Heart transplantation
| Heart transplantation | |
|---|---|
| Other names: Cardiac transplant, heart transplant | |
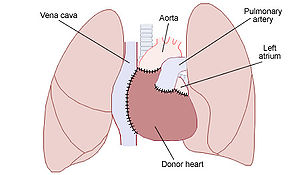 | |
| Placement of a donor heart in an orthotopic procedure. Note how the back of the person's left atrium and great vessels are left in place. | |
| Specialty | Cardiothoracic surgery[1] |
| Indications | End-stage heart failure[1] |
| Contraindications | High pulmonary vascular resistance, cancer[2] |
| Types | Orthotopic (usual position) Heterotopic (unusual position)[1][3] |
| Steps | 1) Find compatible donor 2) Bi-caval method (orthotopic) a) Join the donor left atrium to the recipients atrial cuff b) Model the pulmonary artery and aorta c) Release the cross-clamp in donor to complete the remaining joins[1] |
| Success | Improves quality and duration of life[2] |
| Complications | Rejection, infection, allograft vasculopathy[2] |
| Outcome | One year survival > 90%[2] Five years survival 75%[2] |
| Frequency | 5,000 per year[4] |
| |
A heart transplantation is major surgery to remove a seriously diseased heart from a person (recipient) and replace it with a normal one from another person (donor).[1] It is performed when, despite other treatments, the heart fails to pump blood effectively such as in end-stage heart failure or severe coronary artery disease.[1] It is generally an option for a young person with severe irreversible heart failure who has a life expectancy of less than 6 months.[2]
Just over half of recipients have non-ischaemic cardiomyopathy, a third have coronary artery disease, and the rest comprise of valvular heart disease, congenital heart disease and re-transplantations.[1] When performed for heart failure, recipients generally have severe limitation of physical activity, while on optimal treatment, and have undergone other appropriate procedures such as cardiac resynchronisation therapy and have an implantable cardioverter-defibrillator.[1] Scoring systems exist to guide suitability of a recipient.[6] Generally, donors have brainstem death (heart-beating donors); though a few centers have programs using donors following circulatory determined death (non-heart beating donors).[1]
It is not safe to perform a heart transplant if there is high pulmonary vascular resistance or an active cancer.[2] Other reasons for not doing the surgery include active infection, severe kidney or liver failure, recent pulmonary embolism, severe lung disease, or diabetes with complications.[1] Having another serious disease with a poor outcome, recent stroke, drug and alcohol misuse, or obesity can also increase risks.[2] In some centers the surgery is only done in people under the age 60 years.[2] Complications include rejection and allograft vasculopathy.[2] The requirement of immunosuppression may increase the risk of infection, particularly in the first year after surgery.[1] Other problems that might occur include high blood pressurre, high cholesterol and cancer, particularly skin cancer.[2] Better results are achieved if the donor heart is placed within 4 hours of its retrieval, and if the recipient is younger.[1]
Most are performed as a single heart transplant, but it may be combined with a lung, liver or kidney transplant.[1] The donor is fully heparinised before the heart is retrieved and placed in cold saline in an insulated organ transport box.[1] The more common method is bi-caval, a type of orthotopic procedure where the donor heart is placed in the same spot as the persons prior heart.[1][3] It involves joining the donor left atrium to the recipients atrial cuff, and then modelling the pulmonary artery and aorta, before releasing the cross-clamp to complete the remaining joins.[1] A heterotopic (“piggy-backed”) procedure may be done to assist left ventricular function, and involves leaving the prior heart in place while joining the donor heart to its right.[3] Heart transplantation can improve the quality and duration of life, particularly in younger recipients.[2][7] As the donor heart has lost its nerve supply, some of its functions are different.[2] It beats faster and loses the normal blood pressure variation though the day.[2]
As of 2020 more than 120,000 heart transplants have been performed since the first in 1967, by South African cardiac surgeon Christiaan Barnard.[1] More than 5,000 heart transplants are performed each year worldwide.[4] More than half are performed in the US.[8] Expected survival after surgery at one year is greater than 90% and at five years is 75%.[2] In transplants carried out between 1992 and 2001, the greatest risk of death is in the first year after the procedure, and the average survival is 11 years.[1] If another heart transplant is repeated at a later date, the risks of death are higher.[1] Globally, organ donation has limited the number of procedures performed.[1]
Medical uses
A heart transplant is most often performed in a person with a severely weakened heart, when other treatments have not worked.[9] People who are in need of a heart transplant but do not qualify may be candidates for an artificial heart[8] or a left ventricular assist device (LVAD), as a bridge-to-transplantation.[1]
Recipient
Just over half of recipients have non-ischaemic cardiomyopathy, a third have coronary artery disease, and the rest comprise of valvular heart disease, congenital heart disease and re-transplantations.[1] When performed for heart failure, recipients should generally have severe limitation of physical activity, while on optimal treatment and have undergone other appropriate heart procedures such as cardiac resynchronisation therapy and have implantable cardioverter-defibrillator.[1] Composite scoring systems exist to guide suitability of a recipient for heart transplant.[6]
Donor
Generally, donors have been confirmed to have brain stem death (heart-beating donors).[1] A few centres have re-established transplant programs using donors following circulatory determined death (non-heart beating donors).[1] Echocardiography and coronary angiography play a role in assessing suitability of the donor.[1] ABO blood group determines donor and recipient compatibility, and testing for anti-HLA antibodies might be required.[1]
Contraindications
Some people are less suitable for a heart transplant and have an increase chance of complications.[1]
Absolute contraindications:
- Irreversible kidney, lung, or liver disease[4]
- Active cancer if it is likely to impact the person's survival
- Life-threatening diseases unrelated to the cause of heart failure, including acute infection or systemic disease such as systemic lupus erythematosus, sarcoidosis, or amyloidosis
- Vascular disease of the neck and leg arteries.
- High pulmonary vascular resistance – over 5 or 6 Wood units.
Relative contraindications:[10]
- Insulin-dependent diabetes with severe organ dysfunction
- Recent thromboembolism such as stroke
- Severe obesity
- Age over 65 years (some variation between centers) – older people are usually evaluated on an individual basis.
- Active substance use disorder, such as alcohol, recreational drugs or tobacco smoking (which increases the chance of lung disease)
Complications
Potential complications include:[11]
- Post-operative complications include infection, sepsis. The surgery death rate was 5–10% in 2011.[12]
- Acute or chronic graft rejection
- Atrial arrhythmia
- Lymphoproliferative malignancy
- Increased risk of secondary infections due to immunosuppressive medication
- Serum sickness due to anti-thymocyte globulin
- Tricuspid valve regurgitation Repeated endomyocardial biopsy can cause
- Bleeding and thrombosis [14]
Rejection
Since the transplanted heart originates from another organism, the recipient's immune system typically attempts to reject it. The risk of rejection never fully goes away, and the person will be on immunosuppressive drugs for the rest of their life. These drugs may cause unwanted side effects, such as an increased likelihood of infections or the development of certain cancers. Recipients can acquire kidney disease from a heart transplant due to the side effects of immunosuppressant medications. Many recent advances in reducing complications due to tissue rejection stem from mouse heart transplant procedures.[15]
People who have had heart transplants are monitored in various ways to test for the development of rejection.[16]
During heart transplant, the vagus nerve is severed, thus removing parasympathetic influence over the myocardium. However, some limited return of sympathetic nerves has been demonstrated in humans.[17]
Procedure
There are generally two types of procedure; orthotopic, involving removing the recipient's heart and implanting the donor's heart in the chest of the recipient, and heterotopic, involving leaving the recipient's heart where it is and attaching the donor heart to it.[18] Equipment required includes carefully selected recipient and donor, cardiopulmonary bypass, surgical instruments and qualified personnel.[18]
Donor retrieval

The donor is fully heparinised before the heart is retrieved and placed in cold saline in an insulated organ transport box.[1] Ischemic time is ideally limited to around 4 hours or less.[19]
Organ implantation
The orthotopic procedure is when the donor heart is placed in the same spot as the persons prior heart.[1] It can biatrial or bicaval.[1] An alternative less commonly performed method is heterotopic.[1] There is also the domino transplant.[20] A heart transplant may be combined with a lung, liver or kidney transplant.[1]
Bicaval
The more common method is bi-caval.[1]
Biatrial
Domino
The explanted heart from the recipient of a combined heart-lung recipient is used as a donor heart for a second recipient.[20]
Heterotopic
A heterotopic (“piggy-backed”) procedure may be done to assist left ventricular function, and involves leaving the prior heart in place while joining the donor heart to its right.[3]
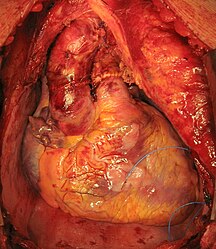
-
Transplanted heart in the thorax of recipient
Post-procedure
-
Chest scar after heart transplant
-
Chest X-ray: unusual heart contour due to a heterotopic heart transplantation. There is a native heart with a left ventricular aneurysm on the left, and the slightly smaller donor heart next to it on the right.
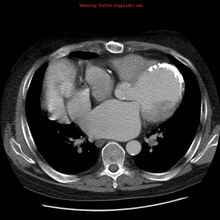
-
CT chest: demonstrates the left anatomic connections in a heterotopic transplant
Outcome
Expected survival after surgery at one year is greater than 90% and at five years is 75%.[2] In transplants carried out between 1992 and 2001, the greatest risk of death is in the first year after the procedure, and the average survival is 11 years.[1] If a person survives the first year, the average survival increases to 13 years.[1] If the another heart transplant is repeated at a later date, the risks of death are higher.[1]
In 2007, researchers from the Johns Hopkins University School of Medicine discovered that "men receiving female hearts had a 15% increase in the risk of adjusted cumulative mortality" over five years compared to men receiving male hearts. Survival rates for women did not significantly differ based on male or female donors.[21]
Frequency
As of 2020 more than 120,000 heart transplants have been performed since the first in 1967.[1] More than 5,000 heart transplants are performed each year worldwide.[4] More than half are performed in the US.[8]
History
In 1907, Simon Flexner wrote the paper "Tendencies in Pathology," in which he said that it would be possible one day by surgery to replace diseased human organs – including arteries, stomach, kidneys and heart.[22]
Early heart transplantations
The world's first human-to-human heart transplant was performed on Louis Washkansky on 3 December 1967 at Groote Schuur Hospital, South Africa, by Christiaan Barnard, utilizing the techniques developed by American surgeons Norman Shumway and Richard Lower.[23][24] Washkansky, however, died 18 days later from pneumonia.[25][26] Barnard later modified the orthotropic biatrial method to preserve the sino-atrial node.[27]
On 6 December 1967, at Maimonides Hospital in Brooklyn, New York, Adrian Kantrowitz performed the world's first heart transplant in a baby.[28][29] The infant's new heart stopped beating after 7 hours and could not be restarted. At a following press conference, Kantrowitz emphasized that he did not consider the operation a success.[30] Norman Shumway performed the first adult heart transplant in the US on 6 January 1968, at the Stanford University Hospital.[31] The fourth surgeon in the world to attempt the surgery was P. K. Sen, who performed the world's sixth human heart transplant in India on 16 February 1968.[31] A team led by Donald Ross performed the first heart transplant in the United Kingdom on 3 May 1968.[32] Worldwide, more than 100 transplants were performed by various doctors during 1968.[33] Only a third of these patients lived longer than three months.[34] In response to the poor results in most units around the world during the years following Barnard's first transplant, the UK announced a clinical moratorium on heart transplants in 1973. It was felt at the time that cardiac transplantation required more research into the management of rejection, more donors and a change in public opinion. Shumway's and Barnard's units continued.[35]
Later years
The introduction cyclosporine in 1983 allowed much smaller amounts of corticosteroids to be used to prevent many cases of rejection (the "corticosteroid-sparing" effect of cyclosporine).[36]
On June 9, 1984, "JP" Lovette IV of Denver, Colorado, became the world's first successful pediatric heart transplant. Columbia-Presbyterian Medical Center surgeons transplanted the heart of 4-year-old John Nathan Ford of Harlem into 4-year-old JP a day after the Harlem child died of injuries received in a fall from a fire escape at his home. JP was born with multiple heart defects. The transplant was done by a surgical team led by Eric Rose of the New York–Presbyterian Hospital. Reemtsma and Fred Bowman were also members of the team for the six-hour operation.[37]
In 1988, the first "domino" heart transplant was performed, in which a patient in need of a lung transplant with a healthy heart will receive a heart-lung transplant, and their original heart will be transplanted into someone else.[38]
Sri Lanka's first heart transplant was successfully performed at the Kandy General Hospital on 7 July 2017.[39]
Cross-species transplantation
In 1963, American surgeon James Hardy, who had carried out the first human lung transplantation, visited Keith Reemtsma and was impressed by the outcome of his chimpanzee kidney transplantations.[40] On 24 January 1964, Hardy became the first to transplant a heart into a human when he transplanted a chimpanzee heart into the chest of dying Boyd Rush.[41][42] Hardy used a defibrillator to shock the heart to restart beating, but he survived less than 2 hours.[40] Author Donald McRae states that Hardy could feel the "icy disdain" from fellow surgeons at the Sixth International Transplantation Conference several weeks after this attempt with the chimpanzee heart.[43] The consent form Hardy asked Rush's stepsister to sign did not include the possibility that a chimpanzee heart might be used, although Hardy stated that he did include this in verbal discussions.[42][44]
The great disparity between the number of people needing transplants and the number of procedures being performed spurred research into the transplantation of non-human hearts into humans after 1993. Xenografts from other species and artificial hearts are two less successful alternatives to allografts.[45]
In 1997 Dhaniram Baruah of Assam, India was arrested for transplanting a pig's heart into a 32-year old man, who died on the eighth day after surgery.[46] On 7 January 2022, with a one-off approval by the United States Food and Drug Administration on grounds of compassionate use in a person who had no other option, David Bennett, aged 57, of Maryland became the first person to receive a gene-edited pig heart in a transplant led by Bartley P. Griffith at the University of Maryland Medical Center.[47]
Research directions
Ex vivo machine perfusion is an emerging technology under investigation to create a similar environment around a beating donor heart while simultaneously keeping it warm.[48] It is being trialled in Australia,[49] the UK,[50] and others.[51]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 Page, Aravinda; Abu-Omar, Abu (2020). "70. Heart transplantation". In Raja, Shahzad G. (ed.). Cardiac Surgery: A Complete Guide. Switzerland: Springer. pp. 639–644. ISBN 978-3-030-24176-6. Archived from the original on 2023-11-13. Retrieved 2023-11-12.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 Bunce, Nicholas H.; Ray, Robin; Patel, Hitesh (2020). "30. Cardiology". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. p. 1076. ISBN 978-0-7020-7870-5. Archived from the original on 2022-02-15. Retrieved 2022-02-15.
- ↑ 3.0 3.1 3.2 3.3 Arora, Sonali; Attawar, Sandeep (3 October 2021). "Current Status of Cardiac Transplantation in the 21st Century". Indian Journal of Clinical Cardiology: 263246362110452. doi:10.1177/26324636211045223. ISSN 2632-4636. Archived from the original on 16 February 2022. Retrieved 16 February 2022.
- ↑ 4.0 4.1 4.2 4.3 Sai Kiran Bhagra; Stephen Pettit; Jayan Parameshwar (2019), "Cardiac transplantation: indications, eligibility and current outcomes", Heart, British Medical Journal, 105 (3): 252–260, doi:10.1136/heartjnl-2018-313103, PMID 30209127, S2CID 52194404, archived from the original on 2022-01-11, retrieved 2022-01-25
- ↑ Jungschleger, JGM; Boldyrev, SY; Kaleda, VI; Dark, JH (January 2018). "Standard orthotopic heart transplantation". Annals of cardiothoracic surgery. 7 (1): 169–171. doi:10.21037/acs.2018.01.18. PMID 29492395.
- ↑ 6.0 6.1 Mantha, Aditya; Lee, Ramon O.; Wolfson, Aaron M. (1 February 2022). "Patient selection for heart transplant: balancing risk". Current Opinion in Organ Transplantation. 27 (1): 36–44. doi:10.1097/MOT.0000000000000943. ISSN 1531-7013. PMID 34939963. Archived from the original on 14 February 2022. Retrieved 14 February 2022.
- ↑ Burch M.; Aurora P. (2004). "Current status of paediatric heart, lung, and heart-lung transplantation". Archives of Disease in Childhood. 89 (4): 386–89. doi:10.1136/adc.2002.017186. PMC 1719883. PMID 15033856.
- ↑ 8.0 8.1 8.2 Cook JA, Shah KB, Quader MA, et al. (2015). "The total artificial heart". Journal of Thoracic Disease. 7 (12): 2172–80. doi:10.3978/j.issn.2072-1439.2015.10.70. PMC 4703693. PMID 26793338.
- ↑ "Heart Transplant | NHLBI, NIH". www.nhlbi.nih.gov. Archived from the original on 15 January 2022. Retrieved 20 February 2022.
- ↑ Mehra MR, Canter CE, Hannan MM, Semigran MJ, Uber PA, et al. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: A 10-year update. J Heart Lung Transplant. 2016 Jan. 35 (1):1–23.
- ↑ Ludhwani, Dipesh; Fan, Ji; Kanmanthareddy, Arun (2020). "Heart Transplantation Rejection". StatPearls. PMID 30725742. Archived from the original on 11 January 2022. Retrieved 25 June 2020 – via NCBI Bookshelf.
{{cite journal}}: Cite journal requires|journal=(help) Last Update: December 23, 2019. - ↑ Jung SH, Kim JJ, Choo SJ, Yun TJ, Chung CH, Lee JW (2011). "Long-term mortality in adult orthotopic heart transplant recipients". J. Korean Med. Sci. 26 (5): 599–603. doi:10.3346/jkms.2011.26.5.599. PMC 3082109. PMID 21532848.
- ↑ Shanmuganathan, Mayooran; Dar, Owais (2020). "73. Complications of heart transplantation". In Raja, Shahzad G. (ed.). Cardiac Surgery: A Complete Guide. Switzerland: Springer. p. 669. ISBN 978-3-030-24176-6. Archived from the original on 2022-02-12. Retrieved 2022-02-13.
- ↑ Rizk J, Mehra MR. Anticoagulation management strategies in heart transplantation. Prog Cardiovasc Dis. 2020;63(3):210–18. doi:10.1016/j.pcad.2020.02.002
- ↑ Bishay R (2011). "The 'Mighty Mouse' Model in Experimental Cardiac Transplantation". Hypothesis. 9 (1): e5.
- ↑ Costanzo MR, Dipchand A, Starling R, Anderson A, Chan M, Desai S, Fedson S, Fisher P, et al. (2010). "The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients". The Journal of Heart and Lung Transplantation. 29 (8): 914–56. doi:10.1016/j.healun.2010.05.034. PMID 20643330.
- ↑ Arrowood, James A.; Minisi, Anthony J.; Goudreau, Evelyne; Davis, Annette B.; King, Anne L. (1997-11-18). "Absence of Parasympathetic Control of Heart Rate After Human Orthotopic Cardiac Transplantation". Circulation. 96 (10): 3492–98. doi:10.1161/01.CIR.96.10.3492. ISSN 0009-7322. PMID 9396446. Archived from the original on 2018-06-12. Retrieved 2022-01-25.
- ↑ 18.0 18.1 Ahmed, Talha; Jain, Ankit (2022). "Heart Transplantation". StatPearls. StatPearls Publishing. PMID 32491503. Archived from the original on 2022-02-22. Retrieved 2022-02-22.
- ↑ John, Ranjit; Liao, Kenneth (1 June 2010). "Orthotopic Heart Transplantation". Operative Techniques in Thoracic and Cardiovascular Surgery. 15 (2): 138–146. doi:10.1053/j.optechstcvs.2010.04.001. ISSN 1522-2942. Archived from the original on 18 February 2022. Retrieved 18 February 2022.
- ↑ 20.0 20.1 Shudo, Yasuhiro; Ma, Michael; Boyd, Jack H.; Woo, Yiping Joseph (March 2017). "Current status of domino heart transplantation". Journal of Cardiac Surgery. 32 (3): 229–232. doi:10.1111/jocs.13104. ISSN 1540-8191. PMID 28219115. Archived from the original on 2022-02-23. Retrieved 2022-02-23.
- ↑ Weiss, E. S.; Allen, J. G.; Patel, N. D.; Russell, S. D.; Baumgartner, W. A.; Shah, A. S.; Conte, J. V. (2009). "The Impact of Donor-Recipient Sex Matching on Survival After Orthotopic Heart Transplantation: Analysis of 18 000 Transplants in the Modern Era". Circulation: Heart Failure. 2 (5): 401–08. doi:10.1161/CIRCHEARTFAILURE.108.844183. PMID 19808369.
- ↑ May Transplant the Human Heart Archived 2021-10-28 at the Wayback Machine (.PDF), The New York Times, January 2, 1908.
- ↑ Hamilton, David (2012). "16. Brain death and the year of the heart". A History of Organ Transplantation: Ancient Legends to Modern Practice. Pittsburgh: University of Pittsburgh Press. pp. 340–358. ISBN 978-0-8229-4413-3. Archived from the original on 2022-02-20. Retrieved 2022-02-20.
- ↑ Cooper, David (2017). "9. Life's defining moment: the first human-to-human heart transplant". Christiaan Barnard:: The Surgeon Who Dared. Fonthill Media. pp. 175–214. ISBN 978-178155-639-9. Archived from the original on 2022-02-21. Retrieved 2022-02-21.
- ↑ McRae, D. (2006). Every Second Counts: The Race to Transplant the First Human Heart, New York: Penguin (Berkley/Putnam).
- ↑ "First U.S. Human-to-Human Heart Transplant". Wayne State University Digital Collections. Archived from the original on 14 November 2017. Retrieved 20 February 2022.
- ↑ Jungschleger, Jérôme G. M.; Boldyrev, Sergey Yu; Kaleda, Vasily I.; Dark, John H. (January 2018). "Standard orthotopic heart transplantation". Annals of Cardiothoracic Surgery. 7 (1): 16971–16171. doi:10.3978/16440. ISSN 2304-1021. Archived from the original on 2021-10-03. Retrieved 2022-02-20.
- ↑ "First U.S. Human-to-Human Heart Transplant". Wayne State University Digital Collections. Archived from the original on 14 November 2017. Retrieved 20 February 2022.
- ↑ Lyons, Richard D. "Heart Transplant Fails to Save 2-Week-old Baby in Brooklyn; Heart Transplant Fails to Save Baby Infants' Surgery Harder Working Side by Side Gives Colleague Credit" Archived 2021-08-28 at the Wayback Machine, The New York Times, December 7, 1967. Accessed November 19, 2008.
- ↑ Heart: An American Medical Odyssey, Dick Cheney, Richard B. Cheney, Jonathan Reiner, MD, with Liz Cheney, Scribner (division of Simon & Schuster), 2013. "Three days later, on December 6, 1967, Dr. Adrian Kantrowitz" Archived September 30, 2021, at the Wayback Machine
- ↑ 31.0 31.1 Jones, David S.; Sivaramakrishnan, Kavita (10 January 2018). "Transplant Buccaneers: P.K. Sen and India's First Heart Transplant, February 1968". Journal of the History of Medicine and Allied Sciences. 73 (3): 303–332. doi:10.1093/jhmas/jrx059. PMID 29329407.(subscription required)
- ↑ Early heart transplant surgery in the UK : witness seminar transcript. London: Wellcome Trust. 1999. ISBN 978-1-84129-007-2.
- ↑ Major Medical Milestones Leading Up To the First Human Heart Transplantation Archived 2016-07-14 at the Wayback Machine, Kate Elzinga, from Proceedings of the 18th Annual History of Medicine Days Conference 2009: The University of Calgary Faculty of Medicine, Alberta, Canada, Cambridge Scholars Publishing, 2011. " . . following Barnard's landmark heart transplantation on December 3, 1967, 107 human heart transplants were performed by 64 surgical teams in 24 countries in 1968. . "
- ↑ The Adrian Kantrowitz Papers, Replacing Hearts: Left Ventricle Assist Devices and Transplants, 1960–1970 Archived 2018-01-06 at the Wayback Machine, National Institutes of Health, U.S. National Library of Medicine.
- ↑ Tansey, EM; Reynolds, LA (September 1999). "Early Heart Transplant Surgery in the UK" (PDF). Wellcome Witnesses to Twentieth Century Medicine. Archived (PDF) from the original on 2021-08-31. Retrieved 2022-02-20 – via Queen Mary, University of London.
- ↑ Transplantation of the heart: An overview of 40 years' clinical and research experience at Groote Schuur Hospital and the University of Cape Town Archived 2021-10-22 at the Wayback Machine, South African Medical Journal, "Part I. Surgical experience and clinical studies." J Hassoulas, Vol. 102, No. 6 (2012).
- ↑ "Talk About a Guy With a Lot of Heart 1st kid to get new ticker wants to be doc" Archived 2021-04-26 at the Wayback Machine NY Daily News, 13 April 2003
- ↑ Raffa, G.M.; Pellegrini, C.; Viganò, M. (November 2010). "Domino Heart Transplantation: Long-Term Outcome of Recipients and Their Living Donors: Single Center Experience". Transplantation Proceedings. 42 (9): 3688–93. doi:10.1016/j.transproceed.2010.09.002. PMID 21094839.
- ↑ First ever heart transplant in Sri Lanka successful Archived 2021-10-03 at the Wayback Machine, Hiru News, 9 July 2017.
- ↑ 40.0 40.1 Cooper, David K. C. (January 2012). "A brief history of cross-species organ transplantation". Proceedings (Baylor University. Medical Center). 25 (1): 49–57. doi:10.1080/08998280.2012.11928783. ISSN 0899-8280. PMC 3246856. PMID 22275786.
- ↑ Hardy James D.; Chavez Carlos M.; Kurrus Fred D.; Neely William A.; Eraslan Sadan; Turner M. Don; Fabian Leonard W.; Labecki Thaddeus D. (1964). "Heart Transplantation in Man". JAMA. 188 (13). doi:10.1001/jama.1964.03060390034008.
- ↑ 42.0 42.1 Every Second Counts: The Race to Transplant the First Human Heart, Donald McRae, New York: Penguin (Berkley/Putnam), 2006, Ch. 7 "Mississippi Gambling" Archived 2021-10-01 at the Wayback Machine, pp. 123–27. This source states the heartbeat for approximately one hour.
- ↑ Every Second Counts, McRae, page 126, top Archived 2021-10-01 at the Wayback Machine.
- ↑ Xenotransplantation: Law and Ethics, Sheila McLean, Laura Williamson, University of Glasgow, UK, Ashgate Publishing, 2005, p. 50 Archived 2021-09-30 at the Wayback Machine.
- ↑ Till Lehmann (director) (2007). The Heart-Makers: The Future of Transplant Medicine (documentary film). Germany: LOOKS film and television.
- ↑ Daar, Abdallah S. (1999). "9. Xenotransplantation: science, risk and international regulatory efforts". In Caulfield, Timothy A.; Williams-Jones, Bryn (eds.). The Commercialization of Genetic Research: Ethical, Legal, and Policy Issues. New York: Springer. pp. 216–217. ISBN 978-1-4613-7135-9. Archived from the original on 2022-02-20. Retrieved 2022-02-20.
- ↑ Sade, Robert M.; Mukherjee, Rupak (1 March 2022). "Ethical Issues in Xenotransplantation: The First Pig-to-Human Heart Transplant". The Annals of Thoracic Surgery. 113 (3): 712–714. doi:10.1016/j.athoracsur.2022.01.006. ISSN 0003-4975. Archived from the original on 21 February 2022. Retrieved 20 February 2022.
- ↑ Pinnelas, Rebecca; Kobashigawa, Jon A (1 January 2022). "Ex vivo normothermic perfusion in heart transplantation: a review of the TransMedics® Organ Care System". Future Cardiology. 18 (1): 5–15. doi:10.2217/fca-2021-0030. ISSN 1479-6678. PMID 34503344. Archived from the original on 21 February 2022. Retrieved 20 February 2022.
- ↑ Woods, Emily (2021-10-11). "Donor hearts given longer life under trial". The Canberra Times. Australian Associated Press. Archived from the original on 2022-01-13. Retrieved 2022-01-25.
- ↑ "The technology: OCS Heart system for heart transplant | Advice | NICE". www.nice.org.uk. Archived from the original on 25 February 2021. Retrieved 20 February 2022.
- ↑ Verzelloni Sef, A; Sef, D; Garcia Saez, D; Trkulja, V; Walker, C; Mitchell, J; McGovern, I; Stock, U (1 August 2021). "Heart Transplantation in Adult Congenital Heart Disease with the Organ Care System Use: A 4-Year Single-Center Experience". ASAIO Journal. 67 (8): 862–868. doi:10.1097/MAT.0000000000001482. ISSN 1058-2916. PMID 34039886. S2CID 235217756.
External links
- Photograph of first U.S. heart transplant Archived 2021-10-06 at the Wayback Machine