Secretin
Secretin is a hormone that regulates water homeostasis throughout the body and influences the environment of the duodenum by regulating secretions in the stomach, pancreas, and liver. It is a peptide hormone produced in the S cells of the duodenum, which are located in the intestinal glands.[3] In humans, the secretin peptide is encoded by the SCT gene.[4]
Secretin helps regulate the pH of the duodenum by inhibiting the secretion of gastric acid from the parietal cells of the stomach and stimulating the production of bicarbonate from the ductal cells of the pancreas.[5][6] It also stimulates the secretion of bicarbonate and water by cholangiocytes in the bile duct, protecting it from bile acids by controlling the pH and promoting the flow in the duct.[7] Meanwhile, in concert with secretin's actions, the other main hormone simultaneously issued by the duodenum, cholecystokinin (CCK), stimulates the gallbladder to contract, delivering its stored bile.
Prosecretin is a precursor to secretin, which is present in digestion. Secretin is stored in this unusable form, and is activated by gastric acid. This indirectly results in the neutralisation of duodenal pH, thus ensuring no damage is done to the small intestine by the aforementioned acid.[8]
In 2007, secretin was discovered to play a role in osmoregulation by acting on the hypothalamus, pituitary gland, and kidney.[9][10]
History
In 1902, William Bayliss and Ernest Starling were studying how the nervous system controls the process of digestion.[11] It was known that the pancreas secreted digestive juices in response to the passage of food (chyme) through the pyloric sphincter into the duodenum. They discovered (by cutting all the nerves to the pancreas in their experimental animals) that this process was not, in fact, governed by the nervous system. They determined that a substance secreted by the intestinal lining stimulates the pancreas after being transported via the bloodstream. They named this intestinal secretion secretin. This type of 'chemical messenger' substance is now called a hormone, a term coined by Starling in 1905.[12]
Secretin is frequently erroneously stated to have been the first hormone identified.[13] However, British researchers George Oliver and Edward Albert Schäfer had already published their findings of an adrenal extract increasing blood pressure and heart rate in brief reports in 1894 and a full publication in 1895, making adrenaline the first discovered hormone.[14][15]
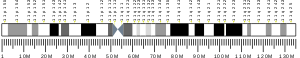
Structure
Secretin is initially synthesized as a 120 amino acid precursor protein known as prosecretin. This precursor contains an N-terminal signal peptide, spacer, secretin itself (residues 28–54), and a 72-amino acid C-terminal peptide.[4]
The mature secretin peptide is a linear peptide hormone, which is composed of 27 amino acids and has a molecular weight of 3055. A helix is formed in the amino acids between positions 5 and 13. The amino acids sequences of secretin have some similarities to that of glucagon, vasoactive intestinal peptide (VIP), and gastric inhibitory peptide (GIP). Fourteen of 27 amino acids of secretin reside in the same positions as in glucagon, 7 the same as in VIP, and 10 the same as in GIP.[16]
Secretin also has an amidated carboxyl-terminal amino acid which is valine.[17] The sequence of amino acids in secretin is H–His-Ser-Asp-Gly-Thr-Phe-Thr-Ser-Glu-Leu-Ser-Arg-Leu-Arg-Asp-Ser-Ala-Arg-Leu-Gln-Arg-Leu-Leu-Gln-Gly-Leu-Val–NH2.[17]
Physiology
Production and secretion
Secretin is synthesized in cytoplasmic secretory granules of S-cells, which are found mainly in the mucosa of the duodenum, and in smaller numbers in the jejunum of the small intestine.[18]
Secretin is released into circulation and/or intestinal lumen in response to low duodenal pH that ranges between 2 and 4.5 depending on species; the acidity is due to hydrochloric acid in the chyme that enters the duodenum from the stomach via the pyloric sphincter.[19] Also, the secretion of secretin is increased by the products of protein digestion bathing the mucosa of the upper small intestine.[20]
Secretin release is inhibited by H2 antagonists, which reduce gastric acid secretion. As a result, if the pH in the duodenum increases above 4.5, secretin cannot be released.[21]
Function
pH regulation
Secretin primarily functions to neutralize the pH in the duodenum, allowing digestive enzymes from the pancreas (e.g., pancreatic amylase and pancreatic lipase) to function optimally.[22]
Secretin targets the pancreas; pancreatic centroacinar cells have secretin receptors in their plasma membrane. As secretin binds to these receptors, it stimulates adenylate cyclase activity and converts ATP to cyclic AMP.[23] Cyclic AMP acts as second messenger in intracellular signal transduction and causes the organ to secrete a bicarbonate-rich fluid that flows into the intestine. Bicarbonate is a base that neutralizes the acid, thus establishing a pH favorable to the action of other digestive enzymes in the small intestine.[24]
Secretin also increases water and bicarbonate secretion from duodenal Brunner's glands to buffer the incoming protons of the acidic chyme,[22] and also reduces acid secretion by parietal cells of the stomach.[25] It does this through at least three mechanisms: 1) By stimulating release of somatostatin, 2) By inhibiting release of gastrin in the pyloric antrum, and 3) By direct downregulation of the parietal cell acid secretory mechanics.[26][19]
It counteracts blood glucose concentration spikes by triggering increased insulin release from pancreas, following oral glucose intake.[27]
Osmoregulation
Secretin modulates water and electrolyte transport in pancreatic duct cells,[28] liver cholangiocytes,[29] and epididymis epithelial cells.[30] It is found[31] to play a role in the vasopressin-independent regulation of renal water reabsorption.[9]
Secretin is found in the magnocellular neurons of the paraventricular and supraoptic nuclei of the hypothalamus and along the neurohypophysial tract to neurohypophysis. During increased osmolality, it is released from the posterior pituitary. In the hypothalamus, it activates vasopressin release.[10] It is also needed to carry out the central effects of angiotensin II. In the absence of secretin or its receptor in the gene knockout animals, central injection of angiotensin II was unable to stimulate water intake and vasopressin release.[32]
It has been suggested that abnormalities in such secretin release could explain the abnormalities underlying type D syndrome of inappropriate antidiuretic hormone hypersecretion (SIADH).[10] In these individuals, vasopressin release and response are normal, although abnormal renal expression, translocation of aquaporin 2, or both are found.[10] It has been suggested that "Secretin as a neurosecretory hormone from the posterior pituitary, therefore, could be the long-sought vasopressin independent mechanism to solve the riddle that has puzzled clinicians and physiologists for decades."[10]
Food intake
Secretin and its receptor are found in discrete nuclei of the hypothalamus, including the paraventricular nucleus and the arcuate nucleus, which are the primary brain sites for regulating body energy homeostasis. It was found that both central and peripheral injection of Sct reduce food intake in mouse, indicating an anorectic role of the peptide. This function of the peptide is mediated by the central melanocortin system.[33]
Uses
Secretin is used in a diagnostic tests for pancreatic function; secretin is injected and the pancreatic output can then be imaged with magnetic resonance imaging, a noninvasive procedure, or secretions generated as a result can gathered either through an endoscope or through tubes inserted through the mouth, down into the duodenum.[34][35][36]
A recombinant human secretin has been available since 2004 for these diagnostic purposes.[37] There were problems with the availability of this agent from 2012 to 2015.[38]
Research
A wave of enthusiasm for secretin as a possible treatment for autism arose in the 1990s based on a hypothetical gut-brain connection; as a result the NIH ran a series of clinical trials that showed that secretin was not effective, which brought an end to popular interest.[39][40][41]
A high-affinity and optimized secretin receptor antagonist (Y10,c[E16,K20],I17,Cha22,R25)sec(6-27) has been designed and developed which has allowed the structural characterization of secreting inactive conformation.[42]
See also
References
- ^ a b c ENSG00000274473 GRCh38: Ensembl release 89: ENSG00000070031, ENSG00000274473 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Häcki WH (September 1980). "Secretin". Clinics in Gastroenterology. 9 (3): 609–632. doi:10.1016/S0300-5089(21)00474-0. PMID 7000396.
- ^ a b Kopin AS, Wheeler MB, Leiter AB (March 1990). "Secretin: structure of the precursor and tissue distribution of the mRNA". Proceedings of the National Academy of Sciences of the United States of America. 87 (6): 2299–2303. Bibcode:1990PNAS...87.2299K. doi:10.1073/pnas.87.6.2299. JSTOR 2354038. PMC 53674. PMID 2315322.
- ^ Whitmore TE, Holloway JL, Lofton-Day CE, Maurer MF, Chen L, Quinton TJ, et al. (2000). "Human secretin (SCT): gene structure, chromosome location, and distribution of mRNA". Cytogenetics and Cell Genetics. 90 (1–2): 47–52. doi:10.1159/000015658. PMID 11060443. S2CID 12850155.
- ^ Costanzo, Linda S. (2006). Physiology (3rd ed.). Philadelphia, PA: Saunders Elsevier. ISBN 9781416023203. OCLC 62326921.
- ^ Banales JM, Huebert RC, Karlsen T, Strazzabosco M, LaRusso NF, Gores GJ (May 2019). "Cholangiocyte pathobiology". Nature Reviews. Gastroenterology & Hepatology. 16 (5): 269–281. doi:10.1038/s41575-019-0125-y. PMC 6563606. PMID 30850822.
- ^ Gafvelin G, Jörnvall H, Mutt V (September 1990). "Processing of prosecretin: isolation of a secretin precursor from porcine intestine". Proceedings of the National Academy of Sciences of the United States of America. 87 (17): 6781–6785. Bibcode:1990PNAS...87.6781G. doi:10.1073/pnas.87.17.6781. PMC 54621. PMID 2395872.
- ^ a b Chu JY, Chung SC, Lam AK, Tam S, Chung SK, Chow BK (April 2007). "Phenotypes developed in secretin receptor-null mice indicated a role for secretin in regulating renal water reabsorption". Molecular and Cellular Biology. 27 (7): 2499–2511. doi:10.1128/MCB.01088-06. PMC 1899889. PMID 17283064.
- ^ a b c d e Chu JY, Lee LT, Lai CH, Vaudry H, Chan YS, Yung WH, Chow BK (September 2009). "Secretin as a neurohypophysial factor regulating body water homeostasis". Proceedings of the National Academy of Sciences of the United States of America. 106 (37): 15961–15966. Bibcode:2009PNAS..10615961C. doi:10.1073/pnas.0903695106. JSTOR 40484830. PMC 2747226. PMID 19805236.
- ^ Bayliss WM, Starling EH (September 1902). "The mechanism of pancreatic secretion". The Journal of Physiology. 28 (5): 325–353. doi:10.1113/jphysiol.1902.sp000920. PMC 1540572. PMID 16992627.
- ^ Hirst BH (October 2004). "Secretin and the exposition of hormonal control". The Journal of Physiology. 560 (Pt 2): 339. doi:10.1113/jphysiol.2004.073056. PMC 1665254. PMID 15308687.
- ^ Henriksen JH, Schaffalitzky de Muckadell OB (January 2002). "[Secretin--the first hormone]" [Secretin--the first hormone]. Ugeskrift for Laeger (in Danish). 164 (3): 320–325. PMID 11816326. INIST 13419424.
- ^ Oliver G, Schäfer EA (July 1895). "The Physiological Effects of Extracts of the Suprarenal Capsules". The Journal of Physiology. 18 (3): 230–276. doi:10.1113/jphysiol.1895.sp000564. PMC 1514629. PMID 16992252.
- ^ Oliver G, Schäfer EA (July 1895). "The Physiological Effects of Extracts of the Suprarenal Capsules". The Journal of Physiology. 18 (3): 230–276. doi:10.1113/jphysiol.1895.sp000564. PMC 1514629. PMID 16992252.
- ^ Williams RL (1981). Textbook of Endocrinology. Philadelphia: Saunders. p. 697. ISBN 978-0-7216-9398-9.
- ^ a b DeGroot LJ (1989). McGuigan JE (ed.). Endocrinology. Philadelphia: Saunders. pp. 2748. ISBN 978-0-7216-2888-2.
- ^ Polak JM, Coulling I, Bloom S, Pearse AG (1971). "Immunofluorescent localization of secretin and enteroglucagon in human intestinal mucosa". Scandinavian Journal of Gastroenterology. 6 (8): 739–744. doi:10.3109/00365527109179946. PMID 4945081.
- ^ a b Frohman LA, Felig P (2001). "Gastrointestinal Hormones and Carcinoid Syndrome". In Ghosh PK, O'Dorisio TM (eds.). Endocrinology & metabolism. New York: McGraw-Hill, Medical Pub. Div. pp. 1675–701. ISBN 978-0-07-022001-0.
- ^ Ganong WF (2003). "Regulation of Gastrointestinal Function". Review of Medical Physiology (21st ed.). New York: McGraw-Hill, Medical Pub. Div. ISBN 978-0-07-140236-1.[page needed]
- ^ Rominger JM, Chey WY, Chang TM (July 1981). "Plasma secretin concentrations and gastric pH in healthy subjects and patients with digestive diseases". Digestive Diseases and Sciences. 26 (7): 591–597. doi:10.1007/BF01367670. PMID 7249893. S2CID 7039025.
- ^ a b Hall JE, Guyton AC (2006). Textbook of medical physiology. St. Louis, Mo: Elsevier Saunders. pp. 800–1. ISBN 978-0-7216-0240-0.
- ^ Gardner JD (1978). "Receptors and gastrointestinal hormones". In Sleisenger MH, Fordtran JS (eds.). Gastrointestinal Disease (2nd ed.). Philadelphia: WB Saunders Company. pp. 179–95.
- ^ Osnes M, Hanssen LE, Flaten O, Myren J (March 1978). "Exocrine pancreatic secretion and immunoreactive secretin (IRS) release after intraduodenal instillation of bile in man". Gut. 19 (3): 180–184. doi:10.1136/gut.19.3.180. PMC 1411891. PMID 631638.
- ^ Palmer KR, Penman ID (2010). "Alimentary track and pancreatic disease". In Colledge NR, Walker BR, Ralston SH (eds.). Davidson's Principles and Practice of Medicine (20th ed.). Edinburgh: Churchill Livingstone. p. 844. ISBN 978-0-7020-3085-7.
- ^ Boron WF, Boulpaep EL (2012). "Acid secretion". Medical Physiology (2nd ed.). Philadelphia: Saunders. p. 1352. ISBN 978-1-4377-1753-2.
- ^ Kraegen EW, Chisholm DJ, Young JD, Lazarus L (March 1970). "The gastrointestinal stimulus to insulin release. II. A dual action of secretin". The Journal of Clinical Investigation. 49 (3): 524–529. doi:10.1172/JCI106262. PMC 322500. PMID 5415678.
- ^ Villanger O, Veel T, Raeder MG (March 1995). "Secretin causes H+/HCO3- secretion from pig pancreatic ductules by vacuolar-type H(+)-adenosine triphosphatase". Gastroenterology. 108 (3): 850–859. doi:10.1016/0016-5085(95)90460-3. PMID 7875488.
- ^ Marinelli RA, Pham L, Agre P, LaRusso NF (May 1997). "Secretin promotes osmotic water transport in rat cholangiocytes by increasing aquaporin-1 water channels in plasma membrane. Evidence for a secretin-induced vesicular translocation of aquaporin-1". The Journal of Biological Chemistry. 272 (20): 12984–12988. doi:10.1074/jbc.272.20.12984. PMID 9148905.
- ^ Chow BK, Cheung KH, Tsang EM, Leung MC, Lee SM, Wong PY (June 2004). "Secretin controls anion secretion in the rat epididymis in an autocrine/paracrine fashion". Biology of Reproduction. 70 (6): 1594–1599. doi:10.1095/biolreprod.103.024257. PMID 14749298. S2CID 1189550.
- ^ Cheng CY, Chu JY, Chow BK (September 2009). "Vasopressin-independent mechanisms in controlling water homeostasis". Journal of Molecular Endocrinology. 43 (3): 81–92. doi:10.1677/JME-08-0123. PMID 19318428.
- ^ Lee VH, Lee LT, Chu JY, Lam IP, Siu FK, Vaudry H, Chow BK (December 2010). "An indispensable role of secretin in mediating the osmoregulatory functions of angiotensin II". FASEB Journal. 24 (12): 5024–5032. doi:10.1096/fj.10-165399. PMC 2992369. PMID 20739612.
- ^ Cheng CY, Chu JY, Chow BK (January 2011). "Central and peripheral administration of secretin inhibits food intake in mice through the activation of the melanocortin system". Neuropsychopharmacology. 36 (2): 459–471. doi:10.1038/npp.2010.178. PMC 3055665. PMID 20927047.
- ^ Lieb JG, Draganov PV (May 2008). "Pancreatic function testing: here to stay for the 21st century". World Journal of Gastroenterology. 14 (20): 3149–3158. doi:10.3748/WJG.14.3149. PMC 2712845. PMID 18506918.
- ^ Domínguez Muñoz JE (June 2010). "Diagnosis of chronic pancreatitis: Functional testing". Best Practice & Research. Clinical Gastroenterology. 24 (3): 233–241. doi:10.1016/j.bpg.2010.03.008. PMID 20510825.
- ^ "Secretin stimulation test". MedlinePlus Medical Encyclopedia. United States National Library of Medicine. Retrieved 2008-11-01.
- ^ "Human Secretin". Patient Information Sheets. United States Food and Drug Administration. 2004-07-13. Archived from the original on May 11, 2009. Retrieved 2008-11-01.
- ^ American Society of Health-System Pharmacists (5 August 2015). "Secretin Injection". Current Drug Shortage Bulletin. Archived from the original on 9 November 2016. Retrieved 9 November 2016.
- ^ Stokstad E (18 July 2008). "News this Week: Stalled Trial for Autism Highlights Dilemma of Alternative Treatments". Science. p. 324.
- ^ "The Use of Secretin to Treat Autism". NIH News Alert. United States National Institutes of Health. 1998-10-16. Retrieved 2008-11-30.
- ^ Sandler AD, Sutton KA, DeWeese J, Girardi MA, Sheppard V, Bodfish JW (December 1999). "Lack of benefit of a single dose of synthetic human secretin in the treatment of autism and pervasive developmental disorder". The New England Journal of Medicine. 341 (24): 1801–1806. doi:10.1056/NEJM199912093412404. PMID 10588965.
- ^ Dong M, Harikumar KG, Raval SR, Milburn JE, Clark C, Alcala-Torano R, et al. (July 2020). "Rational development of a high-affinity secretin receptor antagonist". Biochemical Pharmacology. 177: 113929. doi:10.1016/j.bcp.2020.113929. PMC 7299832. PMID 32217097.
Further reading
- Saus E, Brunet A, Armengol L, Alonso P, Crespo JM, Fernández-Aranda F, et al. (October 2010). "Comprehensive copy number variant (CNV) analysis of neuronal pathways genes in psychiatric disorders identifies rare variants within patients". Journal of Psychiatric Research. 44 (14): 971–978. doi:10.1016/j.jpsychires.2010.03.007. PMID 20398908.[permanent dead link]
- Bertenshaw GP, Turk BE, Hubbard SJ, Matters GL, Bylander JE, Crisman JM, et al. (April 2001). "Marked differences between metalloproteases meprin A and B in substrate and peptide bond specificity". The Journal of Biological Chemistry. 276 (16): 13248–13255. doi:10.1074/jbc.M011414200. PMID 11278902.
- Lee LT, Lam IP, Chow BK (November 2008). "A functional variable number of tandem repeats is located at the 5' flanking region of the human secretin gene plays a downregulatory role in expression". Journal of Molecular Neuroscience. 36 (1–3): 125–131. doi:10.1007/s12031-008-9083-5. PMID 18566919. S2CID 29982279.
- Nussdorfer GG, Bahçelioglu M, Neri G, Malendowicz LK (February 2000). "Secretin, glucagon, gastric inhibitory polypeptide, parathyroid hormone, and related peptides in the regulation of the hypothalamus- pituitary-adrenal axis". Peptides. 21 (2): 309–324. doi:10.1016/S0196-9781(99)00193-X. PMID 10764961. S2CID 42207065.
- Lossi L, Bottarelli L, Candusso ME, Leiter AB, Rindi G, Merighi A (December 2004). "Transient expression of secretin in serotoninergic neurons of mouse brain during development". The European Journal of Neuroscience. 20 (12): 3259–3269. doi:10.1111/j.1460-9568.2004.03816.x. PMID 15610158. S2CID 398304.
- Lee SM, Yung WH, Chen L, Chow BK (February 2005). "Expression and spatial distribution of secretin and secretin receptor in human cerebellum". NeuroReport. 16 (3): 219–222. doi:10.1097/00001756-200502280-00003. PMID 15706223. S2CID 10500720.
- Lam IP, Lee LT, Choi HS, Alpini G, Chow BK (July 2009). "Bile acids inhibit duodenal secretin expression via orphan nuclear receptor small heterodimer partner (SHP)". American Journal of Physiology. Gastrointestinal and Liver Physiology. 297 (1): G90–G97. doi:10.1152/ajpgi.00094.2009. PMC 2711755. PMID 19372104.
- Yamagata T, Aradhya S, Mori M, Inoue K, Momoi MY, Nelson DL (August 2002). "The human secretin gene: fine structure in 11p15.5 and sequence variation in patients with autism". Genomics. 80 (2): 185–194. doi:10.1006/geno.2002.6814. PMID 12160732.
- Lee LT, Tan-Un KC, Chow BK (July 2006). "Retinoic acid-induced human secretin gene expression in neuronal cells is mediated by cyclin-dependent kinase 1". Annals of the New York Academy of Sciences. 1070 (1): 393–398. Bibcode:2006NYASA1070..393L. doi:10.1196/annals.1317.051. PMID 16888198. S2CID 36959997.
- Onori P, Wise C, Gaudio E, Franchitto A, Francis H, Carpino G, et al. (July 2010). "Secretin inhibits cholangiocarcinoma growth via dysregulation of the cAMP-dependent signaling mechanisms of secretin receptor". International Journal of Cancer. 127 (1): 43–54. doi:10.1002/ijc.25028. PMID 19904746. S2CID 2789418.
- Lee LT, Tan-Un KC, Pang RT, Lam DT, Chow BK (July 2004). "Regulation of the human secretin gene is controlled by the combined effects of CpG methylation, Sp1/Sp3 ratio, and the E-box element". Molecular Endocrinology. 18 (7): 1740–1755. doi:10.1210/me.2003-0461. PMID 15118068.
- Lu Y, Owyang C (July 2009). "Secretin-induced gastric relaxation is mediated by vasoactive intestinal polypeptide and prostaglandin pathways". Neurogastroenterology and Motility. 21 (7): 754–e47. doi:10.1111/j.1365-2982.2009.01271.x. PMC 2743409. PMID 19239625.
- Gandhi S, Rubinstein I, Tsueshita T, Onyuksel H (January 2002). "Secretin self-assembles and interacts spontaneously with phospholipids in vitro". Peptides. 23 (1): 201–204. doi:10.1016/S0196-9781(01)00596-4. PMID 11814635. S2CID 19705403.
- Lam IP, Lee LT, Choi HS, Chow BK (July 2006). "Localization of small heterodimer partner (SHP) and secretin in mouse duodenal cells". Annals of the New York Academy of Sciences. 1070 (1): 371–375. Bibcode:2006NYASA1070..371L. doi:10.1196/annals.1317.047. PMID 16888194. S2CID 37244976.
- Luttrell LM (July 2008). "Reviews in molecular biology and biotechnology: transmembrane signaling by G protein-coupled receptors". Molecular Biotechnology. 39 (3): 239–264. doi:10.1007/s12033-008-9031-1. PMID 18240029. S2CID 45173229.
- Du K, Couvineau A, Rouyer-Fessard C, Nicole P, Laburthe M (October 2002). "Human VPAC1 receptor selectivity filter. Identification of a critical domain for restricting secretin binding". The Journal of Biological Chemistry. 277 (40): 37016–37022. doi:10.1074/jbc.M203049200. PMID 12133828.
- Portela-Gomes GM, Johansson H, Olding L, Grimelius L (November 1999). "Co-localization of neuroendocrine hormones in the human fetal pancreas". European Journal of Endocrinology. 141 (5): 526–533. doi:10.1530/eje.0.1410526. PMID 10576771.
- Mutoh H, Ratineau C, Ray S, Leiter AB (April 2000). "Review article: transcriptional events controlling the terminal differentiation of intestinal endocrine cells". Alimentary Pharmacology & Therapeutics. 14 (Suppl 1): 170–175. doi:10.1046/j.1365-2036.2000.014s1170.x. PMID 10807420. S2CID 25989697.
External links
- Overview at colostate.edu
- Secretin at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Nosek TM. "Section 6/6ch2/s6ch2_17". Essentials of Human Physiology. Archived from the original on 2016-03-24.
- CS1 Danish-language sources (da)
- Wikipedia articles needing page number citations from January 2016
- Articles with short description
- Short description is different from Wikidata
- Genes on human chromosome 11
- All articles with dead external links
- Articles with dead external links from October 2022
- Articles with permanently dead external links
- Peptide hormones
- Intestinal hormones
- Digestive system
- Treatment of autism
- 1902 in biology