Sural nerve
| sural nerve | |
|---|---|
 Dissection of popliteal space to show the formation of a type 1 sural nerve | |
 Cartoon version adapted from Steele et al. depicting type 1 sural nerve | |
| Details | |
| From | Union of Medial sural cutaneous nerve + sural communicating nerve |
| To | Sural nerve forms after piercing out of deep fascia or after an anastomosis, terminates as lateral dorsal cutaneous nerve |
| Innervates | Supplies cutaneous sensation to the skin of the posterolateral leg and lateral ankle. |
| Identifiers | |
| Latin | nervus suralis |
| MeSH | D013497 |
| TA98 | A14.2.07.062 |
| TA2 | 6586 |
| FMA | 44688 |
| Anatomical terms of neuroanatomy | |
The sural nerve (L4-S1) is generally considered a pure cutaneous nerve of the posterolateral leg to the lateral ankle. The sural nerve originates from a combination of either the sural communicating branch and medial sural cutaneous nerve, or the lateral sural cutaneous nerve. This group of nerves is termed the sural nerve complex. There are eight documented variations of the sural nerve complex. Once formed the sural nerve takes its course midline posterior to posterolateral around the lateral malleolus. The sural nerve terminates as the lateral dorsal cutaneous nerve.
Anatomy
The sural nerve (L4-S1) is a cutaneous sensory nerve of the posterolateral calf with cutaneous innervation to the distal one-third of the lower leg.[1] Formation of the sural nerve is the result of either anastomosis of the medial sural cutaneous nerve and the sural communicating nerve, or it may be found as a continuation of the lateral sural cutaneous nerve[2] traveling parallel to the medial sural cutaneous nerve. The sural nerve specifically innervates cutaneous sensorium over the posterolateral leg and lower lateral ankle via lateral calcaneal branches.
Innervation
The sural nerve provides cutaneous innervation to the skin of the posterior to posterolateral leg. This nerve is part of the sciatic nerve sensorium. It only provides autonomic and sensory nerve fibers to the skin of the posterolateral leg and ankle. These fibers originate from perikaryon located in the spinal ganglia and travel via the lumbosacral plexus via nerve roots L4-S1.[3] When testing for deficits understand that often multiple nerves (lateral calcaneal nerve, sural nerve, and lateral dorsal cutaneous nerves of the foot) provide a complicated marriage of converging sensorium around the lower extremity.
Anatomic Course
Grossly, the course of this nerve leads it from its highly varied anastomotic formation[4] to its more predictable terminal course down the remaining posterior leg. The anastomosis forming the sural nerve typically occurs in the deep fascia above or within the surrounding space above the gastrocnemius muscle. Once formed, the sural nerve then pierces out of a fascial crura and travels from its posterior midline position wrapping laterally around the lateral malleolus; once around the lateral malleolus the name of the nerve changes to the lateral dorsal cutaneous nerve. Eight variations of sural nerve origin have been described with categorical subtyping.[2]
Anatomic Formation
The nerves contributing to the formation of the sural nerve (medial sural cutaneous nerve, lateral sural cutaneous nerve, sural communicating nerve) are deemed the sural nerve complex by some anatomists and surgeons. Eight formations of the sural nerve complex have been described in cadaveric studies.[2][5][6][7]
Morphometrics
The pathway of the sural nerve (once formed) is consistent as it travels superficially in the posterior leg over the distal part of the gastrocnemius over the beginning of the achilles tendon and then travels parallel to the achilles with the small saphenous vein to send of lateral calcaneal branches while the remaining nerve passes under the lateral malleolus and finally finding its terminal name as the sural nerve becomes the lateral dorsal cutaneous nerve. The formation patterns of the sural nerve complex is much more complicated and highly varied as documented by anatomists.[2][8] The most common formation is the anastomotic scenario described above; the sural communicating branch joins the medial sural cutaneous nerve to become the sural nerve. Type 1 and 2 sural nerve complex formation prevalence is estimated up to greater than 70%, Although the remaining types (3-8) provide difficulty in making consistent clinical approximation of this nerve in the random population.
The sural nerve then travels out of deep fascia to the subcutaneous posterior sura. Although, these types of sural nerve complex (type 1 and 2) are of the highest prevalence [2]there are multiple scenarios which other contributing nerves that range in morphology of formation, sural nerve size, and location of the sural nerve union.[2] Anatomists limit the name of the sural nerve from its origins after an anastomosis of the SCB (type 1) and medial sural cutaneous nerve or we name it for when it penetrates out of the deep fascia of the posterior sura.[9]
Clinical significance
The sural nerve has a purely sensory function, and so its removal results in only a relatively minor consequential deficit. Due to its large size and significant length it has had a significant contribution in medicine twofold; the sural nerve is the most frequently accessed donor nerve site for peripheral nerve grafting and serves as the primary diagnostic site for nerve conduction studies for understanding of peripheral nerve pathologies.[10][11] It is frequently a site of iatrogenic nerve injury during percutaneous repair of the Achilles tendon or surgical interventions on the lower extremity.[12]
The sural nerve is also a source for iatrogenic injuries during orthopedic interventions of the lower ankle and extremity. For this reason, and due to its large size and significant length it has had a significant contribution in medicine in the form of nerve biopsy and diagnostics of peripheral nerve diseases. Sural mononeuropathy is uncommon, however If affected, it can be due to diabetes, peripheral neuropathies, or trauma. [13] Sometimes inflammatory or vasculitic diseases will selectively involve the sural nerve. In addition, the sural nerve will be involved in any kind of generalized peripheral sensory or sensorimotor neuropathy. Sensory changes from sural neuropathy are variable but usually occur in the posterolateral aspect of the leg and the dorsolateral foot. These can sometimes be painful with paresthesias and dysesthesias.[14] Nerve conduction studies can be used to delineate sural nerve lesions.[15] Treatment will depend on the cause of the neuropathy. Occasionally biopsy of the nerve is performed for diagnostic purposes. For example, ganglions are usually resected. Traumatic neuropathy is usually treated non-surgically.[13][16] It is often the donor nerve when a nerve allograft is performed.[17]
Sural nerve block
A sural nerve block can be used for quick anesthetization to the foot and lower leg. Because this technique requires few injections to reach adequate anesthesia, a smaller volume of anesthetic is needed.[18] The sural nerve is rather superficial, which makes it more accessible to surgeons. Therefore, it is relatively easier than other procedures. Also, due to its superficial properties, the sural nerve is easily blocked at multiple levels at or above the ankle. In one study, regional anesthesia of the foot and ankle, when performed by surgeons, was completely successful 95% of the time.[19] Sural nerve block is not advised if a patient is allergic to the anesthetic solution, has infected tissue at the injection site, has severe bleeding disorder, or has preexisting neurological damage.[20]
Additional images
-
Dissection of popliteal space to show the formation of a type 1 sural nerve
-
Cartoon version adapted from Steele et al. depicting type 1 sural nerve
-
8 documented types of sural nerve formation
-
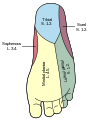
Areas of skin sensation supplied by nerves in the leg.
-
Areas of skin supplied by nerves of the leg - the sural nerve supplies the lateral ankle.
-
Deep nerves of the front of the leg.
-
Course of nerves at the bottom of the foot.
References
![]() This article incorporates text in the public domain from page 963 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 963 of the 20th edition of Gray's Anatomy (1918)
- ^ Moore, Keith (August 2017). Clinically Oriented Anatomy. Philadelphia, PA: Lippincot Williams and Wilkins. ISBN 978-1-4963-4721-3.[page needed]
- ^ a b c d e f Steele, Robert; Coker, Charles; Freed, Blair; Wright, Barth; Brauer, Philip (November 2021). "Anatomy of the sural nerve complex: Unaccounted anatomic variations and morphometric data". Annals of Anatomy. 238: 151742. doi:10.1016/j.aanat.2021.151742. PMID 33932499.
- ^ Glatte, Patrick; Buchmann, Sylvia J.; Hijazi, Mido Max; Illigens, Ben Min-Woo; Siepmann, Timo (10 September 2019). "Architecture of the Cutaneous Autonomic Nervous System". Frontiers in Neurology. 10: 970. doi:10.3389/fneur.2019.00970. PMC 6746903. PMID 31551921.
- ^ Tubbs, Shane (May 2016). Bergmans's Comprehensive Encyclopedia of Human Anatomic Variation. John Wiley & Sons. p. 1113. ISBN 978-1-118-43035-4.
- ^ Rea, Paul (2015). "Lower Limb Nerve Supply". Essential Clinically Applied Anatomy of the Peripheral Nervous System in the Limbs. pp. 101–177. doi:10.1016/b978-0-12-803062-2.00003-6. ISBN 978-0-12-803062-2.
- ^ Ortigiiela, Maria E.; Wood, Michael B.; Cahill, Donald R. (November 1987). "Anatomy of the sural nerve complex". The Journal of Hand Surgery. 12 (6): 1119–1123. doi:10.1016/s0363-5023(87)80129-6. PMID 3693848.
- ^ Ramakrishnan, Piravin (November 2015). "Anatomical variations of the formation and course of the sural nerve: A systematic review and meta-analysis". Annals of Anatomy. 202: 36–44. doi:10.1016/j.aanat.2015.08.002. PMID 26342158.
- ^ Ramakrishnan, Piravin (November 2015). "Anatomical variations of the formation and course of the sural nerve: A systematic review and meta-analysis". Annals of Anatomy. 202: 36–44. doi:10.1016/j.aanat.2015.08.002. PMID 26342158. Background and information section reviews the many anatomy papers that demonstrate extreme variability in the formation of the sural nerve
- ^ Seema, S. R. (16 December 2013). "Study of Sural Nerve Complex in Human Cadavers". ISRN Anatomy. 2013: 827276. doi:10.5402/2013/827276. PMC 4392956. PMID 25938105.
- ^ Ikiz, Z Asli Aktan; Uçerler, Hülya; Bilge, Okan (July 2005). "The Anatomic Features of the Sural Nerve With an Emphasis on its Clinical Importance". Foot & Ankle International. 26 (7): 560–567. doi:10.1177/107110070502600712. PMID 16045849. S2CID 11029085.
- ^ Pyun, Sung-Bom; Kang, Seok; Kwon, Hee-Kyu (2010). "Anatomical and Electrophysiological Myotomes Corresponding to the Flexor Carpi Ulnaris Muscle". Journal of Korean Medical Science. 25 (3): 454–457. doi:10.3346/jkms.2010.25.3.454. PMC 2826750. PMID 20191047.
- ^ McGee, Roddy; Watson, Troy; Eudy, Adam; Brady, Candice; Vanier, Cheryl; LeCavalier, Daniel; Hoang, Victor (June 2021). "Anatomic relationship of the sural nerve when performing Achilles tendon repair using the percutaneous Achilles repair system, a cadaveric study". Foot and Ankle Surgery. 27 (4): 427–431. doi:10.1016/j.fas.2020.05.011. PMID 32553425. S2CID 219902087.
- ^ a b Stickler, D. E.; Morley, K. N.; Massey, E. W. (October 2006). "Sural neuropathy: Etiologies and predisposing factors". Muscle & Nerve. 34 (4): 482–484. doi:10.1002/mus.20580. PMID 16691605. S2CID 25070694.
- ^ Yuebing, Li; Lederman, Richard J. (March 2014). "Sural mononeuropathy: A report of 36 cases: Short Reports". Muscle & Nerve. 49 (3): 443–445. doi:10.1002/mus.24107. PMID 24531991. S2CID 2184884.
- ^ Kimura J. Electrodiagnosis in Diseases of Nerve and Muscle: Principles and Practice. 1983 Philadelphia, FA Davis, p 502.
- ^ Mcleod, J G (1 October 2000). "Sural nerve biopsy". Journal of Neurology, Neurosurgery & Psychiatry. 69 (4): 431. doi:10.1136/jnnp.69.4.431. PMC 1737139. PMID 10990498.
- ^ Piedra Buena, Ignacio T.; Fichman, Matias (2022). "Sural Nerve Graft". StatPearls. StatPearls Publishing. PMID 32491647.
- ^ Crystal, Chad S.; Blankenship, Robert B. (2005). "Local Anesthetics and Peripheral Nerve Blocks in the Emergency Department". Emergency Medicine Clinics of North America. 23 (2): 477–502. doi:10.1016/j.emc.2004.12.012. PMID 15829393.
- ^ Myerson, Mark S.; Ruland, Charles M.; Allon, Steven M. (June 1992). "Regional Anesthesia for Foot and Ankle Surgery". Foot & Ankle. 13 (5): 282–288. doi:10.1177/107110079201300510. PMID 1624194. S2CID 43439010.
- ^ Sural Nerve Block at eMedicine
External links
Referenced papers:
- Steele et al. 208 sample cadaveric review 2021
- Ramakrishnan et al.systematic review on sural nerve formation 2015
Anatomy web references
- Anatomy photo:11:07-0202 at the SUNY Downstate Medical Center
- Sural nerve at the Duke University Health System's Orthopedics program
- Cutaneous field