Lipoma
| Lipoma | |
|---|---|
 | |
| Lipoma on forearm | |
| Specialty | Dermatology, general surgery |
| Symptoms | Soft, movable, usually painless lump[1] |
| Usual onset | 40 to 60 years old[1] |
| Types | Superficial, deep[2] |
| Causes | Unclear[1] |
| Risk factors | Family history, obesity, insufficient exercise[1][3] |
| Diagnostic method | Based on physical exam[1] |
| Differential diagnosis | Liposarcoma, hibernoma, lipomatosis[4] |
| Treatment | Observation, surgery[1] |
| Prognosis | Good[1] |
| Frequency | ~2%[2] |
A lipoma is a non-cancerous soft tissue tumor made of fat tissue.[1] They are generally soft to the touch, movable, and painless.[1] They usually occur just under the skin, but occasionally may be deeper.[1] Most are less than 5 cm in size.[2] Common locations include upper back, shoulders, and abdomen.[4] A few people have a number of lipomas.[3]
The cause is generally unclear.[1] Risk factors include family history, obesity, and lack of exercise.[1][3] Diagnosis is typically based on a physical exam.[1] Occasionally medical imaging or tissue biopsy is used to confirm the diagnosis.[1]
Treatment is typically by observation or surgical removal.[1] Rarely, the condition may recur following removal, but this can generally be managed with repeat surgery.[1] They are not generally associated with a future risk of cancer.[1]
About 2% of people are affected.[2] Lipomas typically occur in adults between 40 and 60 years of age.[1] Males are more often affected than females.[1] They are the most common noncancerous soft tissue tumor.[5] The first use of the term "lipoma" to describe these tumors was in 1709.[6]
Types
The many subtypes of lipomas include:[7]: 624–5
- Adenolipomas are lipomas associated with eccrine sweat glands.[8]: 627
- Angiolipoleiomyomas are acquired, solitary, asymptomatic acral nodules, characterized histologically by well-circumscribed subcutaneous tumors composed of smooth muscle cells, blood vessels, connective tissue, and fat.[7]: 627
- Angiolipomas are painful subcutaneous nodules having all other features of a typical lipoma.[7]: 624 [9]
- Cerebellar pontine angle and internal auditory canal lipomas[10]
- Chondroid lipomas are deep-seated, firm, yellow tumors that characteristically occur on the legs of women.[7]: 625
- Corpus callosum lipoma is a rare congenital brain condition that may or may not present with symptoms.[11] This occurs in the corpus callosum, also known as the calossal commissure, which is a wide, flat bundle of neural fibers beneath the cortex in the human brain.
- Hibernomas are lipomas of brown fat.
- Intradermal spindle cell lipomas are distinct in that they most commonly affect women and have a wide distribution, occurring with relatively equal frequency on the head and neck, trunk, and upper and lower extremities.[7]: 625 [9]
- A fibrolipoma is a lipoma with focal areas of large amounts of fibrous tissue. A sclerotic lipoma is a predominantly fibrous lesion with focal areas of fat.[12]
- Neural fibrolipomas are overgrowths of fibro-fatty tissue along a nerve trunk, which often leads to nerve compression.[7]: 625
- Pleomorphic lipomas, like spindle-cell lipomas, occur for the most part on the backs and necks of elderly men and are characterized by floret giant cells with overlapping nuclei.[7]: 625
- Spindle-cell lipomas are asymptomatic, slow-growing, subcutaneous tumors that have a predilection for the posterior back, neck, and shoulders of older men.[7]: 625
- Superficial subcutaneous lipomas, the most common type of lipoma, lie just below the surface of the skin.[13] Most occur on the trunk, thigh, and forearm, although they may be found anywhere in the body where fat is located.
Causes
The tendency to develop a lipoma is not necessarily hereditary, although hereditary conditions such as familial multiple lipomatosis might include lipoma development.[14][15] Genetic studies in mice have shown a correlation between the HMG I-C gene (previously identified as a gene related to obesity) and lipoma development. These studies support prior epidemiologic data in humans showing a correlation between HMG I-C and mesenchymal tumors.[16]
Cases have been reported where minor injuries are alleged to have triggered the growth of a lipoma, called a "post-traumatic lipoma".[17] However, the link between trauma and the development of lipomas is controversial.[18]
Other conditions
Lipomatosis is believed to be a hereditary condition in which multiple lipomas are present on the body.
Adiposis dolorosa (Dercum disease) is a rare condition involving multiple painful lipomas, swelling, and fatigue. Early studies mentioned prevalence in obese postmenopausal women. However, current literature demonstrates that Dercum disease is present in more women than men of all body types; the average age for diagnosis is 35 years.[19]
Benign symmetric lipomatosis (Madelung disease) is another condition involving lipomatosis. It nearly always appears in middle-aged males after many years of alcoholism, but nonalcoholic males and females can also be affected.[citation needed]
Diagnosis
A physical exam is typically the easiest way to diagnose it. Rarely, a tissue biopsy or imaging may be required. The imaging modality of choice is magnetic resonance imaging (MRI), because it has superior sensitivity of distinguishing it from liposarcoma as well as mapping the surrounding anatomy.[20]
-
X-ray of a lipoma
-
Medical ultrasonography of a lipoma in the thenar eminence: It is hyperechoic compared to adjacent muscle, and relatively well-defined, with miniature hyperechoic lines.[21]
-
Ultrasonography of a liposarcoma for comparison: In this case a heterogeneous mass consisting of an upper hyperechoic portion, corresponding to lipomatous matrix, and areas of hypoechogenicity corresponding to nonlipomatous components.[22]
-
Ultrasonography of a liposarcoma mimicking lipoma. A homogeneous hypoechoic mass presenting with the same appearance of lipoma. It was clinically distinguished by having rapid growth.[22]
-
MRI showing lipoma of the arm
-
X-ray showing lipoma
-
-
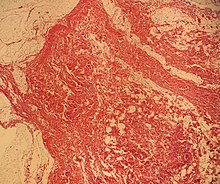
Histopathology of a lipoma: The mass is composed of lobules of mature white adipose tissue divided by fibrous septa containing thin-walled capillary-sized vessels.[23]
Treatment
Usually, treatment of lipomas is not necessary, unless they become painful or restrict movement. They are usually removed for cosmetic reasons if they grow very large or for histopathology to verify that they are not a more dangerous type of tumor such as a liposarcoma.[13] This last point can be important, as the characteristics of a tumor are not known until after it is removed and medically examined.
Lipomas are normally removed by simple excision.[24] The removal can often be done under local anesthetic and takes less than 30 minutes. This cures the great majority of cases, with about 1–2% of lipomas recurring after excision.[25] Liposuction is another option if the lipoma is soft and has a small connective tissue component. Liposuction typically results in less scarring; however, with large lipomas, it may fail to remove the entire tumor, which can lead to regrowth.[26]
New methods under development are supposed to remove the lipomas without scarring. One is removal by injecting compounds that trigger lipolysis, such as steroids or phosphatidylcholine.[24][27] Other potential methods based on tissue-targeted heating include cauterization, electrosurgery, and harmonic scalpel.[28]
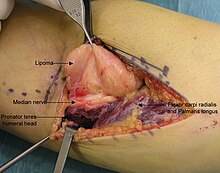
- Resection of an intermuscular lipoma in the elbow region
-
Intraoperative photo.
-
Operating field after removal of the lipoma: Arrow marks the median nerve that was compressed by the lipoma.
-
The resected lipoma
(8 cm × 6 cm × 3 cm)
- Other lipomas
-
Lipoma removed from human torso
-
Lipoma removed from the breast
-
This lipoma was removed from the thigh of a 39-year-old male patient. It measured about 10 cm in diameter at the time of removal. In the center is a section of skin which was removed with the lipoma.
Prognosis
Lipomas are rarely life-threatening, and the common subcutaneous lipomas are not a serious condition. Lipomas growing in internal organs can be more dangerous; for example, lipomas in the gastrointestinal tract can cause bleeding, ulceration, and painful obstructions (so-called "malignant by location", despite being a benign growth histologically).[29][30] Malignant transformation of lipomas into liposarcomas is very rare, and most liposarcomas are not produced from pre-existing benign lesions.[25] A few cases of malignant transformation have been described for bone and kidney lipomas,[31][32] but it is possible that these few reported cases were well-differentiated liposarcomas in which the subtle malignant characteristics were missed when the tumor was first examined.[33] Deep lipomas have a greater tendency to recur than superficial lipomas because complete surgical removal of deep lipomas is not always possible.[33][34]
The presence of multiple lipomas, lipomatosis, is more commonly encountered in men. Some superficial lipomas can extend into deep fascia and may complicate excision. Liposarcoma is found in 1% of lipomas and is more likely to occur in lesions of the lower extremities, shoulders, and retroperitoneal areas. Other risk factors for liposarcoma include large size (>5 cm), associated with calcification, rapid growth, and/or invasion into nearby structures or through fascia into muscle tissue.[35]
Epidemiology
Around 2% of the general population has a lipoma.[2] These tumors can occur at any age, but are most common in middle age, often appearing in people from 40 to 60 years old.[24] Cutaneous lipomas are rare in children, but these tumors can occur as part of the inherited disease Bannayan-Zonana syndrome.[36][37]
Lipomas are usually relatively small with diameters of about 1–3 cm,[38] but in rare cases they can grow over several years into "giant lipomas" that are 10–20 cm across and weigh up to 4–5 kg.[39][40]
Other animals
Lipomas occur in many animals, but are most common in older dogs, particularly older Labrador Retrievers, Doberman Pinschers, and Miniature Schnauzers.[41] Overweight female dogs are especially prone to developing these tumors, and most older or overweight dogs have at least one lipoma.[42][43] In dogs, lipomas usually occur in the trunk or upper limbs.[41] They are also found less commonly in cattle and horses, and rarely in cats and pigs.[43][44] However, a pedunculated lipoma can cause entrapment and torsion of the intestine in horses, causing necrosis, colic, and possibly death. The intestine becomes wound around the stalk of the lipoma and loses blood supply.[45]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 "Lipoma-OrthoInfo – AAOS". orthoinfo.aaos.org. May 2012. Archived from the original on 8 November 2017. Retrieved 8 November 2017.
- ↑ 2.0 2.1 2.2 2.3 2.4 Kransdorf, Mark J.; Murphey, Mark D. (2006). Imaging of Soft Tissue Tumors. Lippincott Williams & Wilkins. p. 81. ISBN 978-0-7817-4771-4. Archived from the original on 2019-12-21. Retrieved 2017-11-08.
- ↑ 3.0 3.1 3.2 Fletcher, Christopher D. M.; Unni, K. Krishnan; Mertens, Fredrik (2002). Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC. p. 20. ISBN 9789283224136. Archived from the original on 2019-12-21. Retrieved 2017-11-08.
- ↑ 4.0 4.1 Lindberg, Matthew R. (2015). Diagnostic Pathology: Soft Tissue Tumors E-Book. Elsevier Health Sciences. p. 44. ISBN 978-0-323-40041-1. Archived from the original on 2019-01-27. Retrieved 2017-11-08.
- ↑ Elder, David E.; Elenitsas, Rosalie; Murphy, George F.; Rosenbach, Misha; Rubin, Adam I.; Seykora, John T.; Xu, Xiaowei (2023). Lever's Dermatopathology: Histopathology of the Skin. Lippincott Williams & Wilkins. p. 3255. ISBN 978-1-9751-7449-1. Archived from the original on 2023-02-28. Retrieved 2023-02-28.
- ↑ Olson, James Stuart (1989). The History of Cancer: An Annotated Bibliography. ABC-CLIO. p. 15. ISBN 978-0-313-25889-3. Archived from the original on 2018-08-12. Retrieved 2017-11-08.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 James, William D.; Berger, Timothy G.; Elston, Dirk M. (2005). Andrews' Diseases of the Skin: Clinical Dermatology (10th ed.). London: Elsevier. ISBN 978-0-7216-2921-6.
- ↑ James, William D.; Berger, Timothy G.; Elston, Dirk M. (2011). Andrews' Diseases of the Skin: Clinical Dermatology (11th ed.). London: Elsevier. ISBN 978-1-4377-0314-6.
- ↑ 9.0 9.1 Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. p. 1838. ISBN 978-1-4160-2999-1.
- ↑ Crowson MG, Symons SP, Chen JM (2013). "Left cerebellopontine angle lipoma with mild brainstem compression in a 13-year-old female". Otology & Neurotology. 34 (5): e34–e35. doi:10.1097/mao.0b013e3182814d6e. PMID 23507992.
- ↑ Wallace D (December 1976). "Lipoma of the corpus callosum". J Neurol Neurosurg Psychiatry. 39 (12): 1179–85. doi:10.1136/jnnp.39.12.1179. PMC 492562. PMID 1011028.
- ↑ "Lipoma Variant: Fibrolipoma". Stanford University School of Medicine. Archived from the original on 2020-02-12. Retrieved 2020-02-10.
- ↑ 13.0 13.1 Lipomas at eMedicine
- ↑ Leffell DJ, Braverman IM (August 1986). "Familial multiple lipomatosis. Report of a case and a review of the literature". J. Am. Acad. Dermatol. 15 (2 Pt 1): 275–9. doi:10.1016/S0190-9622(86)70166-7. PMID 3745530.
- ↑ Toy BR (October 2003). "Familial multiple lipomatosis". Dermatol. Online J. 9 (4): 9. PMID 14594582. Archived from the original on 2012-09-30. Retrieved 2008-05-31.
- ↑ Arlotta P, Tai AK, Manfioletti G, Clifford C, Jay G, Ono SJ (May 2000). "Transgenic mice expressing a truncated form of the high mobility group I-C protein develop adiposity and an abnormally high prevalence of lipomas". J Biol Chem. 275 (19): 14394–400. doi:10.1074/jbc.M000564200. PMID 10747931.
- ↑ Signorini M, Campiglio GL (March 1998). "Posttraumatic lipomas: where do they really come from?". Plast. Reconstr. Surg. 101 (3): 699–705. doi:10.1097/00006534-199803000-00017. PMID 9500386.
- ↑ Aust MC, Spies M, Kall S, Jokuszies A, Gohritz A, Vogt P (2007). "Posttraumatic lipoma: fact or fiction?". Skinmed. 6 (6): 266–70. doi:10.1111/j.1540-9740.2007.06361.x. PMID 17975353. Archived from the original on 2009-02-15.
- ↑ Karen Louise Herbst, Ph.D., M.D. (2012). "Dercum's Disease White Paper" (PDF). Archived (PDF) from the original on 2015-05-13. Retrieved 2015-03-14.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: multiple names: authors list (link) - ↑ Rohit Sharma; Frank Gaillard; et al. "Lipoma". Radiopaedia. Archived from the original on 2019-07-11. Retrieved 2018-09-27.
- ↑ 21.0 21.1 Chernev, Ivan; Tingey, Spencer (2013). "Thenar Intramuscular Lipoma: A Case Report". Journal of Medical Cases. 4 (10): 676–678. CiteSeerX 10.1.1.868.8123. doi:10.4021/jmc1474w.
- ↑ 22.0 22.1 Content originally copied from: Mak, Chee-Wai; Tzeng, Wen-Sheng (2012). "Sonography of the Scrotum". Sonography. doi:10.5772/27586. ISBN 978-953-307-947-9. from Kerry Thoirs (2012-02-03). Sonography. doi:10.5772/27586. ISBN 978-953-307-947-9. Archived from the original on 2019-06-27. Retrieved 2019-02-06., Published: February 3, 2012, under the CC-BY-3.0 license Archived 2011-02-23 at the Wayback Machine.
- ↑ Kim, Hei Sung (30 March 2016). "Lipoma on the antitragus of the ear". Journal of Clinical Research in Dermatology. 3 (2): 01–02. doi:10.15226/2378-1726/3/2/00121.
- ↑ 24.0 24.1 24.2 Salam GA (March 2002). "Lipoma excision". Am Fam Physician. 65 (5): 901–4. PMID 11898962. Archived from the original on 2008-05-11. Retrieved 2006-08-31.
- ↑ 25.0 25.1 Dalal KM, Antonescu CR, Singer S (March 2008). "Diagnosis and management of lipomatous tumors". J Surg Oncol. 97 (4): 298–313. doi:10.1002/jso.20975. PMID 18286473.
- ↑ Al-basti HA, El-Khatib HA (2002). "The use of suction-assisted surgical extraction of moderate and large lipomas: long-term follow-up". Aesthetic Plast Surg. 26 (2): 114–7. doi:10.1007/s00266-002-1492-1. PMID 12016495.
- ↑ Bechara FG, Sand M, Sand D, et al. (2006). "Lipolysis of lipomas in patients with familial multiple lipomatosis: an ultrasonography-controlled trial". J Cutan Med Surg. 10 (4): 155–9. doi:10.2310/7750.2006.00040. PMID 17234112.
- ↑ Boyer, M (2015). "A review of techniques and procedures for lipoma treatment". Clinical Dermatology. doi:10.11138/cderm/2015.3.4.105. Archived from the original on 2017-08-17. Retrieved 2020-05-16.
- ↑ Thompson WM (1 April 2005). "Imaging and findings of lipomas of the gastrointestinal tract". AJR Am J Roentgenol. 184 (4): 1163–71. doi:10.2214/ajr.184.4.01841163. PMID 15788588.
- ↑ Taylor AJ, Stewart ET, Dodds WJ (1 December 1990). "Gastrointestinal lipomas: a radiologic and pathologic review". AJR Am J Roentgenol. 155 (6): 1205–10. doi:10.2214/ajr.155.6.2122666. PMID 2122666.
- ↑ Milgram JW (1990). "Malignant transformation in bone lipomas". Skeletal Radiol. 19 (5): 347–52. doi:10.1007/BF00193088. PMID 2165632.
- ↑ Lowe BA, Brewer J, Houghton DC, Jacobson E, Pitre T (May 1992). "Malignant transformation of angiomyolipoma". J. Urol. 147 (5): 1356–8. doi:10.1016/S0022-5347(17)37564-X. PMID 1569683.
- ↑ 33.0 33.1 Goldblum, John R.; Weiss, Sharon W.; Enzinger, Franz M. (2008). Enzinger and Weiss's soft tissue tumors (5th ed.). Mosby Elsevier. ISBN 978-0-323-04628-2.
- ↑ Fletcher, C.D.M., Unni, K.K., Mertens, F. (2002). Pathology and Genetics of Tumours of Soft Tissue and Bone. World Health Organization Classification of Tumours. Vol. 4. Lyon: IARC Press. ISBN 978-92-832-2413-6.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ E.J. Mayeaux Jr. (2009). The Essential Guide to Primary Care Procedures, p.386, Wolters Kluwer Health. ISBN 978-0-7817-7390-4.
- ↑ Buisson P, Leclair MD, Jacquemont S, et al. (September 2006). "Cutaneous lipoma in children: 5 cases with Bannayan-Riley-Ruvalcaba syndrome". J. Pediatr. Surg. 41 (9): 1601–3. doi:10.1016/j.jpedsurg.2006.05.013. PMID 16952599.
- ↑ Gujrati M, Thomas C, Zelby A, Jensen E, Lee JM (August 1998). "Bannayan-Zonana syndrome: a rare autosomal dominant syndrome with multiple lipomas and hemangiomas: a case report and review of literature". Surg Neurol. 50 (2): 164–8. doi:10.1016/S0090-3019(98)00039-1. PMID 9701122.
- ↑ Lipoma—topic overview Archived 2007-12-11 at the Wayback Machine at webmd.com
- ↑ Hakim E, Kolander Y, Meller Y, Moses M, Sagi A (August 1994). "Gigantic lipomas". Plast. Reconstr. Surg. 94 (2): 369–71. doi:10.1097/00006534-199408000-00025. PMID 8041830.
- ↑ Terzioglu A, Tuncali D, Yuksel A, Bingul F, Aslan G (March 2004). "Giant lipomas: a series of 12 consecutive cases and a giant liposarcoma of the thigh". Dermatol Surg. 30 (3): 463–7. doi:10.1111/j.1524-4725.2004.30022.x. PMID 15008886.
- ↑ 41.0 41.1 Adipose Tissue Tumors Archived 2016-03-04 at the Wayback Machine The Merck Veterinary Manual, (9th ed.)
- ↑ Lipomas Archived 2008-07-20 at the Wayback Machine Veterinary & Aquatic Services Department, Purina
- ↑ 43.0 43.1 Lipoma Archived 2008-10-14 at the Wayback Machine Virginia Polytechnic Institute and State University
- ↑ Lipomas (Fatty Tumors) Archived 2008-05-18 at the Wayback Machine Veterinary Q & A
- ↑ The Merck Veterinary Manual (9th ed.). Merial. 2005. ISBN 978-0-911910-50-6.
External links
| Classification | |
|---|---|
| External resources |
- humpath #2626 Archived 2013-09-21 at the Wayback Machine
- Pages with script errors
- CS1 errors: missing periodical
- CS1 maint: multiple names: authors list
- Webarchive template wayback links
- All articles with unsourced statements
- Articles with unsourced statements from June 2008
- Articles with invalid date parameter in template
- Dermal and subcutaneous growths
- Soft tissue disorders
- Benign neoplasms
- Soft tissue tumor
- RTT



![Medical ultrasonography of a lipoma in the thenar eminence: It is hyperechoic compared to adjacent muscle, and relatively well-defined, with miniature hyperechoic lines.[21]](https://upload.wikimedia.org/wikipedia/commons/1/1c/Ultrasonography_of_a_lipoma.jpg)
![T1 MRI of the same lipoma: High intensity signal mass with regions of ill-defined margins.[21]](https://upload.wikimedia.org/wikipedia/commons/thumb/e/e7/T1_MRI_of_thenar_intramuscular_lipoma.jpg/183px-T1_MRI_of_thenar_intramuscular_lipoma.jpg)
![Ultrasonography of a liposarcoma for comparison: In this case a heterogeneous mass consisting of an upper hyperechoic portion, corresponding to lipomatous matrix, and areas of hypoechogenicity corresponding to nonlipomatous components.[22]](https://upload.wikimedia.org/wikipedia/commons/thumb/a/a9/Scrotal_ultrasonography_of_liposarcoma.jpg/248px-Scrotal_ultrasonography_of_liposarcoma.jpg)
![Ultrasonography of a liposarcoma mimicking lipoma. A homogeneous hypoechoic mass presenting with the same appearance of lipoma. It was clinically distinguished by having rapid growth.[22]](https://upload.wikimedia.org/wikipedia/commons/thumb/3/34/Scrotal_ultrasonography_of_liposarcoma_mimicking_a_lipoma.jpg/226px-Scrotal_ultrasonography_of_liposarcoma_mimicking_a_lipoma.jpg)


![Histopathology of a lipoma: The mass is composed of lobules of mature white adipose tissue divided by fibrous septa containing thin-walled capillary-sized vessels.[23]](https://upload.wikimedia.org/wikipedia/commons/thumb/a/a2/Histopathology_of_lipoma.jpg/207px-Histopathology_of_lipoma.jpg)