Pancreatic islets
| Pancreatic islets | |
|---|---|
 | |
 A pancreatic islet from a mouse in a typical position, close to a blood vessel; insulin in red, nuclei in blue. | |
| Details | |
| Part of | Pancreas |
| System | Endocrine |
| Identifiers | |
| Latin | insulae pancreaticae |
| MeSH | D007515 |
| TA98 | A05.9.01.019 |
| TA2 | 3128 |
| FMA | 16016 |
| Anatomical terms of microanatomy | |
The pancreatic islets or islets of Langerhans are the regions of the pancreas that contain its endocrine (hormone-producing) cells, discovered in 1869 by German pathological anatomist Paul Langerhans.[1] The pancreatic islets constitute 1–2% of the pancreas volume and receive 10–15% of its blood flow.[2][3] The pancreatic islets are arranged in density routes throughout the human pancreas, and are important in the metabolism of glucose.[4]
Structure
There are about 1 million islets distributed throughout the pancreas of a healthy adult human. While islets vary in size, the average diameter is about 0.2 mm.[5]:928 Each islet is separated from the surrounding pancreatic tissue by a thin, fibrous, connective tissue capsule which is continuous with the fibrous connective tissue that is interwoven throughout the rest of the pancreas.[5]:928
Microanatomy
Hormones produced in the pancreatic islets are secreted directly into the blood flow by (at least) five types of cells. In rat islets, endocrine cell types are distributed as follows:[6]
- Alpha cells producing glucagon (20% of total islet cells)
- Beta cells producing insulin and amylin (≈70%)
- PP cells (gamma cells or F cells) producing pancreatic polypeptide (<5%)
- Delta cells producing somatostatin (<10%)
- Epsilon cells producing ghrelin (<1%)
It has been recognized that the cytoarchitecture of pancreatic islets differs between species.[7][8][9] In particular, while rodent islets are characterized by a predominant proportion of insulin-producing beta cells in the core of the cluster and by scarce alpha, delta and PP cells in the periphery, human islets display alpha and beta cells in close relationship with each other throughout the cluster.[7][9]
The proportion of beta cells in islets varies depending on the species, in humans it is about 40–50%. In addition to endocrine cells, there are stromal cells (fibroblasts), vascular cells (endothelial cells, pericytes), immune cells (granulocytes, lymphocytes, macrophages, dendritic cells,) and neural cells.[10]
A large amount of blood flows through the islets, 5–6 mL/min per 1 g of islet. It is up to 15 times more than in exocrine tissue of the pancreas.[10]
Islets can influence each other through paracrine and autocrine communication, and beta cells are coupled electrically to six to seven other beta cells, but not to other cell types.[11]
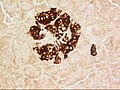
-
A pancreatic islet, stained.
-
A pancreatic islet, showing alpha cells
-
A pancreatic islet, showing beta cells.
Function
The paracrine feedback system of the pancreatic islets has the following structure:[12]
- Glucose/Insulin: activates beta cells and inhibits alpha cells.
- Glycogen/Glucagon: activates alpha cells which activates beta cells and delta cells.
- Somatostatin: inhibits alpha cells and beta cells. Also inhibits the secretion of pancreatic polypeptide.[13]
A large number of G protein-coupled receptors (GPCRs) regulate the secretion of insulin, glucagon, and somatostatin from pancreatic islets,[14] and some of these GPCRs are the targets of drugs used to treat type-2 diabetes (ref GLP-1 receptor agonists, DPPIV inhibitors).
-
Mouse islet immunostained for pancreatic polypeptide
-
Mouse islet immunostained for insulin
-
Mouse islet immunostained for glucagon
Electrical activity
Electrical activity of pancreatic islets has been studied using patch clamp techniques. It has turned out that the behavior of cells in intact islets differs significantly from the behavior of dispersed cells.[15]
Clinical significance
Diabetes
The beta cells of the pancreatic islets secrete insulin, and so play a significant role in diabetes. It is thought that they are destroyed by immune assaults.
Because the beta cells in the pancreatic islets are selectively destroyed by an autoimmune process in type 1 diabetes, clinicians and researchers are actively pursuing islet transplantation as a means of restoring physiological beta cell function, which would offer an alternative to a complete pancreas transplant or artificial pancreas.[16][17] Islet transplantation emerged as a viable option for the treatment of insulin requiring diabetes in the early 1970s with steady progress over the following three decades.[18] Clinical trials as of 2008[update] have shown that insulin independence and improved metabolic control can be reproducibly obtained after transplantation of cadaveric donor islets into patients with unstable type 1 diabetes.[17] Alternatively, daily insulin injections are an effective treatment for type 1 diabetes patients who are not candidates for islet transplantation.
People with high body mass index (BMI) are unsuitable pancreatic donors due to greater technical complications during transplantation. However, it is possible to isolate a larger number of islets because of their larger pancreas, and therefore they are more suitable donors of islets.[19]
Islet transplantation only involves the transfer of tissue consisting of beta cells that are necessary as a treatment of this disease. It thus represents an advantage over whole pancreas transplantation, which is more technically demanding and poses a risk of, for example, pancreatitis leading to organ loss.[19] Another advantage is that patients do not require general anesthesia.[20]
Islet transplantation for type 1 diabetes (as of 2008[update]) requires potent immunosuppression to prevent host rejection of donor islets.[21]
The islets are transplanted into a portal vein, which is then implanted in the liver.[19] There is a risk of portal venous branch thrombosis and the low value of islet survival a few minutes after transplantation, because the vascular density at this site is after the surgery several months lower than in endogenous islets. Thus, neovascularization is key to islet survival, that is supported, for example, by VEGF produced by islets and vascular endothelial cells.[10][20] However, intraportal transplantation has some other shortcomings, and so other alternative sites that would provide better microenvironment for islets implantation are being examined.[19] Islet transplant research also focuses on islet encapsulation, CNI-free (calcineurin-inhibitor) immunosuppression, biomarkers of islet damage or islet donor shortage.[22]
An alternative source of beta cells, such insulin-producing cells derived from adult stem cells or progenitor cells would contribute to overcoming the shortage of donor organs for transplantation. The field of regenerative medicine is rapidly evolving and offers great hope for the nearest future. However, type 1 diabetes is the result of the autoimmune destruction of beta cells in the pancreas. Therefore, an effective cure will require a sequential, integrated approach that combines adequate and safe immune interventions with beta cell regenerative approaches.[23] It has also been demonstrated that alpha cells can spontaneously switch fate and transdifferentiate into beta cells in both healthy and diabetic human and mouse pancreatic islets, a possible future source for beta cell regeneration.[24] In fact, it has been found that islet morphology and endocrine differentiation are directly related.[25] Endocrine progenitor cells differentiate by migrating in cohesion and forming bud-like islet precursors, or "peninsulas", in which alpha cells constitute the peninsular outer layer and beta cells form later beneath them. Cryopreservation has shown promise to improve the supply chain of pancreatic islets for better transplantation outcomes. [26]
Additional images
-
Illustration of dog pancreas. 250x.
Research
Cannabinoid receptors are found widely expressed in islets of Langerhans, and several studies have investigated specific distribution and mechanisms of CB1 versus CB2 receptors in relation to pancreatic endocrine functions, where they play an important homeostatic role, as endocannabinoids modulate pancreatic β-cells function, proliferation, and survival, as well as insulin production, secretion, and resistance.[27][28][29][30]
See also
- Betatrophin
- Neuroendocrine tumor
- Pancreatic neuroendocrine tumor
- Adrift Just Off the Islets of Langerhans, a novelette by Harlan Ellison
References
- ^ Langerhans P (1869). "Beitrage zur mikroscopischen anatomie der bauchspeichel druse". Inaugural-dissertation. Berlin: Gustav Lange.
- ^ Barrett KE, Boitano S, Barman SM, Brooks HL (2009-07-22). Ganong's review of medical physiology (23 ed.). McGraw Hill Medical. p. 316. ISBN 978-0-07-160568-7.
- ^ Functional Anatomy of the Endocrine Pancreas
- ^ Pour, Parviz M.; Standop, Jens; Batra, Surinder K. (January 2002). "Are islet cells the gatekeepers of the pancreas?". Pancreatology. 2 (5): 440–448. doi:10.1159/000064718. PMID 12378111. S2CID 37257345.
- ^ a b Sleisenger, edited by Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt; consulting editor, Marvin H. (2015). Sleisenger & Fordtran's gastrointestinal and liver disease pathophysiology, diagnosis, management (10th ed.). St. Louis, Missouri: Elsevier Health Sciences. ISBN 978-1-4557-4989-8.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ Elayat AA; el-Naggar MM; Tahir M; Bassam dahrouj (1995). "An immunocytochemical and morphometric study of the rat pancreatic islets". Journal of Anatomy. 186. (Pt 3) (Pt 3): 629–37. PMC 1167020. PMID 7559135.
- ^ a b Brissova M, Fowler MJ, Nicholson WE, Chu A, Hirshberg B, Harlan DM, Powers AC (2005). "Assessment of human pancreatic islet architecture and composition by laser scanning confocal microscopy". Journal of Histochemistry and Cytochemistry. 53 (9): 1087–97. doi:10.1369/jhc.5C6684.2005. PMID 15923354.
- ^ Ichii H, Inverardi L, Pileggi A, Molano RD, Cabrera O, Caicedo A, Messinger S, Kuroda Y, Berggren PO, Ricordi C (2005). "A novel method for the assessment of cellular composition and beta-cell viability in human islet preparations". American Journal of Transplantation. 5 (7): 1635–45. CiteSeerX 10.1.1.578.5893. doi:10.1111/j.1600-6143.2005.00913.x. PMID 15943621. S2CID 234176.
- ^ a b Cabrera O, Berman DM, Kenyon NS, Ricordi C, Berggren PO, Caicedo A (2006). "The unique cytoarchitecture of human pancreatic islets has implications for islet cell function". Proceedings of the National Academy of Sciences of the United States of America. 103 (7): 2334–9. Bibcode:2006PNAS..103.2334C. doi:10.1073/pnas.0510790103. ISSN 1091-6490. PMC 1413730. PMID 16461897.
- ^ a b c Jansson, Leif; Barbu, Andreea; Bodin, Birgitta; Drott, Carl Johan; Espes, Daniel; Gao, Xiang; Grapensparr, Liza; Källskog, Örjan; Lau, Joey; Liljebäck, Hanna; Palm, Fredrik (2016-04-02). "Pancreatic islet blood flow and its measurement". Upsala Journal of Medical Sciences. 121 (2): 81–95. doi:10.3109/03009734.2016.1164769. ISSN 0300-9734. PMC 4900068. PMID 27124642.
- ^ Kelly, Catriona; McClenaghan, Neville H.; Flatt, Peter R. (2011). "Role of islet structure and cellular interactions in the control of insulin secretion". Islets. 3 (2): 41–47. doi:10.4161/isl.3.2.14805. PMID 21372635.
- ^ Wang, Michael B.; Bullock, John; Boyle, Joseph R. (2001). Physiology. Hagerstown, MD: Lippincott Williams & Wilkins. p. 391. ISBN 978-0-683-30603-3.
- ^ Marques, Joana Moreira; Nunes, Rute; Florindo, Helena; Ferreira, Domingos; Sarmento, Bruno (2021). "A demanding path from iPSCs toward pancreatic β- and α-cells". Recent Advances in IPSC-Derived Cell Types. Advances in Stem Cell Biology. 4: 227–256. doi:10.1016/B978-0-12-822230-0.00002-8. ISBN 9780128222300. S2CID 234135648. Retrieved 18 January 2023.
- ^ Amisten, S; Salehi, A; Rorsman, P; Jones, PM; Persaud, SJ (2013). "An atlas and functional analysis of G-protein coupled receptors in human islets of Langerhans". Pharmacol Ther. 139 (3): 359–91. doi:10.1016/j.pharmthera.2013.05.004. PMID 23694765.
- ^ Pérez-Armendariz M, Roy C, Spray DC, Bennett MV (1991). "Biophysical properties of gap junctions between freshly dispersed pairs of mouse pancreatic beta cells". Biophysical Journal. 59 (1): 76–92. Bibcode:1991BpJ....59...76P. doi:10.1016/S0006-3495(91)82200-7. PMC 1281120. PMID 2015391.
- ^ Meloche RM (2007). "Transplantation for the treatment of type 1 diabetes". World Journal of Gastroenterology. 13 (47): 6347–55. doi:10.3748/wjg.13.6347. PMC 4205453. PMID 18081223.
- ^ a b Hogan A, Pileggi A, Ricordi C (2008). "Transplantation: current developments and future directions; the future of clinical islet transplantation as a cure for diabetes". Frontiers in Bioscience. 13 (13): 1192–205. doi:10.2741/2755. PMID 17981623.
- ^ Piemonti L, Pileggi A (2013). "25 Years of the Ricordi Automated Method for Islet Isolation". CellR4. 1 (1): 8–22. PMC 6267808. PMID 30505878.
- ^ a b c d Niclauss, Nadja; Meier, Raphael; Bédat, Benoît; Berishvili, Ekaterine; Berney, Thierry (2016-01-27), Stettler, C.; Christ, E.; Diem, P. (eds.), "Beta-Cell Replacement: Pancreas and Islet Cell Transplantation", Endocrine Development, 31, S. Karger AG: 146–162, doi:10.1159/000439412, ISBN 978-3-318-05638-9, PMID 26824893, retrieved 2020-09-11
- ^ a b Gamble, Anissa; Pepper, Andrew R.; Bruni, Antonio; Shapiro, A. M. James (2018-03-04). "The journey of islet cell transplantation and future development". Islets. 10 (2): 80–94. doi:10.1080/19382014.2018.1428511. ISSN 1938-2014. PMC 5895174. PMID 29394145.
- ^ Chatenoud L (2008). "Chemical immunosuppression in islet transplantation—friend or foe?". New England Journal of Medicine. 358 (11): 1192–3. doi:10.1056/NEJMcibr0708067. ISSN 0028-4793. PMID 18337609.
- ^ Chang, Charles A.; Lawrence, Michael C.; Naziruddin, Bashoo (October 2017). "Current issues in allogeneic islet transplantation". Current Opinion in Organ Transplantation. 22 (5): 437–443. doi:10.1097/MOT.0000000000000448. ISSN 1087-2418. PMID 28692442. S2CID 37483032.
- ^ Pileggi A, Cobianchi L, Inverardi L, Ricordi C (2006). "Overcoming the challenges now limiting islet transplantation: a sequential, integrated approach". Annals of the New York Academy of Sciences. 1079 (1): 383–98. Bibcode:2006NYASA1079..383P. doi:10.1196/annals.1375.059. ISSN 0077-8923. PMID 17130583. S2CID 33009393.
- ^ van der Meulen, T.; Mawla, A.M.; DiGruccio, M.R.; Adams, M.W.; Nies, V.; Dolleman, S.; Liu, S.; Ackermann, A.M.; Caceres, E.; Hunter, A.E.; Kaestner, K.H.; Donaldson, C.J.; Huising, M.O. (2017). "Virgin Beta Cells Persist throughout Life at a Neogenic Niche within Pancreatic Islets". Cell Metabolism. 25 (4): 911–926. doi:10.1016/j.cmet.2017.03.017. PMC 8586897. PMID 28380380.
- ^ Sharon, N.; Chawla, R.; Mueller, J.; Vanderhooft, J.; Whitehorn, L.J.; Rosenthal, B.; Gürtler, M.; Estanboulieh, R.R.; Shvartsman, D.; Gifford, D.K.; Trapnell, C.; Melton, D. (2019). "A Peninsular Structure Coordinates Asynchronous Differentiation with Morphogenesis to Generate Pancreatic Islets". Cell. 176 (4): 790–804.e13. doi:10.1016/j.cell.2018.12.003. ISSN 0092-8674. PMC 6705176. PMID 30661759.
- ^ Zhan, L., Rao, J.S., Sethia, N. et al. Pancreatic islet cryopreservation by vitrification achieves high viability, function, recovery and clinical scalability for transplantation. Nat Med (2022). https://doi.org/10.1038/s41591-022-01718-1
- ^ Bermúdez-Silva, F. J.; Suárez, J.; Baixeras, E.; Cobo, N.; Bautista, D.; Cuesta-Muñoz, A. L.; Fuentes, E.; Juan-Pico, P.; Castro, M. J.; Milman, G.; Mechoulam, R.; Nadal, A.; Rodríguez de Fonseca, F. (2008-03-01). "Presence of functional cannabinoid receptors in human endocrine pancreas". Diabetologia. 51 (3): 476–487. doi:10.1007/s00125-007-0890-y. ISSN 1432-0428. PMID 18092149.
- ^ Flores, Luis E.; Alzugaray, María E.; Cubilla, Marisa A.; Raschia, María A.; Del Zotto, Héctor H.; Román, Carolina L.; Suburo, Ángela M.; Gagliardino, Juan J. (October 2013). "Islet Cannabinoid Receptors: Cellular Distribution and Biological Function". Pancreas. 42 (7): 1085–1092. doi:10.1097/MPA.0b013e31828fd32d. ISSN 0885-3177. PMID 24005231. S2CID 36905885.
- ^ Juan-Picó, Pablo; Fuentes, Esther; Javier Bermúdez-Silva, F.; Javier Díaz-Molina, F.; Ripoll, Cristina; Rodríguez de Fonseca, Fernando; Nadal, Angel (2006-02-01). "Cannabinoid receptors regulate Ca2+ signals and insulin secretion in pancreatic β-cell". Cell Calcium. 39 (2): 155–162. doi:10.1016/j.ceca.2005.10.005. ISSN 0143-4160. PMID 16321437.
- ^ Farokhnia, Mehdi (2020-02-19). "Effects of oral, smoked, and vaporized cannabis on endocrine pathways related to appetite and metabolism: a randomized, double-blind, placebo-controlled, human laboratory study". Transl Psychiatry. 10 (71): 71. doi:10.1038/s41398-020-0756-3. PMC 7031261. PMID 32075958.
External links
- Pancreas at the Human Protein Atlas
- CS1 errors: generic name
- CS1 maint: multiple names: authors list
- CS1: long volume value
- Articles with short description
- Short description matches Wikidata
- Articles containing potentially dated statements from 2008
- All articles containing potentially dated statements
- Articles with BNF identifiers
- Articles with BNFdata identifiers
- Articles with GND identifiers
- Articles with J9U identifiers
- Articles with LCCN identifiers
- Articles with NKC identifiers
- Articles with TA98 identifiers
- Pancreas anatomy