California encephalitis orthobunyavirus
| California encephalitis orthobunyavirus | |
|---|---|
| Other names: California encephalitis virus | |
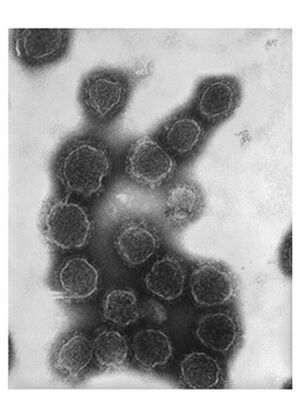 | |
| Transmission electron microscopy photograph of California encephalitis virus virions | |
| Specialty | Infectious disease |
| Symptoms | Fever, chills, nausea, vomiting, headache, lethargy and abdominal pain |
| Diagnostic method | ELISA technique |
| Differential diagnosis | Eastern Equine Encephalitis,St. Louis Encephalitis, Varicella zoster encephalitis, Fungal meningitis, Bacterial meningitis |
| Treatment | Supportive care, corticosteroids |
| Frequency | 75 cases per year |
California encephalitis orthobunyavirus type strain California encephalitis virus was discovered in Kern County, California, and causes encephalitis in humans.[1] Encephalitis is an acute inflammation of the brain that can cause minor symptoms, such as headaches, to more severe symptoms such as seizures. Mosquitoes serve as its carrier and for this reason this virus is known as an arbovirus [2]
California encephalitis orthobunyavirus belongs to the Bunyavirales order of viruses. The La Crosse Virus from the same genus is also a common cause of encephalitis in the United States. Other viruses with similar disease symptoms but genetically unrelated include: Saint Louis encephalitis and West Nile virus.[3][4][5]
Signs and symptoms
The incubation period of California encephalitis is usually 3–7 days. An early symptoms phase of 1–4 days commonly precedes the onset of encephalitis, manifesting as fever, chills, nausea, vomiting, headache, lethargy and abdominal pain.[6][7]
The encephalitis is characterized by fever, drowsiness, and lack of mental alertness and orientation.Cases of seizures occur in significant percentage of children, while focal neurologic findings, like focal motor abnormalities and paralysis, irregular and abnormal reflexes develop in at a lower percentage of children. Some individuals may go into a coma.[8][9]
The total duration of illness rarely exceeds 10–14 days. Recurrent unprovoked seizures occur even after the illness has passed develops in 20% of patients, especially those who had seizures during the acute illness. In adults, infection is asymptomatic, which means that the patient is a carrier of the infection, but experiences no symptoms or only mild feverish illness.[6]
The mortality rate is less than 1% and most patients with encephalitis clinical symptoms recover completely. Up to 20% of patients develop behavioral problems or recurrent seizures.[6]
Cause
| California encephalitis orthobunyavirus | |
|---|---|
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Ellioviricetes |
| Order: | Bunyavirales |
| Family: | Peribunyaviridae |
| Genus: | Orthobunyavirus |
| Species: | California encephalitis orthobunyavirus
|
In terms of the etiology of California encephalitis virus we find that CE is due to a group of viruses of the genus Bunyavirus and the family Bunyaviridae. They are spherical, lipid membrane–enclosed viruses ( 90-110 nm ), and have 3 negative-sense RNA segments.[10]
Transmission of the virus occurs via Aedes. triseriatus, Aedes. albopictus and Aedes japonicus as vectors[10]
The mosquito acquires the virus via a blood meal[10]
The genome size is 12.5Kb, it has 4 genes and 3 viral segments[11][12]
Pathophysiology
Initial infection by the virus and primary spread of the virus causes the onset of non-specific symptoms such as headache and fever. Secondary spread and the multiplication of the virus in the CNS causes symptoms such as stiff neck, lethargy and seizures. It then can result in encephalitis, when inflammation of the brain, produced by infection by the virus, damages nerve cells, which affects signaling of the brain to the body[6][13]
After the virus enters the body via a mosquito bite, the virus undergoes local replication at the skin site where virus entered the body. A primary spread of virus occurs, with seeding of the reticuloendothelial system, mainly in the liver, spleen, and lymph nodes.[6] With the ongoing replication of the virus a secondary spread occurs, with the seeding of the CNS. Not all the cases reach this stage, depending on the efficiency of viral replication at the different stages and the degree of virus spread. The California encephalitis virus invades the CNS through either the cerebral capillary endothelial cells or the choroid plexus.[6]
Diagnosis

In terms of the evaluation of California encephalitis virus we find that via ELISA technique specific immunoglobulin M and neutralizing antibodies can be identified[8]Additionally, the following are also used:[8]
- Electroencephalography
- CBC
Differential diagnosis
The DDx for California encephalitis virus are as follows:[8]
- Eastern Equine Encephalitis
- St. Louis Encephalitis
- Varicella zoster encephalitis
- Fungal meningitis
- Bacterial meningitis
- Carcinomatous meningitis
- Aseptic meningitis
Treatment

Treatments are given to manage the symptoms the patient is having.[14] In patients who are very sick, supportive treatment, such as mechanical ventilation, is equally important. Corticosteroids are used to reduce brain swelling and inflammation. Sedatives may be needed for irritability or restlessness. Acetaminophen is used for fever and headache. Anticonvulsants are used to prevent seizures. If brain function is severely affected, interventions like physical therapy and speech therapy may be needed after the illness is controlled.[8][9]
Epidemiology
Factors influencing the transmission and control of arboviral encephalitis, in general, include: the season, geographical location, patient age, and the regional climate. There are approximately 75 cases reported per year.[6] In the US the highest occurrence is in the Midwestern states, with most cases occurring in the late summer to early fall. Outdoor activities, especially in woodland areas, are associated with an increased risk of infection.[6]
History

It was first discovered and isolated in 1943, from mosquitoes collected in Kern County, California. Two years later the first human cases of encephalitis were attributed to this new virus. Three cases in total were reported, and all three cases were in residents of Kern County in the Central Valley of California.[15]
In all three cases there was strong laboratory evidence confirming infection, due to the presence of neutralizing antibodies linked to California encephalitis.[6]
Since then, most cases of encephalitis have been associated with the La Crosse virus, and California encephalitis is a rare cause of disease in the Western world.[6]
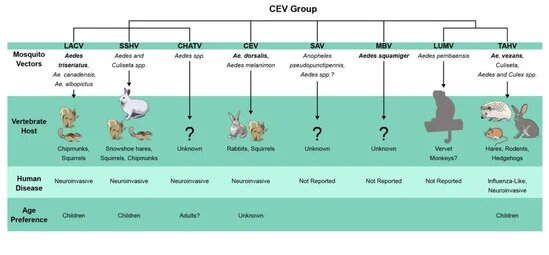
The original California Encephalitis virus was isolated and put alongside fifteen other related viruses that are now categorized as the "California serogroup". From 1996 to 1998, approximately three times as many reported human cases of arboviral encephalitis were caused by California serogroup viruses than were reported for western equine encephalomyelitis viruses, St. Louis encephalitis, and eastern equine encephalomyelitis viruses combined.[6]
References
- ↑ Hammon, W. M.; Reeves, W. C. (November 1952). "California Encephalitis Virus, a Newly Described Agent". California Medicine. 77 (5): 303–309. PMC 1521486. PMID 13009479.
- ↑ "Encephalitis". National Institute of Neurological Disorders and Stroke. Archived from the original on 25 March 2023. Retrieved 14 April 2023.
- ↑ Young, Paul R.; Ng, Lisa F. P.; Hall, Roy A.; Smith, David W.; Johansen, Cheryl A. (1 January 2014). "14 - Arbovirus Infections". Manson's Tropical Infectious Diseases (Twenty-third Edition). W.B. Saunders. pp. 129–161.e3. ISBN 978-0-7020-5101-2. Archived from the original on 18 December 2022. Retrieved 16 April 2023.
- ↑ Simon, Leslie V.; Kong, Erwin L.; Graham, Charles (2023). "St. Louis Encephalitis". StatPearls. StatPearls Publishing. Archived from the original on 23 March 2023. Retrieved 17 April 2023.
- ↑ "Symptoms, Diagnosis, & Treatment | West Nile Virus | CDC". www.cdc.gov. 14 October 2022. Archived from the original on 26 October 2017. Retrieved 17 April 2023.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 Eldridge, B. F.; Glaser, C.; Pedrin, R. E.; Chiles, R. E. (March 2009). "The First Reported Case of California Encephalitis in More Than 50 Years". Emerging Infectious Diseases. 7 (3): 451–452. doi:10.3201/eid0703.010316. PMC 2631795. PMID 11384526.
- ↑ "Other Arbovirus Infections - Infectious Diseases". MSD Manual Professional Edition. Archived from the original on 17 April 2023. Retrieved 17 April 2023.
- ↑ 8.0 8.1 8.2 8.3 8.4 "California Encephalitis Workup: Approach Considerations, CT Scanning and MRI". Medscape. 15 July 2021. Archived from the original on 8 December 2022. Retrieved 6 April 2023.
- ↑ 10.0 10.1 10.2 "California Encephalitis: Background, Etiology, Epidemiology". Medscape. 15 July 2021. Archived from the original on 8 January 2019. Retrieved 14 April 2023.
- ↑ "California encephalitis virus". NCBI. Retrieved 14 April 2023.
- ↑ "California encephalitis orthobunyavirus". pubchem.ncbi.nlm.nih.gov. Archived from the original on 14 April 2023. Retrieved 14 April 2023.
- ↑ "California Encephalitis Clinical Presentation: History and Physical Examination, Complications". emedicine.medscape.com. Archived from the original on 29 November 2022. Retrieved 19 April 2023.
- ↑ Kaneshiro, N. K. (2010-07-26). "Encephalitis". Times Health Guide. The New York Times. Archived from the original on 2013-05-29. Retrieved 2012-02-25.
- ↑ Anderson, W. E.; Soliman, E.; Perez, N.; Gotuzzo, E. (2011-07-17). "California Encephalitis". Medscape Reference. WebMD. Archived from the original on 2012-02-02. Retrieved 2012-02-25.
External links
| Classification |
|---|