Video:Malaria
| Malaria (Tutorial) | |
|---|---|
| On Commons | |
| Steps for video creation | |
| Step 1 | Preview my changes (10 sec) |
| Step 2 | Upload to Commons (10 min) |
Overview
Malaria is a mosquito-borne infectious disease, that affects humans and other animals.[1]

Symptoms
It causes symptoms that typically include, fever, tiredness, vomiting, and headaches.[2]

Severe malaria symptoms
In severe cases, Malaria can cause yellow skin, seizures, coma, or death.[2]

Symptom timing
Symptoms usually begin ten to fifteen days after being bitten by an infected mosquito.[1]
Risk of no treatment
If not properly treated, people may have recurrences of the disease, months later.[1]

Partial immunity
In those who have recently survived an infection, reinfection usually causes milder symptoms.[2]

Partial immunity limitations
This partial resistance disappears over months, to years, if the person has no continuing exposure to malaria.[2]

Cause
Malaria is caused by single-celled microorganisms of the Plasmodium group.[1]

Initial infection
The disease is most commonly spread by an infected female, Anopheles mosquito.[1] The mosquito bite introduces the parasites from the mosquito's saliva, into a person's blood.[1]

Spread to liver
The parasites travel in the blood, to the liver, where they mature and reproduce.[2]

Types of malaria
Five species of the parasite Plasmodium can infect and be spread by humans, [2] with most deaths caused by P. falciparum.[2][1]
Diagnosis
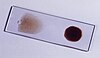
Malaria is typically diagnosed by the microscopic examination of blood, using blood films,
Rapid diagnosis
or with antigen-based rapid diagnostic tests, [2] although PCR tests are not widely used, in areas where malaria is common, due to their cost and complexity.[3]

Prevention
The risk of disease can be reduced, by preventing mosquito bites through the use of mosquito nets, and insect repellents,

Wider prevention
or with mosquito control measures, such as spraying insecticides, and draining standing water.[2]

Prophylaxis
Several medications are available to prevent malaria in travellers to areas where the disease is common.[1]

Prophylaxis in infants and pregnancy
Occasional doses of the combination medication sulfadoxine and pyrimethamine, are recommended in infants, and pregnancy after the first trimester, in areas with high rates of malaria.[1]

Vaccine
Despite a need, no effective vaccine exists, although efforts to develop one are ongoing.[1]

Treatment (primary)
The recommended treatment for malaria is a combination of antimalarial medications, that includes an artemisinin.[2][1]

Treatment (secondary)
The second medication may be either mefloquine, lumefantrine, or sulfadoxine pyrimethamine.[4]

Treatment (alternatives)
Quinine, along with doxycycline, may be used if an artemisinin is not available.[4]

Diagnosis before treatment
It is recommended that in areas where the disease is common, malaria is confirmed before treatment is started, due to concerns of increasing drug resistance.[1]

Epidemiology
The disease is widespread in the tropical and subtropical regions, in a broad band around the equator with 216 million cases in 2016.[2] [5][6]

Risk of death
resulting in an estimated 445,000 to 731,000 deaths. Approximately 90% of both cases, and deaths, occurred in Africa.[7]

Rates of disease
Rates of disease decreased by 37% between the years 2000 and 2015,[7] but increased from 2014, during which there were 198 million cases.[8]

Populations at risk
Malaria is commonly associated with poverty, and has a major negative effect on economic development.[9][10]

Effect on economies
For instance, in Africa, it is estimated to result in losses of US$12 billion a year, due to increased healthcare costs, lost ability to work, and negative effects on tourism.[11]

References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 "Malaria Fact sheet N°94". WHO. March 2014. Archived from the original on 3 September 2014. Retrieved 28 August 2014.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Caraballo H (2014). "Emergency department management of mosquito-borne illness: Malaria, dengue, and west nile virus". Emergency Medicine Practice. 16 (5). Archived from the original on 2016-08-01.
- ↑ Nadjm B, Behrens RH (2012). "Malaria: An update for physicians". Infectious Disease Clinics of North America. 26 (2): 243–59. doi:10.1016/j.idc.2012.03.010. PMID 22632637.
- ↑ 4.0 4.1 Organization, World Health (2010). Guidelines for the treatment of malaria (2nd ed.). Geneva: World Health Organization. p. ix. ISBN 978-92-4-154792-5.
- ↑ World Malaria Report 2017 (PDF). WHO. 2017. ISBN 978-92-4-156552-3.
- ↑ GBD 2015 Mortality and Causes of Death, Collaborators (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ 7.0 7.1 "Malaria Fact sheet N°94". WHO. Archived from the original on 3 September 2014. Retrieved 2 February 2016.
- ↑ WHO (2014). World Malaria Report 2014. Geneva: World Health Organization. pp. 32–42. ISBN 978-92-4-156483-0.
- ↑ Gollin D, Zimmermann C (August 2007). Malaria: Disease Impacts and Long-Run Income Differences (PDF) (Report). Institute for the Study of Labor. Archived (PDF) from the original on 2016-03-18.
- ↑ Worrall E, Basu S, Hanson K (2005). "Is malaria a disease of poverty? A review of the literature". Tropical Health and Medicine. 10 (10): 1047–59. doi:10.1111/j.1365-3156.2005.01476.x. PMID 16185240.

- ↑ Greenwood BM, Bojang K, Whitty CJ, Targett GA (2005). "Malaria". Lancet. 365 (9469): 1487–98. doi:10.1016/S0140-6736(05)66420-3. PMID 15850634.