Cavernous sinus thrombosis
| Cavernous sinus thrombosis | |
|---|---|
 | |
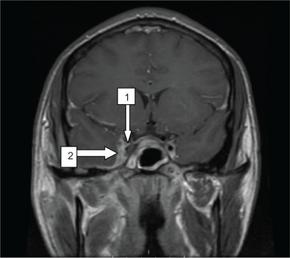
| Oblique section through the cavernous sinus. | |
| Specialty | Neurology |
| Symptoms | Headache, eye pain, bulging eyes, fever, double vision[1] |
| Complications | Meningitis, brain abscess, pituitary insufficiency[2] |
| Types | Septic (infection), aseptic (no infection)[3] |
| Risk factors | Boil of the nose, sinusitis, dental infection, injury, surgery, easy blood clot formation[3][2] |
| Diagnostic method | CT scan or MRI[2] |
| Differential diagnosis | Carotid cavernous fistula, meningioma, orbital cellulitis[3] |
| Treatment | Antibiotics, heparin, corticosteroids, surgery[1] |
| Frequency | Rare[1] |
| Deaths | Up to 30% die[1] |
Cavernous sinus thrombosis (CST) is the formation of a blood clot within the cavernous sinus, a cavity at the base of the brain which drains blood from the brain back to the heart.[1] Symptoms may include headache, eye pain, bulging eyes, fever, and double vision.[1] Often one eye is involved initially followed by involvement of the second eye.[3] Complications may include meningitis, brain abscess, and pituitary insufficiency.[2]
There are two types–septic (infection) and aseptic (not infection).[3] Risk factors include infections of the face such as boils on the nose, sinusitis, and dental infections.[2] The bacteria most commonly involved include Staphylococcus aureus and Streptococcus.[2] Other risk factors include injury, surgery, and easy blood clot formation.[3] Diagnosis is generally based on either CT scan or MRI.[2] It is a type of cerebral venous sinus thrombosis.[3]
It is a medical emergency.[1] Treatment may include antibiotics, heparin, and corticosteroids.[1] Occasionally surgery is required to drain an abscess the contributed to the condition.[1][3] Up to 30% of people die, despite treatment.[1] Among those who survive vision loss and seizures may occur.[1] Cavernous sinus thrombosis is rare, affecting possibly 0.2 to 1.6 people per 100,000 per year.[1][3]
Signs and symptoms
The clinical presentation of CST can be varied. Both acute, fulminant disease and indolent, subacute presentations have been reported in the literature. The most common signs of CST are related to anatomical structures affected within the cavernous sinus, notably cranial nerves III-VI, as well as symptoms resulting from impaired venous drainage from the orbit and eye.[4] Classic presentations are abrupt onset of unilateral periorbital edema, headache, photophobia, and bulging of the eye (proptosis).[5]
Other common signs and symptoms include:
Ptosis, chemosis, cranial nerve palsies (III, IV, V, VI). Sixth nerve palsy is the most common. Sensory deficits of the ophthalmic and maxillary branch of the fifth nerve are common. Periorbital sensory loss and impaired corneal reflex may be noted. Papilledema, retinal hemorrhages, and decreased visual acuity and blindness may occur from venous congestion within the retina. Fever, tachycardia and sepsis may be present. Headache with nuchal rigidity may occur. Pupil may be dilated and sluggishly reactive. Infection can spread to contralateral cavernous sinus within 24–48 hours of initial presentation.[5]
Cause
Septic

Septic CST most commonly results from contiguous spread of infection from a nasal furuncle (50%), sphenoidal or ethmoidal sinuses (30%) and dental infections (10%).[6] Less common primary sites of infection include tonsils, soft palate, middle ear, or orbit (orbital cellulitis). The highly anastomotic venous system of the paranasal sinuses allows retrograde spread of infection to the cavernous sinus via the superior and inferior ophthalmic veins. It was previously thought that veins in the area were valveless and that this was the major cause of the retrograde spread, but Studies have since shown that the ophthalmic and facial veins are not valveless.[7]
Staphylococcus aureus is the most common infectious microbe, found in 70% of the cases.[6] Streptococcus is the second leading cause. Gram-negative rods and anaerobes may also lead to cavernous sinus thrombosis. Rarely, Aspergillus fumigatus and mucormycosis cause CST.
Aseptic
Aseptic cavernous sinus thrombosis is much less common and is usually associated with other disorders including trauma, circulatory problems, nasopharynx cancers and other tumours of the skull base, dehydration, and anemia.[8][9]
Diagnosis
The diagnosis of cavernous sinus thrombosis is made clinically, with imaging studies to confirm the clinical impression. Proptosis, ptosis, chemosis, and cranial nerve palsy beginning in one eye and progressing to the other eye establish the diagnosis. Cavernous sinus thrombosis is a clinical diagnosis with laboratory tests and imaging studies confirming the clinical impression.[10]
Lab tests
CBC, ESR, blood cultures and sinus cultures help establish and identify an infectious primary source. Lumbar puncture is necessary to rule out meningitis.
Medical imaging
Sinus films are helpful in the diagnosis of sphenoid sinusitis. Opacification, sclerosis, and air-fluid levels are typical findings. Contrast-enhanced CT scan may reveal underlying sinusitis, thickening of the superior ophthalmic vein, and irregular filling defects within the cavernous sinus; however, findings may be normal early in the disease course. An MRI using flow parameters and an MR venogram are more sensitive than a CT scan and are the imaging studies of choice to diagnose cavernous sinus thrombosis. Findings may include deformity of the internal carotid artery within the cavernous sinus, and an obvious signal hyperintensity within thrombosed vascular sinuses on all pulse sequences.Cerebral angiography can be performed, but it is invasive and not very sensitive. Orbital venography is difficult to perform, but it is excellent in diagnosing occlusion of the cavernous sinus.[11]
Differential diagnosis
- Orbital cellulitis
- Internal carotid artery aneurysm
- Stroke
- Migraine headache
- Allergic blepharitis
- Thyroid exophthalmos
- Brain tumor
- Meningitis
- Mucormycosis
- Trauma
Treatment
Recognizing the primary source of infection (i.e., facial cellulitis, middle ear, and sinus infections) and treating the primary source expeditiously is the best way to prevent cavernous sinus thrombosis.[12]
Antibiotics
Broad-spectrum intravenous antibiotics are used until a definite pathogen is found.
- Nafcillin 1.5 g IV q4h
- Cefotaxime 1.5 to 2 g IV q4h
- Metronidazole 15 mg/kg load followed by 7.5 mg/kg IV q6h
Vancomycin may be substituted for nafcillin if significant concern exists for infection by methicillin-resistant Staphylococcus aureus or resistant Streptococcus pneumoniae.[13] Appropriate therapy should take into account the primary source of infection as well as possible associated complications such as brain abscess, meningitis, or subdural empyema.
All people with CST are usually treated with prolonged courses (3–4 weeks) of IV antibiotics. If there is evidence of complications such as intracranial suppuration, 6–8 weeks of total therapy may be warranted.
All patients should be monitored for signs of complicated infection, continued sepsis, or septic emboli while antibiotic therapy is being administered.
Heparin
Anticoagulation with heparin is controversial. Retrospective studies show conflicting data. This decision should be made with subspecialty consultation.[14] One systematic review concluded that anticoagulation treatment appeared safe and was associated with a potentially important reduction in the risk of death or dependency.[15]
Steroids
Steroid therapy is also controversial in many cases of CST.[16][17][18][19] However, corticosteroids are absolutely indicated in cases of pituitary insufficiency. Corticosteroid use may have a critical role in patients with Addisonian crisis secondary to ischaemia or necrosis of the pituitary that complicates CST.[20][21]
Surgery
Surgical drainage with sphenoidotomy is indicated if the primary site of infection is thought to be the sphenoidal sinuses.[22]
Prognosis
Cavernous sinus thrombosis has a mortality rate of less than 20% in areas with access to antibiotics. Before antibiotics were available, the mortality was 80–100%. Morbidity rates also dropped from 70% to 22% due to earlier diagnosis and treatment.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 "Cavernous sinus thrombosis". nhs.uk. 14 May 2018. Archived from the original on 10 October 2017. Retrieved 7 April 2022.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 "Cavernous Sinus Thrombosis - Eye Disorders". Merck Manuals Professional Edition. Archived from the original on 30 October 2021. Retrieved 7 April 2022.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Plewa, MC; Tadi, P; Gupta, M (January 2022). "Cavernous Sinus Thrombosis". PMID 28846357.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Cavernous Sinus Thrombosis". National Center for Biotechnology Information, U.S. National Library of Medicine. Archived from the original on 13 April 2021. Retrieved 7 July 2021.
- ↑ 5.0 5.1 "Cavernous sinus thrombosis: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Archived from the original on 5 July 2016. Retrieved 27 May 2016.
- ↑ 6.0 6.1 "Cavernous Sinus Thrombosis - Eye Disorders". Archived from the original on 2010-11-29. Retrieved 2021-07-18.
- ↑ Zhang J, Stringer MD (July 2010). "Ophthalmic and facial veins are not valveless". Clin. Experiment. Ophthalmol. 38 (5): 502–10. doi:10.1111/j.1442-9071.2010.02325.x. PMID 20491800.
- ↑ Brismar, G; Brismar, J (February 1977). "Aseptic thrombosis of orbital veins and cavernous sinus. Clinical symptomatology". Acta Ophthalmologica. 55 (1): 9–22. doi:10.1111/j.1755-3768.1977.tb06091.x. PMID 576549.
- ↑ "Guidelines Cavernous sinus thrombosis" (PDF). Archived (PDF) from the original on 2017-08-29. Retrieved 2021-07-18.
- ↑ "Cavernous Sinus Thrombosis". National Center for Biotechnology Information, U.S. National Library of Medicine. Archived from the original on 13 April 2021. Retrieved 7 July 2021.
- ↑ "Cavernous Sinus Thrombosis". National Center for Biotechnology Information, U.S. National Library of Medicine. Archived from the original on 13 April 2021. Retrieved 7 July 2021.
- ↑ "Cellulitis". The Lecturio Medical Concept Library. Archived from the original on 14 October 2021. Retrieved 7 July 2021.
- ↑ Munckhof WJ, Krishnan A, Kruger P, Looke D (April 2008). "Cavernous sinus thrombosis and meningitis from community-acquired methicillin-resistant Staphylococcus aureus infection". Intern Med J. 38 (4): 283–7. doi:10.1111/j.1445-5994.2008.01650.x. PMID 18380704.
- ↑ Bhatia, K; Jones, NS (September 2002). "Septic cavernous sinus thrombosis secondary to sinusitis: are anticoagulants indicated? A review of the literature". The Journal of Laryngology and Otology. 116 (9): 667–76. doi:10.1258/002221502760237920. PMID 12437798.
- ↑ Coutinho, J; de Bruijn, SF; Deveber, G; Stam, J (2011). "Anticoagulation for cerebral sinus thrombosis". Cochrane Database Syst Rev (CD002005): CD002005. doi:10.1002/14651858.cd002005.pub2. PMC 7065450. PMID 21833941.
- ↑ Southwick, FS; Richardson EP, Jr; Swartz, MN (March 1986). "Septic thrombosis of the dural venous sinuses". Medicine. 65 (2): 82–106. doi:10.1097/00005792-198603000-00002. PMID 3512953. S2CID 38338711.
- ↑ Gallagher, RM; Gross, CW; Phillips, CD (November 1998). "Suppurative intracranial complications of sinusitis". The Laryngoscope. 108 (11 Pt 1): 1635–42. doi:10.1097/00005537-199811000-00009. PMID 9818818.
- ↑ Clifford-Jones, RE; Ellis, CJ; Stevens, JM; Turner, A (1 December 1982). "Cavernous sinus thrombosis". Journal of Neurology, Neurosurgery & Psychiatry. 45 (12): 1092–1097. doi:10.1136/jnnp.45.12.1092. PMC 2164682. PMID 20784555.
- ↑ Igarashi, H; Igarashi, S; Fujio, N; Fukui, K; Yoshida, A (1995). "Magnetic resonance imaging in the early diagnosis of cavernous sinus thrombosis". Ophthalmologica. 209 (5): 292–6. doi:10.1159/000310635. PMID 8570157.
- ↑ Silver, HS; Morris, LR (May 1983). "Hypopituitarism Secondary to Cavernous Sinus Thrombosis". Southern Medical Journal. 76 (5): 642–646. doi:10.1097/00007611-198305000-00027. PMID 6302919. S2CID 45343762.
- ↑ Sahjpaul, RL; Lee, DH (April 1999). "Infratentorial subdural empyema, pituitary abscess, and septic cavernous sinus thrombophlebitis secondary to paranasal sinusitis: case report". Neurosurgery. 44 (4): 864–6, discussion 866–8. doi:10.1097/00006123-199904000-00101. PMID 10201313.
- ↑ Kozłowski, Z; Mazerant, M; Skóra, W; Dabrowska, K (2008). "[Sphenoidotomy--the treatment of patients with isolated sphenoid sinus diseases]". Otolaryngologia Polska. 62 (5): 582–6. doi:10.1016/S0030-6657(08)70319-6. PMID 19004262.
Further reading
- Wald, ER (June 2007). "Periorbital and orbital infections". Infectious Disease Clinics of North America. 21 (2): 393–408, vi. doi:10.1016/j.idc.2007.03.008. PMID 17561075.
- Osborn, Melissa K; Steinberg, James P (January 2007). "Subdural empyema and other suppurative complications of paranasal sinusitis". The Lancet Infectious Diseases. 7 (1): 62–67. doi:10.1016/S1473-3099(06)70688-0. PMID 17182345.
External links
| Classification | |
|---|---|
| External resources |