Video:Cystic fibrosis
| Cystic fibrosis (Tutorial) | |
|---|---|
| Commons / NC | |
| Steps for video creation | |
| Step 1 | Preview my changes (10 sec) |
| Step 2 | Upload to Commons (10 min) |
Definition
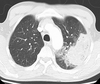
Cystic fibrosis (or CF for short) is a genetic disorder that affects mostly the lungs, but also the pancreas, liver, kidneys, and intestines.[1][2]

Symptoms
Long-term issues include difficulty breathing, and coughing up mucus, as a result of frequent lung infections.[1]
Other symptoms
Other signs and symptoms may include sinus infections, poor growth, fatty stool, clubbing of the fingers and toes, and infertility in most males.[1]

Cause
CF is inherited in an autosomal recessive manner.[1]

Mechanism of genetic defect
It is caused by the presence of mutations in both copies of the gene for the cystic fibrosis transmembrane conductance regulator, (or CFTR) protein.[1]
Carriers
Those with a single working copy of CFTR, are carriers, and otherwise mostly normal.[3]

Systems affected by genetic defect
CFTR is involved in the production of sweat, digestive fluids, and mucus.[4]

Effects of genetic defect
When the CFTR is not functional, secretions which are usually thin, become thick.[5]

Diagnosis
The condition is diagnosed by a sweat test, and genetic testing.[1] In parts of the world, where the defect in the gene is very common, screening of infants at birth with a sweat test may take place.[1]

Treatment
There is no known cure for cystic fibrosis,[3] and the most common complications come from lung infections.

Treatment of pneumonia
Acute lung infections are treated with antibiotics, which may be given intravenously, inhaled, or by mouth.[1]

Physiotherapy
Airway clearance techniques, such as chest physiotherapy have some short-term benefit, but the long-term effects are unclear.[6]

Prevention of lung infections
Sometimes, when someone has repeated infections, the antibiotic azithromycin is used long term.[1] Inhaled hypertonic saline, and salbutamol, may also be useful.[1]

Lung transplant
and lung transplantation may be an option, when lung function becomes very poor.[1]

Pancreatic enzyme replacement
Aside from treatment of the lungs, pancreatic enzyme replacement, and fat-soluble vitamin supplementation are also important, especially in the young.[1]

Prognosis
The average life expectancy, for those affected by CF, is between 42, and 50 years, in the developed world,[7][8] with lung problems being responsible for roughly 80% of related deaths.[1]

Epidemiology
CF is most common among people of Northern European ancestry, and affects about one out of every 3,000 newborns.[1] In addition, about one in 25 people in Northern Europe is a CF gene carrier.[3] The disease is least common in Africans, and Asians.[1]

History
Cystic fibrosis was first recognized as a specific disease, by Dorothy Andersen, in 1938, although descriptions of conditions that fit the disease, have been found as far back as the year 1595.[2]

Etymology
The name "cystic fibrosis" refers to the characteristic scarring (fibrosis), and cysts, that form within the pancreas.[2][9]

References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 O'Sullivan, BP; Freedman, SD (30 May 2009). "Cystic fibrosis". Lancet. 373 (9678): 1891–904. doi:10.1016/s0140-6736(09)60327-5. PMID 19403164.
- ↑ 2.0 2.1 2.2 Hodson, Margaret; Geddes, Duncan; Bush, Andrew, eds. (2012). Cystic fibrosis (3rd ed.). London: Hodder Arnold. p. 3. ISBN 978-1-4441-1369-3. Archived from the original on 2017-09-08.
- ↑ 3.0 3.1 3.2 Massie, J; Delatycki, MB (December 2013). "Cystic fibrosis carrier screening". Paediatric Respiratory Reviews. 14 (4): 270–5. doi:10.1016/j.prrv.2012.12.002. PMID 23466339.
- ↑ Buckingham, Lela (2012). Molecular diagnostics fundamentals, methods, and clinical applications (2nd ed.). Philadelphia: F.A. Davis Co. p. 351. ISBN 978-0-8036-2975-2. Archived from the original on 2017-09-08.
- ↑ Yankaskas JR, Marshall BC, Sufian B, Simon RH, Rodman D (2004). "Cystic fibrosis adult care consensus conference report". Chest. 125 (90010): 1–39. CiteSeerX 10.1.1.562.1904. doi:10.1378/chest.125.1_suppl.1S. PMID 14734689.
- ↑ Warnock, L.; Gates, A. (21 December 2015). "Chest physiotherapy compared to no chest physiotherapy for cystic fibrosis". The Cochrane Database of Systematic Reviews (12): CD001401. doi:10.1002/14651858.CD001401.pub3. PMID 26688006.
- ↑ Ong, T; Ramsey, BW (15 September 2015). "Update in Cystic Fibrosis 2014". American Journal of Respiratory and Critical Care Medicine. 192 (6): 669–75. doi:10.1164/rccm.201504-0656UP. PMID 26371812.
- ↑ Nazareth, D; Walshaw, M (October 2013). "Coming of age in cystic fibrosis - transition from paediatric to adult care". Clinical Medicine. 13 (5): 482–6. doi:10.7861/clinmedicine.13-5-482. PMC 4953800. PMID 24115706.
- ↑ Andersen DH (1938). "Cystic fibrosis of the pancreas and its relation to celiac disease: a clinical and pathological study". Am J Dis Child. 56 (2): 344–399. doi:10.1001/archpedi.1938.01980140114013.