Talk:Stroke/Archive 2
| This is an archive of past discussions. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
| Archive 1 | Archive 2 |
Semi-protected edit request on 9 March 2014
This edit request has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
Under Hemorrhagic
Please remove
"Hemorrhagic strokes result in tissue injury by causing compression of tissue from an expanding hematoma or hematomas. This can distort and injure tissue." In addition, the pressure may lead to a loss of blood supply to affected tissue with resulting infarction, and the blood released by brain hemorrhage appears to have direct toxic effects on brain tissue and vasculature.[27][37] Inflammation contributes to the secondary brain injury after hemorrhage.[37]"
Hemorrhagic strokes are due to cardiovascular disease - due to a weakness in the vessel wall or a chronic remodeling of the vasculature that can lead to small or large aneurysm that can rupture and bleed. They ARE NOT trauma. Which this makes it sound like. You have 2 MAIN types of hemorrhagic strokes: intracerebral and subarachnoid.
Intracerebral strokes are from a rupture of microaneurysms in lenticulostriate vessels. Subarachnoid hemorrhagic strokes are due to rupture of a weakened vessel wall in the circle of willis. The blood can compress the brain causing neurologic deficits, have a direct toxic effect on neural tissue, cause damage via secondary inflammation. Fibrosis/healing of the tissue can also lead to loss of function of the affected area.
Trauma is a separate cause of bleeding. It's pathology is getting smacked in the head.
Necrosis MD (talk) 04:39, 9 March 2014 (UTC)
- The text you are commenting on does not mention external trauma at all? But of course the expanding blood causes tissue distortion. Sorry do not see the issue. Doc James (talk · contribs · email) (if I write on your page reply on mine) 06:29, 9 March 2014 (UTC)
- I also find it odd, but [1] calls subarachnoid hemorrhages strokes.
This can occur following ischemia (lack of blood flow) caused by blockage (thrombosis, arterial embolism), or a hemorrhage[1] of central nervous system (CNS),[2] or intracranial blood-vessels.[3]
- The text you are commenting on does not mention external trauma at all? But of course the expanding blood causes tissue distortion. Sorry do not see the issue. Doc James (talk · contribs · email) (if I write on your page reply on mine) 06:29, 9 March 2014 (UTC)
(←) I don't think Necrosis MD has it right. Yes, intracerebral haemorrhage results from vascular pathology but not just from microaneurysms but also from other aneurysms, arteriovenous malformations, amyloid angiopathy, large vessel aneurysms and tumours amongst other pathologies. Most professional guidelines regard subarachnoid haemorrhage as a subtype of stroke, because it leads to sudden neurological symptoms attributable to a vascular cause.
The sources in the introduction need work. I am a little puzzled to find Feigin's paper referenced there. JFW | T@lk 11:05, 9 March 2014 (UTC)
 Not done: please establish a consensus for this alteration before using the
Not done: please establish a consensus for this alteration before using the {{edit semi-protected}}template. — {{U|Technical 13}} (t • e • c) 15:55, 9 March 2014 (UTC)
- Hi JFW - I'm new here and haven't read all of the introductions just yet. Will get to them ASAP. My argument is more to disambiguate that particular paragraph. It really only mentions trauma as a cause of bleeding in the brain which is more of a cerebral vacular injury vs a CVA. Don't CVAs particulary reference vascular pathology more than vascular accidents? Yes, I would say traumas resulting in epidural hematomas and subdural hematomas can cause bleeding in the brain etc, but should be thought of more as an injury instead of a chronic process resulting in a CVA. — Preceding unsigned comment added by Necrosis MD (talk • contribs) 19:31, 9 March 2014
- Hi Necrosis MD. I think you might have misunderstood the first sentence of the section. It doesn't make any pronouncement about the causes of haemorrhagic strokes, but moves straight on the to the sequelae - direct tissue injury, perfusion deficit, and inflammation. The underlying causes are addressed in an earlier subsection of the "Causes" section; this is where the various forms of underlying pathology are listed and the distinction from SAH is also discussed. I have added a short sentence about underlying causes in the subsection of "pathophysiology" also, but it still uncited. JFW | T@lk 19:01, 9 March 2014 (UTC)
Semi-protected edit request on 21 March 2014
This edit request has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
"Cerebrovascular *diease* was the second leading cause of death worldwide in 2004.[5]" 202.72.153.83 (talk) 07:30, 21 March 2014 (UTC)
 Already done .. by CFCF. Sam Sailor Sing 08:32, 21 March 2014 (UTC)
Already done .. by CFCF. Sam Sailor Sing 08:32, 21 March 2014 (UTC)
Newer Treatments in Stroke Rehabilitation through Occupational Therapy
Since Occupational Therapy is a field that is ever evolving and treatments are unique to each individual it should be noted that new techniques and forms of treatment are constantly being introduced and tested. One of these is electrographic biofeedback or EMG. In this treatment electrodes are placed over the muscle group of the affected area, the patient is then told to relax and contract the muscle. They are then shown visual and or auditory feedback (OT: Evidence Based Interventions for Stroke pg 146). This can even be in the form of a game. It is a form of operant conditioning and has proved positive results.
There have also been some studies done on the use of robotics to aide in the rehabilitation of the post-stroke treatment. This allows therapists to focus very clearly on one particular muscle group while adjusting the intensity quite accurately to the patient. However robotics can be quite expensive and not every facility will have the means to provide a service like this.
Lastly one of the newer trends is the use of virtual reality. This is somewhat similar to EMG where it provides a visual stimulus for the patient. This stimulus can be anything from watching the actual movement of a wrist or the swinging of a golf club or baseball bat. Of course this depends on the level of impairment and where they are in their recovery.
Gillen, G., & Burkhardt, A. (2004). Stroke rehabilitation: A function-based approach. St. Louis MO: Mosby. A functional guide to the rehabilitation of patients who have suffered cerebrovascular accidents (stroke).
Krug, Giulianne, MA OTR/L, and Guy McCommack, PhD, OTR/L. Occupational Therapy: Evidence Based Interventions for Stroke. 2009. MS. University of Missouri, Missouri.Www.msma.org. Mar. 2009. Web. 3 Apr. 2014. A reference to current treatments in Occupational Therapy for stroke. Intended for practicing physicians and health care providers.
Teasell, Robert W., MD, and Lalit Kalra, MD. "What's New in Stroke Rehabilitation." What's New in Stroke Rehabilitation. N.p., 3 Dec. 2003. Web. 03 Apr. 2014.Somewhat outdated but trends in rehabilitation of stroke. — Preceding unsigned comment added by Cmpowers23 (talk • contribs) 19:35, 6 April 2014 (UTC)
Circulatory Shock vs Hypoperfusion
Jfdwolff - This is an interesting point and I am not sure that the two are equal. There are cases reported of watershed infarcts in patients with chronic heart failure who take too much antihypertensive medication. Would this be considered circulatory shock? Or is it rather the dysfunction of cerebral autoregulation coupled with hypotension. Perhaps the wording should be changed from "systemic hypoperfusion" to "cerebral hypoperfusion"? I do not feel strongly on this one way or another but I think it is worth mulling over. See "Mechanisms" in this article for more: "Elisa Cuadrado-Godia, Angel Ois, Jaume Roquer. Heart Failure in Acute Ischemic Stroke. Curr Cardiol Rev. 2010 August; 6(3): 202–213. PMC 2994112" Acallen88 (talk) 16:13, 9 April 2014 (UTC)
Fully-protected edit request on 26 October 2014
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
The section entitled "thrombolysis" requires editing because it fails to adequately address the fact that this treatment option is controversial. I propose replacing this section with the following:
Thrombolysis Thrombolysis with recombinant tissue plasminogen activator (rtPA) is a controversial treatment for acute ischemic stroke. A randomised controlled trial (RCT) in 1995 reported that patients treated within three hours of the onset of symptoms were 12% more likely to be in the “alive and independent” group three months after treatment1. A second study in 2008 reported that patients treated between three and 4.5 hours were 7% more likely to be alive and independent2. Treatment does not improve survival. A 2012 systematic review calculated that treatment produces an extra 2.5% risk of death in the short term and an overall 6% increased risk of deterioration due to intracranial haemorrhage (bleeding in the brain)3. Treatment is endorsed by the American Heart Association (AHA), the European Stroke Organisation, and the Australian Stroke Foundation.
Critics of this therapy argue that in contrast to the two positive studies above, nine large RCT showed no benefit to stroke patients4-12, including four that were stopped early due to excess harm7-10. The two positive studies have also been criticised as having major design flaws, especially that the placebo groups of both studies included people with more severe strokes, making the outcome of those in the treated groups look better by comparison13, 14. Published systematic reviews vary in terms of which RCT they include or exclude from their analysis, which has a major impact on the calculated outcomes3, 15, and concern has been expressed about experts having declared financial ties to the manufacturer, including the AHA panel, and authors of the systematic reviews and published statistical analyses16. Treatment is not endorsed as “standard of care” by the American Academy of Emergency Medicine, the Canadian Association of Emergency Physicians, or the Australasian College for Emergency Medicine17-19.
1. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. New England Journal of Medicine. 1995;333(24):1581-7. 2. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. New England Journal of Medicine. 2008;359(13):1317-29. 3. Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 2012;379(9834):2364-72. 4. Randomised controlled trial of streptokinase, aspirin, and combination of both in treatment of acute ischaemic stroke. Multicentre Acute Stroke Trial--Italy (MAST-I) Group. Lancet. 1995;346(8989):1509-14. 5. Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA. 1995;274(13):1017-25. 6. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 1998;352(9136):1245-51. 7. Thrombolytic therapy with streptokinase in acute ischemic stroke. The Multicenter Acute Stroke Trial--Europe Study Group. New England Journal of Medicine. 1996;335(3):145-50. 8. Donnan GA, Davis SM, Chambers BR, Gates PC, Hankey GJ, McNeil JJ, et al. Streptokinase for acute ischemic stroke with relationship to time of administration: Australian Streptokinase (ASK) Trial Study Group. JAMA. 1996;276(12):961-6. 9. Clark WM, Wissman S, Albers GW, Jhamandas JH, Madden KP, Hamilton S. Recombinant tissue-type plasminogen activator (Alteplase) for ischemic stroke 3 to 5 hours after symptom onset. The ATLANTIS Study: a randomized controlled trial. Alteplase Thrombolysis for Acute Noninterventional Therapy in Ischemic Stroke. JAMA. 1999;282(21):2019-26. 10. Clark WM, Albers GW, Madden KP, Hamilton S. The rtPA (alteplase) 0- to 6-hour acute stroke trial, part A (A0276g) : results of a double-blind, placebo-controlled, multicenter study. Thromblytic therapy in acute ischemic stroke study investigators. Stroke. 2000;31(4):811-6. 11. Hacke W, Furlan AJ, Al-Rawi Y, Davalos A, Fiebach JB, Gruber F, et al. Intravenous desmoteplase in patients with acute ischaemic stroke selected by MRI perfusion-diffusion weighted imaging or perfusion CT (DIAS-2): a prospective, randomised, double-blind, placebo-controlled study. Lancet Neurology. 2009;8(2):141-50. 12. group ISTc, Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012;379(9834):2352-63. 13. Fatovich DM. Believing is seeing: Stroke thrombolysis remains unproven after the third international stroke trial (IST-3). Emergency Medicine Australasia. 2012;24(5):477-9. 14. Hoffman JR, Schriger DL. A Graphic Reanalysis of the NINDS Trial. Annals of Emergency Medicine. 2009;54(3):329-36.e35. 15. Wardlaw JM, Murray V, Berge E, Del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database of Systematic Reviews. 2009(4):CD000213. 16. Lenzer J. Why we can't trust clinical guidelines. British Medical Journal. 2013;346(f3830). 17. ACEM.org.au. Position statement on intravenous thrombolysis for ischaemic stroke. 2012; Available from: http://www.acem.org.au/media/S129_v01__Jul-12__Intravenous_thrombolysis.pdf. 18. AAEM. Position Statement on the Use of Intravenous Thrombolytic Therapy in the Treatment of Stroke. American Academy of Emergency Medicine; 2002 [07 May 2014]; Available from: http://www.aaem.org/em-resources/position-statements/clinical-practice/thrombolytic-therapy. 19. CAEP. Position statement: Thrombolytic Therapy For Acute Ischemic Stroke. [cited 2014 10 October]; Available from: http://caep.ca/resources/position-statements-and-guidelines/thrombolytic-therapy-acute-ischemic-stroke.
124.150.71.82 (talk) 06:36, 10 October 2014 (UTC)
- For starters we typically only use secondary sources from the last 5 years. These include recent meta analysis. There is this 2014 Cochrane review https://www.ncbi.nlm.nih.gov/pubmed/25072528 and this 2014 Lancet review https://www.ncbi.nlm.nih.gov/pubmed/25106063
- It is not particularly controversial before 3 hours and after 4.5 hours. The controversy is between these two times and we say "Between three and four and a half hours the effects are less clear." already Doc James (talk · contribs · email) (if I write on your page reply on mine) 20:42, 10 October 2014 (UTC)
Be VERY careful between ischemic and hemorraghic stroke
Not that any Pt's themselves would try to use anticoagulants etc themselves... but it is KEY to differentiate between ISCHEMIC and HEMORRAGHIC stroke. I am aware the intro does this, however, surgery fails to CLEARLY outline that aspirin, anticoagulants, and carotid endarterectomy is for ischemic stroke ONLY, and is actually CONTRAindicated in hemorraghic stroke, and brain MRI is usually done to rule OUT hemorraghic type if suspected!! VERY important from medical standpoint just to let you know! 134.148.68.23 (talk) 10:22, 14 October 2014 (UTC)
Semi-protected edit request on 26 October 2014
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
75.110.127.86 (talk) 18:44, 26 October 2014 (UTC)
 Not done: as you have not requested a change.
Not done: as you have not requested a change.
If you want to suggest a change, please request this in the form "Please replace XXX with YYY" or "Please add ZZZ between PPP and QQQ".
Please also cite reliable sources to back up your request, without which no information should be added to, or changed in, any article. - Arjayay (talk) 18:57, 26 October 2014 (UTC)
Edit Request on 2 November 2014
I am part of a nursing communications class that has been assigned various Wikipedia articles to look at improving the information available on communication within those articles. Communication is an important part of every day life as people constantly interact in multiple ways to send and receive messages. When communication is impaired as it often is in the case of a stroke victim, people have trouble sending and receiving the intended messages being communicated. I would like to request to add a few general sentences about how communication is affected for people who have had a stroke and are experiencing emotional difficulties.
My proposed edit would read: As a result of these post-stroke emotional difficulties, emotional communication can be affected. Emotional communication is expressed through facial expressions, body language or posture, and nonverbal speech such as tone of voice, pitch, volume, and rhythm when speaking. After a stroke as occurred however, these basic means of communicating and expressing emotions may be impaired. These impairments are likely to result in problems with both the receiving and sending of messages between people. [4] I would suggest putting it under the prognosis section in the paragraph that reads: Emotional problems resulting from stroke can result from direct damage to emotional centers in the brain or from frustration and difficulty adapting to new limitations. Post-stroke emotional difficulties include anxiety, panic attacks, flat affect (failure to express emotions), mania, apathy and psychosis. My edit would be placed after this information but as part of this idea in the same paragraph. If you are curious about our assignment and the discussion my group has had over this article you can go to our sandbox at https://en.wikipedia.org/wiki/User_talk:Lh13lg/strokes_sandbox. Thank you. Lh13lg (talk) 18:20, 2 November 2014 (UTC)
Thank you very much Doc James! I am happy to have been able to contribute to this article! Lh13lg (talk) 19:52, 3 November 2014 (UTC)
References
- ^ Sims NR, Muyderman H (September 2009). "Mitochondria, oxidative metabolism and cell death in stroke". Biochimica et Biophysica Acta. 1802 (1): 80–91. doi:10.1016/j.bbadis.2009.09.003. PMID 19751827.
- ^ Cite error: The named reference
Robbinswas invoked but never defined (see the help page). - ^ Feigin VL, Rinkel GJ, Lawes CM; et al. (2005). "Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies". Stroke. 36 (12): 2773–80. doi:10.1161/01.STR.0000190838.02954.e8. PMID 16282541.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Heilman, K. M. (2014). Disorders of Emotional Communication After Stroke. In The Behaviorial Consequences of Stroke (7). Retrieved from http://link.springer.com/chapter/10.1007/978-1-4614-7672-6_7
Edit Request on 4 November 2014
I am also a part of the nursing communications class and was also assigned this page to make additions to, in regards to communication and the stroke. This edit builds on the previous edit made and explains the social impacts a stroke can have on a stroke survivor along with physical self perception. It would provide another look at how some have been and are affected by communication impairments after a stroke.
The proposed edit is: Disruption in self-identity, relationships with others, and emotional well-being are sometimes social consequences after stroke due to the lack of ability to communicate. Many patients who experience communication impairments after a stroke find it more difficult to cope with the social issues rather than physical impairments. Wider aspects of care must address the emotional impact speech impairment has on those who experience difficulties with speech after a stroke. [1] Those who experience a stroke, have a risk of experiencing paralysis which could result in self disturbed body image which may also lead to other social issues. [2] This edit was intended to be under the Prognosis section of the article. For any further details about our project and edits being made, our group has created a sandbox page where we have been discussing and practicing edits: https://en.wikipedia.org/wiki/User:Lh13lg/strokes_sandbox Thank you for taking the time to consider my edit Sg13vp (talk) 01:47, 5 November 2014 (UTC)
References
- ^ Mackenzie, Catherine. "Dysarthria in stroke: A narrative review of its description and the outcome of intervention". International Journal of Speech-Language Pathology: 125-136.
- ^ Ackley, Betty; Ladwig, Gail B.; Kelley, Helen (2010). Nursing diagnosis handbook: an evidence-based guide to planning care (9th ed.). Maryland Heights, MO.: Mosby.
Semi-protected edit request on 14 March 2015
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
Thrombectomy has now been shown beneficial with up to 50% reduction in mortality and significant benefits in functional outcome. This is now standard of care for acute strokes within 6 hours, with proximal vessel occlusion on CT angiography. This was demonstrated in several large trials, including the ESCAPE trial and MR CLEAN. 71.17.245.145 (talk) 00:45, 14 March 2015 (UTC)
 Not done: please provide reliable sources that support the change you want to be made. —
Not done: please provide reliable sources that support the change you want to be made. — {{U|Technical 13}} (e • t • c)02:35, 15 March 2015 (UTC)
Semi-protected edit request on 4 April 2015
An edit to the Prevention section summary on 11 June 2014 introduced a couple minor errors.
1) It seems to have left out the word risk from the phrase those with a high cardiovascular [risk] it provides some protection.
2) It also replaced the phrase aspirin, clopidogrel and dipyridamole may be given to prevent platelets from aggregating. with treatment with medications such as aspirin, clopidogrel and dipyridamole be beneficial., presumably leaving out may from may be beneficial, but I'm not an expert on the subject matter or context, so I'll leave the details to someone more knowledgeable.
Previous Version: https://en.wikipedia.org/w/index.php?title=Stroke&oldid=612088366#Prevention
Edited Version: https://en.wikipedia.org/w/index.php?title=Stroke&oldid=612467448#Prevention
The revised version might read (changes in bold):
In people who have had a myocardial infarction or those with a high cardiovascular risk it provides some protection against a first stroke.[52][53] In those who have previously had a stroke, treatment with medications such as aspirin, clopidogrel and dipyridamole may be beneficial.[52]
I'm new as a contributor, so if I didn't stick to the guidelines feel free to edit my page talk / change request. Thanks.
Dlaverick (talk) 04:24, 3 April 2015 (UTC)
Citation under Pathophysiology: Ischemic Subheading, last sentence of paragraph two
Study found "Even though the change in [Ca2+]c was if anything enhanced, cell viability was improved, arguing that mitochondrial Ca2+ uptake plays a critical role in driving cell death. " (Duchen 2012) Name of journal article: "Mitochondria, calcium-dependent neuronal death and neurodegenerative disease"; Published online 2012 May 22. doi: 10.1007/s00424-012-1112-0 — Preceding unsigned comment added by Aashhleyy (talk • contribs) 19:23, 12 April 2015 (UTC)
Wikidata
Hellow. Why this page isn't linked by other languages. Regards--مصعب (talk) 21:57, 14 August 2015 (UTC)
Meta-analysis of thrombectomy
doi:10.1001/jama.2015.13767 - better functional outcomes and perfusion, same death rates and same rate of haemorrhagic strokes. JFW | T@lk 20:58, 3 November 2015 (UTC)
Semi-protected edit request on 5 November 2015
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
"Varies Over the Course of the Day" is descriptive term used in stroke and other neurological conditions to describe symptomology of varied abilities of individuals affected. I request it be researched and added to the encyclopedia. You can start with source "Teaching Dementia Care Skill and Understanding" by Nancy L. Mace, Dorothy H Coons, Shelly Weaverdyck, and "Handbook of Neurological Disorders" at Google Books.com Phyllis Mitchell
65.189.63.38 (talk) 11:50, 5 November 2015 (UTC)
 Not done: it's not clear what changes you want to be made. Please mention the specific changes in a "change X to Y" format. Are you requesting that an entire article be created for "Varies Over the Course of the Day"? Or that this term be used in some form in the Stroke page Cannolis (talk) 12:54, 5 November 2015 (UTC)
Not done: it's not clear what changes you want to be made. Please mention the specific changes in a "change X to Y" format. Are you requesting that an entire article be created for "Varies Over the Course of the Day"? Or that this term be used in some form in the Stroke page Cannolis (talk) 12:54, 5 November 2015 (UTC)
Post-stroke epilepsy
Who develops an why doi:10.1016/S1474-4422(15)00248-3 JFW | T@lk 08:05, 13 January 2016 (UTC)
Dutch link
Please, place a reference to the Dutch version of this page: https://nl.wikipedia.org/wiki/Herseninfarct — Preceding unsigned comment added by DutchStevie (talk • contribs) 23:07, 14 February 2016 (UTC)
- The Dutch version of this article is Cerebrovasculair accident; Cerebral infarction is the English version of the page that you mention; all this linking being done at Wikidata. Otherwise, it would be unusual to place a link to a Dutch-language Wikipedia article here. Dhtwiki (talk) 02:36, 15 February 2016 (UTC)
Working over 40 hours makes people have strokes more often,...
...and I think that it definitely belongs under either the Cause section or the Prevention section.
Source: http://www.ctvnews.ca/mobile/health/working-longer-hours-increases-stroke-risk-by-up-to-33-per-cent-study-1.2527247
Gamingforfun365 (talk) 02:29, 6 March 2016 (UTC)
Cryptogenic stroke
NEJM this week doi:10.1056/NEJMcp1503946 JFW | T@lk 08:13, 26 May 2016 (UTC)
Nomenclature of hemorrhagic stroke
Ujongbakuto made some changes including bullet points and bolding to the section that discusses hemorrhagic stroke. Unfortunately this article seems to have perpetuated some imprecisions about nomenclature. Extradural and subdural haematomata are not forms of stroke (although they can cause focal neurology) and I have now found a useful source after corresponding with a recognised authority on the subject. Subarachnoid haemorrhage is considered a form of haemorrhagic stroke but is often treated separately. This needs to be very clear. JFW | T@lk 10:10, 27 June 2016 (UTC)
External links modified
Hello fellow Wikipedians,
I have just modified one external link on Stroke. Please take a moment to review my edit. If you have any questions, or need the bot to ignore the links, or the page altogether, please visit this simple FaQ for additional information. I made the following changes:
- Added archive https://web.archive.org/web/20090210050456/http://www.stanfordhospital.com:80/healthLib/atoz/cardiac/effects.html to http://www.stanfordhospital.com/healthLib/atoz/cardiac/effects.html
When you have finished reviewing my changes, please set the checked parameter below to true or failed to let others know (documentation at {{Sourcecheck}}).
![]() An editor has reviewed this edit and fixed any errors that were found.
An editor has reviewed this edit and fixed any errors that were found.
- If you have discovered URLs which were erroneously considered dead by the bot, you can report them with this tool.
- If you found an error with any archives or the URLs themselves, you can fix them with this tool.
Cheers.—InternetArchiveBot (Report bug) 15:33, 10 November 2016 (UTC)
Lancet
Seminar doi:10.1016/S0140-6736(16)30962-X
Hankey going solo. JFW | T@lk 09:18, 2 December 2016 (UTC)
Life expectancy after stroke unclear
The article states "About half of people who have had a stroke live less than one year.[2]" (last paragraph of introduction) which appears incompatible with this source https://www.ncbi.nlm.nih.gov/pubmed/19641331 which states that "Life expectancy after stroke increased up to 4 years from 1978 to the end of 2001". Can an expert look into this?
N.B. the latter source states life expectancy increase, such that actual life expectancy must be higher than 4 years (and also 1 year). 2pem (talk) 19:44, 19 December 2016 (UTC)
Ischemic stroke
"An ischemic stroke is typically caused by blockage of a blood vessel."
The word "typically" is needed IMO as
We have ischemic strokes caused by vasospasms with cocaine
We have watershed ischemic strokes caused by hypotension.[3]
Doc James (talk · contribs · email) 12:18, 7 January 2017 (UTC)
F A S T ?
Should the F.A.S.T. (Face, Arm, Speech, Time) criteria (FAST_(stroke)) be added near the top? If someone thinks a person may have had a stroke, this will be one of the first pages they will encounter, and these are the three symptoms a layperson needs to know to recognise a stroke. The fouth - speed is the essence - is why it would be a real service to make that information readily available. --Hugh7 (talk) 03:38, 25 January 2017 (UTC)
Semi-protected edit request on 13 March 2017
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
Please add the following female-specific risk factors: Hypertensive disorders during pregnancy increase the risk of ischemic stroke. Late menopause and gestational hypertension increase the risk of hemorrhagic stroke. Oophorectomy, hypertensive disorders during pregnancy, preterm delivery, and stillbirth increase the risk of any stroke. Hysterectomy is possibly protective against any stroke.
Please add the following male-specific risk factors: Medical androgen deprivation therapy increases the risk of ischemic stroke. Medical androgen deprivation therapy and erectile dysfunction increase the risk of any stroke.
Source: PMID 27842176 194.151.7.238 (talk) 13:57, 13 March 2017 (UTC)
- Will have a look at some point. If anyone wants to beat me to it the article is a recent (Jan 2017) systematic review that is bound to meet WP:MEDRES. PriceDL (talk) 15:27, 13 March 2017 (UTC)
 Not done: please provide reliable sources that support the change you want to be made. —MRD2014 📞 contribs 15:00, 18 April 2017 (UTC)
Not done: please provide reliable sources that support the change you want to be made. —MRD2014 📞 contribs 15:00, 18 April 2017 (UTC)
Definition
This is a definition "is when poor blood flow to the brain results in cell death"
This is the cause "is the result of poor blood flow to the brain, resulting in cell death."
IMO the first sentence should be used. Others thoughts? Doc James (talk · contribs · email) 02:35, 23 June 2017 (UTC)
Interventional neuroradiology and mechanical thrombectomy
A new paragraph explaining mechanical thrombectomy should be added in the "Management" section, in addition to thrombolysis and surgery/craniectomy. After the publication of five major trials appeared in NEJM in 2015, it became the standard therapy for AIS (acute ischemic stroke) with LVO (large vessel occlusion, e.g. internal carotid or middle cerebral or basilar artery) in all the major hospitals with an interventional neuroradiology unit.
It is important to update the page because this treatment is really a game-changer. I can provide text and sources if you want. Here's the semplification of the procedure: https://www.youtube.com/watch?v=7gn96se6j00&feature=youtu.be
Some sources: 1^ Main trials and European guidelines (ESO-ESNR-ESMINT): https://www.swissneuroradiology.ch/tl_files/events/Consensus_thrombectomy_ESO_Karolinska_ESMINT_ESNR.PDF 2^ Availability in the USA: https://www.ncbi.nlm.nih.gov/pubmed/27895242 3^ AHA-ASA on stroke treatment: http://www.strokeassociation.org/STROKEORG/AboutStroke/Treatment/Stroke-Treatment_UCM_492017_SubHomePage.jsp 4^ AHA "new approach urged": http://news.heart.org/guidelines-urge-new-approach-to-treating-worst-strokes/ 5^ NHS on thrombectomy: https://www.theguardian.com/society/2017/apr/11/nhs-england-stroke-treatment-mechanical-thrombectomy — Preceding unsigned comment added by PaoloMD (talk • contribs) 10:48, 22 July 2017 (UTC)
- We already have such as section Stroke#Surgery Doc James (talk · contribs · email) 14:56, 22 July 2017 (UTC)
- Hello Doc James. The section linked is about surgical prevention (i.e. carotid TEA, even if stenting is also cited); but also in the "Treatment:Surgery" section, endovascular and surgical treatments are confused and mixed because the word "thrombectomy" is not present at all and the "removal of the clot" is described as "surgical" (it is not).
- There are also more errors: AHA recommends administration of tPA within 4.5h (not 3h); endovascular intervention within 6h (not 7h); the meta-analysis published on JAMA supporting the statement "It however does not change the risk of death" is 2 years old and takes into accounts methods that are not used anymore in the clinical practice; actually thrombectomy does change mortality if patients are correctly selected: [1]. On the other side intra-arterial fibrinolysis, cited as a procedure that improves the outcome, is not performed anymore at all! — Preceding unsigned comment added by PaoloMD (talk • contribs) 16:38, 22 July 2017 (UTC)
- It is the second "surgery section" you are looking for. SPecifically it says
- "Surgical removal of the blood clot causing the ischemic stroke may improve outcomes if done within 7 hours of the start of symptoms in those with an anterior circulation large artery clot."Doc James (talk · contribs · email) 23:50, 22 July 2017 (UTC)
- You wrote about "surgical prevention", but I answered about "surgical treatment". The removal of the clot is not surgical, but that's not the main point (it is matter of definitions): the main point is that endovascular therapy is today the standard treatment in the western world and the argument is way underestimated in the article. Also there are many errors concerning guidelines, as I already mentioned.
- It would be interesting to read opinions from other users on this topic. — Preceding unsigned comment added by PaoloMD (talk • contribs) 16:47, 25 July 2017 (UTC)
- We already have such as section Stroke#Surgery Doc James (talk · contribs · email) 14:56, 22 July 2017 (UTC)
References
Mirror therapy
I would like this information to be added to the Wikipedia article "Stroke." It would go in the rehabilitation section, middle of paragraph 4, following the sentence, "Physiotherapists can also work with patients to improve awareness and use of the hemiplegic side."...
We would like to add, "One such intervention is mirror therapy which is significantly associated with immediately improved motor function of the upper extremity in patients with stroke."[1]
References
- ^ Thieme, H; Pohl, M; Behrens, J; Dohle, C (March 14, 2012). "Mirror therapy for improving motor function after stroke". PMID 23390640.
{{cite journal}}: Cite journal requires|journal=(help)
It's a valid rehabilitation procedure. Further info. I agree with the added content and source, although the words "significantly" and "immediately" should be excluded as not universally proven. --Zefr (talk) 15:33, 5 February 2018 (UTC)
The page is locked, I am a new user. Can you do the edit for me?--Lhaynes2 (talk) 16:20, 5 February 2018 (UTC)
Citation needed
Hemorrhagic strokes may occur on the background of alterations to the blood vessels in the brain, such as cerebral amyloid angiopathy, cerebral arteriovenous malformation and an intracranial aneurysm, which can cause intraparenchymal or subarachnoid hemorrhage.[citation needed][1]--Yeggarik (talk) 11:47, 24 March 2018 (UTC)
References
- ^ Smith, SD; Eskey, CJ (January 2011). "Hemorrhagic stroke". Radiologic clinics of North America. 49 (1): 27–45. doi:10.1016/j.rcl.2010.07.011. PMID 21111128.
- Could you check the DOI identifier, which points to an error page for me, but which is the same on other pages encountered, such as that pointed to by Pubmed number? Dhtwiki (talk) 20:22, 24 March 2018 (UTC)
Discussion concering efficacy of thrombolysis in ischemic stroke
This topic has been discussed extensively elsewhere, but it is not known to many colleagues that there are major concerns with the quality of the evidence for thrombolysis in stroke. There have been numerous (nine, I believe) RCTs on rtPA, and only two (NINDS-2, ECASS-3) showed some sort of benefit with an improved clinical outcome with a NNT of ~10. But more importantly, there are great weaknesses in the way those two studies were conducted and interpreted. I would like to refer to Justin Morgenstern ("Thrombolytics for stroke: The evidence", First10EM blog, May 26, 2017. Available at: https://first10em.com/thrombolytics-for-stoke/) for a very detailed and thorough discussion of the various studies. Also, there is a great discussion between Dr. J. Hoffman (sceptic) and Dr. G. Albers (advocate) right here, for those who are interested in listening to both sides: https://www.youtube.com/watch?v=J-iL5hoOriE
It would be nice to see a more detailed reflection of those concerns here on this site, therefore I suggest a "Discussion" part in the "Management"-section. However, my account is not eligible to add one. Friddeadine (talk) 14:02, 1 April 2018 (UTC)
Use and limitation of CT scan in identifying stroke.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1308759/pdf/westjmed00315-0070.pdf
- Often the ischemic (blockage) stroke simply does not show up for the first 24 hours or so, well after the window for thrombolytic ("clot busting") treatment. FriendlyRiverOtter (talk) 18:50, 17 April 2018 (UTC)
- FriendlyRiverOtter Please clarify why you are posting this here. The article is pretty clear that stroke is a clinical diagnosis and that CT serves mainly to exclude haemorrhage in the acute phase. JFW | T@lk 18:54, 17 April 2018 (UTC)
It's not clear in our info box at the top in which we state, "Based on symptoms and medical imaging[6]" as if diagnosing a stroke is as straightforward as a broken arm. And rightly or wrongly, the info box is all a lot of wiki readers use.
And in 5.2 Imagining section, we write, "scans (without contrast enhancements) sensitivity= 16%." We need some immediate text to let people know that 16% is not just a typo, and why CT is still use. And right then and there, not merely at the bottom of the section.
And plus, I always welcome one more reference. FriendlyRiverOtter (talk) 19:22, 17 April 2018 (UTC)
I made some changes, hope you like them. Time permitting, please jump in and add your touch. :-) FriendlyRiverOtter (talk) 18:29, 18 April 2018 (UTC)
- Have adjusted to a single sentence "Based on symptoms with medical imaging typically used to rule out bleeding"
- This well true initially "ischemic stroke often doesn't appear in CT scan". Later on they do typically appear on CT scans.
- Your thoughts User:FriendlyRiverOtter? Doc James (talk · contribs · email) 12:36, 21 April 2018 (UTC)
Hi, like the changes particular in the info box. Thanks. FriendlyRiverOtter (talk) 14:44, 24 April 2018 (UTC)
Relegating photo without symptoms, days since symptoms, etc, to Talk page
| Stroke | |
|---|---|
| Other names | Cerebrovascular accident (CVA), cerebrovascular insult (CVI), brain attack |
 | |
| CT scan of the brain showing a right-hemispheric ischemic stroke. | |
| Specialty | Neurology |
| Symptoms | Inability to move or feel on one side of the body, problems understanding or speaking, feeling like the world is spinning, loss of vision to one side[1][2] |
| Complications | Persistent vegetative state[3] |
| Causes | Ischemic (blockage) and hemorrhagic (bleeding)[4]
. . . |
This photo does not include patient's symptoms, time period since symptoms began, nothing. In fact, by including a ischemic (blockage) stroke as obvious as the rash on a baby's bottom, it's feeding into common misconceptions. A lot of lay persons think that if you're having stroke symptoms, you go to the hospital and a CT scan can tell you, yeah or nay, are you having a stroke. When in fact, it's the much more interesting answer that a CT scan can rule out a bleeding stroke, but cannot rule in a blockage stroke.FriendlyRiverOtter (talk) 17:41, 24 April 2018 (UTC)
Just not a whole lot of information there. FriendlyRiverOtter (talk) 17:54, 24 April 2018 (UTC)
https://commons.wikimedia.org/wiki/File:MCA_Territory_Infarct.svg
- It is an image of a prior stroke and as such is perfectly appropriate. Not every picture must show all possible aspects of the condition in question.
- User:Lucien Monfils how long after the stroke was this CT done? That would be useful info to add.Doc James (talk · contribs · email) 00:25, 26 April 2018 (UTC)
Always the question of whether an imperfect picture is better than no picture at all. And since a lot of lay persons really do seem to think that a clear CT scan gives the all-clear, A-Okay, no stroke verdict, in this case I tend to think no picture at all, instead of one which misleads in the direction people are already inclined to believe. And I should point out that I myself am a lay person, who used to believe that a CT scan of potential stroke provided a definite answer. FriendlyRiverOtter (talk) 19:03, 26 April 2018 (UTC)
2018 review article on misdiagnosis
ref name="Diagnostic Error in Stroke—Reasons and Proposed Solutions, Current Ather. Reports, 2018"
Bakradze, Ekaterina; Liberman, AL (13 February 2018). "Diagnostic Error in Stroke—Reasons and Proposed Solutions". Current Atherosclerosis Reports. 20 (2). PMID 29441421.</ref>
- A recent review article, and it seems like it has some good info.FriendlyRiverOtter (talk) 21:12, 3 May 2018 (UTC)
- I added a subsection on "Misdiagnosis." Still more work to be done. FriendlyRiverOtter (talk) 22:27, 3 May 2018 (UTC)
https://en.wikipedia.org/w/index.php?title=Stroke&diff=839509845&oldid=839152618
- I added a subsection on "Misdiagnosis." Still more work to be done. FriendlyRiverOtter (talk) 22:27, 3 May 2018 (UTC)
References
- ^ Cite error: The named reference
Donnan2008was invoked but never defined (see the help page). - ^ Cite error: The named reference
HLB2014Swas invoked but never defined (see the help page). - ^ PhD, Gary Martin (2009). Palliative Care Nursing: Quality Care to the End of Life, Third Edition. Springer Publishing Company. p. 290. ISBN 9780826157928. Archived from the original on 2017-08-03.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Cite error: The named reference
HLB2014Wwas invoked but never defined (see the help page).
Should we put in X-ray of hemorrhagic stroke? And this is what doctors look to rule out before giving clot-busting medication.
http://learningradiology.com/notes/generalnotes/hemorrhagicstroke.htm
This seems to be a pretty good X-ray and explanation. I'm just not that familiar with standards regarding fair use of photographs. FriendlyRiverOtter (talk) 18:14, 10 May 2018 (UTC)
http://learningradiology.com/images/generalimages/Hem%20stroke-ann.jpg
- That image is all rights reserved.
- We have an image of a hemorrhagic stroke here Stroke#Hemorrhagic
- Ischemic strokes are more common and thus I oppose switching them.
- Additionally most strokes at presentation are not "acute" Doc James (talk · contribs · email) 18:19, 10 May 2018 (UTC)
Most people think a CT scan of a potential stroke is like an X-ray of a potential broken arm, yeah or nay, it gives a definite verdict. So, yes, I continue to have problems with an X-ray where the stroke is clear as a Christmas tree! , especially an ischemic one.
By not acute, do you mean the symptoms such as drooping face on one side, etc, are softer, vaguer symptoms? FriendlyRiverOtter (talk) 18:40, 10 May 2018 (UTC)
So, OUCH!! Most parents and families do wait until it's too late. FriendlyRiverOtter (talk) 17:46, 11 May 2018 (UTC)
"Young stroke"
Dedicated review on this area doi:10.1016/S1474-4422(18)30233-3 JFW | T@lk 14:05, 15 August 2018 (UTC)
Semi-protected edit request on 7 September 2018
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
Updated reference relating to the link between stroke and dementia (meta-analysis of all available data in the leading dementia journal): https://www.alzheimersanddementia.com/article/S1552-5260(18)33250-3/abstract DrDJLlewellyn (talk) 17:27, 7 September 2018 (UTC)
 Not done: According to the page's protection level you should be able to edit the page yourself. If you seem to be unable to, please reopen the request with further details. — Newslinger talk 11:07, 12 September 2018 (UTC)
Not done: According to the page's protection level you should be able to edit the page yourself. If you seem to be unable to, please reopen the request with further details. — Newslinger talk 11:07, 12 September 2018 (UTC)
- As User:DrDJLlewellyn appears to have a COI, I have added the paper in question to our article. Thanks for posting here. Doc James (talk · contribs · email) 19:50, 12 September 2018 (UTC)
Semi-protected edit request on 6 November 2018
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
I want to add below paragraph to stroke prevention section; If an ischemic stroke or transient ischemic attack happens on aspirin monotherapy, the addition of or a switch to another antiplatelet agent, especially in the first days after the event, may decrease the furture vascular event and stroke risk.[1] Mdfurkanyilmaz (talk) 06:23, 6 November 2018 (UTC)
 Not done: per WP:CLOSEPARAPHRASE. Spintendo 01:48, 22 November 2018 (UTC)
Not done: per WP:CLOSEPARAPHRASE. Spintendo 01:48, 22 November 2018 (UTC)
References
- ^ Lee, Meng; Saver, Jeffrey L.; Hong, Keun-Sik; Rao, Neal M.; Wu, Yi-Ling; Ovbiagele, Bruce (09 2017). "Antiplatelet Regimen for Patients With Breakthrough Strokes While on Aspirin: A Systematic Review and Meta-Analysis". Stroke. 48 (9): 2610–2613. doi:10.1161/STROKEAHA.117.017895. ISSN 1524-4628. PMID 28701574.
{{cite journal}}: Check date values in:|date=(help)
Stroke Management at Discharge
[1]Large clinical trials with ischemic older adult patients, who were not previously on statins, showed that implementing statin therapy upon discharge reduced the risk of major cardiovascular adverse events, hospital readmission, and mortality within a 2-year period. — Preceding unsigned comment added by Cancorbinhall (talk • contribs) 17:01, 17 January 2019 (UTC)
--Cancorbinhall (talk) 18:31, 17 January 2019 (UTC)[2]
References
- ^ Sladojevic, N; et al. "ROCK as a therapeutic target for ischemic stroke".
{{cite journal}}: Cite journal requires|journal=(help); Explicit use of et al. in:|last1=(help) - ^ Li, Y; et al. "2017 Taiwan lipid guidelines for high risk patients".
{{cite journal}}: Cite journal requires|journal=(help); Explicit use of et al. in:|last1=(help)
Stroke classification drawing
The text under this drawing misidentifies the images - the "blood clot" is 1a and the "blood pool" is 2b, but the image labels "brain death" as 2a, not 1b as written. Conversely the "ruptured blood vessel" is 1b, not 2a. — Preceding unsigned comment added by 100.19.27.163 (talk) 04:38, 4 March 2019 (UTC)
Semi-protected edit request on 12 September 2019
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
In the part where Intracerebral Haemorrhage is written, that is the title 'Intracerebral Haemorrhage' under the heading 'Causes' 11:17, 12 September 2019 (UTC)TanishqKakade% (talk)←, please change the spelling of Haemorrhage from 'hemorrhage ' to 'haemorrhage' as it is the correct spelling. TanishqKakade% (talk) 11:17, 12 September 2019 (UTC) −
 Not done: Both are correct - Hemorrhage is American English, and Haemorrhage is British English. It appears that this article favors the American spelling, and per WP:ENGVAR and MOS:RETAIN it should be left as is. Thanks, ‑‑ElHef (Meep?) 12:53, 12 September 2019 (UTC)
Not done: Both are correct - Hemorrhage is American English, and Haemorrhage is British English. It appears that this article favors the American spelling, and per WP:ENGVAR and MOS:RETAIN it should be left as is. Thanks, ‑‑ElHef (Meep?) 12:53, 12 September 2019 (UTC)
Semi-protected edit request on 5 November 2019
This edit request has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
I would like to add the specialty of Vascular Surgery as part of the treating specialty of strokes. We play a massive role in diagnosing TIA's and Ischemic strokes followed by the surgical treatment via carotid endarterectomies, carotid artery stenting and more recently, transcarotid artery revascularization. The Society of Vascular surgery page has ample information to support these claims. — Preceding unsigned comment added by Sreekanna (talk • contribs) 01:33, 5 November 2019 (UTC)
 Not done: Per WP:EXISTS, just because an organization exists does not automatically make it notable. We cannot simply list every known organisation that perform a function. If there is referenced material that supports how Vascular Surgery is more than just a clinic (i.e. leads the field in some measure), then do provide the links in a new request — IVORK Talk 02:28, 5 November 2019 (UTC)
Not done: Per WP:EXISTS, just because an organization exists does not automatically make it notable. We cannot simply list every known organisation that perform a function. If there is referenced material that supports how Vascular Surgery is more than just a clinic (i.e. leads the field in some measure), then do provide the links in a new request — IVORK Talk 02:28, 5 November 2019 (UTC)
This edit request has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
To further comment on my previous request to add Vascular surgery as part of the primary specialties treating stroke, please find the following peer-reviewed articles to prove that we do lead the field in terms of diagnosis and lead outcomes in contemporary management. https://www.ncbi.nlm.nih.gov/pubmed/31672680 https://www.jvascsurg.org/article/S0741-5214(19)30379-9/fulltext https://www.ncbi.nlm.nih.gov/pubmed/30095343 https://www.ahajournals.org/doi/10.1161/01.STR.0000019048.04306.A1 https://www.jvascsurg.org/article/S0741-5214%2811%2901635-1/fulltext https://academic.oup.com/eurheartj/article/39/9/763/4095038
In general a stroke or TIA (non devastating CVA) requires a refferal to a vascular surgeon who will diagnose carotid stenosis in vascular labs and choose to intervene on it to prevent recurrent major strokes or primary ones in high risk individuals. The book Rutherfords Vascular surgery has multiple chapters dedicated to the care of ischemic stroke and its prevention. Carotid endarterectomies are one of the most common procedures done by Vascular surgeons, it is also noted as " surgery to open up arteries to the brain" in this article. Vascular surgeons are also at the forefront of innovating new devices and techniques to treat and prevent strokes for example the transcarotid revascularization or neuroembolic protection devices. Extracranial cerebrovascular diseases make up a significant portion of the patient population seen by Vascular surgeons. The reason I want to make this addition is because many patients, including mine have been dumbfounded by the fact that we deal with strokes in any way.
Sree Kanna, MD. — Preceding unsigned comment added by Sreekanna (talk • contribs) 21:50, 5 November 2019 (UTC)
 Not done @Sreekanna:, while I recognise (as possibly the previous responder did not} that vascular surgery is a clinical specialty, not an organisation seeking advertisement, and agree that vascular surgeons often play a key part in stroke management and interventions, in order for us to add the content you've enquired about, we would need you to suggest what specific additions you would like to be added to the article, as in "please provide the text you wish to be added". Fish+Karate 10:34, 18 November 2019 (UTC)
Not done @Sreekanna:, while I recognise (as possibly the previous responder did not} that vascular surgery is a clinical specialty, not an organisation seeking advertisement, and agree that vascular surgeons often play a key part in stroke management and interventions, in order for us to add the content you've enquired about, we would need you to suggest what specific additions you would like to be added to the article, as in "please provide the text you wish to be added". Fish+Karate 10:34, 18 November 2019 (UTC)
Semi-protected edit request on 6 January 2020
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
Please add to the end of 11.2 Neuroprotection the following section: Microglia also play a role in neuroprotection following ischemic stroke via specialized purinergic somatic junctions found on neuronal cell bodies. [1] 193.6.209.30 (talk) 13:34, 6 January 2020 (UTC)
References
- ^ Cserép et al., Science 12 Dec 2019:eaax6752 DOI: 10.1126/science.aax6752 https://science.sciencemag.org/content/early/2019/12/11/science.aax6752
![]() Not done - Lab research too preliminary to mention. --Zefr (talk) 18:13, 6 January 2020 (UTC)
Not done - Lab research too preliminary to mention. --Zefr (talk) 18:13, 6 January 2020 (UTC)
ICD 11
Just to note that in ICD 11 "Stroke has now formally been listed as a neurological disorder and not a disorder of the circulatory system".[1] --Iztwoz (talk) 08:28, 13 February 2020 (UTC)
References
- ^ The, Lancet (8 June 2019). "ICD-11". Lancet (London, England). 393 (10188): 2275. doi:10.1016/S0140-6736(19)31205-X. PMID 31180012.
Probable poor grammar, not sure?
So, I'm not expert on Strokes, which is why I'm posting here instead of just changing it. In the article, there is a sentence that reads "Prevention includes decreasing risk factors, as well as possibly aspirin, statins..." To me, that reads as saying that statins and aspirin should be avoided as they are risk factors. In the next paragraph, it says "Aspirin should be used." So, in the first example, are they listing modes of prevention instead of risk factors to be avoided? If so, that's very unclear, and I hope someone will modify it.
"Yes...It's Raining" 23:23, 29 June 2020 (UTC)
- That was muddied wording. I rewrote 3 sentences to clarify. Next time, don't be shy - go ahead and edit, as many editors follow this article. Zefr (talk) 23:45, 29 June 2020 (UTC)
Semi-protected edit request on 28 October 2020
This edit request to Stroke has been answered. Set the |answered= or |ans= parameter to no to reactivate your request. |
 Not done: it's not clear what changes you want to be made. Please mention the specific changes in a "change X to Y" format and provide a reliable source if appropriate. ◢ Ganbaruby! (Say hi!) 15:01, 31 October 2020 (UTC)
Not done: it's not clear what changes you want to be made. Please mention the specific changes in a "change X to Y" format and provide a reliable source if appropriate. ◢ Ganbaruby! (Say hi!) 15:01, 31 October 2020 (UTC)
Extended content
| ||
|---|---|---|
Epidemiology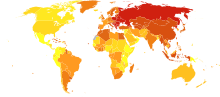 58–316 317–417 418–466 467–518 519–575 576–640 641–771 772–974 975-1,683 1,684–3,477 
Stroke was the second most frequent cause of death worldwide in 2011, accounting for 6.2 million deaths (~11% of the total).[2] Approximately 17 million people had a stroke in 2010 and 33 million people have previously had a stroke and were still alive.[3] Between 1990 and 2010 the number of strokes decreased by approximately 10% in the developed world and increased by 10% in the developing world.[3] Overall, two-thirds of strokes occurred in those over 65 years old.[3] South Asians are at particularly high risk of stroke, accounting for 40% of global stroke deaths.[4] It is ranked after heart disease and before cancer.[5] In the United States stroke is a leading cause of disability, and recently declined from the third leading to the fourth leading cause of death.[6] Geographic disparities in stroke incidence have been observed, including the existence of a "stroke belt" in the southeastern United States, but causes of these disparities have not been explained. Disparities also exist along socioeconomic lines; rates of long-term mortality among stroke survivors were higher for individuals residing in low income neighborhoods than in more affluent ones.[7] Further, based on the results of a meta analysis of twelve cohort and case-control studies, reduced SES standing could also explain more than 30% of stroke risk globally, irrespective of traditional risk factors. [8] The risk of stroke increases exponentially from 30 years of age, and the cause varies by age.[9] Advanced age is one of the most significant stroke risk factors. 95% of strokes occur in people age 45 and older, and two-thirds of strokes occur in those over the age of 65.[10][11] A person's risk of dying if he or she does have a stroke also increases with age. However, stroke can occur at any age, including in childhood. Family members may have a genetic tendency for stroke or share a lifestyle that contributes to stroke. Higher levels of Von Willebrand factor are more common amongst people who have had ischemic stroke for the first time.[12] The results of this study found that the only significant genetic factor was the person's blood type. Having had a stroke in the past greatly increases one's risk of future strokes. Men are 25% more likely to suffer strokes than women,[10] yet 60% of deaths from stroke occur in women.[13] Since women live longer, they are older on average when they have their strokes and thus more often killed.[10] Some risk factors for stroke apply only to women. Primary among these are pregnancy, childbirth, menopause, and the treatment thereof (HRT). Pubhealth0 (talk) 05:53, 28 October 2020 (UTC) References
|
The article promotes Mediterranean diet, with unreliable evidence, without mentioning other important studies about diet.
The article "Stroke" says "Nutrition, specifically the Mediterranean-style diet, has the potential for decreasing the risk of having a stroke by more than half.[127]", referring to a source which is not a high quality evidence, but rather an article, promoting the mentioned diet.
The article "Mediterranean diet" says: "There is some evidence that the Mediterranean diet lowers the risk of heart disease and early death, although a 2019 review determined that the evidence had low quality and was uncertain.[5][6]", referring to a high quality evidence.
Speaking about diet, the following studies supporting a low-fat, plant-based diet to prevent stroke are not mentioned.
- Joshipura, K.J. et al. 1999. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA 282: 1233–1239.
- Johnsen, S.P. et al. 2003. Intake of fruit and vegetables and the risk of ischemic stroke in a cohort of Danish men and women. Am. J. Clin. Nutr. 78: 57–64.
- Sauvaget, C. et al. 2003. Vegetable and fruit intake and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Stroke 34: 2355–2360.
- Steffen, L.M. et al. 2003. Associations of whole-grain, refined-grain, and fruit and vegetable consumption with risks of all-cause mortality and incident coronary artery disease and ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Am. J. Clin. Nutr. 78: 383–390.
- Thomas Campbell, 2017, A plant-based diet and stroke
- Thomas Campbell, China–Cornell–Oxford Project — Preceding unsigned comment added by Andrej Adamenko (talk • contribs) 11:50, 9 February 2021 (UTC)
Wiki Education Foundation-supported course assignment
![]() This article was the subject of a Wiki Education Foundation-supported course assignment, between 1 July 2019 and 23 August 2019. Further details are available on the course page. Student editor(s): Storm1625.
This article was the subject of a Wiki Education Foundation-supported course assignment, between 1 July 2019 and 23 August 2019. Further details are available on the course page. Student editor(s): Storm1625.
Above undated message substituted from Template:Dashboard.wikiedu.org assignment by PrimeBOT (talk) 10:18, 17 January 2022 (UTC)
Other names
Stroke has many names, so i suggest you add 2 other used names to the template: Cerebral Infarction (Ischemic) and Intracranial Hemorrhage (Hemorrhagic). Aidenless (talk) 15:42, 28 September 2022 (UTC)
- Both of those conditions cause a stroke, but are not the result of a stroke. Zefr (talk) 16:20, 28 September 2022 (UTC)
Glycine
Some websites (at least in Russian) recommend giving 10 tablets of glycine to a patient right after symptoms appear. Is this recommendation correct? Nemohuman (talk) 15:55, 15 October 2022 (UTC)