List of WHO AWaRe antibiotics for common infections in primary care

This is a list of antibiotics for common infections in primary care as detailed in the WHO AWaRe classification in the World Health Organization's book The WHO AWaRe (Access, Watch, Reserve) antibiotic book (2022).
| Colour key: |
Respiratory
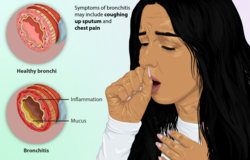
Bronchitis
| Infection | Frequency/risk factors | Symptoms | Tests | Advice and guidance | AWaRe antibiotic use | |
|---|---|---|---|---|---|---|
| Acute bronchitis | Frequency:
Common[1]
Winter[1] |
Cough (>5 days) +/- fever[1]
Normal heart rate and respiratory rate[1] |
Investigations generally initially unnecessary in otherwise well adults.[2]
Consider testing for COVID-19.[1] |
Mostly viral[1] Typically resolve without treatment[3] Yellow/green sputum does not indicate bacterial infection[1] Cough may last weeks (10–20 days)[1] Bronchodilators and mucolytics, though usefulness unclear[1] |
Antibiotic not recommended, unless severe symptoms or weak immune system.[1] | |
| Adults | Children | |||||
|
Typically resolve without treatment.[4] |
Antibiotic considered if fever ≥39.0 °C, bilateral otitis media in children younger than 2 years.[1] | |||||
Mild community-acquired pneumonia
| Infection | Frequency/risk factors | Symptoms | Tests | Advice and guidance | AWaRe antibiotic use | |
|---|---|---|---|---|---|---|
| Mild community-acquired pneumonia | Frequency:
Common worldwide[5] Leading cause of hospital admission Risk factors: Children < 5 years (low income countries), adults > 65 years (high-income countries)[5] |
Cough (new or worse) + fever (≥ 38.0 °C)[5]
Sputum, shortness of breath, chest hurts[5] Tachypnea, crepitations, reduced oxygen saturation[5]
|
Tests in mild illness usually not required.[5]
Consider: Testing for HIV, tuberculosis (high risk groups)[5] Blood tests: blood cultures, complete blood count, CRP |
General
Antipyretics: paracetamol, ibuprofen[5] Seek medical care if worsening of symptoms.[5] Prevention Vaccines against pneumonia, flu, COVID-19, H. influenzae[5] |
Adults | Children |
| Treatment duration | ||||||
| 5 days or longer in severe illness.[5] | 3 to 5 days or longer depending on severity.[5] | |||||
| Mild illness | ||||||
| First choice:
Amoxicillin 1 gram 3x daily by mouth[5] or Phenoxymethylpenicillin 500 milligrams 4x daily by mouth[5] Second choice: Amoxicillin/clavulanic acid 875 mg+125 mg 3x daily by mouth[5] or Doxycycline 100 milligrams 2x daily by mouth[5] |
First choice:
Amoxicillin (80–90 milligrams/kg/day) by mouth[5] | |||||
| Severe illness | ||||||
|
First choice: Cefotaxime 2 grams 3x daily into vein or muscle by injection[5] or |
First choice: or or | |||||
| +/- Clarithromycin 500 mg twice daily by mouth or into vein[5] | +/- Gentamicin | |||||
| Second choice:
Amoxicillin/clavulanic acid 1 gram + 200 mg three times daily into vein[5] |
In HIV +ve babies younger than 1 year
Add Sulfamethoxazole/trimethoprim for 3 weeks[5] | |||||
| +/- Clarithromycin 500 mg 2x daily by mouth or into vein[5] | No improvement with first choice after 48–72 hours
Cefotaxime into vein or muscle[5] or Ceftriaxone into vein or muscle[5] | |||||
Chronic obstructive bronchitis
| Frequency/risk factors | Symptoms | Tests | Advice and guidance | AWaRe antibiotic use | |||
|---|---|---|---|---|---|---|---|
| Chronic obstructive bronchitis (COPD) exacerbation | Worsening shortness of breath + cough in known COPD.[6]
Increased sputum production[6] |
Culture of sputum in mild disease not always helpful as may give confusing results.[6]
Consider: Blood tests[6] |
Consider: Short-acting bronchodilator[6] Prevention Reduce indoor air pollution[6] Vaccinations: pneumonia vaccine, influenza vaccine, COVID-19 vaccine[6] |
Antibiotics not necessary in mild illness.[6] | |||
| Treatment duration | |||||||
| Adults | Children | ||||||
| First choice
Amoxicillin 500 milligrams 3x daily by mouth[6] Second choice Cefalexin 500 milligrams 3x daily by mouth[6] or Doxycycline 100 milligrams 2x daily by mouth[6] or Amoxicillin/clavulanic acid 500+125 milligrams 3x daily by mouth if severe[6] |
|||||||
ENT
Acute otitis media
| Infection | Frequency/risk factors | Symptoms | Tests | Advice and guidance | AWaRe antibiotic use | |
|---|---|---|---|---|---|---|
| Acute otitis media (OM)[7] |
317 million worldwide (2017)[8] Affects 80% of children by age 5 years.[9] Most common reason for antibiotic use in young children.[9] |
Typically young children with ear pain (one or both).[8]
Pulling ear, irritability, headache, fever (in 2/3), vomiting,[7] discharge.[8] Bulging red tympanic membrane.[8] +/- Viral upper respiratory tract infection.[7] |
Diagnosis using otoscope.[7]
|
Mostly viral and resolve without treatment, particularly in high income countries.[10]
Antipyretics; (paracetamol, ibuprofen).[8] No ibuprofen if younger than 3-months[8] Prevention: hand hygiene, pneumococcal vaccine, flu vaccine, Hib vaccine[8] |
For severe symptoms, weak immune system, fever ≥39.0 °C, bilateral OM in children younger than 2 years.[8] | |
| Treatment duration: 5 days[8] | ||||||
| Adults | Children | |||||
| First choice | First choice | |||||
| First choice
Amoxicillin 500 mg 3x daily by mouth[4][8] |
First choice
Amoxicillin by mouth[8] | |||||
| Second choice | Second choice | |||||
| Amoxicillin/clavulanic acid 500 mg+125 mg 3x daily by mouth[8] | Amoxicillin/clavulanic acid by mouth[8] | |||||
Pharyngitis
| Infection | Frequency/risk factors | Symptoms | Tests | Advice and guidance | AWaRe antibiotic use | |
|---|---|---|---|---|---|---|
| Pharyngitis[11] | >80% viral[11] | Sore throat[11]
Viral: + cough, headache, muscle aches[11] Bacterial: + fever, cervical lymphadenopathy, exudate[11] |

|
Most resolve without treatment.[11] | Antibiotics where rheumatic fever is endemic.[11] | |
| Treatment duration: 5 or 10 days depending on risk.[11] | ||||||
| Adults | Children | |||||
| First choice | First choice | |||||
|
Amoxicillin 500 milligrams 3x daily by mouth[4][11] or Phenoxymethylpenicillin 500 milligrams 4x daily by mouth[4][11] |
or | |||||
| Second choice | Second choice | |||||
| or
Clarithromycin 500 milligrams twice daily by mouth[11] |
or | |||||
Acute sinusitis
| Infection | Frequency/risk factors | Symptoms | Tests | Advice and guidance | AWaRe antibiotic use | |
|---|---|---|---|---|---|---|
| Acute sinusitis[12] | Common[12] | Blocked and runny nose[12]
Facial pain and pressure[12] |
Tests usually not required.[12]
For illness duration <10-days; nasal irrigation, analgesia.[12] Antibiotics not always needed.[12] |
Most preceded by upper respiratory tract infection (URTI), and resolve without treatment.[12]
Symptoms may last for up to 1 month.[12] Yellow/green nasal discharge not necessarily bacterial.[12] Prevention: some protection with pneumococcal vaccine, Hib vaccine[12] |
Antibotics if severe symptoms: fever ≥39.0 °C, purulent discharge from nose, facial pain (>3 days)[12] | |
| Treatment duration: 5 days[12] | ||||||
| Adults | Children | |||||
| Amoxicillin 1 gram 3x daily by mouth[12]
or Amoxicillin/clavulanic acid 500+125 milligrams 3x daily by mouth[12] |
Amoxicillin[12]
or | |||||
Dental infection
| Infection | Symptoms | Management | Advice | Notes | AWaRe antibiotic use | |
|---|---|---|---|---|---|---|
| Dental infection | Dental disease: Toothache radiating to ear/jaw.[13]
Pericoronitis: Toothache + swollen gum[13] Necrotizing periodontal disease: severe toothache, swollen and bleeding gums[13] Noma: severe disease with destruction of soft tissue/bone[13] |
May require imaging, blood tests, culture[13]
Painkillers[13] |
Most resolve without antibiotics[13]
Salt water gargles[13] Painkillera: ibuprofen, paracetamol[13] Effectiveness of mouthwashes unclear.[13] Prevention: Good oral hygiene, reduce dietary sugar, brush teeth, stop smoking.[13]
|
Frequency: common worldwide.[13]
Risk factors: high sugar diet, poor oral hygiene, smoking, dental caries, chewing tobacco, malnutrition.[13] |
Dental treatment more likely to help than antibiotics.[13]
Metronidazole may be an option for deeper infection.[13] | |
| Treatment duration: 3 to 5 days depending on response[13] | ||||||
| Adults | Children | |||||
| Amoxicillin 500 milligrams 3x daily by mouth[13]
or Phenoxymethylpenicillin 500 milligrams 4x daily by mouth[13] |
Amoxicillin[13]
or | |||||
Acute localized lymphadenitis
| Infection | Frequency | Symptoms | Tests | Advice | AWaRe antibiotic use | |
|---|---|---|---|---|---|---|
| Acute localized lymphadenitis | Frequency: common worldwide[14] | Sudden painful red large lymph node[14]
Fever[14] |
Tests usually not necessary, though may need tests for HIV, tuberculosis, malignancy in some.[14]
Persistent large lymph nodes require further tests.[14] |
Most large lymph nodes have a viral cause, though unilateral symptoms possible likely bacterial.[14] | Treatment of localized acute bacterial lymphadenitis | |
| Treatment duration: 5 days[14] | ||||||
| Adults | Children | |||||
| Amoxicillin/clavulanic acid 500 mg+125 mg 4x daily by mouth, or 1gram+200 mg 4x daily into vein[14]
or Cefalexin 500 mg 4x daily by mouth[14] or Cloxacillin 500 mg 4x daily by mouth[14] |
Amoxicillin/clavulanic acid into vein[14]
or
Cloxacillin into vein[14] | |||||
Eyes
| Infection | Frequency/risk factors | Symptoms | Test | Advice | AWaRe antibiotic use | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Conjunctivitis | Itchy, gritty, red, watery eye[15] | 
|
Most resolve within a week without antibiotics.[15] | ||||||||
| Treatment duration: varies between treatments from single dose, to 3 days, or 5 days [15] | |||||||||||
| Adults | Children | ||||||||||
| Gentamicin 0.3% eye drops, 1 drop in affected eye 4x daily[15] | Gentamicin 0.3% eye drops, 1 drop in affected eye 4x daily[15] | ||||||||||
| Or
Ofloxacin 0.3% eye drops, 1 drop in affected eye 4x daily[15] |
Ofloxacin 0.3% eye drops, 1 drop in affected eye 4x daily[15] | ||||||||||
| or
Tetracycline 1% ointment, 1 cm in affected eye 4x daily[15] |
Tetracycline 1% ointment, 1 cm in affected eye 4x daily[15] | ||||||||||
| Gonococcal conjunctivitis:
Ceftriaxone 250 milligrams into muscle (single dose) [15] combined with Azithromycin 1 gram by mouth (single dose) [15] |
Gonococcal conjunctivitis:
Ceftriaxone 50 mg/kg into muscle (single dose)[15] Chlamydial ophthalmia: Azithromycin by mouth[15] | ||||||||||
| Keratitis | [15] | ||||||||||
| Adults | Children | ||||||||||
| Endophthalmitis | [15] | 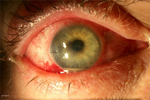
|
|||||||||
| Adults | Children | ||||||||||
| Periorbital cellulitis | [15] | 
|
|||||||||
| Adults | Children | ||||||||||
| Trachoma [16] | 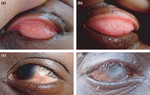
|
||||||||||
| Adults | Children | ||||||||||
Genitourinary
| Infection | Frequency/risk factors | Symptoms | Tests | Advice | AWaRe guidance | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Urinary tract infection (UTI)[17] | Common: females, increasing age, sexual activity[18]
Most caused by E.coli[18] |
Dysuria[18]
Urinary urgency, frequency[17] Lower abdominal pain[17] |
Urine culture: children, men, pregnant women, recurrent UTI[18] | Prevention: Pass urine after sex, showers not baths, girls to wipe front to back[17]
Drink water[17] In young otherwise healthy non-pregnant females with mild symptoms antibiotics may not always be required.[4] |
||||||
| Treatment duration: 3–5 days[18] | ||||||||||
| Adults | Children | |||||||||
| Amoxicillin/clavulanic acid 500+125 milligrams 3x daily by mouth[18]
or Nitrofurantoin 100 milligrams twice daily (modified release) or 50 milligrams 4x daily (immediate release), by mouth[18] or Sulfamethoxazole/trimethoprim[18] or Trimethoprim 200 milligrams twice daily for 3-days by mouth[18] |
Amoxicillin/clavulanic acid[18]
or or Sulfamethoxazole/trimethoprim[18] or | |||||||||
| Chlamydia[19] | 
|
Prevention: safe sex, condoms, treat sexual partners[19] | ||||||||
| Uncomplicated urogenital infection | ||||||||||
| or | ||||||||||
| Anorectal infection | ||||||||||
| In pregnancy | ||||||||||
| Gonorrhea | [20] | Ceftriaxone 250 milligrams into muscle[20]
combined with Azithromycin 1 gram by mouth[20] |
||||||||
| Syphilis | [21] | Late syphilis:
Benzathine benzylpenicillin[21] or Procaine benzypenicillin[21] |
Congenital syphilis | |||||||
| Neurosyphilis:
or Procaine benzypenicillin[21] |
Benzylpenicillin[21] | |||||||||
| In pregnancy:
Benzathine benzylpenicillin[21] or Procaine benzylpenicillin[21] |
||||||||||
| Trichomoniasis | [22] | 
|
Metronidazole[22] | |||||||
Skin
| Infection | Frequency/risk factors | Symptoms | Tests | Advice | AWaRe guidance | ||||
|---|---|---|---|---|---|---|---|---|---|
| Superficial skin infections | Impetigo: Reddish papules, vesicles, pustules, yellowish crusts.[23]
Erysipelas: painful raised, well-defined, redness of skin of rapid onset, generally feeling unwell, +/-fever.[23] Cellulitis: painful redness of skin, +/-fever.[23] |
Swabs of intact skin generally unnecessary[23] |
|
Localized bullous impetigo: mupirocin 2% ointment may suffice.[23]
Severe infections may require intravenous antibiotics.[23] | |||||
| Treatment duration: 5 days[23] | |||||||||
| Adults | Children | ||||||||
| Amoxicillin/clavulanic acid 500 mg+125 mg 3x daily by mouth[23]
or Cefalexin 500 milligrams 3x daily by mouth[23] or Cloxacillin 500 milligrams 3x daily by mouth[23] |
Amoxicillin/clavulanic acid[23]
or or | ||||||||
| Wounds/burns related infection[4] | 
|
||||||||
| Adults | Children | ||||||||
| Amoxicillin/clavulanic acid 500 mg+125 mg 3x daily by mouth
or Cefalexin or Cloxacillin[4] |
Amoxicillin /clavulanic acid
or Cefalexin or Cloxacillin[4] | ||||||||
Gastrointestinal
| Infection | Management | Advice | Image | Notes | AWaRe guidance (adults) | AWaRe guidance (children) |
|---|---|---|---|---|---|---|
| Infectious bloody diarrhoea or dysentery[24] | Mostly viral and resolve without treatment.[24] | 
|
First choice
Second choice or |
First choice
Second choice or | ||
| or | or | |||||
| or | or | |||||
| Cholera[24] | Rehydration[24] | 
|
First choice | First choice | ||
| or | Second choice | |||||
| Second choice | or | |||||
| Enteric fever[25] | Consider local resistance pattern[25] | Low antibiotic resistance
Mild and severe cases: Ciprofloxacin[26] High antibiotic resistance Mild cases Azithromycin[26] Severe cases Ceftriaxone[26] |
Low antibiotic resistance
Mild and severe cases: Ciprofloxacin[26] High antibiotic resistance Mild cases Azithromycin[26] Severe cases Ceftriaxone[26] |
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 The WHO AWaRe. pp. 29-35
- ↑ Smith, Maeve P.; Lown, Mark; Singh, Sonal; Ireland, Belinda; Hill, Adam T.; Linder, Jeffrey A.; Irwin, Richard S.; Adams, Todd M.; Altman, Kenneth W.; Azoulay, Elie; Barker, Alan F.; Blackhall, Fiona; Birring, Surinder S.; Bolser, Donald C.; Boulet, Louis-Philippe; Braman, Sidney S.; Brightling, Christopher; Callahan-Lyon, Priscilla; Chang, Anne B.; Cowley, Terrie; Davenport, Paul; El Solh, Ali A.; Escalante, Patricio; Field, Stephen K.; Fisher, Dina; French, Cynthia T.; Grant, Cameron; Harding, Susan M.; Harnden, Anthony; Hill, Adam T.; Irwin, Richard S.; Kahrilas, Peter J.; Kavanagh, Joanne; Lai, Kefang; Kahrilas, Peter J.; Lilly, Craig; Lown, Mark; Madison, J. Mark; Malesker, Mark A.; Mazzone, Stuart; McGarvey, Lorcan; Molasoitis, Alex; Murad, M. Hassan; Narasimhan, Mangala; Newcombe, Peter; Oppenheimer, John; Rosen, Mark; Rubin, Bruce; Russell, Richard J.; Ryu, Jay H.; Singh, Sonal; Smith, Jaclyn; Smith, Maeve P.; Tarlo, Susan M.; Vertigan, Anne E.; Weinberger, Miles (May 2020). "Acute Cough Due to Acute Bronchitis in Immunocompetent Adult Outpatients". Chest. 157 (5): 1256–1265. doi:10.1016/j.chest.2020.01.044. Archived from the original on 2023-12-04. Retrieved 2023-11-30.
- ↑ Moja, L; Zanichelli, V; Mertz, D; Gandra, S; Cappello, B; Cooke, GS; Chuki, P; Harbarth, S; Pulcini, C; Mendelson, M; Tacconelli, E; Ombajo, LA; Chitatanga, R; Zeng, M; Imi, M; Elias, C; Ashorn, P; Marata, A; Paulin, S; Muller, A; Aidara-Kane, A; Wi, TE; Were, WM; Tayler, E; Figueras, A; Da Silva, CP; Van Weezenbeek, C; Magrini, N; Sharland, M; Huttner, B; Loeb, M (9 February 2024). "WHO's essential medicines and AWaRe: recommendations on first- and second-choice antibiotics for empiric treatment of clinical infections". Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. doi:10.1016/j.cmi.2024.02.003. PMID 38342438. Archived from the original on 29 February 2024. Retrieved 27 February 2024.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Zanichelli, Veronica; Sharland, Michael; Cappello, Bernadette; Moja, Lorenzo; Getahun, Haileyesus; Pessoa-Silva, Carmem; Sati, Hatim; van Weezenbeek, Catharina; Balkhy, Hanan; Simão, Mariângela; Gandra, Sumanth; Huttner, Benedikt (1 April 2023). "The WHO AWaRe (Access, Watch, Reserve) antibiotic book and prevention of antimicrobial resistance". Bulletin of the World Health Organization. 101 (4): 290–296. doi:10.2471/BLT.22.288614. ISSN 0042-9686. Archived from the original on 7 May 2023. Retrieved 17 November 2023.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 5.21 5.22 5.23 5.24 5.25 5.26 5.27 5.28 5.29 5.30 5.31 The WHO AWaRe. pp. 147-161
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 The WHO AWaRe. pp. 162-168
- ↑ 7.0 7.1 7.2 7.3 Danishyar, Amina; Ashurst, John V. (2024). "Acute Otitis Media". StatPearls. StatPearls Publishing. PMID 29262176. Archived from the original on 2022-10-10. Retrieved 2024-02-23.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 8.14 The WHO AWaRe. pp. 36-45
- ↑ 9.0 9.1 El Feghaly, Rana E.; Nedved, Amanda; Katz, Sophie E.; Frost, Holly M. (May 2023). "New insights into the treatment of acute otitis media". Expert Review of Anti-Infective Therapy. 21 (5): 523–534. doi:10.1080/14787210.2023.2206565. ISSN 1744-8336. PMID 37097281. Archived from the original on 2024-01-10. Retrieved 2024-01-09.
- ↑ Venekamp, Roderick P; Sanders, Sharon L; Glasziou, Paul P; Rovers, Maroeska M (15 November 2023). "Antibiotics for acute otitis media in children". Cochrane Database of Systematic Reviews. 2023 (11). doi:10.1002/14651858.CD000219.pub5. Archived from the original on 16 November 2023. Retrieved 3 December 2023.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 11.13 11.14 11.15 11.16 The WHO AWaRe. pp. 46-60
- ↑ 12.00 12.01 12.02 12.03 12.04 12.05 12.06 12.07 12.08 12.09 12.10 12.11 12.12 12.13 12.14 12.15 12.16 12.17 The WHO AWaRe. pp. 61-71
- ↑ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 13.11 13.12 13.13 13.14 13.15 13.16 13.17 13.18 13.19 The WHO AWaRe. pp. 72-95
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 The WHO AWaRe. pp. 95-104
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 15.12 15.13 15.14 15.15 The WHO AWaRe. pp. 105-139
- ↑ The WHO AWaRe. pp. 140-146
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 "Suffering from a urinary tract infection?". Centers for Disease Control and Prevention. 14 January 2022. Archived from the original on 10 January 2024. Retrieved 16 January 2024.
- ↑ 18.00 18.01 18.02 18.03 18.04 18.05 18.06 18.07 18.08 18.09 18.10 18.11 18.12 The WHO AWaRe. pp. 278-292
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 The WHO AWaRe. pp. 230-240
- ↑ 20.0 20.1 20.2 The WHO AWaRe. pp. 241-253
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 21.7 The WHO AWaRe. pp. 254-2270
- ↑ 22.0 22.1 The WHO AWaRe. pp. 271-277
- ↑ 23.00 23.01 23.02 23.03 23.04 23.05 23.06 23.07 23.08 23.09 23.10 23.11 23.12 23.13 The WHO AWaRe. pp. 193-205
- ↑ 24.00 24.01 24.02 24.03 24.04 24.05 24.06 24.07 24.08 24.09 24.10 24.11 24.12 24.13 24.14 24.15 24.16 24.17 24.18 24.19 The WHO AWaRe. pp. 169-184
- ↑ 25.0 25.1 25.2 Parry, Christopher M.; Qamar, Farah N.; Rijal, Samita; McCann, Naina; Baker, Stephen; Basnyat, Buddha (May 2023). "What Should We Be Recommending for the Treatment of Enteric Fever?". Open Forum Infectious Diseases. 10 (Suppl 1): S26–S31. doi:10.1093/ofid/ofad179. ISSN 2328-8957. PMID 37274536. Archived from the original on 2023-06-06. Retrieved 2024-02-15.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 The WHO AWaRe (Access, Watch, Reserve) antibiotic book Archived 2023-08-13 at the Wayback Machine. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO.
Bibliography
- The WHO AWaRe (Access, Watch, Reserve) antibiotic book. World Health Organization. 2022. Archived from the original on 13 August 2023. Retrieved 4 December 2023.