemsup, Suwanna Ruangkanchanasetr, and Passara Jongkhajornpongs available under the CC BY 4.0 license.
- ↑ 121.00 121.01 121.02 121.03 121.04 121.05 121.06 121.07 121.08 121.09 121.10 121.11 121.12 121.13 121.14 Hua, My; Talbot, Prue (2016). "Potential health effects of electronic cigarettes: A systematic review of case reports". Preventive Medicine Reports. 4: 169–178. doi:10.1016/j.pmedr.2016.06.002. ISSN 2211-3355. PMC 4929082. PMID 27413679.
 This article incorporates text by My Hua and Prue Talbot available under the CC BY 4.0 license.
This article incorporates text by My Hua and Prue Talbot available under the CC BY 4.0 license.
- ↑ 122.00 122.01 122.02 122.03 122.04 122.05 122.06 122.07 122.08 122.09 122.10 122.11 122.12 122.13 122.14 122.15 122.16 122.17 122.18 122.19 122.20 122.21 122.22 122.23 122.24 122.25 122.26 122.27 122.28 122.29 122.30 122.31 122.32 122.33 122.34 122.35 122.36 122.37 122.38 122.39 122.40 122.41 122.42 122.43 122.44 122.45 122.46 122.47 122.48 122.49 122.50 122.51 122.52 122.53 122.54 122.55 122.56 122.57 122.58 122.59 122.60 122.61 122.62 122.63 122.64 122.65 122.66 122.67 122.68 122.69 122.70 122.71 Górna, Ilona; Napierala, Marta; Florek, Ewa (2020). "Electronic Cigarette Use and Metabolic Syndrome Development: A Critical Review". Toxics. 8 (4): 105. doi:10.3390/toxics8040105. ISSN 2305-6304. PMC 7711672. PMID 33212878.
 This article incorporates text by Ilona Górna, Marta Napierala, Ewa Florek available under the CC BY 4.0 license.
This article incorporates text by Ilona Górna, Marta Napierala, Ewa Florek available under the CC BY 4.0 license.
- ↑ 123.0 123.1 Gorlova, Olga Y; Xu, Ying; Guo, Yanfang; Liu, Kaiqian; Liu, Zheng; Wang, Xiaobo (2016). "E-Cigarette Awareness, Use, and Harm Perception among Adults: A Meta-Analysis of Observational Studies". PLOS ONE. 11 (11): e0165938. Bibcode:2016PLoSO..1165938X. doi:10.1371/journal.pone.0165938. ISSN 1932-6203. PMC 5115669. PMID 27861501.
- ↑ Vasiljevic, Milica; St John Wallis, Amelia; Codling, Saphsa; Couturier, Dominique-Laurent; Sutton, Stephen; Marteau, Theresa M (2018). "E-cigarette adverts and children's perceptions of tobacco smoking harms: an experimental study and meta-analysis". BMJ Open. 8 (7): e020247. doi:10.1136/bmjopen-2017-020247. ISSN 2044-6055. PMC 6082488. PMID 30012646.
 This article incorporates text by Milica Vasiljevic, Amelia St John Wallis, Saphsa Codlin, Dominique-Laurent Couturier, Stephen Sutton, and Theresa M Marteau available under the CC BY 4.0 license.
This article incorporates text by Milica Vasiljevic, Amelia St John Wallis, Saphsa Codlin, Dominique-Laurent Couturier, Stephen Sutton, and Theresa M Marteau available under the CC BY 4.0 license.
- ↑ 125.0 125.1 125.2 125.3 125.4 125.5 125.6 Kaur, Gagandeep; Pinkston, Rakeysha; Mclemore, Benathel; Dorsey, Waneene C.; Batra, Sanjay (2018). "Immunological and toxicological risk assessment of e-cigarettes". European Respiratory Review. 27 (147): 170119. doi:10.1183/16000617.0119-2017. ISSN 0905-9180. PMC 9489161. PMID 29491036.
- ↑ 126.0 126.1 126.2 126.3 126.4 126.5 126.6 126.7 Benowitz, Neal L.; Fraiman, Joseph B. (2017). "Cardiovascular effects of electronic cigarettes". Nature Reviews Cardiology. 14 (8): 447–456. doi:10.1038/nrcardio.2017.36. ISSN 1759-5002. PMC 5519136. PMID 28332500.
- ↑ 127.0 127.1 Sosnowski, Tomasz R.; Odziomek, Marcin (2018). "Particle Size Dynamics: Toward a Better Understanding of Electronic Cigarette Aerosol Interactions With the Respiratory System". Frontiers in Physiology. 9: 853. doi:10.3389/fphys.2018.00853. ISSN 1664-042X. PMC 6046408. PMID 30038580.
 This article incorporates text by Tomasz R. Sosnowski and Marcin Odziomek available under the CC BY 4.0 license.
This article incorporates text by Tomasz R. Sosnowski and Marcin Odziomek available under the CC BY 4.0 license.
- ↑ "E-Cigarettes". Oncology Times. 36 (15): 49–50. August 2014. doi:10.1097/01.COT.0000453432.31465.77.
- ↑ "Nicotine addiction". Health Canada. 7 March 2013.
- ↑ "DrugFacts: Cigarettes and Other Tobacco Products". National Institute on Drug Abuse. May 2016.
- ↑ 131.00 131.01 131.02 131.03 131.04 131.05 131.06 131.07 131.08 131.09 131.10 131.11 Clapp, Phillip W.; Jaspers, Ilona (November 2017). "Electronic Cigarettes: Their Constituents and Potential Links to Asthma". Current Allergy and Asthma Reports. 17 (11): 79. doi:10.1007/s11882-017-0747-5. ISSN 1529-7322. PMC 5995565. PMID 28983782.
- ↑ Detailed reference list is located at a separate image page.
- ↑ Pham, Kien; DeFina, Sam; Wang, He (24 February 2021). "E-Cigarettes Promote Macrophage-Tumor Cells Crosstalk: Focus on Breast Carcinoma Progression and Lung Metastasis". Exploratory Research and Hypothesis in Medicine. 000 (000): 000–000. doi:10.14218/erhm.2021.00002. PMC 9005083. PMID 35419501.
- ↑ Ebersole, Jeffrey; Samburova, Vera; Son, Yeongkwon; Cappelli, David; Demopoulos, Christina; Capurro, Antonina; Pinto, Andres; Chrzan, Brian; Kingsley, Karl; Howard, Katherine; Clark, Nathaniel; Khlystov, Andrey (2020). "Harmful chemicals emitted from electronic cigarettes and potential deleterious effects in the oral cavity". Tobacco Induced Diseases. 18 (May). doi:10.18332/tid/116988. ISSN 1617-9625. PMC 7233525. PMID 32435175.
 This article incorporates text by Jeffrey Ebersole, Vera Samburova, Yeongkwon Son, David Cappelli, Christina Demopoulos, Antonina Capurro, Andres Pinto, Brian Chrzan, Karl Kingsley, Katherine Howard, Nathaniel Clark, and Andrey Khlystov available under the CC BY 4.0 license.
This article incorporates text by Jeffrey Ebersole, Vera Samburova, Yeongkwon Son, David Cappelli, Christina Demopoulos, Antonina Capurro, Andres Pinto, Brian Chrzan, Karl Kingsley, Katherine Howard, Nathaniel Clark, and Andrey Khlystov available under the CC BY 4.0 license.
- ↑ 135.0 135.1 135.2 135.3 135.4 135.5 Hendlin, Yogi H.; Vora, Manali; Elias, Jesse; Ling, Pamela M. (2019). "Financial Conflicts of Interest and Stance on Tobacco Harm Reduction: A Systematic Review". American Journal of Public Health. 109 (7): e1–e8. doi:10.2105/AJPH.2019.305106. ISSN 0090-0036. PMC 6603486. PMID 31095414.
- ↑ 136.0 136.1 Meng, Xing-chen; Guo, Xin-xin; Peng, Zhen-yan; Wang, Chun; Liu, Ran (27 March 2023). "Acute effects of electronic cigarettes on vascular endothelial function: a systematic review and meta-analysis of randomized controlled trials". European Journal of Preventive Cardiology. 30 (5): 425–435. doi:10.1093/eurjpc/zwac248. PMID 36316290.
- ↑ 137.0 137.1 137.2 Sobczak, Andrzej; Kosmider, Leon; Koszowski, Bartosz; Goniewicz, Maciej Ł. (2020). "E-cigarettes and their impact on health: from pharmacology to clinical implications". Polish Archives of Internal Medicine. doi:10.20452/pamw.15229. ISSN 1897-9483. PMC 7685201. PMID 32155137.
- ↑ 138.0 138.1 138.2 Kashyap, Vivek K.; Dhasmana, Anupam; Massey, Andrew; Kotnala, Sudhir; Zafar, Nadeem; Jaggi, Meena; Yallapu, Murali M.; Chauhan, Subhash C. (9 September 2020). "Smoking and COVID-19: Adding Fuel to the Flame". International Journal of Molecular Sciences. 21 (18): 6581. doi:10.3390/ijms21186581. PMC 7555793. PMID 32916821.
 This article incorporates text by Vivek K. Kashyap, Anupam Dhasmana, Andrew Massey, Sudhir Kotnala, Nadeem Zafar, Meena Jaggi, Murali M. Yallapu, and Subhash C. Chauhan available under the CC BY 4.0 license.
This article incorporates text by Vivek K. Kashyap, Anupam Dhasmana, Andrew Massey, Sudhir Kotnala, Nadeem Zafar, Meena Jaggi, Murali M. Yallapu, and Subhash C. Chauhan available under the CC BY 4.0 license.
- ↑ 139.0 139.1 McAlinden, Kielan Darcy; Eapen, Mathew Suji; Lu, Wenying; Sharma, Pawan; Sohal, Sukhwinder Singh (2020). "The rise of electronic nicotine delivery systems and the emergence of electronic-cigarette-driven disease". American Journal of Physiology-Lung Cellular and Molecular Physiology. 319 (4): L585–L595. doi:10.1152/ajplung.00160.2020. ISSN 1040-0605. PMID 32726146.
- ↑ 140.0 140.1 140.2 140.3 Walley, Susan C.; Wilson, Karen M.; Winickoff, Jonathan P.; Groner, Judith (2019). "A Public Health Crisis: Electronic Cigarettes, Vape, and JUUL". Pediatrics. 143 (6): e20182741. doi:10.1542/peds.2018-2741. ISSN 0031-4005. PMID 31122947.
- ↑ "Electronic Cigarettes – Are e-cigarettes less harmful than regular cigarettes?". Centers for Disease Control and Prevention. 2 November 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 142.0 142.1 142.2 142.3 Oh, Anne Y.; Kacker, Ashutosh (December 2014). "Do electronic cigarettes impart a lower potential disease burden than conventional tobacco cigarettes?: Review on e-cigarette vapor versus tobacco smoke". The Laryngoscope. 124 (12): 2702–2706. doi:10.1002/lary.24750. PMID 25302452.
- ↑ 143.0 143.1 143.2 MacDonald, Marjorie; O'Leary, Renee; Stockwell, Tim; Reist, Dan (2016). "Clearing the air: protocol for a systematic meta-narrative review on the harms and benefits of e-cigarettes and vapour devices". Systematic Reviews. 5 (1): 85. doi:10.1186/s13643-016-0264-y. ISSN 2046-4053. PMC 4875675. PMID 27209032.
 This article incorporates text by Marjorie MacDonald, Renee O'Leary, Tim Stockwell, and Dan Reist available under the CC BY 4.0 license.
This article incorporates text by Marjorie MacDonald, Renee O'Leary, Tim Stockwell, and Dan Reist available under the CC BY 4.0 license.
- ↑ 144.0 144.1 144.2 144.3 144.4 Dagaonkar RS, R.S.; Udwadi, Z.F. (2014). "Water pipes and E-cigarettes: new faces of an ancient enemy" (PDF). Journal of the Association of Physicians of India. 62 (4): 324–328. PMID 25327035.
- ↑ 145.0 145.1 145.2 145.3 145.4 Burstyn, Igor (9 January 2014). "Peering through the mist: systematic review of what the chemistry of contaminants in electronic cigarettes tells us about health risks". BMC Public Health. 14 (1): 18. doi:10.1186/1471-2458-14-18. ISSN 1471-2458. PMC 3937158. PMID 24406205.
- ↑ "Regulation of Electronic Cigarettes ("E-Cigarettes")" (PDF). National Association of County and City Health Officials. Archived from the original (PDF) on 6 November 2014.
- ↑ 147.0 147.1 147.2 147.3 147.4 Pepper, J. K.; Brewer, N. T. (2013). "Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review". Tobacco Control. 23 (5): 375–384. doi:10.1136/tobaccocontrol-2013-051122. ISSN 0964-4563. PMC 4520227. PMID 24259045.
- ↑ McCausland, Kahlia; Maycock, Bruce; Jancey, Jonine (2017). "The messages presented in online electronic cigarette promotions and discussions: a scoping review protocol". BMJ Open. 7 (11): e018633. doi:10.1136/bmjopen-2017-018633. ISSN 2044-6055. PMC 5695349. PMID 29122804.
- ↑ "American Cancer Society Position Statement on Electronic Cigarettes". American Cancer Society. 2023.
- ↑ "Ways to quit". Canadian Cancer Society. 2016. Archived from the original on 2015-12-08. Retrieved 2015-02-24.
- ↑ "Nicotine products can help people to cut down before quitting smoking". National Institute for Health and Care Excellence. June 2013. Archived from the original on 2015-11-19. Retrieved 2015-02-24.
- ↑ "Standards of Medical Care in Diabetes--2015: Summary of Revisions". Diabetes Care. 54 (38): S25. 2015. doi:10.2337/dc15-S003. PMID 25537706.
- ↑ Smith, Nikki (20 January 2016). "Headlines about e-cigarettes don't mean they're 'not safer than tobacco'". Cancer Research UK.
- ↑ 154.0 154.1 Greenhill, Richard; Dawkins, Lynne; Notley, Caitlin; Finn, Mark D.; Turner, John J.D. (2016). "Adolescent Awareness and Use of Electronic Cigarettes: A Review of Emerging Trends and Findings". Journal of Adolescent Health. 59 (6): 612–619. doi:10.1016/j.jadohealth.2016.08.005. ISSN 1054-139X. PMID 27693128.
- ↑ 155.0 155.1 155.2 155.3 155.4 155.5 Palazzolo, Dominic L. (November 2013). "Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review". Frontiers in Public Health. 1 (56): 56. doi:10.3389/fpubh.2013.00056. PMC 3859972. PMID 24350225.
 This article incorporates text by Dominic L. Palazzolo available under the CC BY 3.0 license.
This article incorporates text by Dominic L. Palazzolo available under the CC BY 3.0 license.
- ↑ 156.0 156.1 Nansseu, Jobert Richie N.; Bigna, Jean Joel R. (2016). "Electronic Cigarettes for Curbing the Tobacco-Induced Burden of Noncommunicable Diseases: Evidence Revisited with Emphasis on Challenges in Sub-Saharan Africa". Pulmonary Medicine. 2016: 1–9. doi:10.1155/2016/4894352. ISSN 2090-1836. PMC 5220510. PMID 28116156.
 This article incorporates text by Jobert Richie N. Nansseu and Jean Joel R. Bigna available under the CC BY 4.0 license.
This article incorporates text by Jobert Richie N. Nansseu and Jean Joel R. Bigna available under the CC BY 4.0 license.
- ↑ 157.0 157.1 157.2 157.3 157.4 157.5 Drope, Jeffrey; Cahn, Zachary; Kennedy, Rosemary; Liber, Alex C.; Stoklosa, Michal; Henson, Rosemarie; Douglas, Clifford E.; Drope, Jacqui (2017). "Key issues surrounding the health impacts of electronic nicotine delivery systems (ENDS) and other sources of nicotine". CA: A Cancer Journal for Clinicians. 67 (6): 449–471. doi:10.3322/caac.21413. ISSN 0007-9235. PMID 28961314.
- ↑ 158.00 158.01 158.02 158.03 158.04 158.05 158.06 158.07 158.08 158.09 158.10 158.11 158.12 158.13 158.14 158.15 158.16 158.17 158.18 158.19 158.20 158.21 158.22 158.23 158.24 158.25 158.26 158.27 158.28 158.29 158.30 158.31 158.32 158.33 158.34 158.35 158.36 158.37 158.38 158.39 158.40 158.41 158.42 158.43 158.44 158.45 158.46 158.47 158.48 158.49 158.50 158.51 158.52 158.53 158.54 158.55 158.56 158.57 158.58 158.59 158.60 158.61 Glantz, Stanton A.; Bareham, David W. (January 2018). "E-Cigarettes: Use, Effects on Smoking, Risks, and Policy Implications". Annual Review of Public Health. 39 (1): 215–235. doi:10.1146/annurev-publhealth-040617-013757. ISSN 0163-7525. PMC 6251310. PMID 29323609.
 This article incorporates text by Stanton A. Glantz and David W. Bareham available under the CC BY 4.0 license.
This article incorporates text by Stanton A. Glantz and David W. Bareham available under the CC BY 4.0 license.
- ↑ Bush, Ashley M.; Holsinger, James W.; Prybil, Lawrence D. (2016). "Employing the Precautionary Principle to Evaluate the Use of E-Cigarettes". Frontiers in Public Health. 4: 5. doi:10.3389/fpubh.2016.00005. ISSN 2296-2565. PMC 4740382. PMID 26870723.
- ↑ 160.0 160.1 160.2 160.3 Traboulsi, Hussein; Cherian, Mathew; Abou Rjeili, Mira; Preteroti, Matthew; Bourbeau, Jean; Smith, Benjamin M.; Eidelman, David H.; Baglole, Carolyn J. (15 May 2020). "Inhalation Toxicology of Vaping Products and Implications for Pulmonary Health". International Journal of Molecular Sciences. 21 (10): 3495. doi:10.3390/ijms21103495. ISSN 1422-0067. PMC 7278963. PMID 32429092.
 This article incorporates text by Hussein Traboulsi, Mathew Cherian, Mira Abou Rjeili, Matthew Preteroti, Jean Bourbeau, Benjamin M. Smith, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
This article incorporates text by Hussein Traboulsi, Mathew Cherian, Mira Abou Rjeili, Matthew Preteroti, Jean Bourbeau, Benjamin M. Smith, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
- ↑ Banks E, AM; Yazidjoglou, A; Brown, S; Nguyen, M; Martin, M; Beckwith, K; Daluwatta, A; Campbell, S; Joshy, G (20 March 2023). "Electronic cigarettes and health outcomes: umbrella and systematic review of the global evidence". The Medical journal of Australia. doi:10.5694/mja2.51890. PMID 36939271.
- ↑ 162.0 162.1 162.2 162.3 162.4 162.5 162.6 162.7 162.8 162.9 Bhatnagar, A.; Whitsel, L. P.; Ribisl, K. M.; Bullen, C.; Chaloupka, F.; Piano, M. R.; Robertson, R. M.; McAuley, T.; Goff, D.; Benowitz, N. (24 August 2014). "Electronic Cigarettes: A Policy Statement From the American Heart Association". Circulation. 130 (16): 1418–1436. doi:10.1161/CIR.0000000000000107. PMID 25156991.
- ↑ Bullen, Chris; Knight-West, Oliver (2016). "E-cigarettes for the management of nicotine addiction". Substance Abuse and Rehabilitation. 7: 111–118. doi:10.2147/SAR.S94264. ISSN 1179-8467. PMC 4993405. PMID 27574480.
- ↑ 164.0 164.1 164.2 164.3 164.4 Smith, L; Brar, K; Srinivasan, K; Enja, M; Lippmann, S (June 2016). "E-cigarettes: How "safe" are they?". The Journal of Family Practice. 65 (6): 380–385. PMID 27474819.
- ↑ Hartmann-Boyce, Jamie; Begh, Rachna; Aveyard, Paul (2018). "Electronic cigarettes for smoking cessation". BMJ. 360: j5543. doi:10.1136/bmj.j5543. ISSN 0959-8138. PMID 29343486.
- ↑ 166.0 166.1 166.2 166.3 166.4 166.5 166.6 Zborovskaya, Y (2017). "E-Cigarettes and Smoking Cessation: A Primer for Oncology Clinicians". Clinical Journal of Oncology Nursing. 21 (1): 54–63. doi:10.1188/17.CJON.54-63. PMID 28107337.
- ↑ 167.0 167.1 Wang, Richard J.; Bhadriraju, Sudhamayi; Glantz, Stanton A. (February 2021). "E-Cigarette Use and Adult Cigarette Smoking Cessation: A Meta-Analysis". American Journal of Public Health. 111 (2): 230–246. doi:10.2105/AJPH.2020.305999. ISSN 0090-0036. PMC 7811087. PMID 33351653.
- ↑ Vajdi, Borna; Tuktamyshov, Rasikh (2020). "Electronic cigarettes — myocardial infarction, hemodynamic compromise during pregnancy, and systolic and diastolic dysfunction: Minireview". World Journal of Cardiology. 12 (10): 475–483. doi:10.4330/wjc.v12.i10.475. ISSN 1949-8462. PMC 7596422. PMID 33173566.
- ↑ 169.0 169.1 169.2 Kim, Jinyung; Lee, Serim; Chun, JongSerl (14 September 2022). "An International Systematic Review of Prevalence, Risk, and Protective Factors Associated with Young People's E-Cigarette Use". International journal of environmental research and public health. MDPI AG. 19 (18): 11570. doi:10.3390/ijerph191811570. ISSN 1660-4601. PMC 9517489. PMID 36141845.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Jinyung Kim, Serim Lee, and JongSerl Chun available under the CC BY 4.0 license.
This article incorporates text by Jinyung Kim, Serim Lee, and JongSerl Chun available under the CC BY 4.0 license.
- ↑ "Electronic Cigarettes – What's the bottom line?" (PDF). Centers for Disease Control and Prevention. 22 February 2018.
- ↑ 171.0 171.1 171.2 171.3 171.4 171.5 "Electronic Cigarettes – An Overview" (PDF). German Cancer Research Center. 2013.
- ↑ 172.0 172.1 172.2 Evans, S. E.; Hoffman, A. C. (2014). "Electronic cigarettes: abuse liability, topography and subjective effects". Tobacco Control. 23 (Supplement 2): ii23–ii29. doi:10.1136/tobaccocontrol-2013-051489. ISSN 0964-4563. PMC 3995256. PMID 24732159.
- ↑ 173.0 173.1 Sanford, Sanford; Goebel, Lynne (2014). "E-cigarettes: an up to date review and discussion of the controversy". W V Med J. 110 (4): 10–5. PMID 25322582.
- ↑ 174.00 174.01 174.02 174.03 174.04 174.05 174.06 174.07 174.08 174.09 174.10 174.11 Breland, Alison; Soule, Eric; Lopez, Alexa; Ramôa, Carolina; El-Hellani, Ahmad; Eissenberg, Thomas (2017). "Electronic cigarettes: what are they and what do they do?". Annals of the New York Academy of Sciences. 1394 (1): 5–30. Bibcode:2017NYASA1394....5B. doi:10.1111/nyas.12977. ISSN 0077-8923. PMC 4947026. PMID 26774031.
- ↑ Bullen, Christopher (2014). "Electronic Cigarettes for Smoking Cessation". Current Cardiology Reports. 16 (11): 538. doi:10.1007/s11886-014-0538-8. ISSN 1523-3782. PMID 25303892.
- ↑ Caponnetto, P.; Russo, C.; Bruno, C.M.; Alamo, A.; Amaradio, M.D.; Polosa, R. (March 2013). "Electronic cigarette: a possible substitute for cigarette dependence". Monaldi Archives for Chest Disease. 79 (1): 12–19. doi:10.4081/monaldi.2013.104. ISSN 1122-0643. PMID 23741941.
- ↑ Wilder 2016, p. 87.
- ↑ Li, Gerard; Saad, Sonia; Oliver, Brian; Chen, Hui (2018). "Heat or Burn? Impacts of Intrauterine Tobacco Smoke and E-Cigarette Vapor Exposure on the Offspring's Health Outcome". Toxics. 6 (3): 43. doi:10.3390/toxics6030043. ISSN 2305-6304. PMC 6160993. PMID 30071638.
 This article incorporates text by Gerard Li, Sonia Saad, Brian G. Oliver, and Hui Chen available under the CC BY 4.0 license.
This article incorporates text by Gerard Li, Sonia Saad, Brian G. Oliver, and Hui Chen available under the CC BY 4.0 license.
- ↑ 179.0 179.1 179.2 179.3 Hartmann-Boyce, Jamie; McRobbie, Hayden; Lindson, Nicola; Bullen, Chris; Begh, Rachna; Theodoulou, Annika; Notley, Caitlin; Rigotti, Nancy A; Turner, Tari; Butler, Ailsa R; Fanshawe, Thomas R; Hajek, Peter (29 April 2021). "Electronic cigarettes for smoking cessation". Cochrane Database of Systematic Reviews. 2021 (6). doi:10.1002/14651858.CD010216.pub5. ISSN 1465-1858. PMC 8092424. PMID 33913154.
- ↑ 180.0 180.1 Zhao, Kai; Li, Jing; Zhou, Ping; Xu, Ling; Yang, Mingfei (14 November 2022). "Is electronic cigarette use a risk factor for stroke? A systematic review and meta-analysis". Tobacco Induced Diseases. 20 (November): 1–8. doi:10.18332/tid/154364. PMC 9661377. PMID 36447455.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Kai Zhao, Jing Li, Ping Zhou, Ling Xu, and Mingfei Yang available under the CC BY 4.0 license.
This article incorporates text by Kai Zhao, Jing Li, Ping Zhou, Ling Xu, and Mingfei Yang available under the CC BY 4.0 license.
- ↑ 181.00 181.01 181.02 181.03 181.04 181.05 181.06 181.07 181.08 181.09 181.10 Lyzwinski, Lynnette Nathalie; Naslund, John A.; Miller, Christopher J.; Eisenberg, Mark J. (11 April 2022). "Global youth vaping and respiratory health: epidemiology, interventions, and policies". npj Primary Care Respiratory Medicine. 32 (1): 14. doi:10.1038/s41533-022-00277-9. PMC 9001701. PMID 35410990.
 This article incorporates text by Lynnette Nathalie Lyzwinski, John A. Naslund, Christopher J. Miller, and Mark J. Eisenberg available under the CC BY 4.0 license.
This article incorporates text by Lynnette Nathalie Lyzwinski, John A. Naslund, Christopher J. Miller, and Mark J. Eisenberg available under the CC BY 4.0 license.
- ↑ McNeill 2018, p. 175.
- ↑ McNeill 2015, p. 76.
- ↑ 184.0 184.1 Couch, Elizabeth T.; Chaffee, Benjamin W.; Gansky, Stuart A.; Walsh, Margaret M. (July 2016). "The changing tobacco landscape". The Journal of the American Dental Association. 147 (7): 561–569. doi:10.1016/j.adaj.2016.01.008. ISSN 0002-8177. PMC 4925234. PMID 26988178.
- ↑ Camenga, Deepa R.; Tindle, Hilary A. (2018). "Weighing the Risks and Benefits of Electronic Cigarette Use in High-Risk Populations". Medical Clinics of North America. 102 (4): 765–779. doi:10.1016/j.mcna.2018.03.002. ISSN 0025-7125. PMID 29933828.
- ↑ 186.0 186.1 186.2 186.3 Armendáriz-Castillo, Isaac; Guerrero, Santiago; Vera-Guapi, Antonella; Cevallos-Vilatuña, Tiffany; García-Cárdenas, Jennyfer M.; Guevara-Ramírez, Patricia; López-Cortés, Andrés; Pérez-Villa, Andy; Yumiceba, Verónica; Zambrano, Ana K.; Leone, Paola E.; Paz-y-Miño, César (23 December 2019). "Genotoxic and Carcinogenic Potential of Compounds Associated with Electronic Cigarettes: A Systematic Review". BioMed Research International. 2019: 1–8. doi:10.1155/2019/1386710. PMC 6948324. PMID 31950030.}
 This article incorporates text by Isaac Armendáriz-Castillo, Santiago Guerrero, Antonella Vera-Guapi, Tiffany Cevallos-Vilatuña, Jennyfer M García-Cárdenas, Patricia Guevara-Ramírez, Andrés López-Cortés, Andy Pérez-Villa, Verónica Yumiceba, Ana K Zambrano, Paola E Leone, and César Paz-Y-Miño available under the CC BY 4.0 license.
This article incorporates text by Isaac Armendáriz-Castillo, Santiago Guerrero, Antonella Vera-Guapi, Tiffany Cevallos-Vilatuña, Jennyfer M García-Cárdenas, Patricia Guevara-Ramírez, Andrés López-Cortés, Andy Pérez-Villa, Verónica Yumiceba, Ana K Zambrano, Paola E Leone, and César Paz-Y-Miño available under the CC BY 4.0 license.
- ↑ Legg, Tess; Legendre, Michél; Gilmore, Anna B (November 2021). "Paying lip service to publication ethics: scientific publishing practices and the Foundation for a Smoke-Free World". Tobacco Control. 30 (e1): e65–e72. doi:10.1136/tobaccocontrol-2020-056003. PMC 8606453. PMID 33911028.
- ↑ Burki, Talha Khan (June 2021). "Conflicts of interest in tobacco industry-funded research". The Lancet Oncology. 22 (6): 758. doi:10.1016/S1470-2045(21)00281-3. PMID 33965060.
- ↑ 189.0 189.1 Chaffee, Benjamin W.; Couch, Elizabeth T.; Ryder, Mark I. (2016). "The tobacco-using periodontal patient: role of the dental practitioner in tobacco cessation and periodontal disease management". Periodontology 2000. 71 (1): 52–64. doi:10.1111/prd.12120. ISSN 0906-6713. PMC 4842013. PMID 27045430.
- ↑ 190.0 190.1 Bhatnagar, Aruni (2016). "Cardiovascular Perspective of the Promises and Perils of E-Cigarettes". Circulation Research. 118 (12): 1872–1875. doi:10.1161/CIRCRESAHA.116.308723. ISSN 0009-7330. PMC 5505630. PMID 27283531.
- ↑ Chen, Jinsong; Bullen, Chris; Dirks, Kim (2017). "A Comparative Health Risk Assessment of Electronic Cigarettes and Conventional Cigarettes". International Journal of Environmental Research and Public Health. 14 (4): 382. doi:10.3390/ijerph14040382. ISSN 1660-4601. PMC 5409583. PMID 28379177.
 This article incorporates text by Jinsong Chen, Chris Bullen, and Kim Dirks available under the CC BY 4.0 license.
This article incorporates text by Jinsong Chen, Chris Bullen, and Kim Dirks available under the CC BY 4.0 license.
- ↑ 192.0 192.1 Sharma, H; Ruikar, M (April 2023). "Electronic cigarettes: Ally or an enemy in combating tobacco-use-associated diseases - An integrative review". Indian journal of dental research : official publication of Indian Society for Dental Research. 34 (2): 216–222. doi:10.4103/ijdr.ijdr_890_21. PMID 37787216.
- ↑ Priemer, David S.; Gravenmier, Curtis; Batouli, Amir; Hooper, Jody E. (1 November 2020). "Overview of Pathologic Findings of Vaping in the Context of an Autopsy Patient With Chronic Injury". Archives of Pathology & Laboratory Medicine. 144 (11): 1408–1413. doi:10.5858/arpa.2019-0637-RA. PMID 32383974.
- ↑ 194.00 194.01 194.02 194.03 194.04 194.05 194.06 194.07 194.08 194.09 194.10 194.11 194.12 194.13 194.14 194.15 194.16 Tobin, Stacey C. (22 September 2021). "Developmental Nicotine Exposure in Mice Affects Epigenetic Factors in the Brain Across Multiple Generations". National Institute on Drug Abuse.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Chatkin, José Miguel; Dullius, Cynthia Rocha (2016). "The management of asthmatic smokers". Asthma Research and Practice. 2 (1): 10. doi:10.1186/s40733-016-0025-7. ISSN 2054-7064. PMC 5142412. PMID 27965778.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ↑ Buck, Jordan M; Yu, Li; Knopik, Valerie S; Stitzel, Jerry A (14 September 2021). "DNA methylome perturbations: an epigenetic basis for the emergingly heritable neurodevelopmental abnormalities associated with maternal smoking and maternal nicotine exposure". Biology of Reproduction. 105 (3): 644–666. doi:10.1093/biolre/ioab138. PMC 8444709. PMID 34270696.
- ↑ 197.0 197.1 197.2 197.3 197.4 197.5 197.6 Serror, K.; Chaouat, M.; Legrand, Matthieu M.; Depret, F.; Haddad, J.; Malca, N.; Mimoun, M.; Boccara, D. (2018). "Burns caused by electronic vaping devices (e-cigarettes): A new classification proposal based on mechanisms". Burns. 44 (3): 544–548. doi:10.1016/j.burns.2017.09.005. ISSN 0305-4179. PMID 29056367.
- ↑ 198.0 198.1 198.2 198.3 198.4 198.5 Tzortzi, Anna; Kapetanstrataki, Melpo; Evangelopoulou, Vaso; Behrakis, Panagiotis (2020). "A Systematic Literature Review of E-Cigarette-Related Illness and Injury: Not Just for the Respirologist". International Journal of Environmental Research and Public Health. 17 (7): 2248. doi:10.3390/ijerph17072248. ISSN 1660-4601. PMC 7177608. PMID 32230711.
 This article incorporates text by Anna Tzortzi, Melpo Kapetanstrataki, Vaso Evangelopoulou, and Panagiotis Behrakis available under the CC BY 4.0 license.
This article incorporates text by Anna Tzortzi, Melpo Kapetanstrataki, Vaso Evangelopoulou, and Panagiotis Behrakis available under the CC BY 4.0 license.
- ↑ 199.0 199.1 199.2 Saitta, D; Ferro, GA; Polosa, R (Mar 2014). "Achieving appropriate regulations for electronic cigarettes". Therapeutic Advances in Chronic Disease. 5 (2): 50–61. doi:10.1177/2040622314521271. PMC 3926346. PMID 24587890.
- ↑ 200.0 200.1 200.2 200.3 200.4 200.5 200.6 Zhao, Di; Aravindakshan, Atul; Hilpert, Markus; Olmedo, Pablo; Rule, Ana M.; Navas-Acien, Ana; Aherrera, Angela (2020). "Metal/Metalloid Levels in Electronic Cigarette Liquids, Aerosols, and Human Biosamples: A Systematic Review". Environmental Health Perspectives. 128 (3): 036001. doi:10.1289/EHP5686. ISSN 0091-6765. PMC 7137911. PMID 32186411.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 201.00 201.01 201.02 201.03 201.04 201.05 201.06 201.07 201.08 201.09 201.10 201.11 201.12 201.13 201.14 201.15 Rom, Oren; Pecorelli, Alessandra; Valacchi, Giuseppe; Reznick, Abraham Z. (2014). "Are E-cigarettes a safe and good alternative to cigarette smoking?". Annals of the New York Academy of Sciences. 1340 (1): 65–74. doi:10.1111/nyas.12609. ISSN 0077-8923. PMID 25557889.
- ↑ 202.0 202.1 "E-Cigarettes". Tobacco Control Research Branch of the National Cancer Institute. 2023.
- ↑ 203.0 203.1 203.2 203.3 203.4 203.5 Jenssen, Brian P.; Boykan, Rachel (2019). "Electronic Cigarettes and Youth in the United States: A Call to Action (at the Local, National and Global Levels)". Children. 6 (2): 30. doi:10.3390/children6020030. ISSN 2227-9067. PMC 6406299. PMID 30791645.
 This article incorporates text by Brian P. Jenssen and Rachel Boykan available under the CC BY 4.0 license.
This article incorporates text by Brian P. Jenssen and Rachel Boykan available under the CC BY 4.0 license.
- ↑ 204.0 204.1 204.2 204.3 204.4 204.5 204.6 204.7 204.8 Thirión-Romero, Ireri; Pérez-Padilla, Rogelio; Zabert, Gustavo; Barrientos-Gutiérrez, Inti (2019). "Respiratory Impact of Electronic Cigarettes and Low-Risk Tobacco". Revista de Investigación Clínica. 71 (1). doi:10.24875/RIC.18002616. ISSN 0034-8376. PMID 30810544.
- ↑ 205.0 205.1 205.2 Besaratinia, Ahmad; Tommasi, Stella (2021). "The consequential impact of JUUL on youth vaping and the landscape of tobacco products: The state of play in the COVID-19 era". Preventive Medicine Reports. 22: 101374. doi:10.1016/j.pmedr.2021.101374. ISSN 2211-3355. PMC 8207461. PMID 34168950.
- ↑ 206.0 206.1 "Did You Know? – Public Health Impact". Surgeon General of the United States. 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 207.00 207.01 207.02 207.03 207.04 207.05 207.06 207.07 207.08 207.09 207.10 207.11 207.12 207.13 207.14 207.15 207.16 207.17 207.18 207.19 207.20 207.21 207.22 207.23 207.24 207.25 207.26 207.27 207.28 207.29 207.30 207.31 207.32 207.33 207.34 207.35 207.36 207.37 207.38 207.39 207.40 207.41 207.42 207.43 207.44 207.45 207.46 207.47 207.48 207.49 207.50 207.51 207.52 207.53 207.54 207.55 207.56 207.57 207.58 207.59 207.60 207.61 207.62 207.63 207.64 Franck, Caroline; Filion, Kristian B.; Kimmelman, Jonathan; Grad, Roland; Eisenberg, Mark J. (2016). "Ethical considerations of e-cigarette use for tobacco harm reduction". Respiratory Research. 17 (1): 53. doi:10.1186/s12931-016-0370-3. ISSN 1465-993X. PMC 4869264. PMID 27184265.
 This article incorporates text by Caroline Franck, Kristian B. Filion, Jonathan Kimmelman, Roland Grad and Mark J. Eisenberg available under the CC BY 4.0 license.
This article incorporates text by Caroline Franck, Kristian B. Filion, Jonathan Kimmelman, Roland Grad and Mark J. Eisenberg available under the CC BY 4.0 license.
- ↑ Kumar, Navin; Hampsher, Sam; Walter, Nathan; Nyhan, Kate; De Choudhury, Munmun (9 October 2022). "Interventions to mitigate vaping misinformation: protocol for a scoping review". Systematic Reviews. 11 (1): 214. doi:10.1186/s13643-022-02094-0. PMC 9548303. PMID 36210470.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Navin Kumar, Sam Hampsher, Nathan Walter, Kate Nyhan, and Munmun De Choudhury available under the CC BY 4.0 license.
This article incorporates text by Navin Kumar, Sam Hampsher, Nathan Walter, Kate Nyhan, and Munmun De Choudhury available under the CC BY 4.0 license.
- ↑ 209.00 209.01 209.02 209.03 209.04 209.05 209.06 209.07 209.08 209.09 209.10 209.11 209.12 209.13 209.14 209.15 209.16 209.17 209.18 209.19 209.20 209.21 209.22 209.23 209.24 209.25 U.S. Department of Health and Human Services (2016). E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General (PDF) (Report). Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Surgeon General of the United States. pp. 1–298.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 210.00 210.01 210.02 210.03 210.04 210.05 210.06 210.07 210.08 210.09 210.10 210.11 210.12 210.13 210.14 210.15 210.16 210.17 210.18 210.19 Ruszkiewicz, Joanna A.; Zhang, Ziyan; Gonçalves, Filipe Marques; Tizabi, Yousef; Zelikoff, Judith T.; Aschner, Michael (2020). "Neurotoxicity of e-cigarettes". Food and Chemical Toxicology. 138: 111245. doi:10.1016/j.fct.2020.111245. ISSN 0278-6915. PMC 7089837. PMID 32145355.
- ↑ "Electronic Cigarettes". Centers for Disease Control and Prevention. 7 September 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 212.0 212.1 212.2 Barraza, Leila F.; Weidenaar, Kim E.; Cook, Livia T.; Logue, Andrea R.; Halpern, Michael T. (2017). "Regulations and policies regarding e-cigarettes". Cancer. 123 (16): 3007–3014. doi:10.1002/cncr.30725. ISSN 0008-543X. PMID 28440949.
- ↑ 213.0 213.1 213.2 213.3 213.4 213.5 213.6 213.7 Bhalerao, Aditya; Sivandzade, Farzane; Archie, Sabrina Rahman; Cucullo, Luca (2019). "Public Health Policies on E-Cigarettes". Current Cardiology Reports. 21 (10). doi:10.1007/s11886-019-1204-y. ISSN 1523-3782. PMC 6713696. PMID 31463564.
 This article incorporates text by Aditya Bhalerao, Farzane Sivandzade, Sabrina Rahman Archie, and Luca Cucullo available under the CC BY 4.0 license.
This article incorporates text by Aditya Bhalerao, Farzane Sivandzade, Sabrina Rahman Archie, and Luca Cucullo available under the CC BY 4.0 license.
- ↑ 214.0 214.1 Overbeek, Daniel L.; Kass, Alexandra P.; Chiel, Laura E.; Boyer, Edward W.; Casey, Alicia M. H. (2020). "A review of toxic effects of electronic cigarettes/vaping in adolescents and young adults". Critical Reviews in Toxicology. 50 (6): 531–538. doi:10.1080/10408444.2020.179444. ISSN 1040-8444. PMID 32715837.
- ↑ Detailed reference list is located at a separate image page.
- ↑ 216.0 216.1 216.2 216.3 216.4 216.5 216.6 216.7 Singh, Jasjot; Luquet, Emilie; Smith, DavidP.T.; Potgieter, HermanJ.; Ragazzon, Patricia (2016). "Toxicological and analytical assessment of e-cigarette refill components on airway epithelia" (PDF). Science Progress. 99 (4): 351–398. doi:10.3184/003685016X14773090197706. ISSN 0036-8504. PMID 28742478.
- ↑ Ghosh, Sohini; Drummond, M. Bradley (2016). "Electronic cigarettes as smoking cessation tool: are we there?". Current Opinion in Pulmonary Medicine. 23 (2): 111–116. doi:10.1097/MCP.0000000000000348. ISSN 1070-5287. PMC 5480094. PMID 27906858.
- ↑ 218.0 218.1 218.2 218.3 218.4 Ramôa, C. P.; Eissenberg, T.; Sahingur, S. E. (2017). "Increasing popularity of waterpipe tobacco smoking and electronic cigarette use: Implications for oral healthcare". Journal of Periodontal Research. 52 (5): 813–823. doi:10.1111/jre.12458. ISSN 0022-3484. PMC 5585021. PMID 28393367.
- ↑ Tegin, Gulay; Mekala, Hema Madhuri; Sarai, Simrat Kaur; Lippmann, Steven (2018). "E-Cigarette Toxicity?". Southern Medical Journal. 111 (1): 35–38. doi:10.14423/SMJ.0000000000000749. ISSN 1541-8243. PMID 29298367.
- ↑ 220.0 220.1 220.2 Dinakar, Chitra; Longo, Dan L.; O'Connor, George T. (2016). "The Health Effects of Electronic Cigarettes". New England Journal of Medicine. 375 (14): 1372–1381. doi:10.1056/NEJMra1502466. ISSN 0028-4793. PMID 27705269.
- ↑ 221.0 221.1 221.2 221.3 221.4 221.5 221.6 Hiemstra, Pieter S.; Bals, Robert (2016). "Basic science of electronic cigarettes: assessment in cell culture and in vivo models". Respiratory Research. 17 (1): 127. doi:10.1186/s12931-016-0447-z. ISSN 1465-993X. PMC 5055681. PMID 27717371.
 This article incorporates text by Pieter S. Hiemstra and Robert Bals available under the CC BY 4.0 license.
This article incorporates text by Pieter S. Hiemstra and Robert Bals available under the CC BY 4.0 license.
- ↑ 222.0 222.1 222.2 222.3 222.4 Gualano, Maria Rosaria; Passi, Stefano; Bert, Fabrizio; La Torre, Giuseppe; Scaioli, Giacomo; Siliquini, Roberta (2015). "Electronic cigarettes: assessing the efficacy and the adverse effects through a systematic review of published studies". Journal of Public Health. 37 (3): 488–497. doi:10.1093/pubmed/fdu055. ISSN 1741-3842. PMID 25108741.
- ↑ Górski, Paweł (2019). "E-cigarettes or heat-not-burn tobacco products — advantages or disadvantages for the lungs of smokers". Advances in Respiratory Medicine. 87 (2): 123–134. doi:10.5603/ARM.2019.0020. ISSN 2543-6031. PMID 31038725.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 157, Humectants (Delivery Solvents).
- ↑ 225.00 225.01 225.02 225.03 225.04 225.05 225.06 225.07 225.08 225.09 225.10 225.11 225.12 225.13 225.14 225.15 225.16 225.17 225.18 Qasim, Hanan; Karim, Zubair A.; Rivera, Jose O.; Khasawneh, Fadi T.; Alshbool, Fatima Z. (2017). "Impact of Electronic Cigarettes on the Cardiovascular System". Journal of the American Heart Association. 6 (9): e006353. doi:10.1161/JAHA.117.006353. ISSN 2047-9980. PMC 5634286. PMID 28855171.
- ↑ Lauterstein, Dana; Hoshino, Risa; Gordon, Terry; Watkins, Beverly-Xaviera; Weitzman, Michael; Zelikoff, Judith (2014). "The Changing Face of Tobacco Use Among United States Youth". Current Drug Abuse Reviews. 7 (1): 29–43. doi:10.2174/1874473707666141015220110. ISSN 1874-4737. PMC 4469045. PMID 25323124.
- ↑ "Talking to Youth and Young Adults to Prevent E-cigarette Use - Why It Matters". Centers for Disease Control and Prevention. 12 October 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Must Know Facts About E-Cigarettes | Vaping 101 | Vaping Prevention Resources". United States Food and Drug Administration. United States Department of Health and Human Services. 2023.
- ↑ Livingston, Catherine J.; Freeman, Randall J.; Costales, Victoria C.; Westhoff, John L.; Caplan, Lee S.; Sherin, Kevin M.; Niebuhr, David W. (2019). "Electronic Nicotine Delivery Systems or E-cigarettes: American College of Preventive Medicine's Practice Statement". American Journal of Preventive Medicine. 56 (1): 167–178. doi:10.1016/j.amepre.2018.09.010. ISSN 0749-3797. PMID 30573147.
- ↑ Smith, Marissa J.; Buckton, Christina; Patterson, Chris; Hilton, Shona (20 March 2023). "User-generated content and influencer marketing involving e-cigarettes on social media: a scoping review and content analysis of YouTube and Instagram". BMC Public Health. 23 (1): 530. doi:10.1186/s12889-023-15389-1. PMC 10029293. PMID 36941553.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Marissa J. Smith, Christina Buckton, Chris Patterson, and Shona Hilton available under the CC BY 4.0 license.
This article incorporates text by Marissa J. Smith, Christina Buckton, Chris Patterson, and Shona Hilton available under the CC BY 4.0 license.
- ↑ Arnaud, Nicolas; Holtmann, Martin; Melchers, Peter; Klein, Marianne; Schimansky, Gisela; Krömer, Thomas; Reis, Olaf; Thomasius, Rainer (1 March 2022). "Nutzung elektronischer Zigaretten (E-Zigaretten) und E-Shishas durch Kinder und Jugendliche: Evidenzpapier der Gemeinsamen Suchtkommission der kinder- und jugendpsychiatrischen und psychotherapeutischen Fachgesellschaft und Verbände (DGKJP, BAG, BKJPP)". Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie (in Deutsch). 50 (2): 121–132. doi:10.1024/1422-4917/a000831. PMID 34668740.
- ↑ 232.0 232.1 232.2 232.3 232.4 232.5 232.6 232.7 England, Lucinda J.; Aagaard, Kjersti; Bloch, Michele; Conway, Kevin; Cosgrove, Kelly; Grana, Rachel; Gould, Thomas J.; Hatsukami, Dorothy; Jensen, Frances; Kandel, Denise; Lanphear, Bruce; Leslie, Frances; Pauly, James R.; Neiderhiser, Jenae; Rubinstein, Mark; Slotkin, Theodore A.; Spindel, Eliot; Stroud, Laura; Wakschlag, Lauren (2017). "Developmental toxicity of nicotine: A transdisciplinary synthesis and implications for emerging tobacco products". Neuroscience & Biobehavioral Reviews. 72: 176–189. doi:10.1016/j.neubiorev.2016.11.013. ISSN 0149-7634. PMC 5965681. PMID 27890689.
- ↑ 233.0 233.1 233.2 Lødrup Carlsen, Karin C.; Skjerven, Håvard O.; Carlsen, Kai-Håkon (2018). "The toxicity of E-cigarettes and children's respiratory health". Paediatric Respiratory Reviews. 28: 63–67. doi:10.1016/j.prrv.2018.01.002. ISSN 1526-0542. PMID 29580719.
- ↑ 234.0 234.1 234.2 234.3 234.4 Wolff, Mary S.; Buckley, Jessie P.; Engel, Stephanie M.; McConnell, Rob S.; Barr, Dana B. (2017). "Emerging exposures of developmental toxicants". Current Opinion in Pediatrics. 29 (2): 218–224. doi:10.1097/MOP.0000000000000455. ISSN 1040-8703. PMC 5473289. PMID 28059904.
- ↑ Khan, Ali Mahmood; Ahmed, Saeed; Sarfraz, Zouina; Farahmand, Pantea (January 2023). "Vaping and Mental Health Conditions in Children: An Umbrella Review". Substance Abuse: Research and Treatment. 17: 117822182311673. doi:10.1177/11782218231167322. PMC 10134143. PMID 37124582.
{{cite journal}}: Check|pmc=value (help) - ↑ 236.0 236.1 236.2 236.3 236.4 236.5 236.6 236.7 236.8 Collaco, Joseph M.; McGrath-Morrow, Sharon A. (2017). "Electronic Cigarettes: Exposure and Use Among Pediatric Populations". Journal of Aerosol Medicine and Pulmonary Drug Delivery. 31 (2): 71–77. doi:10.1089/jamp.2017.1418. ISSN 1941-2711. PMC 5915214. PMID 29068754.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 9, Summary–Conclusion 11-4..
- ↑ Rodger, James (1 October 2019). "Brit suspected to be first to die from condition linked to vaping". Coventry Telegraph.
- ↑ 239.0 239.1 "Illinois Resident Experiencing Respiratory Illness After Vaping Dies". Illinois Department of Public Health. 23 August 2019. Archived from the original on 22 April 2020. Retrieved 4 May 2020.
- ↑ "E-cigarette, or Vaping, Associated Lung Injury (EVALI)". California Department of Public Health. 14 December 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Detailed reference list is located at a separate image page.
- ↑ 242.0 242.1 242.2 Kaisar, Mohammad Abul; Prasad, Shikha; Liles, Tylor; Cucullo, Luca (2016). "A Decade of e-Cigarettes: Limited Research & Unresolved Safety Concerns". Toxicology. 365: 67–75. doi:10.1016/j.tox.2016.07.020. ISSN 0300-483X. PMC 4993660. PMID 27477296.
- ↑ 243.0 243.1 243.2 243.3 243.4 Jo, Catherine L.; Ambs, Anita; Dresler, Carolyn M.; Backinger, Cathy L. (2017). "Child-resistant and tamper-resistant packaging: A systematic review to inform tobacco packaging regulation". Preventive Medicine. 95: 89–95. doi:10.1016/j.ypmed.2016.11.013. ISSN 0091-7435. PMC 5299541. PMID 27939602.
- ↑ 244.0 244.1 Crowley, Ryan A. (2015). "Electronic Nicotine Delivery Systems: Executive Summary of a Policy Position Paper From the American College of Physicians". Annals of Internal Medicine. 162 (8): 583–4. doi:10.7326/M14-2481. ISSN 0003-4819. PMID 25894027.
- ↑ 245.0 245.1 245.2 Biyani, S; Derkay, CS (28 April 2015). "E-cigarettes: Considerations for the otolaryngologist". International Journal of Pediatric Otorhinolaryngology. 79 (8): 1180–3. doi:10.1016/j.ijporl.2015.04.032. PMID 25998217.
- ↑ 246.0 246.1 246.2 246.3 246.4 246.5 246.6 Kim, Ki-Hyun; Kabir, Ehsanul; Jahan, Shamin Ara (2016). "Review of electronic cigarettes as tobacco cigarette substitutes: their potential human health impact". Journal of Environmental Science and Health, Part C. 34 (4): 262–275. doi:10.1080/10590501.2016.1236604. ISSN 1059-0501. PMID 27635466.
- ↑ 247.0 247.1 McNeill 2015, p. 63.
- ↑ Chatham-Stephens K, Law R, Taylor E, Melstrom P, Bunnell R, Wang B, Apelberg B, Schier JG (April 2014). "Notes from the field: calls to poison centers for exposures to electronic cigarettes—United States, September 2010 – February 2014". MMWR Morb. Mortal. Wkly. Rep. 63 (13): 292–3. PMC 5779356. PMID 24699766.
- ↑ 249.00 249.01 249.02 249.03 249.04 249.05 249.06 249.07 249.08 249.09 249.10 249.11 249.12 249.13 249.14 249.15 249.16 249.17 Chatham-Stephens, Kevin; Law, Royal; Taylor, Ethel; Kieszak, Stephanie; Melstrom, Paul; Bunnell, Rebecca; Wang, Baoguang; Day, Hannah; Apelberg, Benjamin; Cantrell, Lee; Foster, Howell; Schier, Joshua G. (June 2016). "Exposure Calls to U. S. Poison Centers Involving Electronic Cigarettes and Conventional Cigarettes—September 2010 – December 2014". Journal of Medical Toxicology. 12 (4): 350–357. doi:10.1007/s13181-016-0563-7. ISSN 1556-9039. PMC 5135675. PMID 27352081.
- ↑ 250.0 250.1 250.2 250.3 Nelluri, Bhargava Krishna; Murphy, Katie; Mookadam, Farouk (2015). "Electronic cigarettes and cardiovascular risk: hype or up in smoke?". Future Cardiology. 11 (3): 271–273. doi:10.2217/fca.15.13. ISSN 1479-6678. PMID 26021631.
- ↑ Chatham-Stephens, Kevin (20 October 2014). "Young Children and e-Cigarette Poisoning". Medscape.
- ↑ 252.0 252.1 252.2 252.3 252.4 252.5 Govindarajan, Preethi; Spiller, Henry A.; Casavant, Marcel J.; Chounthirath, Thitphalak; Smith, Gary A. (2018). "E-Cigarette and Liquid Nicotine Exposures Among Young Children". Pediatrics. 141 (5): e20173361. doi:10.1542/peds.2017-3361. ISSN 0031-4005. PMID 29686144.
- ↑ 253.0 253.1 253.2 253.3 253.4 "Some E-cigarette Users Are Having Seizures, Most Reports Involving Youth and Young Adults". United States Food and Drug Administration. 3 April 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Jenssen, Brian P.; Walley, Susan C. (2019). "E-Cigarettes and Similar Devices". Pediatrics. 143 (2): e20183652. doi:10.1542/peds.2018-3652. ISSN 0031-4005. PMC 6644065. PMID 30835247.
- ↑ 255.0 255.1 "New CDC study finds dramatic increase in e-cigarette-related calls to poison centers". Centers for Disease Control and Prevention. 3 April 2014.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 256.0 256.1 Kamboj, A.; Spiller, H. A.; Casavant, M. J.; Chounthirath, T.; Smith, G. A. (2016). "Pediatric Exposure to E-Cigarettes, Nicotine, and Tobacco Products in the United States". Pediatrics. 137 (6): e20160041. doi:10.1542/peds.2016-0041. ISSN 0031-4005. PMID 27244861.
- ↑ 257.0 257.1 "E-Cigarettes and Liquid Nicotine". American Association of Poison Control Centers. 2018.
- ↑ "Electronic Cigarettes and Liquid Nicotine Data" (PDF). American Association of Poison Control Centers. 31 December 2015. Archived from the original (PDF) on 28 January 2016. Retrieved 9 January 2016.
- ↑ 259.0 259.1 259.2 259.3 259.4 259.5 Chun, Lauren F; Moazed, Farzad; Calfee, Carolyn S; Matthay, Michael A.; Gotts, Jeffrey Earl (2017). "Pulmonary Toxicity of E-cigarettes". American Journal of Physiology. Lung Cellular and Molecular Physiology. 313 (2): L193–L206. doi:10.1152/ajplung.00071.2017. ISSN 1040-0605. PMC 5582932. PMID 28522559.
- ↑ 260.0 260.1 McNeill 2018, p. 148.
- ↑ Orr, KK; Asal, NJ (November 2014). "Efficacy of Electronic Cigarettes for Smoking Cessation". The Annals of Pharmacotherapy. 48 (11): 1502–1506. doi:10.1177/1060028014547076. PMID 25136064.
- ↑ 262.0 262.1 Peterson, Lisa A.; Hecht, Stephen S. (2017). "Tobacco, e-cigarettes, and child health". Current Opinion in Pediatrics. 29 (2): 225–230. doi:10.1097/MOP.0000000000000456. ISSN 1040-8703. PMC 5598780. PMID 28059903.
- ↑ 263.00 263.01 263.02 263.03 263.04 263.05 263.06 263.07 263.08 263.09 263.10 263.11 263.12 263.13 "Be Smoke-free and Help Your Pets Live Longer, Healthier Lives - Electronic Nicotine Delivery Systems". United States Food and Drug Administration. 19 October 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "E-cigarettes and Pet Safety". VCA Corporate. 2019.
- ↑ 265.0 265.1 Yang, L.; Rudy, S. F.; Cheng, J. M.; Durmowicz, E. L. (2014). "Electronic cigarettes: incorporating human factors engineering into risk assessments". Tobacco Control. 23 (Supplement 2): ii47–ii53. doi:10.1136/tobaccocontrol-2013-051479. ISSN 0964-4563. PMC 3995290. PMID 24732164.
- ↑ 266.0 266.1 "FDA's Plan for Tobacco and Nicotine Regulation". United States Food and Drug Administration. 15 March 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 9, Summary–Conclusion 14-2..
- ↑ 268.0 268.1 SA, Meo; SA, Al Asiri (2014). "Effects of electronic cigarette smoking on human health" (PDF). Eur Rev Med Pharmacol Sci. 18 (21): 3315–9. PMID 25487945.
- ↑ 269.0 269.1 269.2 Biyani, Sneh; Derkay, Craig S. (2017). "E-cigarettes: An update on considerations for the otolaryngologist". International Journal of Pediatric Otorhinolaryngology. 94: 14–16. doi:10.1016/j.ijporl.2016.12.027. ISSN 0165-5876. PMID 28167004.
- ↑ 270.0 270.1 270.2 270.3 Brown, C. J.; Cheng, J. M. (2014). "Electronic cigarettes: product characterisation and design considerations". Tobacco Control. 23 (Supplement 2): ii4–ii10. doi:10.1136/tobaccocontrol-2013-051476. ISSN 0964-4563. PMC 3995271. PMID 24732162.
- ↑ "State Health Officer's Report on E-Cigarettes: A Community Health Threat" (PDF). California Department of Public Health. January 2015.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 272.0 272.1 Frey, Leslie T.; Tilburg, William C. (2016). "Child-Resistant Packaging for E-Liquid: A Review of US State Legislation". American Journal of Public Health. 106 (2): 266–268. doi:10.2105/AJPH.2015.302957. ISSN 0090-0036. PMC 4815607. PMID 26691114.
- ↑ "The Potential Adverse Health Consequences of Exposure to Electronic Cigarettes and Electronic Nicotine Delivery Systems". Oncology Nursing Forum. 42 (5): 445–446. 2015. doi:10.1188/15.ONF.445-446. ISSN 0190-535X. PMID 26302273.
- ↑ 274.0 274.1 274.2 274.3 274.4 Modesto-Lowe, Vania; Alvarado, Camille (2017). "E-cigs . . . Are They Cool? Talking to Teens About E-Cigarettes". Clinical Pediatrics. 56 (10): 947–952. doi:10.1177/0009922817705188. ISSN 0009-9228. PMID 28443340.
- ↑ 275.0 275.1 275.2 275.3 275.4 275.5 "Do You Vape? See These Tips on How to Keep E-Liquids Away from Children". United States Food and Drug Administration. 2 May 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 276.0 276.1 276.2 "FDA, FTC take action against companies misleading kids with e-liquids that resemble children's juice boxes, candies and cookies". United States Food and Drug Administration. 1 May 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "E-Liquids Misleadingly Labeled or Advertised as Food Products". United States Food and Drug Administration. 25 September 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 278.0 278.1 278.2 "Companies cease sales of e-liquids with labeling or advertising that resembled kid-friendly foods following FDA, FTC warnings". United States Food and Drug Administration. 23 August 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Mayer, Bernd (January 2014). "How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century". Archives of Toxicology. 88 (1): 5–7. doi:10.1007/s00204-013-1127-0. ISSN 0340-5761. PMC 3880486. PMID 24091634.
- ↑ Eggleston, William; Nacca, Nicholas; Stork, Christine M.; Marraffa, Jeanna M. (2016). "Pediatric death after unintentional exposure to liquid nicotine for an electronic cigarette". Clinical Toxicology. 54 (9): 1–2. doi:10.1080/15563650.2016.1207081. ISSN 1556-3650. PMID 27383772.
- ↑ "E-Cigarette Poisonings Among Toddlers Skyrocketed 1500% Over 3 Years". Yahoo! News. 9 May 2016.
- ↑ 282.0 282.1 McNeill 2015, p. 67–68.
- ↑ "Electronic cigarettes". Therapeutic Goods Administration. 30 March 2015.
- ↑ 284.0 284.1 Giroud, Christian; de Cesare, Mariangela; Berthet, Aurélie; Varlet, Vincent; Concha-Lozano, Nicolas; Favrat, Bernard (2015). "E-Cigarettes: A Review of New Trends in Cannabis Use". International Journal of Environmental Research and Public Health. 12 (8): 9988–10008. doi:10.3390/ijerph120809988. ISSN 1660-4601. PMC 4555324. PMID 26308021.
 This article incorporates text by Christian Giroud, Mariangela de Cesare, Aurélie Berthet, Vincent Varlet, Nicolas Concha-Lozano, and Bernard Favrat available under the CC BY 4.0 license.
This article incorporates text by Christian Giroud, Mariangela de Cesare, Aurélie Berthet, Vincent Varlet, Nicolas Concha-Lozano, and Bernard Favrat available under the CC BY 4.0 license.
- ↑ Lim, Carmen C. W.; Sun, Tianze; Leung, Janni; Chung, Jack Y. C.; Gartner, Coral; Connor, Jason; Hall, Wayne; Chiu, Vivian; Stjepanović, Daniel; Chan, Gary C. K. (1 January 2022). "Prevalence of Adolescent Cannabis Vaping: A Systematic Review and Meta-analysis of US and Canadian Studies". JAMA Pediatrics. 176 (1): 42. doi:10.1001/jamapediatrics.2021.4102. PMC 8546627. PMID 34694342.
- ↑ 286.0 286.1 286.2 "Tips to Help Avoid "Vape" Battery Explosions". United States Food and Drug Administration. 20 December 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 287.0 287.1 287.2 287.3 287.4 Patterson, Scott B.; Beckett, Allison R.; Lintner, Alicia; Leahey, Carly; Greer, Ashley; Brevard, Sidney B.; Simmons, Jon D.; Kahn, Steven A. (2017). "A Novel Classification System for Injuries After Electronic Cigarette Explosions". Journal of Burn Care & Research. 38 (1): e95–e100. doi:10.1097/BCR.0000000000000471. ISSN 1559-047X. PMID 27893577.
- ↑ 288.0 288.1 288.2 "Know the Risks". Surgeon General of the United States. 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 9, Summary–Conclusion 14-1..
- ↑ 290.0 290.1 E-Cigarette Fire Risks and Reported Incidents 2015, p. 5.
- ↑ 291.00 291.01 291.02 291.03 291.04 291.05 291.06 291.07 291.08 291.09 291.10 291.11 291.12 291.13 291.14 291.15 291.16 291.17 291.18 291.19 291.20 291.21 291.22 291.23 291.24 291.25 291.26 291.27 291.28 291.29 291.30 291.31 291.32 291.33 "Electronic Cigarette Fires and Explosions in the United States 2009 – 2016" (PDF). United States Fire Administration. July 2017. pp. 1–56.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 292.0 292.1 292.2 292.3 292.4 Arnaout, A.; Khashaba, H.; Dobbs, T.; Dewi, F.; Pope-Jones, S.; Sack, A.; Estela, C.; Nguyen, D. (2017). "The Southwest UK Burns Network (SWUK) experience of electronic cigarette explosions and review of literature". Burns. 43 (4): e1–e6. doi:10.1016/j.burns.2017.01.008. ISSN 0305-4179. PMID 28412133.
- ↑ McNeill 2018, p. 149.
- ↑ 294.0 294.1 294.2 294.3 294.4 294.5 294.6 Harshman, Jamie; Vojvodic, Miliana; Rogers, Alan D. (2017). "Burns associated with e-cigarette batteries: A case series and literature review". CJEM. 20 (S2): 1–9. doi:10.1017/cem.2017.32. ISSN 1481-8035. PMID 28566106.
- ↑ Treitl, Daniela; Solomon, Rachele; Davare, Dafney L.; Sanchez, Rafael; Kiffin, Chauniqua (2017). "Full and Partial Thickness Burns from Spontaneous Combustion of E-Cigarette Lithium-Ion Batteries with Review of Literature". The Journal of Emergency Medicine. 53 (1): 121–125. doi:10.1016/j.jemermed.2017.03.031. ISSN 0736-4679. PMID 28501385.
- ↑ "5 Tips to Help Avoid Vape Battery Explosions" (PDF). United States Food and Drug Administration. April 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Protect Your Family From E-Cigarettes – The Facts You Need to Know" (PDF). California Department of Public Health. 29 October 2014. Archived from the original (PDF) on 10 January 2019. Retrieved 4 May 2020.
- ↑ 298.00 298.01 298.02 298.03 298.04 298.05 298.06 298.07 298.08 298.09 298.10 Paley, Grace L.; Echalier, Elizabeth; Eck, Thomas W.; Hong, Augustine R.; Farooq, Asim V.; Gregory, Darren G.; Lubniewski, Anthony J. (2016). "Corneoscleral Laceration and Ocular Burns Caused by Electronic Cigarette Explosions". Cornea. 35 (7): 1015–1018. doi:10.1097/ICO.0000000000000881. ISSN 0277-3740. PMC 4900417. PMID 27191672.
- ↑ Hickey, Sean; Goverman, Jeremy; Friedstat, Jonathan; Sheridan, Robert; Schulz, John (2018). "Thermal injuries from exploding electronic cigarettes". Burns. 44 (5): 1294–1301. doi:10.1016/j.burns.2018.02.008. ISSN 0305-4179. PMID 29503045.
- ↑ Makadia, Luv D.; Roper, P. Jervey; Andrews, Jeannette O.; Tingen, Martha S. (2017). "Tobacco Use and Smoke Exposure in Children: New Trends, Harm, and Strategies to Improve Health Outcomes". Current Allergy and Asthma Reports. 17 (8): 55. doi:10.1007/s11882-017-0723-0. ISSN 1529-7322. PMID 28741144.
- ↑ 301.0 301.1 301.2 301.3 301.4 301.5 Brian Vaught; Joseph Spellman; Anil Shah; Alexander Stewart; David Mullin (2017). "Facial trauma caused by electronic cigarette explosion". Ear, Nose, & Throat Journal. 96 (3): 139–142. doi:10.1177/014556131709600314. PMID 28346645.
- ↑ 302.00 302.01 302.02 302.03 302.04 302.05 302.06 302.07 302.08 302.09 302.10 302.11 302.12 302.13 302.14 302.15 302.16 302.17 Szumilas, Paweł; Wilk, Aleksandra; Szumilas, Kamila; Karakiewicz, Beata (6 February 2022). "The Effects of E-Cigarette Aerosol on Oral Cavity Cells and Tissues: A Narrative Review". Toxics. MDPI AG. 10 (2): 74. doi:10.3390/toxics10020074. ISSN 2305-6304. PMC 8878056. PMID 35202260.
 This article incorporates text by Paweł Szumilas, Aleksandra Wilk, Kamila Szumilas, and Beata Karakiewicz available under the CC BY 4.0 license.
This article incorporates text by Paweł Szumilas, Aleksandra Wilk, Kamila Szumilas, and Beata Karakiewicz available under the CC BY 4.0 license.
- ↑ Caplan, David (22 December 2016). "Man Suffers 3rd-Degree Burns After E-Cigarette Explodes in His Pocket While Riding Bus". ABC News.
- ↑ McNeill 2015, p. 43-46.
- ↑ McNeill 2015, p. 83-84.
- ↑ 306.0 306.1 306.2 306.3 306.4 306.5 306.6 306.7 McNeill 2018, p. 144.
- ↑ Sheckter, Clifford; Chattopadhyay, Arhana; Paro, John; Karanas, Yvonne (2016). "Burns resulting from spontaneous combustion of electronic cigarettes: a case series". Burns & Trauma. 4 (1): 35. doi:10.1186/s41038-016-0061-9. ISSN 2321-3876. PMC 5151131. PMID 27995151.
 This article incorporates text by Clifford Sheckter, Arhana Chattopadhyay, John Paro, and Yvonne Karanas available under the CC BY 4.0 license.
This article incorporates text by Clifford Sheckter, Arhana Chattopadhyay, John Paro, and Yvonne Karanas available under the CC BY 4.0 license.
- ↑ 308.0 308.1 308.2 Bart Jansen (23 January 2015). "Packing e-Cigarettes in luggage is a fire risk, FAA warns". USA Today.
- ↑ 309.0 309.1 Ashley Hasley III (26 January 2015). "The FAA wants you to carry on your e-Cigs". The Washington Post.
- ↑ 310.0 310.1 310.2 310.3 Lacasse, Yves; Légaré, Martin; Maltais, François (2015). "E-Cigarette Use in Patients Receiving Home Oxygen Therapy". Canadian Respiratory Journal. 22 (2): 83–85. doi:10.1155/2015/215932. ISSN 1198-2241. PMC 4390016. PMID 25848719.
 This article incorporates text by Yves Lacasse, Martin Légaré, and François Maltais available under the CC BY 4.0 license.
This article incorporates text by Yves Lacasse, Martin Légaré, and François Maltais available under the CC BY 4.0 license.
- ↑ Choi, Humberto; Lin, Yu; Race, Elliot; Macmurdo, Maeve G. (February 2021). "Electronic Cigarettes and Alternative Methods of Vaping". Annals of the American Thoracic Society. 18 (2): 191–199. doi:10.1513/AnnalsATS.202005-511CME. PMID 33052707.
- ↑ 312.00 312.01 312.02 312.03 312.04 312.05 312.06 312.07 312.08 312.09 312.10 312.11 312.12 312.13 Emma, Rosalia; Caruso, Massimo; Campagna, Davide; Pulvirenti, Roberta; Li Volti, Giovanni (September 2022). "The Impact of Tobacco Cigarettes, Vaping Products and Tobacco Heating Products on Oxidative Stress". Antioxidants. 11 (9): 1829. doi:10.3390/antiox11091829. PMC 9495690. PMID 36139904.
 This article incorporates text by Rosalia Emma, Massimo Caruso, Davide Campagna, Roberta Pulvirenti, and Giovanni Li Volti available under the CC BY 4.0 license.
This article incorporates text by Rosalia Emma, Massimo Caruso, Davide Campagna, Roberta Pulvirenti, and Giovanni Li Volti available under the CC BY 4.0 license.
- ↑ 313.0 313.1 "Cancer Research UK Briefing: Electronic Cigarettes" (PDF). Cancer Research UK. May 2014.
- ↑ 314.0 314.1 Orr, M. S. (2014). "Electronic cigarettes in the USA: a summary of available toxicology data and suggestions for the future". Tobacco Control. 23 (Supplement 2): ii18–ii22. doi:10.1136/tobaccocontrol-2013-051474. ISSN 0964-4563. PMC 3995288. PMID 24732158.
- ↑ Rahman, Muhammad; Hann, Nicholas; Wilson, Andrew; Worrall-Carter, Linda (15 December 2014). "Electronic cigarettes: patterns of use, health effects, use in smoking cessation and regulatory issues". Tobacco Induced Diseases. 12 (1): 21. doi:10.1186/1617-9625-12-21. PMC 4350653. PMID 25745382.
- ↑ 316.0 316.1 316.2 316.3 316.4 316.5 Hikisz, Pawel; Jacenik, Damian (11 March 2023). "The Tobacco Smoke Component, Acrolein, as a Major Culprit in Lung Diseases and Respiratory Cancers: Molecular Mechanisms of Acrolein Cytotoxic Activity". Cells. 12 (6): 879. doi:10.3390/cells12060879. PMC 10047238. PMID 36980220.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Pawel Hikisz1 and Damian Jacenik available under the CC BY 4.0 license.
This article incorporates text by Pawel Hikisz1 and Damian Jacenik available under the CC BY 4.0 license.
- ↑ 317.0 317.1 317.2 317.3 317.4 317.5 Tang, Moon-shong; Lee, Hyun-Wook; Weng, Mao-wen; Wang, Hsiang-Tsui; Hu, Yu; Chen, Lung-Chi; Park, Sung-Hyun; Chan, Huei-wei; Xu, Jiheng; Wu, Xue-Ru; Wang, He; Yang, Rui; Galdane, Karen; Jackson, Kathryn; Chu, Annie; Halzack, Elizabeth (January 2022). "DNA damage, DNA repair and carcinogenicity: Tobacco smoke versus electronic cigarette aerosol". Mutation Research/Reviews in Mutation Research. 789: 108409. doi:10.1016/j.mrrev.2021.108409. PMC 9208310. PMID 35690412.
- ↑ SGUS 2014, p. 115.
- ↑ SGUS 2014, p. 116.
- ↑ 320.00 320.01 320.02 320.03 320.04 320.05 320.06 320.07 320.08 320.09 320.10 320.11 320.12 Zhang, Qing; Wen, Cai (15 May 2023). "The risk profile of electronic nicotine delivery systems, compared to traditional cigarettes, on oral disease: a review". Frontiers in Public Health. 11. doi:10.3389/fpubh.2023.1146949. PMC 10226679. PMID 37255760.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Qing Zhang and Cai Wen available under the CC BY 4.0 license.
This article incorporates text by Qing Zhang and Cai Wen available under the CC BY 4.0 license.
- ↑ 321.0 321.1 Gemenetzidis, Emilios; Bose, Amrita; Riaz, Adeel M.; Chaplin, Tracy; Young, Bryan D.; Ali, Muhammad; Sugden, David; Thurlow, Johanna K.; Cheong, Sok-Ching; Teo, Soo-Hwang; Wan, Hong; Waseem, Ahmad; Parkinson, Eric K.; Fortune, Farida; Teh, Muy-Teck (16 March 2009). "FOXM1 Upregulation Is an Early Event in Human Squamous Cell Carcinoma and it Is Enhanced by Nicotine during Malignant Transformation". PLoS ONE. 4 (3): e4849. doi:10.1371/journal.pone.0004849. PMC 2654098. PMID 19287496.
 This article incorporates text by Emilios Gemenetzidis, Amrita Bose, Adeel M Riaz, Tracy Chaplin, Bryan D Young, Muhammad Ali, David Sugden, Johanna K Thurlow, Sok-Ching Cheong, Soo-Hwang Teo, Hong Wan, Ahmad Waseem, Eric K Parkinson, Farida Fortune, and Muy-Teck Teh available under the CC BY-SA 2.0 license.
This article incorporates text by Emilios Gemenetzidis, Amrita Bose, Adeel M Riaz, Tracy Chaplin, Bryan D Young, Muhammad Ali, David Sugden, Johanna K Thurlow, Sok-Ching Cheong, Soo-Hwang Teo, Hong Wan, Ahmad Waseem, Eric K Parkinson, Farida Fortune, and Muy-Teck Teh available under the CC BY-SA 2.0 license.
- ↑ 322.00 322.01 322.02 322.03 322.04 322.05 322.06 322.07 322.08 322.09 322.10 322.11 322.12 322.13 322.14 322.15 322.16 322.17 322.18 322.19 322.20 322.21 322.22 322.23 322.24 322.25 322.26 322.27 322.28 322.29 322.30 322.31 322.32 322.33 322.34 322.35 322.36 322.37 322.38 322.39 Sanner, Tore; Grimsrud, Tom K. (2015). "Nicotine: Carcinogenicity and Effects on Response to Cancer Treatment – A Review". Frontiers in Oncology. 5: 196. doi:10.3389/fonc.2015.00196. ISSN 2234-943X. PMC 4553893. PMID 26380225.
 This article incorporates text by Tore Sanner, and Tom K. Grimsrud available under the CC BY 4.0 license.
This article incorporates text by Tore Sanner, and Tom K. Grimsrud available under the CC BY 4.0 license.
- ↑ Schaal, C.; Chellappan, S. P. (2014). "Nicotine-Mediated Cell Proliferation and Tumor Progression in Smoking-Related Cancers". Molecular Cancer Research. 12 (1): 14–23. doi:10.1158/1541-7786.MCR-13-0541. ISSN 1541-7786. PMC 3915512. PMID 24398389.
- ↑ 324.0 324.1 324.2 324.3 324.4 Collaco, Joseph M. (2015). "Electronic Use and Exposure in the Pediatric Population". JAMA Pediatrics. 169 (2): 177–182. doi:10.1001/jamapediatrics.2014.2898. PMC 5557497. PMID 25546699.
- ↑ 325.0 325.1 325.2 Zona, Stefania; Bella, Laura; Burton, Matthew J.; Nestal de Moraes, Gabriela; Lam, Eric W.-F. (November 2014). "FOXM1: An emerging master regulator of DNA damage response and genotoxic agent resistance". Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms. 1839 (11): 1316–1322. doi:10.1016/j.bbagrm.2014.09.016. PMC 4316173. PMID 25287128.
 This article incorporates text by Stefania Zona, Laura Bella, Matthew J. Burton, Gabriela Nestal de Moraes, and Eric W.-F. Lam⁎ available under the CC BY 3.0 license.
This article incorporates text by Stefania Zona, Laura Bella, Matthew J. Burton, Gabriela Nestal de Moraes, and Eric W.-F. Lam⁎ available under the CC BY 3.0 license.
- ↑ 326.0 326.1 326.2 Halasi, Marianna; Gartel, Andrei L. (1 March 2013). "FOX(M1) News—It Is Cancer". Molecular Cancer Therapeutics. 12 (3): 245–254. doi:10.1158/1535-7163.MCT-12-0712. PMC 3596487. PMID 23443798.
- ↑ Arnold, Carrie (2014). "Vaping and Health: What Do We Know about E-Cigarettes?". Environmental Health Perspectives. 122 (9): A244–A249. doi:10.1289/ehp.122-A244. ISSN 0091-6765. PMC 4154203. PMID 25181730.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 328.00 328.01 328.02 328.03 328.04 328.05 328.06 328.07 328.08 328.09 328.10 Brooks, Arrin C.; Henderson, Brandon J. (29 January 2021). "Systematic Review of Nicotine Exposure's Effects on Neural Stem and Progenitor Cells". Brain Sciences. 11 (2): 172. doi:10.3390/brainsci11020172. PMC 7912116. PMID 33573081.
 This article incorporates text by Arrin C. Brooks and Brandon J. Henderson available under the CC BY 4.0 license.
This article incorporates text by Arrin C. Brooks and Brandon J. Henderson available under the CC BY 4.0 license.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 8, Summary–Conclusion 10-4..
- ↑ 330.0 330.1 National Academies of Sciences, Engineering, and Medicine 2018, p. 200, Metals.
- ↑ Wu, Liang; Wang, Li'ao; Yang, Jun; Jia, Wenqing; Xu, Yulun (31 March 2022). "Clinical Features, Treatments, and Prognosis of Intramedullary Spinal Cord Metastases From Lung Cancer: A Case Series and Systematic Review". Neurospine. 19 (1): 65–76. doi:10.14245/ns.2142910.455. PMC 8987539. PMID 35130420.
- ↑ Khodabandeh, Zhila; Valilo, Mohammad; Velaei, Kobra; Pirpour Tazehkand, Abbas (September 2022). "The potential role of nicotine in breast cancer initiation, development, angiogenesis, invasion, metastasis, and resistance to therapy". Breast Cancer. 29 (5): 778–789. doi:10.1007/s12282-022-01369-7. PMID 35583594.
- ↑ Di Vita, Maria (2013). "Strong correlation between diet and development of colorectal cancer". Frontiers in Bioscience. 18 (1): 190. doi:10.2741/4095. PMID 23276917.
- ↑ 334.0 334.1 Shin, Vivian Y.; Cho, Chi-Hin (April 2005). "Nicotine and gastric cancer". Alcohol. 35 (3): 259–264. doi:10.1016/j.alcohol.2005.04.007. PMID 16054988.
- ↑ 335.0 335.1 335.2 Saba, Raya; Alsayed, Alhareth; Zacny, James P.; Dudek, Arkadiusz Z. (January 2016). "The Role of Forkhead Box Protein M1 in Breast Cancer Progression and Resistance to Therapy". International Journal of Breast Cancer. 2016: 1–8. doi:10.1155/2016/9768183. PMC 4752991. PMID 30852780.
 This article incorporates text by Raya Saba, Alhareth Alsayed, James P. Zacny, and Arkadiusz Z. Dudek available under the CC BY 4.0 license.
This article incorporates text by Raya Saba, Alhareth Alsayed, James P. Zacny, and Arkadiusz Z. Dudek available under the CC BY 4.0 license.
- ↑ 336.0 336.1 336.2 336.3 Russo, Patrizia; Cardinale, Alessio; Margaritora, Stefano; Cesario, Alfredo (November 2012). "Nicotinic receptor and tobacco-related cancer". Life Sciences. 91 (21–22): 1087–1092. doi:10.1016/j.lfs.2012.05.003. PMID 22705232.
- ↑ Zhao, Yue (2016). "The Oncogenic Functions of Nicotinic Acetylcholine Receptors". Journal of Oncology. 2016: 1–9. doi:10.1155/2016/9650481. PMC 4769750. PMID 26981122.
- ↑ Woźniak, Łukasz; Skąpska, Sylwia; Marszałek, Krystian (19 November 2015). "Ursolic Acid—A Pentacyclic Triterpenoid with a Wide Spectrum of Pharmacological Activities". Molecules. 20 (11): 20614–20641. doi:10.3390/molecules201119721. PMC 6332387. PMID 26610440.
 This article incorporates text by Łukasz Woźniak, Sylwia Skąpska, and Krystian Marszałek available under the CC BY 4.0 license.
This article incorporates text by Łukasz Woźniak, Sylwia Skąpska, and Krystian Marszałek available under the CC BY 4.0 license.
- ↑ 339.0 339.1 Liao, Guo-Bin; Li, Xin-Zhe; Zeng, Shuo; Liu, Cheng; Yang, Shi-Ming; Yang, Li; Hu, Chang-Jiang; Bai, Jian-Ying (December 2018). "Regulation of the master regulator FOXM1 in cancer". Cell Communication and Signaling. 16 (1): 57. doi:10.1186/s12964-018-0266-6. PMC 6134757. PMID 30208972.
 This article incorporates text by Guo-Bin Liao, Xin-Zhe Li, Shuo Zeng, Cheng Liu, Shi-Ming Yang, Li Yang, Chang-Jiang Hu, and Jian-Ying Bai available under the CC BY 4.0 license.
This article incorporates text by Guo-Bin Liao, Xin-Zhe Li, Shuo Zeng, Cheng Liu, Shi-Ming Yang, Li Yang, Chang-Jiang Hu, and Jian-Ying Bai available under the CC BY 4.0 license.
- ↑ 340.0 340.1 340.2 Flach, Susanne; Maniam, Pavithran; Manickavasagam, Jaiganesh (2019). "E‐cigarettes and head and neck cancers: A systematic review of the current literature". Clinical Otolaryngology. 44 (5): 749–756. doi:10.1111/coa.13384. ISSN 1749-4478. PMID 31148389.
- ↑ Szukalska, Marta; Szyfter, Krzysztof; Florek, Ewa; Rodrigo, Juan P.; Rinaldo, Alessandra; Mäkitie, Antti A.; Strojan, Primož; Takes, Robert P.; Suárez, Carlos; Saba, Nabil F.; Braakhuis, Boudewijn J.M.; Ferlito, Alfio (5 November 2020). "Electronic Cigarettes and Head and Neck Cancer Risk—Current State of Art". Cancers. 12 (11): 3274. doi:10.3390/cancers12113274. PMC 7694366. PMID 33167393.
 This article incorporates text by Marta Szukalska, Krzysztof Szyfter, Ewa Florek, Juan P. Rodrigo, Alessandra Rinaldo, Antti A. Mäkitie, Primož Strojan, Robert P. Takes, Carlos Suárez, Nabil F. Saba, Boudewijn J.M. Braakhuis, and Alfio Ferlito available under the CC BY 4.0 license.
This article incorporates text by Marta Szukalska, Krzysztof Szyfter, Ewa Florek, Juan P. Rodrigo, Alessandra Rinaldo, Antti A. Mäkitie, Primož Strojan, Robert P. Takes, Carlos Suárez, Nabil F. Saba, Boudewijn J.M. Braakhuis, and Alfio Ferlito available under the CC BY 4.0 license.
- ↑ 342.0 342.1 Pucci, Susanna; Zoli, Michele; Clementi, Francesco; Gotti, Cecilia (21 January 2022). "α9-Containing Nicotinic Receptors in Cancer". Frontiers in Cellular Neuroscience. 15: 805123. doi:10.3389/fncel.2021.805123.
 This article incorporates text by Susanna Pucci, Michele Zoli, Francesco Clementi, and Cecilia Gotti available under the CC BY 4.0 license.
This article incorporates text by Susanna Pucci, Michele Zoli, Francesco Clementi, and Cecilia Gotti available under the CC BY 4.0 license.
- ↑ 343.0 343.1 Maan, Meenu; Abuzayeda, Moosa; Kaklamanos, Eleftherios G.; Jamal, Mohamed; Dutta, Mainak; Moharamzadeh, Keyvan (13 April 2023). "Molecular insights into the role of electronic cigarettes in oral carcinogenesis". Critical Reviews in Toxicology. 0 (0): 1–14. doi:10.1080/10408444.2023.2190764. PMID 37051806.
- ↑ 344.0 344.1 Sultan, Ahmed S.; Jessri, Maryam; Farah, Camile S. (2018). "Electronic nicotine delivery systems: Oral health implications and oral cancer risk". Journal of Oral Pathology & Medicine. doi:10.1111/jop.12810. ISSN 0904-2512. PMID 30507043.
- ↑ 345.0 345.1 Alawsi, F.; Nour, R.; Prabhu, S. (2015). "Are e-cigarettes a gateway to smoking or a pathway to quitting?". BDJ. 219 (3): 111–115. doi:10.1038/sj.bdj.2015.591. ISSN 0007-0610. PMID 26271862.
- ↑ 346.0 346.1 McNeill 2018, p. 162.
- ↑ Papaefstathiou, E.; Stylianou, M.; Agapiou, A. (2019). "Main and side stream effects of electronic cigarettes". Journal of Environmental Management. 238: 10–17. doi:10.1016/j.jenvman.2019.01.030. ISSN 0301-4797. PMID 30836280.
- ↑ 348.00 348.01 348.02 348.03 348.04 348.05 348.06 348.07 348.08 348.09 348.10 348.11 348.12 Cai, Hua; Wang, Chen (2017). "Graphical review: The redox dark side of e-cigarettes; exposure to oxidants and public health concerns". Redox Biology. 13: 402–406. doi:10.1016/j.redox.2017.05.013. ISSN 2213-2317. PMC 5493817. PMID 28667909.
- ↑ 349.0 349.1 349.2 DeVito, Elise E.; Krishnan-Sarin, Suchitra (2018). "E-cigarettes: Impact of E-Liquid Components and Device Characteristics on Nicotine Exposure". Current Neuropharmacology. 16 (4): 438–459. doi:10.2174/1570159X15666171016164430. ISSN 1570-159X. PMC 6018193. PMID 29046158.
- ↑ 350.0 350.1 350.2 350.3 350.4 Schupp, J. C.; Prasse, A.; Erythropel, H. C. (February 2020). "E-Zigaretten – Funktionsweise, Inhaltsstoffe und die Vaping-assoziierte akute Lungenschädigung" [E-Cigarettes - Operating Principle, Ingredients, and Associated Acute Lung Injury]. Pneumologie (in Deutsch). 74 (02): 77–87. doi:10.1055/a-1078-8126. ISSN 0934-8387. PMC 7366312. PMID 32016924.
- ↑ 351.0 351.1 MacLean, Robert Ross; Valentine, Gerald W.; Jatlow, Peter I.; Sofuoglu, Mehmet (2017). "Inhalation of Alcohol Vapor: Measurement and Implications". Alcoholism: Clinical and Experimental Research. 41 (2): 238–250. doi:10.1111/acer.13291. ISSN 0145-6008. PMC 6143144. PMID 28054395.
- ↑ 352.0 352.1 352.2 352.3 352.4 Wetzel, Tanner J.; Wyatt, Todd A. (2020). "Dual Substance Use of Electronic Cigarettes and Alcohol". Frontiers in Physiology. 11. doi:10.3389/fphys.2020.593803. ISSN 1664-042X. PMC 7667127. PMID 33224040.
 This article incorporates text by Tanner J Wetzel and Todd A Wyatt available under the CC BY 4.0 license.
This article incorporates text by Tanner J Wetzel and Todd A Wyatt available under the CC BY 4.0 license.
- ↑ 353.0 353.1 353.2 353.3 Schick, Suzaynn F.; Blount, Benjamin C; Jacob, Peyton; Saliba, Najat A; Bernert, John T; El Hellani, Ahmad; Jatlow, Peter; Pappas, R Steve; Wang, Lanqing; Foulds, Jonathan; Ghosh, Arunava; Hecht, Stephen S; Gomez, John C; Martin, Jessica R; Mesaros, Clementina; Srivastava, Sanjay; St. Helen, Gideon; Tarran, Robert; Lorkiewicz, Pawel K; Blair, Ian A; Kimmel, Heather L; Doerschuk, Claire M.; Benowitz, Neal L; Bhatnagar, Aruni (2017). "Biomarkers of Exposure to New and Emerging Tobacco and Nicotine Delivery Products". American Journal of Physiology. Lung Cellular and Molecular Physiology. 313 (3): L425–L452. doi:10.1152/ajplung.00343.2016. ISSN 1040-0605. PMC 5626373. PMID 28522563.
- ↑ 354.0 354.1 354.2 354.3 354.4 Schraufnagel DE (2015). "Electronic Cigarettes: Vulnerability of Youth". Pediatr Allergy Immunol Pulmonol. 28 (1): 2–6. doi:10.1089/ped.2015.0490. PMC 4359356. PMID 25830075.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 4, Summary.
- ↑ 356.0 356.1 356.2 356.3 356.4 356.5 356.6 Rinkoo, ArvindVashishta; Kaur, Jagdish (2017). "Getting real with the upcoming challenge of electronic nicotine delivery systems: The way forward for the South-East Asia region". Indian Journal of Public Health. 61 (5): S7–S11. doi:10.4103/ijph.IJPH_240_17. ISSN 0019-557X. PMID 28928312.
- ↑ 357.0 357.1 357.2 357.3 357.4 Cormet-Boyaka, Estelle; Zare, Samane; Nemati, Mehdi; Zheng, Yuqing (2018). "A systematic review of consumer preference for e-cigarette attributes: Flavor, nicotine strength, and type". PLOS ONE. 13 (3): e0194145. Bibcode:2018PLoSO..1394145Z. doi:10.1371/journal.pone.0194145. ISSN 1932-6203. PMC 5854347. PMID 29543907.
 This article incorporates text by Samane Zare, Mehdi Nemati, and Yuqing Zheng available under the CC BY 4.0 license.
This article incorporates text by Samane Zare, Mehdi Nemati, and Yuqing Zheng available under the CC BY 4.0 license.
- ↑ 358.0 358.1 358.2 358.3 Bourke, Liam; Bauld, Linda; Bullen, Christopher; Cumberbatch, Marcus; Giovannucci, Edward; Islami, Farhad; McRobbie, Hayden; Silverman, Debra T.; Catto, James W.F. (2017). "E-cigarettes and Urologic Health: A Collaborative Review of Toxicology, Epidemiology, and Potential Risks" (PDF). European Urology. 71 (6): 915–923. doi:10.1016/j.eururo.2016.12.022. hdl:1893/24937. ISSN 0302-2838. PMID 28073600.
- ↑ 359.0 359.1 Wilder 2016, p. 82.
- ↑ 360.0 360.1 Naik, Pooja; Cucullo, Luca (2015). "Pathobiology of tobacco smoking and neurovascular disorders: untied strings and alternative products". Fluids and Barriers of the CNS. 12 (1): 25. doi:10.1186/s12987-015-0022-x. ISSN 2045-8118. PMC 4628383. PMID 26520792.
- ↑ 361.0 361.1 National Academies of Sciences, Engineering, and Medicine 2018, p. 197, Other Toxicants–Caffeine.
- ↑ 362.0 362.1 McNeill 2018, p. 19.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 175, Exposure to Flavorings.
- ↑ 364.0 364.1 364.2 Jankowski, Mateusz; Brożek, Grzegorz; Lawson, Joshua; Skoczyński, Szymon; Zejda, Jan (2017). "E-smoking: Emerging public health problem?". International Journal of Occupational Medicine and Environmental Health. 30 (3): 329–344. doi:10.13075/ijomeh.1896.01046. ISSN 1232-1087. PMID 28481369.
- ↑ 365.0 365.1 Bonilla, Alex; Blair, Alexander J.; Alamro, Suliman M.; Ward, Rebecca A.; Feldman, Michael B.; Dutko, Richard A.; Karagounis, Theodora K.; Johnson, Adam L.; Folch, Erik E.; Vyas, Jatin M. (2019). "Recurrent spontaneous pneumothoraces and vaping in an 18-year-old man: a case report and review of the literature". Journal of Medical Case Reports. 13 (1): 283. doi:10.1186/s13256-019-2215-4. ISSN 1752-1947. PMC 6732835. PMID 31495337.
 This article incorporates text by Alex Bonilla, Alexander J. Blair, Suliman M. Alamro, Rebecca A. Ward, Michael B. Feldman, Richard A. Dutko, Theodora K. Karagounis, Adam L. Johnson, Erik E. Folch, and Jatin M. Vyas available under the CC BY 4.0 license.
This article incorporates text by Alex Bonilla, Alexander J. Blair, Suliman M. Alamro, Rebecca A. Ward, Michael B. Feldman, Richard A. Dutko, Theodora K. Karagounis, Adam L. Johnson, Erik E. Folch, and Jatin M. Vyas available under the CC BY 4.0 license.
- ↑ Zhang, Yixuan; Wang, Lu; Mutlu, Gökhan M.; Cai, Hua (2021). "More to Explore: Further Definition of Risk Factors for COPD – Differential Gender Difference, Modest Elevation in PM2.5, and e-Cigarette Use". Frontiers in Physiology. 12. doi:10.3389/fphys.2021.669152. ISSN 1664-042X. PMC 8131967. PMID 34025456.
 This article incorporates text by Yixuan Zhang, Lu Wang, Gökhan M Mutlu, and Hua Cai available under the CC BY 4.0 license.
This article incorporates text by Yixuan Zhang, Lu Wang, Gökhan M Mutlu, and Hua Cai available under the CC BY 4.0 license.
- ↑ Leventhal, Adam M; Tackett, Alayna P; Whitted, Lauren; Jordt, Sven Eric; Jabba, Sairam V (November 2023). "Ice flavours and non-menthol synthetic cooling agents in e-cigarette products: a review". Tobacco Control. 32 (6): 769–777. doi:10.1136/tobaccocontrol-2021-057073. PMC 9613790. PMID 35483721.
{{cite journal}}: Check|pmc=value (help) - ↑ 368.0 368.1 368.2 368.3 368.4 Stefaniak, Aleksandr B.; LeBouf, Ryan F.; Ranpara, Anand C.; Leonard, Stephen S. (2021). "Toxicology of flavoring- and cannabis-containing e-liquids used in electronic delivery systems". Pharmacology & Therapeutics. 224: 107838. doi:10.1016/j.pharmthera.2021.107838. ISSN 0163-7258. PMC 8251682. PMID 33746051.
- ↑ 369.0 369.1 369.2 369.3 369.4 369.5 369.6 Shields, Peter G.; Berman, Micah; Brasky, Theodore M.; Freudenheim, Jo L.; Mathe, Ewy A; McElroy, Joseph; Song, Min-Ae; Wewers, Mark D. (2017). "A Review of Pulmonary Toxicity of Electronic Cigarettes In The Context of Smoking: A Focus On Inflammation". Cancer Epidemiology, Biomarkers & Prevention. 26 (8): 1175–1191. doi:10.1158/1055-9965.EPI-17-0358. ISSN 1055-9965. PMC 5614602. PMID 28642230.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 172, FLAVORINGS.
- ↑ 371.0 371.1 Editorial Staff (7 July 2016). "Popcorn Lung: A Dangerous Risk of Flavored E-Cigarettes". American Lung Association.
- ↑ McNeill 2018, p. 159.
- ↑ Konstantinos E. Farsalinos; I. Gene Gillman; Stephen S. Hecht; Riccardo Polosa; Jonathan Thornburg (16 November 2016). Analytical Assessment of e-Cigarettes: From Contents to Chemical and Particle Exposure Profiles. Elsevier Science. p. 22. ISBN 978-0-12-811242-7.
- ↑ 374.0 374.1 374.2 374.3 374.4 Benowitz, Neal L.; Burbank, Andrea D. (2016). "Cardiovascular toxicity of nicotine: Implications for electronic cigarette use". Trends in Cardiovascular Medicine. 26 (6): 515–23. doi:10.1016/j.tcm.2016.03.001. ISSN 1050-1738. PMC 4958544. PMID 27079891.
- ↑ Dhand, Rajiv (2017). "Inhaled Drug Therapy 2016: The Year in Review". Respiratory Care. 62 (7): 978–996. doi:10.4187/respcare.05624. ISSN 0020-1324. PMID 28559466.
- ↑ 376.0 376.1 376.2 Schraufnagel, Dean E.; Blasi, Francesco; Drummond, M. Bradley; Lam, David C. L.; Latif, Ehsan; Rosen, Mark J.; Sansores, Raul; Van Zyl-Smit, Richard (2014). "Electronic Cigarettes. A Position Statement of the Forum of International Respiratory Societies". American Journal of Respiratory and Critical Care Medicine. 190 (6): 611–618. doi:10.1164/rccm.201407-1198PP. ISSN 1073-449X. PMID 25006874.
- ↑ 377.0 377.1 377.2 377.3 National Academies of Sciences, Engineering, and Medicine 2018, p. 197, Other Toxicants–Pharmaceutical Drugs.
- ↑ 378.0 378.1 378.2 378.3 378.4 Kaur, Gurjot; Muthumalage, Thivanka; Rahman, Irfan (2018). "Mechanisms of toxicity and biomarkers of flavoring and flavor enhancing chemicals in emerging tobacco and non-tobacco products". Toxicology Letters. 288: 143–155. doi:10.1016/j.toxlet.2018.02.025. ISSN 0378-4274. PMC 6549714. PMID 29481849.
- ↑ 379.0 379.1 379.2 379.3 Huang, Shu-Jie; Xu, Yan-Ming; Lau, Andy T. Y. (2017). "Electronic cigarette: A recent update of its toxic effects on humans". Journal of Cellular Physiology. 233 (6): 4466–4478. doi:10.1002/jcp.26352. ISSN 0021-9541. PMID 29215738.
- ↑ McNeill 2018, p. 160.
- ↑ 381.0 381.1 Born, H.; Persky, M.; Kraus, D. H.; Peng, R.; Amin, M. R.; Branski, R. C. (2015). "Electronic Cigarettes: A Primer for Clinicians". Otolaryngology–Head and Neck Surgery. 153 (1): 5–14. doi:10.1177/0194599815585752. ISSN 0194-5998. PMID 26002957.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 56, Characteristics of E-Cigarette Devices.
- ↑ Detailed reference list is located at a separate image page.
- ↑ 384.0 384.1 Lachenmeier, Dirk W.; Rehm, Jürgen (2015). "Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach". Scientific Reports. 5: 8126. Bibcode:2015NatSR...5E8126L. doi:10.1038/srep08126. ISSN 2045-2322. PMC 4311234. PMID 25634572.
- ↑ 385.0 385.1 385.2 385.3 385.4 385.5 385.6 385.7 England, Lucinda J.; Bunnell, Rebecca E.; Pechacek, Terry F.; Tong, Van T.; McAfee, Tim A. (August 2015). "Nicotine and the Developing Human". American Journal of Preventive Medicine. 49 (2): 286–93. doi:10.1016/j.amepre.2015.01.015. ISSN 0749-3797. PMC 4594223. PMID 25794473.
- ↑ Kim, Jason H.; Patel, Sandeep (2017). "Is It Worth Discriminating Against Patients Who Smoke? A Systematic Literature Review on the Effects of Tobacco Use in Foot and Ankle Surgery". The Journal of Foot and Ankle Surgery. 56 (3): 594–599. doi:10.1053/j.jfas.2017.02.006. ISSN 1067-2516. PMID 28476393.
- ↑ 387.0 387.1 Schivo, Michael; Avdalovic, Mark V.; Murin, Susan (February 2014). "Non-Cigarette Tobacco and the Lung". Clinical Reviews in Allergy & Immunology. 46 (1): 34–53. doi:10.1007/s12016-013-8372-0. ISSN 1080-0549. PMID 23673789.
- ↑ 388.0 388.1 Callahan-Lyon, P. (2014). "Electronic cigarettes: human health effects". Tobacco Control. 23 (Supplement 2): ii36–ii40. doi:10.1136/tobaccocontrol-2013-051470. ISSN 0964-4563. PMC 3995250. PMID 24732161.
- ↑ Marsot, A.; Simon, N. (March 2016). "Nicotine and Cotinine Levels With Electronic Cigarette: A Review". International Journal of Toxicology. 35 (2): 179–185. doi:10.1177/1091581815618935. ISSN 1091-5818. PMID 26681385.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 7, Summary–Conclusion 8-2.
- ↑ McNeill 2018, p. 55.
- ↑ McNeill 2018, p. 57.
- ↑ 393.0 393.1 Aly, Ameera Syafiqah; Mamikutty, Rokiah; Marhazlinda, Jamaludin (31 October 2022). "Association between Harmful and Addictive Perceptions of E-Cigarettes and E-Cigarette Use among Adolescents and Youth—A Systematic Review and Meta-Analysis". Children. 9 (11): 1678. doi:10.3390/children9111678. PMC 9689130. PMID 36360406.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Ameera Syafiqah Aly, Rokiah Mamikutty, and Jamaludin Marhazlinda1 available under the CC BY 4.0 license.
This article incorporates text by Ameera Syafiqah Aly, Rokiah Mamikutty, and Jamaludin Marhazlinda1 available under the CC BY 4.0 license.
- ↑ Keijsers, Merel; Vega-Corredor, Maria Cecilia; Hoermann, Simon; Tomintz, Melanie (January 2022). "Cue Reactivity to Electronic Cigarettes: A Systematic Review". Substance Abuse: Research and Treatment. 16: 117822182211149. doi:10.1177/11782218221114971. PMC 9340385. PMID 35923180.
- ↑ Bold, Krysten W.; Sussman, Steve; O'Malley, Stephanie S.; Grana, Rachel; Foulds, Jonathan; Fishbein, Howard; Krishnan-Sarin, Suchitra (2018). "Measuring E-cigarette dependence: Initial guidance". Addictive Behaviors. 79: 213–218. doi:10.1016/j.addbeh.2017.11.015. ISSN 0306-4603. PMC 5807200. PMID 29174664.
- ↑ Fried, Nicholas D.; Gardner, Jason D. (2020). "Heat-not-burn tobacco products: an emerging threat to cardiovascular health". American Journal of Physiology-Heart and Circulatory Physiology. 319 (6): H1234–H1239. doi:10.1152/ajpheart.00708.2020. ISSN 0363-6135. PMC 7792702. PMID 33006919.
- ↑ 397.0 397.1 397.2 397.3 397.4 397.5 397.6 397.7 Cervellin, Gianfranco; Borghi, Loris; Mattiuzzi, Camilla; Meschi, Tiziana; Favaloro, Emmanuel; Lippi, Giuseppe (16 December 2013). "E-Cigarettes and Cardiovascular Risk: Beyond Science and Mysticism". Seminars in Thrombosis and Hemostasis. 40 (1): 060–065. doi:10.1055/s-0033-1363468. ISSN 0094-6176. PMID 24343348.
- ↑ Schroeder, M. J.; Hoffman, A. C. (2014). "Electronic cigarettes and nicotine clinical pharmacology". Tobacco Control. 23 (Supplement 2): ii30–ii35. doi:10.1136/tobaccocontrol-2013-051469. ISSN 0964-4563. PMC 3995273. PMID 24732160.
- ↑ FDA (4 May 2009). "FDA 2009 Study Data: Evaluation of e-cigarettes" (PDF). Food and Drug Administration (US) -center for drug evaluation and research.
- ↑ Jeong, Won Tae; Cho, Hyun Ki; Lee, Hyung Ryeol; Song, Ki Hoon; Lim, Heung Bin (2019). "Comparison of the content of tobacco alkaloids and tobacco-specific nitrosamines in 'heat-not-burn' tobacco products before and after aerosol generation". Inhalation Toxicology. 30 (13–14): 527–533. doi:10.1080/08958378.2019.1572840. ISSN 0895-8378. PMID 30741569.
- ↑ Lee, Stella Juhyun; Rees, Vaughan W.; Yossefy, Noam; Emmons, Karen M.; Tan, Andy S. L. (1 July 2020). "Youth and Young Adult Use of Pod-Based Electronic Cigarettes From 2015 to 2019". JAMA Pediatrics. 174 (7): 714. doi:10.1001/jamapediatrics.2020.0259. ISSN 2168-6203. PMC 7863733. PMID 32478809.
- ↑ Soulet, Sebastien; Sussman, Roberto A. (22 November 2022). "Critical Review of the Recent Literature on Organic Byproducts in E-Cigarette Aerosol Emissions". Toxics. 10 (12): 714. doi:10.3390/toxics10120714. PMC 9787926. PMID 36548547.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Sebastien Soulet and Roberto A. Sussman available under the CC BY 4.0 license.
This article incorporates text by Sebastien Soulet and Roberto A. Sussman available under the CC BY 4.0 license.
- ↑ Voos, Natalie; Goniewicz, Maciej L.; Eissenberg, Thomas (2 November 2019). "What is the nicotine delivery profile of electronic cigarettes?". Expert Opinion on Drug Delivery. 16 (11): 1193–1203. doi:10.1080/17425247.2019.1665647. ISSN 1742-5247. PMC 6814574. PMID 31495244.
- ↑ 404.0 404.1 404.2 Bickel, WK; Pope, DA; Kaplan, BA; DeHart, WB; Koffarnus, MN; Stein, JS (December 2018). "Electronic cigarette substitution in the experimental tobacco marketplace: A review". Preventive medicine. 117: 98–106. doi:10.1016/j.ypmed.2018.04.026. PMC 6685072. PMID 29702131.
- ↑ Di Matteo, Vincenzo; Pierucci, Massimo; Di Giovanni, Giuseppe; Benigno, Arcangelo; Esposito, Ennio (2007). "The Neurobiological Bases for the Pharmacotherapy of Nicotine Addiction". Current Pharmaceutical Design. 13 (12): 1269–1284. doi:10.2174/138161207780618920. ISSN 1381-6128. PMID 17504235.
- ↑ 406.0 406.1 406.2 406.3 406.4 406.5 "Electronic Cigarettes (E-cigarettes)". National Institute on Drug Abuse. March 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 407.0 407.1 Golub, Justin S.; Samy, Ravi N. (2015). "Preventing or reducing smoking-related complications in otologic and neurotologic surgery". Current Opinion in Otolaryngology & Head and Neck Surgery. 23 (5): 334–340. doi:10.1097/MOO.0000000000000184. ISSN 1068-9508. PMID 26339963.
- ↑ 408.0 408.1 408.2 National Academies of Sciences, Engineering, and Medicine 2018, p. 193, Minor Tobacco Alkaloids.
- ↑ Toda, Noboru; Toda, Hiroshi (2010). "Nitric oxide-mediated blood flow regulation as affected by smoking and nicotine". European Journal of Pharmacology. 649 (1–3): 1–13. doi:10.1016/j.ejphar.2010.09.042. ISSN 0014-2999. PMID 20868673.
- ↑ 410.0 410.1 410.2 Garcia, Alexandra N.; Salloum, Ihsan M. (2015). "Polysomnographic sleep disturbances in nicotine, caffeine, alcohol, cocaine, opioid, and cannabis use: A focused review". The American Journal on Addictions. 24 (7): 590–598. doi:10.1111/ajad.12291. ISSN 1055-0496. PMID 26346395.
- ↑ Irish, Leah A.; Kline, Christopher E.; Gunn, Heather E.; Buysse, Daniel J.; Hall, Martica H. (2015). "The role of sleep hygiene in promoting public health: A review of empirical evidence". Sleep Medicine Reviews. 22: 23–36. doi:10.1016/j.smrv.2014.10.001. ISSN 1087-0792. PMC 4400203. PMID 25454674.
- ↑ Siqueira, Lorena M. (2016). "Nicotine and Tobacco as Substances of Abuse in Children and Adolescents". Pediatrics. 139 (1): e20163436. doi:10.1542/peds.2016-3436. ISSN 0031-4005. PMID 27994114.
- ↑ 413.0 413.1 413.2 413.3 413.4 413.5 "WHO Right to Call for E-Cigarette Regulation". World Lung Federation. 26 August 2014.
- ↑ 414.0 414.1 National Academies of Sciences, Engineering, and Medicine 2018, p. 111, Other Effects of Nicotine–Cardiovascular Effects.
- ↑ Morris, Pamela B.; Ference, Brian A.; Jahangir, Eiman; Feldman, Dmitriy N.; Ryan, John J.; Bahrami, Hossein; El-Chami, Mikhael F.; Bhakta, Shyam; Winchester, David E.; Al-Mallah, Mouaz H.; Sanchez Shields, Monica; Deedwania, Prakash; Mehta, Laxmi S.; Phan, Binh An P.; Benowitz, Neal L. (2015). "Cardiovascular Effects of Exposure to Cigarette Smoke and Electronic Cigarettes". Journal of the American College of Cardiology. 66 (12): 1378–1391. doi:10.1016/j.jacc.2015.07.037. ISSN 0735-1097. PMID 26383726.
- ↑ 416.0 416.1 416.2 Maddatu, Judith; Anderson-Baucum, Emily; Evans-Molina, Carmella (2017). "Smoking and the risk of type 2 diabetes". Translational Research. 184: 101–107. doi:10.1016/j.trsl.2017.02.004. ISSN 1931-5244. PMC 5429867. PMID 28336465.
- ↑ 417.0 417.1 417.2 Ghanem, A.; Abduljabbar, T.; Akram, Z.; Vohra, F.; Kellesarian, S.V.; Javed, F. (2017). "A systematic review and meta-analysis of pre-clinical studies assessing the effect of nicotine on osseointegration". International Journal of Oral and Maxillofacial Surgery. 46 (4): 496–502. doi:10.1016/j.ijom.2016.12.003. ISSN 0901-5027. PMID 28189374.
- ↑ 418.0 418.1 Greenberg, Jordan M.; Carballosa, Carlos M.; Cheung, Herman S. (2017). "Concise Review: The Deleterious Effects of Cigarette Smoking and Nicotine Usage and Mesenchymal Stem Cell Function and Implications for Cell-Based Therapies". STEM CELLS Translational Medicine. 6 (9): 1815–1821. doi:10.1002/sctm.17-0060. ISSN 2157-6564. PMC 5689746. PMID 28696009.
- ↑ Lee, Peter N.; Fariss, Marc W. (2016). "A systematic review of possible serious adverse health effects of nicotine replacement therapy". Archives of Toxicology. 91 (4): 1565–1594. doi:10.1007/s00204-016-1856-y. ISSN 0340-5761. PMC 5364244. PMID 27699443.
- ↑ Gomes, João Pedro; Watad, Abdulla; Shoenfeld, Yehuda (2017). "Nicotine and Autoimmunity: the Lotus' Flower in Tobacco". Pharmacological Research. 128: 101–109. doi:10.1016/j.phrs.2017.10.005. ISSN 1043-6618. PMID 29051105.
- ↑ Machaalani, Rita; Chen, Hui (2018). "Brain derived neurotrophic factor (BDNF), its tyrosine kinase receptor B (TrkB) and nicotine". NeuroToxicology. 65: 186–195. doi:10.1016/j.neuro.2018.02.014. hdl:10453/122789. ISSN 0161-813X. PMID 29499216. S2CID 3688206.
- ↑ Smith, Tracy T.; Rupprecht, Laura E.; Denlinger-Apte, Rachel L.; Weeks, Jillian J.; Panas, Rachel S.; Donny, Eric C.; Sved, Alan F. (2017). "Animal research on nicotine reduction: Current evidence and research gaps". Nicotine & Tobacco Research. 19 (9): 1005–1015. doi:10.1093/ntr/ntx077. ISSN 1462-2203. PMC 5896531. PMID 28379511.
- ↑ "THE FACTS on e-cigarette use among youth and young adults". Surgeon General of the United States. 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 424.0 424.1 Yuan, Menglu; Cross, Sarah J.; Loughlin, Sandra E.; Leslie, Frances M. (2015). "Nicotine and the adolescent brain". The Journal of Physiology. 593 (16): 3397–3412. doi:10.1113/JP270492. ISSN 0022-3751. PMC 4560573. PMID 26018031.
- ↑ 425.0 425.1 425.2 Chapman 2015, p. 6.
- ↑ "People who want to quit smoking should consult their GP". Faculty of Public Health. July 2014. Archived from the original on 2016-06-15.
- ↑ Collaco, Joseph M.; McGrath-Morrow, Sharon A. (2018). "Electronic Cigarettes: Exposure and Use Among Pediatric Populations". Journal of Aerosol Medicine and Pulmonary Drug Delivery. 31 (2): 71–77. doi:10.1089/jamp.2017.1418. ISSN 1941-2711. PMC 5915214. PMID 29068754.
- ↑ "Why Is Nicotine Unsafe for Kids, Teens, and Young Adults?". Centers for Disease Control and Prevention. 2 November 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 429.0 429.1 Wyman, Anne E.; Hines, Stella E. (2018). "Update on metal-induced occupational lung disease". Current Opinion in Allergy and Clinical Immunology. 18 (2): 73–79. doi:10.1097/ACI.0000000000000420. ISSN 1528-4050. PMID 29337701.
- ↑ V.Courtney Broaddus; Robert C Mason; Joel D Ernst; Talmadge E King Jr.; Stephen C Lazarus; John F. Murray; Jay A. Nadel; Arthur Slutsky; Michael Gotway (17 March 2015). Murray & Nadel's Textbook of Respiratory Medicine. Elsevier Health Sciences. p. 820. ISBN 978-0-323-26193-7.
- ↑ 431.0 431.1 431.2 Kleinstreuer, Clement; Feng, Yu (2013). "Lung Deposition Analyses of Inhaled Toxic Aerosols in Conventional and Less Harmful Cigarette Smoke: A Review". International Journal of Environmental Research and Public Health. 10 (9): 4454–4485. doi:10.3390/ijerph10094454. ISSN 1660-4601. PMC 3799535. PMID 24065038.
- ↑ Chattopadhyay, Suhana; Malayil, Leena; Mongodin, Emmanuel F.; Sapkota, Amy R. (April 2021). "A roadmap from unknowns to knowns: Advancing our understanding of the microbiomes of commercially available tobacco products". Applied Microbiology and Biotechnology. 105 (7): 2633–2645. doi:10.1007/s00253-021-11183-4. PMC 7948171. PMID 33704513.
- ↑ 433.0 433.1 433.2 Casey, AM; Muise, ED; Crotty Alexander, LE (October 2020). "Vaping and e-cigarette use. Mysterious lung manifestations and an epidemic". Current opinion in immunology. 66: 143–150. doi:10.1016/j.coi.2020.10.003. ISSN 0952-7915. PMC 7755270. PMID 33186869.
- ↑ 434.0 434.1 434.2 434.3 Davis, Lauren C.; Sapey, Elizabeth; Thickett, David R.; Scott, Aaron (31 March 2022). "Predicting the pulmonary effects of long-term e-cigarette use: are the clouds clearing?". European Respiratory Review. 31 (163): 210121. doi:10.1183/16000617.0121-2021. PMC 9488959. PMID 35022257.
- ↑ 435.0 435.1 435.2 435.3 435.4 435.5 Bagale, Kamal; Kulkarni, Ritwij (30 September 2022). "A Systematic Review of the Literature Examining the Effects of Cigarette Smoke and e-Cigarette Vapor on the Virulence of Human Pathogenic Bacteria". International Journal of Environmental Research and Public Health. 19 (19): 12518. doi:10.3390/ijerph191912518. PMC 9565164. PMID 36231813.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Kamal Bagale and Ritwij Kulkarni available under the CC BY 4.0 license.
This article incorporates text by Kamal Bagale and Ritwij Kulkarni available under the CC BY 4.0 license.
- ↑ 436.00 436.01 436.02 436.03 436.04 436.05 436.06 436.07 436.08 436.09 436.10 436.11 436.12 Quinones Tavarez, Zahira; Li, Dongmei; Croft, Daniel P.; Gill, Steven R.; Ossip, Deborah J.; Rahman, Irfan (2020). "The Interplay Between Respiratory Microbiota and Innate Immunity in Flavor E-Cigarette Vaping Induced Lung Dysfunction". Frontiers in Microbiology. 11. doi:10.3389/fmicb.2020.589501. ISSN 1664-302X. PMC 7772214. PMID 33391205.
 This article incorporates text by Zahira Quinones Tavarez, Dongmei Li, Daniel P. Croft, Steven R. Gill, Deborah. Ossip, and Irfan Rahman5 available under the CC BY 4.0 license.
This article incorporates text by Zahira Quinones Tavarez, Dongmei Li, Daniel P. Croft, Steven R. Gill, Deborah. Ossip, and Irfan Rahman5 available under the CC BY 4.0 license.
- ↑ "Position Statement on Electronic Cigarettes [ECs] or Electronic Nicotine Delivery Systems [ENDS]" (PDF). The International Union against Tuberculosis and Lung Disease. October 2013. p. 8.
- ↑ McNeill 2018, p. 12.
- ↑ Wills, Thomas A.; Soneji, Samir S.; Choi, Kelvin; Jaspers, Ilona; Tam, Elizabeth K. (2021). "E-cigarette use and respiratory disorders: an integrative review of converging evidence from epidemiological and laboratory studies". European Respiratory Journal. 57 (1): 1901815. doi:10.1183/13993003.01815-2019. ISSN 0903-1936. PMC 7817920. PMID 33154031.
- ↑ Tarran, Robert; Barr, R Graham; Benowitz, Neal L; Bhatnagar, Aruni; Chu, Hong W; Dalton, Pamela; Doerschuk, Claire M; Drummond, M Bradley; Gold, Diane R; Goniewicz, Maciej L; Gross, Eric R; Hansel, Nadia N; Hopke, Philip K; Kloner, Robert A; Mikheev, Vladimir B; Neczypor, Evan W; Pinkerton, Kent E; Postow, Lisa; Rahman, Irfan; Samet, Jonathan M; Salathe, Matthias; Stoney, Catherine M; Tsao, Philip S; Widome, Rachel; Xia, Tian; Xiao, DaLiao; Wold, Loren E (2021). "E-Cigarettes and Cardiopulmonary Health". Function. 2 (2). doi:10.1093/function/zqab004. ISSN 2633-8823. PMC 7948134. PMID 33748758.
- ↑ Agudelo, Christina W.; Samaha, Ghassan; Garcia-Arcos, Itsaso (2020). "Alveolar lipids in pulmonary disease. A review". Lipids in Health and Disease. 19 (1). doi:10.1186/s12944-020-01278-8. ISSN 1476-511X. PMC 7268969. PMID 32493486.
 This article incorporates text by Christina W. Agudelo, Ghassan Samaha, and Itsaso Garcia-Arcos available under the CC BY 4.0 license.
This article incorporates text by Christina W. Agudelo, Ghassan Samaha, and Itsaso Garcia-Arcos available under the CC BY 4.0 license.
- ↑ Vogel, Wendy H. (2016). "E-Cigarettes: Are They as Safe as the Public Thinks?". Journal of the Advanced Practitioner in Oncology. 7 (2): 235–240. doi:10.6004/jadpro.2016.7.2.9. ISSN 2150-0878. PMC 5226315. PMID 28090372.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 7, Summary.
- ↑ Critselis, Elena; Panagiotakos, Demosthenes (13 March 2023). "Impact of Electronic Cigarette use on Cardiovascular Health: Current Evidence, Causal Pathways, and Public Health Implications". Angiology: 000331972311619. doi:10.1177/00033197231161905. PMID 36913951.
- ↑ Herman, Melissa; Tarran, Robert (November 2020). "E‐cigarettes, nicotine, the lung and the brain: multi‐level cascading pathophysiology". The Journal of Physiology. 598 (22): 5063–5071. doi:10.1113/JP278388. PMC 7721976. PMID 32515030.
- ↑ 446.0 446.1 446.2 446.3 446.4 Zainol Abidin, Najihah; Zainal Abidin, Emilia; Zulkifli, Aziemah; Karuppiah, Karmegam; Syed Ismail, Sharifah Norkhadijah; Amer Nordin, Amer Siddiq (2017). "Electronic cigarettes and indoor air quality: a review of studies using human volunteers". Reviews on Environmental Health. 0 (3): 235–244. doi:10.1515/reveh-2016-0059. ISSN 2191-0308. PMID 28107173.
- ↑ "Position Statement Electronic Cigarettes". Cancer Council Australia, Heart Foundation of Australia.
- ↑ 448.0 448.1 Effah, Felix; Taiwo, Benjamin; Baines, Deborah; Bailey, Alexis; Marczylo, Tim (3 October 2022). "Pulmonary effects of e-liquid flavors: a systematic review". Journal of Toxicology and Environmental Health, Part B. 25 (7): 343–371. doi:10.1080/10937404.2022.2124563. PMC 9590402. PMID 36154615.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Felix Effah, Benjamin Taiwo, Deborah Baines, Alexis Bailey, and Tim Marczylo available under the CC BY 4.0 license.
This article incorporates text by Felix Effah, Benjamin Taiwo, Deborah Baines, Alexis Bailey, and Tim Marczylo available under the CC BY 4.0 license.
- ↑ 449.0 449.1 Schiliro, Marta; Vogel, Elizabeth R.; Paolini, Lucia; Pabelick, Christina M. (2021). "Cigarette Smoke Exposure, Pediatric Lung Disease, and COVID-19". Frontiers in Physiology. 12. doi:10.3389/fphys.2021.652198. ISSN 1664-042X. PMC 8110920. PMID 33986692.
 This article incorporates text by Marta Schiliro, Elizabeth R. Vogel, Lucia Paolini, and Christina M. Pabelick1 available under the CC BY 4.0 license.
This article incorporates text by Marta Schiliro, Elizabeth R. Vogel, Lucia Paolini, and Christina M. Pabelick1 available under the CC BY 4.0 license.
- ↑ 450.0 450.1 National Academies of Sciences, Engineering, and Medicine 2018, p. 448, =Vulnerable/Susceptible Populations, Asthma and Other Respiratory Diseases of Childhood.
- ↑ McNeill 2018, p. 174.
- ↑ Eissenberg, Thomas (October 2013). "NIDA TV Spotlight on Electronic Cigarettes". National Institute on Drug Abuse.
- ↑ 453.0 453.1 "Vape Epidemic". United States Department of Health and Human Services. 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Heldt, Nathan A.; Reichenbach, Nancy; McGary, Hannah M.; Persidsky, Yuri (February 2021). "Effects of Electronic Nicotine Delivery Systems and Cigarettes on Systemic Circulation and Blood-Brain Barrier". The American Journal of Pathology. 191 (2): 243–255. doi:10.1016/j.ajpath.2020.11.007. PMC 7863131. PMID 33285126.
- ↑ 455.0 455.1 455.2 "White Paper: Electronic Cigarettes in the Indoor Environment" (PDF). American Industrial Hygiene Association. 19 October 2014. Archived from the original (PDF) on 25 January 2017. Retrieved 18 August 2016.
- ↑ 456.0 456.1 456.2 456.3 456.4 456.5 Boudi, F Brian; Patel, Sonia; Boudi, Ava; Chan, Connie (2019). "Vitamin E Acetate as a Plausible Cause of Acute Vaping-related Illness". Cureus. 11 (12): e6350. doi:10.7759/cureus.6350. ISSN 2168-8184. PMC 6952050. PMID 31938636.
 This article incorporates text by F Brian Boudi, Sonia Patel, Ava Boudi, Connie Chan available under the CC BY 3.0 license.
This article incorporates text by F Brian Boudi, Sonia Patel, Ava Boudi, Connie Chan available under the CC BY 3.0 license.
- ↑ Henry, Travis S.; Kligerman, Seth J.; Raptis, Constantine A.; Mann, Howard; Sechrist, Jacob W.; Kanne, Jeffrey P. (2019). "Imaging Findings of Vaping-Associated Lung Injury". American Journal of Roentgenology: 1–8. doi:10.2214/AJR.19.22251. ISSN 0361-803X. PMID 31593518. S2CID 203985885.
- ↑ 458.0 458.1 Laudanski, Krzysztof; Wain, Justin (22 January 2022). "Considerations for Cannabinoids in Perioperative Care by Anesthesiologists". Journal of Clinical Medicine. 11 (3): 558. doi:10.3390/jcm11030558. PMC 8836924. PMID 35160010.
 This article incorporates text by Krzysztof Laudanski and Justin Wain2 available under the CC BY 4.0 license.
This article incorporates text by Krzysztof Laudanski and Justin Wain2 available under the CC BY 4.0 license.
- ↑ 459.00 459.01 459.02 459.03 459.04 459.05 459.06 459.07 459.08 459.09 459.10 459.11 459.12 459.13 459.14 459.15 459.16 459.17 459.18 459.19 459.20 459.21 459.22 Mescolo, Federica; Ferrante, Giuliana; La Grutta, Stefania (20 August 2021). "Effects of E-Cigarette Exposure on Prenatal Life and Childhood Respiratory Health: A Review of Current Evidence". Frontiers in Pediatrics. 9: 711573. doi:10.3389/fped.2021.711573. PMC 8430837. PMID 34513764.
 This article incorporates text by Federica Mescolo, Giuliana Ferrante, and Stefania La Grutta available under the CC BY 4.0 license.
This article incorporates text by Federica Mescolo, Giuliana Ferrante, and Stefania La Grutta available under the CC BY 4.0 license.
- ↑ "New York State Department of Health Announces Update on Investigation into Vaping-Associated Pulmonary Illnesses". New York State Department of Health. 5 September 2019.
- ↑ Layden, Jennifer E.; Ghinai, Isaac; Pray, Ian; et al. (5 March 2020). "Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin — Final Report". New England Journal of Medicine. doi:10.1056/NEJMoa1911614. ISSN 0028-4793. PMID 31491072.
- ↑ Jonas, Andrea M.; Raj, Rishi (October 2020). "Vaping-Related Acute Parenchymal Lung Injury". Chest. 158 (4): 1555–1565. doi:10.1016/j.chest.2020.03.085. PMID 32442559. S2CID 218857503.
- ↑ Public Health Agency of Canada (11 October 2019). "Statement from the Council of Chief Medical Officers of Health on vaping in Canada". Chief Public Health Officer of Canada.
- ↑ 464.0 464.1 464.2 464.3 "Tetrahydrocannabinol (THC)-containing Vaping Products: Vaping Illnesses". United States Food and Drug Administration. 6 September 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Transcript of CDC Telebriefing: Update on Lung Injury Associated with E-cigarette Use, or Vaping". Centers for Disease Control and Prevention. 8 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 466.0 466.1 466.2 466.3 Dickson, EJ (10 September 2019). "Three Companies Subpoenaed in Weed Vape Illness Investigation". Rolling Stone.
- ↑ Goldman, Henry (9 September 2019). "Cuomo Signals N.Y. Crackdown on Vaping Products After Illnesses". Bloomberg News.
- ↑ 468.0 468.1 O'Donnell, Jayne; Robinson, David (15 November 2019). "People are vaping a deadly substance along with THC. Why isn't vitamin E acetate illegal?". USA Today.
- ↑ Farber, Madeline (20 November 2019). "Washington state bans vape products that contain vitamin E acetate". Fox News.
- ↑ Zarkhin, Fedor (22 November 2019). "Vitamin E acetate banned from Oregon cannabis vaping products". The Oregonian.
- ↑ Szklarski, Cassandra (8 November 2019). "Health Canada 'actively monitoring' U.S. vaping illness breakthrough". National Post. The Canadian Press.
- ↑ 472.0 472.1 Gaitan, Daniel (18 November 2022). "Six involved in illegal THC cartridge scheme sentenced in Kenosha County Circuit Court". Kenosha News.
- ↑ "Mother and sons convicted in Kenosha County THC vape ring avoid prison time". WISN-TV. 18 November 2022.
- ↑ "Kenosha County THC vape ring convict arrested on drug charges". FOX6 News Milwaukee. 2 August 2022.
- ↑ Vergano, Dan (30 August 2019). "The Vaping Lung Illness Outbreak Has Now Spread To 25 States". BuzzFeed News.
- ↑ Joyner, April (18 August 2019). "CDC probes lung illnesses linked to e-cigarette use". Reuters.
- ↑ 477.0 477.1 477.2 477.3 477.4 477.5 477.6 477.7 Zong, Huiqi; Hu, Zhekai; Li, Weina; Wang, Mina; Zhou, Qi; Li, Xiang; Liu, Hongxu (20 February 2024). "Electronic cigarettes and cardiovascular disease: epidemiological and biological links". Pflügers Archiv - European Journal of Physiology. doi:10.1007/s00424-024-02925-0. PMC 11139732. PMID 38376568.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Huiqi Zong, Zhekai Hu, Weina Li, Mina Wang, Qi Zhou, Xiang Li, Hongxu Liu available under the CC BY 4.0 license.
This article incorporates text by Huiqi Zong, Zhekai Hu, Weina Li, Mina Wang, Qi Zhou, Xiang Li, Hongxu Liu available under the CC BY 4.0 license.
- ↑ 478.0 478.1 478.2 478.3 478.4 La Rosa, Giusy; Vernooij, Robin; Qureshi, Maria; Polosa, Riccardo; O’Leary, Renée (April 2023). "Clinical testing of the cardiovascular effects of e-cigarette substitution for smoking: a living systematic review". Internal and Emergency Medicine. 18 (3): 917–928. doi:10.1007/s11739-022-03161-z. PMC 10081981. PMID 36609804.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Giusy La Rosa, Robin Vernooij, Maria Qureshi, Riccardo Polosa, and Renée O’Leary available under the CC BY 4.0 license.
This article incorporates text by Giusy La Rosa, Robin Vernooij, Maria Qureshi, Riccardo Polosa, and Renée O’Leary available under the CC BY 4.0 license.
- ↑ 479.0 479.1 Skotsimara, Georgia; Antonopoulos, Alexios S; Oikonomou, Evangelos; Siasos, Gerasimos; Ioakeimidis, Nikolaos; Tsalamandris, Sotirios; Charalambous, Georgios; Galiatsatos, Nikos; Vlachopoulos, Charalambos; Tousoulis, Dimitris (2019). "Cardiovascular effects of electronic cigarettes: A systematic review and meta-analysis". European Journal of Preventive Cardiology. 26 (11): 1219–1228. doi:10.1177/2047487319832975. ISSN 2047-4873. PMID 30823865.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 3, Summary.
- ↑ Siddiqi, Tariq Jamal; Rashid, Ahmed Mustafa; Siddiqi, Ahmed Kamal; Anwer, Anusha; Usman, Muhammad Shariq; Sakhi, Hifza; Bhatnagar, Aruni; Hamburg, Naomi M.; Hirsch, Glenn A.; Rodriguez, Carlos J.; Blaha, Michael J.; DeFilippis, Andrew P.; Benjamin, Emelia J.; Hall, Michael E. (September 2023). "Association of Electronic Cigarette Exposure on Cardiovascular Health: A Systematic Review and Meta-Analysis". Current Problems in Cardiology. 48 (9): 101748. doi:10.1016/j.cpcardiol.2023.101748. PMID 37088177.
- ↑ Sharma, A; Gupta, I; Venkatesh, U; Singh, AK; Golamari, R; Arya, P (15 January 2023). "E-cigarettes and myocardial infarction: A systematic review and meta-analysis". International journal of cardiology. 371: 65–70. doi:10.1016/j.ijcard.2022.09.007. PMID 36087629.
- ↑ 483.0 483.1 483.2 483.3 483.4 Solesio, Maria E; Mitaishvili, Erna; Lymperopoulos, Anastasios (2019). "Adrenal βarrestin1 targeting for tobacco–associated cardiac dysfunction treatment: Aldosterone production as the mechanistic link". Pharmacology Research & Perspectives. 7 (4). doi:10.1002/prp2.497. ISSN 2052-1707. PMC 6581946. PMID 31236278.
 This article incorporates text by Maria E Solesio, Erna Mitaishvili, and Anastasios Lymperopoulos available under the CC BY 4.0 license.
This article incorporates text by Maria E Solesio, Erna Mitaishvili, and Anastasios Lymperopoulos available under the CC BY 4.0 license.
- ↑ Milosz Knur; Jonasz Dragon; Krzysztof Labuzek; Boguslaw Okopien (January 2018). "[The impact of electronic cigarettes usage on the endothelial function and the progression of atherosclerosis]". Polski Merkuriusz Lekarski : Organ Polskiego Towarzystwa Lekarskiego. 44 (259): 26–30. PMID 29374420.
- ↑ 485.0 485.1 485.2 Chapman 2015, p. 5.
- ↑ 486.0 486.1 Nelluri, Bhargava; Murphy, Katie; Mookadam, Farouk; Mookadam, Martina (2016). "The current literature regarding the cardiovascular effects of electronic cigarettes". Future Cardiology. 12 (2): 167–179. doi:10.2217/fca.15.83. ISSN 1479-6678. PMID 26916427.
- ↑ Oakes, Joshua M.; Fuchs, Robert M.; Gardner, Jason D.; Lazartigues, Eric; Yue, Xinping (2018). "Nicotine and the renin-angiotensin system". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 315 (5): R895–R906. doi:10.1152/ajpregu.00099.2018. ISSN 0363-6119. PMC 6295500. PMID 30088946.
- ↑ Guzik, Amy; Bushnell, Cheryl (2017). "Stroke Epidemiology and Risk Factor Management". CONTINUUM: Lifelong Learning in Neurology. 23 (1, Cerebrovascular Disease): 15–39. doi:10.1212/CON.0000000000000416. ISSN 1080-2371. PMID 28157742.
- ↑ 489.00 489.01 489.02 489.03 489.04 489.05 489.06 489.07 489.08 489.09 489.10 Brar, Esha; Saxena, Anish; Dukler, Claudia; Xu, Fangxi; Saxena, Deepak; Cheema Brar, Preneet; Guo, Yuqi; Li, Xin (2021). "Vaping, SARS-CoV-2, and Multisystem Inflammatory Syndrome: A Perfect Storm". Frontiers in Pediatrics. 9. doi:10.3389/fped.2021.647925. ISSN 2296-2360. PMC 8149601. PMID 34055688.
 This article incorporates text by Esha Brar, Anish Saxena, Claudia Dukler, Fangxi Xu, Deepak Saxena, Preneet Cheema Brar, Yuqi Guo, and Xin Li available under the CC BY 4.0 license.
This article incorporates text by Esha Brar, Anish Saxena, Claudia Dukler, Fangxi Xu, Deepak Saxena, Preneet Cheema Brar, Yuqi Guo, and Xin Li available under the CC BY 4.0 license.
- ↑ 490.0 490.1 490.2 490.3 490.4 490.5 Kaur, Gagandeep; Lungarella, Giuseppe; Rahman, Irfan (10 June 2020). "SARS-CoV-2 COVID-19 susceptibility and lung inflammatory storm by smoking and vaping". Journal of Inflammation. 17 (1): 21. doi:10.1186/s12950-020-00250-8. PMC 7284674. PMID 32528233.
 This article incorporates text by Gagandeep Kaur, Giuseppe Lungarella, and Irfan Rahman available under the CC BY 4.0 license.
This article incorporates text by Gagandeep Kaur, Giuseppe Lungarella, and Irfan Rahman available under the CC BY 4.0 license.
- ↑ Gupta, Priya Sarin; Kalagher, Kelly M. (2021). "Where There Is (No) Smoke, There Is Still Fire: a Review of Trends, Reasons for Use, Preferences and Harm Perceptions of Adolescent and Young Adult Electronic Cigarette Use". Current Pediatrics Reports. doi:10.1007/s40124-021-00240-1. ISSN 2167-4841. PMC 8107807. PMID 33996271.
- ↑ 492.0 492.1 492.2 Gordon, Terry; Karey, Emma; Rebuli, Meghan E.; Escobar, Yael-Natalie H.; Jaspers, Ilona; Chen, Lung Chi (6 January 2022). "E-Cigarette Toxicology". Annual Review of Pharmacology and Toxicology. 62 (1): 301–322. doi:10.1146/annurev-pharmtox-042921-084202. PMC 9386787. PMID 34555289.
- ↑ 493.0 493.1 AL-Qaysi, Wafaa Waleed; Abdulla, Fatma H. (December 2021). "Analytical methods for the identification of micro/nano metals in e-cigarette emission samples: a review". Chemical Papers. 75 (12): 6169–6180. doi:10.1007/s11696-021-01779-5. PMC 8370834. PMID 34421189.
- ↑ Jonas, Andrea (18 July 2022). "Impact of vaping on respiratory health". BMJ: e065997. doi:10.1136/bmj-2021-065997. PMID 35851281.
- ↑ Benowitz, Neal L; Goniewicz, Maciej L; Halpern-Felsher, Bonnie; Krishnan-Sarin, Suchitra; Ling, Pamela M; O'Connor, Richard J; Pent, Mary Ann; Robertson, Rose Marie; Bhatnagar, Aruni (September 2022). "Tobacco product use and the risks of SARS-CoV-2 infection and COVID-19: current understanding and recommendations for future research". The Lancet Respiratory Medicine. 10 (9): 900–915. doi:10.1016/S2213-2600(22)00182-5. PMID 35985357.
- ↑ 496.0 496.1 Singhal, S; Degano, C; Berenbaum, E; Keller-Olaman, S (January 2022). "Does Vaping Increase the Risk of COVID-19 Transmission and Make Individuals Who Vape Susceptible to Infection and Prone to Severe Illness? A Review". Journal (Canadian Dental Association). 88: m1. PMID 35881057.
- ↑ 497.0 497.1 497.2 497.3 Pincus, J; Sandoval, V; Dick, B; Sanekommu, G; Rajasekaran, R; Ramasamy, R; Raheem, O (10 January 2022). "E-Cigarette-Associated Endothelial Damage: A Potential Mechanism for Erectile Dysfunction". Sexual medicine reviews. 10 (1): 168–173. doi:10.1016/j.sxmr.2021.01.003. PMID 33931382.
- ↑ 498.0 498.1 Martheswaran, Tanisha; Shmunes, Margaret H.; Ronquillo, Yasmyne C.; Moshirfar, Majid (2021). "The impact of vaping on ocular health: a literature review". International Ophthalmology. doi:10.1007/s10792-021-01842-w. ISSN 0165-5701. PMID 33860887.
- ↑ 499.0 499.1 499.2 499.3 499.4 Konstantinidou, Fani; Stuppia, Liborio; Gatta, Valentina (September 2020). "Looking Inside the World of Granulosa Cells: The Noxious Effects of Cigarette Smoke". Biomedicines. 8 (9): 309. doi:10.3390/biomedicines8090309. PMID 32867029.
 This article incorporates text by Fani Konstantinidou, Liborio Stuppia, and Valentina Gatta available under the CC BY 4.0 license.
This article incorporates text by Fani Konstantinidou, Liborio Stuppia, and Valentina Gatta available under the CC BY 4.0 license.
- ↑ 500.0 500.1 500.2 500.3 500.4 500.5 Verhaegen, A.; Van Gaal, L. (2017). "Do E-cigarettes induce weight changes and increase cardiometabolic risk? A signal for the future". Obesity Reviews. 18 (10): 1136–1146. doi:10.1111/obr.12568. ISSN 1467-7881. PMID 28660671.
- ↑ 501.0 501.1 Keith, Rachel; Bhatnagar, Aruni (2021). "Cardiorespiratory and Immunologic Effects of Electronic Cigarettes". Current Addiction Reports. 8 (2): 336–346. doi:10.1007/s40429-021-00359-7. ISSN 2196-2952. PMC 7935224. PMID 33717828.
- ↑ 502.0 502.1 502.2 Laviolette, Steven R. (February 2021). "Molecular and neuronal mechanisms underlying the effects of adolescent nicotine exposure on anxiety and mood disorders". Neuropharmacology. 184: 108411. doi:10.1016/j.neuropharm.2020.108411. PMID 33245960.
- ↑ Colyer-Patel, Karis; Kuhns, Lauren; Weidema, Alix; Lesscher, Heidi; Cousijn, Janna (March 2023). "Age-dependent effects of tobacco smoke and nicotine on cognition and the brain: A systematic review of the human and animal literature comparing adolescents and adults". Neuroscience & Biobehavioral Reviews. 146: 105038. doi:10.1016/j.neubiorev.2023.105038. PMID 36627063.
- ↑ 504.0 504.1 504.2 504.3 504.4 504.5 Ding, Jack Baichao; Hu, Kevin (13 December 2021). "Cigarette Smoking and Schizophrenia: Etiology, Clinical, Pharmacological, and Treatment Implications". Schizophrenia Research and Treatment. 2021: 1–8. doi:10.1155/2021/7698030. PMID 34938579.
 This article incorporates text by Jack Baichao Ding and Kevin Hu available under the CC BY 4.0 license.
This article incorporates text by Jack Baichao Ding and Kevin Hu available under the CC BY 4.0 license.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 9, Summary–Conclusion 12-1..
- ↑ Irusa, Karina F.; Vence, Brian; Donovan, Terry (2020). "Potential oral health effects of e‐cigarettes and vaping: A review and case reports". Journal of Esthetic and Restorative Dentistry. 32 (3): 260–264. doi:10.1111/jerd.12583. ISSN 1496-4155. PMID 32243711.
- ↑ 507.0 507.1 Javed, Fawad; Kellesarian, Sergio V.; Sundar, Isaac K.; Romanos, Georgios E.; Rahman, Irfan (2017). "Recent Updates on Electronic Cigarette Aerosol and Inhaled Nicotine Effects on Periodontal and Pulmonary Tissues". Oral Diseases. 23 (8): 1052–1057. doi:10.1111/odi.12652. ISSN 1354-523X. PMC 5545167. PMID 28168771.
- ↑ Youssef, Moustafa; Marzouk, Tamer; Abdelsalam, Hossam; Malmstrom, Hans; Barmak, Abdul Basir; Fraser, David; Tsigarida, Alexandra (April 2023). "The effect of electronic cigarette use on peri-implant conditions in men: a systematic review and meta-analysis". Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 135 (4): 492–500. doi:10.1016/j.oooo.2022.08.010. PMID 36216745.
- ↑ Baniulyte, G.; Ali, K. (1 March 2023). "Do e-cigarettes have a part to play in peri-implant diseases?". Evidence-Based Dentistry. 24 (1): 7–8. doi:10.1038/s41432-023-00864-w. PMID 36890255.
- ↑ Kotewar, Samrudhi S; Pakhale, Aayushi; Tiwari, Rupali; Reche, Amit; Singi, Shriya R (13 August 2023). "Electronic Nicotine Delivery System: End to Smoking or Just a New Fancy Cigarette". Cureus. doi:10.7759/cureus.43425. PMC 10497069. PMID 37706142.
{{cite journal}}: Check|pmc=value (help) - ↑ 511.0 511.1 Guo, Xingtong; Hou, Lili; Peng, Xuepei; Tang, Fuyou (9 February 2023). "The prevalence of xerostomia among e-cigarette or combustible tobacco users: A systematic review and meta-analysis". Tobacco Induced Diseases. 21 (February): 1–11. doi:10.18332/tid/156676. PMID 36777290.
- ↑ 512.0 512.1 512.2 512.3 512.4 512.5 512.6 Visconti, Michael J.; Ashack, Kurt A. (2019). "Dermatologic manifestations associated with electronic cigarette use". Journal of the American Academy of Dermatology. 81 (4): 1001–1007. doi:10.1016/j.jaad.2019.03.088. ISSN 0190-9622. PMID 30965061. S2CID 106409405.
- ↑ 513.0 513.1 Patel, S; Wooles, N; Martin, T (November 2020). "A systematic review of the impact of cigarettes and electronic cigarettes in otology". The Journal of Laryngology & Otology. 134 (11): 951–956. doi:10.1017/S0022215120002315. PMID 33272335.
- ↑ 514.0 514.1 514.2 514.3 Fiani, Brian; Noblett, Christian; Nanney, Jacob M; Gautam, Neha; Pennington, Elisabeth; Doan, Thao; Nikolaidis, Daniel (29 June 2020). "The Impact of "Vaping" Electronic Cigarettes on Spine Health". Cureus. doi:10.7759/cureus.8907.
 This article incorporates text by Brian Fiani, Christian Noblett, Jacob M Nanney, Neha Gautam, Elisabeth Pennington, Thao Doan, and Daniel Nikolaidis available under the CC BY 4.0 license.
This article incorporates text by Brian Fiani, Christian Noblett, Jacob M Nanney, Neha Gautam, Elisabeth Pennington, Thao Doan, and Daniel Nikolaidis available under the CC BY 4.0 license.
- ↑ Nicholson, Thomas; Scott, Aaron; Newton Ede, Matthew; Jones, Simon W. (2021). "The impact of E-cigarette vaping and vapour constituents on bone health". Journal of Inflammation. 18 (1). doi:10.1186/s12950-021-00283-7. ISSN 1476-9255. PMC 8097983. PMID 33952248.
 This article incorporates text by Thomas Nicholson, Aaron Scott, Matthew Newton Ede, and Simon W. Jones available under the CC BY 4.0 license.
This article incorporates text by Thomas Nicholson, Aaron Scott, Matthew Newton Ede, and Simon W. Jones available under the CC BY 4.0 license.
- ↑ Damay, Vito Anggarino; Setiawan, Setiawan; Lesmana, Ronny; Akbar, Mohammad Rizki; Lukito, Antonia Anna (30 September 2022). "How Electronic Cigarette Affects the Vascular System". Journal of Smoking Cessation. 2022: 1–9. doi:10.1155/2022/3216580. PMC 9553677. PMID 36262466.
{{cite journal}}: Check|pmc=value (help) - ↑ 517.0 517.1 517.2 517.3 Fracol, Megan; Dorfman, Robert; Janes, Lindsay; Kulkarni, Swati; Bethke, Kevin; Hansen, Nora; Kim, John (2017). "The Surgical Impact of E-Cigarettes: A Case Report and Review of the Current Literature". Archives of Plastic Surgery. 44 (6): 477–481. doi:10.5999/aps.2017.00087. ISSN 2234-6163. PMC 5801784. PMID 29069879.
- ↑ Ashour, Omar; Al-Huneidy, Leen; Noordeen, Hilali (March 2023). "The implications of vaping on surgical wound healing: A systematic review". Surgery: S0039606023000922. doi:10.1016/j.surg.2023.02.017. PMID 36997424.
- ↑ 519.0 519.1 Karanjkar, Rijula R.; Preshaw, Philip M.; Ellis, Janice S.; Holliday, Richard (February 2023). "Effect of tobacco and nicotine in causing staining of dental hard tissues and dental materials: A systematic review and meta‐analysis". Clinical and Experimental Dental Research. 9 (1): 150–164. doi:10.1002/cre2.683. PMC 9932248. PMID 36372903.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Rijula R Karanjkar, Philip M Preshaw, Janice S Ellis, and Richard Holliday available under the CC BY 4.0 license.
This article incorporates text by Rijula R Karanjkar, Philip M Preshaw, Janice S Ellis, and Richard Holliday available under the CC BY 4.0 license.
- ↑ 520.0 520.1 520.2 Paolone, Gaetano; Pavan, Francesca; Mandurino, Mauro; Baldani, Sofia; Guglielmi, Paolo Chiara; Scotti, Nicola; Cantatore, Giuseppe; Vichi, Alessandro (March 2023). "Color stability of resin‐based composites exposed to smoke. A systematic review". Journal of Esthetic and Restorative Dentistry. 35 (2): 309–321. doi:10.1111/jerd.13009. PMID 36602255.
- ↑ Caponnetto, Pasquale; Campagna, Davide; Papale, Gabriella; Russo, Cristina; Polosa, Riccardo (2012). "The emerging phenomenon of electronic cigarettes". Expert Review of Respiratory Medicine. 6 (1): 63–74. doi:10.1586/ers.11.92. ISSN 1747-6348. PMID 22283580. S2CID 207223131.
- ↑ "Supporting regulation of electronic cigarettes". www.apha.org. US: American Public Health Association. 18 November 2014.
- ↑ Wang, Guanghe; Liu, Wenjing; Song, Weimin (2019). "Toxicity assessment of electronic cigarettes". Inhalation Toxicology. 31 (7): 259–273. doi:10.1080/08958378.2019.1671558. ISSN 0895-8378. PMID 31556766. S2CID 203439670.
- ↑ Hanewinkel, Reiner; Niederberger, Kathrin; Pedersen, Anya; Unger, Jennifer B.; Galimov, Artur (31 March 2022). "E-cigarettes and nicotine abstinence: a meta-analysis of randomised controlled trials". European Respiratory Review. 31 (163): 210215. doi:10.1183/16000617.0215-2021. PMC 9488503. PMID 35321930.
- ↑ Staal, Yvonne C.M.; van de Nobelen, Suzanne; Havermans, Anne; Talhout, Reinskje (2018). "New Tobacco and Tobacco-Related Products: Early Detection of Product Development, Marketing Strategies, and Consumer Interest". JMIR Public Health and Surveillance. 4 (2): e55. doi:10.2196/publichealth.7359. ISSN 2369-2960. PMC 5996176. PMID 29807884.
 This article incorporates text by Yvonne CM Staal, Suzanne van de Nobelen, Anne Havermans, and Reinskje Talhout available under the CC BY 4.0 license.
This article incorporates text by Yvonne CM Staal, Suzanne van de Nobelen, Anne Havermans, and Reinskje Talhout available under the CC BY 4.0 license.
- ↑ Bam, T. S.; Bellew, W.; Berezhnova, I.; Jackson-Morris, A.; Jones, A.; Latif, E.; Molinari, M. A.; Quan, G.; Singh, R. J.; Wisotzky, M. (1 January 2014). "Position statement on electronic cigarettes or electronic nicotine delivery systems [Official statement]". The International Journal of Tuberculosis and Lung Disease. 18 (1): 5–7. doi:10.5588/ijtld.13.0815. PMID 24365545.
- ↑ Offermann, Francis (June 2014). "The Hazards of E-Cigarettes" (PDF). ASHRAE Journal. 56 (6).
- ↑ 528.0 528.1 "Surgeon General Reports Youth and Young Adult E-Cigarette Use Poses a Public Health Threat". United States Department of Health and Human Services. 8 December 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "American Lung Association Statement on E-Cigarettes". American Lung Association. 25 August 2014.
- ↑ Wilder 2016, p. 84.
- ↑ Heydari, Gholamreza; Ahmady, ArezooEbn; Chamyani, Fahimeh; Masjedi, Mohammadreza; Fadaizadeh, Lida (2017). "Electronic cigarette, effective or harmful for quitting smoking and respiratory health: A quantitative review papers". Lung India. 34 (1): 25–28. doi:10.4103/0970-2113.197119. ISSN 0970-2113. PMC 5234193. PMID 28144056.
- ↑ Berlinski, Ariel (2020). "2019 Year in Review: Aerosol Therapy". Respiratory Care. 65 (5): 705–712. doi:10.4187/respcare.07738. ISSN 0020-1324. PMID 32345761.
- ↑ Collaco, Joseph M.; Aoyama, Brianna C.; Rice, Jessica L.; McGrath-Morrow, Sharon A. (3 October 2021). "Influences of environmental exposures on preterm lung disease". Expert Review of Respiratory Medicine. 15 (10): 1271–1279. doi:10.1080/17476348.2021.1941886. PMID 34114906.
- ↑ Glasser, Allison M.; Collins, Lauren; Pearson, Jennifer L.; Abudayyeh, Haneen; Niaura, Raymond S.; Abrams, David B.; Villanti, Andrea C. (2016). "Overview of Electronic Nicotine Delivery Systems: A Systematic Review". American Journal of Preventive Medicine. 52 (2): e33–e66. doi:10.1016/j.amepre.2016.10.036. ISSN 0749-3797. PMC 5253272. PMID 27914771.
- ↑ 535.0 535.1 Dicpinigaitis, Peter V. (2017). "Effect of tobacco and electronic cigarette use on cough reflex sensitivity". Pulmonary Pharmacology & Therapeutics. 47: 45–48. doi:10.1016/j.pupt.2017.01.013. ISSN 1094-5539. PMID 28185897.
- ↑ Neuberger, Manfred (2015). "The electronic cigarette: a wolf in sheep's clothing". Wiener Klinische Wochenschrift. 127 (9–10): 385–387. doi:10.1007/s00508-015-0753-3. ISSN 0043-5325. PMID 26230008.
- ↑ 537.0 537.1 Hess, Isabel; Lachireddy, Kishen; Capon, Adam (2016). "A systematic review of the health risks from passive exposure to electronic cigarette vapour". Public Health Research & Practice. 26 (2). doi:10.17061/phrp2621617. ISSN 2204-2091. PMID 27734060.
- ↑ Marynak K; Holmes CB; King BA; Promoff G; Bunnell R; McAfee T (12 December 2014). "State laws prohibiting sales to minors and indoor use of electronic nicotine delivery systems--United States, November 2014". MMWR Morb. Mortal. Wkly. Rep. 63 (49): 1145–1050. PMC 4584536. PMID 25503916.
- ↑ Khan, Mohammad Saud; Khateeb, Faisal; Akhtar, Jamal; Khan, Zubair; Lal, Amos; Kholodovych, Veronika; Hammersley, Jeffrey (2018). "Organizing pneumonia related to electronic cigarette use: A case report and review of literature". The Clinical Respiratory Journal. 12 (3): 1295–1299. doi:10.1111/crj.12775. ISSN 1752-6981. PMID 29392888.
- ↑ Dautzenberg, B.; Adler, M.; Garelik, D.; Loubrieu, J.F.; Mathern, G.; Peiffer, G.; Perriot, J.; Rouquet, R.M.; Schmitt, A.; Underner, M.; Urban, T. (2017). "Practical guidelines on e-cigarettes for practitioners and others health professionals. A French 2016 expert's statement". Revue des Maladies Respiratoires. 34 (2): 155–164. doi:10.1016/j.rmr.2017.01.001. ISSN 0761-8425. PMID 28189437.
- ↑ 541.0 541.1 541.2 Merecz-Sadowska, Anna; Sitarek, Przemyslaw; Zielinska-Blizniewska, Hanna; Malinowska, Katarzyna; Zajdel, Karolina; Zakonnik, Lukasz; Zajdel, Radoslaw (19 January 2020). "A Summary of In Vitro and In Vivo Studies Evaluating the Impact of E-Cigarette Exposure on Living Organisms and the Environment". International Journal of Molecular Sciences. 21 (2): 652. doi:10.3390/ijms21020652. ISSN 1422-0067. PMC 7013895. PMID 31963832.
 This article incorporates text by Anna Merecz-Sadowska, Przemyslaw Sitarek, Hanna Zielinska-Blizniewska, Katarzyna Malinowska, Karolina Zajdel, Lukasz Zakonnik, and Radoslaw Zajdel available under the CC BY 4.0 license.
This article incorporates text by Anna Merecz-Sadowska, Przemyslaw Sitarek, Hanna Zielinska-Blizniewska, Katarzyna Malinowska, Karolina Zajdel, Lukasz Zakonnik, and Radoslaw Zajdel available under the CC BY 4.0 license.
- ↑ "e-Cigarettes: a safe way to quit?". NPS MedicineWise. 11 June 2014. Archived from the original on 19 March 2017.
- ↑ Chapman 2015, p. 1.
- ↑ 544.0 544.1 National Academies of Sciences, Engineering, and Medicine 2018, p. 84, Secondhand Exposure to E-Cigarette Aerosol–Synthesis.
- ↑ Grana RA, Ling PM (2014). ""Smoking revolution": a content analysis of electronic cigarette retail websites". Am J Prev Med. 46 (4): 395–403. doi:10.1016/j.amepre.2013.12.010. PMC 3989286. PMID 24650842.
- ↑ WHO 2016, p. 4.
- ↑ "E-cigarettes not proven quitting aid, says BMA". British Medical Association. 30 January 2013. Archived from the original on 26 February 2013.
- ↑ "Know The Risks: E-Cigarettes & Young People – Aerosol and Other Risks". Surgeon General of the United States. 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ McNeill 2015, p. 65.
- ↑ "E-Cigarettes and Pregnancy". Centers for Disease Control and Prevention. 25 February 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 551.00 551.01 551.02 551.03 551.04 551.05 551.06 551.07 551.08 551.09 551.10 Holbrook, Bradley D. (2016). "The effects of nicotine on human fetal development". Birth Defects Research Part C: Embryo Today: Reviews. 108 (2): 181–192. doi:10.1002/bdrc.21128. ISSN 1542-975X. PMID 27297020.
- ↑ Ramlal, Meera; Van der Meer, Renske; Bendien, Sarah (March 2024). "Treatable Traits in Pregnant Women with Asthma". Respiration. 103 (4): 217–232. doi:10.1159/000536455. PMC 10997272. PMID 38471469.
{{cite journal}}: Check|pmc=value (help) - ↑ Breland, Alison; McCubbin, Andrea; Ashford, Kristin (2019). "Electronic nicotine delivery systems and pregnancy: Recent research on perceptions, cessation, and toxicant delivery". Birth Defects Research. 111 (17): 1284–1293. doi:10.1002/bdr2.1561. ISSN 2472-1727. PMC 7121906. PMID 31364280.
- ↑ "Electronic Nicotine Delivery Systems (ENDS), including E-cigarettes". New Zealand Ministry of Health. 2014. Archived from the original on 2015-05-11.
- ↑ Kaur, J.; Rinkoo, A. V. (2014). "A call for an urgent ban on E-cigarettes in India--a race against time". Global Health Promotion. 22 (2): 71–74. doi:10.1177/1757975914537322. ISSN 1757-9759. PMID 24938513.
- ↑ 556.0 556.1 556.2 Cool, Taylor; Baena, Alessandra Rodriguez y; Forsberg, E. Camilla (30 December 2021). "Clearing the Haze: How Does Nicotine Affect Hematopoiesis before and after Birth?". Cancers. 14 (1): 184. doi:10.3390/cancers14010184. PMC 8750289. PMID 35008347.
 This article incorporates text by Taylor Cool, Alessandra Rodriguez y Baena, and E. Camilla Forsberg available under the CC BY 4.0 license.
This article incorporates text by Taylor Cool, Alessandra Rodriguez y Baena, and E. Camilla Forsberg available under the CC BY 4.0 license.
- ↑ Suter, Melissa A.; Mastrobattista, Joan; Sachs, Maike; Aagaard, Kjersti (2015). "Is There Evidence for Potential Harm of Electronic Cigarette Use in Pregnancy?". Birth Defects Research Part A: Clinical and Molecular Teratology. 103 (3): 186–195. doi:10.1002/bdra.23333. ISSN 1542-0752. PMC 4830434. PMID 25366492.
- ↑ National Academies of Sciences, Engineering, and Medicine 2018, p. 18–19, Summary.
- ↑ McGrath-Morrow, Sharon A.; Gorzkowski, Julie; Groner, Judith A.; Rule, Ana M.; Wilson, Karen; Tanski, Susanne E.; Collaco, Joseph M.; Klein, Jonathan D. (1 March 2020). "The Effects of Nicotine on Development". Pediatrics. 145 (3): e20191346. doi:10.1542/peds.2019-1346. PMC 7049940. PMID 32047098.
- ↑ Siu, AL (22 September 2015). "Behavioral and Pharmacotherapy Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Women: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 163 (8): 622–34. doi:10.7326/M15-2023. PMID 26389730.
- ↑ 561.0 561.1 "E-cigarettes (Vaping)". Mother To Baby | Fact Sheets. Organization of Teratology Information Specialists (OTIS). 1 October 2021. PMID 35951787.
- ↑ 562.0 562.1 562.2 Addo Ntim, Susana; Martin, Bria; Termeh-Zonoozi, Yasmin (20 October 2022). "Review of Use Prevalence, Susceptibility, Advertisement Exposure, and Access to Electronic Nicotine Delivery Systems among Minorities and Low-Income Populations in the United States". International Journal of Environmental Research and Public Health. 19 (20): 13585. doi:10.3390/ijerph192013585. PMC 9603140. PMID 36294164.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Susana Addo Ntim, Bria Martin, and Yasmin Termeh-Zonoozi available under the CC BY 4.0 license.
This article incorporates text by Susana Addo Ntim, Bria Martin, and Yasmin Termeh-Zonoozi available under the CC BY 4.0 license.
- ↑ Mock, Jeremiah (2019). "Notes from the Field: Environmental Contamination from E-cigarette, Cigarette, Cigar, and Cannabis Products at 12 High Schools — San Francisco Bay Area, 2018–2019". MMWR Morb Mortal Wkly Rep. 68 (40): 897–899. doi:10.15585/mmwr.mm6840a4. PMC 6788397. PMID 31600185.
- ↑ Zhang, Zeling; Mei, Xiaotong; He, Ziliang; Xie, Xiya; Yang, Yang; Mei, Chengyu; Xue, Dong; Hu, Tong; Shu, Ming; Zhong, Weihong (February 2022). "Nicotine metabolism pathway in bacteria: mechanism, modification, and application". Applied Microbiology and Biotechnology. 106 (3): 889–904. doi:10.1007/s00253-022-11763-y. PMID 35072735.
- ↑ 565.00 565.01 565.02 565.03 565.04 565.05 565.06 565.07 565.08 565.09 565.10 565.11 565.12 565.13 565.14 565.15 565.16 565.17 565.18 565.19 565.20 565.21 565.22 Hendlin, Yogi Hale; Bialous, Stella A. (January 2020). "The environmental externalities of tobacco manufacturing: A review of tobacco industry reporting". Ambio. 49 (1): 17–34. doi:10.1007/s13280-019-01148-3. PMC 6889105. PMID 30852780.
 This article incorporates text by Yogi Hale and Stella A. Bialous available under the CC BY 4.0 license.
This article incorporates text by Yogi Hale and Stella A. Bialous available under the CC BY 4.0 license.
- ↑ 566.0 566.1 566.2 Brian Clark Howard (11 April 2012). "Cigarettes vs. e-Cigarettes: Which Is Less Environmentally Harmful?". National Geographic. Archived from the original on 24 March 2015.
- ↑ Novotny, T. E.; Zhao, F. (1 March 1999). "Consumption and production waste: another externality of tobacco use". Tobacco Control. 8 (1): 75–80. doi:10.1136/tc.8.1.75. PMC 1763907. PMID 10465821.
- ↑ 568.0 568.1 568.2 568.3 568.4 568.5 568.6 568.7 568.8 "Tips for Safe Disposal of E-Cigarettes and E-Liquid Waste". United States Food and Drug Administration. 23 August 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Vaping liquids, e-cigarettes, and other nicotine wastes" (PDF). Minnesota Pollution Control Agency. November 2022.
- ↑ Bullen, Christopher (November 2014). "Electronic Cigarettes for Smoking Cessation". Current Cardiology Reports. 16 (11): 538. doi:10.1007/s11886-014-0538-8. PMID 25303892.
- ↑ 571.0 571.1 Ling, Pamela M.; Kim, Minji; Egbe, Catherine O.; Patanavanich, Roengrudee; Pinho, Mariana; Hendlin, Yogi (1 March 2022). "Moving targets: how the rapidly changing tobacco and nicotine landscape creates advertising and promotion policy challenges". Tobacco Control. 31 (2): 222–228. doi:10.1136/tobaccocontrol-2021-056552. PMID 35241592.
- ↑ 572.0 572.1 572.2 Raj, A. Thirumal; Sujatha, Govindarajan; Muruganandhan, Jayanandan; Kumar, S. Satish; Bharkavi, SK Indu; Varadarajan, Saranya; Patil, Shankargouda; Awan, Kamran Habib (April 2020). "Reviewing the oral carcinogenic potential of E-cigarettes using the Bradford Hill criteria of causation". Translational Cancer Research. 9 (4): 3142–3152. doi:10.21037/tcr.2020.01.23. PMC 8798817. PMID 35117678.
- ↑ 573.0 573.1 573.2 573.3 Hilts, Philip J. (15 April 1994). "Tobacco Chiefs Say Cigarettes Aren't Addictive". The New York Times.
- ↑ Hilts, Philip J. (17 April 1994). "April 10-16: Smoke at the Capital; Tobacco Executives Testify for Cigarettes". The New York Times.
- ↑ Almeida-da-Silva, Cássio Luiz Coutinho; Matshik Dakafay, Harmony; O'Brien, Kenji; Montierth, Dallin; Xiao, Nan; Ojcius, David M. (June 2021). "Effects of electronic cigarette aerosol exposure on oral and systemic health". Biomedical Journal. 44 (3): 252–259. doi:10.1016/j.bj.2020.07.003. PMID 33039378.
- ↑ 576.0 576.1 576.2 576.3 576.4 576.5 McCausland, Kahlia; Maycock, Bruce; Leaver, Tama; Jancey, Jonine (2019). "The Messages Presented in Electronic Cigarette–Related Social Media Promotions and Discussion: Scoping Review". Journal of Medical Internet Research. 21 (2): e11953. doi:10.2196/11953. ISSN 1438-8871. PMC 6379814. PMID 30720440.
 This article incorporates text by Kahlia McCausland, Bruce Maycock, Tama Leaver, and Jonine Jancey available under the CC BY 4.0 license.
This article incorporates text by Kahlia McCausland, Bruce Maycock, Tama Leaver, and Jonine Jancey available under the CC BY 4.0 license.
- ↑ 577.0 577.1 Daiber, Andreas; Kuntic, Marin; Oelze, Matthias; Hahad, Omar; Münzel, Thomas (July 2023). "E-cigarette effects on vascular function in animals and humans". Pflügers Archiv - European Journal of Physiology. 475 (7): 783–796. doi:10.1007/s00424-023-02813-z. PMC 10264525. PMID 37084087.
{{cite journal}}: Check|pmc=value (help) - ↑ 578.0 578.1 578.2 578.3 578.4 578.5 Sircar, Neil; Fleming, Mary E.; Bialous, Stella A. (26 October 2022). "Does a human rights-based approach to harm reduction support commercialized harm reduction? Brief research". Frontiers in Public Health. 10: 1001036. doi:10.3389/fpubh.2022.1001036. PMID 36388311.
 This article incorporates text by Neil Sircar, Mary E. Fleming, and Stella A. Bialous available under the CC BY 4.0 license.
This article incorporates text by Neil Sircar, Mary E. Fleming, and Stella A. Bialous available under the CC BY 4.0 license.
- ↑ 579.0 579.1 "FDA Warns of Health Risks Posed by E-Cigarettes". United States Food and Drug Administration. 27 September 2017. Archived from the original on 1 November 2017.
- ↑ 580.0 580.1 580.2 "Summary of Results: Laboratory Analysis of Electronic Cigarettes Conducted By FDA". United States Food and Drug Administration. 22 April 2014. Archived from the original on 29 June 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "New Data Show More Than 2.5 Million U.S. Youth Currently Use E-Cigarettes". United States Food and Drug Administration. 6 October 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Gallagher, Kp.; Vargas, Pa.; Santos-Silva, Ar. (January 2024). "The use of E-cigarettes as a risk factor for oral potentially malignant disorders and oral cancer: a rapid review of clinical evidence". Medicina Oral Patología Oral y Cirugia Bucal: e18–e26. doi:10.4317/medoral.26042. PMID 37992145.
- ↑ "WMA Statement on Electronic Cigarettes and Other Electronic Nicotine Delivery Systems". World Medical Association. October 2012.
- ↑ Stone, Emily; Marshall, Henry (2019). "Tobacco and electronic nicotine delivery systems regulation". Translational Lung Cancer Research. 8 (S1): S67–S76. doi:10.21037/tlcr.2019.03.13. ISSN 2218-6751. PMC 6546633. PMID 31211107.
- ↑ Darville, Audrey; Hahn, Ellen J. (2019). "E-cigarettes and Atherosclerotic Cardiovascular Disease: What Clinicians and Researchers Need to Know". Current Atherosclerosis Reports. 21 (5): 15. doi:10.1007/s11883-019-0777-7. ISSN 1523-3804. PMID 30877398. S2CID 80617347.
- ↑ WHO 2016, p. 6.
- ↑ Kaplan, Sheila (5 July 2021). "Juul Is Fighting to Keep Its E-Cigarettes on the U.S. Market". The New York Times. ISSN 0362-4331.
- ↑ 588.0 588.1 Dayen, David (7 July 2021). "Juul: Taking Academic Corruption to a New Level". The American Prospect.
- ↑ 589.0 589.1 589.2 Dayen, David (5 August 2021). "Senators Want Juul Punished for Buying an Academic Journal". The American Prospect.
- ↑ Carroll Chapman, SL; Wu, LT (18 Mar 2014). "E-cigarette prevalence and correlates of use among adolescents versus adults: A review and comparison". Journal of Psychiatric Research. 54: 43–54. doi:10.1016/j.jpsychires.2014.03.005. PMC 4055566. PMID 24680203.
- ↑ Chen, I‐Ling; Todd, Ian; Fairclough, Lucy C. (2019). "Immunological and pathological effects of electronic cigarettes". Basic & Clinical Pharmacology & Toxicology. 125 (3): 237–252. doi:10.1111/bcpt.13225. ISSN 1742-7835. PMID 30861614.
- ↑ Schneider, Sven; Diehl, Katharina (2016). "Vaping as a Catalyst for Smoking? An Initial Model on the Initiation of Electronic Cigarette Use and the Transition to Tobacco Smoking Among Adolescents". Nicotine & Tobacco Research. 18 (5): 647–653. doi:10.1093/ntr/ntv193. ISSN 1462-2203. PMID 26386472.
- ↑ Perikleous, Evanthia P.; Steiropoulos, Paschalis; Paraskakis, Emmanouil; Constantinidis, Theodoros C.; Nena, Evangelia (2018). "E-Cigarette Use Among Adolescents: An Overview of the Literature and Future Perspectives". Frontiers in Public Health. 6: 86. doi:10.3389/fpubh.2018.00086. ISSN 2296-2565. PMC 5879739. PMID 29632856.
 This article incorporates text by Evanthia P. Perikleous, Paschalis Steiropoulos, Emmanouil Paraskakis, Theodoros C. Constantinidis, and Evangelia Nena available under the CC BY 4.0 license.
This article incorporates text by Evanthia P. Perikleous, Paschalis Steiropoulos, Emmanouil Paraskakis, Theodoros C. Constantinidis, and Evangelia Nena available under the CC BY 4.0 license.
- ↑ McNeill 2018, p. 190.
- ↑ McCubbin, Andrea; Fallin-Bennett, Amanda; Barnett, Janine; Ashford, Kristin (2017). "Perceptions and use of electronic cigarettes in pregnancy". Health Education Research. 32 (1): 22–32. doi:10.1093/her/cyw059. ISSN 0268-1153. PMC 5914445. PMID 28158490.
- ↑ McNeill 2018, p. 189.
- ↑ McNeill 2018, p. 20.
- ↑ 598.0 598.1 598.2 "Electronic cigarette use among smokers slows as perceptions of harm increase". ASH UK. 22 May 2015.
- ↑ McNeill 2015, p. 79.
- ↑ McNeill 2015, p. 6, 11, 79-80.
- ↑ Camenga, Deepa R.; Klein, Jonathan D. (2016). "Tobacco Use Disorders". Child and Adolescent Psychiatric Clinics of North America. 25 (3): 445–460. doi:10.1016/j.chc.2016.02.003. ISSN 1056-4993. PMC 4920978. PMID 27338966.
- ↑ Correa, John B.; Ariel, Idan; Menzie, Nicole S.; Brandon, Thomas H. (2017). "Documenting the emergence of electronic nicotine delivery systems as a disruptive technology in nicotine and tobacco science". Addictive Behaviors. 65: 179–184. doi:10.1016/j.addbeh.2016.10.021. ISSN 0306-4603. PMC 5140675. PMID 27816664.
- ↑ McKee, M. (2014). "Electronic cigarettes: peering through the smokescreen". Postgraduate Medical Journal. 90 (1069): 607–609. doi:10.1136/postgradmedj-2014-133029. ISSN 0032-5473. PMID 25294933.
- ↑ 604.0 604.1 de Andrade, M.; Angus, K.; Hastings, G. (2015). "Teenage perceptions of electronic cigarettes in Scottish tobacco-education school interventions: co-production and innovative engagement through a pop-up radio project". Perspectives in Public Health. 136 (5): 288–293. doi:10.1177/1757913915612109. ISSN 1757-9139. PMID 26543156.
- ↑ Tomashefski, Amy (2016). "The perceived effects of electronic cigarettes on health by adult users: A state of the science systematic literature review". Journal of the American Association of Nurse Practitioners. 28 (9): 510–515. doi:10.1002/2327-6924.12358. ISSN 2327-6886. PMID 26997487.
- ↑ McNeill 2018, p. 188.
- ↑ Wagener, Theodore L.; Meier, Ellen; Tackett, Alayna P.; Matheny, James D.; Pechacek, Terry F. (2016). "A Proposed Collaboration Against Big Tobacco: Common Ground Between the Vaping and Public Health Community in the United States". Nicotine & Tobacco Research. 18 (5): 730–736. doi:10.1093/ntr/ntv241. ISSN 1462-2203. PMC 6959509. PMID 26508399.
- ↑ Collins, Lauren; Glasser, Allison M; Abudayyeh, Haneen; Pearson, Jennifer L; Villanti, Andrea C (2018). "E-Cigarette Marketing and Communication: How E-Cigarette Companies Market E-Cigarettes and the Public Engages with E-cigarette Information". Nicotine & Tobacco Research. 21 (1): 14–24. doi:10.1093/ntr/ntx284. ISSN 1462-2203. PMC 6610165. PMID 29315420.



