Ebstein's anomaly
| Ebstein's anomaly | |
|---|---|
 | |
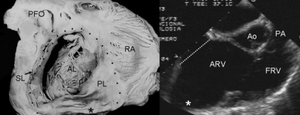
| Pathological specimen and ultrasound image of a heart with Ebstein's anomaly: Abbreviations: RA: right atrium; ARV: atrialized right ventricle; FRV: functional right ventricle; AL: anterior leaflet; SL: septal leaflet; LA: left atrium; LV: left ventricle; asterisk: grade II tethering of the tricuspid septal leaflet | |
| Specialty | Cardiology |
| Diagnostic method | Echocardiogram, chest X-ray, ECG[1] |
| Frequency | 2.4 per 10,000 live births[1] |
Ebstein's anomaly is a congenital heart defect in which the tricuspid valve leaflets have not formed properly, causing blood to leak backwards into the right atrium.[1] It may present at birth or in adulthood and signs and symptoms vary with the degree of tricuspid regurgitation and right heart involvement.[1] There may initially be no symptoms.[1] If diagnosed before birth, the unborn baby may develop hydrops and irregular heart beat, and has a 48% chance of being still born.[1] An affected newborn baby may appear blue or have signs of right heart failure.[2] It is typically associated with other heart problems, particularly atrial septal defect.[1]
Diagnosis is by echocardiogram.[3] Other tests include chest X-ray and ECG.[1] Treatment may include oxygen, prostaglandin infusion, inhaled nitric oxide and milrinone.[1] Mechanical ventilation and support with inotropes may be required.[1] Medical management buys time for the baby to develop beyond the immediate newborn period, when surgery is safer.[1]
It is rare, occurring in around 2.4 per 10,000 live births.[1] It accounts for 0.3% to 0.5% of heart defects present at birth and for 40% of tricuspid valve abnormalities at birth.[3] It was first described in 1866 by Wilhelm Ebstein.[1]
Signs and symptoms
The annulus of the valve is still in the normal position. The valve leaflets, however, are to a varying degree, attached to the walls and septum of the right ventricle. A subsequent "atrialization" of a portion of the morphologic right ventricle (which is then contiguous with the right atrium) is seen. This causes the right atrium to be large and the anatomic right ventricle to be small in size.[citation needed]
- S3 heart sound
- S4 heart sound
- Triple or quadruple gallop due to widely split S1 and S2 sounds plus a loud S3 and/or S4
- Systolic murmur of tricuspid regurgitation = Holosystolic or early systolic murmur along the lower left sternal border depending on the severity of the regurgitation
- Right atrial hypertrophy
- Right ventricular conduction defects
- Wolff-Parkinson-White syndrome often accompanies
Ebstein anomaly is the congenital heart lesion most commonly associated with supraventricular tachycardia.
Related abnormalities
It is typically associated with other heart problems, particularly atrial septal defect.[1]
Anatomic abnormalities
Typically, anatomic abnormalities of the tricuspid valve exist, with enlargement of the anterior leaflet of the valve. The other leaflets are described as being plastered to the endocardium.[citation needed] Tethering the underlying ventricular wall is the most common for the posterior and septal leaflets, and sail-like anterior leaflets may be tethered to the RV free wall also.[citation needed] About 50% of individuals with Ebstein's anomaly have an associated shunt between the right and left atria, either an atrial septal defect or a patent foramen ovale.[4]
Electrophysiologic abnormalities
About 50% of individuals with Ebstein's anomaly have an accessory pathway with evidence of Wolff-Parkinson-White syndrome, secondary to the atrialized right ventricular tissue. This can lead to abnormal heart rhythms including atrioventricular re-entrant tachycardia.[citation needed]
Other abnormalities that can be seen on the ECG include:
- signs of right atrial enlargement or tall and broad 'Himalayan' P waves
- first degree atrioventricular block manifesting as a prolonged PR-interval[5]
- low amplitude QRS complexes in the right precordial leads
- atypical right bundle branch block
- T wave inversion in V1-V4 and Q waves in V1-V4 and II, III and aVF.[6]
Risk factors
An enlargement of the aorta may occur; an increased risk of abnormality is seen in babies of women taking lithium during the first trimester of pregnancy[7] (though some have questioned this)[8] and in those with Wolff-Parkinson-White syndrome.
Diagnosis
The diagnosis of this condition is based on the following:[9]
- 3D echocardiography
- Electrocardiogram
- Radiography
- Cardiac MRI
-
Ebstein's anomaly shows dilatation at atrioventricular junction and aneurysmal fibrous sac asterisk (and echocardiogram asterisk)
-
ECGs recorded during sinus rhythm and AVRT in a 9-year-old girl with Ebstein's anomaly and a Mahaim accessory pathway.
-
A 10-lead ECG of a woman with Ebstein's anomaly: The ECG shows signs of right atrial enlargement, best seen in V1. Other P waves are broad and tall, these are termed "Himalayan" P waves. Also, a right bundle-branch block pattern and a first-degree atrioventricular block (prolonged PR-interval) due to intra-atrial conduction delay are seen. No evidence of a Kent-bundle is seen in this patient. The T wave inversion in V1-4 and a marked Q wave in III occur; these changes are characteristic for Ebstein's anomaly and do not reflect ischemic ECG changes in this patient.
Treatment
Medication
Ebstein's cardio physiology typically presents as an (antidromic) AV reentrant tachycardia with associated pre-excitation. In this setting, the preferred medication treatment agent is procainamide. Since AV-blockade may promote conduction over the accessory pathway, drugs such as beta blockers, calcium channel blockers, and digoxin are contraindicated[citation needed].
If atrial fibrillation with pre-excitation occurs, treatment options include procainamide, flecainide, propafenone, dofetilide, and ibutilide, since these medications slow conduction in the accessory pathway causing the tachycardia and should be administered before considering electrical cardioversion. Intravenous amiodarone may also convert atrial fibrillation and/or slow the ventricular response.[citation needed]
Surgery
The Canadian Cardiovascular Society (CCS) recommends surgical intervention for these indications:[10]
- Limited exercise capacity (NYHA III-IV)
- Increasing heart size (cardiothoracic ratio greater than 65%)
- Important cyanosis (resting oxygen saturation less than 90% - level B)
- Severe tricuspid regurgitation with symptoms
- Transient ischemic attack or stroke
The CCS further recommends patients who require operation for Ebstein's anomaly should be operated on by congenital heart surgeons who have substantial specific experience and success with this operation. Every effort should be made to preserve the native tricuspid valve.[10]
Epidemiology
It is rare, occurring in around 2.4 per 10,000 live births.[1] It accounts for 0.3% to 0.5% of heart defects present at birth and for 40% of tricuspid valve abnormalities at birth.[3]
History
Ebstein's anomaly was named after Wilhelm Ebstein, who in 1866 described the heart of the 19-year-old Joseph Prescher.[1][11]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 Boston, Umar S.; Bayle, Ken; Kumar, T. K. Susheel; Knott-Craig, Christopher J. (2020). "107. Neonatal Ebstein's Anomaly". In Raja, Shahzad G. (ed.). Cardiac Surgery: A Complete Guide. Switzerland: Springer. pp. 971–980. ISBN 978-3-030-24176-6. Archived from the original on 2023-06-30. Retrieved 2023-05-30.
- ↑ "Ebstein's anomaly - About the Disease - Genetic and Rare Diseases Information Center". rarediseases.info.nih.gov. Archived from the original on 20 November 2021. Retrieved 13 October 2022.
- ↑ 3.0 3.1 3.2 Ramcharan, Tristan K. W.; Goff, Donna A.; Greenleaf, Christopher E.; Shebani, Suhair O.; Salazar, Jorge D.; Corno, Antonio F. (October 2022). "Ebstein's Anomaly: From Fetus to Adult-Literature Review and Pathway for Patient Care". Pediatric Cardiology. 43 (7): 1409–1428. doi:10.1007/s00246-022-02908-x. ISSN 1432-1971. PMID 35460366. Archived from the original on 2022-10-16. Retrieved 2022-10-13.
- ↑ Mohan, Jagdish C. (2014). A Practical Approach to Clinical Echocardiography. Jaypee Brothers Medical Pub. p. 119. ISBN 978-93-5152-140-2.
- ↑ "Atrioventricular Block". The Lecturio Medical Concept Library. Archived from the original on 9 July 2021. Retrieved 3 July 2021.
- ↑ Khairy P, Marelli AJ (December 2007). "Clinical use of electrocardiography in adults with congenital heart disease". Circulation. 116 (23): 2734–46. doi:10.1161/CIRCULATIONAHA.107.691568. PMID 18056539. Archived from the original on 2013-02-24. Retrieved 2021-10-31.
- ↑ Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK (2007). "Ebstein's anomaly". Circulation. 115 (2): 277–85. doi:10.1161/CIRCULATIONAHA.106.619338. PMID 17228014.
- ↑ Yacobi S, Ornoy A (2008). "Is lithium a real teratogen? What can we conclude from the prospective versus retrospective studies? A review". Isr J Psychiatry Relat Sci. 45 (2): 95–106. PMID 18982835.[permanent dead link]
- ↑ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Ebstein malformation of the tricuspid valve". www.orpha.net. Archived from the original on 2 October 2020. Retrieved 19 January 2022.
- ↑ 10.0 10.1 Silversides, C. K.; Salehian, O.; Oechslin, E.; Schwerzmann, M.; Vonder Muhll, I.; Khairy, P.; Horlick, E.; Landzberg, M.; Meijboom, F.; Warnes, C.; Therrien, J. (2010). "Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: Complex congenital cardiac lesions". The Canadian Journal of Cardiology. 26 (3): e98–117. doi:10.1016/S0828-282X(10)70356-1. PMC 2851473. PMID 20352139.
- ↑ W. Ebstein. Über einen sehr seltenen Fall von Insufficienz der Valvula tricuspidalis, bedingt durch eine angeborene hochgradige Missbildung derselben. Archiv für Anatomie, Physiologie und wissenschaftliche Medicin, Leipzig, 1866, 238-254.
External links
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- All articles with dead external links
- Articles with dead external links from August 2019
- Articles with invalid date parameter in template
- Articles with permanently dead external links
- All articles with unsourced statements
- Articles with unsourced statements from February 2021
- Articles with unsourced statements from October 2021
- Congenital heart defects