Toxic encephalopathy
| Toxic encephalopathy | |
|---|---|
Toxic encephalopathy is a neurologic disorder caused by exposure to neurotoxic organic solvents such as toluene, following exposure to heavy metals such as manganese, as a side effect of melarsoprol treatment for African trypanosomiasis, adverse effects to prescription drugs, or exposure to extreme concentrations of any natural toxin such as cyanotoxins found in shellfish or freshwater cyanobacteria crusts. Toxic encephalopathy can occur following acute or chronic exposure to neurotoxicants, which includes all natural toxins. Exposure to toxic substances can lead to a variety of symptoms, characterized by an altered mental status, memory loss, and visual problems. Toxic encephalopathy can be caused by various chemicals, some of which are commonly used in everyday life, or cyanotoxins which are bio-accumulated from harmful algal blooms (HABs) which have settled on the benthic layer of a waterbody. Toxic encephalopathy can permanently damage the brain and currently treatment is mainly just for the symptoms.
Signs and symptoms
"Encephalopathy" is a general term describing brain malfunctions and "toxic" asserts that the malfunction is caused by toxins on the brain. The most prominent characteristic of toxic encephalopathy is an altered mental status. Acute intoxication is a reversible symptom of exposure to many synthetic chemical neurotoxicants. Acute intoxication symptoms include lightheadedness, dizziness, headache and nausea, and regular cumulative exposure to these neurotoxicants over a number of years puts the individual at high risk for developing toxic encephalopathy. Chronic exposure to low levels of neurotoxic chemicals can also cause reversible changes in mood and affect which resolve with cessation of exposure. Acute and chronic toxic encephalopathy on the other hand, are persistent changes in neurological function that typically occur with exposure to higher concentrations and longer durations respectively. The symptoms of acute and chronic toxic encephalopathy do not resolve with cessation of exposure and can include memory loss, dementia, small personality changes/increased irritability, insidious onset of concentration difficulties, headache, lightheadedness, ataxia, involuntary movements (parkinsonism), fatigue, seizures, arm strength problems, and depression.[1] A paper by Feldman and colleagues described neurobehavioral effects in a 57-year-old house painter with regular exposure to large amounts of solvents.[2]
Magnetic Resonance Imaging (MRI) analyses have also demonstrated increased rates of dopamine synthesis in the putamen, reduced anterior and total corpus callosum volume, demyelination in the parietal white matter, basal ganglia, and thalamus, as well as atypical activation of frontal areas of the brain due to neural compensation.[citation needed]
The regions of interest on SPECT brain imaging include a majority of all cortical regions, and the globus pallidus in Carbon monoxide poisoning. Based on medical literature on SPECT brain imaging, signature patterns for toxic encephalopathy is a nonspecific patchy, diffuse pattern on the cortex, and sometimes is shown in subcortical regions, if exposure was severe.[citation needed]
A thorough and standard diagnostic process is paramount with toxic encephalopathy, including a careful occupational, medication and medical history, standardized imaging and neuropsychological testing.[citation needed]
Causes
In addition, chemicals, such as lead, that could instigate toxic encephalopathy are sometimes found in everyday products such as prescription drugs, cleaning products, building materials, pesticides, air fresheners, and even perfumes. These harmful chemicals can be inhaled (in the case of air fresheners) or applied (in the case of perfumes).[3][4] The substances diffuse into the brain rapidly, as they are lipophilic and readily transported across the blood–brain barrier. This is a result of increased membrane solubility and local blood flow, with central nervous system (CNS) solvent uptake being further increased with high levels of physical activity.[5] When they are not detoxified immediately, the symptoms of toxic encephalopathy begin to emerge.[4] However, in chronic situations, these effects may not become severe enough to be noticed until much later. Increased exposure time and increased concentration of the chemicals will worsen the effects of toxic encephalopathy, due to the associated structural CNS damage and direct functional impairment consequences.[5]
Subacute toxic encephalopathies are challenging to identify due to their often insidious tempo of evolution, nonspecific manifestations, relative infrequency as individual entities, and frequent lack of specific diagnostic testing. Yet they are crucial to recognize in aggregate, subacute toxic encephalopathies are a common problem that can lead to severe, irreversible harm if not diagnosed and treated efficiently. This article reviews the clinically relevant aspects of some of the more important subacute toxic encephalopathy syndromes caused by inorganic toxins, carbon monoxide (CO), anti- biotics, antineoplastic agents, and psychiatric medications.[6]
All therapeutic interventions are double-edged swords with benefits and adverse effects, and pharmacotherapy is not an exception. Shortly after the introduction of conventional antipsychotic drugs into clinical practice, relatively rare but serious complications with hyperthermia, muscle rigidity, autonomic instability, and disturbed mental status were recognized to develop in some patients treated with antipsychotics. This type of encephalopathy induced by the use of antipsychotics was referred to as neuroleptic malignant syndrome (NMS), and almost all physicians prescribing antipsychotics are nowadays aware of this adverse phenomenon. Another well-known type of encephalopathy associated with psychotropic drug therapy is serotonin toxicity (ST) or serotonin syndrome (SS), which is characterized by autonomic and neuromuscular symptoms and altered mental status. In contrast with the idiosyncratic nature of NMS, ST is a spectrum pathophysiological state assumed to derive from excess serotonergic neural transmission caused by serotonin-related psychotropic agents. In these two decades, pharmacotherapy with psychotropic drugs for patients with mental illness has been dramatically changed, and classical prototypal antipsychotics and antidepressants have been replaced with atypical antipsychotics and selective serotonin reuptake inhibitors (SSRIs), respectively. These newly developed psychotropic drugs are generally safer and more tolerable than older drugs. However, atypical antipsychotics are not free of the risk of development of NMS, and the explosive prevalence of SSRIs prescribed not only for depression but also for a number of psychiatric diagnoses such as anxiety, eating, impulse-control, and personality disorders may increase the incidence of ST. Therefore, these two pathological states still remain as major adverse effects of psychotropic drugs involving altered functioning of the central nervous system (CNS), to which all clinicians prescribing psychoactive drugs should pay attention. The popularity of SSRIs also increased the case reports of patients with discontinuation syndrome, which sometimes includes CNS symptoms like anxiety and irritability. In this chapter, the author provides a comprehensive overview of the above- mentioned adverse effects affecting the CNS function associated with psychotropic pharmacotherapy. In addition, several other pathological conditions potentially causing encephalopathic symptoms in psychiatric patients treated with psychotropic drugs, e.g., hyponatremia, valproate-induced hyperammonemia, transient splenial lesion of the corpus callosum, and so on, are also described.[citation needed]
Fume events on aircraft have been linked to cases of toxic encephalopathy, for example in the case of JetBlue Captain Andrew Myers, who as a result of exposure needed a cane to walk, experienced tremors and struggled to speak. In the following year, the Federal Aviation Administration revoked Myers' medical certificate; the workers compensation board agreed that Myers experienced brain damage as a result of the event.[7]
Diagnosis
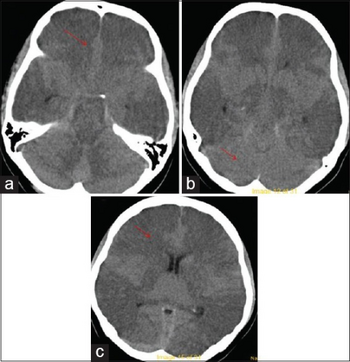
Rapid diagnosis is important to attempt to prevent further damage to the brain and further neurologic deficits. It is a diagnosis of exclusion, so a full work up for other possible etiologies (hepatic, uremic, infectious, oncologic) should be performed. In addition to the neurological examination, diagnostic testing could include MRI, PET or SPECT brain imaging, EEG, QEEG and most importantly, neuropsychological testing. Screening for heavy metals, as well as other toxins, should be done immediately as those are some of the most common causes and the patient can then remove themselves from the dangerous environment. In addition, a full examination of blood (CBC) and metabolites (CMP) should be done.[citation needed]
Treatment
Treatment is mainly for the symptoms that toxic encephalopathy causes, and vary depending on how severe the case is. Diet changes and nutritional supplements may help some patients. To reduce or halt seizures, anticonvulsants may be prescribed. Dialysis or organ replacement surgery may be needed in some severe cases.[8]
Lifelong abstinence from alcohol, a well-established neurotoxin and cause of the condition, is encouraged to prevent further loss of neurocognitive function.[citation needed]
Management of affected individuals consists of immediate removal from exposure to the toxic substance(s), treatment of the common clinical manifestation of depression if present, and counselling for the provision of life strategies to help cope with the potentially debilitating condition.[5]
Prognosis
Toxic encephalopathy is often irreversible. If the source of the problem is treated by removing the toxic chemical from the system, further damage can be prevented, but prolonged exposure to toxic chemicals can quickly destroy the brain.[9] Long-term studies have demonstrated residual cognitive impairment (primarily attention and information-processing impairment resulting in dysfunction in working memory) up to 10 years following cessation of exposure.[5] Severe cases of toxic encephalopathy can be life-threatening.[10]
Research
Research is being done by organizations such as NINDS (National Institute of Neurological Disorders and Stroke) on what substances can cause encephalopathy, why they do this, and eventually how to protect, treat, and cure the brain from this condition.[11]
See also
Notes
- ↑ Ratner MH, Feldman RG, and White RF: Neurobehavioral Toxicology. In: Ramachandran V.S. (ed); Encyclopedia of the Human Brain. New York, Elsevier Science, Vol. 3, pp 423-439, 2002.
- ↑ Feldman, R G; Ratner, M H; Ptak, T (May 1999). "Chronic toxic encephalopathy in a painter exposed to mixed solvents". Environmental Health Perspectives. 107 (5): 417–422. doi:10.1289/ehp.99107417. PMC 1566426. PMID 10210698.
- ↑ "National Toxic Encephalopathy Foundation". Archived from the original on 2019-06-28. Retrieved 2009-03-30.
- ↑ 4.0 4.1 Rogers, Sherry (1996). "Toxic Brain Encephalopathy". TOTAL WELLNESS Newsletter. Prestige Publishing. Archived from the original on 2018-11-06. Retrieved 2009-04-21.
- ↑ 5.0 5.1 5.2 5.3 Baker, E. (2008). Chronic toxic encephalopathy caused by occupational solvent exposure. Annals of Neurology. 63(5): 545-547
- ↑ Lerner, David P.; Tadevosyan, Aleksey; Burns, Joseph D. (November 2020). "Toxin-Induced Subacute Encephalopathy". Neurologic Clinics. 38 (4): 799–824. doi:10.1016/j.ncl.2020.07.006. PMID 33040862. S2CID 222301922.
- ↑ Feldman, Kiera. "'We are slowly being poisoned.' How toxic fumes seep into the air you breathe on planes". Los Angeles Times. Archived from the original on 2022-07-18. Retrieved 2022-08-04.
- ↑ "Is there any treatment?". Disorders A-Z. National Institute of Neurological Disorders and Stroke. 2007-02-12. Archived from the original on 2009-03-23. Retrieved 2009-04-12.
- ↑ "What is the prognosis?". Disorders A-Z. National Institute of Neurological Disorders and Stroke. 2007-02-12. Archived from the original on 2009-03-23. Retrieved 2009-04-12.
- ↑ Upledger, John (July 2004). "Toxic Brain Injury(Encephalopathy)". Massage Today. MPA. Archived from the original on 2018-01-19. Retrieved 2009-04-12.
- ↑ "What research is being done?". Disorders A-Z. National Institute of Neurological Disorders and Stroke. 2007-02-12. Archived from the original on 2009-03-23. Retrieved 2009-04-12.
References
- Lerner, David P.; Tadevosyan, Aleksey; Burns, Joseph D. (November 2020). "Toxin-Induced Subacute Encephalopathy". Neurologic Clinics. 38 (4): 799–824. doi:10.1016/j.ncl.2020.07.006. PMID 33040862. S2CID 222301922.
- Bradley, Walter (2004). Neurology in Clinical Practice (4 ed.). Taylor & Francis. ISBN 9997625897.
- Baker, Edward L. (May 2008). "Chronic toxic encephalopathy caused by occupational solvent exposure". Annals of Neurology. 63 (5): 545–547. doi:10.1002/ana.21394. PMID 18409195. S2CID 41546628.
- Feldman, R G; Ratner, M H; Ptak, T (May 1999). "Chronic toxic encephalopathy in a painter exposed to mixed solvents". Environmental Health Perspectives. 107 (5): 417–422. doi:10.1289/ehp.99107417. PMC 1566426. PMID 10210698.
- Encephalopathy Associated with Psychotropic Drug Therapy Yuji Odagaki Department of Psychiatry, Faculty of Medicine, Saitama Medical University Department of Psychiatry, Moro Hospital Japan
External links
- Pages with script errors
- All articles with unsourced statements
- Articles with unsourced statements from July 2021
- Articles with invalid date parameter in template
- Articles with unsourced statements from June 2022
- Articles with unsourced statements from December 2020
- Webarchive template wayback links
- Neurodegenerative disorders