User:QuackGuru/Sand 24
https://pubmed.ncbi.nlm.nih.gov/33251101/ The perfect storm: A case of COVID-19 infection in an adolescent patient with EVALI
Cited by https://pubmed.ncbi.nlm.nih.gov/35334588/ https://pubmed.ncbi.nlm.nih.gov/35822508/
https://pubmed.ncbi.nlm.nih.gov/36636876/ PMID: 36636876 DOI: 10.1080/15563650.2022.2160342 [1]
https://pubmed.ncbi.nlm.nih.gov/32775191/ E-cigarette or vaping product use associated lung injury, (EVALI) - A diagnosis of exclusion
https://en.wikipedia.org/wiki/Vaping-associated_pulmonary_injury Check recent edits.
https://pubmed.ncbi.nlm.nih.gov/32042584/ Vaping Associated Pulmonary Injury (VAPI) with superimposed Mycoplasma pneumoniae infection primary source cited by: https://pubmed.ncbi.nlm.nih.gov/35573056/ [2]
https://pubmed.ncbi.nlm.nih.gov/35533314/
https://pubmed.ncbi.nlm.nih.gov/32805203/ wait for review
https://en.wikipedia.org/wiki/Wikipedia:WikiProject_Resource_Exchange/Resource_Request
https://web.archive.org/web/20210707222659/https://www.nytimes.com/2021/07/05/health/juul-vaping-fda.html Add link to read full article.
https://pubmed.ncbi.nlm.nih.gov/30284626/ review for heated tobacco product article
https://pubmed.ncbi.nlm.nih.gov/33913154/ Cochrane Database Syst Rev
Unable to open. [3] https://pubmed.ncbi.nlm.nih.gov/33974919/
Unable to open.[4] [4] https://pubmed.ncbi.nlm.nih.gov/34103460/
Unable to open.[5] [5] https://pubmed.ncbi.nlm.nih.gov/33574049/
Unable to open.[6] [6] https://pubmed.ncbi.nlm.nih.gov/34053714/
Unable to open.[7] [7] https://pubmed.ncbi.nlm.nih.gov/34130236/
Unable to open.[8] [8] https://pubmed.ncbi.nlm.nih.gov/33821574/
Unable to open.[9] [9] https://pubmed.ncbi.nlm.nih.gov/33528766/
Unable to open.[10] [10] https://pubmed.ncbi.nlm.nih.gov/33746051/
Unable to open.[11] [11] https://pubmed.ncbi.nlm.nih.gov/31710359/
Unable to open.[12] [12] https://pubmed.ncbi.nlm.nih.gov/33285247/
Unable to open.[13] [13] https://pubmed.ncbi.nlm.nih.gov/33753133/ PMC available on September 1, 2022.
https://en.wikipedia.org/wiki/Vitamin_E#Vaping-associated_lung_injury Needs checking.
https://en.wikipedia.org/wiki/%CE%91-Tocopheryl_acetate#Ingredient_in_vape_liquids Needs checking.
https://en.wikipedia.org/w/index.php?title=Vaping-associated_pulmonary_injury&oldid=1033851213 07:21, 16 July 2021
| QuackGuru/Sand 24 | |
|---|---|
| Other names: Vaping-associated lung injury (VALI),[14] e-cigarette, or vaping, product use associated lung injury (EVALI)[15] | |
 | |
| CT scan of the chest showing diffuse lung infiltrates found in three cases of vaping-associated pulmonary injury.[16] | |
| Specialty | Pulmonology,[15] Intensive care medicine[15] |
| Symptoms | Shortness of breath,[17] hypoxia,[17] fever,[17] cough,[17] diarrhea[17] |
| Causes | Possibly, multiple chemicals are responsible for causing the vaping-induced lung injury cases.[18] Most cases are likely associated with vaping vitamin E acetate.[19] Nicotine e-cigarette use has been linked to the vaping-induced lung injury cases in a small subset of users.[20] |
| Diagnostic method | Chest X-ray,[15] CT scan[16] |
| Treatment | Corticosteroids,[15] Corticosteroids with methylprednisolone[21] Glucocorticoid therapy[19] Oxygen therapy[17] Mechanical ventilation[19] Intubation and mechanical ventilation, with extracorporeal membrane oxygenation (seldom required)[19] |
| Deaths | 68 US;[22] one in Europe[23] (2,807 cases in the US[22] and 20 cases in Canada[24]) |
Vaping-associated pulmonary injury (VAPI)[17] also known as vaping-associated lung injury (VALI)[14] or e-cigarette, or vaping, product use associated lung injury (EVALI),[15] is a lung disease associated with the use of vaping products that can be severe and life-threatening.[22] Symptoms can initially mimic common pulmonary diagnoses like pneumonia, but individuals typically do not respond to antibiotic therapy.[17] High clinical suspicion is necessary to make the diagnosis of VAPI.[17] COVID-19 and VAPI have similar presenting symptoms.[25] Commonly reported symptoms include shortness of breath, cough, fatigue, body aches, fever, nausea, vomiting, and diarrhea.[17] Individuals usually present for care within a few days to weeks of symptom onset.[17] VAPI cases of people with the preexisting conditions asthma, cardiac disease, or being overweight, may be more at risk for lung damage.[26] Cases of VAPI have been underdiagnosed by health care providers.[21]
In September 2019, the US Centers for Disease Control and Prevention (CDC) reported an outbreak of severe lung disease linked to vaping,[27] or the process of inhaling aerosolized substances with battery-operated electronic cigarettes (e-cigarettes),[28] ciga-likes, or vape mods.[29] Cases of a cluster of lung injuries first occurred in April 2019.[30] Case reports of vaping-related lung illnesses were first noted in the literature in 2012.[31] Similar cases of vaping-induced lung injury were reported in the UK and Japan before the outbreak occurred.[29][32] As of February 18, 2020, a total of 2,807 hospitalized cases have been reported to the CDC, with 68 confirmed deaths in the US.[22] Cases peaked in September 2019 and a steady decline followed, with a significant drop from its peak, as of February 2020.[22] As of August 14, 2020, 20 cases of lung injuries in Canada have been reported to the Public Health Agency of Canada.[24] The first uptick in cases had occurred in Utah in 2020 since the decline in 2019.[19]
All CDC-reported cases of VAPI involved a history of using e-cigarette, or vaping, products and most patients reported a history of using a tetrahydrocannabinol (THC)-containing product.[22] Vitamin E acetate has been found in product samples tested by US Food and Drug Administration (FDA).[22] The CDC has stated that the THC cutting agent vitamin E acetate is a very strong culprit of concern in VAPI,[33] but evidence was not sufficient to rule out a contribution from other chemicals of concern, including chemicals in either THC or non-THC products, in some of the reported VAPI cases as of February 2020.[22] Considering that a variety of compounds of vaping devices can induce pulmonary toxicity, it is improbable that there is just one substance that led to the range of patterns of lethal lung damage.[34] Nicotine e-cigarette use has been linked to the VAPI cases in a small subset of users.[20]
The CDC advices patients to discontinue use of e-cigarette, or vaping, products as it should be an integral part of the care approach upon hospital admission and should be re-emphasized during outpatient follow-up.[15] The Public Health Agency of Canada recommends for adults and parents or guardians who are smoking or vaping to contact a health care provider for guidance on ways to stop.[24] Cessation of e-cigarette, or vaping, products might speed recovery from this injury; resuming use of e-cigarette, or vaping, products has the potential to cause recurrence of symptoms or lung injury.[15] Long-term effects and the risk of recurrence of VAPI are not known.[15]
Signs and symptoms
Some people experience detrimental lung and systemic unfavorable effects following vaping.[35] Commonly reported symptoms include shortness of breath, cough, fatigue, body aches, fever, nausea, vomiting, and diarrhea.[17] Additional symptoms may include chest pain, abdominal pain, chills, or weight loss.[36] Symptoms can initially mimic common pulmonary diagnoses like pneumonia, but individuals typically do not respond to antibiotic therapy.[17] In some patients, gastrointestinal symptoms can precede respiratory symptoms.[15] Individuals typically present for care within a few days to weeks of symptom onset.[17] At the time of hospital presentation, the individual is often hypoxic and meets systemic inflammatory response syndrome (SIRS) criteria, including fever.[17] Physical exam can reveal rapid heart rate or rapid breathing.[30] Auscultation of the lungs tends to be unremarkable, even in patients with severe lung disease.[15] In some cases, the affected individuals have progressive respiratory failure, leading to intubation.[17] Several affected individuals have needed to be placed in the intensive care unit (ICU) and on mechanical ventilation.[27] Time to recovery for hospital discharge has ranged from days to weeks.[17]
Among adolescents, the most commonly identified symptoms were nonspecific and included difficulty breathing and cough.[37] This includes one report of hemoptysis and one report of blood-tinged sputum.[37] Constitutional symptoms, including but not limited to, fever, chills, night sweats, fatigue, weakness, malaise, and myalgias were also reported among adolescents.[37] Abdominal symptoms such as nausea and vomiting, abdominal pain or discomfort, and diarrhea were also detected among adolescents.[37] Non-specific chest pain were also identified among adolescents.[37] Tachypnea, oxygen saturation less then 90%, tachycardia, and diminished breathing noises were some of the frequent findings on physical inspection among adolescents.[37] Among adolescents diagnosed with VAPI, asthma was the most commonly identified comorbidity.[37] This could suggest that adolescents with asthma may have a greater likelihood of developing VAPI.[37] Most adolescents recovered and were released from the hospital, with several exhibiting symptom relief and return to usual or close-to-usual lung health after stopping vaping.[37]
Mechanism
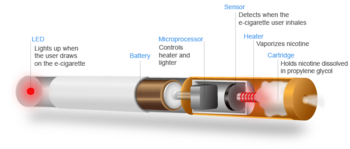
Vaping refers to the practice of inhaling an aerosol from an electronic cigarette device,[17] which works by heating a liquid that can contain various substances, including nicotine, tetrahydrocannabinol (THC), flavoring, and additives (e.g. glycerin, propylene glycol).[29] The long-term health impacts of vaping are unknown.[17] The safety of both nicotine vaping and cannabinoid oils vaping is uncertain.[14]
Most individuals treated for VAPI report vaping the cannabis compounds THC and/or cannabidiol (CBD), and some also report vaping nicotine products.[17] In addition to vaping, some individuals have also experienced VAPI through "dabbing".[17] Dabbing uses a different type of device to heat and extract cannabinoids for inhalation.[17] It is a process that entails superheating and inhaling particles into the lungs that contain THC and other types of cannabidiol plant materials.[38]
E cigarette products and aerosols may contain tobacco-specific nitrosamines, aldehydes, metals, volatile organic compounds, phenolic compounds, polycyclic aromatic hydrocarbons, tobacco alkaloids, flavorings, and drugs.[39] For example, there is substantial evidence showing that propylene glycol, vitamin E acetate, and metals such as lead and arsenic are important components of some e-cigarettes.[39] Propylene glycol and glycerin are typically used as diluents in nicotine-containing e-cigarette products, whereas oils (e.g. medium chain triglycerides) are often used as diluents in THC products.[39]
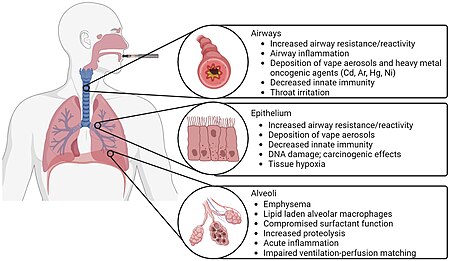
VAPI appears to be a type of acute lung injury, similar to acute fibrinous pneumonitis, organizing pneumonia, or diffuse alveolar damage.[40] VAPI appears to be a general term for various causes of acute lung damage due to vaping.[41] There is no evidence of an infectious etiology causing VAPI.[36]
Chemicals of concern and possible causes
Considering that a variety of compounds of vaping devices can induce pulmonary toxicity, it is improbable that there is just one substance that led to the range of patterns of lethal lung damage.[34] As of April 2020, vitamin E acetate has not been established as the only chemical for causing all the VAPI cases.[34] Evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC or non-THC products, in some of the reported VAPI cases as of February 25 2021.[22] Given that the exclusive use of nicotine-containing products has been reported by a small percentage of persons with VAPI, and that many persons with VAPI report combined use of THC- and nicotine-containing products, the possibility that nicotine-containing products play a role in this outbreak cannot be excluded.[15] In 2019, some people diagnosed with a VAPI reported using only nicotine-containing products.[42] Nicotine e-cigarette use has been linked to the VAPI cases in a small subset of users.[20] Various substances have been under investigation,[22] and there may be more than one cause of the vaping-induced lung injuries.[43] The US Food and Drug Administration (FDA) has not found one product or substance that is involved in all of the cases; however, the agency found that THC is present in most of the samples being tested.[44]
The Centers for Disease Control and Prevention (CDC) stated that the latest national and state findings suggest products containing THC, particularly from informal sources like friends, family, or in-person or online dealers, are linked to most of the cases and play a major role in the outbreak.[22] The CDC has stated that vitamin E acetate is a very strong culprit of concern in VAPI, having been found in 29 out of 29 lung biopsies tested from ten different states.[33] A snapshot of the lab activities conducted by the US FDA included: 843 of the 1,090 samples connected to patients (77%) have undergone some level of testing, as of February 12, 2020.[44] 511 of these samples have been found to contain THC.[44] 50% of the THC products have been found to contain vitamin E acetate as a diluent.[44] The concentration of vitamin E acetate determined in a subset of these samples has ranged from 23% to 88%.[44] 29% of the THC products have been found to contain another diluent such as medium chain triglycerides.[44]
Vitamin E acetate is the synthetic ester of tocopherol and acetate.[45] Previous research suggests that when vitamin E acetate is inhaled, it may interfere with normal lung functioning.[22] Studies into the toxic effects of inhaled vitamin E acetate have shown that this chemical may play a role in inducing inflammation responses in cells.[46] Vitamin E acetate may alter lung surfactant function and cause respiratory impairment.[39] Heating vitamin E acetate may generate ketene, a highly reactive compound that acts as a lung irritant.[39] A 2021 review states, "One possible mechanism for VEA-mediated lung toxicity is that, since vitamin E is a natural component of lung surfactant, increasing levels of VEA in the lungs may alter the properties of a person’s lung surfactant leading to pulmonary injury and toxicity."[47] The aerosolization of vitamin E acetate generates ketene, that is irritant to airways and disrupts phospholipid bilayer decreasing surfactant effectiveness.[48]
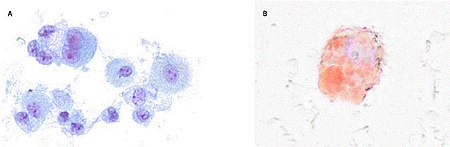
Mice exposed to aerosols generated from vitamin E acetate have demonstrated elevated levels of bronchoalveolar lavage lipid-laden macrophages on Oil-Red-O stain, which is in keeping with the bronchoalveolar lavage findings in people with VAPI.[45] The presence of lipid-laden macrophages led to studies looking at macrophage lipid metabolism.[45] It is possible that increasing concentrations of vitamin E or vitamin E acetate could affect the physical structure and phase behavior of surfactants.[45] This may then impair the ability of the surfactants to maintain alveolar surface tension, leading to respiratory dysfunction.[45] Furthermore, vitamin E acetate forms a toxic compound, ketene, when heated.[45] Ketene is a known lung irritant and thus may also contribute to the chemical pneumonitis seen in people with VAPI.[45] Ketene created from heated vitamin E acetate is a potential cause for the lung damage observed in people with VAPI.[47]
A 2020 study found more 500 chemicals contained in illicit THC vape cartridges that were retrieved from people with VAPI.[47] In contrast to CBD-infused and medical-grade vape cartridges, several of these chemicals were exclusive to illicit THC vape cartridges.[47] These chemicals that were exclusive to illicit THC vape cartridges include decane, 2,2-dimethoxybutane, tetramethyl silicate, siloxanes, methyl and ethyl esters, in addition to vitamin E acetate and other acetates.[47] Additional chemicals have been implicated in some e-cigarette users of cases of VAPI.[46] Some of these include THC, various hydrocarbons, terpenes, pesticides, plasticizers, and assorted metals.[46] Other vaping chemicals, such as medium-chain triglycerides, have also been the subject of study in relation to their possible role in this severe form of lung injury.[46] Other chemicals under investigation as possible causes include limonene, coconut oil,[18] and petroleum distillates.[39] THC can degenerate into methacrolein and benzene.[50]
Flavorings such as vanilla, cinnamon, damascenone, menthol, terpenes, benzyl alcohol, aldehydes, and pyrazines are potentially toxic chemicals that may be one or more of the potential toxicants to blame for causing the vaping-induced lung injuries.[43] Heavy metals such as nickel, lead, chromium, zinc, manganese, and cobalt are potentially toxic chemicals that may be one or more of the potential toxicants to blame for causing the vaping-induced lung injuries.[43]
The solvents propylene glycol and glycerin are potentially toxic chemicals that may be one or more of the potential toxicants to blame for causing the vaping-induced lung injuries.[43] A 2019 review of 17 pathology samples collected from VAPI cases identified no pathologic features of exogenous lipoid pneumonia.[51] Instead, features of airway centric pneumonitis—with bronchiolitis, bronchial wall edema, and mucosal ulceration—in addition to the accumulation of lipid laden macrophages and cytoplasmic vacuolization were found; this was theorized to be the result of exposure to e-liquids containing an exogenous lipid (glycerin) rather than exogenous lipoid pneumonia.[51]
Thermal degradation products, believed to originate from the e-liquid, mainly from propylene glycol and glycerin, include formaldehyde, acetaldehyde, and acrolein, are potentially toxic chemicals that may be one or more of the potential toxicants blamed for causing the vaping-induced lung injuries.[43] Regardless of the limited information available, multiple lung irritants and toxicants are known to be present in the vaping aerosol, which may influence the development of VAPI, such as carbonyls, alkyl alcohols, esters, carboxylic acids, short-chain alkanes, silicon compounds, hydrocarbons, volatile organic compounds, terpenes, reactive oxygen species, and heavy metals, which are known to cause different magnitudes of cytotoxicity, alveolar epithelial harm and lung inflammation, in vivo as well as in vitro.[20] A potential synergistic effect in the development of VAPI may be due to the present of a multitude of toxic chemical mixtures in the emissions of e-cigarettes, resulting from a shortage of regulation on these products.[20]
When aerosolized e-liquids are inhaled, the particles come in direct contact with the entire respiratory system.[49] Consequently, chemicals in e-cigarette aerosols, such as menthol and ethyl maltol may lead to inflammation, which is thought to be the dominant cause or contribution to VAPI.[49] It has also been postulated that the pro-inflammatory effects caused by vape aerosols are partially mediated by reactive oxygen species, which may lead to cellular apoptosis through reactive oxygen species-mediated autophagy; this cellular death pathway is also mechanistically attributed to emphysema.[49] In addition, pulmonary inflammation and fibrosis may result in bronchiolitis obliterans, which is characterized by hypertrophy of the bronchiolar smooth muscle, peribronchiolar inflammatory infiltrates, mucus accumulation in the bronchiolar lumen and bronchiolar scarring.[49] This scarring is irreversible and bronchiolitis obliterans has no known cure.[49] While healthy patients may achieve complete improvement, the pulmonary health of most patients progressively worsens, and some may even require mechanical ventilation or lung transplants in severe cases.[49]
Diagnosis
High clinical suspicion is necessary to make the diagnosis of VAPI.[17] VAPI is considered a diagnosis of exclusion because no specific tests or markers existed for its diagnosis.[15] Health care providers were advised to evaluate for alternative diagnoses (e.g., cardiac, gastrointestinal, rheumatologic, neoplastic, environmental, or occupational exposures, or causes of acute respiratory distress syndrome) as suggested by clinical presentation and medical history, while also considering multiple etiologies, including the possibility of VAPI occurring with a concomitant infection.[15] VAPI cases of people with the preexisting conditions asthma, cardiac disease, or being overweight, may be more at risk for lung damage.[26] Cases of VAPI have been underdiagnosed by health care providers.[21]
All health care providers evaluating patients for VAPI were urged to consider obtaining a thorough patient history, including symptoms and recent use of e-cigarette, or vaping, products, along with substances used, duration and frequency of use, and method of use.[15] Additionally a detailed physical examination was recommended, specifically including vital signs and pulse-oximetry.[15] Laboratory testing guided by clinical findings, which might include a respiratory virus panel to rule out infectious diseases, complete blood count with differential, serum inflammatory markers (C-reactive protein [CRP], erythrocyte sedimentation rate [ESR]), liver transaminases, and urine toxicology testing, including testing for THC were recommended.[15]
Imaging, typically a chest X-ray, with consideration for a chest CT if chest X-ray results did not correlate with the clinical picture or to evaluate severe or worsening disease were urged.[15] Consulting with specialists (e.g. critical care, pulmonology, medical toxicology, or infectious disease) could help guide further evaluation.[15] The diagnosis is commonly suspected when the person does not respond to antibiotic therapy, and testing does not reveal an alternative diagnosis.[17] Many of the reported cases involved worsening respiratory failure within 48 hours of admission, following the administration of empiric antibiotic therapy.[16] Lung biopsies are not necessary for the diagnosis but are performed as clinically indicated to rule out the likelihood of infection.[38]
There are non-specific laboratory abnormalities that have been reported in association with the disease, including elevations in white blood cell count (with neutrophilic predominance and absence of eosinophilia), transaminases, procalcitonin, and inflammatory markers.[17][16] Infectious disease testing, including blood and sputum cultures and tests for influenza, Mycoplasma, and Legionella were all found to be negative in the majority of reported cases.[16] Imaging abnormalities are typically bilateral and are usually described as "pulmonary infiltrates or opacities" on chest X-ray and "ground-glass opacities" on chest CT.[17]
Bronchoalveolar lavage specimens may exhibit an increased level of neutrophils in combination with lymphocytes and vacuole-laden macrophages.[27] Lavage cytology with oil red O staining demonstrated extensive lipid-laden alveolar macrophages.[16][52] In the few cases in which lung biopsies were performed, the results were consistent with acute lung injury and included a broad range of features, such as acute fibrinous pneumonitis, diffuse alveolar damage, lipid-laden macrophages, and organizing pneumonia.[30][38] Lung biopsies often showed neutrophil predominance as well, with rare eosinophils.[40]
Case definitions
Based on the clinical characteristics of VAPI cases from ongoing federal and state investigations, interim surveillance case definitions for confirmed and probable cases have been developed.[15]
The CDC surveillance case definition for confirmed cases of severe pulmonary disease associated with e-cigarette use:[53]
- Using an e-cigarette ("vaping") or dabbing during the 90 days before symptom onset AND[53]
- Pulmonary infiltrate, such as opacities on plain film chest radiograph or ground-glass opacities on chest computed tomography AND[53]
- Absence of pulmonary infection on initial work-up. Minimum criteria include:[53]
- A negative respiratory viral panel[53]
- A negative influenza polymerase chain reaction or rapid test if local epidemiology supports testing.[53]
- All other clinically indicated respiratory infectious disease testing (e.g., urine antigen for Streptococcus pneumoniae and Legionella, sputum culture if productive cough, bronchoalveolar lavage culture if done, blood culture, human immunodeficiency virus–related opportunistic respiratory infections if appropriate) must be negative AND[53]
- No evidence in medical record of alternative plausible diagnoses (e.g., cardiac, rheumatologic, or neoplastic process).[53]
The CDC surveillance case definition for probable cases of severe pulmonary disease associated with e-cigarette use:[53]
- Using an e-cigarette ("vaping") or dabbing in 90 days before symptom onset AND[53]
- Pulmonary infiltrate, such as opacities on plain film chest radiograph or ground-glass opacities on chest computed tomography AND[53]
- Infection identified via culture or polymerase chain reaction, but clinical team believes this is not the sole cause of the underlying respiratory disease process OR minimum criteria to rule out pulmonary infection not met (testing not performed) and clinical team believes this is not the sole cause of the underlying respiratory disease process AND[53]
- No evidence in medical record of alternative plausible diagnoses (e.g., cardiac, rheumatologic, or neoplastic process).[53]
These surveillance case definitions are meant for public health data collection purposes and are not intended to be used as a clinical diagnostic tool or to guide clinical care; they are subject to change and will be updated as additional information becomes available.[53]
Differential diagnosis
As VAPI is a diagnosis of exclusion, a variety of respiratory diseases must be ruled out before a diagnosis of VAPI can be made.[15] The differential diagnosis should include more common diagnostic possibilities, such as community-acquired pneumonia, as well as do-not-miss diagnoses, such as pulmonary embolism.[15] Other commonly documented hospital diagnoses for cases of severe pulmonary disease associated with e-cigarette use have included acute respiratory distress syndrome (ARDS), sepsis, acute hypoxic respiratory failure, and pneumonitis.[17]
As of 2019, distinctions were still being made between processes occurring in association with vaping or the use of nicotine-containing liquids and those considered as alternative diagnoses to VAPI.[30] These processes include the following:
- Acute eosinophilic pneumonia has been associated with nicotine vaping.[30]
- COVID-19 and VAPI have similar presenting symptoms[25] such as cough, fever, shortness of breath, and non-specific gastrointestinal complaints.[54] Therefore, a high level of suspicion for VAPI is still recommended during the COVID-19 era since the possible overlap of clinical manifestations between COVID-19 and VAPI may lead to late VAPI diagnosis and treatment.[25]
- Diffuse alveolar hemorrhage has been associated with vaping.[30] Nicotine vaping has also associated with diffuse alveolar hemorrhage.[55]
- Giant cell pneumonitis has been associated with nicotine vaping.[55] Heavy metals-containing nicotine vaping has also associated giant cell pneumonitis that took 6 months to develop.[55]
- Hypersensitivity pneumonitis has been associated with nicotine vaping.[30][55]
- Lipoid pneumonia has been associated with vaping.[30] It has also been associated with nicotine vaping.[55] It has been associated with THC-containing vaping.[52]
- Organizing pneumonia has been associated with THC-containing vaping.[30] It has also been associated with nicotine vaping.[55]
- Pneumonia has been associated with butane hash-containing vaping.[30]
- Respiratory bronchiolitis interstitial lung disease has been associated with nicotine vaping.[30]
- Vaping-induced spontaneous pneumomediastinum is a different ailment that can also cause hospitalization.[56]
The use of imaging and other diagnostic modalities, including chest CT, bronchoscopy with bronchoalveolar lavage, and lung biopsy, may provide additional information to determine the presence of these processes and potentially establish a definitive diagnosis, but are generally not performed unless clinically indicated.[15]
Treatment
Recommendations for primary care
As of October 18, 2019[update], the CDC has published updated interim guidance based on the most current data to provide a framework for health care providers in their management and follow-up of persons with symptoms of VAPI.[15] Initial management involves deciding whether to admit a patient with possible VAPI to the hospital.[15] The CDC recommends that patients with suspected VAPI should be admitted if they have decreased O2 saturation (below 95%) on room air, are in respiratory distress, or have comorbidities that compromise pulmonary reserve.[15]
Once admitted, initiation of corticosteroids should be considered, which have been found to be helpful in treating this injury.[15] Several case reports describe improvement with corticosteroids, likely because of a blunting of the inflammatory response.[15] In a group of patients in Illinois and Wisconsin, 92% of 50 patients received corticosteroids, and those that began glucocorticoid therapy continued on it for at least seven days.[30] Steroids are typically not required for more than two weeks.[21] The medical team documented in 65% of 46 patient notes that "respiratory improvement was due to the use of glucocorticoids".[30] Among 140 cases reported nationally to the CDC that received corticosteroids, 82% of patients improved.[15] In patients with more severe illness, a more aggressive empiric therapy with corticosteroids as well as antimicrobial and antiviral therapy may be warranted.[15] Most patients who had received corticosteroids with methylprednisolone responded well.[21] Some unresponsive patients to steroids need more intense regimens such as extracorporeal membrane oxygenation (ECMO).[21]
As a large proportion of patients were admitted to an intensive care unit based on data submitted to the CDC, many patients require supplemental oxygen via nasal cannula, high-flow oxygen, bilevel positive airway pressure (BiPAP), or mechanical ventilation.[17]
During influenza season, health care providers should consider influenza in all patients with suspected VAPI.[57] Decisions on initiation or discontinuation of treatment should be based on specific clinical features and, when appropriate, in consultation with specialists.[57]
Special consideration should be given to high-risk patients such as the elderly, those with a history of cardiac or lung disease, or pregnant individuals.[15] Patients over 50 years old have an increased risk of intubation and might need longer hospitalizations.[15]
Commonly used treatments among adolescents were steroids, antibiotics, mechanical ventilation, and corticosteroids, with IV methylprednisolone.[37] Among adolescents, mechanical ventilation is frequently needed.[37] ECMO was more widely used among adolescents.[37] Other treatments provided to adolescents included albuterol, ipratropium, analgesic, acetaminophen, lidocaine patches, ketorolac tromethamine, IV opioids, enteral codeine, and gabapentin.[37]
The CDC has stated that patients should be advised to discontinue the use of vaping products upon hospital admission and during outpatient follow-up, to speed recovery and avoid potential recurrence of symptoms or lung injury.[15] Evidence-based tobacco product quitting strategies include behavioral counseling and US FDA-approved cessation medications.[15] Among adolescents, providing information about quitting vaping plays an influential role in reducing risk of relapse of VAPI and improving outcomes.[37] Adolescents who were identified as having spontaneous pneumothorax were at an especially greater risk of relapse of VAPI.[37] It is unclear if quitting vaping lowers this risk.[37]
Follow-up care
Due to reports of relapse during corticosteroid tapers after hospitalization, the CDC recommends scheduling a follow-up visit no later than one to two weeks after discharge from inpatient hospital treatment for VAPI, with considerations for performing pulse-oximetry testing and repeat CXR.[15] In one to two months, health care providers should consider additional follow-up testing, including spirometry, diffusion capacity testing, and another repeat CXR.[15] In patients with persistent hypoxemia (O2 saturation <95%) requiring home oxygen at discharge, consider ongoing pulmonary follow-up.[15] In patients treated with high-dose corticosteroids, consider endocrinology follow-up to monitor adrenal function.[15]
As it is unknown whether patients with a history of VAPI are at increased risk for severe complications with influenza or other respiratory infections, follow-up care should also include annual vaccination against influenza for all persons over 6 months of age, including patients with a history of VAPI, as well as administration of the pneumococcal vaccine according to current guidelines.[15]
An important part of both inpatient and follow-up care for VAPI involves advising patients to discontinue use of e-cigarette or vaping products.[58]
Public health recommendations
The CDC and the US FDA recommend that people not use e-cigarettes or other vaping products that contain THC, particularly products purchased off the street or obtained from informal sources like friends, family, or online sellers.[44] In addition, CDC recommends that individuals not modify or add any substances to e-cigarettes or other vaping products that are not intended by the manufacturer.[15]
The Public Health Agency of Canada recommends for adults and parents or guardians who are smoking or vaping to contact a health care provider for guidance on ways to stop.[24] The Public Health Agency of Canada recommends to lesson one's risk, do not try a vape.[24] The Public Health Agency of Canada recommends for youth, avoiding using a vape.[24] The Public Health Agency of Canada advises that if a person has currently or previously vaped, and shows signs of a cough or breathing difficulty, chest discomfort, or is overall feeling sick, go to a health care provider.[24] The Public Health Agency of Canada advocates for health care providers to talk to patients about their past vaping experiences as part of an assessment of those exhibiting respiratory ailments.[24]
To reduce the risk of recurrence, patients who have been treated for VAPI should not use e-cigarette, or vaping, products.[15] For patients who have addiction to THC-containing or nicotine-containing products, cognitive-behavioral therapy, contingency management, motivational enhancement therapy, and multidimensional family therapy have been shown to help, and consultation with addiction medicine services should be considered.[15]
Health effects
Long-term effects and the risk of recurrence of VAPI are not known.[15] The potential effects of lipid–vapor inhalation in alveolar lipid metabolism are still largely unknown.[59]
Epidemiology
An outbreak of vaping-related lung injuries in 2019 and 2020 affected certain users in the US[22] and Canada.[24] The majority of those affected were young adults aged 18 to 34.[60] As of February 18, 2020, a total of 2,807 hospitalized cases have been reported to the CDC from all 50 states, the District of Columbia, and two US territories (Puerto Rico and US Virgin Islands).[22] Cases peaked in September 2019, and a slow decline followed.[22] As of August 14, 2020, 20 cases of lung injuries in Canada have been reported to the Public Health Agency of Canada.[24] The CDC has received complete gender and age data on these cases with 66% of cases being male.[22] The median age of cases is 24 years and ranges from 13 to 85 years.[22] 76% of cases are under 35 years old.[22] There have been 68 confirmed deaths in the US in 29 states and the District of Columbia from this outbreak ranging from ages 15–75 years old.[22] Fatalities were higher in non-Hispanic whites, those aged 35 years or older, and those with known histories of asthma, cardiac disease or a mental health condition.[61] Just over 50% of fatalities were in men and in obese individuals.[61] 50% of hospitalized cases needed management in the intensive care unit, 20% needed intubation and ventilation, and 2% of hospitalized cases resulted in death.[43]
Of the 2,668 cases reported to the CDC, information on substance use is known for 2,022 cases as of January 14, 2020.[22] 82% reported using THC-containing products; 33% reported exclusive use of THC-containing products.[22] 57% reported using nicotine-containing products; 14% reported exclusive use of nicotine-containing products.[22] Due to the subsequent identification of the primary cause of VAPI, and the considerable decline in VAPI cases and deaths since a peak in September 2019, CDC stopped collecting these data from states as of February 2020.[22]
On September 28, 2019, the first reported case of vaping-associated pulmonary injury was identified in Canada.[62] Chief Public Health Officer of Canada announced on October 11, 2019 that they are aware of the initial cases of vaping-induced lung illness.[63] As of August 14, 2020, 20 cases of lung injuries have been reported to the Public Health Agency of Canada.[24] Reported cases were from Alberta (1), British Columbia (5), New Brunswick (2), Newfoundland and Labrador (1), Ontario (5), and Quebec (6).[24] The majority of cases in Canada involving lung injuries do not seem to have been linked with the use of THC-infused products.[24]
In September 2019, a US Insurance Journal article stated that at least 15 incidents of vaping related illnesses have been reported worldwide prior to 2019, occurring from Guam to Japan to the UK to the US.[64] 12 cases of health problems with nicotine-containing e-cigarettes were reported to the UK's Medicines and Healthcare products Regulatory Agency (MHRA), with at least one case bearing high similarities to the lipoid pneumonia cases reported in the US.[64] One lipoid pneumonia-related death in the UK was associated with e-cigarettes in 2010.[65] Since many of the cases in North America were traced to THC-cartridges as well as the use of e-cigarette vape products, but THC remains illegal in European countries, the disease burden related to vaping has been significantly lower in Europe despite the prevalence of e-cigarette use.[66]
According to case reports since 2012, e-cigarette users with symptoms without direct etiology have undergone various diagnoses, including acute lung injury, atypical pneumonitis, and eosinophilic or lipoid pneumonia.[67] The large spread of cases throughout the US and cases resembling VAPI in other areas of the planet endorse the feasibility that other manifestations of VAPI occurred before this outbreak.[21] Similar cases of vaping-induced lung injury were reported in Japan and the UK before the outbreak occurred.[29][32] This suggests the phenomenon has the possibility of being more pervasive.[29] Between 2018 and 2020, seven people required hospitalization in 5 countries including the UK, Canada, Belgium, Spain, and Germany.[68] The first uptick in cases had occurred in Utah in 2020 since the decline in 2019.[19]
Other names
Vaping-associated pulmonary injury (VAPI)[17] is also variously known as vaping associated pulmonary injury (VAPI),[69] vaping-associated lung injury (VALI),[14] vaping product use-associated lung injury (VALI),[70] electronic vaping-associated lung injury (EVALI),[71] vaping-associated injury,[72] e-cigarette, or vaping, product use associated lung injury (EVALI),[15] e-cigarette or vaping associated lung injury (EVALI),[48] EC vaping associated lung injury (EVALI),[54] E-cigarette (e-cig), or Vaping product use, associated Acute Lung Injury,[20] e-cigarette– or vaping-associated acute lung injury (EVALI),[73] e-cigarette and vaping acute lung disease (EVALD),[74] electronic cigarette-induced acute lung injury,[75] e-cigarette–induced lung injury,[76] vaping-related acute lung injury (VpALI),[13] vaping-associated lung disease,[55] vaping-associated lung illness,[77] vaping associated lung injury (vpali),[69] vaping-induced lung injury,[78] vaping-induced pulmonary disease,[79] vaping use-associated lung injury,[80] vaping product-associated lung injury,[21] vaping associated respiratory syndrome,[29] vape-related lung disease,[81] vape-related lung illness,[82] vaping related lung injury,[50] vape-related pulmonary illness,[83] vaporizer-linked respiratory failure,[84] vaping-linked lung illness,[85] or vape lung.[86]
References
- ↑ Sund, Lachlan J.; Dargan, Paul I.; Archer, John R. H.; Wood, David M. (February 1, 2023). "E-cigarette or vaping-associated lung injury (EVALI): a review of international case reports from outside the United States of America". Clinical Toxicology. 61 (2): 91–97. doi:10.1080/15563650.2022.2160342. PMID 36636876.
- ↑ Harrell, Melissa B.; Clendennen, Stephanie L.; Sumbe, Aslesha; Case, Kathleen R.; Mantey, Dale S.; Swan, Sunaina (May 7, 2022). "Cannabis Vaping Among Youth and Young Adults: a Scoping Review". Current Addiction Reports. 9 (3): 217–234. doi:10.1007/s40429-022-00413-y. PMC 9078633. PMID 35573056.
 This article incorporates text by Melissa B. Harrell, Stephanie L. Clendennen, Aslesha Sumbe, Kathleen R. Case, Dale S. Mantey, and Sunaina Swan available under the CC BY 4.0 license.
This article incorporates text by Melissa B. Harrell, Stephanie L. Clendennen, Aslesha Sumbe, Kathleen R. Case, Dale S. Mantey, and Sunaina Swan available under the CC BY 4.0 license.
- ↑ Dekhou, Antonio; Oska, Nicole; Partiali, Benjamin; Johnson, Jared; Chung, Michael T.; Folbe, Adam (2021). "E-Cigarette Burns and Explosions: What are the Patterns of Oromaxillofacial Injury?". Journal of Oral and Maxillofacial Surgery. doi:10.1016/j.joms.2021.03.008. ISSN 0278-2391. PMID 33974919.
- ↑ 4.0 4.1 Petrella, Francesco (2021). "Electronic cigarettes, vaping-related lung injury and lung cancer: where do we stand?". European Journal of Cancer Prevention. 30 (4): 293–296. doi:10.1097/CEJ.0000000000000630. ISSN 0959-8278. PMID 34103460.
- ↑ 5.0 5.1 Shahandeh, Negeen; Chowdhary, Harshika; Middlekauff, Holly R (2021). "Vaping and cardiac disease". Heart: heartjnl-2020-318150. doi:10.1136/heartjnl-2020-318150. ISSN 1355-6037. PMID 33574049.
- ↑ 6.0 6.1 Schwarz, Evan S. (2021). "Inhalants". Critical Care Clinics. 37 (3): 687–702. doi:10.1016/j.ccc.2021.03.014. ISSN 0749-0704. PMID 34053714.
- ↑ 7.0 7.1 Sreedharan, Subhashaan; Mian, Mustafa; Robertson, Ross A.; Rhodes, Alexander (2021). "Radiological findings of e-cigarette or vaping product use associated lung injury: A systematic review". Heart & Lung. 50 (5): 736–741. doi:10.1016/j.hrtlng.2021.05.004. ISSN 0147-9563. PMID 34130236.
- ↑ 8.0 8.1 Kaslow, Jacob A.; Rosas‐Salazar, Christian; Moore, Paul E. (2021). "E‐cigarette and vaping product use‐associated lung injury in the pediatric population: A critical review of the current literature". Pediatric Pulmonology. 56 (7): 1857–1867. doi:10.1002/ppul.25384. ISSN 8755-6863. PMID 33821574.
- ↑ 9.0 9.1 Feldman, Ryan; Stanton, Matthew; Suelzer, Elizabeth M. (2021). "Compiling Evidence for EVALI: A Scoping Review of In Vivo Pulmonary Effects After Inhaling Vitamin E or Vitamin E Acetate". Journal of Medical Toxicology. 17 (3): 278–288. doi:10.1007/s13181-021-00823-w. ISSN 1556-9039. PMID 33528766.
- ↑ 10.0 10.1 Stefaniak, Aleksandr B.; LeBouf, Ryan F.; Ranpara, Anand C.; Leonard, Stephen S. (2021). "Toxicology of flavoring- and cannabis-containing e-liquids used in electronic delivery systems". Pharmacology & Therapeutics. 224: 107838. doi:10.1016/j.pharmthera.2021.107838. ISSN 0163-7258. PMID 33746051.
- ↑ 11.0 11.1 Khan, Leah (2019). "Substance Use in Adolescents: Latest Trends". Pediatric Annals. 48 (11). doi:10.3928/19382359-20191018-02. ISSN 0090-4481. PMID 31710359.
- ↑ 12.0 12.1 Spahn, Jamie E.; Stavchansky, Salomon A.; Cui, Zhengrong (2021). "Critical research gaps in electronic cigarette devices and nicotine aerosols". International Journal of Pharmaceutics. 593: 120144. doi:10.1016/j.ijpharm.2020.120144. ISSN 0378-5173. PMID 33285247.
- ↑ 13.0 13.1 13.2 Bonner, Emily; Chang, Yvonne; Christie, Emerson; Colvin, Victoria; Cunningham, Brittany; Elson, Daniel; Ghetu, Christine; Huizenga, Juliana; Hutton, Sara J.; Kolluri, Siva K.; Maggio, Stephanie; Moran, Ian; Parker, Bethany; Rericha, Yvonne; Rivera, Brianna N.; Samon, Samantha; Schwichtenberg, Trever; Shankar, Prarthana; Simonich, Michael T.; Wilson, Lindsay B.; Tanguay, Robyn L. (September 2021). "The chemistry and toxicology of vaping". Pharmacology & Therapeutics. 225: 107837. doi:10.1016/j.pharmthera.2021.107837. ISSN 0163-7258. PMC 8263470. PMID 33753133.
- ↑ 14.0 14.1 14.2 14.3 Xantus, Gabor Zoltan (2020). "Vaping-associated lung injury—VALI facts, assumptions and opportunities: review of the present situation". Postgraduate Medical Journal. 96 (1132): 61–63. doi:10.1136/postgradmedj-2019-137185. ISSN 0032-5473. PMID 31767670.
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 15.12 15.13 15.14 15.15 15.16 15.17 15.18 15.19 15.20 15.21 15.22 15.23 15.24 15.25 15.26 15.27 15.28 15.29 15.30 15.31 15.32 15.33 15.34 15.35 15.36 15.37 15.38 15.39 15.40 15.41 15.42 15.43 Siegel, David A.; Jatlaoui, Tara C.; Koumans, Emily H.; Kiernan, Emily A.; Layer, Mark; Cates, Jordan E.; et al. (October 2019). "Update: Interim Guidance for Health Care Providers Evaluating and Caring for Patients with Suspected E-cigarette, or Vaping, Product Use Associated Lung Injury — United States, October 2019". Morbidity and Mortality Weekly Report (MMWR). 68 (41): 919–927. doi:10.15585/mmwr.mm6841e3. ISSN 0149-2195. PMC 6802682. PMID 31633675.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 Davidson, Kevin; Brancato, Alison; Heetderks, Peter; Mansour, Wissam; Matheis, Edward; Nario, Myra; Rajagopalan, Shrinivas; Underhill, Bailey; Wininger, Jeremy; Fox, Daniel (September 13, 2019). "Outbreak of Electronic-Cigarette–Associated Acute Lipoid Pneumonia — North Carolina, July–August 2019". Morbidity and Mortality Weekly Report (MMWR). 68 (36): 784–786. doi:10.15585/mmwr.mm6836e1. ISSN 0149-2195. PMC 6755817. PMID 31513559.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 17.00 17.01 17.02 17.03 17.04 17.05 17.06 17.07 17.08 17.09 17.10 17.11 17.12 17.13 17.14 17.15 17.16 17.17 17.18 17.19 17.20 17.21 17.22 17.23 17.24 17.25 17.26 17.27 17.28 CDPH Health Alert: Vaping-Associated Pulmonary Injury (PDF). California Tobacco Control Program (Report). California Department of Public Health. August 28, 2019. pp. 1–5.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 18.0 18.1 Feldman, Ryan; Meiman, Jonathan; Stanton, Matthew; Gummin, David D. (June 2020). "Culprit or correlate? An application of the Bradford Hill criteria to Vitamin E acetate". Archives of Toxicology. 94 (6): 2249–2254. doi:10.1007/s00204-020-02770-x. ISSN 0340-5761. PMID 32451600.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 Smith, Maxwell L.; Gotway, Michael B.; Crotty Alexander, Laura E.; Hariri, Lida P. (2020). "Vaping-related lung injury". Virchows Archiv. 478 (1): 81–88. doi:10.1007/s00428-020-02943-0. ISSN 0945-6317. PMC 7590536. PMID 33106908.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 Marrocco, Antonella; Singh, Dilpreet; Christiani, David C.; Demokritou, Philip (March 16, 2022). "E-cigarette vaping associated acute lung injury (EVALI): state of science and future research needs". Critical Reviews in Toxicology. 52 (3): 188–220. doi:10.1080/10408444.2022.2082918. PMC 9716650. PMID 35822508.
{{cite journal}}: Check|pmc=value (help) - ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 21.7 Cherian, Sujith V.; Kumar, Anupam; Estrada-Y-Martin, Rosa M. (2020). "E-Cigarette or Vaping Product-Associated Lung Injury: A Review". The American Journal of Medicine. 133 (6): 657–663. doi:10.1016/j.amjmed.2020.02.004. ISSN 0002-9343. PMID 32179055.
- ↑ 22.00 22.01 22.02 22.03 22.04 22.05 22.06 22.07 22.08 22.09 22.10 22.11 22.12 22.13 22.14 22.15 22.16 22.17 22.18 22.19 22.20 22.21 22.22 "Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products". Centers for Disease Control and Prevention. February 25, 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Zulfiqar, Hassam; Rahman, Omar (March 14, 2021). Vaping Associated Pulmonary Injury. StatPearls Publishing. PMID 32809491.
- ↑ 24.00 24.01 24.02 24.03 24.04 24.05 24.06 24.07 24.08 24.09 24.10 24.11 24.12 "Vaping-associated lung illness". Public Health Agency of Canada. August 20, 2020.
- ↑ 25.0 25.1 25.2 Schiliro, Marta; Vogel, Elizabeth R.; Paolini, Lucia; Pabelick, Christina M. (2021). "Cigarette Smoke Exposure, Pediatric Lung Disease, and COVID-19". Frontiers in Physiology. 12. doi:10.3389/fphys.2021.652198. ISSN 1664-042X. PMC 8110920. PMID 33986692.
 This article incorporates text by Marta Schiliro, Elizabeth R. Vogel, Lucia Paolini, and Christina M. Pabelick1 available under the CC BY 4.0 license.
This article incorporates text by Marta Schiliro, Elizabeth R. Vogel, Lucia Paolini, and Christina M. Pabelick1 available under the CC BY 4.0 license.
- ↑ 26.0 26.1 Keith, Rachel; Bhatnagar, Aruni (June 2021). "Cardiorespiratory and Immunologic Effects of Electronic Cigarettes". Current Addiction Reports. 8 (2): 336–346. doi:10.1007/s40429-021-00359-7. PMC 7935224. PMID 33717828.
- ↑ 27.0 27.1 27.2 Carlos, W. Graham; Crotty Alexander, Laura E; Gross, Jane E; Dela Cruz, Charles S; Keller, Jonathan M; Pasnick, Susan; Jamil, Shazia (October 2019). "Vaping Associated Pulmonary Illness (VAPI)". American Journal of Respiratory and Critical Care Medicine. 200 (7): P13–P14. doi:10.1164/rccm.2007P13. ISSN 1073-449X. PMID 31532695.
- ↑ Triantafyllou, Georgios A.; Tiberio, Perry J.; Zou, Richard H.; Lamberty, Phillip E.; Lynch, Michael J.; Kreit, John W.; Gladwin, Mark T.; Morris, Alison; Chiarchiaro, Jared (October 2019). "Vaping-Associated Acute Lung Injury: A Case Series". American Journal of Respiratory and Critical Care Medicine. 200 (11): 1430–1431. doi:10.1164/rccm.201909-1809LE. ISSN 1535-4970. PMID 31574235.
- ↑ 29.0 29.1 29.2 29.3 29.4 29.5 Gotts, Jeffrey E; Jordt, Sven-Eric; McConnell, Rob; Tarran, Robert (2019). "What are the respiratory effects of e-cigarettes?". BMJ. 366: l5275. doi:10.1136/bmj.l5275. ISSN 0959-8138. PMID 31570493.
- ↑ 30.00 30.01 30.02 30.03 30.04 30.05 30.06 30.07 30.08 30.09 30.10 30.11 30.12 Layden, Jennifer E.; Ghinai, Isaac; Pray, Ian; et al. (March 5, 2020). "Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin — Final Report". New England Journal of Medicine. doi:10.1056/NEJMoa1911614. ISSN 0028-4793. PMID 31491072.
- ↑ Jonas, Andrea M.; Raj, Rishi (October 2020). "Vaping-Related Acute Parenchymal Lung Injury". Chest. 158 (4): 1555–1565. doi:10.1016/j.chest.2020.03.085. PMID 32442559. S2CID 218857503.
- ↑ 32.0 32.1 Schupp, J. C.; Prasse, A.; Erythropel, H. C. (February 2020). "E-Zigaretten – Funktionsweise, Inhaltsstoffe und die Vaping-assoziierte akute Lungenschädigung" [E-Cigarettes - Operating Principle, Ingredients, and Associated Acute Lung Injury]. Pneumologie (in Deutsch). 74 (02): 77–87. doi:10.1055/a-1078-8126. ISSN 0934-8387. PMC 7366312. PMID 32016924.
- ↑ 33.0 33.1 33.2 33.3 "Transcript of CDC Telebriefing: Update on Lung Injury Associated with E-cigarette Use, or Vaping". Centers for Disease Control and Prevention (CDC). November 8, 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 34.0 34.1 34.2 Casey, AM; Muise, ED; Crotty Alexander, LE (2020). "Vaping and e-cigarette use. Mysterious lung manifestations and an epidemic". Current opinion in immunology. 66: 143–150. doi:10.1016/j.coi.2020.10.003. ISSN 0952-7915. PMC 7755270. PMID 33186869.
- ↑ Hage, R.; Fretz, V.; Schuurmans, M.M. (September 2020). "Electronic cigarettes and vaping associated pulmonary illness (VAPI): A narrative review". Pulmonology. 26 (5): 291–303. doi:10.1016/j.pulmoe.2020.02.009.
- ↑ 36.0 36.1 "Frequently Asked Questions". Centers for Disease Control and Prevention. December 1, 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 37.00 37.01 37.02 37.03 37.04 37.05 37.06 37.07 37.08 37.09 37.10 37.11 37.12 37.13 37.14 37.15 Gonsalves, Clarelle L.; Zhu, Jie Wei; Kam, April J. (January 2021). "Diagnosis and Acute Management of E-Cigarette or Vaping Product Use–Associated Lung Injury in the Pediatric Population: A Systematic Review". The Journal of Pediatrics. 228: 260–270. doi:10.1016/j.jpeds.2020.09.040.
- ↑ 38.0 38.1 38.2 Mukhopadhyay, Sanjay; Mehrad, Mitra; Dammert, Pedro; Arrossi, Andrea V; Sarda, Rakesh; Brenner, David S; Maldonado, Fabien; Choi, Humberto; Ghobrial, Michael (October 2019). "Lung Biopsy Findings in Severe Pulmonary Illness Associated With E-Cigarette Use (Vaping): A Report of Eight Cases". American Journal of Clinical Pathology. 153 (1): 30–39. doi:10.1093/ajcp/aqz182. ISSN 0002-9173. PMID 31621873.
- ↑ 39.0 39.1 39.2 39.3 39.4 39.5 Belok, Samuel H.; Parikh, Raj; Bernardo, John; Kathuria, Hasmeena (2020). "E-cigarette, or vaping, product use-associated lung injury: a review". Pneumonia. 12 (1). doi:10.1186/s41479-020-00075-2. ISSN 2200-6133. PMC 7585559. PMID 33110741.
 This article incorporates text by Samuel H Belok, Raj Parikh, John Bernardo, and Hasmeena Kathuria available under the CC BY 4.0 license.
This article incorporates text by Samuel H Belok, Raj Parikh, John Bernardo, and Hasmeena Kathuria available under the CC BY 4.0 license.
- ↑ 40.0 40.1 Butt, Yasmeen M.; Smith, Maxwell L.; Tazelaar, Henry D.; Vaszar, Laszlo T.; Swanson, Karen L.; Cecchini, Matthew J.; Boland, Jennifer M.; Bois, Melanie C.; Boyum, James H.; Froemming, Adam T.; Khoor, Andras; Mira-Avendano, Isabel; Patel, Aiyub; Larsen, Brandon T. (October 2019). "Pathology of Vaping-Associated Lung Injury". The New England Journal of Medicine. 381 (18): 1780–1781. doi:10.1056/NEJMc1913069. ISSN 0028-4793. PMID 31577870.
- ↑ Boland, Jennifer M; Aesif, Scott W (October 2019). "Vaping-Associated Lung Injury". American Journal of Clinical Pathology. 153 (1): 1–2. doi:10.1093/ajcp/aqz191. ISSN 0002-9173. PMID 31651033.
- ↑ Ghinai, Isaac; Navon, Livia; Gunn, Jayleen K.L.; Duca, Lindsey M.; Brister, Sarah; Love, Sarah; Brink, Rachel; Fajardo, Geroncio; Johnson, Jona; Saathoff-Huber, Lori; King, Brian A.; Jones, Christopher M.; Krishnasamy, Vikram P.; Layden, Jennifer E. (January 24, 2020). "Characteristics of Persons Who Report Using Only Nicotine-Containing Products Among Interviewed Patients with E-cigarette, or Vaping, Product Use–Associated Lung Injury — Illinois, August–December 2019". MMWR. Morbidity and Mortality Weekly Report. 69 (3): 84–89. doi:10.15585/mmwr.mm6903e1. PMC 7367041. PMID 31971930.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 43.0 43.1 43.2 43.3 43.4 43.5 Ind, Philip W (2020). "E-cigarette or vaping product use-associated lung injury". British Journal of Hospital Medicine. 81 (4): 1–9. doi:10.12968/hmed.2019.0371. ISSN 1750-8460. PMID 32339005.
- ↑ 44.0 44.1 44.2 44.3 44.4 44.5 44.6 "Lung Injuries Associated with Use of Vaping Products". United States Food and Drug Administration. April 13, 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 45.0 45.1 45.2 45.3 45.4 45.5 45.6 O'Callaghan, Marissa; Boyle, Niamh; Fabre, Aurelie; Keane, Michael P.; McCarthy, Cormac (March 10, 2022). "Vaping-Associated Lung Injury: A Review". Medicina (Kaunas, Lithuania). MDPI AG. 58 (3): 412. doi:10.3390/medicina58030412. ISSN 1648-9144. PMC 8949983. PMID 35334588.}
 This article incorporates text by Marissa O’Callaghan, Niamh Boyle, Aurelie Fabre, Michael P. Keane, and Cormac McCarthy available under the CC BY 4.0 license.
This article incorporates text by Marissa O’Callaghan, Niamh Boyle, Aurelie Fabre, Michael P. Keane, and Cormac McCarthy available under the CC BY 4.0 license.
- ↑ 46.0 46.1 46.2 46.3 Kaur, Gurjot; Gaurav, Anshuman; Lamb, Thomas; Perkins, Melanie; Muthumalage, Thivanka; Rahman, Irfan (2020). "Current Perspectives on Characteristics, Compositions, and Toxicological Effects of E-Cigarettes Containing Tobacco and Menthol/Mint Flavors". Frontiers in Physiology. 11. doi:10.3389/fphys.2020.613948. ISSN 1664-042X. PMC 7710937. PMID 33329065.
 This article incorporates text by Gurjot Kaur1, Anshuman Gaurav1, Thomas Lamb, Melanie Perkins, Thivanka Muthumalage, and Irfan Rahman2 available under the CC BY 4.0 license.
This article incorporates text by Gurjot Kaur1, Anshuman Gaurav1, Thomas Lamb, Melanie Perkins, Thivanka Muthumalage, and Irfan Rahman2 available under the CC BY 4.0 license.
- ↑ 47.0 47.1 47.2 47.3 47.4 McDonough, Samantha R.; Rahman, Irfan; Sundar, Isaac Kirubakaran (2021). "Recent updates on biomarkers of exposure and systemic toxicity in e-cigarette users and EVALI". American Journal of Physiology-Lung Cellular and Molecular Physiology. 320 (5): L661–L679. doi:10.1152/ajplung.00520.2020. ISSN 1040-0605. PMC 8174828. PMID 33501893.
- ↑ 48.0 48.1 Virgili, Fabrizio; Nenna, Raffaella; Ben David, Shira; Mancino, Enrica; Di Mattia, Greta; Matera, Luigi; Petrarca, Laura; Midulla, Fabio (December 2022). "E-cigarettes and youth: an unresolved Public Health concern". Italian Journal of Pediatrics. 48 (1): 97. doi:10.1186/s13052-022-01286-7. PMC 9194784. PMID 35701844.
 This article incorporates text by Fabrizio Virgili, Raffaella Nenna, Shira Ben David, Enrica Mancino, Greta Di Mattia, Luigi Matera, Laura Petrarca, and Fabio Midulla available under the CC BY 4.0 license.
This article incorporates text by Fabrizio Virgili, Raffaella Nenna, Shira Ben David, Enrica Mancino, Greta Di Mattia, Luigi Matera, Laura Petrarca, and Fabio Midulla available under the CC BY 4.0 license.
- ↑ 49.0 49.1 49.2 49.3 49.4 49.5 49.6 Hofmann, Joseph J.; Poulos, Victoria C.; Zhou, Jiahai; Sharma, Maksym; Parraga, Grace; McIntosh, Marrissa J. (January 24, 2024). "Review of quantitative and functional lung imaging evidence of vaping-related lung injury". Frontiers in Medicine. 11. doi:10.3389/fmed.2024.1285361. PMC 10847544. PMID 38327710.
{{cite journal}}: Check|pmc=value (help) This article incorporates text by Joseph J. Hofmann, Victoria C. Poulos, Jiahai Zhou, Maksym Sharma, Grace Parraga, and Marrissa J. McIntosh available under the CC BY 4.0 license.
This article incorporates text by Joseph J. Hofmann, Victoria C. Poulos, Jiahai Zhou, Maksym Sharma, Grace Parraga, and Marrissa J. McIntosh available under the CC BY 4.0 license.
- ↑ 50.0 50.1 Jonas, Andrea (July 18, 2022). "Impact of vaping on respiratory health". BMJ: e065997. doi:10.1136/bmj-2021-065997. PMID 35851281.
- ↑ 51.0 51.1 Traboulsi, Hussein; Cherian, Mathew; Abou Rjeili, Mira; Preteroti, Matthew; Bourbeau, Jean; Smith, Benjamin M.; Eidelman, David H.; Baglole, Carolyn J. (2020). "Inhalation Toxicology of Vaping Products and Implications for Pulmonary Health". International Journal of Molecular Sciences. 21 (10): 3495. doi:10.3390/ijms21103495. ISSN 1422-0067. PMC 7278963. PMID 32429092.
 This article incorporates text by Hussein Traboulsi, Mathew Cherian, Mira Abou Rjeili, Matthew Preteroti, Jean Bourbeau, Benjamin M. Smith, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
This article incorporates text by Hussein Traboulsi, Mathew Cherian, Mira Abou Rjeili, Matthew Preteroti, Jean Bourbeau, Benjamin M. Smith, David H. Eidelman, and Carolyn J. Baglole available under the CC BY 4.0 license.
- ↑ 52.0 52.1 Maddock, Sean D.; Cirulis, Meghan M.; Callahan, Sean J.; Keenan, Lynn M.; Pirozzi, Cheryl S.; Raman, Sanjeev M.; Aberegg, Scott K. (October 10, 2019). "Pulmonary Lipid-Laden Macrophages and Vaping". The New England Journal of Medicine. 381 (15): 1488–1489. doi:10.1056/NEJMc1912038. ISSN 0028-4793. PMID 31491073.
- ↑ 53.00 53.01 53.02 53.03 53.04 53.05 53.06 53.07 53.08 53.09 53.10 53.11 53.12 53.13 Schier, Joshua G.; Meiman, Jonathan G.; Layden, Jennifer; Mikosz, Christina A.; VanFrank, Brenna; King, Brian A; et al. (CDC 2019 Lung Injury Response Group.) (2019). "Severe Pulmonary Disease Associated with Electronic-Cigarette–Product Use – Interim Guidance". Morbidity and Mortality Weekly Report (MMWR). 68 (36): 787–790. doi:10.15585/mmwr.mm6836e2. ISSN 0149-2195. PMC 6755818. PMID 31513561.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 54.0 54.1 Mescolo, Federica; Ferrante, Giuliana; La Grutta, Stefania (August 20, 2021). "Effects of E-Cigarette Exposure on Prenatal Life and Childhood Respiratory Health: A Review of Current Evidence". Frontiers in Pediatrics. 9: 711573. doi:10.3389/fped.2021.711573. PMC 8430837. PMID 34513764.
- ↑ 55.0 55.1 55.2 55.3 55.4 55.5 55.6 Henry, Travis S.; Kanne, Jeffrey P.; Kligerman, Seth J. (September 2019). "Imaging of Vaping-Associated Lung Disease". The New England Journal of Medicine. 381 (15): 1486–1487. doi:10.1056/NEJMc1911995. ISSN 0028-4793. PMID 31491070.
- ↑ Mir, Mikael; Rauf, Ibtisam; Goksoy, Sarah; Khedr, Anwar; Jama, Abbas B; Mushtaq, Hisham; Jain, Nitesh K; Khan, Syed Anjum; Surani, Salim; Koritala, Thoyaja (May 25, 2022). "Electronic Cigarettes: Are They Smoking Cessation Aids or Health Hazards?". Cureus. doi:10.7759/cureus.25330. PMC 9232181. PMID 35761921.
- ↑ 57.0 57.1 "For Healthcare Providers". Severe lung disease. Centers for Disease Control and Prevention (CDC). October 22, 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Henry, Travis S.; Kligerman, Seth J.; Raptis, Constantine A.; Mann, Howard; Sechrist, Jacob W.; Kanne, Jeffrey P. (2020). "Imaging Findings of Vaping-Associated Lung Injury". American Journal of Roentgenology. 214 (3): 498–505. doi:10.2214/AJR.19.22251. ISSN 0361-803X. PMID 31593518.
- ↑ Agudelo, Christina W.; Samaha, Ghassan; Garcia-Arcos, Itsaso (2020). "Alveolar lipids in pulmonary disease. A review". Lipids in Health and Disease. 19 (1). doi:10.1186/s12944-020-01278-8. ISSN 1476-511X. PMC 7268969. PMID 32493486.
 This article incorporates text by Christina W. Agudelo, Ghassan Samaha, and Itsaso Garcia-Arcos available under the CC BY 4.0 license.
This article incorporates text by Christina W. Agudelo, Ghassan Samaha, and Itsaso Garcia-Arcos available under the CC BY 4.0 license.
- ↑ King, Brian A.; Jones, Christopher M.; Baldwin, Grant T.; Briss, Peter A. (2020). "The EVALI and Youth Vaping Epidemics — Implications for Public Health". New England Journal of Medicine. 382 (8): 689–691. doi:10.1056/NEJMp1916171. ISSN 0028-4793. PMID 31951683.
- ↑ 61.0 61.1 Takakuwa, Kevin M.; Schears, Raquel M. (2021). "The emergency department care of the cannabis and synthetic cannabinoid patient: a narrative review". International Journal of Emergency Medicine. 14 (1). doi:10.1186/s12245-021-00330-3. ISSN 1865-1372. PMC 7874647. PMID 33568074.
 This article incorporates text by Kevin M. Takakuwa and Raquel M. Schears available under the CC BY 4.0 license.
This article incorporates text by Kevin M. Takakuwa and Raquel M. Schears available under the CC BY 4.0 license.
- ↑ "Quebec resident confirmed as first Canadian case of vaping-related illness". CBC.ca. September 27, 2019.
- ↑ Public Health Agency of Canada (October 11, 2019). "Statement from the Council of Chief Medical Officers of Health on vaping in Canada". Chief Public Health Officer of Canada.
- ↑ 64.0 64.1 Langreth, Robert; Etter, Lauren (September 30, 2019). "How Early Signs of Lung Effects of Vaping Were Missed and Downplayed". Insurance Journal.
- ↑ Rodger, James (October 1, 2019). "Brit suspected to be first to die from condition linked to vaping". Coventry Telegraph.
- ↑ Wheaton, Sarah (September 12, 2019). "Europe's missing 'vaping sickness'". Politico.
- ↑ Muthumalage, Thivanka; Lucas, Joseph H.; Wang, Qixin; Lamb, Thomas; McGraw, Matthew D.; Rahman, Irfan (2020). "Pulmonary Toxicity and Inflammatory Response of Vape Cartridges Containing Medium-Chain Triglycerides Oil and Vitamin E Acetate: Implications in the Pathogenesis of EVALI". Toxics. 8 (3): 46. doi:10.3390/toxics8030046. ISSN 2305-6304. PMC 7560420. PMID 32605182.
 This article incorporates text by Thivanka Muthumalage, Joseph H. Lucas, Qixin Wang, Thomas Lamb, Matthew D. McGraw, and Irfan Rahman1 available under the CC BY 4.0 license.
This article incorporates text by Thivanka Muthumalage, Joseph H. Lucas, Qixin Wang, Thomas Lamb, Matthew D. McGraw, and Irfan Rahman1 available under the CC BY 4.0 license.
- ↑ Bhatt, Jayesh Mahendra; Ramphul, Manisha; Bush, Andrew (2020). "An update on controversies in e-cigarettes". Paediatric Respiratory Reviews. 36: 75–86. doi:10.1016/j.prrv.2020.09.003. ISSN 1526-0542. PMC 7518964. PMID 33071065.
- ↑ 69.0 69.1 Brar, Esha; Saxena, Anish; Dukler, Claudia; Xu, Fangxi; Saxena, Deepak; Cheema Brar, Preneet; Guo, Yuqi; Li, Xin (2021). "Vaping, SARS-CoV-2, and Multisystem Inflammatory Syndrome: A Perfect Storm". Frontiers in Pediatrics. 9. doi:10.3389/fped.2021.647925. ISSN 2296-2360. PMC 8149601. PMID 34055688.
- ↑ Chadi, Nicholas; Vyver, Ellie; Bélanger, Richard E (September 17, 2021). "Protecting children and adolescents against the risks of vaping". Paediatrics & Child Health. 26 (6): 358–365. doi:10.1093/pch/pxab037. PMC 8448493. PMID 34552676.
- ↑ Esquer, Carolina; Echeagaray, Oscar; Firouzi, Fareheh; Savko, Clarissa; Shain, Grant; Bose, Pria; Rieder, Abigail; Rokaw, Sophie; Witon-Paulo, Andrea; Gude, Natalie; Sussman, Mark (February 2022). "Fundamentals of vaping-associated pulmonary injury leading to severe respiratory distress". Life Science Alliance. 5 (2): 1555–1565. doi:10.26508/lsa.202101246. PMC 8616545. PMID 34810278.
- ↑ Priemer, David S.; Gravenmier, Curtis; Batouli, Amir; Hooper, Jody E. (November 1, 2020). "Overview of Pathologic Findings of Vaping in the Context of an Autopsy Patient With Chronic Injury". Archives of Pathology & Laboratory Medicine. 144 (11): 1408–1413. doi:10.5858/arpa.2019-0637-RA. PMID 32383974.
- ↑ Choi, Humberto; Lin, Yu; Race, Elliot; Macmurdo, Maeve G. (February 2021). "Electronic Cigarettes and Alternative Methods of Vaping". Annals of the American Thoracic Society. 18 (2): 191–199. doi:10.1513/AnnalsATS.202005-511CME. PMID 33052707.
- ↑ Bush, Andrew; Ferkol, Thomas; Valiulis, Algirdas; Mazur, Artur; Chkhaidze, Ivane; Maglakelidze, Tamaz; Sargsyan, Sergey; Boyajyan, Gevorg; Cirstea, Olga; Doan, Svitlana; Katilov, Oleksandr; Pokhylko, Valeriy; Dubey, Leonid; Poluziorovienė, Edita; Prokopčiuk, Nina; Taminskienė, Vaida; Valiulis, Arūnas (February 8, 2021). "Unfriendly Fire: How the Tobacco Industry is Destroying the Future of Our Children". Acta medica Lituanica. 28 (1): 6–18. doi:10.15388/Amed.2020.28.1.6. PMC 8311841. PMID 34393624.
- ↑ Javelle, Emilie (June 2020). "Electronic cigarette and vaping should be discouraged during the new coronavirus SARS-CoV-2 pandemic". Archives of Toxicology. 94 (6): 2261–2262. doi:10.1007/s00204-020-02744-z. PMC 7165073. PMID 32303807.
- ↑ Rebuli, Meghan E.; Rose, Jason J.; Noël, Alexandra; Croft, Daniel P.; Benowitz, Neal L.; Cohen, Alan H.; Goniewicz, Maciej L.; Larsen, Brandon T.; Leigh, Noel; McGraw, Matthew D.; Melzer, Anne C.; Penn, Arthur L.; Rahman, Irfan; Upson, Dona; Crotty Alexander, Laura E.; Ewart, Gary; Jaspers, Ilona; Jordt, Sven Eric; Kligerman, Seth; Loughlin, Ceila E.; McConnell, Rob; Neptune, Enid R.; Nguyen, Tran B.; Pinkerton, Kent E.; Witek, Theodore J. (January 2023). "The E-cigarette or Vaping Product Use–Associated Lung Injury Epidemic: Pathogenesis, Management, and Future Directions: An Official American Thoracic Society Workshop Report". Annals of the American Thoracic Society. 20 (1): 1–17. doi:10.1513/AnnalsATS.202209-796ST. PMC 9819258. PMID 36584985.
{{cite journal}}: Check|pmc=value (help) - ↑ Baker, Melissa M.; Procter, Theresa D.; Belzak, Lisa; Ogunnaike-Cooke, Susanna (2022). "Vaping-associated lung illness (VALI) in Canada: a descriptive analysis of VALI cases reported from September 2019 to December 2020". Health promotion and chronic disease prevention in Canada : research, policy and practice. Health Promotion and Chronic Disease Prevention Branch (HPCDP) Public Health Agency of Canada. 42 (1): 37–44. doi:10.24095/hpcdp.42.1.06. ISSN 2368-738X. PMID 35044143.
- ↑ Christiani, David C. (September 2019). "Vaping-Induced Lung Injury". The New England Journal of Medicine. 382 (10): 960–962. doi:10.1056/NEJMe1912032. ISSN 0028-4793. PMID 31491071.
- ↑ Hswen, Yulin; Brownstein, John S. (2019). "Real-Time Digital Surveillance of Vaping-Induced Pulmonary Disease". The New England Journal of Medicine. 381 (18): 1778–1780. doi:10.1056/NEJMc1912818. ISSN 0028-4793. PMID 31539466.
- ↑ Fried, Nicholas D.; Gardner, Jason D. (2020). "Heat-not-burn tobacco products: an emerging threat to cardiovascular health". American Journal of Physiology-Heart and Circulatory Physiology. 319 (6): H1234–H1239. doi:10.1152/ajpheart.00708.2020. ISSN 0363-6135. PMC 7792702. PMID 33006919.
- ↑ Fentem, Sarah (October 4, 2019). "As More People Die After Using Vaping Products, St. Louis Doctor Warns Of The Risks". KWMU.
- ↑ Naftulin, Julia (September 6, 2019). "A number of vape-related lung illnesses are linked to 'Dank Vapes,' a mysterious black market brand selling THC products". Insider.
- ↑ Bentley, Jimmy (October 7, 2019). "First Massachusetts Vape-Related Death Confirmed". Patch Media.
- ↑ Kapnick, Izzy (October 25, 2019). "Vaping Companies Brace for Wave of Lawsuits Over Lung Illness". Courthouse News Service.
- ↑ Mole, Beth (September 12, 2019). "Black-market THC-vape operation busted in Wisconsin, police say". Ars Technica.
- ↑ Carlos, W. Graham; Crotty Alexander, Laura E; Gross, Jane E; Dela Cruz, Charles S; Keller, Jonathan M; Pasnick, Susan; Jamil, Shazia (October 2019). "ATS Health Alert—Vaping Associated Pulmonary Illness (VAPI)". American Journal of Respiratory and Critical Care Medicine. 200 (7): P15–P16. doi:10.1164/rccm.2007P15. ISSN 1073-449X. PMID 31532698.
Further reading
- "Lung Illnesses Associated with Use of Vaping Products". United States Food and Drug Administration. April 13, 2020.
- Corum, Jonathan (January 13, 2020). "Vaping Illness Tracker 2: 2,602 Cases and 59 Deaths". The New York Times.
- Taylor, Joanne; Wiens, Terra; Peterson, Jason; Saravia, Stefan; Lunda, Mark; Hanson, Kaila; et al. (November 2019). "Characteristics of E-cigarette, or Vaping, Products Used by Patients with Associated Lung Injury and Products Seized by Law Enforcement — Minnesota, 2018 and 2019". Morbidity and Mortality Weekly Report (MMWR). 68 (47): 1096–1100. doi:10.15585/mmwr.mm6847e1. ISSN 0149-2195. PMC 6881051. PMID 31774740.
- Blount, Benjamin C.; Karwowski, Mateusz P.; Shields, Peter G.; Morel-Espinosa, Maria; Valentin-Blasini, Liza; Gardner, Michael; et al. (February 2020). "Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI". New England Journal of Medicine. 382 (8): 697–705. doi:10.1056/NEJMoa1916433. ISSN 0028-4793. PMC 7032996. PMID 31860793.
External links
- "E-Cigarettes and Vaping-Related Disease". The New England Journal of Medicine. 2025.
| Classification |
|---|