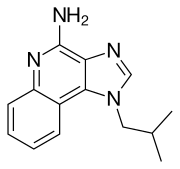
Imiquimod
 | |
| Names | |
|---|---|
| Trade names | Aldara, others[1] |
| Other names | 1-isobutyl-1H-imidazo[4,5-c]quinolin-4-amine |
| |
| Clinical data | |
| Main uses | Genital warts, superficial basal cell carcinoma, molluscum contagiosum, actinic keratosis[2][3] |
| Side effects | Swelling, redness, skin peeling, blistering at the site[2] |
| Pregnancy category | |
| Routes of use | Topical |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a698010 |
| Legal | |
| License data | |
| Legal status | |
| Pharmacokinetics | |
| Elimination half-life | 30 hours (topical dose), 2 hours (subcutaneous dose) |
| Chemical and physical data | |
| Formula | C14H16N4 |
| Molar mass | 240.310 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Imiquimod, sold under the brand name Aldara among others, is a medication used to treat genital warts, superficial basal cell carcinoma, molluscum contagiosum, and actinic keratosis.[2][3] It is applied as a cream.[3]
Common side effects include swelling, redness, skin peeling, and blistering at the site.[2] Other side effects may include headaches, nausea, and muscle pains.[3] How it works is not clear; though it dose activate certain parts of the immune system.[2]
Imiquimod was approved for medical use in the United States in 1997.[2] It is available as a generic medication.[5] In the United Kingdom 12 doses costs the NHS about 50£.[3] This amount in the United States costs about 16 USD as of 2021.[5]
Medical uses
Imiquimod is a patient-applied cream prescribed to treat genital warts, Bowens disease (squamous cell carcinoma in situ), and, secondary to surgery, for basal cell carcinoma,[6][7] as well as actinic keratosis.[8]
Imiquimod 5% cream is indicated for the topical treatment of:
- external genital and perianal warts (condylomata acuminata) in adults;[9]
- small superficial basal-cell carcinomas (sBCCs) in adults;[9]
- clinically typical, non-hyperkeratotic, non-hypertrophic actinic keratoses (AKs) on the face or scalp in immunocompetent adults when size or number of lesions limit the efficacy and / or acceptability of cryotherapy and other topical treatment options are contraindicated or less appropriate.[9]
Imiquimod 3.75% cream is indicated for the topical treatment of clinically typical, non-hyperkeratotic, non-hypertrophic, visible or palpable actinic keratosis of the full face or balding scalp in immunocompetent adults when other topical treatment options are contraindicated or less appropriate.[10]
-
Imiquimod to actinic keratosis
-
Imiquimod to actinic keratosis
-
Imiquimod to actinic keratosis
Side effects
Side effects include local inflammatory reactions, such as blisters, a burning sensation, skin redness, dry skin, itching, skin breakdown, skin crusting or scabbing, skin drainage, skin flaking or scaling, skin ulceration, sores, swelling, as well as systemic reactions, such as fever, "flu-like" symptoms, headache, and tiredness.[8][11]
People who have had an organ transplant and are taking immune-suppressing drugs should not use imiquimod.[8]
Mechanism of action

Imiquimod yields profound antitumoral activity by acting on several immunological levels synergistically.[12] Imiquimod stimulates the innate immune system by activating toll-like receptor 7 (TLR7), commonly involved in pathogen recognition.[13][14] Cells activated by imiquimod via TLR-7 secrete cytokines (primarily interferon-α (IFN-α), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α)).[15] There is evidence that imiquimod, when applied to skin, can lead to the activation of Langerhans cells, which subsequently migrate to local lymph nodes to activate the adaptive immune system.[16] Other cell types activated by imiquimod include natural killer cells, macrophages and B-lymphocytes.[16]
Imiquimod exerts its effect by increasing levels of the opioid growth factor receptor (OGFr). In experiments, blocking OGFr function with siRNA technology resulted in loss of any antiproliferative effect of imiquimod.[17]
History
Scientists at 3M's pharmaceutical division discovered imiquimod as part of a program to discover inhibitors of herpes simplex virus replication based on a known adenine derivative.[18]: 369–372 3M obtained the first FDA approval for it in 1997 as a treatment for external genital and perianal warts under the brand, "Aldara".[19] In 2004, 3M obtained FDA approval to market imiquimod as a treatment for superficial basal cell carcinoma.[20]
In 2006, 3M sold its pharmaceutical business in the Americas to Graceway Pharmaceuticals, its European pharmaceutical business to Meda AB, and its pharmaceutical business in other territories to two private equity firms.[21]
Graceway declared bankruptcy in 2011, after the expiration of the patents on imiquimod, and its assets, including the rights to imiquimod branding and approvals in the Americas, were purchased by Medicis Pharmaceutical.[22]
Imiquimod 5% was approved for medical use in the European Union in September 1998.[9] Imiquimod 3.75% was approved for medical use in the European Union in August 2012.[10]
As of 2015, imiquimod is generic and is available worldwide under many brands.[1]
Society and culture
Cost
The cost of this medication in the U.S. is $52 (USD) for 24 cream(s) of topical cream 5% Imiquimod[23]
-
Imiquimod costs (US)
-
Imiquimod prescriptions (US)
Research
One randomized double-blind Phase III clinical study found clearance of genital warts (an FDA-approved indication) improved from 9% with placebo to 24.9% with 3.75% imiquimod cream applied for up to eight weeks.[24]
Imiquimod has been tested for treatment of molluscum contagiosum. Two large randomized controlled trials, however, found no evidence of effectiveness of imiquimod in treating children with molluscum contagiosum, and concerning adverse effects were also noted.[25] These disprove earlier anecdotal claims and smaller, less reliable studies.[26][27][28][29]
Imiquimod has also been tested for treatment of vulvar intraepithelial neoplasia,[30] vaginal intraepithelial neoplasia,[31] common warts (a 2012 Cochrane review found no randomized controlled trials),[32] plantar warts,[33] warts in people with suppressed immune systems,[34] flat warts on face and neck,[33] and warts under and around fingernails and toenails.[33] As of 2014, insufficient evidence exists to recommend treatment of warts (other than genital warts) with imiquimod, due to the small size of and lack of controls in existing studies.[35][33]
References
- ↑ 1.0 1.1 Drugs.com Drugs.com international listings for imiquimod Archived 2016-03-04 at the Wayback Machine Page accessed June 14, 2015
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 "Imiquimod Monograph for Professionals". Drugs.com. Archived from the original on 4 March 2016. Retrieved 19 July 2021.
- ↑ 3.0 3.1 3.2 3.3 3.4 BNF (80 ed.). BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 1352. ISBN 978-0-85711-369-6.
{{cite book}}: CS1 maint: date format (link) - ↑ 4.0 4.1 "Imiquimod topical Use During Pregnancy". Drugs.com. 29 May 2019. Archived from the original on 17 July 2020. Retrieved 14 July 2020.
- ↑ 5.0 5.1 "Imiquimod Prices, Coupons & Savings Tips". GoodRx. Archived from the original on 13 November 2016. Retrieved 19 July 2021.
- ↑ 'Imiquimod should be used for treatment of [superficial basal cell carcinoma] only when surgery is medically less appropriate ... .' USA Food And Drug Administration, 'FDA Approval for Imiquimod', [1] Archived 2015-04-06 at the Wayback Machine, current at 2011-Jan-1, accessed 2012-Oct-19
- ↑ American Cancer Society, Guide To Cancer Drugs, [2] Archived 2015-03-04 at the Wayback Machine (accessed 2014-Apr-28)
- ↑ 8.0 8.1 8.2 European Medicines Agency. First published Sept 14,2009, updated March 25, 2015. EMA Summary of Product Characteristics Archived 2017-09-25 at the Wayback Machine
- ↑ 9.0 9.1 9.2 9.3 "Aldara EPAR". European Medicines Agency (EMA). Archived from the original on 28 December 2020. Retrieved 14 July 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ↑ 10.0 10.1 "Zyclara EPAR". European Medicines Agency (EMA). Archived from the original on 15 July 2020. Retrieved 14 July 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ↑ PDR Health PDR: Aldara Archived 2021-04-28 at the Wayback Machine
- ↑ Schön, M.P; Schön, M (2007). "Imiquimod: Mode of action". British Journal of Dermatology. 157: 8–13. doi:10.1111/j.1365-2133.2007.08265.x. PMID 18067624. S2CID 36643157.
- ↑ Walter, Anne; Schäfer, Matthias; Cecconi, Virginia; Matter, Claudia; Urosevic-Maiwald, Mirjana; Belloni, Benedetta; Schönewolf, Nicola; Dummer, Reinhard; Bloch, Wilhelm; Werner, Sabine; Beer, Hans-Dietmar; Knuth, Alexander; Van Den Broek, Maries (2013). "Aldara activates TLR7-independent immune defence". Nature Communications. 4: 1560. Bibcode:2013NatCo...4.1560W. doi:10.1038/ncomms2566. PMID 23463003.
- ↑ Hemmi, Hiroaki; Kaisho, Tsuneyasu; Takeuchi, Osamu; Sato, Shintaro; Sanjo, Hideki; Hoshino, Katsuaki; Horiuchi, Takao; Tomizawa, Hideyuki; Takeda, Kiyoshi; Akira, Shizuo (2002). "Small anti-viral compounds activate immune cells via the TLR7 MyD88–dependent signaling pathway". Nature Immunology. 3 (2): 196–200. doi:10.1038/ni758. PMID 11812998. S2CID 1694900.
- ↑ Sauder, D.N. (2003). "Imiquimod: Modes of action". British Journal of Dermatology. 149: 5–8. doi:10.1046/j.0366-077x.2003.05628.x. PMID 14616337. S2CID 41274637.
- ↑ 16.0 16.1 Miller, R.L; Gerster, J.F; Owens, M.L; Slade, H.B; Tomai, M.a (1999). "Review Article Imiquimod applied topically: A novel immune response modifier and new class of drug". International Journal of Immunopharmacology. 21 (1): 1–14. doi:10.1016/s0192-0561(98)00068-x. PMID 10411278.
- ↑ Zagon IS, Donahue RN, Rogosnitzky M, McLaughlin PJ (August 2008). "Imiquimod upregulates the opioid growth factor receptor to inhibit cell proliferation independent of immune function". Exp. Biol. Med. (Maywood). 233 (8): 968–79. doi:10.3181/0802-RM-58. PMID 18480416. S2CID 35164284.
- ↑ Randall L. Halcomb. TLR-7 Agonists for the Treatment of Viral Hepatitis. Chapter 10 in Successful Strategies for the Discovery of Antiviral Drugs. Issue 32 of RSC drug discovery series. Eds Manoj C. Desai and Nicholas A. Meanwell. Royal Society of Chemistry, 2013. ISBN 9781849736572
- ↑ Centerwatch. Centerwatch:Aldara (imiquimod) Archived 2019-08-05 at the Wayback Machine Page accessed June 14, 2015
- ↑ National Cancer Institute. Updated: July 3, 2013 NCI: FDA Approval for Imiquimod Archived 2018-01-23 at the Wayback Machine
- ↑ 3M. November 9, 2006. Press release: 3M Reaches Agreements to Sell its Pharmaceuticals Business Archived 2019-08-21 at the Wayback Machine
- ↑ "Jennifer A. Johnson for the Phoenix Business Journal Nov 29, 2011". Archived from the original on December 23, 2011. Retrieved December 26, 2020.
- ↑ "Imiquimod topical Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 9 June 2016. Retrieved 1 April 2021.
- ↑ "Phase 3 Study of Imiquimod Creams in the Treatment of External Genital Warts - Study Results - ClinicalTrials.gov". clinicaltrials.gov. Archived from the original on 2021-04-28. Retrieved 2020-12-26.
- ↑ "Aldara (imiquimod) cream for topical use. Prescribing information". Archived from the original on 2013-11-02.
- ↑ Molluscum Contagiosum~treatment at eMedicine
- ↑ Theos, A. U.; Cummins, R; Silverberg, N. B.; Paller, A. S. (2004). "Effectiveness of imiquimod cream 5% for treating childhood molluscum contagiosum in a double-blind, randomized pilot trial". Cutis. 74 (2): 134–8, 141–2. PMID 15379366.
- ↑ Bayerl, C; Feller, G; Goerdt, S (2003). "Experience in treating molluscum contagiosum in children with imiquimod 5% cream". The British Journal of Dermatology. 149 Suppl 66: 25–9. doi:10.1046/j.0366-077x.2003.05631.x. PMID 14616342. S2CID 23728783.
- ↑ Arican, Ozer (2006). "Topical treatment of molluscum contagiosum with imiquimod 5% cream in Turkish children". Pediatrics International. 48 (4): 403–5. doi:10.1111/j.1442-200X.2006.02229.x. PMID 16911087. S2CID 2867793.
- ↑ Van Seters, Manon; Van Beurden, Marc; Ten Kate, Fiebo J.W.; Beckmann, Ilse; Ewing, Patricia C.; Eijkemans, Marinus J.C.; Kagie, Marjolein J.; Meijer, Chris J.M.; Aaronson, Neil K.; Kleinjan, Alex; Heijmans-Antonissen, Claudia; Zijlstra, Freek J.; Burger, Matthé P.M.; Helmerhorst, Theo J.M. (2008). "Treatment of Vulvar Intraepithelial Neoplasia with Topical Imiquimod". New England Journal of Medicine. 358 (14): 1465–73. doi:10.1056/NEJMoa072685. PMID 18385498.
- ↑ Buck, Henry W.; Guth, Kathy J. (2003). "Treatment of Vaginal Intraepithelial Neoplasia (Primarily Low Grade) with Imiquimod 5% Cream". Journal of Lower Genital Tract Disease. 7 (4): 290–3. doi:10.1097/00128360-200310000-00011. PMID 17051086. S2CID 44649376.
- ↑ Kwok, Chun Shing; Gibbs, Sam; Bennett, Cathy; Holland, Richard; Abbott, Rachel (2012). "Topical treatments for cutaneous warts". Cochrane Database of Systematic Reviews (9): CD001781. doi:10.1002/14651858.CD001781.pub3. PMID 22972052.
- ↑ 33.0 33.1 33.2 33.3 "Imiquimod for non-genital cutaneous warts". www.dpic.org. Archived from the original on 2020-12-01. Retrieved 2020-12-26.
- ↑ Harwood, C.A.; Perrett, C.M.; Brown, V.L.; Leigh, I.M.; Mcgregor, J.M.; Proby, C.M. (2005). "Imiquimod cream 5% for recalcitrant cutaneous warts in immunosuppressed individuals". British Journal of Dermatology. 152 (1): 122–129. doi:10.1111/j.1365-2133.2005.06322.x. PMID 15656812. S2CID 42369353. Archived from the original on 2021-06-24. Retrieved 2020-12-26.
- ↑ Ahn, Christine S.; Huang, William W. (2014). "Imiquimod in the Treatment of Cutaneous Warts: An Evidence-Based Review". American Journal of Clinical Dermatology. 15 (5): 387–99. doi:10.1007/s40257-014-0093-5. PMID 25186654. S2CID 26624740.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Pages using duplicate arguments in template calls
- Webarchive template wayback links
- CS1 maint: date format
- CS1: long volume value
- Drugs with non-standard legal status
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- Drug has EMA link
- Drugboxes which contain changes to watched fields
- Antiviral drugs
- Antineoplastic drugs
- Imidazoquinolines
- RTT




