Morel-Lavallée lesion
| Morel-Lavallée lesion | |
|---|---|
| Other names: ML effusion, ML hematoma, posttraumatic pseudocyst, posttraumatic soft tissue cyst, closed degloving injury, chronic expanding hematoma[1] | |
 | |
| A Morel-Lavallée lesion involving the left pelvis as seen on CT scan. | |
| Specialty | Orthopedics |
| Symptoms | Bruising, increased skin mobility, swelling[2] |
| Complications | Infection, abnormal shaped area[2] |
| Usual onset | Immediately to days after injury[2] |
| Types | Type 1 to 6[2] |
| Causes | Injury[2] |
| Diagnostic method | Based on examination, supported by medical imaging[2] |
| Differential diagnosis | Abscess, contusion, hematoma, prepatellar bursitis[1] |
| Treatment | Closely watching, drainage using a needle, surgery[2] |
| Frequency | Rare[1] |
Morel-Lavallée lesion (MLL) is a type of degloving injury.[2] Generally it occurs around the thigh or pelvis; though other areas may be involved.[2] Symptoms may include bruising, increased skin mobility, and swelling.[2] This may not appear for a couple of days.[2] Complications may involved infection or an abnormal shape to the area.[2]
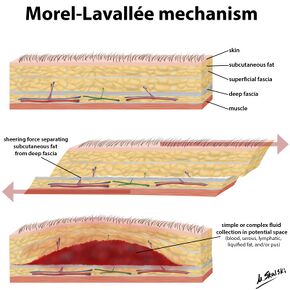
It most commonly occurs as a result of significant trauma, such as a motor vehicle collision.[2][1] Associated injuries may include breaks of the pelvis or femur.[2] The underlying mechanism involves separation of the subcutaneous tissue from the fascia underneath, without a break in the skin.[2] This creates a space in which fluid collects.[1] Diagnosis is based on examination and may be supported by medical imaging.[2]
Management typically involve closely watching, drainage using a needle, or surgery.[2] Other options may include compression therapy or sclerotherapy.[1] After treatment their is a risk of occurrence.[1] Morel-Lavallée lesions are relatively rare.[1] It was first described in 1863 by Victor-Auguste-François Morel-Lavallée.[2]
Signs and symptoms

Symptoms may include bruising, increased skin mobility, and swelling.[2] This may not appear for a couple of days.[2] Complications may involved infection or an abnormal shape to the area.[2] Generally it occurs around the thigh or pelvis; though other areas may be involved.[2]
Mechanism
Diagnosis
Diagnosis is based on examination and may be supported by medical imaging.[2] MRI or ultrasound are particularly useful.[3] On CT scan a MLL has lower Hounsfield units than a hematoma (17 versus 75).[1]


References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Greenhill, D; Haydel, C; Rehman, S (January 2016). "Management of the Morel-Lavallée Lesion". The Orthopedic clinics of North America. 47 (1): 115–25. doi:10.1016/j.ocl.2015.08.012. PMID 26614926.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 Scolaro, JA; Chao, T; Zamorano, DP (October 2016). "The Morel-Lavallée Lesion: Diagnosis and Management". The Journal of the American Academy of Orthopaedic Surgeons. 24 (10): 667–72. doi:10.5435/JAAOS-D-15-00181. PMID 27579812.
- ↑ Gaillard, Frank. "Morel-Lavallée lesion | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Archived from the original on 3 December 2022. Retrieved 5 May 2023.
- ↑ De Coninck, Tineke; Vanhoenacker, Filip; Verstraete, Koenraad (16 December 2017). "Imaging Features of Morel-Lavallée Lesions". Journal of the Belgian Society of Radiology. 101 (S2): 15. doi:10.5334/jbr-btr.1401.