YWHAH
14-3-3 protein eta also referred to as 14-3-3η is a protein that in humans is encoded by the YWHAH gene.
Function
This gene product belongs to the 14-3-3 family of proteins that are normally intracellular in nature and help to mediate signal transduction by binding to phosphoserine-containing proteins. This highly conserved protein family is found in both plants and mammals, and this protein is 99% identical to the mouse, rat and bovine orthologs. This gene contains a 7 bp repeat sequence in its 5' UTR, and changes in the number of this repeat has been associated with early-onset schizophrenia.[5]
Protein-protein interactions
YWHAH has been shown to interact with:
Externalization
14-3-3n is normally intracellular. Two main mechanisms resulting in the release of 14-3-3η into the extracellular environment have been reported:
14-3-3 proteins are components of small extracellular vesicles that are secreted by most, if not all cells. Tumor necrosis factor alpha stimulation of macrophages, but not IL-6, promotes the secretion of 14-3-3η into the extracellular space through a TNF alpha-dependent necroptotic mechanism.
Role in rheumatoid arthritis
A 2021 systematic literature review published by authors from the NHS Foundation Trust in the United Kingdom conclude the following about the 14-3-3n biomarker:
- adequate evidence for helping to assess the veracity of the diagnosis and severity of early rheumatoid arthritis (RA);
- can be combined with existing markers for severity and to provide possible ways of stratifying patients into more effective treatment groups; and
- a welcome new addition for rheumatologist’s diagnostic, treatment and strategy in RA. [19]
Role of extracellular 14-3-3η
Exogenous 14-3-3η stimulation has been reported to stimulate various cell types including macrophages, monocytes, and fibroblast-like synoviocytes activating key cell signalling cascades including:
Stimulation of cells by extracellular 14-3-3η has been reported to increase key factors relevant to the pathophysiology of rheumatoid arthritis, including:
- Tumor necrosis factor alpha
- Interleukin 6
- CCL2/MCP-1
- Matrix metalloproteinase (MMPs)
- RANKL
Exogenous stimulation of human fibroblast-like synoviocytes, in a dose dependent manner, resulted in the development of invadosomes.[20] Silencing of 14-3-3n via shRNA resulted in decreased invadosome formation. Invadosomes are finger-like projections that bud from the cell membrane and are directly associated with increasing the migratory or invasive potential of cells. In RA, this might account for how the disease travels to neighboring joints.
Taken together, extracellular 14-3-3η upregulates pro-inflammatory factors directly that are targeted with small molecules and/or biological Disease-modifying antirheumatic drug (DMARDs), including TNF, IL-6 and Janus kinases. The table below defines the medicines by target.
| Target | Inhibitor |
|---|---|
| Tumor Necrosis Factor | Adalimumab |
| Interleukin 6 | Tocilizumab |
| Janus Kinase | Tofacitnib |
Key Clinical Findings
The body of independent evidence supporting the clinical utility of 14-3-3η continues to expand. As of 2022, there have been over 50 peer-reviewed citations and 200 conference proceedings describing the clinical value of the 14-3-3η biomarker. [21]
Diagnostic Value of 14-3-3η Marker. As shown in the table above, a number of studies have evaluated the specificity, sensitivity and value of 14-3-3η in combination with rheumatoid factor (RF) and/or the anti-cyclic citrullinated protein (ACPA, anti-CCP). According to Abdelhafiz et al. meta-analysis of all studies reported a pooled sensitivity of 73% (95% CI: 71 - 75) and a pooled specificity of 88% (95% CI: 87 - 90). In an Early Undifferentiated Polyarthritis (EUPA) cohort from the University of Sherbrooke where 14-3-3n were assessed in 331 subjects, the diagnostic accuracy of RF, CCP and RF and/or CCP was increased by: 24.0%, 36.8% and 15.0% respectively. [22]
Prognostic Value of the 14-3-3η Marker. An analysis of 331 patients from the EUPA cohort with five (5) years of longitudinal follow-up demonstrated that baseline 14-3-3η positivity, at the diagnostic cut-off of > 0.19 ng/ml, was associated with more radiographic progression over the five (5) years. Sustained and/or elevated 14-3-3η positivity over the course of the five (5) years of follow-up was associated with a higher likelihood of radiographic progression. Serial decreases in 14-3-3η of 0.76 ng/ml or reversion to a negative test during follow-up was associated with less subsequent radiographic progression. [23]
Serial Changes in 14-3-3η Marker with Effective Disease Management. 14-3-3η has been described as a modifiable marker, with post-treatment levels having been reported to decrease, stay the same, or in some cases increase despite patients being treated with different classes of therapy including small molecule and biological DMARDs like Methotrexate, Adalimumab, Tocilizumab, Tofacitinib and Upadacitinib. [24] [25] Post-treatment decreases and/or reversion to a negative 14-3-3η test is typically associated with better patient outcomes, whereas sustained positivity and/or increases in the 14-3-3η marker longitudinally is often associated with worse outcomes.
Further research is required to determine if certain therapies have a greater impact on the modifiability of 14-3-3η. Current data points towards more of a proximal or interactive effect between 14-3-3η and TNF alpha.
Targeting Drug Free Remission. With the advent of more effective RA treatments and more aggressive patient management strategies, drug free remission is now a possibility however, an important consideration when weaning a patient off of a DMARD is the concomitant risk of flaring. In a cohort of 331 patients from the EUPA cohort, Carrier et al. demonstrated that 14-3-3η positivity at the time of remission was associated with increased likelihood of radiographic progression. [26] Whilst further research is required to investigate how 14-3-3η informs risk of flaring and radiographic progression in patients that have achieved remission, the current data indicates that patients in clinical remission with a positive 14-3-3η test should be considered as higher risk for disease progression.
Detection of 14-3-3η Pre-Disease or in Other Arthritides. As earlier detection of RA is often associated with better clinical outcomes, evaluating how 14-3-3η informs risk of disease onset in asymptomatic patients is and will continue to be of paramount importance to investigate. In a study by Hitchon et al, the authors demonstrated that 14-3-3η levels were detectable in 1st degree relatives of patients diagnosed with RA, and that levels of 14-3-3η increased in 1st degree relatives at the time of transition to RA. The authors suggested that 14-3-3η was an imminent marker of RA transition. Additional studies in a larger subset of patients is required to fully evaluate when, why and how 14-3-3η levels increase in at-risk patients.[27]
14-3-3η has also been demonstrated to be detectable in lupus patients diagnosed with secondary Sjogren’s, albeit at lower levels than RA patients.
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000128245 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000018965 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Entrez Gene: YWHAH tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein, eta polypeptide".
- ^ a b Vincenz C, Dixit VM (August 1996). "14-3-3 proteins associate with A20 in an isoform-specific manner and function both as chaperone and adapter molecules". The Journal of Biological Chemistry. 271 (33): 20029–20034. doi:10.1074/jbc.271.33.20029. PMID 8702721.
- ^ a b c Ichimura T, Wakamiya-Tsuruta A, Itagaki C, Taoka M, Hayano T, Natsume T, Isobe T (April 2002). "Phosphorylation-dependent interaction of kinesin light chain 2 and the 14-3-3 protein". Biochemistry. 41 (17): 5566–5572. doi:10.1021/bi015946f. PMID 11969417.
- ^ Van Der Hoeven PC, Van Der Wal JC, Ruurs P, Van Dijk MC, Van Blitterswijk J (January 2000). "14-3-3 isotypes facilitate coupling of protein kinase C-zeta to Raf-1: negative regulation by 14-3-3 phosphorylation". The Biochemical Journal. 345 (2): 297–306. doi:10.1042/bj3450297. PMC 1220759. PMID 10620507.
- ^ Mils V, Baldin V, Goubin F, Pinta I, Papin C, Waye M, et al. (March 2000). "Specific interaction between 14-3-3 isoforms and the human CDC25B phosphatase". Oncogene. 19 (10): 1257–1265. doi:10.1038/sj.onc.1203419. PMID 10713667.
- ^ Yu T, Robb VA, Singh V, Gutmann DH, Newsham IF (August 2002). "The 4.1/ezrin/radixin/moesin domain of the DAL-1/Protein 4.1B tumour suppressor interacts with 14-3-3 proteins". The Biochemical Journal. 365 (Pt 3): 783–789. doi:10.1042/BJ20020060. PMC 1222735. PMID 11996670.
- ^ Wakui H, Wright AP, Gustafsson J, Zilliacus J (March 1997). "Interaction of the ligand-activated glucocorticoid receptor with the 14-3-3 eta protein". The Journal of Biological Chemistry. 272 (13): 8153–8156. doi:10.1074/jbc.272.13.8153. PMID 9079630.
- ^ Sato S, Fujita N, Tsuruo T (October 2002). "Regulation of kinase activity of 3-phosphoinositide-dependent protein kinase-1 by binding to 14-3-3". The Journal of Biological Chemistry. 277 (42): 39360–39367. doi:10.1074/jbc.M205141200. PMID 12177059.
- ^ a b Sun L, Bittner MA, Holz RW (October 2003). "Rim, a component of the presynaptic active zone and modulator of exocytosis, binds 14-3-3 through its N terminus". The Journal of Biological Chemistry. 278 (40): 38301–38309. doi:10.1074/jbc.M212801200. PMID 12871946.
- ^ Tang SJ, Suen TC, McInnes RR, Buchwald M (September 1998). "Association of the TLX-2 homeodomain and 14-3-3eta signaling proteins". The Journal of Biological Chemistry. 273 (39): 25356–25363. doi:10.1074/jbc.273.39.25356. PMID 9738002.
- ^ De Valck D, Heyninck K, Van Criekinge W, Vandenabeele P, Fiers W, Beyaert R (September 1997). "A20 inhibits NF-kappaB activation independently of binding to 14-3-3 proteins". Biochemical and Biophysical Research Communications. 238 (2): 590–594. doi:10.1006/bbrc.1997.7343. PMID 9299557.
- ^ Johnson BA, Stehn JR, Yaffe MB, Blackwell TK (May 2002). "Cytoplasmic localization of tristetraprolin involves 14-3-3-dependent and -independent mechanisms". The Journal of Biological Chemistry. 277 (20): 18029–18036. doi:10.1074/jbc.M110465200. PMID 11886850.
- ^ Kaplan A, Bueno M, Fournier AE (February 2017). "Extracellular functions of 14-3-3 adaptor proteins". Cellular Signalling. 31: 26–30. doi:10.1016/j.cellsig.2016.12.007. PMID 27993556.
- ^ Trimova G, Yamagata K, Iwata S, Hirata S, Zhang T, Uemura F, et al. (February 2020). "Tumour necrosis factor alpha promotes secretion of 14-3-3η by inducing necroptosis in macrophages". Arthritis Research & Therapy. 22 (1): 24. doi:10.1186/s13075-020-2110-9. PMC 7017620. PMID 32051018.
- ^ Abdelhafiz D, Kilborn S, Bukhari M (June 2021). "The role of 14-3-3 η as a biomarker in rheumatoid arthritis". Rheumatology and Immunology Research. 2 (2): 87–90. doi:10.2478/rir-2021-0012. PMC 9524784. PMID 36465971. S2CID 238231522.
- ^ Kadiri M, Charbonneau M, Lalanne C, Harper K, Balg F, Marotta A, Dubois CM (December 2021). "14-3-3η Promotes Invadosome Formation via the FOXO3-Snail Axis in Rheumatoid Arthritis Fibroblast-like Synoviocytes". International Journal of Molecular Sciences. 23 (1): 123. doi:10.3390/ijms23010123. PMC 8745703. PMID 35008549.
- ^ Abdelhafiz D, Kilborn S, Bukhari M (June 2021). "The role of 14-3-3 η as a biomarker in rheumatoid arthritis". Rheumatology and Immunology Research. 2 (2): 87–90. doi:10.2478/rir-2021-0012. PMC 9524784. PMID 36465971. S2CID 238231522.
- ^ Carrier N, Marotta A, de Brum-Fernandes AJ, Liang P, Masetto A, Ménard HA, Maksymowych WP, Boire G. Serum levels of 14-3-3η protein supplement C-reactive protein and rheumatoid arthritis-associated antibodies to predict clinical and radiographic outcomes in a prospective cohort of patients with recent-onset inflammatory polyarthritis. Arthritis Res Ther. 2016 Feb 1;18:37. doi: 10.1186/s13075-016-0935-z. PMID: 26832367; PMCID: PMC4736641.
- ^ Carrier N, Marotta A, de Brum-Fernandes AJ, Liang P, Masetto A, Ménard HA, Maksymowych WP, Boire G. Serum levels of 14-3-3η protein supplement C-reactive protein and rheumatoid arthritis-associated antibodies to predict clinical and radiographic outcomes in a prospective cohort of patients with recent-onset inflammatory polyarthritis. Arthritis Res Ther. 2016 Feb 1;18:37. doi: 10.1186/s13075-016-0935-z. PMID: 26832367; PMCID: PMC4736641.
- ^ Hirata, S., Marotta, A., Gui, Y. et al. Serum 14-3-3η level is associated with severity and clinical outcomes of rheumatoid arthritis, and its pretreatment level is predictive of DAS28 remission with tocilizumab. Arthritis Res Ther 17, 280 (2015). https://doi.org/10.1186/s13075-015-0799-7
- ^ Sornasse T, Chahal S, Gui Y, et alAB0104 CORRELATION OF PLASMA 14-3-3Η LEVELS WITH DISEASE ACTIVITY MEASURES IN METHOTREXATE-NAÏVE RA PATIENTS TREATED WITH UPADACITINIB MONOTHERAPY IN THE SELECT-EARLY PHASE 3 STUDY. Annals of the Rheumatic Diseases 2020;79:1351. | http://dx.doi.org/10.1136/annrheumdis-2020-eular.3239
- ^ Carrier N, Marotta A, de Brum-Fernandes AJ, Liang P, Masetto A, Ménard HA, Maksymowych WP, Boire G. Serum levels of 14-3-3η protein supplement C-reactive protein and rheumatoid arthritis-associated antibodies to predict clinical and radiographic outcomes in a prospective cohort of patients with recent-onset inflammatory polyarthritis. Arthritis Res Ther. 2016 Feb 1;18:37. doi: 10.1186/s13075-016-0935-z. PMID: 26832367; PMCID: PMC4736641.
- ^ Hitchon C, Smolik I, Meng X, Robinson D, El-Gabalawy HS. Serum 14-3-3eta Are Elevated in Indigenous North Americans with Rheumatoid Arthritis and May Predict Imminent Synovitis in Their at-Risk First Degree Relatives [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/serum-14-3-3eta-are-elevated-in-indigenous-north-americans-with-rheumatoid-arthritis-and-may-predict-imminent-synovitis-in-their-at-risk-first-degree-relatives/. Accessed May 5, 2022.
Further reading
- Kino T, Pavlakis GN (April 2004). "Partner molecules of accessory protein Vpr of the human immunodeficiency virus type 1". DNA and Cell Biology. 23 (4): 193–205. doi:10.1089/104454904773819789. PMID 15142377.
- Kino T, Chrousos GP (June 2004). "Human immunodeficiency virus type-1 accessory protein Vpr: a causative agent of the AIDS-related insulin resistance/lipodystrophy syndrome?". Annals of the New York Academy of Sciences. 1024 (1): 153–167. Bibcode:2004NYASA1024..153K. doi:10.1196/annals.1321.013. PMID 15265780. S2CID 23655886.
- Ichimura-Ohshima Y, Morii K, Ichimura T, Araki K, Takahashi Y, Isobe T, et al. (April 1992). "cDNA cloning and chromosome assignment of the gene for human brain 14-3-3 protein eta chain". Journal of Neuroscience Research. 31 (4): 600–605. doi:10.1002/jnr.490310403. PMID 1578511. S2CID 84930591.
- Ichimura T, Isobe T, Okuyama T, Takahashi N, Araki K, Kuwano R, Takahashi Y (October 1988). "Molecular cloning of cDNA coding for brain-specific 14-3-3 protein, a protein kinase-dependent activator of tyrosine and tryptophan hydroxylases". Proceedings of the National Academy of Sciences of the United States of America. 85 (19): 7084–7088. Bibcode:1988PNAS...85.7084I. doi:10.1073/pnas.85.19.7084. PMC 282128. PMID 2902623.
- Ichimura T, Uchiyama J, Kunihiro O, Ito M, Horigome T, Omata S, et al. (December 1995). "Identification of the site of interaction of the 14-3-3 protein with phosphorylated tryptophan hydroxylase". The Journal of Biological Chemistry. 270 (48): 28515–28518. doi:10.1074/jbc.270.48.28515. PMID 7499362.
- Jones DH, Ley S, Aitken A (July 1995). "Isoforms of 14-3-3 protein can form homo- and heterodimers in vivo and in vitro: implications for function as adapter proteins". FEBS Letters. 368 (1): 55–58. doi:10.1016/0014-5793(95)00598-4. PMID 7615088.
- Wu C, Friedlander P, Lamoureux C, Zannis-Hadjopoulos M, Price GB (September 1993). "cDNA clones contain autonomous replication activity". Biochimica et Biophysica Acta (BBA) - Gene Structure and Expression. 1174 (3): 241–257. doi:10.1016/0167-4781(93)90193-h. PMID 7690594.
- Swanson KD, Dhar MS, Joshi JG (October 1993). "The human and bovine 14-3-3 eta protein mRNAs are highly conserved in both their translated and untranslated regions". Biochimica et Biophysica Acta (BBA) - Gene Structure and Expression. 1216 (1): 145–148. doi:10.1016/0167-4781(93)90053-G. PMID 8218406.
- Leffers H, Madsen P, Rasmussen HH, Honoré B, Andersen AH, Walbum E, et al. (June 1993). "Molecular cloning and expression of the transformation sensitive epithelial marker stratifin. A member of a protein family that has been involved in the protein kinase C signalling pathway". Journal of Molecular Biology. 231 (4): 982–998. doi:10.1006/jmbi.1993.1346. PMID 8515476.
- Muratake T, Hayashi S, Ichimura Y, Morii K, Kuwano R, Ichikawa T, et al. (1996). "The effect on methamphetamine on the mRNA level for 14.3.3 eta chain in the human cultured cells". Molecular Neurobiology. 11 (1–3): 223–230. doi:10.1007/BF02740697. PMID 8561965. S2CID 20317210.
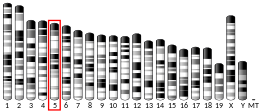
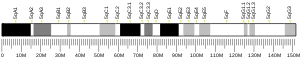
- Tommerup N, Leffers H (April 1996). "Assignment of the human genes encoding 14,3-3 Eta (YWHAH) to 22q12, 14-3-3 zeta (YWHAZ) to 2p25.1-p25.2, and 14-3-3 beta (YWHAB) to 20q13.1 by in situ hybridization". Genomics. 33 (1): 149–150. doi:10.1006/geno.1996.0176. PMID 8617504.
- Andersson B, Wentland MA, Ricafrente JY, Liu W, Gibbs RA (April 1996). "A "double adaptor" method for improved shotgun library construction". Analytical Biochemistry. 236 (1): 107–113. doi:10.1006/abio.1996.0138. PMID 8619474.
- Papin C, Denouel A, Calothy G, Eychène A (May 1996). "Identification of signalling proteins interacting with B-Raf in the yeast two-hybrid system". Oncogene. 12 (10): 2213–2221. PMID 8668348.
- Vincenz C, Dixit VM (August 1996). "14-3-3 proteins associate with A20 in an isoform-specific manner and function both as chaperone and adapter molecules". The Journal of Biological Chemistry. 271 (33): 20029–20034. doi:10.1074/jbc.271.33.20029. PMID 8702721.
- Muratake T, Hayashi S, Ichikawa T, Kumanishi T, Ichimura Y, Kuwano R, et al. (August 1996). "Structural organization and chromosomal assignment of the human 14-3-3 eta chain gene (YWHAH)". Genomics. 36 (1): 63–69. doi:10.1006/geno.1996.0426. PMID 8812417.
- Wakui H, Wright AP, Gustafsson J, Zilliacus J (March 1997). "Interaction of the ligand-activated glucocorticoid receptor with the 14-3-3 eta protein". The Journal of Biological Chemistry. 272 (13): 8153–8156. doi:10.1074/jbc.272.13.8153. PMID 9079630.
- Yu W, Andersson B, Worley KC, Muzny DM, Ding Y, Liu W, et al. (April 1997). "Large-scale concatenation cDNA sequencing". Genome Research. 7 (4): 353–358. doi:10.1101/gr.7.4.353. PMC 139146. PMID 9110174.
- Peng CY, Graves PR, Thoma RS, Wu Z, Shaw AS, Piwnica-Worms H (September 1997). "Mitotic and G2 checkpoint control: regulation of 14-3-3 protein binding by phosphorylation of Cdc25C on serine-216". Science. 277 (5331): 1501–1505. doi:10.1126/science.277.5331.1501. PMID 9278512.
- De Valck D, Heyninck K, Van Criekinge W, Vandenabeele P, Fiers W, Beyaert R (September 1997). "A20 inhibits NF-kappaB activation independently of binding to 14-3-3 proteins". Biochemical and Biophysical Research Communications. 238 (2): 590–594. doi:10.1006/bbrc.1997.7343. PMID 9299557.
- Hsu SY, Kaipia A, Zhu L, Hsueh AJ (November 1997). "Interference of BAD (Bcl-xL/Bcl-2-associated death promoter)-induced apoptosis in mammalian cells by 14-3-3 isoforms and P11". Molecular Endocrinology. 11 (12): 1858–1867. doi:10.1210/mend.11.12.0023. PMID 9369453.