Bursitis
| Bursitis | |
|---|---|
 | |
| Example of olecranon bursitis | |
| Specialty | Orthopedics |
| Symptoms | Swelling, difficulty moving, tenderness, pain[1] |
| Complications | Septic bursitis[2] |
| Types | Aseptic, septic[2] Acute, chronic[3] |
| Causes | Overuse, infection, trauma, inflammatory disorders[3] |
| Diagnostic method | Symptoms and examination[2] |
| Differential diagnosis | Arthritis, fractures, tendinitis, nerve problems[2] |
| Treatment | Rest, ice, compression, NSAIDs[2][3] |
| Prognosis | Generally good[3] |
| Frequency | Common[2] |
Bursitis is inflammation or swelling of one or more fluid filled sacs known as bursae.[3] These sacs are lined with a synovial membrane that produce a lubricating synovial fluid.[4] With bursitis there may be difficulty moving, tenderness, and pain in the area affected.[1] With bursitis of gradual onset pain may be absent.[3] Complications may include septic bursitis.[2]
Causes of bursitis include overuse, infection, trauma, and inflammatory disorders.[3] There are more than 150 bursae in the human body.[4] The most commonly affected are the prepatellar, olecranon, trochanteric, and retrocalcaneal.[2] The bursae are at locations where muscles, tendons, and other tissues slide across prominent areas of bone.[1] Normally they function to improve movement between tissues.[3] Diagnosis is generally based on symptoms and examination and may be supported by additional testing.[2][3] Other causes of similar symptoms include arthritis, fractures, tendinitis, and nerve problems.[2]
Treatment is typically with rest, ice, compression, and nonsteroidal anti-inflammatory medications (NSAIDs).[2][3] Steroid injections or surgery may less commonly be used.[2] Evidence for steroid injections in long term bursitis; however, is lacking as of 2020.[3] Bursitis is common with males and females affected equally.[2][3]
Signs and symptoms

Bursitis commonly affects superficial bursae. These include the subacromial, prepatellar, retrocalcaneal, and pes anserinus bursae of the shoulder, knee, heel and shin, etc. (see below).[4] Symptoms vary from localized warmth and erythema[4] to joint pain and stiffness, to stinging pain that surrounds the joint around the inflamed bursa. In this condition, the pain usually is worse during and after activity, and then the bursa and the surrounding joint becomes stiff the next morning.
Bursitis could possibly also cause a snapping, grinding or popping sound – known as snapping scapula syndrome – when it occurs in the shoulder joint. This is not necessarily painful.
Cause
There can be several concurrent causes. Trauma, auto-immune disorders, infection and iatrogenic (medicine-related) factors can all cause bursitis.[4] Bursitis is commonly caused by repetitive movement and excessive pressure. Shoulders, elbows and knees are the most commonly affected. Inflammation of the bursae may also be caused by other inflammatory conditions such as rheumatoid arthritis, scleroderma, systemic lupus erythematosus, and gout. Immune deficiencies, including HIV and diabetes, can also cause bursitis.[4] Infrequently, scoliosis can cause bursitis of the shoulders; however, shoulder bursitis is more commonly caused by overuse of the shoulder joint and related muscles.
Traumatic injury is another cause of bursitis. The inflammation irritates because the bursa no longer fits in the original small area between the bone and the functionary muscle or tendon. When the bone increases pressure upon the bursa, bursitis results. Sometimes the cause is unknown. It can also be associated with various other chronic systemic diseases.
Diagnosis
The diagnosis of bursitis can be done via a musculoskeletal ultrasound[5]
-
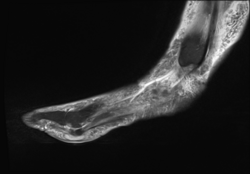
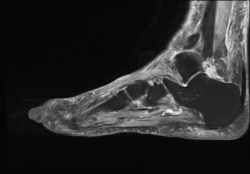
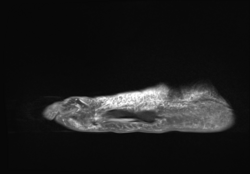
Adventitous bursitis
-
Adventitious bursitis
-
Adventitious bursitis
Types
The most common examples of this condition:
- Prepatellar bursitis, "housemaid's knee"[3]
- Infrapatellar bursitis, "clergyman's knee"[3]
- Trochanteric bursitis, giving pain over lateral aspect of hip
- Olecranon bursitis, "student's elbow", characterised by pain and swelling in the elbow[3]
- Subacromial bursitis, giving shoulder pain, is the most common form of bursitis.[6]
- Achilles bursitis
- Retrocalcaneal bursitis
- Ischial bursitis, "weaver's bottom"[3]
- Iliopsoas bursitis
- Anserine bursitis
Treatment
It is important to differentiate between infected and non-infected bursitis. People may have surrounding cellulitis and systemic symptoms include a fever. The bursa should be aspirated to rule out an infectious process.[4]
Bursae that are not infected can be treated symptomatically with rest, ice, elevation, physiotherapy, anti-inflammatory drugs and pain medication. Since bursitis is caused by increased friction from the adjacent structures, a compression bandage is not suggested because compression would create more friction around the joint. Chronic bursitis can be amenable to bursectomy and aspiration.[4] Bursae that are infected require further investigation and antibiotic therapy. Steroid therapy may also be considered.[4] In cases when all conservative treatment fails, surgical therapy may be necessary. In a bursectomy the bursa is cut out either endoscopically or with open surgery. The bursa grows back in place after a couple of weeks but without any inflammatory component.
See also
References
- ↑ 1.0 1.1 1.2 Hubbard, MJ; Hildebrand, BA; Battafarano, MM; Battafarano, DF (June 2018). "Common Soft Tissue Musculoskeletal Pain Disorders". Primary care. 45 (2): 289–303. doi:10.1016/j.pop.2018.02.006. PMID 29759125.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Aaron, DL; Patel, A; Kayiaros, S; Calfee, R (June 2011). "Four common types of bursitis: diagnosis and management". The Journal of the American Academy of Orthopaedic Surgeons. 19 (6): 359–67. doi:10.5435/00124635-201106000-00006. PMID 21628647.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 Williams, Christopher H.; Sternard, Britni T. (August 15, 2020.). "Bursitis". Bursitis. StatPearls Publishing. Archived from the original on December 1, 2020. Retrieved September 23, 2020.
{{cite book}}: Check date values in:|date=(help) - ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Vigorita, Vincent J.; Ghelman, Bernard; Mintz, Douglas (2008). Orthopaedic Pathology (Second ed.). Philadelphia: Lippincott Williams and Wilkins. p. 719. ISBN 978-0-7817-9670-5.
- ↑ "Bursitis". Medlineplus.gov. Archived from the original on 25 May 2021. Retrieved 27 April 2021.
- ↑ Fauci, Anthony S.; Langford, Carol A., eds. (2010). Harrison's Rheumatology (Second ed.). McGraw-Hill Professional Publishing; Digital Edition. p. 271. ISBN 9780071741460.
External links
| Classification | |
|---|---|
| External resources |
- Bursitis treatment Archived 2010-07-15 at the Wayback Machine from NHS Direct
- Questions and Answers about Bursitis and Tendinitis Archived 2015-01-04 at the Wayback Machine – US National Institute of Arthritis and Musculoskeletal and Skin Diseases