Colorectal serrated lesions and polyps
| Colorectal serrated lesions and polyps | |
|---|---|
| Other names: Sessile serrated polyp (SSP) Sessile serrated adenoma (SSA) - not recommended[1] | |
 | |
| Colorectal polyp | |
| Specialty | Gastroenterology |
| Symptoms | Mostly no symptoms[1] |
| Complications | Colorectal cancer |
| Types | Microvesicular hyperplastic polyp, goblet-cell rich hyperplastic polyp, sessile serrated lesion, sessile serrated lesion with dysplasia, traditional serrated adenoma[1] |
| Diagnostic method | Colonoscopy |
| Treatment | Polypectomy |
Colorectal serrated lesions and polyps, formerly known as sessile serrated lesion,[1] is a premalignant flat (or sessile) lesion of the colon, predominantly seen in the cecum and ascending colon.
There are generally no symptoms.[1]
Types include microvesicular hyperplastic polyp, goblet-cell rich hyperplastic polyp, sessile serrated lesion, sessile serrated lesion with dysplasia, and traditional serrated adenoma.[1]
SSLs are thought to lead to colorectal cancer through the (alternate) serrated pathway.[2][3] This differs from most colorectal cancer, which arises from mutations starting with inactivation of the APC gene.
Multiple SSLs may be part of the serrated polyposis syndrome.[4]
Classification
Types include microvesicular hyperplastic polyp, goblet-cell rich hyperplastic polyp, sessile serrated lesion, sessile serrated lesion with dysplasia, and traditional serrated adenoma.[1]
Signs and symptoms
There are generally no symptoms.[1] They are typically identified on a colonoscopy and excised for a definitive diagnosis and treatment.[1]
Serrated polyposis syndrome
The serrated polyposis syndrome (SPS) is a relatively rare condition characterized by multiple and/or large serrated polyps of the colon. Diagnosis of this disease is made by the fulfillment of any of the World Health Organization’s (WHO) clinical criteria.[5]
Diagnosis
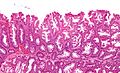
SSLs are diagnosed by their microscopic appearance; histomorphologically, they are characterized by (1) basal dilation of the crypts, (2) basal crypt serration, (3) crypts that run horizontal to the basement membrane (horizontal crypts), and (4) crypt branching. The most common of these features is basal dilation of the crypts.[citation needed]
Unlike conventional colonic adenomas (e.g. tubular adenoma, villous adenoma), they do not (typically) have nuclear changes (nuclear hyperchromatism, nuclear crowding, elliptical/cigar-shaped nuclei).[citation needed]
-
Low magnification micrograph of an SSL.
-
Intermediate magnification micrograph of an SSL.
-
High magnification micrograph of a SSL showing crypt branching.
Treatment
Complete removal of a SSL is considered curative.
Several SSLs confer a higher risk of subsequently finding colorectal cancer and warrant more frequent surveillance. The surveillance guidelines are the same as for other colonic adenomas. The surveillance interval is dependent on (1) the number of adenomas, (2) the size of the adenomas, and (3) the presence of high-grade microscopic features.[6]
Epidemiology
Sessile serrated lesions account for about 25% of all serrated polyps.[7] Advanced SSLs with cytological dysplasia are rare in younger patients,[8] and progression of SSLs appears to be linked with ageing.[9][10]
History
Sessile serrated adenomas were first described in 1996.[11] In 2019, the World Health Organization recommended the use of the term "sessile serrated lesion," rather than sessile serrated polyp or adenoma.[7]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 WHO Classification of Tumours Editorial Board (2019). "6. Tumours of the colon and rectum: colorectal serrated lesions and polyps". Digestive System Tumours (5th ed.). Lyon (France). p. 162. ISBN 978-92-832-4499-8. Archived from the original on 2022-06-13. Retrieved 2022-07-19.
- ↑ Rüschoff J, Aust D, Hartmann A (2007). "[Colorectal serrated adenoma: diagnostic criteria and clinical implications]". Verh Dtsch Ges Pathol (in Deutsch). 91: 119–25. PMID 18314605.
- ↑ Mäkinen MJ (January 2007). "Colorectal serrated adenocarcinoma". Histopathology. 50 (1): 131–50. doi:10.1111/j.1365-2559.2006.02548.x. PMID 17204027. S2CID 2377929.
- ↑ Rosty, C.; Parry, S.; Young, JP. (2011). "Serrated polyposis: an enigmatic model of colorectal cancer predisposition". Pathol Res Int. 2011: 157073. doi:10.4061/2011/157073. PMC 3109311. PMID 21660283.
- ↑ World J Gastroenterol 2012 May 28; 18(20): 2452–2461
- ↑ Levine JS, Ahnen DJ (December 2006). "Clinical practice. Adenomatous polyps of the colon". N. Engl. J. Med. 355 (24): 2551–7. doi:10.1056/NEJMcp063038. PMID 17167138.
- ↑ 7.0 7.1 Crockett, SD; Nagtegaal, ID (October 2019). "Terminology, Molecular Features, Epidemiology, and Management of Serrated Colorectal Neoplasia". Gastroenterology. 157 (4): 949–966.e4. doi:10.1053/j.gastro.2019.06.041. PMID 31323292.
- ↑ Bettington, Mark; Walker, Neal; Rosty, Christophe; Brown, Ian; Clouston, Andrew; McKeone, Diane; Pearson, Sally-Ann; Leggett, Barbara; Whitehall, Vicki (January 2017). "Clinicopathological and molecular features of sessile serrated adenomas with dysplasia or carcinoma". Gut. 66 (1): 97–106. doi:10.1136/gutjnl-2015-310456. PMID 26475632. S2CID 3495692.
- ↑ Fennell, Lochlan; Kane, Alexandra; Liu, Cheng; McKeone, Diane; Hartel, Gunter; Su, Chang; Bond, Catherine; Bettington, Mark; Leggett, Barbara; Whitehall, Vicki (6 July 2021). "Braf mutation induces rapid neoplastic transformation in the aged and aberrantly methylated intestinal epithelium". Gut: gutjnl–2020–322166. doi:10.1136/gutjnl-2020-322166. PMID 34230216.
- ↑ Bettington, M; Brown, I; Rosty, C; Walker, N; Liu, C; Croese, J; Rahman, T; Pearson, SA; McKeone, D; Leggett, B; Whitehall, V (March 2019). "Sessile Serrated Adenomas in Young Patients may have Limited Risk of Malignant Progression". Journal of Clinical Gastroenterology. 53 (3): e113–e116. doi:10.1097/MCG.0000000000001014. PMID 29570172. S2CID 4261352.
- ↑ Torlakovic, E; Snover, DC (July 2006). "Sessile serrated adenoma: a brief history and current status". Critical Reviews in Oncogenesis. 12 (1–2): 27–39. doi:10.1615/critrevoncog.v12.i1-2.30. PMID 17078205.
External links
- Pathology of Serrated Colon Adenomas Archived 2021-05-14 at the Wayback Machine - Medscape
- Pages with script errors
- CS1 Deutsch-language sources (de)
- Articles with hatnote templates targeting a nonexistent page
- All articles with unsourced statements
- Articles with unsourced statements from August 2020
- Articles with invalid date parameter in template
- Webarchive template wayback links
- Digestive system neoplasia
- Histopathology