Adenoviral keratoconjunctivitis
| Adenoviral keratoconjunctivitis | |
|---|---|
| Other names: Epidemic keratoconjunctivitis, keratoconjunctivitis epidemica, pink eye[1] | |
 | |
| Adenoviral keratoconjunctivitis | |
| Specialty | Ophthalmology, infectious diseases |
| Symptoms | Painful red eye, discomfort/irritation, sensitivity to light, watering, blurred vision, discharge[2] |
| Complications | Corneal scarring[3] |
| Usual onset | Sudden in an adult[4] |
| Duration | 7-10 days, can be longer[4] |
| Causes | Adenoviruses, commonly types 8 and 37[4] |
| Diagnostic method | Visualisation, viral culture (with immunofluorescence staining), PCR[4] |
| Differential diagnosis | Herpes simplex type I, acanthamoeba, fungal infection[5] |
| Prevention | Hand washing,[4] adenovirus vaccine (military personnel)[4] |
| Treatment | Usually none, cold compress, artificial tears[3] |
| Frequency | Epidemics, common, adults>children[3] |
Adenoviral keratoconjunctivitis, also known as epidemic keratoconjunctivitis, is a type of adenovirus disease presenting as an eye infection.[6] It typically begins in one eye with sudden onset of redness, watery discharge, and feeling that something is in the eye.[2] There may also be eye pain, intolerance to light, blurry vision, and swollen glands by the ear near the affected eye.[3][7] It is associated with a sore throat and stuffy and runny nose, mainly in adults.[4] In young children high fever, sore throat, ear infection, vomiting, and diarrhea may also occur.[4]
It is commonly caused by adenovirus types 8 and 37.[4] It is contagious and spread by contaminated eye examination instruments and eye solutions, touching eyes by infected people, inadequately chlorinated swimming pools, or other contaminated objects.[4] The time between contact and onset of symptoms is around 5–10 days.[4] Diagnosis is usually based on symptoms and examination.[1]
Usually, the condition is better after 7 to 10-days, with no specific treatment required.[4] Cold compresses and artificial tears may help.[3] Corneal scarring occurs in up to half of cases and the blurred vision may continue for a long time in some people.[3] The virus may remain in the eye for 2 to 3-years after recovering.[4]
Globally it is a common cause of a red eye and tends to occur in large numbers of people at the same time.[3] Adults tend to be affected more frequently than children.[4]
Signs and symptoms

It typically begins in one eye with sudden onset of redness, watery discharge, and feeling that something is in the eye.[2] The eye may be very painful.[7] It then develops with intolerance to light, blurred vision and swollen glands by the ear nearest the affected eye.[3] It may spread to the other eye.[2] The condition is part of adenovirus disease, where it is often associated with a sore throat and stuffy and runny nose, mainly in adults.[4] A type of adenoviral keratoconjunctivitis in very small children can present with a high fever, sore throat, ear infection, vomiting and diarrhea.[4]
Cause
It is commonly caused by types 8 and 37 adenoviruses, spread by contaminated eye examination instruments and eye solutions, touching eyes by infected people, from inadequately chlorinated swimming pools, or other contaminated objects.[4] Onset of symptoms is generally around 5–10 days after exposure.[4] From the onset of symptoms, people remain contagious for about 2 weeks.[1]
Diagnosis

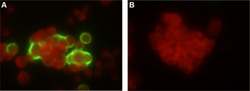
Diagnosis is usually based on symptoms and examination.[1] Occasionally, it may be confirmed by cell culture (with immunofluorescence staining) or PCR.[5]
It may appear similar to herpes simplex type I, acanthamoeba, and fungal infection.[5]
-
Adenovirus in the HEp-2 cells derived from swab samples (by indirect immunofluorescence assay).
Prevention
Adequate infection control measures should be followed as prevention and to reduce epidemic AKC outbreaks.[8]
Treatment
There is currently no effective treatment of the acute phase of AKC.[1] Measures like application of a cool cloth or artificial tears may help with the symptoms.[1]
Topical cidofovir may reduce the incidence of corneal opacities, but local toxicity rules out its use. NMSO3, a sulfated sialyl lipid, has demonstrated a greater antiviral potency against adenovirus in vitro than cidofovir exhibiting minimal cytotoxicity.[9] Topical cyclosporin A (CsA) appears to be effective in for persistent corneal opacities. Topical interferon might be effective to prevent infection; though is not commercially available due to unsettled patent issues.
Topical steroids should be avoided because they prolong viral replication, frequently lead to long-lasting dry eye symptoms, and corneal opacities almost always recur after discontinuation of topical steroids.
Epidemiology
Globally it is a common cause of a red eye and tends to occur in large numbers of people at the same time.[3] Adults tend to be affected more frequently than children.[4]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Epidemic Keratoconjunctivitis - EyeWiki". eyewiki.aao.org. Archived from the original on 1 February 2022. Retrieved 10 May 2022.
- ↑ 2.0 2.1 2.2 2.3 Burrow, Michael K.; Patel, Bhupendra C. (2022). "Keratoconjunctivitis". StatPearls. StatPearls Publishing. PMID 31194419.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Bawazeer, Ahmed (4 June 2019). "Epidemic Keratoconjunctivitis (EKC)". Medscape. Archived from the original on 21 April 2021. Retrieved 16 July 2021.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 Shieh, Wun-Ju (10 September 2021). "Human adenovirus infections in pediatric population - An update on clinico-pathologic correlation". Biomedical Journal: S2319–4170(21)00109–8. doi:10.1016/j.bj.2021.08.009. ISSN 2320-2890. PMID 34506970. Archived from the original on 24 April 2022. Retrieved 23 April 2022.
- ↑ 5.0 5.1 5.2 Pihos, Andria M. (April 2013). "Epidemic keratoconjunctivitis: A review of current concepts in management". Journal of Optometry. 6 (2): 69–74. doi:10.1016/j.optom.2012.08.003. ISSN 1888-4296. Archived from the original on 8 November 2021. Retrieved 8 November 2021.
- ↑ Ison, Michael G. (2019). "341. Adenovirus diseases". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine (26th ed.). Elsevier. p. 2163. ISBN 978-0-323-55087-1. Archived from the original on 2022-04-28. Retrieved 2022-04-27.
- ↑ 7.0 7.1 Flint, S. Jane; Nemerow, Glen R. (2017). "8. Pathogenesis". Human Adenoviruses: From Villains To Vectors. Singapore: World Scientific. p. 153-183. ISBN 978-981-310-979-7. Archived from the original on 2022-05-05. Retrieved 2022-05-05.
- ↑ Reinhard, Thomas; Larkin, Frank (28 January 2006). Cornea and External Eye Disease. google.com.au. ISBN 9783540312260. Archived from the original on 8 November 2021. Retrieved 22 March 2015.
- ↑ Kaneko H; et al. (2001). "Antiviral activity of NMSO3 against adenovirus in vitro". Antiviral Res. 52 (3): 281–8. doi:10.1016/s0166-3542(01)00167-x. PMID 11675145.