Pseudohypertrophy
| Pseudohypertrophy | |
|---|---|
| Other names | false enlargement |
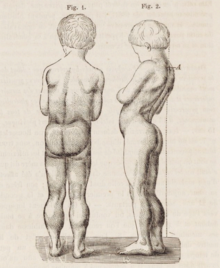 | |
| Drawing of seven-year-old boy with Duchenne muscular dystrophy. There is pseudohypertrophy of the lower limbs. | |
| Symptoms | Weakness |
| Causes | muscle disease, nerve disease |
Pseudohypertrophy, or false enlargement, is an increase in the size of an organ due to infiltration of a tissue not normally found in that organ.[1] It is commonly applied to enlargement of a muscle due to infiltration of fat or connective tissue,[2] famously in Duchenne muscular dystrophy. This is in contrast with typical muscle hypertrophy, in which the muscle tissue itself increases in size.[2] Because pseudohypertrophy is not a result of increased muscle tissue, the muscles look bigger but are actually atrophied and thus weaker.[2][3] Pseudohypertrophy is typically the result of a disease, which can be a disease of muscle or a disease of the nerve supplying the muscle.[2]
Causes of pseudohypertrophy include muscle diseases: dystrophinopathies, limb-girdle muscular dystrophies, metabolic myopathy, Dystrophic myotonias, Non-dystrophic myotonias, endocrine disorders, parasitic muscle conditions, amyloid and sarcoid myopathy, and granulomatous myositis.[2]
Neurological causes include radiculopathy, poliomyelitis, Charcot-Marie-Tooth disease, spinal muscular atrophy.[2]
In pseudohypertrophy where the atrophied muscle tissue has been infiltrated by fat tissue, upon palpitation the seemingly large muscles feel doughy.[3]
Not all muscles infiltrated by fat or other tissue are pseudohypertrophic. In muscular steatosis, sometimes the muscles may appear a normal or a slender size, even though the atrophied muscle has been infiltrated with fat tissue, such as the calf muscles in Bethlem myopathy 1.[4][5][6][7][8] In myosclerosis, the muscle is infiltrated with connective tissue and fibrosis, having a firm, "woody" feel upon palpitation, with the muscles appearing slender.[9][10]
Etymology
Pseudohypertrophy can be broken up into the following roots, suffixes, and prefixes:
- Pseudo means 'false' or 'fake'. The etymology is from the Greek word ψεύδω (pseúdō), which means to lie or deceive.
- hyper means 'extreme' or 'beyond normal'. The etymology is from the Greek word ὑπέρ (hupér), which means over, above; beyond, to the extreme.
- trophy means 'nourishment', or 'development'. The etymology is from the Greek word τροφή (trophḗ), which means food, nourishment.
The term was used by Duchenne de Boulogne in his description of Duchenne muscular dystrophy in one of his works "paralysie musculaire pseudo-hypertrophique."[11]
Other names
As well as being known as 'false enlargement,' when the muscle has been infiltrated by fat tissue, historically it has also been called muscular steatosis, pseudohypertrophic atrophy, lipomatous pseudohypertrophy, interstitial lipomatosis, lipomatous muscular dystrophy, or atrophia lipomatosa.[12] It is also known as fatty atrophy of muscle (not to be confused with fat atrophy, which is atrophy of adipose tissue), as muscle tissue is replaced by fat tissue, the actual muscle atrophies while the fat tissue replaces the bulk.[13]
References
- ^ Adami, John George (1908). The Principles of pathology (1 ed.). p. 540. Retrieved 23 April 2022.
- ^ a b c d e f Walters, J (October 2017). "Muscle hypertrophy and pseudohypertrophy". Practical Neurology. 17 (5): 369–379. doi:10.1136/practneurol-2017-001695. PMID 28778933. S2CID 6444771.
- ^ a b Tyler, Frank H. (1950-03-01). "STUDIES IN DISORDERS OF MUSCLE: III. "Pseudohypertrophy" of Muscle in Progressive Muscular Dystrophy and Other Neuromuscular Diseases". Archives of Neurology & Psychiatry. 63 (3): 425. doi:10.1001/archneurpsyc.1950.02310210071005. ISSN 0096-6754.
- ^ Nalini, A.; Gayathri, N. (2010-07-01). "Bethlem myopathy: A study of two families". Neurology India. 58 (4): 665–666. doi:10.4103/0028-3886.68684. ISSN 0028-3886. PMID 20739820.
- ^ Bönnemann, Carsten G. (2011-06-21). "The collagen VI-related myopathies: muscle meets its matrix". Nature Reviews. Neurology. 7 (7): 379–390. doi:10.1038/nrneurol.2011.81. ISSN 1759-4766. PMC 5210181. PMID 21691338.
- ^ Suh, B.C.; Choi, Y.C.; Kim, S.M.; Choi, B.O.; Shim, D.; Lee, D.H.; Sunwoo, I. (2006). "A Family of Bethlem Myopathy". Journal of the Korean Neurological Association. 24: 614–617. S2CID 74251729.
- ^ Souza, Paulo Victor Sgobbi de; Bortholin, Thiago; Pinheiro, Jhonatan Rafael Siqueira; Naylor, Fernando George Monteiro; Pinto, Wladimir Bocca Vieira de Rezende; Oliveira, Acary Souza Bulle (2017-10-01). "Collagen type VI-related myopathy". Practical Neurology. 17 (5): 406–407. doi:10.1136/practneurol-2017-001661. ISSN 1474-7758. PMID 28578317.
- ^ Telles, Juliana Aparecida Rhein; Voos, Mariana Calil; Anequini, Isabella Pessa; Favero, Francis Meire; Silva, Thiago Henrique; Caromano, Fátima Aparecida (June 2018). "Genetic and functional differences between Bethlem myopathy and Ullrich congenital muscular dystrophy - case studies". Cadernos de Pós-Graduação em Distúrbios do Desenvolvimento. 18 (1): 148–163. doi:10.5935/cadernosdisturbios.v18n1p148-163. ISSN 1519-0307.
- ^ Bradley, W. G.; Hudgson, P.; Gardner-Medwin, D.; Walton, J. N. (August 1973). "The syndrome of myosclerosis". Journal of Neurology, Neurosurgery, and Psychiatry. 36 (4): 651–660. doi:10.1136/jnnp.36.4.651. ISSN 0022-3050. PMC 494424. PMID 4793163.
- ^ Merlini, L.; Martoni, E.; Grumati, P.; Sabatelli, P.; Squarzoni, S.; Urciuolo, A.; Ferlini, A.; Gualandi, F.; Bonaldo, P. (2008-10-14). "Autosomal recessive myosclerosis myopathy is a collagen VI disorder". Neurology. 71 (16): 1245–1253. doi:10.1212/01.wnl.0000327611.01687.5e. ISSN 1526-632X. PMID 18852439.
- ^ Cros, D; Harnden, P; Pellissier, JF; Serratrice, G (January 1989). "Muscle hypertrophy in Duchenne muscular dystrophy. A pathological and morphometric study". Journal of Neurology. 236 (1): 43–7. doi:10.1007/BF00314217. PMID 2915226. S2CID 23619631.
- ^ Swatland, Howard (January 1974). "Developmental disorders of skeletal muscle in cattle, pigs and sheep". The Veterinary Bulletin. 44 (4): 193–194 – via ResearchGate.
- ^ Morrow, J.; Sinclair, C. D. J.; Fischmann, A.; Thornton, J. S.; Yousry, T. A.; Reilly, M. M.; Hanna, M. G. (2012-03-01). "1700 MRI quantification of lower limb muscle fatty atrophy: a potential outcome measure in chronic neuromuscular diseases". Journal of Neurology, Neurosurgery & Psychiatry. 83 (3): e1. doi:10.1136/jnnp-2011-301993.32. ISSN 0022-3050.