Nabothian cyst
| Nabothian cyst | |
|---|---|
 | |
| Nabothian cyst | |
| Frequency | Common[1] |
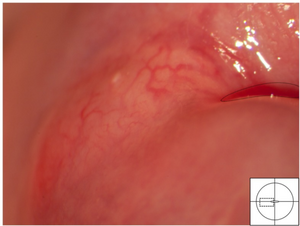
A nabothian cyst (or nabothian follicle) is a mucus-filled cyst on the surface of the cervix.[1] Generally there are no symptoms, but it may appear like a polyp or have an associated discharge.[1] It is mostly seen in females who have had multiple births.[1][2]
They are most often caused when stratified squamous epithelium of the ectocervix (portion nearest to the vagina) grows over the simple columnar epithelium of the endocervix (portion nearest to the uterus). This tissue growth can block the cervical crypts (subdermal pockets usually 2–10 mm in diameter), trapping cervical mucus inside the crypts.
Presentation
Nabothian cysts appear most often as firm bumps on the cervix's surface. A woman may notice the cyst when inserting a diaphragm or cervical cap, or when checking the cervix as part of fertility awareness.[3][unreliable medical source?] A health care provider may notice the cysts during a pelvic exam.
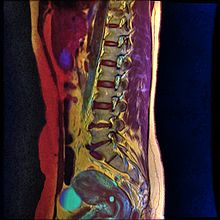
Nabothian cysts are also incidentally found during MRI imaging. During the healing process of chronic cervicitis, squamous epithelium of ectocervix proliferates and enter the cervical canal (endocervix), covering and obstructing the columnar epithelium of endocervical glands. Thus, retention of mucus in the endocervical glands causes cyst formation. The size of the cyst may vary from a few millimetres to 4 cm in diameter.[4]
Diagnosis

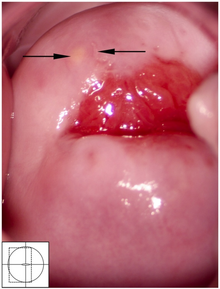
If a cyst has an unusual appearance, a colposcopy will be performed to rule out other diagnoses.[5] If the blood vessels are short, comma-like or corkscrew-shaped and bleed on contact, then the cyst may be a very rare mucin-producing carcinoma of the cervix.[5] Magnetic resonance imaging is used to distinguish cancer from the typical nabothian cyst.[5]
T1-weighted MRI imaging would show intermediate to high intensity while T2-weighted imaging would show high signal intensity. Findings of solid components separating multiple cysts would be suggestive of adenoma malignum (a form of cervical cancer).[4]
Treatment
Nabothian cysts usually require no treatment and frequently resolve on their own.[5] Cryotherapy has been used to treat nabothian cysts but is rarely necessary.[5] Very rarely a cyst may be so large that it prevents a clinician from performing a pap smear, in which case the clinician may puncture the cyst with a needle and drain it.[5] If nabothian cysts occur with chronic cervicitis (inflammation of the cervix) then the underlying cause of the inflammation must be treated.[6]
Eponym
Nabothian cysts are also known as nabothian follicles, mucinous retention cysts, or epithelial inclusion cysts. They are named after German anatomist Martin Naboth (1675–1721), who wrote about them in a 1707 treatise titled De sterilitate mulierum. However, they were earlier described by French surgeon Guillaume Desnoues (1650–1735).[7][better source needed] Since it is a derived term, nabothian is not spelled with a capital first letter.
See also
References
- ↑ 1.0 1.1 1.2 1.3 WHO Classification of Tumours Editorial Board, ed. (2020). "6. Tumours of the uterine cervix: Nabothian cyst". Female genital tumours: WHO Classification of Tumours. Vol. 4 (5th ed.). Lyon (France): International Agency for Research on Cancer. p. 354. ISBN 978-92-832-4504-9. Archived from the original on 2022-06-17. Retrieved 2022-08-03.
- ↑ AlJulaih, Ghadeer H.; Puckett, Yana (2023). "Nabothian Cyst". StatPearls. StatPearls Publishing. Archived from the original on 2023-10-22. Retrieved 2023-10-22.
- ↑ Weschler, Toni (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. pp. 227–228. ISBN 0-06-093764-5.
- ↑ 4.0 4.1 Okamoto, Yoshikazu; Tanaka, Yumiko O.; Nishida, Masato; Tsunoda, Hajime; Yoshikawa, Hiroyuki; Itai, Yuji (March 2003). "MR Imaging of the Uterine Cervix: Imaging-Pathologic Correlation". RadioGraphics. 23 (2): 425–445. doi:10.1148/rg.232025065. ISSN 0271-5333. PMID 12640157.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Women's gynecologic health. Schuiling, Kerri Durnell., Likis, Frances E. Sudbury, Mass.: Jones and Bartlett. 2006. p. 570. ISBN 0763747173. OCLC 57731391.
{{cite book}}: CS1 maint: others (link) - ↑ Adam., Ostrzenski (2002). Gynecology : integrating conventional, complementary, and natural alternative therapy. Philadelphia: Lippincott Williams & Wilkins. p. 235. ISBN 0781727618. OCLC 47013933.
- ↑ "Nabothian Cysts". Who Named It?. 2007. Archived from the original on 2019-11-13. Retrieved 2007-06-22.
External links
| Classification | |
|---|---|
| External resources |