Automated tissue image analysis

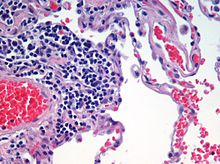
Automated tissue image analysis or histopathology image analysis (HIMA) is a process by which computer-controlled automatic test equipment is used to evaluate tissue samples, using computations to derive quantitative measurements from an image to avoid subjective errors.
In a typical application, automated tissue image analysis could be used to measure the aggregate activity of cancer cells in a biopsy of a cancerous tumor taken from a patient. In breast cancer patients, for example, automated tissue image analysis may be used to test for high levels of proteins known to be present in more aggressive forms of breast cancers.
Applications
Automated tissue imaging analysis can significantly reduce uncertainty in characterizing tumors compared to evaluations done by histologists,[1] or improve the prediction rate of recurrence of some cancers.[2][3] As it is a digital system, suitable for networking, it also facilitates cooperative efforts between distant sites.[4] Systems for automatically analyzing tissue samples also reduce costs and save time.[1]
High-performance CCD cameras are used for acquiring the digital images. Coupled with advanced widefield microscopes and various algorithms for image restoration, this approach can provide better results than confocal techniques at comparable speeds and lower costs.[5]
Processes
The United States Food and Drug Administration classifies these systems as medical devices, under the general instrumentation category of automatic test equipment.[6]
ATIS have seven basic processes (sample preparation, image acquisition, image analysis, results reporting, data storage, network communication, and self-system diagnostics) and realization of these functions highly accurate hardware and well-integrated, complex, and expensive software.[7]
Preparation
Specimen preparation is critical for evaluating the tumor in the automated system. In the first part of the preparation process the biopsied tissue is cut to an appropriate size (typically 4 mm), fixed in buffered formalin, dehydrated in ethanol-xylene, embedded in paraffin, thin sectioned typically to 4 um slices, then mounted onto at least two barcoded slides (a control and a test). Next the paraffin is removed from the tissue, the tissue is rehydrated, then stained. Any inconsistency in these procedures from case to case may result in uncertainties in the outcome of the analysis. These potential and irreducible inconsistencies in analysis results motivated the development of Automated Tissue Image Systems.
Acquisition
Digital micrographs are acquired of the stained specimen on the glass slide. The images are taken by a set of charge-coupled devices (CCD).[8]
Analysis
Image analysis involves complex computer algorithms which identify and characterize cellular color, shape, and quantity of the tissue sample using image pattern recognition technology based on vector quantization. Vector representations of objects in the image, as opposed to bitmap representations, have superior zoom-in ability. Once the sample image has been acquired and resident in the computer's random access memory as a large array of 0's and 1's, a programmer knowledgeable in cellular architecture can develop deterministic algorithms applied to the entire memory space to detect cell patterns from previously defined cellular structures and formations known to be significant.[9]
The aggregate algorithm outcome is a set of measurements that is far superior to any human sensitivity to intensity or luminance and color hue, while at the same time improving test consistency from eyeball to eyeball.[citation needed]
Reporting
The systems have the capability of presenting the resulting data in text and graphically, including on high definition monitors, to the system user. Computer printers, as relatively low image resolution devices, are used mostly to present final pathology reports that could include text and graphics.[citation needed]
Storage
Storage of the acquired data (graphical digital slide files and text data) involves saving system information in a data storage device system having at least convenient retrieval, and file management capabilities.[citation needed]
Medical imaging industry standards includes the Picture Archiving and Communication Systems (PACS), of European origin, which are image and information management solutions in computer networks that allow hospitals and clinics to acquire, distribute and archive medical images and diagnostic reports across the enterprise. Another standard of European origin is the Data and Picture Archiving and Communication System (DPACS). Although medical images can be stored in various formats, a common format has been Digital Imaging and Communications in Medicine (DICOM).[citation needed]
See also
References
- ^ a b O'Gorman, Lawrence; Sanderson, Arthur C.; Preston, Kendall (September 1985). "A System for Automated Liver Tissue Image Analysis: Methods and Results". IEEE Transactions on Biomedical Engineering. BME-32 (9): 696–706. doi:10.1109/TBME.1985.325587. ISSN 0018-9294. PMID 4054933. S2CID 30050996.
- ^ Teverovskiy, M.; Kumar, V.; Junshui Ma; Kotsianti, A.; Verbel, D.; Tabesh, A.; Ho-Yuen Pang; Vengrenyuk, Y.; Fogarasi, S.; Saidi, O. (2004). "Improved prediction of prostate cancer recurrence based on an automated tissue image analysis system". 2004 2nd IEEE International Symposium on Biomedical Imaging: Macro to Nano (IEEE Cat No. 04EX821). Vol. 2. pp. 257–260. CiteSeerX 10.1.1.58.9929. doi:10.1109/ISBI.2004.1398523. ISBN 0-7803-8388-5. S2CID 8724168.
- ^ Ali Tabesh; Mikhail Teverovskiy; Ho-Yuen Pang; Vinay P. Kumar; David Verbel; Angeliki Kotsianti; Olivier Saidi (October 2007). "Multifeature Prostate Cancer Diagnosis and Gleason Grading of Histological Images" (PDF). IEEE Transactions on Medical Imaging. 26 (10): 1366–1378. doi:10.1109/TMI.2007.898536. ISSN 0278-0062. PMID 17948727. S2CID 14673541. Archived from the original (PDF) on 2011-07-27. Retrieved 2010-09-04.
- ^ Bruce Mccullough; Xiaoyou Ying; Thomas Monticello; Marc Bonnefoi (2004). "Digital Microscopy Imaging and New Approaches in Toxicologic Pathology". Toxicologic Pathology. 32 (2): 49–58. doi:10.1080/01926230490451734. PMID 15503664.
- ^ Pornchai Phukpattaranont; Pleumjit Boonyaphiphat (2007). An Automatic Cell Counting Method for a Microscopic Tissue Image from Breast Cancer. IFMBE Proceedings. Vol. 15. pp. 241–244. doi:10.1007/978-3-540-68017-8_63. ISBN 978-3-540-68016-1.
- ^ Stokes, David (2003-11-25). Testing Computer Systems for FDA/MHRA Compliance - David Stokes - Google Books. ISBN 9780849321634. Retrieved 2012-07-12.
- ^ Chen, W.; Foran, D. J. (2006). "Analytica Chimica Acta - Advances in cancer tissue microarray technology: Towards improved understanding and diagnostics". Analytica Chimica Acta. 564 (1): 74–81. doi:10.1016/j.aca.2005.11.083. PMC 2583100. PMID 17723364.
- ^ MacDonald, J. H.; Wells, K.; Reader, A. J.; Ott, R. J. (February 1997). "A CCD-based tissue imaging system". Nuclear Instruments and Methods in Physics Research Section A: Accelerators, Spectrometers, Detectors and Associated Equipment. 392 (1–3). Nuclear Instruments and Methods in Physics Research: 220–226. Bibcode:1997NIMPA.392..220M. doi:10.1016/S0168-9002(97)00297-0.
- ^ Han, J.W.; Breckon, T.P.; Randell, D.A.; Landini, G. (2012). "The Application of Support Vector Machine Classification to Detect Cell Nuclei for Automated Microscopy". Machine Vision and Applications. 23 (1). Springer: 15–24. doi:10.1007/s00138-010-0275-y. S2CID 12446454.
External links
 Media related to Automated tissue image analysis at Wikimedia Commons
Media related to Automated tissue image analysis at Wikimedia Commons