Patiromer
 | |
| Names | |
|---|---|
| Trade names | Veltassa |
| Other names | RLY5016 |
| Clinical data | |
| Drug class | Potassium binder[1] |
| Main uses | High potassium[1] |
| Side effects | Constipation, low magnesium, nausea, abdominal pain[1] |
| Pregnancy category |
|
| Routes of use | By mouth (suspension) |
| Onset of action | 7 hrs; 1-2 wks for max effect[1] |
| Duration of action | 24 hrs |
| Typical dose | 8.4 to 25.2 grams per day[2] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a616012 |
| Legal | |
| License data | |
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | Not absorbed |
| Metabolism | None |
| Excretion | Feces |
| Chemical and physical data | |
| Formula | [(C3H3FO2)182·(C10H10)8·(C8H14)10]n [Ca91(C3H2FO2)182·(C10H10)8·(C8H14)10]n (calcium salt) |
Patiromer, sold under the brand name Veltassa, is a medication used to treat high blood potassium.[1] It is taken by mouth.[1] Its onset of action begins in about 7 hours, with maximum efforts taking a week or two.[1]
Common side effects include constipation, low blood magnesium, nausea, and abdominal pain.[1] Other side effects may include high calcium and intestinal perforation.[4] It works by binding potassium in the gut, increasing its loss in the stool.[2]
Patiromer was approved for medical use in the United States in 2015 and Europe in 2017.[1][3] In the United Kingdom it costs the NHS about £170 per month as of 2021.[4] This amount in the United States costs about 1,000 USD.[5]
Medical uses
Patiromer is used for the treatment of hyperkalemia, but not as an emergency treatment for life-threatening hyperkalemia, as it acts relatively slowly.[2] Such a condition needs other kinds of treatment, for example calcium infusions, insulin plus glucose infusions, salbutamol inhalation, and hemodialysis.[6]
Typical reasons for hyperkalemia are chronic kidney disease and application of drugs that inhibit the renin–angiotensin–aldosterone system (RAAS) – e.g. ACE inhibitors, angiotensin II receptor antagonists, or potassium-sparing diuretics – or that interfere with kidney function in general, such as nonsteroidal anti-inflammatory drugs (NSAIDs).[7][8]
Dosage
It is started at 8.4 grams per day and maybe increased up to 25.2 grams per day.[2]
Side effects
Patiromer was generally well tolerated in studies. Side effects that occurred in more than 2% of patients included in clinical trials were mainly gastro-intestinal problems such as constipation, diarrhea, nausea, and flatulence, and also hypomagnesemia (low levels of magnesium in the blood) in 5% of patients, because patiromer binds magnesium in the gut as well.[2][9]
Interactions
Patiromer was tested for drug-drug interactions with 28 drugs and showed binding or interaction with 14 of these drugs. This could reduce their availability and thus effectiveness,[2] wherefore patiromer has received a boxed warning by the US Food and Drug Administration (FDA), telling patients to wait for at least six hours between taking patiromer and any other oral drugs.[10]
Of the 14 drugs that did show an interaction in vitro, 12 were selected for further testing in phase 1 studies in healthy volunteers to assess whether the results seen in vitro translated into an effect in people. These studies showed patiromer did not alter the absorption of nine of the 12 drugs when co-administered. Patiromer reduced absorption of three drugs when co-administered, however, there was no interaction when patiromer and these three drugs were taken 3 hours apart.[11]
This information was submitted to the FDA in the form of a supplemental New Drug Application (sNDA) and as a result, in November 2016 the FDA approved the removal of the boxed warning regarding the separation of patiromer and other oral medications. The updated label recommends patients take patiromer at least three hours before or three hours after other oral medications.[2]
Pharmacology
Mechanism of action
Patiromer works by binding free potassium ions in the gastrointestinal tract and releasing calcium ions for exchange, thus lowering the amount of potassium available for absorption into the bloodstream and increasing the amount that is excreted via the feces. The net effect is a reduction of potassium levels in the blood serum.[2][7]
Lowering of potassium levels is detectable 7 hours after administration. Levels continue to decrease for at least 48 hours if treatment is continued, and remain stable for 24 hours after administration of the last dose. After this, potassium levels start to rise again over a period of at least four days.[2]
Pharmacokinetics
Patiromer is not absorbed from the gut, is not metabolized, and is excreted in unchanged form with the feces.[2]
Chemistry
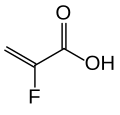
The substance is a cross-linked polymer of 2-fluoroacrylic acid with divinylbenzenes and 1,7-octadiene. It is used in form of its calcium salt (ratio 2:1) and with sorbitol (one molecule per two calcium ions or four fluoroacrylic acid units), a combination called patiromer sorbitex calcium.[12]
-
2-fluoroacrylic acid
-
o-divinylbenzene
-
p-divinylbenzene
-
1,7-octadiene
Patiromer sorbitex calcium is an off-white to light brown, amorphous, free-flowing powder. It is insoluble in water, 0.1 M hydrochloric acid, heptane, and methanol.[2][12]
Society and culture
Legal status
The US FDA approved patiromer in October 2015.[10] It was approved for use in the European Union in July 2017.[3]
Research
In a Phase III multicenter clinical trial including 237 patients with hyperkalemia under RAAS inhibitor treatment, 76% of participants reached normal serum potassium levels within four weeks. After subsequent randomization of 107 responders into a group receiving continued patiromer treatment and a placebo group, re-occurrence of hyperkalemia was 15% versus 60%, respectively.[13]
See also
- Sodium zirconium cyclosilicate, another potassium binder
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 "Patiromer Sorbitex Calcium Monograph for Professionals". Drugs.com. February 2017. Archived from the original on 13 November 2019. Retrieved 13 November 2019.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 "Veltassa- patiromer powder, for suspension". DailyMed. 23 October 2019. Archived from the original on 20 October 2020. Retrieved 18 October 2020.
- ↑ 3.0 3.1 3.2 "Veltassa". Archived from the original on 21 October 2020. Retrieved 26 October 2021.
- ↑ 4.0 4.1 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 1105. ISBN 978-0857114105.
- ↑ "Veltassa Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 24 August 2019. Retrieved 26 October 2021.
- ↑ Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, et al. (November 2010). "Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S829-61. doi:10.1161/CIRCULATIONAHA.110.971069. PMID 20956228.
- ↑ 7.0 7.1 Esteras R, Perez-Gomez MV, Rodriguez-Osorio L, Ortiz A, Fernandez-Fernandez B (August 2015). "Combination use of medicines from two classes of renin-angiotensin system blocking agents: risk of hyperkalemia, hypotension, and impaired renal function". Therapeutic Advances in Drug Safety. 6 (4): 166–76. doi:10.1177/2042098615589905. PMC 4530349. PMID 26301070.
- ↑ Rastegar A, Soleimani M, Rastergar A (December 2001). "Hypokalaemia and hyperkalaemia". Postgraduate Medical Journal. 77 (914): 759–64. doi:10.1136/pmj.77.914.759. PMC 1742191. PMID 11723313.
- ↑ Tamargo J, Caballero R, Delpón E (November 2014). "New drugs for the treatment of hyperkalemia in patients treated with renin-angiotensin-aldosterone system inhibitors -- hype or hope?". Discovery Medicine. 18 (100): 249–54. PMID 25425465.
- ↑ 10.0 10.1 "FDA approves new drug to treat hyperkalemia". FDA. 21 October 2015. Archived from the original on 7 November 2015. Retrieved 19 October 2020.
- ↑ Pharmabiz: US FDA approves removal of boxed warning on Relypsa's hyperkalemia drug, Veltassa Archived 2016-12-21 at the Wayback Machine.
- ↑ 12.0 12.1 RxList: Veltassa Archived 2020-10-26 at the Wayback Machine.
- ↑ Weir MR, Bakris GL, Bushinsky DA, Mayo MR, Garza D, Stasiv Y, et al. (January 2015). "Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors". The New England Journal of Medicine. 372 (3): 211–21. doi:10.1056/NEJMoa1410853. PMID 25415805. S2CID 205097243.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Pages using duplicate arguments in template calls
- Webarchive template wayback links
- Drugs with non-standard legal status
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Chemicals using indexlabels
- Drugs missing an ATC code
- Articles containing unverified chemical infoboxes
- Chemicals that do not have a ChemSpider ID assigned
- Nephrology procedures
- Potassium
- Organic polymers
- RTT